Abstract
Background:
The number of elderly and the burden of non-communicable diseases increase with time. Community involvement is expected to be an important prevention agent for their neighbors. This study aimed to determine the effectiveness of health services delivered by community health workers (CHWs) which focus on physiological indices related to non-communicable diseases among elderly people and to explain the health services or interventions carried out by CHWs.
Methods:
This systematic review was conducted based on the PRISMA guidelines. PubMed, ProQuest Science Database, Scopus, EBSCOhost CINAHL, and Web of Science were taken as the source of databases. Manual search was also conducted for articles published before March 2019 without time restriction. The quality of each study was assessed using Critical Checklist by Joanna Briggs Institute.
Results:
Of the 3,275 initial studies retrieved, 4 studies were included in qualitative synthesis analysis. Three studies arranged a face-to-face interview, while the other study was conducted over the phone. All the 4 studies were intervention studies. Three of them showed a significant improvement in mean systolic blood pressure for the intervention group compared to the control group. The other study showed a significant improvement in weight loss for the intervention group.
Conclusion:
Health services delivered by CHWs was beneficial to elderly people in rural areas on some physiological indices. It suggested that health services delivered CHWs could contribute toward secondary prevention programs.
Keywords: Elderly, Lay health workers, Non-communicable disease, Remote area, Physiological index
Introduction
Aging population has been steadily increasing in the world. In 2000, 6.89% of the population were elderly, while the number increased to 8.92% in 2018 (67 million people) (1). Higher number of elderly people suggests a heavy burden of illness. In 2016, the global number of death was 56.9 million, 71% of them caused by noncommunicable diseases (NCDs), with the leading cause of death in the world was cardiovascular disease, cancer, diabetes mellitus, and chronic lung disease (2).
The WHO issued a Global Action Strategy to combat NCDs, which include increasing public and political awareness, understanding and practicing prevention, and control of NCDs. In addition, WHO also invited all sectors and stakeholders in designing and implementing the prevention of NCDs (3). The application of this strategy is with health education, psychological interventions, such as cognitive-behavioral therapy and motivational interviewing (4), and regular examination of primary health care (5). These preventive and promotion actions require a different approach between urban and rural areas. One of the challenges is the lack of availability of healthcare professionals such as doctors, nurses and other health workers in the rural area (6). Optimizing community empowerment with trained Community Health Workers (CHWs) could be a solution for providing NCD-preventive programs in the rural area (6). The involvement of CHWs is a bridge between the community and health sector (7), which becomes spearheading especially in remote areas (8). CHWs from the community have their own appeals and have attachment to each other, even though some of them doubt their competence (7). Preventive programs involving local society has proven to be cost-effective and even cost-saving in preventing cardiovascular disease (9). People also feel the ease of access to healthcare, being healthier, and being supported by joining these programs (8). Moreover, the performance of CHWs depends on the community, economy, environment, and health system policy and practice (10).
Several systematic reviews reveal the role of CHWs as community empowerment applications for both infectious disease and non-infectious disease. Studies showed that CHWs contribute to the prevention of mental disorders (11), maternal and child health (12–15), HIV (16), breast cancer (17), diabetes (18), and chronic diseases (19). Even though CHW models has been applied in various health prevention programs, no systematic review research has focus on the elderly population living in rural areas. This study focused on applying the CHW model in secondary prevention in elderly population.
We aimed to determine the effectiveness of health services delivered by CHWs for the elderly population and explain the health services or interventions carried out by CHWs. Specifically, it aimed to reveal the benefit of CHWs to the improvement of physiological index for the elderly living in rural areas.
Materials and Methods
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) guidelines (20).
Search strategy
Data were collected from 5 electronic databases, PubMed (1976 to March 2019), ProQuest Science Database (1983 to March 2019), Scopus (1977 to March 2019), EBSCOhost CINAHL (1997 to March 2019), and Web of Science (1977 to March 2019). The combination search term of keywords based on the Medical Subject Heading (MeSH) to attain the potential papers were: elderly, aged, aging, old age, older, age-old, retired, rural, remote, community health post, posyandu, community health cent*, community health service*, non-communicable disease, noncommuni-cable disease, noninfectious disease, chronic disease, heart disease, cancer, diabetes, hypertension, obes*, chronic kidney disease, chronic lung disease, stroke, and prevention. Language and years of publication were not restricted during the initial search. Additional journals were identified based on the reference list of the journals obtained and Google scholar searches. The full-text references were reviewed, and relevant cited publications that were relevant to the study’s objective were also investigated.
Study selection
The title, abstract, and full-text of the studies obtained from the literature search were independently evaluated by two reviewers (VW and FFR). The inclusion criteria were as follows: 1) types of studies: observational study, original study, or intervention study, 2) language: articles written in English, 3) types of participants: average age of participants was 60 years old or above and lived in rural areas, 4) types of exposure: had activities on community health posts that involved community health workers, and 5) types of outcomes: there was at least one physiological index or/and other outcomes related to NCDs. The exclusion criteria were as follows: 1) types of studies: systematic review, meta-analysis, literature review, review paper, protocol, abstract only publication or abstract only at symposium proceeding book, 2) types of participants: no information about living area or living in an urban area. When there were different opinions between the two reviewers, discussion will be held to seek for consensus. A third opinion (KHL) was considered if consensus could not be made between the two reviewers.
Data extraction and synthesis
For all studies included in the qualitative synthesis, the first reviewer (VW) extracted relevant data and the second reviewer (FFR) checked the accuracy independently. The following information was extracted from the selected studies: author, year of publication, region of study participants, study design, sample size, mean age of participants, gender, baseline diseases reported, health service program delivered by community health workers, duration of intervention, and findings to the physiological indices. Discrepancies were resolved through discussion between both reviewers and the third reviewer (KHL) would be involved to make decision if necessary. All the data were recoded and documented in Microsoft Excels.
Quality Assessment
To assess the quality of each analyzed study, we used the Critical Checklist established by the Joanna Briggs Institute (JBI) which was adjusted to the study design. JBI critical appraisal checklists have 13 items for the randomized control trial study and 9 items for the quasi-experimental study. Each item of the checklist was evaluating with “yes,” “no,” “unclear,” and “not applicable” (21). Any disagreement was resolved by discussion between reviewers.
Statistical analysis
Cohen’s Kappa statistic was calculated to measure the agreement between two reviewers on the study selection and quality assessment. The interpretation of Kappa is as follow: a value ≤ 0 suggests no agreement, 0.01–0.20 suggests none to slight, 0.21–0.40 suggests fair, 0.41–0.60 suggests moderate, 0.61–0.80 suggests substantial, and 0.81–1.00 suggests very well to almost perfect agreement (22). Statistical analysis was performed using IBM SPSS (Chicago, IL, USA) Statistics 22.
Results
Study selection
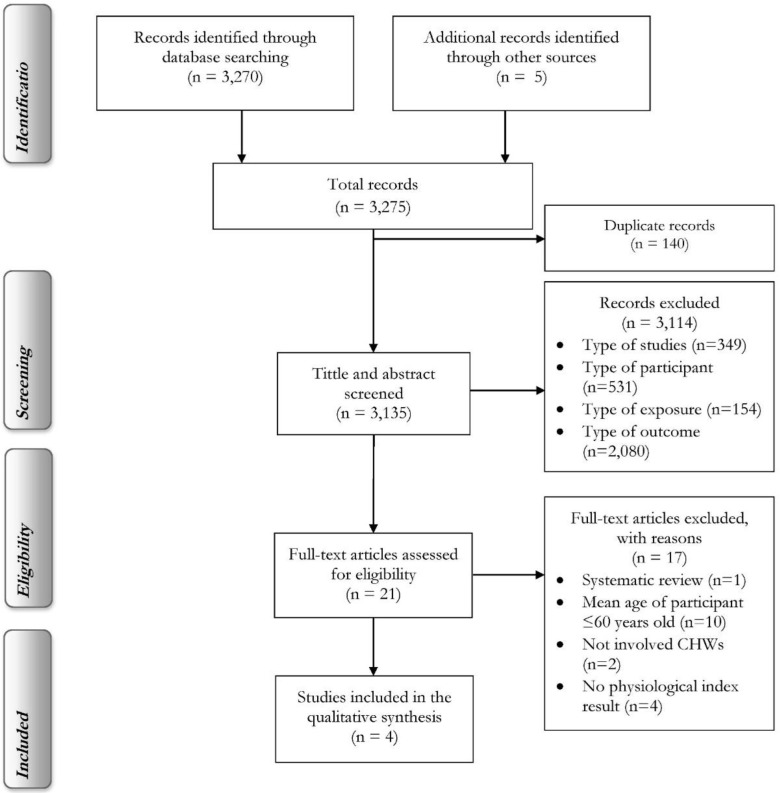
The total number of articles after initial screening was 3,275, including 3,270 extracted from the 5 electronic databases and 5 manually identified through other sources. After removing duplications, the number of articles carried out to screening the title and abstract was 3,134. After further screening the title and abstract as well as the full text, there were 4 studies included in the qualitative synthesis. Detailed information about the review process was shown in Fig. 1. The agreement between the two independent reviewers for screening title and abstract was quite good (Kappa 0.80, P-value <0.001), while full-text screening and quality assessment were also very well (Kappa 0.86 with P-value <0.001 and Kappa 1.00 with P-value <0.001, respectively). All the selected studies fulfilled the quality assessment criteria.
Fig. 1:
PRISMA Flow diagram of study selection process
Study characteristics
The characteristics of the included studies are presented in Table 1. The year of publication of the included studies ranged between 2011 and 2016. Regard to the study setting, 1 study recruited participants from China and India (23), 1 study recruited from Uganda (24), and 2 studies recruited from the United States (25,26). Three studies used experimental study design (23,25, 26) and the remaining one was a quasi-experimental study (24).
Table 1:
Study characteristics of the included studies
| No | First Author, (yr) | Country | Study design | Sample Size | Mean Age (yr old) | Gender |
|---|---|---|---|---|---|---|
| 1 | Tian et al (2015) (23 ) | China and India | Experimental study, cluster-randomized controlled trial | 47 villages (27 in China and 20 in India), 2086 individuals, 1095 intervention and 991 control | Intervention=59.7, control=60.4, total=60.0 | Female: intervention=65.4%, control=66.8% |
| 2 | O’Neil et al (2016) (24 ) | Uganda | Retrospective, quasi-experimental study design | 209 individuals, 93 intervention and 116 control | Intervention=64.1, control=60.1, total=61.9 | Female: intervention=84.1%, control=74.3% |
| 3 | Margolius et al (2012) (25 ) | United States | Experimental study | 204 individuals, 110 intervention and 94 control | Intervention=60.7, control=60.1, total=60.4 | Female: intervention=62.7%, control=63.8% |
| 4 | West et al (2011) (26 ) | United States | Experimental study | 228 individuals, 116 intervention and 112 control | Intervention=70.6, control=71.9, total=71.2 | Female: intervention=91.0%, control=77.0% |
Participants’ characteristics
The total number of participants in the four studies was 2,727, in which 1,405 participants belonged to the intervention group and 1,322 belonged to the control group (23–26). The average age range in the 4 studies was from 60.03 to 71.20 years. More than 60% participants in the studies were females. Some participants reported a history of hypertension (the prevalence ranged from 76.0% to 100.0%), diabetes (11.6–33.3%) (23–25), heart disease (2.4–35.9%) (23,24), obesity (8.3–100.0%) (23,26), stroke (10.2%) (23), asthma/COPD (1.4%), and epilepsy (0.5%) (24).
Community Health Workers program
Details of the health service program in each study were summarized in Table 2. As shown, three studies arranged a face-to-face interview at the clinic, in the village, or at home (23,24, 26), and the other study was conducted over the phone (25). Only one study relied on mobile technology-based electronic decision support system (EDSS) (23). Regard to the follow-up pattern, half studies took a monthly follow-up strategy (23,24), while the other half used weekly follow-up (25). The measure outcomes in these studies were diverse. One study conducted screening for new symptoms, diseases, and side effects since the last visit, measured blood pressure, provided lifestyle counseling, and, when appropriate, prescribed required medications (23). Another study recorded clinical evaluation for each patient using a disease-specific scripted examination (24). The third study focused on overall well-being, adherence to action plans, and blood pressure values (25). The last study reviewed dietary intake and physical activities (26). The intervention durations of these studies were 4 months (26), 6 months (25), at least 6 months (24), and 1 year (23).
Table 2:
Summary of the included studies for systematic review
| No. | First Author, (Yr) | Baseline disease reported | Community Health Workers program | Duration of intervention | Findings of physiological index |
|---|---|---|---|---|---|
| 1 | Tian et al (2015) (23 ) | Hypertension, Coronary Heart Disease, Stroke, Diabetes | CHWs were instructed to provide monthly follow-up visits for the high-risk participants used mobile technology-based electronic decision support system (EDSS) (the Simplified Cardiovascular Manage-ment Study [SimCard]). The CHWs job desk was screening for new symptoms, diseases, and medication side effects, measuring blood pressure, providing life-style counseling, and, when appropriate, prescribing medications. | 1 yr | Mean systolic blood pressure (SD); Intervention group: Pre 161.3 (29.6)mmHg, Post 149.5 (26.1) mmHg; Control group: Pre 161.4 (27.8)mmHg, Post 152.3(27.2) mmHg; Net difference=−2.7, P-value=0.04 Others outcome related NCDs prevention: Anti-hypertensive medication; Net difference= 25.5%, P-value=<0.001 Use of aspirin; Net difference=17.1%, P-value=<0.001 |
| 2 | O’Neil et al (2016) (24 ) | Hypertension, Asthma/COPD, Diabetes, Heart failure, Epilepsy | Chronic Disease in the Community program decentralized chronic disease care by transferring many clinical responsibilities to CHWs. Specially trained CHWs hold monthly meetings in their home villages in the presence of a clinician supervisor from a district hospital. At these meetings, the CHWs record a clinical evaluation of each patient using a disease-specific scripted examination. Thirty days of individually packaged medication from the district hospital supervisor are received on the day of the meeting and are delivered following the evaluation. | >6 months | Mean systolic blood pressure; Intervention group: 147.8 (144.3–151.3) mmHg; Control group: 156.7(153.2–156.7)mmHg, P-value=0.001 |
| 3 | Margolius et al (2012) (25 ) | Hypertension, Diabetes | Clinicians of patient completed an algorithm of antihypertensive medication adjustments. Health coaches (CHWs) made weekly telephone calls to participants to discuss overall well-being, adherence to action plans, and blood pressure values. Patients who reported systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg and excellent medication adherence could choose to increase their antihypertensive medication regimen according to the algorithm without a clinician appointment. | 6 months | Mean systolic blood pressure; Intervention group: Pre 160.3mmHg, Post 136.4mmHg; Control group:Pre 158.2mmHg, Post 136.4mmHg; Net difference=−4.6, P-value=not significant; Mean diastolic blood pressure, Intervention group: Pre 85.1mmHg, Post 79.2mmHg; Control group: Pre 86.9mmHg, Post 81.5mmHg; Net difference=−0.5, P-value=not significant |
| 4 | West et al (2011) (26 ) | Obesity | Coaches (CHWs) reviewed the record of dietary intake and physical activity weekly. Then, returned it to the elderly with feed-back to reinforce behavior changes and identify targets for additional modification. Every week the elderly learns about behavioral strategies, self-monitoring, stimulus control, problem-solving, goal setting, and relapse prevention to support habit change. Group sessions duration about 60 minutes delivered by the CHWs. | 4 months | Average weight loss, Intervention group reduced 3.7 kg compared with an average of 0.3 kg in the control arm. After adjusting for baseline weight, BMI, and gender, participants in the intervention arm had a 9.7 times higher odds (95%CI, 3.5–26.8) of achieving ≥5%weight reduction as compared to those in the control arm (P<.001 ). |
Physiological index
Three studies evaluated the difference in mean systolic blood pressure (SBP) between the intervention and the control groups (23–25) and one of them compared the mean diastolic blood pressure (DBP) additionally (25), while the other study evaluated weight loss instead (26). Results in two studies showed that the intervention group had a better improvement on SBP than the control group (23,24). The other study also showed a better improvement on SBP and DBP (25), however, they were not significant. The last study presented that the intervention group had a greater weight lost (3.7±3.7 kg) compared to the control group after intervention (26).
Other outcomes related to NCDs
Only one among the four studies included other outcomes beyond physiological index (23). The study investigated the differences in the use of aspirin and anti-hypertensive medications between the intervention and the control groups. It showed that the intervention group had a better improvement on both outcomes and achieved statistically significance level.
Discussion
Our study suggested that the existence of CHWs in giving health services in the elderly could enhance the elderly’s physiological index in rural area. While all the participants enrolled in the four studies had at least one NCD before the intervention programs, all the studies showed significant improvements in systolic blood pressure, diastolic blood pressure, or body weight after the intervention. Thus our finding made the evidence stand out that the lay services on prevention program could be benefit on the level of secondary prevention. Even though different methods and study durations were adopted to deliver the intervention, the outcomes are still impressive.
The most important determinant of the success of CHWs is the desire of the community participation to help their neighbors. The existence of CHWs is a solution to the access to health center problems, especially in areas with the special geographical condition and utilizing social-emotional closeness between citizens to encourage each other to improve health level. The support system, such as government support, good program management, continuing education, and infrastructure support is the success key factors of this program (27). Another advantage possessed by CHWs is conveying health messages using local languages, so the messages given are at low risk of misunderstanding (28).
Various terms are used to refer to CHWs, such as Shasthyo Sebika (Bangladesh), Accompagnateurs (Haiti), Community Health Volunteer or Village Health Guide (India), Behvarz (Iran), Kader Posyandu (Indonesia), and Rural Health Worker (Guatemala) (29). Despite having various terms, the core of CHW is community empowerment in the health sector. WHO defines CHW as “Community health workers should be members of the communities where they work, should be selected by the communities, should be answerable to the communities for their activities, should be supported by the health system but not necessarily a part of its organization, and have shorter training than professional workers.” (27).
According to Olaniran et al, basically there are 3 types of CHWs: lay health workers, level 1 paraprofessional, and level 2 paraprofessionals. From the base level, lay health workers usually only get informal education, but sometimes they get little formal education training. Level 1 paraprofessionals refer to people who get short formal education training, where level 2 paraprofessionals have longer training than level 1 paraprofessionals (30). All of the CHWs in this study were at the base level of the CHWs. The CHWs get trained before the research runs. The CHWs’ role varied in these studies, from making phone calls (25) to being allowed to prescribe drugs (24).
Our study had many limitations. First, due to the language barriers of the researchers, publication bias may occur. Studies using native term/language for CHWs were not included. We tried to minimize this problem by not limiting language in the initial search. Second, our study used the United Nations’ standard numerical criteria to define the elderly and the cut of the point was age more than 60 years old (31). However, some studies only used age range. Therefore, we decided to use mean age of 60 years old as a benchmark for the definition of the elderly. Third, the focus of this paper was on secondary prevention because elderly population are rarely free of chronic diseases. This made our study a little unfocused because each participant had a different disease history. Fourth, various duration and types of interventions made it hard to fairly compare the programs carried out by CHWs. Fifth, the results were not a good representative for NCDs prevention programs carried out by CHWs globally, since only 4 studies remained after the screening criteria.
Conclusion
The involvement of CHWs in delivering health services especially in the elderly was proven to improve physiological index, especially on blood pressure and weight, for the elderly with NCDs in the rural area. Although intervention program from each study was different, it still had a positive impact on NCDs prevention. We suggested that further research is needed due to the limitation of this study.
Health services delivered by community health workers is beneficial to elderly people in rural areas. The improvement was essentially on physiological index, including blood pressure and weight. It suggested that health services delivered by CHWs could play an important role in a secondary prevention program. However, due to the limitation of this study, further studies are required to confirm the results.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This study was supported in part by the Ministry of Science and Technology of Taiwan under grant number: MOST 109-2410-H-468-017 to JYW.
Footnotes
Conflict of interest
Non-declared.
References
- 1.The World Bank (2019). Population ages 65 and above (% of total population).Available from: https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS
- 2.World Health Organization (2019). NCD mortality and morbidity. Available from: https://www.who.int/gho/ncd/mortality_morbidity/en/
- 3.World Health Organization (2013). Global Health Action For The Prevention And Control Of Noncommunicable Diseases 2013–2020. WHO Document Production Services, Switzerland, pp 3–5. [Google Scholar]
- 4.Low W, Lee Y, Samy AL. (2015). Non-Communicable Diseases In The Asia-Pacific Region: Prevalence, Risk Factors and Community-Based Prevention. Int J Occup Med Environ Health, 28 (1): 20–6. [DOI] [PubMed] [Google Scholar]
- 5.Alwardat N, Di Renzo L, de Miranda RC, et al. (2018). Association between hypertension and metabolic disorders among elderly patients in North Jordan. Diabetes Metab Syndr, 12 (5): 661–666. [DOI] [PubMed] [Google Scholar]
- 6.Jeet G, Thakur JS, Prinja S, Singh M. (2017). Community health workers for noncommunicable diseases prevention and control in developing countries: Evidence and implications. PLoS One, 12 (7): e0180640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kok MC, Ormel H, Broerse JEW, et al. (2017). Optimising the benefits of community health workers ’ unique position between communities and the health sector: A comparative analysis of factors shaping relationships in four countries. Glob Public Health, 12 (11): 1404–32. [DOI] [PubMed] [Google Scholar]
- 8.Rahmawati R, Bajorek B. (2015). A community health worker-based program for elderly people with hypertension in Indonesia: A qualitative study. Prev Chronic Dis, 12: E175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaziano T, Abrahams-Gessel S, Surka S, et al. (2015). Cardiovascular disease screening by community health workers can be cost-effective in low-resource countries. Health Aff (Millwood), 34 (9): 1538–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kok MC, Kane SS, Tulloch O, et al. (2015). How does context influence performance of community health workers in low- and middle-income countries? Evidence from the literature. Health Res Policy Syst, 13: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mutamba BB, Ginneken N, Van Paintain LS, et al. (2013). Roles and effectiveness of lay community health workers in the prevention of mental, neurological and substance use disorders in low and middle income countries: a systematic review. BMC Health Serv Res, 13:412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duncan MS, Duncan BB. (2011). Effectiveness of community health workers in Brazil. J Ambul Care Manage, 34 (4): 326–38. [DOI] [PubMed] [Google Scholar]
- 13.Gogia S, Singh H. (2010). Home visits by community health workers to prevent neonatal deaths in developing countries: A systematic review. Bull World Health Organ, 88(9): 658–666B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewin S, Munabi-Babigumira S, Glenton C, et al. (2010). Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev, 2010(3):CD004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gilmore B, Mcauliffe E. (2013). Effectiveness of community health workers delivering preventive interventions for maternal and child health in low- and middle-income countries: A systematic review. BMC Public Health, 13:847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mwai GW, Mburu G, Torpey K, et al. (2013). Role and outcomes of community health workers in HIV care in sub-Saharan Africa: A systematic review. J Int AIDS Soc, 16(1):18586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wells KJ, Luque JS, Miladinovic B, et al. (2011). Do community health worker interventions improve rates of screening mammography in the United States? A systematic review. Cancer Epidemiol Biomarkers Prev, 20 (8): 1580–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palmas W, March D, Darakjy S, et al. (2015). Community health worker interventions to improve glycemic control in people with diabetes: A systematic review and meta-analysis. J Gen Intern Med, 30 (7): 1004–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim K, Choi JS, Choi E, et al. (2016). Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: A systematic review. Am J Public Health,106 (4): e3–e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med, 6 (7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joanna Briggs Institute (2019). Critical Appraisal Tools. https://jbi.global/critical-appraisal-tools
- 22.Mchugh ML. (2012). Lessons in biostatistics interrater reliability: the kappa statistic. Biochem Med (Zagreb), 22(3): 276–82. [PMC free article] [PubMed] [Google Scholar]
- 23.Tian M, Ajay VS, Dunzhu D, et al. (2015). A cluster-randomized, controlled trial of a Simplified Multifaceted Management Program for Individuals at high cardiovascular risk (SimCard trial) in rural Tibet, China, and Haryana, India. Circulation, 132(9): 815–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Neil DS, Lam WC, Nyirangirimana P, et al. (2016). Evaluation of care access and hypertension control in a community health worker driven non-communicable disease programme in rural Uganda: the chronic disease in the community project. Health Policy Plan, 31 (7): 878–83. [DOI] [PubMed] [Google Scholar]
- 25.Margolius D, Bodenheimer T, Bennett H, et al. (2012). Health coaching to improve hypertension treatment in a low-income, minority population. Ann Fam Med, 10 (3): 199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.West DS, Bursac Z, Cornell CE, et al. (2011). Lay health educators translate a weight-loss intervention in senior centers: a randomized controlled trial. Am J Prev Med, 41 (4): 385–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lehmann U, Sanders D. (2007). Community health workers: what do we know about them? The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers. Geneva: World Health Organization, 1–42. [Google Scholar]
- 28.Tulenko K, Møgedal S, Afzal M, et al. (2013). Community health workers for universal health-care coverage: from fragmentation to synergy. Bull World Health Organ, 91: 847–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhutta ZA, Lassi ZS, Pariyo G, Huicho L. (2010). Global experience of community health workers for delivery of health related millennium development goals: a systematic review, country case studies, and recommendations for integration into national health systems. [Google Scholar]
- 30.Olaniran A, Smith H, Unkels R, Bar-zeev S. (2017). Who is a community health worker? – a systematic review of definitions. Glob Health Action, 10 (1): 1272223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kowal P, Dowd JE. (2001). Definition of an older person. Proposed working definition of an older person in Africa for the MDS Project. World Health Organization, 10 (2.1): 5188–9286. [Google Scholar]