Abstract
Purpose:
To describe the characteristics and incidence of children developing endophthalmitis within the first 90 days following pediatric cataract surgery.
Setting:
De-identified commercial and Medicare Advantage health claims across the United States.
Design:
Population-based retrospective cohort study.
Methods:
In a retrospective review of approximately 58 million charts in Optum’s de-identified Clinformatics® Data Mart Database, we identified patients <13 years of age who underwent cataract surgery in one or both eyes with or without primary intraocular lens implantation (IOL) between 2003 and 2017. We excluded patients with traumatic cataract, <90 days of continuous insurance coverage, a prior diagnosis of endophthalmitis, and a diagnosis of endophthalmitis occurring after 90 days of cataract surgery. The main outcome measure was the incidence of endophthalmitis occurring within the first 90 days of cataract surgery and the odds ratio for developing endophthalmitis according to demographic and intraoperative factors.
Results:
Cataract surgery was performed on 789 eyes (52.6% male) with a median age of 4 (IQR 1 to 8) years. Rate of IOL implantation at the time of cataract surgery was 66.8%. Endophthalmitis was diagnosed in 4 eyes (0.51%). Median time to diagnosis of endophthalmitis was 6.5 days (Range: 5 to 44 days). There was no significant association between endophthalmitis and age, sex, or primary IOL implantation.
Conclusion:
In this large insurance claims database, we report an incidence of endophthalmitis following pediatric cataract surgery that is more than the rate previously reported by any study with patients of a similar age.
INTRODUCTION
One of the most feared complications after cataract surgery is endophthalmitis, which has been reported to be more common and visually significant in children than in adults.1 The incidence of endophthalmitis following pediatric cataract surgery is not well known due to the small number of cases and rarity of these particularly severe postoperative events. In adults, the incidence of endophthalmitis after cataract surgery has been reported to be between 0.02% and 0.2%, and the rate has declined over time.2–9 A better understanding of the incidence and risk factors of these complications in children through a large-scale study would inform cataract surgeons and families of the risks of surgery, as well as influence the postoperative surveillance of these conditions. In this study, we determined the incidence of endophthalmitis reported in the first 90 days following cataract surgery (defined as lensectomy with or without the implantation of intraocular lens [IOL]) and evaluated the possible risk factors for endophthalmitis in children younger than 13 years of age using a large, administrative claims database.
METHODS
Study Design and Data Source:
This study was a population-based retrospective cohort study using claims data from Optum’s de-identified Clinformatics® Data Mart Database.10 The CDM Database (OptumInsight, Eden Prairie, MN) is a de-identified commercial and Medicare Advantage health claims database. The database includes approximately 17–19 million annual covered lives, for a total of over 57 million unique lives and includes encounters from a 15-year period (January 2003 through December 2017). The population is geographically diverse, spanning all 50 states. The CDM Database is statistically de-identified under the Expert Determination method consistent with HIPAA and managed according to Optum customer data use agreements. These administrative claims submitted for payment by providers and pharmacies are verified, adjudicated, adjusted, and de-identified prior to inclusion. In addition to medical data from inpatient and outpatient facilities for all ocular and non-ocular conditions, sociodemographic information on age, sex, race/ethnicity, and household income of each enrollee is included as well. Participating physicians in the database reported every encounter with every patient seen at their practices. All diagnoses associated with a patient in the electronic health records were included.
Data access for this project was provided by the Stanford Center for Population Health Sciences (PHS) Data Core. The PHS Data Core is supported by a National Institutes of Health (NIH) National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and internal Stanford funding. The content is solely the responsibility of the authors and does not represent the official views of the NIH. The Stanford University School of Medicine Institutional Review Board approved this as a non-regulated study as the data were previously collected and de-identified.
Study Sample Determination:
The database was screened to identify children younger than 13 years of age who were diagnosed with cataract as defined by the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) and International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes listed in Supplemental Table 1. Cataract diagnoses that are associated with trauma were not included. Of the children identified with cataracts, those who underwent cataract surgery were identified, and those who underwent concurrent vitrectomy at the time of surgery were also identified by relevant Current Procedural Terminology (CPT) codes (Table 1). Cases of endophthalmitis were identified by the ICD-9-CM or ICD-10-CM codes for endophthalmitis listed in Supplemental Table 2 and confirmed as a true case of endophthalmitis by a concurrent CPT code of intravitreal aspiration, intravitreal injection, or vitrectomy within 7 days of the ICD code of endophthalmitis (Table 1). Children were excluded if they were identified as having an ICD code for endophthalmitis or panuveitis prior to or on the date of cataract surgery. They were also excluded if they had an ICD code for endophthalmitis or panuveitis more than 90 days after cataract surgery. Children were further excluded if they did not have at least 90 days of continuous enrollment in their health plan following cataract surgery unless they had a diagnosis of endophthalmitis prior to the discontinuation of their health plan coverage and met all other inclusion criteria. In order to most accurately attribute a complication to the eye undergoing cataract surgery, children with bilateral sequential cataract surgeries were excluded if they occurred within 90 days of each other.
Table 1.
Current Procedural Terminology (CPT) Codes Used for Study Sample Determination
| Procedure | CPT Code |
|---|---|
| Cataract Surgery | 66982, 66984, 66920, 66930, 66940, 66850, 66840, 66852 |
| Vitrectomy | 67005, 67010, 67030, 67036, 67039, 67041, 67042, 67043 |
| Vitreous Aspiration | 67015 |
| Intravitreal Injection | 67028 |
Outcomes and variables:
The primary outcome of interest was the incidence of endophthalmitis within 90 days among eyes that underwent cataract surgery performed in the United States. Secondary outcomes were to determine the risk factors for developing endophthalmitis within 90 days of surgery based upon baseline demographic factors (age at time of cataract surgery, sex, race, and household income), intraoperative factors (primary intraocular lens implantation and anterior vitrectomy at time of cataract surgery), and comorbid factors (intellectual disability and dermatitis). Primary intraocular lens (IOL) placement (pseudophakia) was determined by the presence of CPT code 66982 and 66984 on the day of cataract surgery, while no primary IOL placement (aphakia) was determined by the presence of CPT code 66920, 66930, 66940, 66850, 66840, and 66852 on the day of cataract surgery. Vitrectomy at the time of cataract surgery was determined by the presence of vitrectomy CPT codes listed in Table 1 on the day of cataract surgery. The diagnosis codes for the comorbid conditions of interest are listed in Supplemental Table 3.
Statistical Analysis:
Descriptive statistics of the study sample were summarized as frequencies and percentages for categorical variables and median and interquartile range (IQR) for continuous variables. Univariable and multivariable logistic regression models were used to determine the extent to which demographic factors, intraoperative factors, and comorbid factors affected the odds of developing endophthalmitis within 90 days of cataract surgery. A multivariable model for endophthalmitis was created with the cofactors of age, sex, race, and pseudophakia, which were chosen a priori based upon clinical suspicion. Anterior vitrectomy during lensectomy, intellectual disability, and dermatitis were potential covariates of interest for our models, but due to too few instances of children with such characteristics developing our outcome of interest, these cofactors were excluded from our multivariable models. Race and household income were also excluded from multivariable analyses due to unknown values for these variables. Analyses performed were 2-sided, and an alpha of 0.05 was considered to indicate statistical significance. Statistical analyses were performed using Stata software version 16 (Stata Corp., College Station, TX).
RESULTS
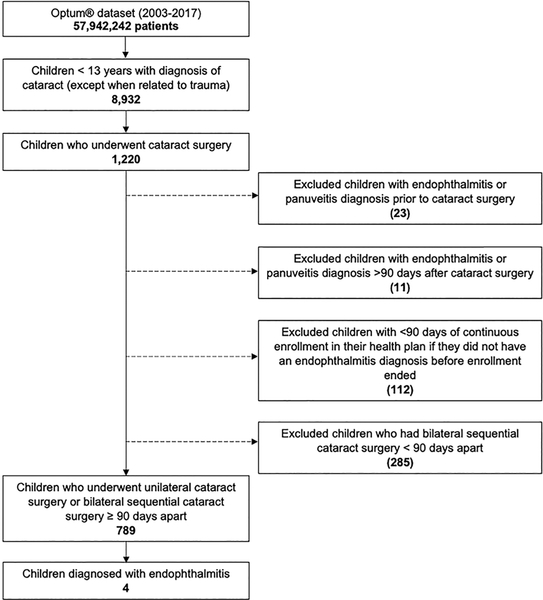
Figure 1 shows the patient selection process for inclusion in this study. Of the nearly 58 million patients screened in the Optum database, 8,932 children younger than 13 years of age were identified as having a diagnosis of cataract unrelated to trauma. Of these children, 1,220 underwent cataract surgery. Twenty-three children were excluded on the basis of having a diagnosis of endophthalmitis (7 patients) or panuveitis (16 patients) on or prior to the date of cataract surgery, and an additional 11 were excluded for having a diagnosis of endophthalmitis (7 patients) and panuveitis (4 patients) greater than 90 days after cataract surgery. Of the children remaining, 112 were excluded for not having at least 90 days of continuous enrollment in their health plan following cataract surgery unless they had a diagnosis of endophthalmitis before end of their enrollment. Finally, 285 children were excluded for having had bilateral cataract surgery less than 90 days apart. Ultimately, 789 children remained in our study cohort.
Figure 1.
Flow Diagram Illustrating Inclusion and Exclusion Criteria for the Study Sample
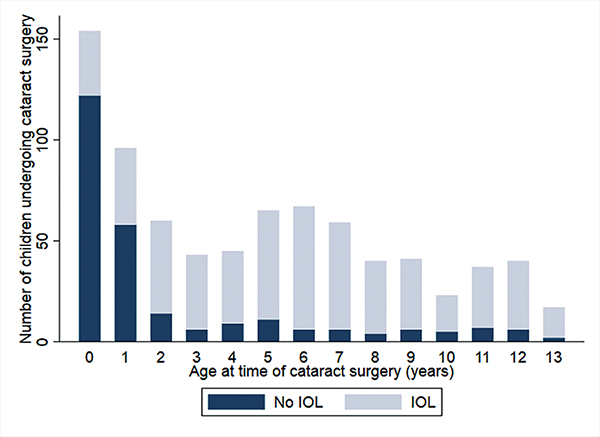
Baseline characteristics of our study cohort are shown in Table 2. Among the 789 children included, 416 (52.7%) were male, 522 (66.2%) were white, 89 (11.4%) Latino, 59 (7.5%) black, 28 (3.6%) Asian, and 91 (11.4%) were not known or did not fit into the above categories. Of those with reported household income, 36.2% children came from households with incomes greater than $100,000. The median age at cataract surgery was 4 years (IQR 1–8 years). Five-hundred and twenty-seven (66.8%) children in the study sample received a primary IOL, with IOL implantation frequency increasing from 76 of 252 (30.2%) children 12 months of age or younger to 451 of 537 (84.0%) children receiving IOL implantation after 12 months of age. Figure 2 shows the age distribution that children received a primary IOL at time of cataract surgery. Other descriptive statistics of our study sample are summarized in Table 2.
Table 2.
Descriptive Characteristics of Study Cohort
| Patient Characteristic | All Children (n = 789) |
|---|---|
| Demographics | |
| Male sex | 416 (52.7) |
| Race/Ethnicity | |
| White | 522 (66.2) |
| Latino | 89 (11.3) |
| Black | 59 (7.5) |
| Asian | 28 (3.6) |
| Unknown | 91 (11.5) |
| Age in years at surgery, median (IQR) | 4 (1, 8) |
| Income | |
| <$40,000 | 57 (7.24) |
| $40-$99,000 | 170 (21.5 |
| >$100,000 | 285 (36.2) |
| Unknown | 277 (35.2) |
| Intraoperative factors | |
| Primary IOL implant | 527 (66.8) |
| Anterior vitrectomy at lensectomy | 205 (26.0) |
| Comorbid factors | |
| Intellectual disability | 56 (7.2) |
| Dermatitis | 4 (0.5) |
IOL = intraocular lens; IQR = interquartile range
Figure 2.
Frequency of Cataract Surgery (n = 789) by Age in Years Stratified by IOL (n = 531) vs No IOL Placement (n = 258) at Time of Surgery
Of the 789 eyes that underwent cataract surgery performed between 2003 and 2017, 4 (0.51%) developed endophthalmitis within 90 days of surgery. Three of the affected children were male, and one was female. Median age of the cases was two years (range <1 to 6 years). None of these children had documented intellectual disability or dermatitis at or before the time of cataract surgery. The median time to develop endophthalmitis was 6.5 days (range 5 to 44 days).
No variables were statistically significantly associated with endophthalmitis in univariable logistic regression analysis. In a multivariable logistic regression model controlling for age, sex, race, and pseudophakia, there were no statistically significant associations with endophthalmitis (Supplemental Table 4).
DISCUSSION
Endophthalmitis following pediatric cataract surgery is difficult to study due to the rarity of cataract surgery in this population. Our current understanding of the rate of complications has relied primarily upon large retrospective studies. The CDM Database allows for evaluation of the rare but serious occurrences of complications such as postoperative endophthalmitis in a real-world, contemporary cohort that is not at risk of selection bias. The race distribution of our cohort is similar to that of the overall population of the United States.11
We reported the incidence of endophthalmitis to be 0.51% among the eyes of children under 13 years of age within 90 days of undergoing cataract surgery. Studies published in prior decades report the incidence of endophthalmitis as ranging from 0%12,13 to 0.45%.14 These studies were performed largely before modern techniques for cataract surgery were routinely adopted, such as the use of intracameral antibiotics and small-gauge cutting devices, thus making them likely less to be generalizable to our practices today. More recently, studies have included greater cohort sizes, as shown in Table 3. Two recent studies focusing on infants are the Infant Aphakia Treatment Study (IATS) in the United States15 and the IoLunder2 cohort study in the British Isles.16 The IATS is the only large-scale cataract surgery randomized controlled trial to date that prospectively studied 114 cataract surgeries with and without primary IOL implantation between 2004 and 2009. They reported a 0.9% incidence of endophthalmitis in their cohort of infants 6 months of age and younger. Although the IATS focused exclusively on infants, their prospective study was designed with enrollment occurring prior to cataract surgery date which allowed for the full capture of the incidence of complications. The IoLunder2 study group also prospectively investigated outcomes following cataract surgery with and without primary IOL implantation between 2009 and 2010 in children under 2 years of age. They found no cases of endophthalmitis among 350 operated eyes. Agarkar et. al. retrospectively reported a rate of endophthalmitis of 0.38% over a period of 12 years (2000–2012) in children 14 years of age or younger in a single-surgeon study of 2,390 cataract surgeries.17 Another recent, large-scale prospective study by the Pediatric Eye Disease Investigator Group (PEDIG) reported one case of endophthalmitis (incidence rate 0.09%) among children younger than 13 years of age in a multi-center study of 1,132 cataract surgeries (2016–2018).18 Eibenberger et. al. retrospectively examined 220 eyes of children less than 18 years old undergoing cataract surgery between 2003 and 2018 and reported 1 case of endophthalmitis (incidence rate 0.45%) which occurred after initial cataract surgery and another case which occurred after vitrectomy for visual axis opacification.19 Most recently, Pershing et. al. published on the rates of endophthalmitis among patients ages 0 to over 85 years whose surgeons participated in the American Academy of Ophthalmology Intelligent Research in Sight (IRIS) Registry.9 They concluded that the youngest subgroup of patients (aged 0 to 17 years) had the highest incidence rate of endophthalmitis of 0.37% in cases performed between 2013 and 2017.20
Table 3.
Studies Reporting Endophthalmitis Incidence Following Pediatric Cataract Surgery Published Since the Year 2000
| Study | Study Design | Ages studied | Years Studied | Follow-Up Period | No. of cases | No. of surgeries | Incidence of Endophthalmitis | Timing of Endophthalmitis |
|---|---|---|---|---|---|---|---|---|
| IATS (2010) | Prospective trial | ≤ 6 months | 2004 – 2009 | 1 year | 1 | 114 | 0.9% | Not reported |
| IoLunder2 (2015) | Prospective cohort | ≤ 2 years | 2009 – 2010 | 5 years | 0 | 350 | 0% | -- |
| Agarkar et. al. (2016) | Retrospective, case series | ≤ 14 years | 2000 – 2012 | 4.5 years (median) | 9 | 2,390 | 0.38% | 2.5 days (median), 1 case at 27 days |
| PEDIG (2019) | Prospective cohort | ≤ 13 years | 2016 – 2018 | 1 year | 1 | 1,132 | 0.09% | 9 months |
| IRIS Registry (2020) | Retrospective cohort | ≤ 17 years | 2013 – 2017 | 5 years | 21 | 5,648 | 0.37% | No reported |
| Eibenberger et. al. (2020) | Retrospective case series | ≤ 17 years | 2003 – 2018 | 5.74 years (median) | 1 | 220 | 0.45% | 9 days |
| Optum Database* | Retrospective, claims based | ≤ 13 years | 2003 – 2017 | 90 days | 4 | 789 | 0.51% | 6.5 days |
Indicates the present study
We found a higher rate of endophthalmitis within our cohort compared to all of these aforementioned studies with the exception of the IATS, which was the only other study to only include infants.9,12–14,18 While the incidence of endophthalmitis in our study cannot be directly compared to the rate of endophthalmitis in prior studies due to differences in patient selection and study design, our cohort presents a mixed-race cohort from the United States similar to that of the IATS, IoLunder2, PEDIG, and IRIS registry studies, while the study by Agarkar was predominantly of Asian race17 and race in the study by Eibenberger19 was not reported. While we are unable to compare detailed surgical techniques and antiseptic practices between our study and prior studies, our study as well as these prior studies were similarly inclusive of children who underwent both IOL implantation and no IOL implantation, and anterior vitrectomy as well as no anterior vitrectomy at the time of surgery. One reason behind our higher incidence of endophthalmitis may be that our data derives from surgeons with varying levels of experience in performing pediatric cataract surgery, whereas prior studies derived subjects from high-volume centers for pediatric cataract surgery with likely highly experienced surgeons. Our rate may have been higher than the rate reported by the IoLunder2 and PEDIG studies due to their prospective study design, may have led to selection bias against reporting cases that resulted in endophthalmitis. For example, in the IoLunder2 study, surgeons voluntarily reported their cataract cases through monthly reporting cards and may have been reluctant to report on cases with poor outcomes. Similarly, the PEDIG study was a registry study which allowed enrollment to start up to 45 days after cataract surgery; therefore, this study may similarly be subject to selection bias in which surgeons may not have chosen to enroll their cases which resulted in endophthalmitis. Conversely, we retrospectively included all coded claims of endophthalmitis that occurred between 1- and 90-days post cataract surgery, thus precluding the potential for selection bias against enrolling children who develop an early complication.
In the adult population, the rates of endophthalmitis have been decreasing over time as demonstrated by large national registries and insurance databases.21,22 The decreased rates are likely related to the safety and effectiveness of intracameral antibiotics published by groups starting in 2006.23,24 Given the increasing adoption of intracameral antibiotics by pediatric ophthalmologists as reported in a survey by Gharaibeh et. al.,1 one might expect a lower rate of postoperative endophthalmitis over time. However, we found that cases of endophthalmitis occurred throughout our 14-year study period. Further longitudinal evaluation using our data source needs to be conducted to comment on whether rates of endophthalmitis are changing over time in children after cataract surgery.
The median time from cataract surgery to development of endophthalmitis was 6.5 days (range 5–44 days), which is later than the timing reported in some prior studies. Agarkar et. al. reported a median time to development of endophthalmitis of 2.5 days.17 Similarly, Wheeler et. al. reported that 82% of their cases of endophthalmitis presented by postoperative day 3.14 Eibenberger et. al reported a single case of endophthalmitis that occurred 9 days after initial cataract surgery,19 and in the PEDIG study, one case of endophthalmitis was reported to occur as late as 9 months after surgery.18 While our later timing of endophthalmitis diagnosis compared to the majority of cases previously reported in the literature may reflect the later development of endophthalmitis, it may also reflect a delay in diagnosis of endophthalmitis. Endophthalmitis is often the result of gram positive bacterial infection with incubation period and onset of positive anterior chamber cultures within 1 week of cataract surgery.25,26
Prior studies in the pediatric population have not found significant associations between endophthalmitis rates and particular predisposing factors, due to too few events to allow for meaningful multivariable analyses. Similarly, we did not find statistically significant associations between any available baseline demographic, intraoperative, or comorbid factors with the development of endophthalmitis in univariable or multivariable analyses.
Good et. al. had previously found that perioperative infections (e.g. upper respiratory tract infection, pneumonia, and nasolacrimal duct obstruction) occurred in all 3 positive cases of endophthalmitis in his case series published in 1990.27 In current practice, the likelihood of children undergoing cataract surgery with a concurrent infectious illness is low, as children are screened and discouraged from surgery until acute illnesses are resolved.
The results of this study should be interpreted within the context of its limitations. First, we must acknowledge the inherent limitations of a retrospective study, which preclude us from being able to control for intraoperative factors such as surgical technique and mode of antimicrobial prophylaxis. Also, studies using claims data have limitations due to the possibility of miscoding. For example, some surgeons may not have coded for an anterior vitrectomy even though they might have performed one at the time of cataract surgery. Another limitation of this study, despite the use of large-scale database, is the low number of endophthalmitis cases, making it difficult identify significant factors associated with the complication. Additionally, we hoped to study other risk factors for endophthalmitis, such as dermatitis and intellectual disability, but due to low overall incidences of these diagnoses, these factors were not included in our multivariable analyses. Finally, the generalizability of our study may be limited due to fact that our data are derived from one large national health insurance plan.
Despite our limitations, this is one of the first studies utilizing claims data to study endophthalmitis after cataract surgery in the pediatric population, and we report a higher incidence of endophthalmitis in our population compared to prior studies of a similar age-group. Using large health claims-based databases, as was done in our study and by Pershing et. al. with the IRIS registry, allows for complete longitudinal capture of clinical data for a large number of patients. Our rigorous inclusion and exclusion criteria also resulted in a homogenous group of patients with congenital and infantile cataracts.
CONCLUSION
In conclusion, our analysis of 789 children under 13 years old undergoing unilateral cataract surgery indicates an incidence of endophthalmitis of 0.51% within 90 days of cataract surgery, a rate higher than that reported in other studies of a similar age group. As with other prior studies, we did not find factors that were strongly associated with endophthalmitis. Our data offers new insights into the diagnosis of these serious postoperative complications, with endophthalmitis being detected slightly later than would be expected, thus leading to possible delayed treatment and poor prognosis. Our study helps to inform cataract surgeons of the potential risk of pediatric cataract surgery to share with patients’ families and emphasizes the need for diligent postoperative follow-up with careful examinations to evaluate for endophthalmitis.
Supplementary Material
VALUE STATEMENT:
What Was Known:
The incidence of postoperative endophthalmitis following pediatric cataract surgery has been previously reported to be up to 0.45%, a rate that is significantly higher than reported in adults.
The timing of postoperative endophthalmitis following pediatric cataract surgery has been reported to primarily occur within 3 days of cataract surgery.
What This Paper Adds:
The incidence of postoperative endophthalmitis in children in the real-world setting may be higher and may be detected later than previously reported.
Cataract surgeons should be aware of the relatively higher risk of endophthalmitis after pediatric cataract surgery when counseling patients’ families and when performing follow-up evaluations in order to detect the earliest signs of endophthalmitis.
ACKNOWLEDGMENT:
The authors thank Laurel Stell, Ph.D, from the Department of Biomedical Data Science, Stanford University, for biostatistical assistance.
Funding/Support: This work was supported in part by the Dong-A University Research Fund, NIH UL1 TR001085, P30 EY026877, and Research to Prevent Blindness, Inc
Footnotes
Financial Disclosures: The authors have no financial disclosures.
REFERENCES
- 1.Gharaibeh AM, Mezer E, Ospina LH, Wygnanski-Jaffe T. Endophthalmitis Following Pediatric Cataract Surgery: An International Pediatric Ophthalmology and Strabismus Council Global Perspective. J Pediatr Ophthalmol Strabismus. 2018;55(1):23–29. [DOI] [PubMed] [Google Scholar]
- 2.Jalali S Post-cataract Surgery Endophthalmitis. In: Das T, ed. Endophthalmitis : A Guide to Diagnosis and Management. Singapore: Springer Singapore; 2018:81–92. [Google Scholar]
- 3.Schmier JK, Hulme-Lowe CK, Covert DW, Lau EC. An updated estimate of costs of endophthalmitis following cataract surgery among Medicare patients: 2010–2014. Clin Ophthalmol. 2016;10:2121–2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gower EW, Keay LJ, Stare DE, et al. Characteristics of Endophthalmitis after Cataract Surgery in the United States Medicare Population. Ophthalmology. 2015;122(8):1625–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller JJ, Scott IU, Flynn HW Jr., Smiddy WE, Newton J, Miller D. Acute-onset endophthalmitis after cataract surgery (2000–2004): incidence, clinical settings, and visual acuity outcomes after treatment. Am J Ophthalmol. 2005;139(6):983–987. [DOI] [PubMed] [Google Scholar]
- 6.Torabi H, Tabatabai SA, Khodabande A. Treatment outcomes of post cataract surgery endophthalmitis in a tertiary referral center in Iran. J Curr Ophthalmol. 2018;30(2):152–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.West ES, Behrens A, McDonnell PJ, Tielsch JM, Schein OD. The incidence of endophthalmitis after cataract surgery among the U.S. Medicare population increased between 1994 and 2001. Ophthalmology. 2005;112(8):1388–1394. [DOI] [PubMed] [Google Scholar]
- 8.Montan P, Lundström M, Stenevi U, Thorburn W. Endophthalmitis following cataract surgery in Sweden. The 1998 national prospective survey. Acta Ophthalmol Scand. 2002;80(3):258–261. [DOI] [PubMed] [Google Scholar]
- 9.Pershing S, Lum F, Hsu S, et al. Endophthalmitis after Cataract Surgery in the United States: A Report from the Intelligent Research in Sight Registry, 2013–2017. Ophthalmology. 2020;127(2):151–158. [DOI] [PubMed] [Google Scholar]
- 10.OptumInsight EP, MN, US.. [Google Scholar]
- 11.Bureau USC. QuickFacts United States. 2019.
- 12.Lundvall A, Zetterström C. Complications after early surgery for congenital cataracts. Acta ophthalmologica Scandinavica. 1999;77(6):677–680. [DOI] [PubMed] [Google Scholar]
- 13.Keech RV, Tongue AC, Scott WE. Complications after surgery for congenital and infantile cataracts. Am J Ophthalmol. 1989;108(2):136–141. [DOI] [PubMed] [Google Scholar]
- 14.Wheeler DT, Stager DR, Weakley DR Jr. Endophthalmitis following pediatric intraocular surgery for congenital cataracts and congenital glaucoma. Journal of pediatric ophthalmology and strabismus. 1992;29(3):139–141. [DOI] [PubMed] [Google Scholar]
- 15.Plager DA, Yang S, Neely D, Sprunger D, Sondhi N. Complications in the first year following cataract surgery with and without IOL in infants and older children. J aapos. 2002;6(1):9–14. [DOI] [PubMed] [Google Scholar]
- 16.Solebo AL, Russell-Eggitt I, Cumberland PM, Rahi JS. Risks and outcomes associated with primary intraocular lens implantation in children under 2 years of age: the IoLunder2 cohort study. Br J Ophthalmol. 2015;99(11):1471–1476. [DOI] [PubMed] [Google Scholar]
- 17.Agarkar S, Desai R, Jambulingam M, Sumeer SH, Raman R. Incidence, management, and visual outcomes in pediatric endophthalmitis following cataract surgery by a single surgeon. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2016;20(5):415–418. [DOI] [PubMed] [Google Scholar]
- 18.Repka MX, Dean TW, Kraker RT, et al. Visual Acuity and Ophthalmic Outcomes in the Year After Cataract Surgery Among Children Younger Than 13 Years. JAMA Ophthalmol. 2019;137(7):817–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eibenberger K, Stifter E, Pusch F, Schmidt-Erfurth U. Simultaneous bilateral pediatric and juvenile cataract surgery under general anesthesia: outcomes and safety. Am J Ophthalmol. 2020. [DOI] [PubMed] [Google Scholar]
- 20.Repka MX, Lum F, Burugapalli B. Strabismus, Strabismus Surgery, and Reoperation Rate in the United States: Analysis from the IRIS Registry. Ophthalmology. 2018;125(10):1646–1653. [DOI] [PubMed] [Google Scholar]
- 21.Behndig A, Montan P, Stenevi U, Kugelberg M, Lundstrom M. One million cataract surgeries: Swedish National Cataract Register 1992–2009. J Cataract Refract Surg. 2011;37(8):1539–1545. [DOI] [PubMed] [Google Scholar]
- 22.Keay L, Gower EW, Cassard SD, Tielsch JM, Schein OD. Postcataract surgery endophthalmitis in the United States: analysis of the complete 2003 to 2004 Medicare database of cataract surgeries. Ophthalmology. 2012;119(5):914–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Preliminary report of principal results from a European multicenter study. J Cataract Refract Surg. 2006;32(3):407–410. [DOI] [PubMed] [Google Scholar]
- 24.Herrinton LJ, Shorstein NH, Paschal JF, et al. Comparative Effectiveness of Antibiotic Prophylaxis in Cataract Surgery. Ophthalmology. 2016;123(2):287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shirodkar AR, Pathengay A, Flynn HW Jr., et al. Delayed- versus acute-onset endophthalmitis after cataract surgery. American journal of ophthalmology. 2012;153(3):391–398.e392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jeong SH, Cho HJ, Kim HS, et al. Acute endophthalmitis after cataract surgery: 164 consecutive cases treated at a referral center in South Korea. Eye. 2017;31(10):1456–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Good WV, Hing S, Irvine AR, Hoyt CS, Taylor DS. Postoperative endophthalmitis in children following cataract surgery. Journal of pediatric ophthalmology and strabismus. 1990;27(6):283–285. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.