Abstract
Uncontrolled inflammation is considered the pathophysiological basis of many prevalent metabolic disorders, such as nonalcoholic fatty liver disease, diabetes, obesity, and neurodegenerative diseases. The inflammatory response is a self-limiting process that produces a superfamily of chemical mediators, called specialized proresolving mediators (SPMs). SPMs include the ω-3-derived family of molecules, such as resolvins, protectins, and maresins, as well as arachidonic acid-derived (ω-6) lipoxins that stimulate and promote resolution of inflammation, clearance of microbes, and alleviation of pain and promote tissue regeneration via novel mechanisms. SPMs function by binding and activating G protein-coupled receptors, such as FPR2/ALX, GPR32, and ERV1, and nuclear orphan receptors, such as RORα. Recently, several studies reported that SPMs have the potential to attenuate lipid metabolism disorders. However, the understanding of pharmacological aspects of SPMs, including tissue-specific biosynthesis, and specific SPM receptors and signaling pathways, is currently limited. Here, we summarize recent advances in the role of SPMs in resolution of inflammatory diseases with metabolic disorders, such as nonalcoholic fatty liver disease and obesity, obtained from preclinical animal studies. In addition, the known SPM receptors and their intracellular signaling are reviewed as targets of resolution of inflammation, and the currently available information on the therapeutic effects of major SPMs for metabolic disorders is summarized.
Keywords: Specialized pro-resolving mediators, Resolvins, Maresins, NAFLDs, Adipose tissue
INTRODUCTION
Excessive inflammation is associated with various chronic diseases, including nonalcoholic steatohepatitis (NASH), diabetic obesity, and cardiovascular and neurodegenerative diseases. Under homeostatic conditions, acute inflammation is self-limiting and resolves by itself. An acute inflammatory response is divided into two phases: the pro-inflammatory initiation phase and the anti-inflammatory resolution phase. In the resolution phase, the cessation of immune cell infiltration occurs in response to chemotactic signals, apoptosis of polymorphonuclear cells, and active clearance of apoptotic cells and debris by macrophages. Charles Serhan was the first researcher to describe lipid mediators for self-resolution of inflammation, called specialized proresolving mediators (SPMs) (Serhan, 2017). His research group identified SPMs via liquid chromatography–tandem mass spectrometry-based analysis of self-limited exudates formed in in vivo animal models and human cells (Serhan et al., 2000). Serhan and colleagues demonstrated that SPMs led to activation of efferocytosis to remove apoptotic neutrophils and inflammatory molecules (Dalli and Serhan, 2012). Furthermore, SPMs could induce a polarity switch of macrophages from pro-inflammatory M1 to anti-inflammatory M2 to resolve acute inflammation and secrete tissue repair and wound healing molecules (Buckley et al., 2014). Presently, it is well known that SPMs modulate pro-inflammatory responses, host defense, pain, tissue remodeling, and organ dysfunction via immunological mechanisms.
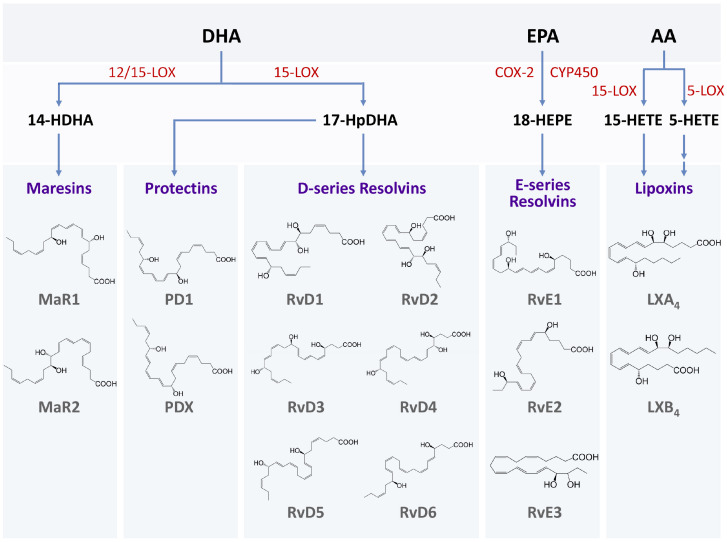
During the resolution phase of acute inflammation, SPMs are biosynthesized from essential polyunsaturated fatty acids (PUFAs), including docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), and arachidonic acid (AA) (Fig. 1). Resolvins are metabolites biosynthesized from ω-3 PUFAs, including DHA and EPA, via diverse lipoxygenases (LOXs), resulting in the production of D- and E-series resolvins (Serhan, 2017). D-series resolvins (RvD1–RvD6) are mainly derived from an epoxide of DHA via a reaction involving 15-LOX and 17S-hydroxy-4Z,7Z,10Z,13Z,15E,19Z-docosahexaenoic acid (17-HDHA) (Chiang and Serhan, 2017). Furthermore, the biosynthesis of protectins (PDs) and maresins (MaRs) occurs from lipoxygenase-mediated epoxide intermediates of DHA. However, lipoxins (LXs) including LXA4 and LXB4 are synthesized from ω-6 arachidonic acid via conversion of 15-hydroperoxyeicosatetraenoic acid (Park et al., 2020). The biosynthesis of these SPMs is mainly initiated during the late phase of the acute inflammatory response, wherein polymorphonuclear neutrophils undergo apoptosis and macrophages perform efferocytosis (Buckley et al., 2014). Moreover, these lipid mediators can influence immune cell responses as well as tissue homeostasis.
Fig. 1.
SPMs and their biosynthesis. Biosynthesis of SPMs starts from the long-chain PUFAs such as docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), and arachidonic acid (AA). Enzymes, including lipoxygenase (LOX) and cyclooxygenase (COX), convert PUFAs towards various SPM families. Maresins (MaR1 and MaR2), protectins (PD1 and PDX), and D-series resolvins (RvD1-RvD6) are derived from DHA. 14-Hydroxy docosahexaenoic acid (14-HDHA) is the intermediate of maresins produced by 12/15-LOX, and 17-hydroperoxy docosahexaenoic acid (17-HpDHA) is the intermediate of other SPM families derived from DHA. E-series resolvins (RvE1, RvE2, and RvE3) are synthesized from EPA. 18-Hydroxyeicosapentaenoic acid (18-HEPE) is the major intermediate which is produced by COX-2 or CYP450. Lipoxins (LXA4 and LXB4), the first SPMs identified, are biosynthesized from AA in two different routes by either 15-LOX or 5-LOX in different cells or tissues.
The inflammatory response plays an essential role in modulating lipid metabolism-related diseases, such as obesity and nonalcoholic fatty liver disease (NAFLD). Acute and chronic inflammation involving recruitment of neutrophils and macrophages is associated with dysregulated metabolism following dampening of functions of homeostatic parenchymal cells (Lumeng and Saltiel, 2011). Obesity and NAFLD are often associated with nonresolving inflammation in adipose and liver tissues, which is a key pathological event that leads to insulin resistance and metabolic dysregulation (Spite et al., 2014). The persistent inflammation can lead to metabolic disorders. In addition, disrupted metabolic homeostasis drives the onset of inflammation. Thus, it is reasonable to hypothesize that SPMs could modulate lipid metabolism-related diseases via resolution of the feedback loop of inflammatory stimulations and metabolic dysfunctions. In this regard, dysregulation of SPM biosynthesis in adipose tissue, the liver, and other tissues is involved in the pathogenesis of lipid metabolic diseases (Spite et al., 2014). In this review, we summarize the following: 1) the role of SPMs in resolution of inflammatory diseases with metabolic disorders, such as NAFLD and obesity; 2) SPM receptors and their intracellular signaling as targets of resolution of inflammation; and 3) the therapeutic effects of major SPM species for the treatment of metabolic disorders with chronic inflammation.
RESOLUTION OF LIVER INFLAMMATION: IMPLICATIONS OF SPMS IN THE PROGRESSION OF NAFLD
NAFLD is an umbrella term for a range of hepatic diseases ranging from simple lipid accumulation (steatosis) to complicated inflammations (steatohepatitis). With impaired adipose tissue homeostasis, the steatotic liver undergoes progressive inflammations to develop nonalcoholic steatohepatitis (NASH), fibrosis, and ultimately cirrhosis (Neuschwander-Tetri, 2020). Lipotoxicity and release of endogenous damage-associated molecular patterns begin the hepatic inflammatory response by accumulation of leukocytes, including activated-neutrophils and macrophages (Koyama and Brenner, 2017). The relevance of compositional change of ω-6 and ω-3 PUFAs in patients with NASH suggested that specific lipid mediators could modulate the symptoms of progressive NASH (Puri et al., 2007).
Several studies have reported the role of eicosanoids, metabolites of inflammatory ω-6 arachidonic acid, in NASH diseases. Moreover, cyclooxygenase 2-mediated prostaglandin E2 production by Kupffer cells induced accumulation of hepatic triglycerides via cyclic adenosine monophosphate (cAMP) (Enomoto et al., 2000). In addition, leukotriene (LT) signaling exhibited a potential effect on the progression from steatosis to NASH (Araújo et al., 2018). In particular, 5-LOX, an enzyme involved in the synthesis of LT family members from arachidonic acid, was remarkably activated in patients and mouse models of NASH (Puri et al., 2009; Horrillo et al., 2010). Pharmacological and genetic ablation of the LT pathway consistently inhibited progression of high fat diet (HFD)-induced hepatic steatosis and inflammatory responses (Horrillo et al., 2010; Martínez-Clemente et al., 2010).
Considering the proresolving function of inflammatory lipid mediators, it is not surprising that SPMs, metabolites of ω-3 PUFAs, have a beneficial effect on the progression of NASH (Table 1). Indeed, the feeding of a ω-3-enriched diet ameliorated steatotic and inflammatory liver injury in mouse models (González-Périz et al., 2006, 2009). These hepatoprotective effects of a ω-3-enriched diet were involved in the production of SPMs including resolvins, protectins, and 17-HDHA. RvE1 reduced hepatic lipid levels and macrophage activation along with adiponectin-mediated improvement of adipose tissue homeostasis (González-Périz et al., 2009). 17-HDHA and protectin D 1 (PD1) mediated beneficial effects of ω-3 PUFAs by downregulation of tumor necrosis factor (TNF) release and DNA damage in the liver (González-Périz et al., 2006). In particular, RvD1 significantly attenuated the symptoms of steatohepatitis, including steatosis, fibrosis, oxidative stress, and inflammatory activations via inhibiting nuclear factor-κB (NF-κB) and mitogen-activated protein kinase (MAPK) signaling in macrophages of mice models (Li et al., 2020). In addition, Kuang et al. (2016) reported that RvD1 and RvE1 decreased excessive activation of hepatic leukocytes in a concanavalin A-induced hepatitis model with mechanisms similar to NF-κB blockade (Kuang et al., 2016).
Table 1.
Effects of SMPs in mouse liver, adipose, vessel, and neuron
| Tissues | SPMS | Receptors | Effects in adipose and liver tissue | Ref |
|---|---|---|---|---|
| Liver | RvD1 | Not studied | Suppresses TLR4-mediated inflammatory signalling in liver | Li et al., 2020 |
| RvD1 | Not studied | Inhibits proinflammatory NF-κB activitiy | Kuang et al., 2016 | |
| RvE1 | Not studied | Inhibits proinflammatory NF-κB activitiy | Kuang et al., 2016 | |
| RvE1 | ChemR23/ERV1 | Induces adiponectin in adipose tissue | González-Périz et al., 2009 | |
| PD1 | Not studied | Decreases TNF release of macrophages and DNA damage of hepatocytes | González-Périz et al., 2006 | |
| MaR1 | Not studied | AMPK-mediated inhibition of liver steatosis | Laiglesia et al., 2018b | |
| MaR1 | Not studied | Suppresses lipotoxicity and ER stress | Rius et al., 2017 | |
| MaR1 | Not studied | Reduces ER stress via AMPK-SERCA2b pathway | Jung et al., 2018 | |
| MaR1 | Not studied | Regulates hepatocyte metabolism by modulating FGF21 | Martinez-Fernandez et al., 2019 | |
| MaR1 | RORα | Induces M2 polarity of liver macrophages | Han et al., 2019 | |
| MaR1 | ALX/FPR2 | Protects I/R liver injuries via Akt signaling | Tang et al., 2021 | |
| Adipose | RvD1 | FPR2/ALX | Increases M2:M1 adipose tissue macrophage ratio | Hellmann et al., 2011 |
| RvD2 | GPR18/DRV2 | Increased UCP1 and PGC1α expression in BAT and increased whole body consumption | Pascoal et al., 2017 | |
| RvD1 | GPR32/DRV1 | Decreased Anti-inflammatory activity* | Claria et al., 2012 | |
| RvE1 | ChemR23/ERV1 | Regulation of NFKb and modulate IL-12 production | Arita et al., 2005 | |
| RvE1 | BLT1 | Induces Pro-inflammatory activity | Claria et al., 2013 | |
| RvE1 | ChemR23/ERV1 | Protect against obesity induced glucose disorder | Sima et al., 2018 | |
| RvE2 | BLT1 | Inhibition of LTB4 mediated NF-κB activation | Arita et al., 2007 | |
| LxA4 | ALX/FPR2 | Significantly increased adiponectin secretion under obese condition | Claria et al., 2012 | |
| LxA4 | GPR32 | Inhibit IL-6 secretion and induce anti-inflammatory cytokine IL-10 | Claria et al., 2012 | |
| ω-3 PUFA | GPCR120 | Regulation of TNF-α-induced inflammatory signalling | Oh et al., 2010 | |
| Blood vessel | RvD1 | FPR2/ALX | Suppress lesional oxidative stress and necrosis | Fredman et al., 2016 |
| RvD2 | Not studied | Halt necrotic expansion and macrophage accumulation | Viola et al., 2016 | |
| Neuron | RvD1 | GPR32 | Induce microglial phagocytosis for amyloid-β | Zhu et al., 2016 |
| PD1 | Not studied | Decrease proinflammatory genes and increases antiapoptotic genes | Lukiw et al., 2005 | |
| PD1 | Not studied | Neuroprotection against proteotoxic and oxidative stress | Calandria et al., 2015b | |
| PD1 | Not studied | Regulates NF-κB activity | Calandria et al., 2015a |
Among the SPMs, MaR1 is the most validated lipid mediator to protect against HFD-induced liver injuries. Moreover, MaR1 ameliorated liver steatosis via decreasing the expression of lipogenic enzymes. Treatment of MaR1 induced activation of AMP-activated protein kinase (AMPK) and its downstream factors that are associated with fatty acid oxidation and autophagy (Laiglesia et al., 2018b). Furthermore, MaR1 was observed to directly affect hepatocytes by increasing AMPK phosphorylation, and ultimately decreasing lipid accumulations and endoplasmic reticulum stress (Rius et al., 2017; Jung et al., 2018). In addition, MaR1 modulated the expression of fibroblast growth factor 21 (FGF21), a key growth factor in systemic metabolism, in cultured hepatocytes (Martinez-Fernandez et al., 2019). In a previous study, nuclear receptor RORα was identified as an important regulator of liver macrophage polarization to induce an anti-inflammatory M2 phenotype in NASH (Han et al., 2017). In addition to effects on hepatocytes, MaR1 contributed to enhancement of RORα-induced M2 polarization in liver macrophages, resulting in resolution of liver inflammation in NASH (Han et al., 2019). Interestingly, RORα was activated by direct binding of MaR1 as an endogenous lipid ligand, suggesting that the MaR1-RORα axis may link inflammation and metabolic dysfunction in the liver. Furthermore, MaR1 reduced hepatic ischemia–reperfusion injury and led to a large decrease in the necrotic area (Tang et al., 2021). Taken together, the ability of MaR1 to ameliorate NAFLD injuries could offer new therapeutic candidates to impede the progression from simple steatosis to NASH in fatty liver diseases.
RESOLUTION OF ADIPOSE TISSUE INFLAMMATION: EFFECTS OF SPMS ON OBESITY-RELATED METABOLIC DYSFUNCTION
Serhan’s research group examined human adipose tissue using liquid chromatography–tandem mass spectrometry-based lipidomics analysis and found that RvD1, RvD2, PD1, MaR1, and LXA4 are endogenous to human subcutaneous adipose tissue (Claria et al., 2013). Using anatomical location-dependent profile analysis, they also demonstrated that perivascular fat depots possess higher biosynthetic capacity of SPMs compared with subcutaneous adipose tissue (Claria et al., 2013). Furthermore, an analysis of pathologic conditions with regard to SPM levels demonstrated that 17-HDHA and PD1 are downregulated in patients with peripheral vascular disease, which is associated with the induction of cytokines such as monocyte chemoattractant protein-1, plasminogen activator inhibitor-1, and interleukin (IL)-10 (Claria et al., 2013). In human omental adipose tissue under nutritional stress, the levels of SPMs such as resolvins, lipoxins, and protectins were reduced with increased activity of IL-10 (Titos et al., 2016). An in vivo mouse study identified RvD1 and RvD2 as the major SPMs regulating the inflammatory responses in adipose tissue and demonstrated the reduction of RvD1, RvD2, and PD1 in adipose tissue from obese mice compared with that from lean mice (Claria et al., 2012). Another in vivo study demonstrated that dietary supplementation of ω-3 PUFAs improved thermogenic activity of brown and white adipose tissues in mice and that recruitment of thermogenic adipocytes was affected by local concentration of oxylipins, including SPMs (Ghandour et al., 2018). The positive correlation between thermogenic activity of human brown adipose tissue and levels of ω-3 fatty acid-derived SPMs (Kulterer et al., 2020) suggested the clinical relevance of the regulatory effects of SPMs in energy metabolism. We next summarize the recent research on the obesity-driven defects in biosynthesis of the major SPMs: resolvins, MaRs, lipoxins, and protectins.
Neuhofer et al. (2013) showed that obesity significantly reduces the levels of RvD1 in gonadal adipose tissue, along with an accumulation of adipose tissue inflammatory factors. RvD1 treatment in leptin receptor-deficient mice enhanced glucose tolerance and insulin sensitivity, together with reduced pro-inflammatory gene expression and crown-like structure formation in epididymal white adipose tissue (Hellmann et al., 2011). In inflamed human adipose tissue, RvD1 treatment increased MAPK activity and inhibited the activity of STAT-1 and related inflammatory genes without affecting the anti-inflammatory effects of IL-10 (Titos et al., 2016). Furthermore, RvD1 treatment modulated overactivation of STAT-3 phosphorylation at Tyr705 but maintained IL-10-induced anti-inflammatory response by inhibiting IL-6, IL-1β, IL-8, and TNF-α activity in adipose tissue (Titos et al., 2016). RvD1 and its precursor DHA were shown to classically polarize macrophages toward an M2-like phenotype by increasing M2 markers, such as IL-10, Arg1, Ym1, REALMα, and CD206, in adipose tissue of obese mice (Titos et al., 2011). Consequently, RvD1 protects against obesity-induced adipose tissue inflammation, insulin resistance, and metabolic liver disease (Titos et al., 2011). RvD1 treatment under calorie restriction status reduced the size of adipocytes in epididymal white adipose tissue, increased adiponectin levels, and reduced circulating leptin levels (Rius et al., 2014). In addition, depletion of RvD1 was related to obesity-associated osteoarthritis, wherein ω-3 PUFAs resulted in reduced expression of pro-inflammatory factors and induced M2 macrophage polarization (Sun et al., 2019).
A recent study demonstrated that RvE1 treatment prevented hyperinsulinemia and hyperglycemia in mice consuming a HFD. Moreover, the fasting glucose or insulin levels in RvE1 receptor (resolvin E1 receptor [ERV1]/ChemR23) knockout mice were not recovered by RvE1 treatment (Pal et al., 2020). Using transgenic mice that overexpressed human ERV1 in myeloid cells, Sima et al. (2018) demonstrated that ERV1 reduced body weight and provided protection against HFD-induced hyperglycemia. In addition, the administration of RvE1 reproduced the protective effects of ERV1 overexpression (Sima et al., 2018). In the same mouse model, endogenous production of SPMs such as RvD1, RvD4, RvD5, PD1, and LXA4 increased, indicating a significant contribution of ERV1 receptor signaling to the regulation of SPM production. Furthermore, RvE1 was identified to modulate the immune response via LTB4 receptor BLT1 in polymorphonuclear leukocytes, by inhibiting the pro-inflammatory response induced by LTB4 via blocking the mobilization of intracellular calcium and NF-κB activation (Arita et al., 2007).
The anti-inflammatory effects of MaRs have been addressed in previous studies. MaR1 treatment reversed the effect of pro-inflammatory cytokine TNF-α and induced Akt phosphorylation in subcutaneous adipose tissue from patients with obesity as well as improved glucose homeostasis in obese mice (Martinez-Fernandez et al., 2020). Furthermore, MaR1 treatment in diet-induced obesity mice regulated FGF21 and its production in hepatocytes, resulting in improved glucose metabolism and insulin sensitivity. In addition, it reversed the HFD-induced downregulation of FGF21, FGFR1, and β-Klotho in white adipose tissue (Martinez-Fernandez et al., 2019). In another study with a similar mouse model, MaR1 treatment improved anti-inflammatory effects by reducing the levels of pro-inflammatory agents IL-1β and TNF-α in colonic mucosa of obese mice (Leon et al., 2020). In an in vitro study using mature 3T3L1 adipocytes, MaR1 treatment reversed the effect of TNF-α-induced lipolysis and autophagy by regulating phosphorylation of hormone sensitive lipase; moreover, it counteracted the cytokine-induced decrease of p62 and prevented the induction of autophagy flux (Laiglesia et al., 2018a). MaR1 treatment also promoted resolution of inflammation in adipose tissue in obese mice by reducing macrophage infiltration, downregulating M1 macrophage phenotype marker expression, reducing the levels of pro-inflammatory markers, and subsequently increasing expression of the anti-inflammatory adipokine adiponectin in white adipose tissue (Martinez-Fernandez et al., 2017).
The mechanism of action of LXA4 was investigated in perigonadal adipose tissue of mice. LXA4 was found to induce the proresolving effect by inhibiting IL-6 secretion and enhancing IL-10 production. This finding suggested a protective effect of LXA4 in reprogramming of pro-inflammatory macrophages to a relatively proresolving phenotype and inhibiting the effect of inflammatory cytokines on adipose tissue inflammation, indicating a possible direct regulation of adipocyte insulin signaling pathways (Börgeson et al., 2012). Claria et al. (2012) identified the expression of LXA4 receptor FPR2/ALX in human adipose tissue. Furthermore, Börgeson et al. (2015) studied the role of lipoxins in preserving p62 and LC3-II levels in obese mice. They also reported that lipoxins regulate M1 to M2 macrophage phenotype conversion to induce resolution of inflammation in adipose tissue. Lipoxins demonstrate this protective effect independent of adiponectin secretion by reducing TNF-α expression and restoring annexin-1 level in the adipose tissue. Moreover, LXA4 administration in HFD mice can induce recovery from renal damage and inflammation due to NF-κB and ERK/P38 MAPK by inhibiting the phosphorylation of ERK/P38 MAPK (Tourki et al., 2020). In addition, pretreatment with a LXA4 antagonist was shown to worsen the inflammation and renal damage, suggesting that LXA4 activity in obese mice can decrease the inflammatory affects caused by NF-κB and ERK/P38 MAPK pathways (Tourki et al., 2020).
Administration of protectin DX (PDX), a double lipoxygenase derivative of docosahexaenoic acid, was found to reduce the increase in body weight and epididymal white adipose tissue mass, improve glucose tolerance, and improve insulin sensitivity (Piao et al., 2020).
ROLE OF SPMS IN LIPID METABOLISM DISORDERS IN ARTERIES AND NEURONS
Atherosclerosis is a complex human disease associated with inflammation and lipid metabolism dysfunction in arteries. Interestingly, imbalances between SPMs and pro-inflammatory mediators in the circulatory system are involved in prevalent atherosclerotic diseases. The ratio of SPMs to pro-inflammatory LTB4 was lower in the human carotid atherosclerotic regions, but the administration of RvD1 promoted recovery in the damaged areas (Fredman et al., 2016). Furthermore, exogenous treatment of RvD2 and MaR1 prevented atheroprogression via suppressing necrosis of endothelial cells and formation of collagen fibrous plaque (Viola et al., 2016). Nuclear localized 5-LOX generated pro-inflammatory LTs instead of proresolving lipoxins and human carotid atherosclerotic regions contained higher expression of nuclear 5-LOX compared with healthy regions (Spanbroek et al., 2003; Qiu et al., 2006). The impaired efferocytosis of vessel macrophages to produce SPMs on their own was found to be another possible mechanism underlying the imbalance of lipid mediators. However, the elevated expression of Mertk receptors to recognize apoptotic cells could support effective efferocytosis and production of SPMs in the artery (Fredman and Tabas, 2017). Therefore, investigation of anti-inflammatory SPMs is important to explore the pathological link between inflammation and lipid metabolism in atherosclerotic cardiovascular disease.
SPMs also modulate neuroinflammation and lipid metabolism-associated neurodegenerative diseases such as Alzheimer’s and Parkinson’s diseases. Alzheimer’s disease is characterized by the excessive accumulation of amyloid-β in the brain. MaR1 and RvD1 alleviate neurodegeneration by promoting microglial phagocytosis of amyloid-β (Zhu et al., 2016). In particular, protectin D1 (PD1), produced by 15-LOX and 5-LOX, is a well-known lipid mediator that promotes the reduction of neurodegenerative injuries. The levels of PD1 were reduced in the hippocampus and temporal lobe of patients with Alzheimer’s disease (Lukiw et al., 2005). Moreover, PD1 inhibited cell death and increased neural cell survival, which alleviated the symptoms of Alzheimer’s and Parkinson’s diseases (Lukiw et al., 2005; Stark and Bazan, 2011; Calandria et al., 2015b). PD1 also regulated the NF-κB cyclic response and showed anti-inflammatory effects (Calandria et al., 2015a). Although SPMs have shown protective effects for neural diseases, few clinical trials have been undertaken to explore the potential use of SPMs for Alzheimer’s and Parkinson’s diseases.
SPM RECEPTORS AND THEIR INTRACELLULAR SIGNALING
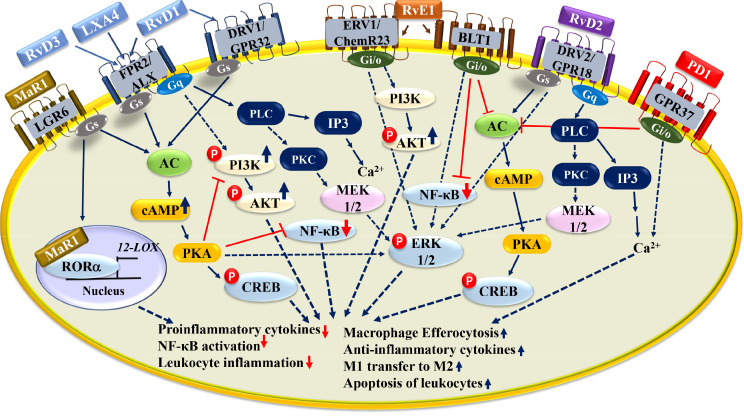
SPMs bind to G protein-coupled receptor (GPCR) family members and activate them. FPR2/ALX is expressed on a wide range of leukocytes and leads to pro- and anti-inflammatory effects (Fig. 2) (Chiang and Serhan, 2017). Lipoxins such as LXA4 and resolvins such as RvD1 and RvD3 can effectively activate FPR2/ALX receptor signaling. Moreover, anti-inflammatory and efferocytotic functions of RvD1 under peritonitis were inhibited when FPR2/ALX receptor signaling was defective (Krishnamoorthy et al., 2012). GPR32 is an orphan receptor predominantly expressed on human neutrophils, monocytes, adipose tissue, and endothelial cells. RvD1, RvD3, and RvD5 activate the cellular response via this receptor. Although RvD1 has a higher affinity for GPR32 than for FPR2/ALX, the former is not expressed in rodents. This finding indicated that the function of RvD1 in rodents is mainly mediated via FPR2/ALX signaling (Schmid et al., 2016; Chiang et al., 2019a). Chimerin receptor 1 (ChemR23 or ERV1) is expressed on immune cells, including monocytes, macrophages, natural killer cells, and dendritic cells. ERV1 was identified as a surface receptor for RvE1 among the GPCRs (Arita et al., 2005). RvE1 treatment reduced IL-12 production and dendritic cell trafficking, but these effects were eliminated by ERV1 siRNA (Arita et al., 2005). GPR37 is mostly expressed on brain cells and macrophages and is associated with neurological diseases, such as Parkinson’s disease (Lopes et al., 2015). Especially, GPR37 was revealed to PD1 receptors, and PD1-induced anti-inflammatory effects were reduced in GPR37 knockout mice (Bang et al., 2018). Recently, the receptors for MaR1 were identified in two studies. First, LGR6, a human leucine-rich repeat containing GPCR, was identified as a stereoselective receptor of MaR1 for efferocytotic functions (Chiang et al., 2019b). Second, MaR1 could act as an endogenous ligand for nuclear receptor RORα, which modulates M2 polarization of macrophages and induces anti-inflammatory effects (Han et al., 2019). The functions of MaR1 differed at different time points: LGR6-mediated phagocyte action was rapid but RORα-mediated M2 polarization was moderately slow. These findings underlie the potential signaling of intracellular functions of SPMs as well as surface GPCRs. Furthermore, PPARγ is a possible potent nuclear receptor for other SPMs, including PD1 and RvD1, to mediate anti-inflammatory responses (Zhao et al., 2011; Liao et al., 2012).
Fig. 2.
SPM receptors and associated intracellular signaling pathways. SPMs signal through specific G-protein coupled receptors (GPCRs). RvD1, RvD3 and LXA4 are agonist for ALX/FPR2 and its activity leads to PKA activation to phosphorylate CREB promoting production of anti-inflammatory cytokines, macrophage polarization. RvD1 also influences AKT phosphorylation via PI3K pathway to inhibit NF-kB mediated pro-inflammatory effects. It also enhances ERK1/2 phosphorylation via MEK1/2 to induce anti-inflammatory effects. RvD2 works through DRV2, leading to ERK1/2 or PLC pathway to promote resolution. RvE1 is an agonist for ChemR23 and BLT1. The ChemR23-RvE1 downstream signaling activates AKT phosphorylation, inhibiting NF-kB inflammatory effects. PD1-GPR37 mechanistic actions also found to block PKA activation. MaR1 acts via two distinct receptors, LGR6 and RORα. MaR1 activates RORα transcriptional activity, leading to M2 polarization and 12-LOX expression, an enzyme required for MaR1 syntheis. MaR1 activates LGR6-mediated cAMP signaling to promote macrophage efferocytosis and resolution.
THERAPEUTIC POTENTIAL OF SPMS IN DISEASES WITH LIPID METABOLISM DISORDERS
SPMs showed high potential to ameliorate diverse inflammatory and lipid-related diseases in preclinical animal models (Table 2). However, few clinical trials of SPMs have been performed, although some SPMs demonstrated significant anti-inflammatory effects, because the stability of SPMs is low due to their complex physiochemical nature and structure (Arita et al., 2006). A synthetic analog of RvE1, RX-10045, was synthesized by Resolvyx Pharmaceuticals. It was tested regarding ocular inflammation diseases, and a phase 2 randomized trial was recently completed (Clinicaltrials.gov; NCT02329743). In addition, a combination of DHA metabolite SPMs, including 17-HDHA, 18-HEPE, and 14-HDHA, called Lipinova, demonstrated resolution of inflammation after orthopedic surgery (Clinicaltrials.gov; NCT03434236). Furthermore, some synthetic analogs of SPMs showed high potency in reducing inflammatory responses. A synthetic benzo-diacetylenic-17R-RvD1-methyl ester (BDA-RvD1) significantly reduced acute recruitment of neutrophils in ischemia–reperfusion-induced lung injury and enhanced phagocytosis (Orr et al., 2015). A benzo-fused ring-modified LXA4 analog (BLXA4-ME) showed proresolving properties and is currently under clinical trials for a topical rinse treatment of gingivitis (Clinicaltrials.gov; NCT02342691). In addition to SPM mimetics, GPCR agonists, especially for the receptor FPR2/ALX, are extensively being developed for clinical trials. AR234245 (Arena Pharmaceuticals) was the first developed synthetic agonist of FPR2/ALX. After the development of AR234245, many pharmaceutical and academic groups have endeavored to develop other FPR2/ALX agonists. ACT-389949 (Actelion Pharmaceuticals) was the first-in-class candidate of anti-inflammatory GPCR agonists to show good safety and toleration in healthy subjects during clinical trials (Stalder et al., 2017). Recently, a clinical trial for peripheral artery diseases with dietary administration of SPM emulsion was endeavored, and the outcomes will be posted soon (Clinicaltrials.gov; NCT02719665).
Table 2.
Potential therapeutic effects of SPM on tissue dysfunction
| SPMs | Dosage | Experimental model | Resolution | Ref |
|---|---|---|---|---|
| RvE1 | 1.2 ng/g (4 days) | Ob/ob mice | Reduces liver steatosis and macrophage activation | González-Périz et al., 2009 |
| RvD1 | 300 ng | C57BL/6J under 4 weeks of MCD diet | Decreases expression of inflammatory genes and stress markers for restoring NASH | Li et al., 2020 |
| MaR1 | 50 ug/kg | Ob/ob and HFD-fed (3 months) mice | Ameliorates hepatic triglycerides and fasting glucose levels | Laiglesia et al., 2018b |
| MaR1 | 5 ug/kg | HFD-fed (3 months) mice | Reduces liver fibrosis | Han et al., 2019 |
| MaR1 | 20 ng | Ischemic/reperfusion injury | Lowered liver injuries including necrosis | Tang et al., 2021 |
| RvE1 | 300 ng | C57BL/6J under 5 weeks of HFD | Restored glucose level in obese mice | Pal et al., 2020 |
| MaR1 | 50 ug/kg (3 h) | Diet induced obesity mice | Induced Akt phosphorylation for better insulin sensitivity | Martinez-Fernandez et al., 2020 |
| MaR1 | 2 mg/kg (10 days) | Genetic obese mice | Blocks the activity of TNFa, IL-1b pro-inflammatory action, and upregulates adiponectin and Glut-4, Akt phosphorylation | Martinez-Fernandez et al., 2017 |
| LxA4 | LXA4 (5ng/g) or benzo-LXA4 (1.7 ng/g) | C57BL/6J and C57BL/6J adiponectin−/− mice under 3 month of HFD | Block adipose tissue inflammation and increases insulin sensitivity | Börgeson et al., 2015 |
| RvD1 | 100 ng | LDLR knockout mice | Reduces fibrous cap in vessels | Fredman et al., 2016 |
SPMs and their corresponding receptors have been targeted to develop therapeutic strategies for the resolution of inflammation and its consequent diseases. However, even after 20 years since SPMs were first identified, no clinically usable drugs have been successfully developed for the therapeutic strategy involving GPCRs and SPM mimetics. Numerous GPCRs have been identified for SPMs, but the downstream signaling is complex and evokes multiple responses, and a lack of in-depth knowledge regarding these physiological responses hampers the exploration of GPCRs for clinical use. Recently, new mechanisms of SPM actions were identified, and it was reported that SPMs can enter cells and directly bind with nuclear receptors as agonistic ligands (Han et al., 2019). Many nuclear receptors interact with lipid mediators as endogenous ligands, such as PPARα–LT, HNF4α–linoleic acid, RORβ–stearic acid, and RORα–MaR1 (Holzer et al., 2017). These mechanisms could broaden the clinical usage of SPMs because the use of nuclear receptors for treatment of human diseases is being established.
CONCLUSIONS
SPMs have the potential to attenuate or prevent chronic inflammatory diseases with lipid metabolism disorders through resolution of the feedback loop of inflammatory stimulations and metabolic dysfunctions. SPMs can trigger anti-inflammatory processes by binding and activating GPCRs and nuclear receptors. Currently, however, the understanding of SPMs and their receptor signaling pathways is limited. Thus, identification and characterization of specific receptors and intracellular signaling pathways for each SPM that are intricately linked to the pathogenesis of lipid metabolism disorders would provide new insights to overcome the hurdles in therapeutic application of SPMs. Due to the high potency of SPMs for resolution of acute and chronic inflammations, clinical SPM therapy for inflammatory and lipid metabolism-related diseases could soon be established.
ACKNOWLEDGMENTS
This study was supported by a grant from the National Research Foundation of Korea (NRF) (2021R1C1C1004023 to Y.H.H.; NRF-2019R1C1C1002014 to Y.H.L.; 2017R1A2B3011870 to M.O.L., and 2018R1A5A2024425 to Y.H.L. and M.O.L.) and 2020 Research Grant from Kangwon National University.
Footnotes
CONFLICT OF INTEREST
The authors declare no competing interest.
REFERENCES
- Araújo A. C., Wheelock C. E., Haeggström J. Z. The eicosanoids, redox-regulated lipid mediators in immunometabolic disorders. Antioxid. Redox Signal. 2018;29:275–296. doi: 10.1089/ars.2017.7332. [DOI] [PubMed] [Google Scholar]
- Arita M., Bianchini F., Aliberti J., Sher A., Chiang N., Hong S., Yang R., Petasis N. A., Serhan C. N. Stereochemical assignment, antiinflammatory properties, and receptor for the omega-3 lipid mediator resolvin E1. J. Exp. Med. 2005;201:713–722. doi: 10.1084/jem.20042031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arita M., Oh S. F., Chonan T., Hong S., Elangovan S., Sun Y. P., Uddin J., Petasis N. A., Serhan C. N. Metabolic inactivation of resolvin E1 and stabilization of its anti-inflammatory actions. J. Biol. Chem. 2006;281:22847–22854. doi: 10.1074/jbc.M603766200. [DOI] [PubMed] [Google Scholar]
- Arita M., Ohira T., Sun Y. P., Elangovan S., Chiang N., Serhan C. N. Resolvin E1 selectively interacts with leukotriene B4 receptor BLT1 and ChemR23 to regulate inflammation. J. Immunol. 2007;178:3912–3917. doi: 10.4049/jimmunol.178.6.3912. [DOI] [PubMed] [Google Scholar]
- Bang S., Xie Y. K., Zhang Z. J., Wang Z., Xu Z. Z., Ji R. R. GPR37 regulates macrophage phagocytosis and resolution of inflammatory pain. J. Clin. Invest. 2018;128:3568–3582. doi: 10.1172/JCI99888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Börgeson E., Johnson A. M., Lee Y. S., Till A., Syed G. H., Ali-Shah S. T., Guiry P. J., Dalli J., Colas R. A., Serhan C. N., Sharma K., Godson C. Lipoxin A4 attenuates obesity-induced adipose inflammation and associated liver and kidney disease. Cell Metab. 2015;22:125–137. doi: 10.1016/j.cmet.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Börgeson E., McGillicuddy F. C., Harford K. A., Corrigan N., Higgins D. F., Maderna P., Roche H. M., Godson C. Lipoxin A4 attenuates adipose inflammation. FASEB J. 2012;26:4287–4294. doi: 10.1096/fj.12-208249. [DOI] [PubMed] [Google Scholar]
- Buckley C. D., Gilroy D. W., Serhan C. N. Proresolving lipid mediators and mechanisms in the resolution of acute inflammation. Immunity. 2014;40:315–327. doi: 10.1016/j.immuni.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calandria J. M., Asatryan A., Balaszczuk V., Knott E. J., Jun B. K., Mukherjee P. K., Belayev L., Bazan N. G. NPD1-mediated stereoselective regulation of BIRC3 expression through cREL is decisive for neural cell survival. Cell Death Differ. 2015a;22:1363–1377. doi: 10.1038/cdd.2014.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calandria J. M., Sharp M. W., Bazan N. G. The docosanoid neuroprotectin D1 induces TH-positive neuronal survival in a cellular model of Parkinson's disease. Cell. Mol. Neurobiol. 2015b;35:1127–1136. doi: 10.1007/s10571-015-0206-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang N., Barnaeva E., Hu X., Marugan J., Southall N., Ferrer M., Serhan C. N. Identification of chemotype agonists for human resolvin D1 receptor DRV1 with pro-resolving functions. Cell Chem. Biol. 2019a;26:244–254.e4. doi: 10.1016/j.chembiol.2018.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang N., Libreros S., Norris P. C., de la Rosa X., Serhan C. N. Maresin 1 activates LGR6 receptor promoting phagocyte immunoresolvent functions. J. Clin. Invest. 2019b;129:5294–5311. doi: 10.1172/JCI129448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang N., Serhan C. N. Structural elucidation and physiologic functions of specialized pro-resolving mediators and their receptors. Mol. Aspects Med. 2017;58:114–129. doi: 10.1016/j.mam.2017.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claria J., Dalli J., Yacoubian S., Gao F., Serhan C. N. Resolvin D1 and resolvin D2 govern local inflammatory tone in obese fat. J. Immunol. 2012;189:2597–2605. doi: 10.4049/jimmunol.1201272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claria J., Nguyen B. T., Madenci A. L., Ozaki C. K., Serhan C. N. Diversity of lipid mediators in human adipose tissue depots. Am. J. Physiol. Cell Physiol. 2013;304:C1141–C1149. doi: 10.1152/ajpcell.00351.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalli J., Serhan C. N. Specific lipid mediator signatures of human phagocytes: microparticles stimulate macrophage efferocytosis and pro-resolving mediators. Blood. 2012;120:e60–e72. doi: 10.1182/blood-2012-04-423525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enomoto N., Ikejima K., Yamashina S., Enomoto A., Nishiura T., Nishimura T., Brenner D. A., Schemmer P., Bradford B. U., Rivera C. A., Zhong Z., Thurman R. G. Kupffer cell-derived prostaglandin E(2) is involved in alcohol-induced fat accumulation in rat liver. Am. J. Physiol. Gastrointest. Liver Physiol. 2000;279:G100–G106. doi: 10.1152/ajpgi.2000.279.1.G100. [DOI] [PubMed] [Google Scholar]
- Fredman G., Hellmann J., Proto J. D., Kuriakose G., Colas R. A., Dorweiler B., Connolly E. S., Solomon R., Jones D. M., Heyer E. J., Spite M., Tabas I. An imbalance between specialized pro-resolving lipid mediators and pro-inflammatory leukotrienes promotes instability of atherosclerotic plaques. Nat. Commun. 2016;7:12859. doi: 10.1038/ncomms12859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman G., Tabas I. Boosting inflammation resolution in atherosclerosis: the next frontier for therapy. Am. J. Pathol. 2017;187:1211–1221. doi: 10.1016/j.ajpath.2017.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghandour R. A., Colson C., Giroud M., Maurer S., Rekima S., Ailhaud G., Klingenspor M., Amri E. Z., Pisani D. F. Impact of dietary omega3 polyunsaturated fatty acid supplementation on brown and brite adipocyte function. J. Lipid Res. 2018;59:452–461. doi: 10.1194/jlr.M081091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Périz A., Horrillo R., Ferre N., Gronert K., Dong B., Moran-Salvador E., Titos E., Martinez-Clemente M., Lopez-Parra M., Arroyo V., Clària J. Obesity-induced insulin resistance and hepatic steatosis are alleviated by omega-3 fatty acids: a role for resolvins and protectins. FASEB J. 2009;23:1946–1957. doi: 10.1096/fj.08-125674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Périz A., Planagumà A., Gronert K., Miquel R., López-Parra M., Titos E., Horrillo R., Ferré N., Deulofeu R., Arroyo V., Rodés J., Clària J. Docosahexaenoic acid (DHA) blunts liver injury by conversion to protective lipid mediators: protectin D1 and 17S-hydroxy-DHA. FASEB J. 2006;20:2537–2539. doi: 10.1096/fj.06-6250fje. [DOI] [PubMed] [Google Scholar]
- Han Y. H., Kim H. J., Na H., Nam M. W., Kim J. Y., Kim J. S., Koo S. H., Lee M. O. RORα induces KLF4-mediated M2 polarization in the liver macrophages that protect against nonalcoholic steatohepatitis. Cell Rep. 2017;20:124–135. doi: 10.1016/j.celrep.2017.06.017. [DOI] [PubMed] [Google Scholar]
- Han Y. H., Shin K. O., Kim J. Y., Khadka D. B., Kim H. J., Lee Y. M., Cho W. J., Cha J. Y., Lee B. J., Lee M. O. A maresin 1/RORα/12-lipoxygenase autoregulatory circuit prevents inflammation and progression of nonalcoholic steatohepatitis. J. Clin. Invest. 2019;129:1684–1698. doi: 10.1172/JCI124219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellmann J., Tang Y., Kosuri M., Bhatnagar A., Spite M. Resolvin D1 decreases adipose tissue macrophage accumulation and improves insulin sensitivity in obese-diabetic mice. FASEB J. 2011;25:2399–2407. doi: 10.1096/fj.10-178657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzer G., Markov G. V., Laudet V. Evolution of nuclear receptors and ligand signaling: toward a soft key-lock model? Curr. Top. Dev. Biol. 2017;125:1–38. doi: 10.1016/bs.ctdb.2017.02.003. [DOI] [PubMed] [Google Scholar]
- Horrillo R., González-Périz A., Martínez-Clemente M., López-Parra M., Ferré N., Titos E., Morán-Salvador E., Deulofeu R., Arroyo V., Clària J. 5-lipoxygenase activating protein signals adipose tissue inflammation and lipid dysfunction in experimental obesity. J. Immunol. 2010;184:3978–3987. doi: 10.4049/jimmunol.0901355. [DOI] [PubMed] [Google Scholar]
- Jung T. W., Kim H. C., Abd El-Aty A. M., Jeong J. H. Maresin 1 attenuates NAFLD by suppression of endoplasmic reticulum stress via AMPK-SERCA2b pathway. J. Biol. Chem. 2018;293:3981–3988. doi: 10.1074/jbc.RA117.000885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koyama Y., Brenner D. A. Liver inflammation and fibrosis. J. Clin. Invest. 2017;127:55–64. doi: 10.1172/JCI88881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamoorthy S., Recchiuti A., Chiang N., Fredman G., Serhan C. N. Resolvin D1 receptor stereoselectivity and regulation of inflammation and proresolving microRNAs. Am. J. Pathol. 2012;180:2018–2027. doi: 10.1016/j.ajpath.2012.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulterer O. C., Niederstaetter L., Herz C. T., Haug A. R., Bileck A., Pils D., Kautzky-Willer A., Gerner C., Kiefer F. W. The presence of active brown adipose tissue determines cold-induced energy expenditure and oxylipin profiles in humans. J. Clin. Endocrinol. Metab. 2020;105:dgaa183. doi: 10.1210/clinem/dgaa183. [DOI] [PubMed] [Google Scholar]
- Kuang H., Hua X., Zhou J., Yang R. Resolvin D1 and E1 alleviate the progress of hepatitis toward liver cancer in long-term concanavalin A-induced mice through inhibition of NF-κB activity. Oncol. Rep. 2016;35:307–317. doi: 10.3892/or.2015.4389. [DOI] [PubMed] [Google Scholar]
- Laiglesia L. M., Lorente-Cebrian S., Lopez-Yoldi M., Lanas R., Sainz N., Martinez J. A., Moreno-Aliaga M. J. Maresin 1 inhibits TNF-alpha-induced lipolysis and autophagy in 3T3-L1 adipocytes. J. Cell. Physiol. 2018a;233:2238–2246. doi: 10.1002/jcp.26096. [DOI] [PubMed] [Google Scholar]
- Laiglesia L. M., Lorente-Cebrián S., Martínez-Fernández L., Sáinz N., Prieto-Hontoria P. L., Burrell M. A., Rodríguez-Ortigosa C. M., Martínez J. A., Moreno-Aliaga M. J. Maresin 1 mitigates liver steatosis in ob/ob and diet-induced obese mice. Int. J. Obes. (Lond.) 2018b;42:572–579. doi: 10.1038/ijo.2017.226. [DOI] [PubMed] [Google Scholar]
- Leon I. C., Quesada-Vazquez S., Sainz N., Guruceaga E., Escote X., Moreno-Aliaga M. J. Effects of Maresin 1 (MaR1) on colonic inflammation and gut dysbiosis in diet-induced obese mice. Microorganisms. 2020;8:1156. doi: 10.3390/microorganisms8081156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumeng C. N., Saltiel A. R. Inflammatory links between obesity and metabolic disease. J. Clin. Invest. 2011;121:2111–2117. doi: 10.1172/JCI57132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Deng X., Bai T., Wang S., Jiang Q., Xu K. Resolvin D1 mitigates non-alcoholic steatohepatitis by suppressing the TLR4-MyD88-mediated NF-κB and MAPK pathways and activating the Nrf2 pathway in mice. Int. Immunopharmacol. 2020;88:106961. doi: 10.1016/j.intimp.2020.106961. [DOI] [PubMed] [Google Scholar]
- Liao Z., Dong J., Wu W., Yang T., Wang T., Guo L., Chen L., Xu D., Wen F. Resolvin D1 attenuates inflammation in lipopolysaccharide-induced acute lung injury through a process involving the PPARγ/NF-κB pathway. Respir. Res. 2012;13:110. doi: 10.1186/1465-9921-13-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes J. P., Morató X., Souza C., Pinhal C., Machado N. J., Canas P. M., Silva H. B., Stagljar I., Gandía J., Fernández-Dueñas V., Luján R., Cunha R. A., Ciruela F. The role of parkinson's disease-associated receptor GPR37 in the hippocampus: functional interplay with the adenosinergic system. J. Neurochem. 2015;134:135–146. doi: 10.1111/jnc.13109. [DOI] [PubMed] [Google Scholar]
- Lukiw W. J., Cui J. G., Marcheselli V. L., Bodker M., Botkjaer A., Gotlinger K., Serhan C. N., Bazan N. G. A role for docosahexaenoic acid-derived neuroprotectin D1 in neural cell survival and Alzheimer disease. J. Clin. Invest. 2005;115:2774–2783. doi: 10.1172/JCI25420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Clemente M., Ferré N., González-Périz A., López-Parra M., Horrillo R., Titos E., Morán-Salvador E., Miquel R., Arroyo V., Funk C. D., Clària J. 5-lipoxygenase deficiency reduces hepatic inflammation and tumor necrosis factor alpha-induced hepatocyte damage in hyperlipidemia-prone ApoE-null mice. Hepatology. 2010;51:817–827. doi: 10.1002/hep.23463. [DOI] [PubMed] [Google Scholar]
- Martinez-Fernandez L., Gonzalez-Muniesa P., Laiglesia L. M., Sainz N., Prieto-Hontoria P. L., Escote X., Odriozola L., Corrales F. J., Arbones-Mainar J. M., Martinez J. A., Moreno-Aliaga M. J. Maresin 1 improves insulin sensitivity and attenuates adipose tissue inflammation in ob/ob and diet-induced obese mice. FASEB J. 2017;31:2135–2145. doi: 10.1096/fj.201600859R. [DOI] [PubMed] [Google Scholar]
- Martinez-Fernandez L., Gonzalez-Muniesa P., Sainz N., Escote X., Martinez J. A., Arbones-Mainar J. M., Moreno-Aliaga M. J. Maresin 1 regulates insulin signaling in human adipocytes as well as in adipose tissue and muscle of lean and obese mice. J. Physiol. Biochem. 2020;77:167–173. doi: 10.1007/s13105-020-00775-9. [DOI] [PubMed] [Google Scholar]
- Martinez-Fernandez L., Gonzalez-Muniesa P., Sainz N., Laiglesia L. M., Escote X., Martinez J. A., Moreno-Aliaga M. J. Maresin 1 regulates hepatic FGF21 in diet-induced obese mice and in cultured hepatocytes. Mol. Nutr. Food Res. 2019;63:e1900358. doi: 10.1002/mnfr.201900358. [DOI] [PubMed] [Google Scholar]
- Neuhofer A., Zeyda M., Mascher D., Itariu B. K., Murano I., Leitner L., Hochbrugger E. E., Fraisl P., Cinti S., Serhan C. N., Stulnig T. M. Impaired local production of proresolving lipid mediators in obesity and 17-HDHA as a potential treatment for obesity-associated inflammation. Diabetes. 2013;62:1945–1956. doi: 10.2337/db12-0828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuschwander-Tetri B. A. Therapeutic landscape for NAFLD in 2020. Gastroenterology. 2020;158:1984–1998.e3. doi: 10.1053/j.gastro.2020.01.051. [DOI] [PubMed] [Google Scholar]
- Oh D. Y., Talukdar S., Bae E. J., Imamura T., Morinaga H., Fan W., Li P., Lu W.J., Watkins S. M., Olefsky J. M. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell. 2010;142:687–698. doi: 10.1016/j.cell.2010.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr S. K., Colas R. A., Dalli J., Chiang N., Serhan C. N. Proresolving actions of a new resolvin D1 analog mimetic qualifies as an immunoresolvent. Am. J. Physiol. Lung Cell. Mol. Physiol. 2015;308:L904–L911. doi: 10.1152/ajplung.00370.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoal L. B., Bombassaro B., Ramalho A. F., Coope A., Moura R. F., Correa-da-Silva F., Ignacio-Souza L., Razolli D., de Oliveira D., Catharino R., Velloso L. A. Resolvin RvD2 reduces hypothalamic inflammation and rescues mice from diet-induced obesity. J. Neuroinflammation. 2017;14:5. doi: 10.1186/s12974-016-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal A., Al-Shaer A. E., Guesdon W., Torres M. J., Armstrong M., Quinn K., Davis T., Reisdorph N., Neufer P. D., Spangenburg E. E., Carroll I., Bazinet R. P., Halade G. V., Clària J., Shaikh S. R. Resolvin E1 derived from eicosapentaenoic acid prevents hyperinsulinemia and hyperglycemia in a host genetic manner. FASEB J. 2020;34:10640–10656. doi: 10.1096/fj.202000830R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J., Langmead C. J., Riddy D. M. New advances in targeting the resolution of inflammation: implications for specialized pro-resolving mediator GPCR drug discovery. ACS Pharmacol. Transl. Sci. 2020;3:88–106. doi: 10.1021/acsptsci.9b00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piao S., Du W., Wei Y., Yang Y., Feng X., Bai L. Protectin DX attenuates IL-1beta-induced inflammation via the AMPK/NF-kappaB pathway in chondrocytes and ameliorates osteoarthritis progression in a rat model. Int. Immunopharmacol. 2020;78:106043. doi: 10.1016/j.intimp.2019.106043. [DOI] [PubMed] [Google Scholar]
- Puri P., Baillie R. A., Wiest M. M., Mirshahi F., Choudhury J., Cheung O., Sargeant C., Contos M. J., Sanyal A. J. A lipidomic analysis of nonalcoholic fatty liver disease. Hepatology. 2007;46:1081–1090. doi: 10.1002/hep.21763. [DOI] [PubMed] [Google Scholar]
- Puri P., Wiest M. M., Cheung O., Mirshahi F., Sargeant C., Min H. K., Contos M. J., Sterling R. K., Fuchs M., Zhou H., Watkins S. M., Sanyal A. J. The plasma lipidomic signature of nonalcoholic steatohepatitis. Hepatology. 2009;50:1827–1838. doi: 10.1002/hep.23229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu H., Gabrielsen A., Agardh H. E., Wan M., Wetterholm A., Wong C. H., Hedin U., Swedenborg J., Hansson G. K., Samuelsson B., Paulsson-Berne G., Haeggström J. Z. Expression of 5-lipoxygenase and leukotriene A4 hydrolase in human atherosclerotic lesions correlates with symptoms of plaque instability. Proc. Natl. Acad. Sci. U.S.A. 2006;103:8161–8166. doi: 10.1073/pnas.0602414103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rius B., Duran-Güell M., Flores-Costa R., López-Vicario C., Lopategi A., Alcaraz-Quiles J., Casulleras M., Lozano J. J., Titos E., Clària J. The specialized proresolving lipid mediator maresin 1 protects hepatocytes from lipotoxic and hypoxia-induced endoplasmic reticulum stress. FASEB J. 2017;31:5384–5398. doi: 10.1096/fj.201700394R. [DOI] [PubMed] [Google Scholar]
- Rius B., Titos E., Moran-Salvador E., Lopez-Vicario C., Garcia-Alonso V., Gonzalez-Periz A., Arroyo V., Claria J. Resolvin D1 primes the resolution process initiated by calorie restriction in obesity-induced steatohepatitis. FASEB J. 2014;28:836–848. doi: 10.1096/fj.13-235614. [DOI] [PubMed] [Google Scholar]
- Schmid M., Gemperle C., Rimann N., Hersberger M. Resolvin D1 polarizes primary human macrophages toward a proresolution phenotype through GPR32. J. Immunol. 2016;196:3429–3437. doi: 10.4049/jimmunol.1501701. [DOI] [PubMed] [Google Scholar]
- Serhan C. N. Discovery of specialized pro-resolving mediators marks the dawn of resolution physiology and pharmacology. Mol. Aspects Med. 2017;58:1–11. doi: 10.1016/j.mam.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serhan C. N., Clish C. B., Brannon J., Colgan S. P., Chiang N., Gronert K. Novel functional sets of lipid-derived mediators with antiinflammatory actions generated from omega-3 fatty acids via cyclooxygenase 2-nonsteroidal antiinflammatory drugs and transcellular processing. J. Exp. Med. 2000;192:1197–1204. doi: 10.1084/jem.192.8.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sima C., Montero E., Nguyen D., Freire M., Norris P., Serhan C. N., Van Dyke T. E. Author correction: ERV1 overexpression in myeloid cells protects against high fat diet induced obesity and glucose intolerance. Sci. Rep. 2018;8:4143. doi: 10.1038/s41598-018-22520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanbroek R., Grabner R., Lotzer K., Hildner M., Urbach A., Ruhling K., Moos M. P., Kaiser B., Cohnert T. U., Wahlers T., Zieske A., Plenz G., Robenek H., Salbach P., Kuhn H., Radmark O., Samuelsson B., Habenicht A. J. Expanding expression of the 5-lipoxygenase pathway within the arterial wall during human atherogenesis. Proc. Natl. Acad. Sci. U.S.A. 2003;100:1238–1243. doi: 10.1073/pnas.242716099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spite M., Clària J., Serhan C. N. Resolvins, specialized proresolving lipid mediators, and their potential roles in metabolic diseases. Cell Metab. 2014;19:21–36. doi: 10.1016/j.cmet.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stalder A. K., Lott D., Strasser D. S., Cruz H. G., Krause A., Groenen P. M., Dingemanse J. Biomarker-guided clinical development of the first-in-class anti-inflammatory FPR2/ALX agonist ACT-389949. Br. J. Clin. Pharmacol. 2017;83:476–486. doi: 10.1111/bcp.13149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark D. T., Bazan N. G. Neuroprotectin D1 induces neuronal survival and downregulation of amyloidogenic processing in Alzheimer's disease cellular models. Mol. Neurobiol. 2011;43:131–138. doi: 10.1007/s12035-011-8174-4. [DOI] [PubMed] [Google Scholar]
- Sun A. R., Wu X., Liu B., Chen Y., Armitage C. W., Kollipara A., Crawford R., Beagley K. W., Mao X., Xiao Y., Prasadam I. Pro-resolving lipid mediator ameliorates obesity induced osteoarthritis by regulating synovial macrophage polarisation. Sci. Rep. 2019;9:426. doi: 10.1038/s41598-018-36909-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang D., Fu G., Li W., Sun P., Loughran P. A., Deng M., Scott M. J., Billiar T. R. Maresin 1 protects the liver against ischemia/reperfusion injury via the ALXR/Akt signaling pathway. Mol. Med. 2021;27:18. doi: 10.1186/s10020-021-00280-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titos E., Rius B., Gonzalez-Periz A., Lopez-Vicario C., Moran-Salvador E., Martinez-Clemente M., Arroyo V., Claria J. Resolvin D1 and its precursor docosahexaenoic acid promote resolution of adipose tissue inflammation by eliciting macrophage polarization toward an M2-like phenotype. J. Immunol. 2011;187:5408–5418. doi: 10.4049/jimmunol.1100225. [DOI] [PubMed] [Google Scholar]
- Titos E., Rius B., Lopez-Vicario C., Alcaraz-Quiles J., Garcia-Alonso V., Lopategi A., Dalli J., Lozano J.J., Arroyo V., Delgado S., Serhan C. N., Clària J. Signaling and immunoresolving actions of resolvin D1 in inflamed human visceral adipose tissue. J. Immunol. 2016;197:3360–3370. doi: 10.4049/jimmunol.1502522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourki B., Kain V., Shaikh S. R., Leroy X., Serhan C. N., Halade G. V. Deficit of resolution receptor magnifies inflammatory leukocyte directed cardiorenal and endothelial dysfunction with signs of cardiomyopathy of obesity. FASEB J. 2020;34:10560–10573. doi: 10.1096/fj.202000495RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viola J. R., Lemnitzer P., Jansen Y., Csaba G., Winter C., Neideck C., Silvestre-Roig C., Dittmar G., Döring Y., Drechsler M., Weber C., Zimmer R., Cenac N., Soehnlein O. Resolving lipid mediators Maresin 1 and Resolvin D2 prevent atheroprogression in mice. Circ. Res. 2016;119:1030–1038. doi: 10.1161/CIRCRESAHA.116.309492. [DOI] [PubMed] [Google Scholar]
- Zhao Y., Calon F., Julien C., Winkler J. W., Petasis N. A., Lukiw W. J., Bazan N. G. Docosahexaenoic acid-derived neuroprotectin D1 induces neuronal survival via secretase- and PPARγ-mediated mechanisms in Alzheimer's disease models. PLoS ONE. 2011;6:e15816. doi: 10.1371/journal.pone.0015816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu M., Wang X., Hjorth E., Colas R. A., Schroeder L., Granholm A. C., Serhan C. N., Schultzberg M. Pro-resolving lipid mediators improve neuronal survival and increase Aβ42 phagocytosis. Mol. Neurobiol. 2016;53:2733–2749. doi: 10.1007/s12035-015-9544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]