Abstract
Background
Perianchor cyst formation (PCF) can occur after arthroscopic rotator cuff repair with poly-L-lactic acid (PLLA) anchors; however, little is known about PCF after all-suture anchor (ASA) use.
Methods
We reviewed patients who underwent double-row arthroscopic rotator cuff repair from 2012 to 2017 with ASAs implanted in the medial row and PLLA anchors in the lateral row. We evaluated PCF (graded on magnetic resonance imaging) and compared physical examination and functional surveys between patients with PCF (WC) and without PCF (WoC) at long-term follow-up.
Results
Among twenty-two patients (23 shoulders), 93% of PLLA anchors (vs. 79% ASA) displayed a grade 0 PCF, P = .100. No PLLA anchors had a grade 3 or 4 PCF, compared to 11% of ASAs, P = .158. At a mean postoperative follow-up time of 113 weeks, there was no significant difference between WC and WoC cohorts with regard to range of motion, rotator cuff strength, American Shoulder and Elbow Surgeons survey scores, or retear rates. However, the WoC cohort had a significantly higher University of California at Los Angeles shoulder survey score at final follow-up (34.3 WoC vs. 30.9 WC, P = .024).
Conclusion
No difference was found in PCF between ASAs and PLLA anchors. At long-term follow-up, WoC patients had significantly improved functional outcome scores, based on the University of California at Los Angeles survey, but equivalent range of motion and rotator cuff strength examinations compared with WC patients.
Keywords: Perianchor cyst, Anchor, Rotator cuff, PLLA, ASA, Shoulder
Rotator cuff tears are common in the American population with a prevalence of 22.1%, and this percentage increases with age.17 For those who undergo arthroscopic rotator cuff repair, the trend has been to use bone anchors in a double-row technique to reattach the tendon to the humeral head to decrease gap formation and improve healing.3,7,11,15,16,21 There are several types of anchors available for the surgeon to use, each with different biologic and mechanical properties. Metallic and nonbioabsorbable anchors were historically used and were found to cause microscopic metallic fragments, interference with postoperative imaging, migration and cartilage damage.24 Newer biocomposite anchors, such as poly-L-lactic acid (PLLA) anchors coated in hydroxyappetite, became available for rotator cuff repairs; however, perianchor cyst formation (PCF) has been reported in up to 37% of PLLA anchors.13 The use of biologically inert anchors, such as screw-type anchors made of polyetheretherketone (PEEK) and all suture anchors (ASAs), have been developed with the goal of reducing the bone reaction, thereby improving the milieu for tendon to bone healing. ASAs are gaining favor for their biologically inert properties, small drill hole needed for implanting the anchors, and equivalent pullout strengths compared with traditional solid-body anchors.7
To our knowledge, there are limited data for investigating the incidence of PCF in a double row repair model comparing ASAs and bioabsorbable anchors within the same patient. Additionally, only few studies have explored the impact of PCF on clinical outcomes in the past two years.13,23,27 This study aimed to investigate PCF in patients who underwent arthroscopic double row, rotator cuff repair using Iconix ASAs for the medial row (Stryker, San Jose, CA) and biocomposite SwiveLock lateral row anchors (Arthrex, Naples, FL). Furthermore, the goal was to evaluate the impact of PCF on clinical outcomes. We hypothesized that ASAs would have fewer PCF and of lower grade than PLLA anchors, due to them being biologically inert. Additionally, we hypothesized there would be no difference in clinical outcomes between patients who had at least one PCF and patients without any PCF.
Methods
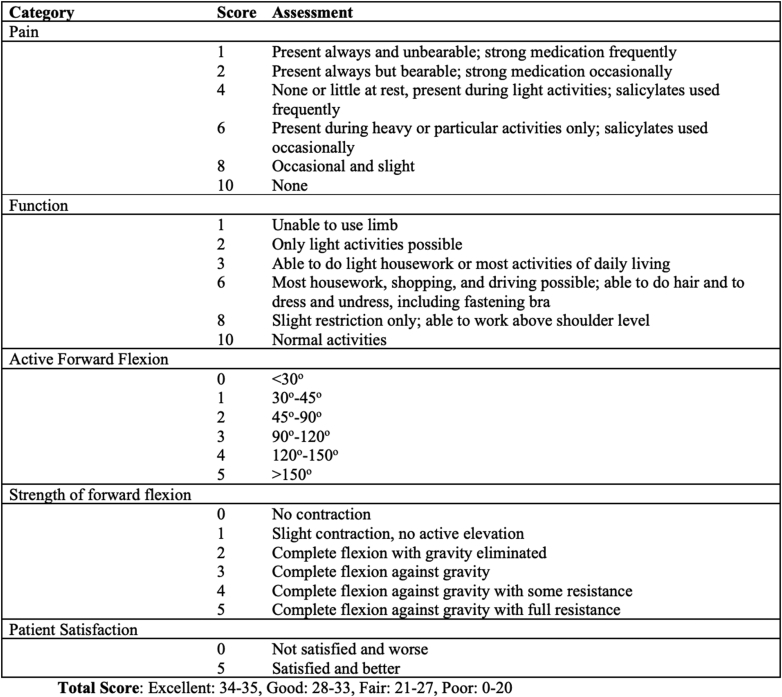
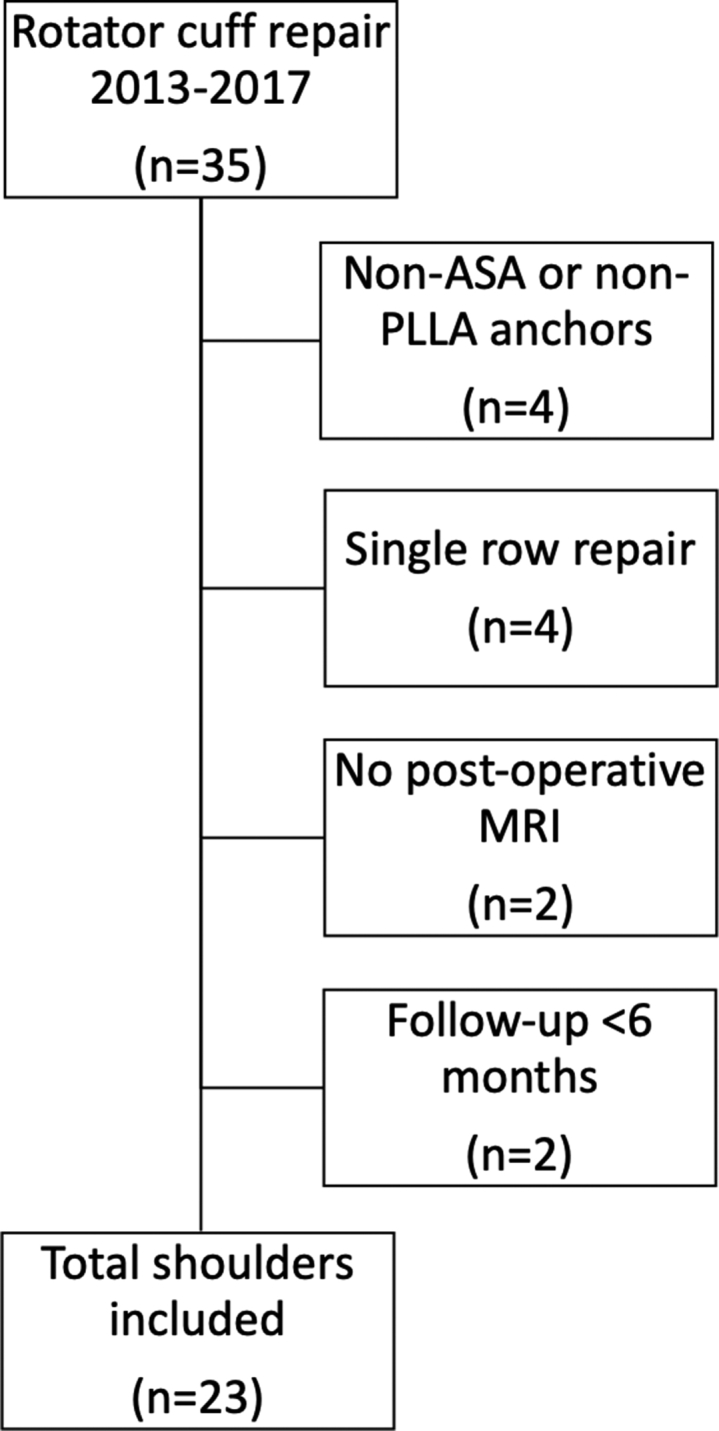
This is an institutional review board–approved cohort study performed at a single institution. Patients included in this study had a rotator cuff tear diagnosed by magnetic resonance imaging (MRI) and underwent arthroscopic rotator cuff repair by a single surgeon with a suture-bridge double-row repair using ASAs in the medial row and PLLA biocomposite anchors in the lateral row from September 2013 to November 2017 (Fig. 1). The ASAs were composed of three strands of #2 ForceFiber (Stryker, ultra-high-molecular-weight polyethylene, polypropylene, and nylon). The PLLA biocomposite anchor was composed of PLLA and tri-calcium phosphate. Beginning in June 2017, all patients were prospectively enrolled and completed a postoperative MRI. Exclusion criteria included patients with anchors other than ASA or PLLA anchors, prior surgery on the ipsilateral shoulder, single-row repair, patients without postoperative MRIs, and follow-up of less than 6 months. All patients received physical examinations at their follow-up visits and received a noncontrast MRI of the postoperative shoulder to determine the presence and size of the cyst. The final physical examination before the postoperative MRI was documented. A single, fellowship-trained musculoskeletal radiologist with 20 years of experience graded the MRI anchor cysts. Cyst formation was graded according to a previously established grading system: 0, no fluid; 1, minimal linear fluid collection; 2, local collection of fluid at the anchor insertion site; 3, fluid collection around the whole length of the anchor but of a diameter less than twice the anchor diameter; and 4, fluid diameter ≥ twice the anchor diameter.8 The initial analysis compared PCF between ASAs and PLLA anchors. In each patient, the individual anchors and the corresponding occurrence of a cyst at the medial and lateral sides were recorded. A second analysis compared shoulders without cyst formation (WoC) to patients with at least one anchor with a ≥grade 1 PCF (WC). The primary outcomes were postoperative cyst formation and grade of cyst. Secondary outcomes included final range of motion (forward flexion [FF], external rotation (ER), internal rotation [IR]), strength 0-5 (supraspinatus, infraspinatus), re-tear rates, and functional scores as determined by the University of California at Los Angeles (UCLA) shoulder survey (Fig. 2) and the American Shoulder and Elbow Surgeons (ASES) survey.1,19 Patients’ age, gender, body mass index, smoking status, and presence of diabetes mellitus at the time of surgery were recorded. Mean duration of time between surgery and postoperative MRI, as well as between surgery and the last follow-up visit, was evaluated.
Figure 1.
Flow diagram of study participants.
Figure 2.
University of California at Los Angeles (UCLA) shoulder survey.
Surgical technique
All patients received a preoperative interscalene block. Surgery was performed with patients in the beach chair position using standard posterior and anterior portals. Diagnostic arthroscopy was performed. The rotator cuff tear was visualized, and a subacromial decompression was performed by resecting the coracoacromial ligament, performing an acromioplasty, and removing the subacromial bursa. A subacromial decompression was not performed in patients who demonstrated a massive rotator cuff tear to preserve the coracoacromial ligament. After establishing rotator cuff tear anatomy and mobility, the cuff edge was debrided, and the greater and lesser tuberosities were prepared with a 5.5-mm motorized shaver. All medial row anchors were Iconix 2.3-mm double loaded suture anchors and placed at the articular margin of the rotator cuff footprint using the Iconix 2.3-mm drill. Sutures were passed through the rotator cuff in a mattress fashion and tied medially using a modified Weston knot. The medial row sutures were then linked to lateral row anchors (biocomposite SwiveLock 4.75 mm). One limb of suture from the posterior anchor and one limb from the anterior anchor were loaded into the SwiveLock anchor. A punch was used to create a hole in the tuberosity, and the anchor was inserted. The sutures were tensioned to compress the tendon onto the tuberosity, and the anchor was screwed into the bone. An articular margin repair was documented from the glenohumeral side.
Postoperatively, a sling was maintained for six weeks. Passive motion with pendulums and supine FF was permitted during the first six weeks. Formal physical therapy was started at six weeks and continued for 18 weeks.
MRI technique
MR images were obtained using a GE Medical Systems 1.5 Tesla magnet (Optima 450w) and a receiving phased array shoulder coil. Multiplanar pulse sequences included high-resolution proton density and fat-suppressed T2-weighed fast spin echo images as well as short TI inversion recovery images to suppress any susceptibility artifact produced by the anchors. Proton density images offered the best spatial resolution with a frequency/phase acquisition matrix of 416/256. T2-weighted fast spin echo and short TI inversion recovery sequences allowed for fluid-tissue contrast to evaluate for cyst formation and had matrices of 320/256 and 288/224, respectively. All images had a slice thickness of 3 mm with a 1-mm gap.
Statistical analysis
Baseline patient characteristics were summarized using standard descriptive statistics: mean, minimum, maximum, and standard deviation (SD) for the continuous variables; and frequency and percent for the categorical variables. Differences in the characteristics between WoC and WC cohorts were tested using the Wilcoxon Mann-Whitney test for the continuous variables and Fisher’s exact test for the categorical variables. The proportions of PCF between the medial and lateral sides were calculated and compared using mixed Poisson regression models. This approach accounts for the fact that incidence of PCF is assessed in a double row repair model comparing both ASAs and PLLA anchors within the same patient; this is in contrast to a more simplistic approach that does not account for placement of ASAs and PLLA anchors within the same patient, for example, a McNemar’s paired test. The point estimates and their corresponding 95% confidence intervals were calculated. The statistical tests were two-sided at a significance level of 0.05. The analyses were performed using the SAS/STAT software, version 9.4, of the SAS System for Windows (copyright 2016 SAS Institute Inc.).
Results
A total of 22 patients (23 shoulders) met inclusion criteria in the study. Patient demographics are listed in Table I. No difference was found between WoC and WC cohorts with regard to age, gender, body mass index, smoking status, and presence of diabetes mellitus. There were 58 ASAs in the medial row and 44 PLLA anchors in the lateral row. Forty-one of 44 (93.2%) PLLA anchors had no PCF compared with 46 of 58 (79.3%) ASAs (confidence interval 0.82-11.25, P = .100). In patients who had a PCF, there was no significant difference in the grade of cyst between ASA and PLLA anchors. The total number of PCF for each grade is reported in Table II.
Table I.
Characteristics of study patients.
| Characteristic | WoC (n = 12) | WC (n = 11) | P value |
|---|---|---|---|
| Age, yr | 62.6 (43-79) | 57.1 (47-67) | .515 |
| Gender, male/female | 3 (25)/9 (75) | 6 (55)/5 (45) | .214 |
| BMI | 26.8 (23-31) | 29 (23.6-36.7) | .280 |
| Smoker, no/yes | 11 (92)/1 (8) | 11 (100)/0 (0) | 1.000 |
| Diabetes, no/yes | 11 (92)/1 (8) | 7 (64)/4 (36) | .155 |
| Time between surgery and postop MRI (wks) | 111.5 (53.4-193.7) | 121.3 (42.4-208.7) | .786 |
| Time between surgery and last follow-up (wks) | 110.7 (48-180) | 116.4 (40-192) | .705 |
WoC, without cyst; WC, with cyst; BMI, body mass index; MRI, magnetic resonance imaging.
Table II.
Grade of perianchor cyst.
| Grade | ASA (n = 58) | PLLA (n = 44) | P value |
|---|---|---|---|
| .158 | |||
| 0 | 46 (79) | 41 (93) | |
| 1 | 2 (3) | 2 (5) | |
| 2 | 4 (7) | 1 (2) | |
| 3 | 5 (9) | 0 | |
| 4 | 1 (2) | 0 |
ASA, all-suture anchor; PLLA, poly-L-lactic acid.
The WoC cohort had twelve shoulders, and the WC cohort had eleven shoulders. There was no significant difference between either mean time of surgery to postoperative MRI (WoC 111.5 weeks, SD 50.1; WC 121.3 weeks, SD 63.2; P = .786) or mean time of surgery to last follow-up (WoC 110.7 weeks, SD 40.8; WC 116.4 weeks, SD 53.2; P = .705). MRI was completed after the last follow-up for 19 of 23 patients and before the last follow-up in 4 of 23 patients (3 WoC, 1 WC). Regarding range of motion, no difference was found in mean FF (WoC 165.0, WC 153.6, P = .051), ER (WoC 41.7, WC 39.5, P = .336), and IR (P = .081). There was no statistically significant difference in supraspinatus strength (P = .317) and infraspinatus strength (P = .478) between WoC and WC cohorts. Range of motion and strength scores are described in Table III. ASES and UCLA scores were obtained for eleven shoulders in the WoC group and ten shoulders in the WC group. The WoC cohort had a significantly higher UCLA score (mean 34.3, 31-35) than the WC cohort (mean 30.9, 19-35), P = .024. The ASES score showed no statistically significant difference between the two cohorts (WoC 93.6, 86.6-100 vs. WC 78.8, 30-100; P = .073). The rotator cuff retear rate was 21.7% (5/23), with two occurring in WoC and three in WC (P = .640).
Table III.
Clinical outcomes.
| Outcome | WoC (n = 12) | WC (n = 11) | P value |
|---|---|---|---|
| FF (degrees) | 165 (160-180) | 153.6 (120-170) | .051 |
| ER (degrees) | 41.7 (30-45) | 39.5 (30-45) | .336 |
| IR (degrees) | .081 | ||
| Buttock | 0 | 3 (27) | |
| L1 | 2 (17) | 1 (9) | |
| L2 | 3 (25) | 0 | |
| L3 | 1 (8) | 3 (27) | |
| L4 | 1 (8) | 3 (27) | |
| L5 | 1 (8) | 0 | |
| T12 | 4 (33) | 1 (9) | |
| Supraspinatus | .317 | ||
| 4/5 | 1 (8) | 3 (27) | |
| 5/5 | 11 (92) | 8 (73) | |
| Infraspinatus | .478 | ||
| 4/5 | 0 | 1 (9) | |
| 5/5 | 12 (100) | 10 (91) | |
| ASES | 93.6 (86.6-100) | 78.8 (30-100) | .073 |
| UCLA | 34.3 (31-35) | 30.9 (19-35) | .024∗ |
| Re-tear | 2 (17) | 3 (27) | .640 |
WoC, without cyst; WC, with cyst; FF, forward flexion; ER, external rotation; IR, internal rotation; ASES, American Shoulder and Elbow Surgeons; UCLA, University of California at Los Angeles.
P < .05, statistically significant P value.
Discussion
This study investigated the bone reaction of ASA and PLLA anchors and the impact of PCF on functional outcomes. Several hypotheses have been proposed as to the etiology of PCF, including micromotion, foreign-body reaction, and synovitis.5 Initially used for labral repairs, ASAs have recently been gaining popularity in rotator cuff repairs because of the satisfactory results of both biomechanical and clinical trials.6,27 ASAs use a smaller implant with reports of equivalent strength and little bone reaction compared with traditional suture anchors.7 Van der Bracht et al showed 90% (43/48) of ASAs had no fluid collection at an average of 1.58 years after rotator cuff repair.26 This is slightly higher than the results obtained in the present study; however, they evaluated fewer anchors and had a shorter interval between surgery and MRI. It has been shown that osteolysis appears twelve weeks postoperatively for PLLA anchors and increases in size as time progresses.22 A recent study by Kim et al compared four different suture anchors (ASA, PEEK, and two different biodegradable anchors) between two groups (ASA + biodegradable 1 vs. PEEK + biodegradable 2) using a double-row rotator cuff repair.14 Their study showed a statistically significant higher rate of PCF around PEEK anchors (41.7%, 15/36) than ASAs (10.8%, 4/37), P < .05. When the ASA was compared to the biodegradable anchor used in the same patient, there was no statistical difference as seen in our study.
It has been theorized the medial row undergoes higher forces than the lateral row during a double-row rotator cuff repair.2,25 This could result in different pressures on the bone-anchor interface, allowing for micromotion in the implant and ultimately changes in rate of PCF. An increased size of the anchor may lead to increased stability and less micromotion.8 Regarding the lateral row, it was initially thought there could be increased bone reaction secondary to softer bone and less coverage by tendinous tissue.28 However, Haneveld et al investigated this phenomenon and found the location of the anchor in the humeral head did not impact the amount of peri-implant fluid.8
Several studies have reported no statistically significant difference in clinical outcomes when comparing patients with and without PCF.18,20,22 Ro et al found no difference in visual analog scale scores, muscle strength, and range of motion between ASA, bioabsorbable, and PEEK anchors at a mean follow-up of 9.6 months.20 However, they did find an association between larger retear size and higher grade PCF. Most rotator cuff repair studies investigating PCF had shorter clinical follow-up times of around 1 to 1.5 years.12,13,20,27 A study by Haneveld et al compared PLLA to PEEK anchors with a mean follow-up of 28.4 ± 8.9 months and found no clinical difference between the two groups.8 Pilge et al had a mean follow-up time of 36 months after mini-open rotator cuff repairs with only a single type of bioabsorbable anchor (Bio-Corkscrew suture anchor; Arthrex, Naples, FL) and found no clinical difference in range of motion or Constant-Murley shoulder outcome score.18 Our article reports similar follow-up times to the study by Haneveld et al with the benefit of having patients as their own internal control. With extended postoperative follow-up, there was still no difference in range of motion or rotator cuff strength between WoC and WC cohorts. In this study, our data demonstrated a significantly higher UCLA score in patients without PCF (34.3 vs. 30.9, P < .05). Additionally, range of motion and rotator cuff strength were measured by visual examination by the senior author. Prior studies report fair to good reliability with standard error measurements of 14-25 degrees for inter-rater and 11-23 degrees for intrarater.9,10 The standard error measurements in addition to the small population size could account for the trend seen toward greater FF scores in the WoC cohort (165° vs. 154°, P = .05). As FF score is a component of the UCLA survey (but not the ASES survey), this could be a contributing factor to the higher UCLA scores in the WoC cohort. It is important to note that the maximum score for FF on the UCLA survey is for >150°, and therefore, any range of motion greater than this may not have clinical significance. Hence, the difference in FF scores seen in our study may not be clinically relevant. Similar to other authors, none of the other range of motion outcomes (ER and IR) in this study were close to approaching a statistically significant difference.
There has been increasing interest in PCF and its clinical implications, especially as increasingly more types of anchors are becoming available to surgeons. This article is in agreement with previous studies finding no difference in clinical outcomes if a cyst develops, even at a more extended follow-up period. Future studies investigating anchor biomechanics, pull-out strength, and ease of use would be valuable to assess whether these factors are important in differentiating between types of anchor and anchor selection for patients.
There were several limitations to this study. First, the small sample size may have made the study underpowered. However, a post-hoc power analysis from a previous study on PCF prevalence revealed that a sample size of 41 anchors in each group achieves >80% power to detect a relative difference of 50% between the studied groups.4 Our study included n = 58 ASA and n = 44 PLLA anchors. All ASAs were placed on the medial row and PLLA anchors on the lateral row, so any force vectors were not standardized between the two anchor types. However, all patients underwent the same surgical treatment, and each patient served as their own control with medial and lateral anchor rows, thus reducing confounding factors. The number of anchors used in each row was not standardized. In some patients, the postoperative range of motion and strength scores were assessed after the MRI was performed, which could have influenced the assessment. There was also no protocol as to the timing of postoperative MRIs.
Conclusion
There was no significant difference in PCF incidence between ASAs and PLLA biocomposite anchors. At extended mean follow-up times of over two years, patients without PCF had significantly higher functional outcome scores. Range of motion and rotator cuff strength were equivalent between the two cohorts.
Disclaimers
Funding: This study was sponsored by Stryker Corporation, who provided funding for postoperative magnetic resonance imaging and research overhead.
Conflicts of interest: Aruna Seneviratne received financial support by Stryker Corporation for research overhead. The other authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors would like to thank Claudia Hogan, BA, Sasha Morledge, and Nada Abdallah, BA, for their assistance with data collection.
Footnotes
Institutional review board approval was received from Northwell Health (17-0332).
References
- 1.Amstutz H.C., Sew Hoy A.L., Clarke I.C. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981:7–20. [PubMed] [Google Scholar]
- 2.Busfield B.T., Glousman R.E., McGarry M.H., Tibone J.E., Lee T.Q. A biomechanical comparison of 2 technical variations of double-row rotator cuff fixation: the importance of medial row knots. Am J Sports Med. 2008;36:901–906. doi: 10.1177/0363546507312640. [DOI] [PubMed] [Google Scholar]
- 3.Carbonel I., Martinez A.A., Calvo A., Ripalda J., Herrera A. Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: a prospective randomized clinical study. Int Orthop. 2012;36:1877–1883. doi: 10.1007/s00264-012-1559-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung S.W., Lee Y.S., Kim J.Y., Lee J.H., Ki S.Y., Oh K.S. Changes in perianchor cyst formation over time after rotator cuff repair: influential factors and outcomes. Am J Sports Med. 2019;47:165–172. doi: 10.1177/0363546518810517. [DOI] [PubMed] [Google Scholar]
- 5.Freehill M.Q., Harms D.J., Huber S.M., Atlihan D., Buss D.D. Poly-L-lactic acid tack synovitis after arthroscopic stabilization of the shoulder. Am J Sports Med. 2003;31:643–647. doi: 10.1177/03635465030310050201. [DOI] [PubMed] [Google Scholar]
- 6.Galland A., Airaudi S., Gravier R., Le Cann S., Chabrand P., Argenson J.N. Pullout strength of all suture anchors in the repair of rotator cuff tears: a biomechanical study. Int Orthop. 2013;37:2017–2023. doi: 10.1007/s00264-013-1984-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goschka A.M., Hafer J.S., Reynolds K.A., Aberle N.S., Baldini T.H., Hawkins M.J. Biomechanical comparison of traditional anchors to all-suture anchors in a double-row rotator cuff repair cadaver model. Clin Biomech (Bristol, Avon) 2015;30:808–813. doi: 10.1016/j.clinbiomech.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Haneveld H., Hug K., Diederichs G., Scheibel M., Gerhardt C. Arthroscopic double-row repair of the rotator cuff: a comparison of bio-absorbable and non-resorbable anchors regarding osseous reaction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1647–1654. doi: 10.1007/s00167-013-2510-3. [DOI] [PubMed] [Google Scholar]
- 9.Hayes K., Walton J.R., Szomor Z.R., Murrell G.A. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47:289–294. doi: 10.1016/s0004-9514(14)60274-9. [DOI] [PubMed] [Google Scholar]
- 10.JG W., M C. Comparison of visual estimation and goniometry in determination of a shoulder joint angle. Physiotherapy. 1990;76:655–657. [Google Scholar]
- 11.Khoriati A.A., Antonios T., Gulihar A., Singh B. Single vs Double row repair in rotator cuff tears - a review and analysis of current evidence. J Clin Orthop Trauma. 2019;10:236–240. doi: 10.1016/j.jcot.2019.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim J.H., Kim Y.S., Park I., Lee H.J., Han S.Y., Jung S. A comparison of open-construct PEEK suture anchor and non-vented biocomposite suture anchor in arthroscopic rotator cuff repair: a prospective randomized clinical trial. Arthroscopy. 2019 doi: 10.1016/j.arthro.2019.08.049. [DOI] [PubMed] [Google Scholar]
- 13.Kim S.H., Kim D.Y., Kwon J.E., Park J.S., Oh J.H. Perianchor cyst formation around biocomposite biodegradable suture anchors after rotator cuff repair. Am J Sports Med. 2015;43:2907–2912. doi: 10.1177/0363546515608484. [DOI] [PubMed] [Google Scholar]
- 14.Kim S.H., Yang S.H., Rhee S.M., Lee K.J., Kim H.S., Oh J.H. The formation of perianchor fluid associated with various suture anchors used in rotator cuff repair: all-suture, polyetheretherketone, and biocomposite anchors. Bone Joint J. 2019;101-B:1506–1511. doi: 10.1302/0301-620X.101B12.BJJ-2019-0462.R2. [DOI] [PubMed] [Google Scholar]
- 15.Lee T.Q. Current biomechanical concepts for rotator cuff repair. Clin Orthop Surg. 2013;5:89–97. doi: 10.4055/cios.2013.5.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma H.L., Chiang E.R., Wu H.T., Hung S.C., Wang S.T., Liu C.L. Clinical outcome and imaging of arthroscopic single-row and double-row rotator cuff repair: a prospective randomized trial. Arthroscopy. 2012;28:16–24. doi: 10.1016/j.arthro.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Minagawa H., Yamamoto N., Abe H., Fukuda M., Seki N., Kikuchi K. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: from mass-screening in one village. J Orthop. 2013;10:8–12. doi: 10.1016/j.jor.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pilge H., Spang J., Rose T., Wolter H., Woertler K., Imhoff A.B. Osteolysis after rotator cuff repair with bioabsorbable anchors. Arch Orthop Trauma Surg. 2012;132:305–310. doi: 10.1007/s00402-011-1369-3. [DOI] [PubMed] [Google Scholar]
- 19.Richards R.R., An K.N., Bigliani L.U., Friedman R.J., Gartsman G.M., Gristina A.G. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 20.Ro K., Pancholi S., Son H.S., Rhee Y.G. Perianchor cyst formation after arthroscopic rotator cuff repair using all-suture-type, bioabsorbable-type, and PEEK-type Anchors. Arthroscopy. 2019;35:2284–2292. doi: 10.1016/j.arthro.2019.03.032. [DOI] [PubMed] [Google Scholar]
- 21.Sobhy M.H., Khater A.H., Hassan M.R., El Shazly O. Do functional outcomes and cuff integrity correlate after single- versus double-row rotator cuff repair? A systematic review and meta-analysis study. Eur J Orthop Surg Traumatol. 2018;28:593–605. doi: 10.1007/s00590-018-2145-7. [DOI] [PubMed] [Google Scholar]
- 22.Stahnke K., Nikulka C., Diederichs G., Haneveld H., Scheibel M., Gerhardt C. Serial MRI evaluation following arthroscopic rotator cuff repair in double-row technique. Arch Orthop Trauma Surg. 2016;136:665–672. doi: 10.1007/s00402-016-2409-9. [DOI] [PubMed] [Google Scholar]
- 23.Stein T., Mehling A.P., Ulmer M., Reck C., Efe T., Hoffmann R. MRI graduation of osseous reaction and drill hole consolidation after arthroscopic Bankart repair with PLLA anchors and the clinical relevance. Knee Surg Sports Traumatol Arthrosc. 2012;20:2163–2173. doi: 10.1007/s00167-011-1721-8. [DOI] [PubMed] [Google Scholar]
- 24.Thakkar R.S., Thakkar S.C., Srikumaran U., McFarland E.G., Fayad L.M. Complications of rotator cuff surgery-the role of postoperative imaging in patient care. Br J Radiol. 2014;87:20130630. doi: 10.1259/bjr.20130630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trantalis J.N., Boorman R.S., Pletsch K., Lo I.K. Medial rotator cuff failure after arthroscopic double-row rotator cuff repair. Arthroscopy. 2008;24:727–731. doi: 10.1016/j.arthro.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Van der Bracht H., Van den Langenbergh T., Pouillon M., Verhasselt S., Verniers P., Stoffelen D. Rotator cuff repair with all-suture anchors: a midterm magnetic resonance imaging evaluation of repair integrity and cyst formation. J Shoulder Elbow Surg. 2018;27:2006–2012. doi: 10.1016/j.jse.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Willemot L., Elfadalli R., Jaspars K.C., Ahw M.H., Peeters J., Jansen N. Radiological and clinical outcome of arthroscopic labral repair with all-suture anchors. Acta Orthop Belg. 2016;82:174–178. No doi. [PubMed] [Google Scholar]
- 28.Yakacki C.M., Poukalova M., Guldberg R.E., Lin A., Saing M., Gillogly S. The effect of the trabecular microstructure on the pullout strength of suture anchors. J Biomech. 2010;43:1953–1959. doi: 10.1016/j.jbiomech.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]