Scapulothoracic dissociation (SD) is a rare and serious type of trauma caused by musculoskeletal, vascular, and brachial plexus injuries owing to lateral displacement of the scapula with a strong blunt external force. The condition was first described by Oreck et al5 in 1984. Open SD (OSD) can be life-threatening.7,1 Herein, we report a case in which we assessed OSD for life-threatening complications as well as the condition of the upper limbs, which prompted life-saving forequarter amputation.
Case report
A 34-year-old man with no significant past medical history fell while riding a motorcycle at 80 km/h, which caused an open fracture of the left upper limb, and was urgently transported to our hospital 15 minutes after the injury occurred. He was a right-handed carpenter. Vital signs at the time of his visit were as follows: Glasgow Coma Scale, 15; body temperature, 36.6°C; blood pressure, 60/40 mmHg; heart rate, 170 beats per minute; respiratory rate, 36 beats per minute; SpO2, 100% with a mask providing 15 L/min oxygen. Immediately after transport, he was intubated and transfused with eight units of red blood cells owing to hemorrhagic shock.
Macroscopic findings showed a large open wound measuring 20 × 30 cm on his left shoulder (Fig. 1A). In addition, an open sternoclavicular joint dislocation was also observed, and the trunk and left upper limb were connected only via part of the pectoralis major and latissimus dorsi muscles. When the clavicle was inverted caudally, a stump of the subclavian artery was found 3 cm peripheral to the thyrocervical trunk bifurcation, and the site was occluded by a thrombus. The distal amputated end of the brachial plexus was identified in the upper limb (Fig. 1B). The color of the upper left limb was pale, and no movement was observed. A plain chest radiograph revealed lateral deviation of the left scapula of approximately 1.5 cm. Three-dimensional computed tomography showed a comminuted fracture of the scapular body and marked lateral displacement of the acromion (Fig. 2) but no thoracic damage. This case was diagnosed as traumatic OSD with a mangled extremity severity score (MESS)3 of 9 points and type 4 of Zelle classification.8
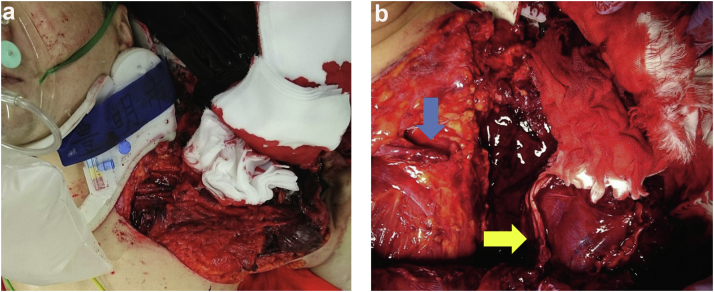
Figure 1.
Preoperative macroscopic findings of the left shoulder. (a) Anterior view, (b) the left shoulder with clavicle inverted caudally demonstrated a stump of the subclavian artery (blue arrow) and the brachial plexus (yellow arrow).
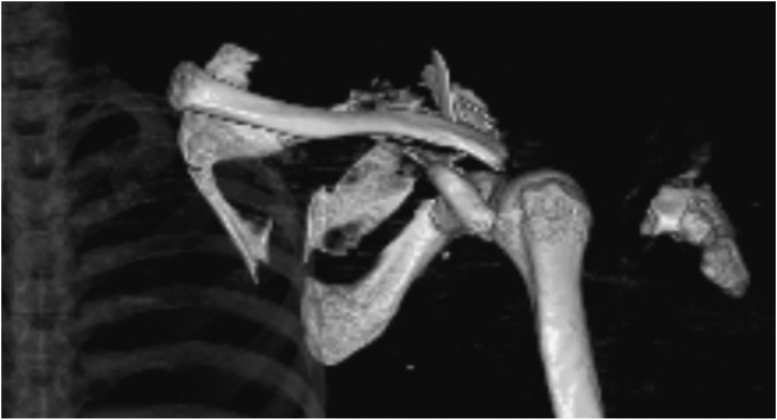
Figure 2.
Three-dimensional computed tomography images of the left shoulder demonstrate a comminuted fracture of the scapular body and marked lateral displacement of the acromion.
As the vascular surgeon determined that revascularization was impossible in this case because the subclavian artery injury was close to the vertebral artery, we performed emergency amputation of the left upper limb. During surgery, the subclavian artery stump was ligated, and the left upper limb was resected, including the clavicle and fractured portion of the scapula. The proximal stump of the brachial plexus was not treated due to risk of major bleeding. The pectoralis major and latissimus dorsi muscles were sutured to cover the scapula. To repair the skin, a full-thickness skin graft from the amputated limb was used. During surgery, the following fluids were administered: 10 units of red blood cells and 4 units of fresh frozen plasma. On postoperative day 3, a poor color tone of the skin graft due to hematoma was observed. Therefore, the skin graft was completely removed, and negative pressure wound therapy was initiated. At two weeks postoperatively, no obvious signs of infection were found, but partial necrosis of pectoralis major and latissimus dorsi muscles was observed. Coronal contrast computed tomography demonstrated the subclavian artery was interrupted after branching into the vertical artery and thyrocervical trunk (Fig. 3). The following types of collateral circulation were observed: pectoralis major muscle from the branch of the internal thoracic artery and latissimus dorsi muscle from the branch of the dorsal scapular artery and intercostal artery. Three weeks after the operation, the scapula and necrotic muscle were debrided, and we performed a meshed split-thickness skin graft from the thigh to cover the defect. After reoperation, no complications occurred, and the patient was discharged 1 month postoperatively. Two years after the operation, the wound was in good condition (Fig. 4), and 10 phantom limb pains remained on the visual analog scale. However, pain control was achieved with pregabalin and buprenorphine hydrochloride. He quit the job of the carpenter. He does not use a prosthetic limb in daily life.
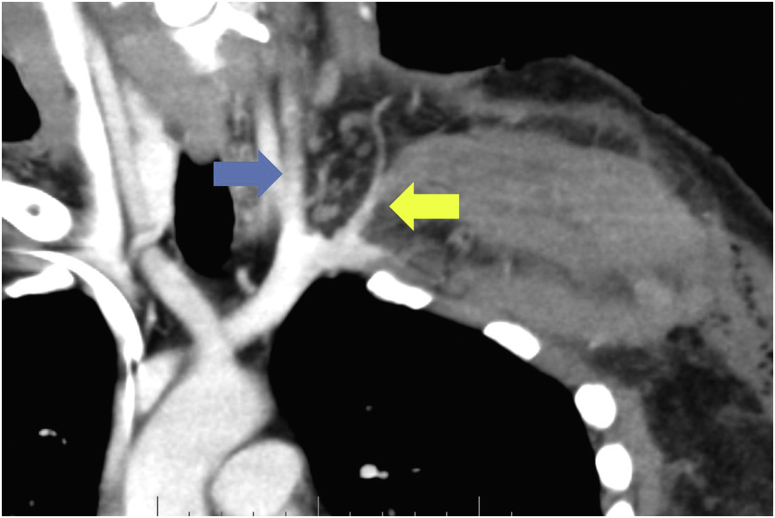
Figure 3.
Coronal contrast computed tomography demonstrate the interrupted subclavian artery after branching into the vertical artery (blue arrow) and thyrocervical trunk (yellow arrow).
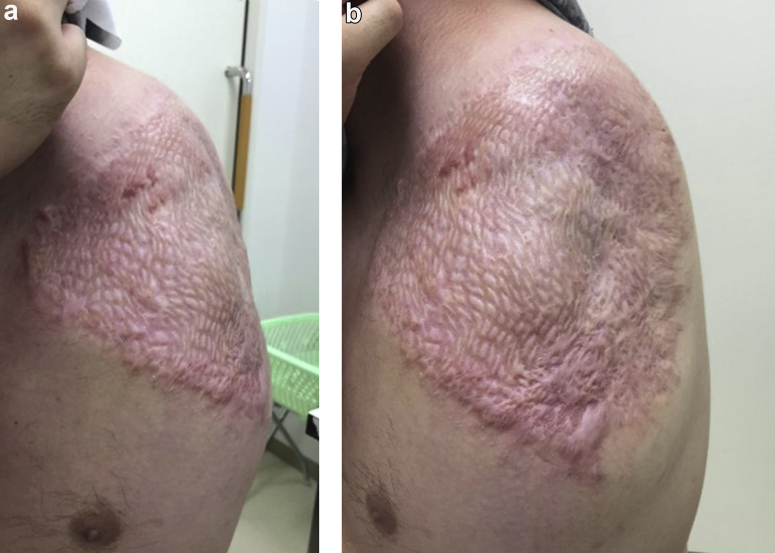
Figure 4.
Postoperative macroscopic findings of the left shoulder at the most recent follow-up. (a) Anterior view, (b) lateral view.
Discussion
SD, unlike scapular dislocation alone, is classified as traction trauma, and is also considered a closed amputation.2 In osteoarticular injuries with SD, it has been reported that 44% of sternoclavicular joint injuries, 24% of acromioclavicular joint dislocations, and 24% of sternoclavicular joint dislocations occur as complications.4 Although the incidence of vascular injury in SD has been reported to be 88%, ischemic necrosis of the upper limbs are complications in less than 10% of vascular injury cases because collateral circulation develops even in the presence of vascular injury.8 On the other hand, when complete brachial plexus avulsion also occurs, the functional recovery of the upper limbs tends to be poor, and upper limbs either remain nonfunctional or are amputated in most cases.8
In this case, there were no life-threatening head or thoracoabdominal complications. However, sternoclavicular joint dislocation, proximal and distal clavicle fractures, and scapular comminuted fractures were observed. The subclavian artery and brachial plexus were completely torn, and injuries were accompanied by severe soft-tissue damage owing to traction. In 1990, Johansen proposed the MESS as an early phase and objective means to evaluate use of amputation in lower limb trauma.3 Skeletal/soft-tissue injury, limb ischemia, shock, and patient age are factors affecting the MESS score, and cases with a score of 7 or higher are determined to have a high likelihood of requiring amputation.3 SD can also be classified using the Zelle classification, which assesses the degree of musculoskeletal, vascular, and neurologic injury.8 In this case, the MESS was 8 points and complete brachial plexus avulsion was observed; therefore, Zell classification was diagnosed as type 4. Amputation was selected in this case because the degree of soft-tissue damage in the musculoskeletal system was high, and blood flow through collateral circulation was not expected.
In cases of closed SD, amputation of the impaired limb is not considered, but in open cases, amputation of the impaired limb is considered beneficial because it is life-threatening and may leave a non-functional upper limb. Forequarter amputation was performed in this case. A report has shown that forequarter amputation was selected as a surgical procedure for bony and soft-tissue sarcomas that occurred in the proximal upper arm and from the thorax to the shoulder.6 In this case, when examined retrospectively, it is possible that reoperation could have been prevented by removing the proximal pectoralis major and latissimus dorsi muscles and the entire scapula.
Conclusion
We treated a patient with a life-threatening case of OSD with severe musculoskeletal injury via forequarter amputation. As an initial response to OSD, it is necessary to properly evaluate the condition of the upper limbs without overlooking life-threatening complications and risk of undergoing surgery.
Disclaimers
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
This study was approved by the Fujita Health University Ethics Review Committee (HM20-055).
References
- 1.Anbarasan A., Mohamad N.H., Mariapan S. Open traumatic scapulothoracic dissociation: case report of a rare injury. Trauma Case Rep. 2018;18:42–45. doi: 10.1016/j.tcr.2018.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ebraheim N.A., An H.S., Jackson W.T., Pearlstein S.R., Burgess A., Tscherne H. Scapulothoracic dissociation. J Bone Jt. 1988;70:428–432. [PubMed] [Google Scholar]
- 3.Helfet D.L., Howey T., Sanders R., Johansen K.J. Limb salvage versus amputation. Preliminary results of the mangled extremity severity score. Clin Orthop Relat Res. 1990;256:80–86. [PubMed] [Google Scholar]
- 4.Lee L.1, Miller T.T., Schultz E., Toledano B. Scapulothoracic dissociation. Am J Orthop. 1998;27:699–702. [PubMed] [Google Scholar]
- 5.Oreck S.L., Burgess A., Levine A.M. Traumatic lateral displacement of the scapula: a radiographic sign of neurovascular disruption. J Bone Joint Surg Am. 1984;66:758–763. [PubMed] [Google Scholar]
- 6.Rickelt J., Hoekstra H., van Coevorden F., de Vreeze R., Verhoef C., van Geel A.N. Forequarter amputation for malignancy. Br J Surg. 2009;96:792–798. doi: 10.1002/bjs.6555. [DOI] [PubMed] [Google Scholar]
- 7.Stepanovic Z.L., Milisavljevic S.S., Prodanovic N.S., Stahel P.F. Open scapulothoracic dissociation. J Trauma Acute Care Surg. 2015;79:698–700. doi: 10.1097/TA.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 8.Zelle B.A., Pape H.C., Gerich T.G., Garapati R., Ceylan B., Krettek C. Functional outcome following scapulothoracic dissociation. J Bone Joint Surg Am. 2004;86:2–8. doi: 10.2106/00004623-200401000-00002. [DOI] [PubMed] [Google Scholar]