Abstract
Background
Recently, magnetic resonance imaging (MRI) classification of medial ulnar collateral ligament (UCL) tears has been introduced, but little is known about the relationship between MRI grading and medial joint laxity. It has been reported that microscopy coils could make it possible to achieve high-resolution images of upper extremities with a superior diagnostic ability to conventional MRI. However, there is no report that has compared the diagnostic reliability between microscopic and conventional MRI. The purpose of this study was to assess the relationship between MRI findings and medial joint laxity evaluated with stress ultrasound (US). Secondary objective was to compare the reliabilities of UCL evaluation between microscopic and conventional MRI.
Methods
One-hundred thirty baseball players who underwent MRI of the elbow for the diagnosis of UCL injury using both conventional and microscopy MRI were included in this study. They also underwent stress US for assessment of medial joint laxity against valgus stress. Our MRI grading system for UCL injuries was compared to medial joint laxity evaluated with stress US. The intrarater and interrater reliabilities of our grading system were assessed with both microscopic and conventional MRI.
Results
Our grading system was related to valgus stability, especially with microscopic MRI. The reliabilities were fair when combined with microscopic MRI, which exhibited better intrarater and interrater reliabilities than conventional MRI.
Conclusion
High-resolution microscopic MRI may contribute to the accurate diagnosis of UCL injuries.
Keywords: Reliability, grading system, elbow, ulnar collateral ligament, microscopic MRI, ultrasound
In recent years, the number of major league baseball pitchers that have undergone ulnar collateral ligament (UCL) reconstruction has increased.2 Recent data have shown that UCL injuries are the leading disabled-list injury and require the highest cost of care for professional baseball players.5 Although the diagnosis of UCL injury should be made with a physical examination as well as imaging studies, surgeons tend to rely solely on magnetic resonance imaging (MRI) findings.4,11 However, there is no consensus on image sequences or a grading system for the diagnosis of UCL injury. We suppose that this might be a reason for the increase in the number of UCL reconstructions. Accurate diagnosis of UCL injury is essential to avoid unnecessary surgeries.
MRI has been widely used for diagnosis of UCL injury; however, there seem a couple of shortcomings. First, MRI is a static examination and do not provide functional or dynamic assessment of ligament laxity.1 Contrary to the static imaging modalities, ultrasound (US) can allow us to dynamically assess the ligament and has been used to quantify UCL insufficiency by adding valgus stress to the elbow joint.9 In addition, US has demonstrated the high diagnostic ability to identify UCL injury as accurately as MRI.3 However, there have been limited studies to evaluate the association between MRI findings of the UCL and medial joint laxity that is evaluated with the stress US.10
Another issue is the limited diagnostic ability of conventional MRI. Previous studies have shown that MRI using a conventional surface coil is a reliable tool for the diagnosis of UCL injury, especially to detect full-thickness tears of the UCL.7 On the other hand, a study demonstrated that conventional MRI has a low sensitivity in the diagnosis of partial-thickness tears.14 These findings indicate that conventional MRI may not be ideal for diagnosing both full- and partial-thickness tears.15 Recently, several authors have reported that the use of microscopy coils has made it possible to achieve high-resolution images of the wrist and elbow.16,17 High-resolution microscopic MRI of the wrist has demonstrated a superior diagnostic ability to conventional MRI.16 Moreover, the high-resolution MRI has been reported to have the potential to clearly depict lesions in the elbow.17 We have been using MRI with a microscopy coil to assess UCL injury with the use of an original grading system. However, this grading system has not been validated, and there is no report that has compared the diagnostic reliability between microscopic and conventional MRI.
This study aimed to assess the relationship between MRI findings and medial joint laxity evaluated with stress US. This study also aimed to compare the reliabilities of UCL evaluation between microscopic and conventional MRI. We hypothesized that MRI findings would be associated with medial joint laxity and that microscopic MRI would exhibit better intrarater and interrater reliabilities than conventional MRI in the assessment of UCL injuries using our grading system.
Materials and methods
This study was conducted at a single orthopedic sports medicine center, which specializes in shoulder and elbow surgery. The institutional review board of our institute approved the study protocol. We retrospectively searched patients’ records to collect subjects of this study. The inclusion criteria were baseball players who underwent 1) MRI of the elbow for the diagnosis of UCL injury using both conventional and microscopy MRI between April 2014 and September 2018 and 2) stress US for assessment of medial joint laxity against valgus stress. Exclusion criteria were as follows: 1) prior surgical treatment, 2) previous traumatic UCL injury, and 3) poor MRI quality (Fig. 1).
Figure 1.
Patient selection. MRI, magnetic resonance imaging; UCL, ulnar collateral ligament.
Magnetic Resonance Imaging
Image acquisition was performed without any contrast agents, using 1.5-Tesla MRI (Intera 1.5-T; Phillips, Amsterdam, the Netherlands). Patients were in the supine position with the forearm fully supinated, keeping the elbow in the isocenter of the magnet (Fig. 2A).17
Figure 2.
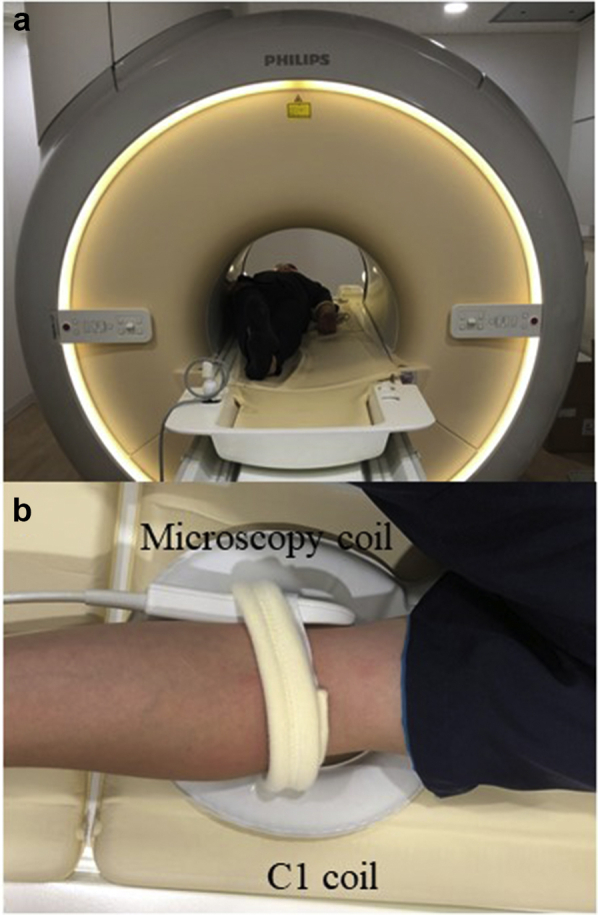
The setting for magnetic resonance imaging. (a) The subject was set in the supine position with the forearm fully supinated. (b) A microscopy coil was positioned at the medial side of the elbow, and a synergy flexible C1 coil under the elbow joint.
For the microscopic MRI, a 47-mm microscopy surface coil (microscopy coil; Philips Medical Systems, Best, The Netherland) and a 17-cm synergy flexible coil (C1 coil; Philips Medical Systems, Best, The Netherland) were simultaneously used according to previous research (Fig. 2B).17 Coronal images were acquired with a 1.5-mm slice thickness, 0-mm slice gap, and 70-mm field of view in the following sequences: proton density-weighted images (PDWI; repetition time [TR], 2000 ms; echo time [TE], 11 ms) and proton density fat-saturated images with spectral adiabatic inversion recovery (TR, 5000 ms; TE, 13 ms).
For the conventional MRI, coronal images with only a C1 coil were acquired with a 3-mm slice thickness, 0.3-mm slice gap, and 150-mm field of view in the following sequences: T1-weighted image (TR, 700 ms; TE 12 ms), T2-weighted image (TR, 5500 ms; TE 100 ms), and PDWI (TR, 1200 ms; TE, 13 ms) (Table I).
Table I.
Summary of magnetic resonance imaging sequences.
| Coil | Sequences | FOV (mm) | TR (ms) | TE (ms) | Thickness (mm) | TSE | NSA | Matrix |
|---|---|---|---|---|---|---|---|---|
| Microscopy coil | PDWI | 70 | 2000 | 11 | 1.5 | 10 | 3 | 224 |
| PD SPAIR | 70 | 5000 | 13 | 1.5 | 13 | 3 | 192 | |
| C1 coil | T1WI | 150 | 700 | 12 | 3 | 4 | 3 | 256 |
| T2WI | 150 | 5500 | 100 | 3 | 16 | 4 | 368 | |
| PDWI | 120 | 1800 | 30 | 3 | 11 | 2 | 320 |
T1WI, T1-weighted image; T2WI, T2-weighted image; PDWI, proton density-weighted image; PD SPAIR, proton density fat-saturated image with spectral adiabatic inversion recovery; FOV, field of view; TR, repetition time; TE, echo time; TSE, turbo spin echo; NSA, number of samples averaged.
MRI evaluation
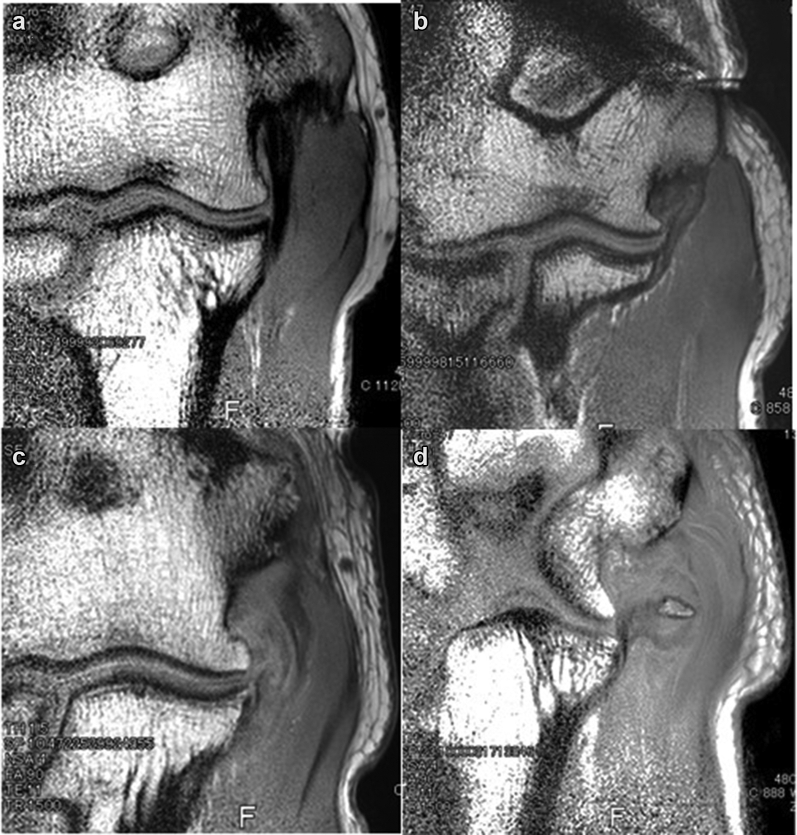
Coronal PDWIs were used to evaluate the UCL.17 The UCL was evaluated using an original grading system: grade I, intact ligament (Fig. 3A); grade II, low-grade, high-signal intensity in the UCL without tear (Fig. 3B); grade III, high-grade, high-signal intensity in the UCL or partial tear (Fig. 3C); grade IV, no ligamentous tissue or full-thickness tears of the UCL (Fig. 3D).
Figure 3.
The grading system of the ulnar collateral ligament (UCL) injury. (a) Grade I, intact ligament; (b) grade II, low-grade high signal intensity in the UCL without tear; (c) grade III, high-grade high signal intensity in the UCL or partial tear of the UCL; (d) grade IV, no ligamentous tissue or full-thickness tear of the UCL.
Two fellowship-trained shoulder and elbow surgeons (T.I. and Y.T.) independently evaluated both microscopic and conventional MRI using the grading scale. They were blinded to any clinical information about the patients. When the grades disagreed, the final grade was determined based on the 3 surgeons’ consensus. For intrarater reliability, one of the surgeons (M.I.) evaluated MRI twice at >4-week intervals.
Ultrasonographic imaging technique
All US scans were performed by one of 2 radiologists or one experienced orthopedic surgeon (S.H.) using a US scanner (EUB-7500; Hitachi Medical, Tokyo, Japan) with a 14-MHz linear transducer. Each subject was placed in the supine position on a bed with the shoulder at 90° of abduction, the elbow at 90° flexion, and the forearm in the neutral position according to the previous study.12 All angles were measured using a goniometer, and the transducer was placed on the oblique coronal plane to visualize the medial joint distance (MJD) (Fig. 4A). The MJD was measured as the distance between the distal-medial corner of the humeral trochlea and the proximal edge of the sublime tubercle of the ulna (Fig. 4B). The distance was measured on the US screen with the use of electronic calipers with a precision of 0.1 mm. The measurements were performed 3 times each in 2 conditions: the forearm on a table (no stress) or without any support (gravity stress) and means of the 3 measurements were calculated for each condition. MJD changes, which was the difference of MJD between the 2 conditions, were used for analysis.1,3
Figure 4.

The stress ultrasound (US) examination of the medial elbow. (a) The subject was placed in the supine position with the shoulder at 90° of abduction, the elbow at 90° flexion, and the forearm in a neutral position. The US images are obtained from the medial side of the elbow. (b) The medial joint distance was measured as the distance between the distal-medial corner of the humeral trochlea (TR) and the proximal edge of the sublime tubercle (ST) of the ulna (asterisks), in millimeters, from the images in nonstress and valgus stress conditions. MEC, medial epicondyle; Med, medial; Dist, distal.
Statistical analysis
MJD changes were compared among each MRI grade. One-way analysis of variance and the Tukey post hoc test were used for comparison of MJD changes among MRI grades, and the level of significance was set at P < .05. The kappa coefficient was used to assess intrarater and interrater reliability as well as the grading correlation between microscopic and conventional MRI. The strength of correlation was categorized according to Landis and Koch8: a kappa value of 0.00–0.20, slight; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, substantial; and 0.81–1.00, almost perfect. All analyses were performed with IBM SPSS Statistics 18 software for Windows (IBM Japan Inc., Tokyo, Japan).
Results
One hundred thirty-five baseball players met the inclusion criteria (Fig. 1). Five subjects were excluded: prior surgical treatment, 1; previous traumatic UCL injury, 2; poor MRI quality, 2. The remaining 130 players with a mean age of 20 years (range, 15–39) were included in this study. Table II summarizes the demographic characteristics of the patients.
Table II.
Patient demographics.
| Demographics | Data |
|---|---|
| Number of elbows | 130 |
| Age, mean (range) | 20 yr (15–39) |
| Affected side | |
| Right | 82 |
| Left | 48 |
| Level of sport | |
| Junior high school | 30 |
| High school | 34 |
| Collegiate | 16 |
| Professional | 50 |
| Position | |
| Pitcher | 102 |
| Catcher | 6 |
| Outfielder | 22 |
With the conventional MRI, 21 (16%) elbows were rated as grade I, 56 (43%) elbows as grade II, 41 (32%) elbows as grade III, and 12 (9%) as grade IV (Table III). MJD changes were significantly related to the MRI grades (P < .001): grade I, 0.5 ± 0.3 mm (range, 0.1–1.3); grade II, 0.8 ± 0.5 mm (range, 0–2.5); grade III, 0.9 ± 0.4 mm (range, 0–2.1); grade IV, 1.8 ± 1.4 mm (range, 0–4.5) (Fig. 5). The post-hoc test detected significant differences between grade I and III (P = .002), grade I and IV (P = .02), and grade III and IV (P = .002). With the microscopic MRI, 32 (25%) elbows were rated as grade I, 55 (42%) elbows as grade II, 31 (24%) elbows as grade III, and 12 (9%) elbows as grade IV. MJD changes significantly increased with the MRI grades (P < .001): grade I, 0.2 ± 0.3 mm (range, 0–1); grade II, 0.7 ± 0.2 mm (range, 0.2–1.1); grade III, 1.3 ± 0.3 mm (range, 0.2–1.8); grade IV, 2.3 ± 0.9 mm (range, 1.5–4.5). All pairs of the grades showed a significant difference in MJD with the post-hoc test (P < .001 for each).
Table III.
MRI grading of the ulnar collateral ligament.
| UCL grade | Conventional MRI | Microscopic MRI |
|---|---|---|
| I | 21 (16%) | 38 (29%) |
| II | 56 (43%) | 49 (38%) |
| III | 41 (32%) | 31 (24%) |
| IV | 12 (9%) | 12 (9%) |
MRI, magnetic resonance imaging; UCL, ulnar collateral ligament.
Figure 5.
Box plots for comparison of medial joint distance changes among grades. (a) Conventional magnetic resonance imaging (MRI). (b) Microscopic MRI. Medial joint distance (MJD) changes significantly increased with the MRI grades in both microscopic and conventional MRI (P < .001 for both).
The correlations between the conventional MRI and microscopic MRI were 0.39 (examiner 1) and 0.23 (examiner 2). Grades were agreed only in 60 (46%) elbows (Table IV): grade I (microscopy MRI), 14/38 (37%); grade II, 26/49 (53%); grade III, 13/31 (42%); grade IV, 7/12 (58%). Furthermore, the intrarater reliabilities of the grading system for the conventional MRI and microscopy MRI were 0.29 and 0.47, respectively, while the interrater reliabilities were 0.11 and 0.55, respectively.
Table IV.
Relationship of grades between conventional and microscopy magnetic resonance imaging (MRI).
| UCL grading | Conventional MRI |
||||
|---|---|---|---|---|---|
| I | II | III | IV | ||
| Microscopy MRI | I | 14 | 16 | 8 | 0 |
| II | 6 | 26 | 15 | 2 | |
| III | 1 | 14 | 13 | 3 | |
| IV | 0 | 0 | 5 | 7 | |
Discussion
The most important finding in this study was that our MRI grading of the UCL was correlated with medial elbow joint stability against valgus stress, especially in evaluation with the microscopic MRI. The grading system demonstrated fair reliability when combined with microscopic MRI, while the conventional MRI showed poorer intrarater and interrater reliabilities than the microscopic MRI, confirming our hypothesis.
In the present study, we revealed that the MRI grading system for UCL injury was significantly correlated with valgus stability evaluated with stress US. Besides, microscopic MRI showed smaller data ranges in each grade than conventional MRI as shown in Fig. 4. This means that the grading in combination with microscopic MRI could more clearly reflect valgus stability of the elbow. The high-resolution images of microscopic MRI possibly contributed to the clinically relevant evaluation of UCL injury.16,17
There has been a variety of grading systems to evaluate the location or degree of UCL injuries.4,11 The location of UCL injuries is usually divided into 3 portions: proximal, mid-substance, and distal.4,11 Partial tears are sometimes divided into 2 grades, low and high, according to the depth of tears.4 High-grade partial or distal tears, as well as complete tears, are thought to be surgical indications because nonoperative management sometimes fails.4,11 However, it is still controversial as to whether the systems that evaluate the location or degree of UCL injuries are clinically meaningful, especially since asymptomatic high-grade partial or distal tears have been reported in baseball players.7 The grading system in this study classified the status of the UCL regardless of tear sites or depth of partial tears. As a result, the intrarater and interrater reliabilities were fair when combined with microscopic MRI. Although the relationship between the grades and symptoms was not investigated, further study is needed to determine the relationship between the grades and symptoms or success rates of treatments.
MRI evaluation of the elbow presents some difficulties because of its size when compared to the sizes of larger joints such as the knee and hip joints.6,13 Thinner slices are necessary to sufficiently evaluate smaller structures in the elbow, including the UCL. Recently, an MRI study reported that images with a smaller slice thickness can be better obtained with a microscopy coil than with a conventional coil.16,17 In this study, we acquired high-resolution images with a 1.5-mm slice thickness using a microscopy coil, which might have contributed to the better intrarater and interrater reliabilities seen with the microscopic MRI than those seen with the conventional MRI.
It is also believed that contrast agents are necessary to identify partial UCL tears.14 However, many reports promote MRI as a noninvasive method of UCL evaluation without contrast agents.11 Microscopic MRI shows potential in detecting partial UCL tears without contrast agents because of the high-resolution images. Although the potential to obtain high-resolution images may be a strength of microscopic MRI, the ability to evaluate deep structures is limited due to the low signal to noise ratio.16 Therefore, there may be a difficulty to assess the ligament of large, fat elbows with microscopic MRI.
There were a few limitations in this study. First, the diagnostic accuracy was not confirmed because no patients had undergone surgical treatment on their elbows. Second, only coronal PDWIs were used to compare the reliabilities between the microscopic MRI and conventional MRI. The UCL was also demonstrated well on axial images, and other sequences may have a higher diagnostic potential.17 Finally, the relationship between the grades and symptoms was not assessed. Regardless of these limitations, we believe that this study may provide important information on diagnosis of UCL injury in baseball players.
Conclusions
The MRI grading system for UCL injury demonstrated a significant correlation with valgus stability evaluated with stress US. The better correlation was observed when evaluated using microscopic MRI. Microscopic MRI also exhibited better intrarater and interrater reliabilities than conventional MRI. The high-resolution microscopic MRI may contribute to the accurate diagnosis of UCL injuries.
Disclaimers
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors are grateful to Koharu Matsuki for English language editing.
Footnotes
Institutional review board approval was received from Funabashi Orthopaedic Hospital (IRB number:2020059). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Ciccotti M.G., Atanda A., Jr., Nazarian L.N., Dodson C.C., Holmes L., Cohen S.B. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med. 2014;42:544–551. doi: 10.1177/0363546513516592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conte S.A., Fleisig G.S., Dines J.S., Wilk K.E., Aune K.T., Patterson-Flynn N., ElAttrache N. Prevalence of ulnar collateral ligament Surgery in professional baseball players. Am J Sports Med. 2015;43:1764–1769. doi: 10.1177/0363546515580792. [DOI] [PubMed] [Google Scholar]
- 3.De Smet A.A., Winter T.C., Best T.M., Bernhardt D.T. Dynamic sonography with valgus stress to assess elbow ulnar collateral ligament injury in baseball pitchers. Skeletal Radiol. 2002;31:671–676. doi: 10.1007/s00256-002-0558-0. [DOI] [PubMed] [Google Scholar]
- 4.Frangiamore S.J., Lynch T.S., Vaughn M.D., Soloff L., Forney M., Styron J.F. Magnetic resonance imaging Predictors of failure in the Nonoperative management of ulnar collateral ligament injuries in professional baseball pitchers. Am J Sports Med. 2017;45:1783–1789. doi: 10.1177/0363546517699832. [DOI] [PubMed] [Google Scholar]
- 5.Gutierrez N.M., Granville C., Kaplan L., Baraga M., Jose J. Elbow MRI findings do not correlate with Future Placement on the disabled list in asymptomatic professional baseball pitchers. Sports Health. 2017;9:222–229. doi: 10.1177/1941738117701769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoshika S., Nimura A., Yamaguchi R., Nasu H., Yamaguchi K., Sugaya H. Medial elbow anatomy: a paradigm shift for UCL injury prevention and management. Clin Anat. 2019;32:379–389. doi: 10.1002/ca.23322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kooima C.L., Anderson K., Craig J.V., Teeter D.M., van Holsbeeck M. Evidence of subclinical medial collateral ligament injury and posteromedial impingement in professional baseball players. Am J Sports Med. 2004;32:1602–1606. doi: 10.1177/0363546503262646. [DOI] [PubMed] [Google Scholar]
- 8.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 9.Nazarian L.N., McShane J.M., Ciccotti M.G., O'Kane P.L., Harwood M.I. Dynamic US of the anterior band of the ulnar collateral ligament of the elbow in asymptomatic major league baseball pitchers. Radiology. 2003;227:149–154. doi: 10.1148/radiol.2271020288. [DOI] [PubMed] [Google Scholar]
- 10.Park J.Y., Kim H., Lee J.H., Heo T., Park H., Chung S.W. Valgus stress ultrasound for medial ulnar collateral ligament injuries in athletes: is ultrasound alone enough for diagnosis? J Shoulder Elbow Surg. 2020;29:578–586. doi: 10.1016/j.jse.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 11.Ramkumar P.N., Frangiamore S.J., Navarro S.M., Lynch T.S., Forney M.C., Kaar S.G. Interobserver and Intraobserver reliability of an MRI-based classification system for injuries to the ulnar collateral ligament. Am J Sports Med. 2018;46:2755–2760. doi: 10.1177/0363546518786970. [DOI] [PubMed] [Google Scholar]
- 12.Sasaki J., Takahara M., Ogino T., Kashiwa H., Ishigaki D., Kanauchi Y. Ultrasonographic assessment of the ulnar collateral ligament and medial elbow laxity in college baseball players. J Bone Joint Surg Am. 2002;84:525–531. doi: 10.2106/00004623-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Steinborn M., Heuck A., Jessel C., Bonel H., Reiser M. Magnetic resonance imaging of lateral epicondylitis of the elbow with a 0.2-T dedicated system. Eur Radiol. 1999;9:1376–1380. doi: 10.1007/s003300050851. [DOI] [PubMed] [Google Scholar]
- 14.Timmerman L.A., Schwartz M.L., Andrews J.R. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med. 1994;22:26–31. doi: 10.1177/036354659402200105. discussion 32. [DOI] [PubMed] [Google Scholar]
- 15.Yoshida M., Goto H., Takenaga T., Tsuchiya A., Sugimoto K., Musahl V. Anterior and posterior bands of the anterior bundle in the elbow ulnar collateral ligament: ultrasound anatomy. J Shoulder Elbow Surg. 2017;26:1803–1809. doi: 10.1016/j.jse.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 16.Yoshioka H., Ueno T., Tanaka T., Shindo M., Itai Y. High-resolution MR imaging of triangular fibrocartilage complex (TFCC): comparison of microscopy coils and a conventional small surface coil. Skeletal Radiol. 2003;32:575–581. doi: 10.1007/s00256-003-0672-7. [DOI] [PubMed] [Google Scholar]
- 17.Yoshioka H., Ueno T., Tanaka T., Kujiraoka Y., Shindo M., Takahashi N. High-resolution MR imaging of the elbow using a microscopy surface coil and a clinical 1.5 T MR machine: preliminary results. Skeletal Radiol. 2004;33:265–271. doi: 10.1007/s00256-004-0763-0. [DOI] [PubMed] [Google Scholar]