Abstract
Background
Non-operative treatment of uncomplicated appendicitis is safe and increasing in popularity, but has other risks and benefits compared with appendicectomy. This study aimed to explore the preference of the general population regarding operative or antibiotic treatment of uncomplicated appendicitis.
Methods
In this prospective study, a clinical scenario and questionnaire were submitted to a panel comprising a sample of an average adult population. The survey was distributed by an independent, external research bureau, and included a comprehensive explanation of the risks and benefits of both treatment options. The primary outcome was the proportion of participants who would prefer antibiotics over surgery. Secondary outcomes were reasons for this preference and the accepted recurrence rate within 1 year when treated with antibiotics only. All outcomes were weighted for the average Dutch population.
Results
Of 254 participants, 49.2 per cent preferred antibiotic treatment for uncomplicated appendicitis, 44.5 per cent preferred surgery, and 6.3 per cent could not make a decision. About half of the participants preferring antibiotics would accept a recurrence risk of more than 50 per cent within 1 year. Avoiding surgery was their main reason. In participants preferring surgery, many tolerated a recurrence risk of no more than 10 per cent when treated with antibiotics. Removal of the cause of appendicitis was their main reason.
Conclusion
Around half of the average population sample preferred antibiotics over surgical treatment of uncomplicated appendicitis and were willing to accept a high recurrence risk to avoid surgery initially. Participants who preferred surgery tolerated only a very low recurrence risk with antibiotic treatment.
This study examined the preference for treatment of uncomplicated appendicitis in 254 participants. Two clearly separated preference groups were identified. Half of the participants (49.2 per cent) preferred antibiotic treatment and the majority of these were willing to accept a risk of recurrence of appendicitis of 50 per cent or higher within 1 year, whereas the majority of the participants who chose surgery would accept a recurrence risk of only 10 per cent as a maximum.
Introduction
Non-operative treatment for suspected uncomplicated appendicitis has been a hot topic in the past decade. Studies1,2 have shown that initial antibiotic treatment without surgery can be just as safe and effective as surgical treatment by appendicectomy. Appendicectomy has an 8 per cent risk of postoperative complications in patients with uncomplicated appendicitis3. Complication risks are lower for antibiotic treatment, but there is a 1-year recurrence risk of about 23 per cent, increasing to almost 40 per cent in the first 5 years4,5. Guidelines6–10 recommend laparoscopic operative treatment as standard, although latest versions7–10 also consider antibiotic treatment as an alternative to surgery if there is low suspicion of gangrenous or perforated appendicitis and the patient is aware of the recurrence risk. In fact, the Royal College of Surgeons11 stated in 2017 that ‘antibiotic treatment is already offered by many British surgeons’. To be able to discuss both therapies with a patient, an understanding of their perspectives about treatment options, and their view of the risks and benefits, is essential.
Few studies have evaluated patients’ preferences in the treatment of uncomplicated appendicitis. A wide range from 9.4 to 57 per cent of patients preferring antibiotic over surgical treatment has been reported12–14. However, these studies appear to be biased owing to the type of participants included. The populations questioned vary from visitors and patients (without appendicitis) presenting at the emergency department14 to medical students12 or a randomly assigned cohort recruited through social media or at public venues13, making it hard to translate these results to the general population. Survey design or interview structure can also influence the study results. Ideally, information is needed about appendicitis treatment preferences of the average population; that is, those who may experience appendicitis in future.
This study aimed to explore the preference for surgical or antibiotic management of uncomplicated appendicitis in a sample of the average Dutch population.
Methods
A web-based survey was developed, with a scenario of a patient presenting with uncomplicated appendicitis. Information on treatment options with associated risks and benefits was provided in a stepwise manner, alternating with questions about treatment preference. After being fully informed, the participant had to choose between ‘antibiotic treatment’, ‘surgery’ or ‘I could not make a decision’. Participants were then asked to substantiate their choice based on 10 listed arguments using a seven-point Likert scale (1, very unimportant; 7, very important) and to rank their top three reasons for treatment preference from the listed arguments. Finally, participants were asked what recurrence risk of appendicitis after 1 year they would accept if treated with antibiotics. All background information provided was extracted from systematic reviews, RCTs, and national data. The full questionnaire and list of arguments is available in Appendix S1.
Baseline characteristics
The following baseline characteristics of each participant were collected: age, sex, socioeconomic status (education, profession, income), history of abdominal surgery, general anaesthesia, appendicitis, intravenous antibiotics or a medical complication in the hospital. Participants were asked whether they were a nurse or doctor.
Participant recruitment
The recruitment of participants was done by No Ties (Zekeringstraat, Amsterdam), an independent external research bureau. Participants were members of the inVotes panel of No Ties. This panel consists of approximately 50 000 members, recruited on a diversity of websites. Of these, 25 000–30 000 are considered active panel members. Members of the inVotes panel have to update their profile data annually, or are excluded from further participation. Participants are rewarded by points, collected for each study in which they participate. These points can be cashed in several online shops, or online gift cards. The panel is certificated by the International Organization of Standardization. No Ties follows the rules of the Centre for Marketing Intelligence and Research.
Sample size
Based on the literature, the expected range of the population preferring antibiotics could vary from 9 to 57 per cent. The broadest confidence interval is expected for an expected proportion of 50 per cent. For a proportion of 50 per cent preferring antibiotics with an absolute precision of 10 per cent and a 95 per cent confidence interval, 97 participants would be needed. For an absolute precision of 5 per cent, 385 patients would be needed. A study population of 250 participants would give an absolute precision of 6.2 per cent, which was chosen for pragmatic reasons and provided an acceptable error margin for the study goal.
Outcomes and analysis
The primary outcome was the proportion of participants who would prefer antibiotic treatment. Secondary outcomes were the most important reasons for their preference. The rankings of these arguments were presented as bar plots and percentages. The answers from the Likert-scale matrix questions were expressed as means and depicted in a bar plots for each subgroup. The proportion of accepted recurrence within 1 year was expressed as the first percentage crossing the median. In addition, the proportion of participants accepting a recurrence risk of appendicitis comparable to the actual risk of 22.6 per cent in the literature was calculated.
All outcomes and results were weighted to mimic the average Dutch population, according to the standard of the national Centre for Marketing Intelligence and Research. Weighting features included sex, age group, social class, and residential area. Differences between groups were calculated as odds ratios with 95 per cent confidence intervals. The mean difference with 95 per cent confidence interval was calculated for normally distributed continuous data.
Results
In total, 808 members of the inVotes panel were approached between 17 April 2020 and 23 April 2020. Of these, 254 (31.4 per cent) completed the survey. All results are reported after weighting. In total, 50.0 per cent of participants were men and the mean (s.d.) age was 49 (17) years (Table 1). Of the 254 participants, 113 (44.5 per cent) preferred surgical treatment, 125 (49.2 per cent) preferred antibiotic treatment, and 16 (6.3 per cent) were undecided.
Table 1.
Baseline characteristics
| All participants (n = 254)* | Prefer surgical treatment (n = 113)* | Prefer antibiotic treatment (n = 125)* | Odds ratio ‡ | |
|---|---|---|---|---|
| Age (years)† | 49(17) | 47(17) | 50(17) | 3.19 (–1.21, 7.60)§ |
| Male sex | 127 (50) | 60 (53) | 63 (50) | 1.11 (0.67, 1.85) |
| History of abdominal surgery | 69 (27) | 36 (32) | 29 (23) | 1.57 (0.88, 2.78) |
| History of anaesthesia | 180 (71) | 84 (74) | 85 (68) | 1.36 (0.78, 2.40) |
| History of appendicitis | 27 (11) | 17 (15) | 9 (7) | 2.31 (0.98, 5.41) |
| History of intravenous antibiotics | 76 (30) | 38 (34) | 31 (25) | 1.54 (0.88, 2.70) |
| History of a medical complication | 29 (11) | 15 (13) | 13 (10) | 1.32 (0.60, 2.91) |
| Works or has worked as nurse or doctor | 13 (5) | 3 (3) | 6 (5) | 0.54 (0.13, 2.22) |
Values in parentheses are percentages unless indicated otherwise; * Numbers and percentages are shown after weighting to mimic the average Dutch population. †Values are mean(s.d.); ‡values in parentheses are 95 per cent confidence intervals. §Mean difference.
When asked for an acceptable recurrence risk after initial antibiotic treatment, the majority (55.5 per cent) of all participants would accept a risk of 31 per cent or higher for recurrent appendicitis (Table 2). Moreover, 63.4 per cent of all participants would accept a recurrence risk higher than 21 per cent, resembling the recurrence risk described in the literature.
Table 2.
Treatment preference in relation to risk of recurrent appendicitis
| Acceptable risk of recurrent appendicitis (%) | All participants (n = 254)* | Prefer surgical treatment (n = 113)* | Prefer antibiotic treatment (n = 125)* |
|---|---|---|---|
| 0 (would always prefer surgery) | 54 (22) | 51 (46) | 1 (1) |
| 1–10 | 14 (6) | 11 (10) | 3 (3) |
| 11–20 | 24 (9) | 16 (14) | 7 (6) |
| 21–30 | 20 (8) | 11 (10) | 6 (5) |
| 31–40 | 27 (11) | 5 (5) | 19 (15) |
| 41–50 | 24 (9) | 4 (4) | 17 (14) |
| 51–60 | 29 (11) | 6 (5) | 21 (17) |
| 61–70 | 15 (6) | 1 (1) | 14 (11) |
| 71–80 | 18 (7) | 3 (2) | 14 (11) |
| 81–90 | 7 (3) | 3 (3) | 4 (3) |
| 91–99 | 5 (2) | 1 (1) | 4 (3) |
| 100 (would always prefer antibiotics) | 16 (6) | 0 (0) | 14 (11) |
Values in parentheses are percentages unless indicated otherwise; * numbers and percentages are shown after weighting to mimic the average Dutch population.
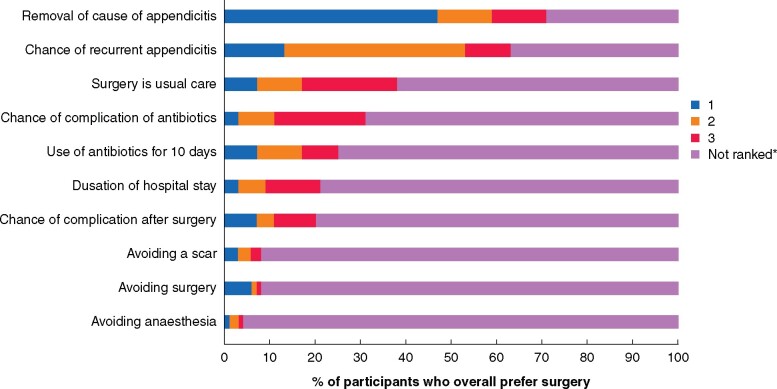
Participants preferring surgical treatment
Among participants preferring surgical treatment, ‘removal of the cause of appendicitis by surgery’ was ranked among the top three reasons by 70.7 per cent and in 46.7 per cent it was ranked as the most important argument (Fig. 1). ‘The chance of recurrent appendicitis’ was ranked in the top three reasons by 62.9 per cent. ‘The fact that surgery is usual care’ was the third most important argument and ranked among the top three reasons by 38.1 per cent. The majority (55.2 per cent) of participants preferring surgical treatment would only accept antibiotic treatment without surgery at a risk of recurrent appendicitis of 10 per cent or less (Table 2). About one-third of participants preferring surgical treatment nevertheless would accept antibiotic treatment at a recurrence risk of at least 21 per cent.
Fig. 1.
Ranking of reasons for treatment choice of participants who overall prefer surgery
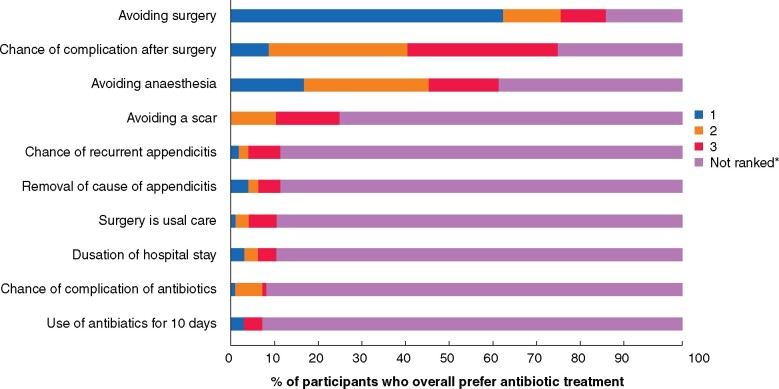
Participants preferring antibiotic treatment
Among participants preferring antibiotic treatment, ‘avoiding surgery’, was ranked among the top three reasons by 83.1 per cent, and 60.1 per cent ranked it as most important (Fig. 2). ‘The chance of a complication after surgery’ and ‘avoiding anaesthesia’ were ranked in the top three reasons by 72.1 per cent and 58.8 per cent respectively. The majority (56.8 per cent) of participants preferring antibiotic treatment would accept a risk of more than 50 per cent for recurrent appendicitis if antibiotic treatment was given (Table 2). Finally, 90.9 per cent of participants preferring antibiotic treatment would accept an appendicitis recurrence risk of 21 per cent or more.
Fig. 2.
Ranking of reasons for treatment choice of participants who overall prefer antibiotic treatment
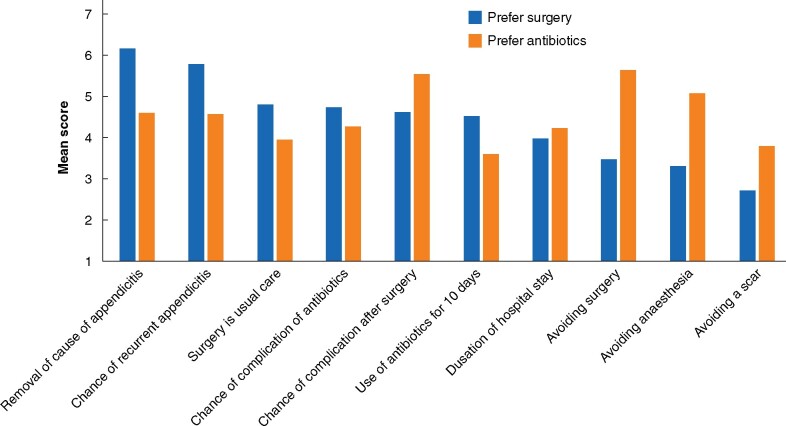
Mean reason-for-preference scores
The mean scores for each reason for preferring antibiotic treatment or surgical treatment are shown in Fig. 3. The only reason that scored under 4 (neutral) in both preference groups, was ‘avoiding a scar’.
Fig. 3.
Mean scores for reasons for participants preferring surgery or antibiotics
Score 1, very unimportant; 4, neutral; 7, very important.
Discussion
The present study has shown that, when choosing surgical or antibiotic treatment for uncomplicated appendicitis, there are two distinct preference groups that accept divergent risks of recurrence of appendicitis after antibiotic treatment without surgery. Approximately half of participants reflecting the average Dutch population preferred antibiotic over surgical treatment. The majority of these participants accepted a risk of recurrent appendicitis of 50 per cent or more within 1 year. Avoiding surgery was the most essential reason for participants to prefer antibiotic treatment. On the other hand, the majority of participants preferring surgical treatment accepted a recurrence risk of no more than 10 per cent for treatment with antibiotics. The most prominent reason was that surgery removes the cause of appendicitis.
Three studies12–14, all undertaken in the USA, have previously explored patient preference in the treatment of uncomplicated appendicitis. Kadera and colleagues14 included 129 patients without suspicion of appendicitis in the emergency department, using interviews to test patients’ knowledge of appendicitis and informing them about antibiotic treatment. In 57 per cent of these patients without appendicitis, antibiotic treatment was preferred over surgery. In patients with a history of appendicitis, this increased to 74 per cent. However, treatment options were presented as comparable options, without explanation of (recurrence) risks and advantages. The other two studies did inform about the risks and advantages of both treatments. Althans and co-workers12 used a questionnaire on 255 medical students, and reported that 66 per cent preferred surgery, 24 per cent antibiotics, and 9 per cent were undecided. Hanson et al.13 also included participants from the medical community: 1728 participants for an online survey, distributed by the University of North Dakota (UND) and UND School of medicine and Health Sciences Newsletter, posters on the UND campus, social media, the American College of Surgeons discussion board, and the Association of VA Surgeons 2016 annual meeting. Only 9 per cent preferred treatment with antibiotics. Afterwards, in interviews of 220 participants recruited at public venues, antibiotic treatment was viewed as more appealing when short-term failure and long-term recurrence rates were lower.
Two of the previous studies informed about risks and benefits, although presented information conflicts with data from published systematic reviews15. This may well have led to less favourable scenarios for antibiotic treatment15. Furthermore, both scenario survey studies12,13 focused on medical participants, which may have influenced the results. In the present study, the data provided were extracted from recent systematic reviews, RCTs, and national data, and up-to-date clinical data on surgical and antibiotic treatments. Moreover, the participants were a sample of the average Dutch population and the results are therefore more generalizable.
In the present study, the scenario provided describes a patient with uncomplicated appendicitis, without including diagnostic dilemmas. Risk assessment by the participant is based on this uncomplicated diagnosis. In practice, differentiation between uncomplicated and complicated appendicitis remains challenging. The CODA2 collaborative included 1552 patients with assumed uncomplicated appendicitis based on imaging, and compared antibiotic and surgical treatment. An appendiceal perforation was found in 15 per cent of initially operated patients. An association was described between the presence of an appendicolith and having complicated appendicitis2. The Appendicitis Acuta (APPAC) trial16 included only patients without an appendicolith, and the rate of complicated cases in the initial surgery arm was only 1.5 per cent. Patients with an appendicolith are potential non-responders to antibiotic treatment and perhaps should not be offered non-operative treatment. Moreover, the chance of having complicated appendicitis has to be taken into account and should be explained to patients.
A recent study17 has evaluated quality of life and patient satisfaction after intervention in an observational follow-up of an RCT comparing appendicectomy with antibiotic treatment. Quality of life was similar in both groups. However, more patients were satisfied with appendicectomy than antibiotic treatment (68 per cent very satisfied, 21 per cent satisfied, 6 per cent indifferent, 4 per cent unsatisfied, and 1 per cent very unsatisfied in appendicectomy group; 53 per cent very satisfied, 21 per cent satisfied, 13 per cent indifferent, 7 per cent unsatisfied, and 6 per cent very unsatisfied in antibiotic group; P < 0.001). This difference is explained by the subgroup of patients initially randomized to antibiotics but eventually needing surgery. Of this subgroup, however, 33 per cent still chose antibiotic treatment as their first choice. The recurrence rate after antibiotics in the APPAC trial (27.3 per cent had an appendicectomy within 1 year) lies below the recurrence risk that present study participants who preferred antibiotics were willing to take. Because patients were randomized to either antibiotics or surgery in the APPAC trial, satisfaction may have been greater when patients were assigned to a treatment group of their own preference. This patient preference model was used by Minneci and colleagues18, who compared antibiotic treatment with surgical management in children (7–17 years old), and treatment was assigned based on the preference of patients and their families. Of all 102 patients, 37 chose non-operative treatment, of whom 24 per cent underwent appendicectomy within 1 year. Compared with the initial-surgery group, patients in the antibiotic group had a shorter period of disability days (8 versus 21 days) and lower appendicitis-related healthcare costs. The incidence of complicated appendicitis was lower in the antibiotic group, but the difference was not statistically significant (2.7 versus 12.3 per cent; P = 0.15)18. This type of study could increase validity compared with RCTs, without compromising internal validity19. Moreover, such studies reflect a situation more comparable to daily clinical practice.
Limitations of this study are the involvement of participants who did not have acute appendicitis at the time of the surgery; only 10.6 per cent had experienced appendicitis once. The web-based survey did not offer an opportunity to validate understanding of all risks and benefits by the participants. Moreover, in real life, the decision about either treatment would often be discussed with family, which was not part of the study. Furthermore, in the light of the latest results from the CODA collaborative2 and the APPAC II trial20, this narrative may have undersold antibiotics. Conservative treatment may need hospital admission for only 1 day or possibly no hospital stay at all2,20,21 instead of the 2 days outlined in the questionnaire, which was common at the time of designing this study. Finally, the narrative did not include information about the rare possibility and unanswered consequence of missed appendiceal neoplasms. As the questionnaire was composed before the results from the CODA collaborative and the APPAC II trial were published, these data were not included in the survey.
The use of antibiotics as first-choice treatment in uncomplicated appendicitis is still under discussion. Guidelines are cautious in advising antibiotics only as standard treatment6,7. The present study contributes to the available evidence that one in two average people may prefer (initial) antibiotic treatment. This group is willing to accept a high risk of recurrent appendicitis when receiving antibiotic treatment instead of surgery, even higher than the actual recurrence risk after antibiotic treatment. In contrast, the surgery preference group would tolerate only a low recurrence risk. Patients with uncomplicated appendicitis should be counselled about both treatment options.
Supplementary Material
Acknowledgements
This was a survey study among participants who participated voluntarily. Participants were informed about the questionnaire and gave consent for participation and publication. The data sets generated and analysed during the present study are not available publicly owing to possible compromise of individual privacy, but are available from the corresponding author on reasonable request.
Conflict of interest. M.A.B. reported receiving institutional grants from J&J/Ethicon, KCI/3M, Bard, and New Compliance; and being an advisory board member and/or speaker and/or instructor for KCI/3M, J&J/Ethicon, Allergan, Bard, Gore, and Smith & Nephew. The authors declare no other conflict of interest.
Supplementary material
Supplementary material is available at BJS Open online.
Contributor Information
W J Bom, Department of Surgery, Amsterdam UMC, location AMC, Amsterdam Gastroenterology Endocrinology Metabolism, University of Amsterdam, Amsterdam, the Netherlands.
J C G Scheijmans, Department of Surgery, Amsterdam UMC, location AMC, Amsterdam Gastroenterology Endocrinology Metabolism, University of Amsterdam, Amsterdam, the Netherlands.
S L Gans, Department of Surgery, Gelre Hospitals, Apeldoorn, the Netherlands.
A A W Van Geloven, Department of Surgery, Tergooi Hospitals, Hilversum, the Netherlands.
M A Boermeester, Department of Surgery, Amsterdam UMC, location AMC, Amsterdam Gastroenterology Endocrinology Metabolism, University of Amsterdam, Amsterdam, the Netherlands.
References
- 1. Rollins KE, Varadhan KK, Neal KR, Lobo DN. Antibiotics versus appendicectomy for the treatment of uncomplicated acute appendicitis: an updated meta-analysis of randomised controlled trials. World J Surg 2016;40:2305–2318 [DOI] [PubMed] [Google Scholar]
- 2. Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, Sanchez SE et al. ; CODA Collaborative. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med 2020;383:1907–1919 [DOI] [PubMed] [Google Scholar]
- 3. van Rossem CC, Bolmers MDM, Schreinemacher MHF, van Geloven AAW, Bemelman WA, Acker GJD et al. Prospective nationwide outcome audit of surgery for suspected acute appendicitis. Br J Surg 2015;103:144–151 [DOI] [PubMed] [Google Scholar]
- 4. Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA 2018;320:1259–1265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sallinen V, Akl EA, You JJ, Agarwal A, Shoucair S, Vandvik PO et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg 2016;103:656–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gorter RR, Eker HH, Gorter-Stam MAW, Abis GSA, Acharya A, Ankersmit M et al. Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg Endosc 2016;30:4668–4690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 2020;15:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schuster KM, Holena DN, Salim A, Savage S, Crandall M. American Association for the Surgery of Trauma emergency general surgery guideline summaries 2018: acute appendicitis, acute cholecystitis, acute diverticulitis, acute pancreatitis, and small bowel obstruction. Trauma Surg Acute Care Open 2019;4:e000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Whalen T, Schwartz M, Heneghan K; American College of Surgeons. Appendectomy, Surgical Removal of the Appendix. https://www.facs.org/education/patient-education/patient-resources/operations/appendectomy (accessed 4 February 2021)
- 10. Lowth M, Jarvis S. Appendicitis. https://patient.info/doctor/appendicitis-pro#nav-4 (accessed 4 February 2021)
- 11.Royal Collage of Surgeons of England. RCS Statement on Treatment of Uncomplicated Appendicitis. https://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/rcs-statement-on-treatment-of-uncomplicated-appendictis/ (accessed 4 February 2021)
- 12. Althans AR, Tamer P, Brady JT, Steinhagen E, Ho VP. Surgery versus antibiotics for uncomplicated appendicitis: which would a medical student want? Surg Infect (Larchmt) 2017;18:868–873 [DOI] [PubMed] [Google Scholar]
- 13. Hanson AL, Crosby RD, Basson MD. Patient preferences for surgery or antibiotics for the treatment of acute appendicitis. JAMA Surg 2018;153:471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kadera SP, Mower WR, Krishnadasan A, Talan DA. Patient perspectives on antibiotics for appendicitis at one hospital. J Surg Res 2016;201:253–257 [DOI] [PubMed] [Google Scholar]
- 15. Talan DA. Questionable assumptions provided in nonoperative treatment of appendicitis survey. JAMA Surg 2018;153:969–970 [DOI] [PubMed] [Google Scholar]
- 16. Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA 2015;313:2340–2348 [DOI] [PubMed] [Google Scholar]
- 17. Sippola S, Haijanen J, Viinikainen L, Grönroos J, Paajanen H, Rautio T et al. Quality of life and patient satisfaction at 7-year follow-up of antibiotic therapy vs appendectomy for uncomplicated acute appendicitis: a secondary analysis of a randomized clinical trial. JAMA Surg 2020;155:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Minneci PC, Mahida JB, Lodwick DL, Sulkowski JP, Nacion KM, Cooper JN et al. Effectiveness of patient choice in nonoperative vs surgical management of pediatric uncomplicated acute appendicitis. JAMA Surg 2016;151:408–415 [DOI] [PubMed] [Google Scholar]
- 19. Wasmann KA, Wijsman P, van Dieren S, Bemelman W, Buskens C. Partially randomised patient preference trials as an alternative design to randomised controlled trials: systematic review and meta-analyses. BMJ Open 2019;9:e031151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sippola S, Haijanen J, Grönroos J, Rautio T, Nordström P, Rantanen T et al. Effect of oral moxifloxacin vs intravenous ertapenem plus oral levofloxacin for treatment of uncomplicated acute appendicitis: the APPAC II randomized clinical trial. JAMA 2021;325:353–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Talan DA, Saltzman DJ, Mower WR, Krishnadasan A, Jude CM, Amii R et al. ; Olive View–UCLA Appendicitis Study Group. Antibiotics-first versus surgery for appendicitis: a US pilot randomized controlled trial allowing outpatient antibiotic management. Ann Emerg Med 2017;70:1.e19–11.e19 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.