Abstract
This is the fifth in a series of papers entitled “Controversies in EUS.” In the current paper, we deal with high-resolution catheter probes, otherwise known as EUS miniprobes (EUS-MPs). The application of miniprobes for early carcinomas in the entire intestinal tract, for subepithelial lesions, and for findings in the bile duct and pancreatic duct as well as endobronchial use is critically discussed. Submucous lesions, especially in the colon, but also early carcinomas in special cases are considered the most important indications. The argument is illustrated by numerous examples.
Keywords: cancer, catheter probes, EUS, high-frequency ultrasound, intraductal ultrasound, miniprobes
INTRODUCTION
This is the fifth in a series of papers entitled “Controversies in EUS.” In the first “What should be known prior to performing EUS exams?” the authors discussed what clinical information and whether other imaging modalities are needed before undertaking EUS examinations.[1] In part II, technical controversies on how EUS should be performed were discussed.[2] In part III and IV, practical issues concerning elastography and contrast-enhanced EUS were raised and discussed from different points of view.[3,4] An additional paper was dealing with ultrasound-guided thermal ablation treatment for pancreatic cancer.[5] Herewith, the demand for miniprobes in clinical endosonography is controversially discussed.
While conventional EUS requires special echoendoscopes and training dedicated to this technique, with flexible, high-frequency catheter probes that can be introduced through the working channel of any endoscope, EUS becomes a handy and potentially powerful diagnostic tool available to all performing routine endoscopic procedures.[6,7] High-resolution catheter probes, or simply miniprobes (EUS-MP), can be directed to very small structures of interest under direct endoscopic control. With a penetration depth of about 20 mm, not only structures of the intestinal wall but also a considerable volume of the surrounding organs can be visualized. The main hypothesis is that EUS-MP represent easy-to-use tools for an immediate investigation of either unexpected endoscopic findings or small lesions and abnormalities that difficult to assess with conventional EUS. The 2nd hypothesis of some of the authors (HS, CFD) but not all is that many structures missed by transabdominal ultrasound can be seen with EUS-MP, rendering both methods the ideal complemental partners in modern diagnostic gastrointestinal imaging. This applies to both intraluminal as well as to intraductal applications such as for lesions of the pancreatic or the bile duct. A periintestinal or periductal cylinder of 1–2 cm quite correctly represents the region of interest.
TECHNICAL NOTES AND PRACTICAL REMARKS
Miniprobes are highly flexible ultrasound probes with a working length of 1700–2700 mm and small outer diameter (1.7–3.4 mm). Their design allows advancement through the instrument channel of standard upper and lower endoscopes with the 2700 mm length suitable also for enteroscopes. Compared with dedicated echoendoscopes, EUS-MP scan at higher frequencies (range, 12–20 MHz), providing high-resolution imaging of the proximal structures but with a limited penetration depth. As a result, for EUS-MP, the optimal depth providing high-resolution imaging is up to 15–20 mm.
While mechanical EUS-MP use a rotating crystal transducer at the tip in a protective plastic sheath producing a 360° view, electronic probes have multiple transducers configured on a ring. Miniprobes for use in gastrointestinal and bronchial endoscopy feature only mechanical scanning systems and are available from Fujifilm and Olympus [Table 1].
Table 1.
Miniprobes currently available in the market for digestive and bronchial endoscopy
| Product brand/name | Type | Frequency (MHz) | Diameter (mm) | Length (mm) |
|---|---|---|---|---|
| Olympus UM - 2R | 360° radial mechanical scanning miniprobe | 12 | 2.5 | 2050 |
| Olympus UM - 3R | 360° radial mechanical scanning miniprobe | 20 | 2.5 | 2050 |
| Olympus UM - S20-17S | 360° radial mechanical scanning miniprobe (for bronchoscopy) | 20 | 1.4 | 2050 |
| Olympus UM - S20-20R | 360° radial mechanical scanning miniprobe | 20 | 2.0 | 2050 |
| Olympus UM - G20-29R | 360° radial mechanical scanning miniprobe (with guidewire) | 20 | 2.9 | 2050 |
| Olympus UM - DG20-31R | 360° radial mechanical dual plane scanning miniprobe (with guidewire) | 20 | 3.2 | 2050 |
| Olympus UM - DP12-25R | 360° radial mechanical dual plane scanning miniprobe | 12 | 2.5 | 2050 |
| Olympus UM - DP20-25R | 360° radial mechanical dual plane scanning miniprobe | 20 | 2.5 | 2050 |
| Fujifilm P2625 - M | 360° radial mechanical scanning miniprobe | 25 | 2.6 | 2200 |
| Fujifilm P2620 - M | 360° radial mechanical scanning miniprobe | 20 | 2.6 | 2200 |
| Fujifilm P2615 - M | 360° radial mechanical scanning miniprobe | 15 | 2.6 | 2200 |
| Fujifilm P2612 - M | 360° radial mechanical scanning miniprobe | 12 | 2.6 | 2200 |
| Fujifilm P2620 - L | 360° radial mechanical scanning miniprobe | 20 | 2.6 | 2700 |
| Fujifilm P2615 - L | 360° radial mechanical scanning miniprobe | 15 | 2.6 | 2700 |
| Fujifilm P2612 - L | 360° radial mechanical scanning miniprobe | 12 | 2.6 | 2700 |
| Fujifilm PB2020 - M | 360° radial mechanical scanning miniprobe (for bronchoscopy) | 20 | 1.9 | 2150 |
Although balloons are available, sonographic coupling to the intestinal wall is better obtained by the injection of saline or water or by direct contact of the probe to the mucosal surface. Therefore, especially in the esophagus, large channel endoscopes are recommendable that allow instillation of water as well as aspiration of air with the EUS-MP inserted. The image quality can be improved by the application of degassed water to obtain a completely echo-free background.[8] Use of a balloon sheath will increase the diameter of the probe from 2.5 or 2.0 mm to 3.6 mm (Olympus), thereby prohibiting efficient suctioning even with a large channel (3.7 mm) endoscope. Balloons are not recommended for gastrointestinal applications. EUS imaging artifacts should be reduced by limiting the amount of pressure applied to the wall with the transducer.[9] For endobronchial ultrasound, balloons are necessary to obtain adequate coupling.[10,11] Wire-guided miniprobes are available for insertion into the biliary system or pancreatic duct.
What is the optimal frequency?
The scanning range of miniprobes (12–20 MHz) allows good echo resolution of 0.07–0.18 mm that is highest in the near field but with a limited penetration depth. The 20-MHz EUS-MP is probably the most versatile for application in the gastrointestinal tract [Table 2].
Table 2.
Main applications of miniprobes
| Technique | Targets | Examples |
|---|---|---|
| Intraluminal scanning (water filling of the lumen, dedicated balloon) | Mucosal neoplasms | Cancer staging (EEC, EGC) |
| Subepithelial lesions | Differential diagnosis | |
| Esophageal wall layers | Gastric varices | |
| Vascular lesions | Dieulafoy’s lesion | |
| Structures within 2 cm from the gastrointestinal wall | Undetermined stenosis | |
| Corrosive esophageal injury | ||
| IDUS | CBD and main pancreatic duct including surrounding tissue | Small pancreatic and biliary tumors, stones, staging of cholangiocarcinoma |
| EDUS | Distal CBD and main pancreatic duct; ampulla | CBD-stones |
| Periampullary tumors |
IDUS: Intraductal ultrasound; EDUS: Extraductal ultrasound; EEC: Early esophageal cancer; EGC: Early gastric cancer; CBD: Common bile duct
With lower frequency probes, visualization of extramural anatomy and staging of advanced tumors might be easier. However, for extramural overview and orientation like staging of advanced tumors as well as for interventions, conventional EUS with radial or longitudinal scanners (at 7.5–12 MHz) is more appropriate. For advanced tumors >20 mm, high-resolution local staging seems to be of limited clinical relevance. On the other hand, higher frequencies (like 30 MHz) provide excellent fine resolution of the intestinal wall, with the drawback of losing sight of external structures. As long as there is limited evidence correlating ultrasonographic features with histopathology,[12] 20 MHz seems to provide the ideal mix between excellent local resolution and visualization of the relevant intestinal anatomy.[13] Optimal positioning of the transducer probe to the lesion is essential for artifact free EUS-MP imaging [Figure 2]. Irregular shape of the lesion surface and difficult anatomic locations such as the esophagogastric junction may result in inconsistent echo layers and poor resolution of echo structure,[14,15,16] especially also in colorectal cancer.[16,17]
Figure 2.
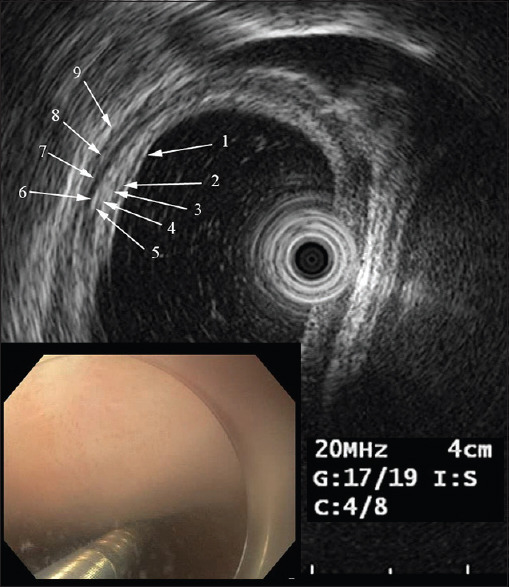
Esophageal wall, nine layers. Tubular squamous esophagus. 1 boundary echo (be), 2 mucosal epithelial layer (ep), 3 tunica/lamina propria mucosae (LPM) with glands, 4 muscularis mucosae (MM), 5 submucosa (SM), 6 muscularis propria stratum circulare (PMC), 7 intermuscular connective tissue (IC), 8 muscularis propria, stratum longitudinale (PML), 9 adventitia (AD). It is obvious that the ideal resolution is obtained only in a relatively small portion of the wall as this depends very much on positioning of the probe
Are diameter, stiffness, and shape important?
Theoretically, the smallest diameter would be the most desirable. It would enable easy introduction through even narrow working channels and atraumatic cannulation of the papilla of Vater for pancreatic or biliary intraductal ultrasound (IDUS). Rigidity of the tip should be minimal to allow steering with the Albarran lever without breaking the transducer. The tip should be rounded and smooth, because otherwise it could be trapped in mucosal folds, potentially leading to damage of the mucosa and the probe. Miniprobes carrying a guide wire port at their tip (available from Olympus [Table 1]) are useful for wire-guided IDUS but are restricted to this application. Very slim probes (<2 mm) are easy to handle at the price of inferior image quality. For most universal use, a 2.5 mm probe with a flexible blunted tip at present seems the best compromise.
Endosonographic anatomy of the gastrointestinal tract by EUS miniprobes
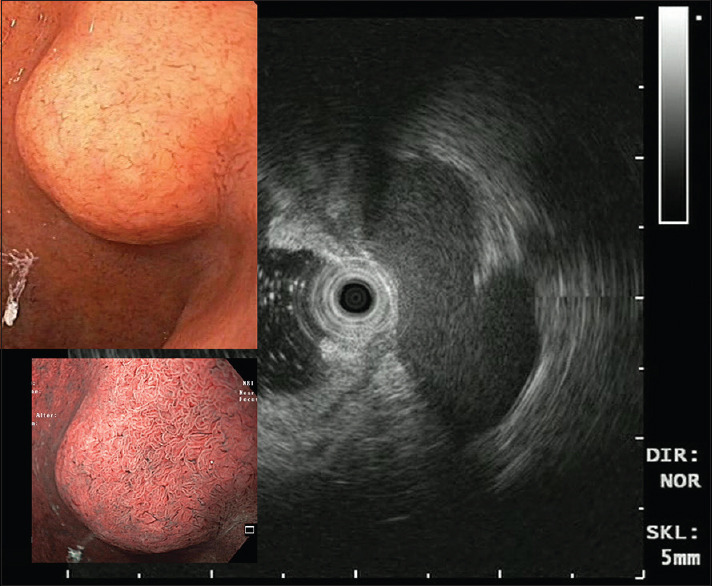
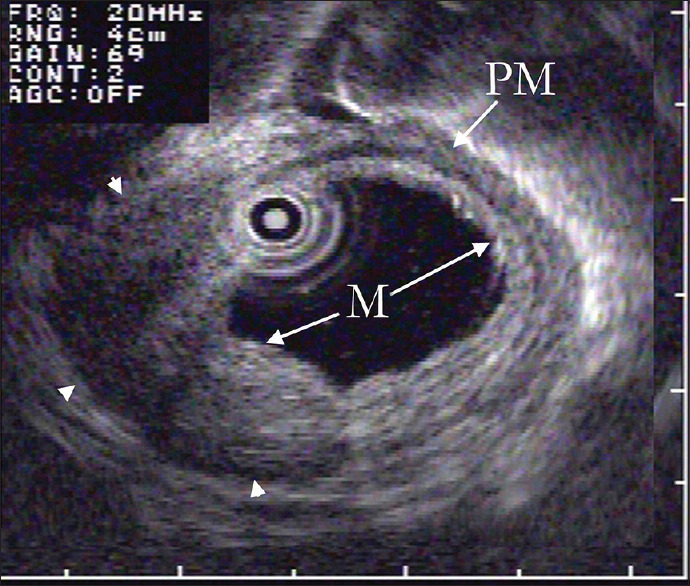
The interpretation of the layered structure in EUS corresponding to the histologic structure of the gastrointestinal wall follows the standard established by a Japanese expert group.[18] The normal echo structure of the gastric wall seen at 20 MHz shows five echo layers corresponding to histological structures[19] [Figure 1].
Figure 1.
Gastric wall. Gastric wall has 5 sonomorphologic layers. (1) Hyperechoic layer, the reflected boundary echo of the epithelial surface and epithelial layer; (2) hypoechoic layer, lamina propria (LPM) of the mucosa (with glands); (3), hyperechoic, slightly wider, corresponds to the submucosa (SM) layer and includes upfront the echo from the muscularis mucosa (MM); layer (4–6) broader hypoechoic corresponds to the proper muscle (PM) layer; and the fifth (7), to the subserosa and peritoneal serosa. EUS-MP separately resolves seven layers separating the circular (4) and longitudinal (6) PM layer, adding the hyperechoic interstitial fascia between them (5)
The esophageal wall [Figures 2 and 3] shows similar echo layers to the gastric wall, but differs in two aspects: layer 2 (lamnia propria layer [LPM], hypoechoic) of squamous epithelium and layer 3 (interface on submucosa, hyperechoic) are broadly reflected and separately visualized, resulting in a nine-layered echo structure [Figures 2 and 3]. Sometimes, even the boundary echoes at muscularis mucosae and the surface of submucosa may be divided into three hyperechoic layers.[18]
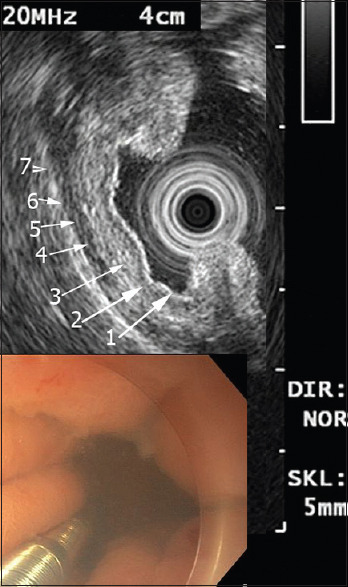
Figure 3.
Esophageal wall, nine layers. Tubular esophagus, long segment of Barrett's esophagus. Layers are the same as in Figure 2, but note layer 4 showing split layers of MM (important for orientation in ESD of Barrett's carcinoma)
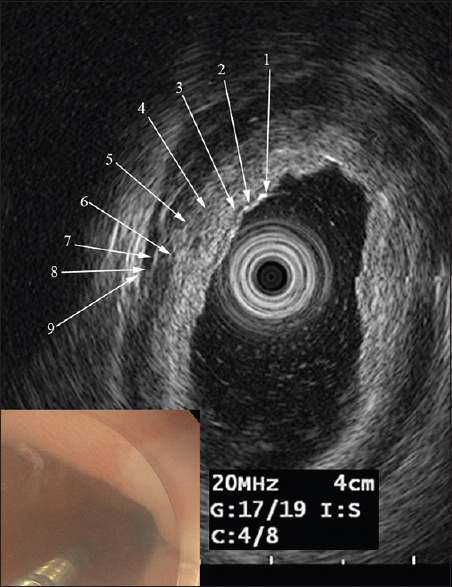
Small intestine [Figure 4] and colonic wall as with the gastric wall show the same 5 echo layers, but the third layer (submucosa) often contains three divided “ladder-like” echoes (muscularis mucosae, submucosa, and interface to muscularis propria).
Figure 4.
Duodenal wall. The thin (2–3 mm) duodenal wall has 5 sonomorphologic layers. (1) Hyperechoic layer, the reflected boundary echo of the epithelial surface and epithelial layer; (2) hypoechoic layer, lamina propria (LPM) of the mucosa (with glands); (3), hyperechoic, corresponds to the submucosa (SM) layer. (4) Broader hypoechoic corresponds to the PM layer; and the fifth (5), to the subserosa and peritoneal serosa. The colonic wall is similar
DIAGNOSTIC APPLICATIONS
Esophageal cancer
In the esophagus, investigation with a 20 MHz miniprobe is able to depict the layers of the wall [Figures 2 and 3] with a resolution unequalled by conventional EUS[20,21,22,23] or other imaging methods.[24,25] According to the Japanese Classification of Esophageal Cancer,[26] early esophageal cancer (EEC) is defined as a cancer confined to the mucosa (T1a = M), regardless of the presence or absence of lymphatic or distant organ metastasis, e.g., EEC: T1aNxMx. Superficial esophageal cancer (SEC) is equivalent to T1. It comprises EEC and submucosal cancer (T1b = SM), regardless of LNM or distant organ metastasis, e.g., SEC: T1NxMx. The formerly used subclassification of superficial type generally corresponds to the following: M1: T1a-EP, M2: T1a-LPM, M3: T1a-MM, SM1: T1bSM1, SM2: T1b-SM2, and SM 3: T1b-SM3.[26]
The indication for endoscopic resection (ER) of early carcinomas relies on the preinterventional assessment of the tumor's allocation to the layers of the wall. Depending on the depth of invasion limited to the layers of the mucosa, M1–M3, or already SM, the indication for ER is considered unquestionable or relative. The prognosis and the further therapeutic procedure then depend on the postinterventional histology. In case of tumors invading the MM with vascular invasion, or of deep SM invasion, an additional therapy (surgery or chemotherapy) is recommended. In these cases, ER cannot be considered as a sufficiently safe curative procedure.
The decisive question is, therefore, the correlation of the preoperative clinical diagnosis with the postoperative histological findings. Preinterventional diagnostic is based on endoscopic assessment using high-resolution image-enhanced magnifying endoscopy (ME) and EUS, usually 20-MHz EUS-MP.
The accuracy of EUS-MP in the determination of deep invasion of SEC-M versus SM, or M1-2 versus M3, SM1 versus SM2 versus SM3, has been reported in previous publications to be between approximately 50% and 90%.[15,16,27,28]
Yu et al. in a recent meta-analysis including 10 studies[27,28,29,30,31,32,33,34,35,36,37] found that ME narrow-band imaging (NBI) had a diagnostic rate for invasion depth staging similar to EUS-MP in 58 esophageal squamous cell carcinomas ESCC.[38] Routine assessment using miniprobe EUS did not increase the accuracy of predicting invasion depth, compared to endoscopy. However, EUS could be helpful in the treatment decision-making process for early gastric cancers (EGCs) with lesions having irregular surfaces, fold change, size >2 cm, or ulcer scar.[39]
Tao et al., in their 2017 review and meta-analysis on the comparison of EUS-MP and ME for the assessment of superficial neoplasms, included data of 754 patients contributed by seven prospective studies.[40] Three studies were on esophageal cancer,[35,37,41] and four studies were on colorectal cancers.[42,43,44,45] They concluded that “both EUS and ME provide a comparable performance for judging the depth of invasion of gastrointestinal neoplasms.”
For 58 ESCC allocated by EUS-MP to the muscularis mucosae (MM) or SM1, this diagnosis was correct in 29.3%, but “overstaged” (histologically pEP or pLPM) in 55.2%, and “understaged” in 15.5% (pSM2),[46] as reviewed by Ishihara et al.[47]
For SCC as well as adenocarcinoma of the esophagus there exists a differentiated classification of the Japan Esophageal Society.[48,49,50,51,52,53,54] What then is the diagnostic accuracy of the endoscopic evaluation? A current overview47 gives the following results: Endoscopic diagnosis M1/M2(B1 vessels): correct 92.4% (661/715). Endoscopic diagnosis M3/SM1 (B2 vessels): correct 55.7%(118/212), pM1/M2(”overstaged”) 27.4%, pSM2 17.0% (”understaged”). Endoscopic diagnosis SM2 (B3 vessels): correct 90.7% (39/43), pMM/SM1 9.3% (”overstaged”).
Thus, the accuracy of preoperative classification of cMM and SM1 esophageal cancers by EUS-MP but also by endoscopic criteria is unsatisfactory, even in expert hands. This applies to squamous cell as well as adenocarcinomas. In the latter, correct EUS classification for short Barrett's cancer at the cardia can be exceptionally challenging.[15,16] In addition, it is difficult to distinguish between cancer invasion and inflammatory cell infiltration.[27] Although EUS can distinguish between definite intramucosal cancers and definite submucosal invasive cancers, it is relatively demanding to exclude minute submucosal invasion even when using EUS-MP.[8]
In their comprehensive up-to-date guidelines on the ER of EECs, Ishihara et al.[47] “weakly recommend” that EUS-MP should not be used as standard procedure for diagnosing the invasion depth of superficial esophageal adenocarcinoma, because there are no studies with high level of evidence for EUS-MP in these patients. They do not comment on EUS-MP in SCC, but their summarizing conclusion that “the accuracy of preoperative diagnosis is thus poor and the least invasive treatment (usually ER) should therefore be selected as the front line in these cases” clearly mirrors the current situation. With the background of still unsatisfactory and complicated classification systems of superficial SCC and even more so of adeno- or Barrett's Ca, some of the authors (HS, CFD) consider EUS-MP a still useful complemental tool. Despite the limitations of EUS-MP in the fine evaluation of early cancers, such as low accuracy for minute submucosal invasion and lesions with ulcerous change, they prove to be a useful clinical tool for the assessment of the resectability of early cancers (diagnosing deep SM-invasion or minute T2) in esophagus and stomach when used very carefully.[8] When both the endoscopic and EUS diagnoses are considered, clinicians can achieve a high accuracy of staging of early esophageal and gastric cancers[8]. If both methods suggest a mucosal depth of invasion, the accuracy of the prediction is increased. Therefore, it seems recommendable to evaluate the invasion depth of SEC using both ME-NBI and EUS before deciding to perform ER.[37,40]
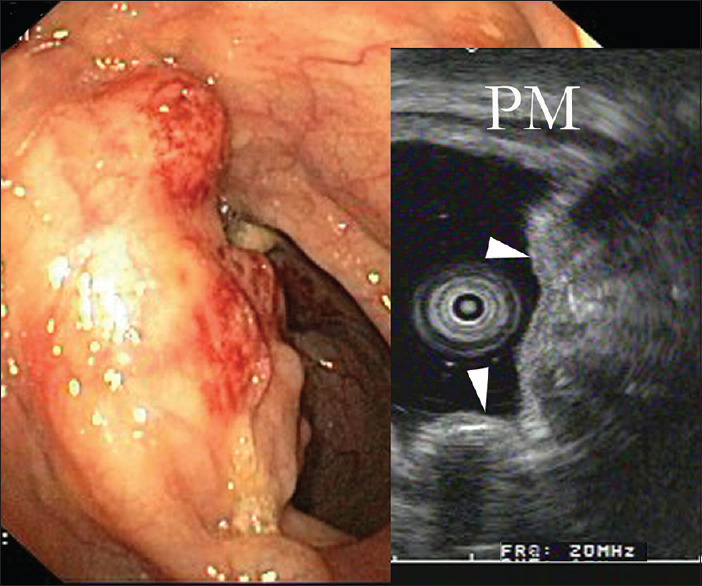
Details of prognostic significance such as invasion of LPM versus MM versus SM, ± vascular invasion or tumor budding[55] are challenges left to the pathologist. Preoperative endoscopic diagnosis should probably at present focus on the question of endoscopic resectability, and because of the considerable risk of overstaging [Figure 5], if in doubt, endoscopic submucosal dissection (ESD) should be performed and the final judgment left to histology.
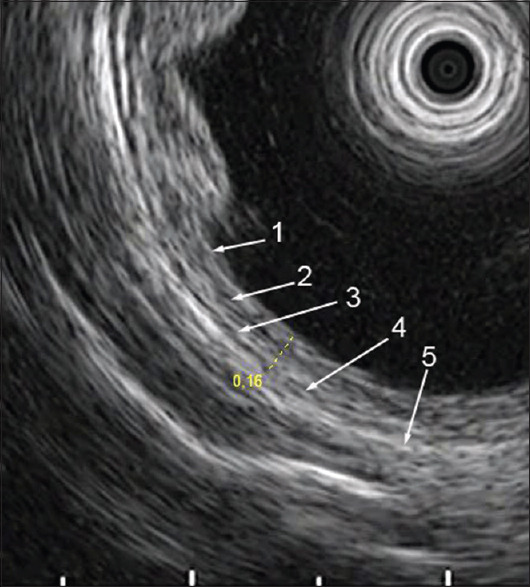
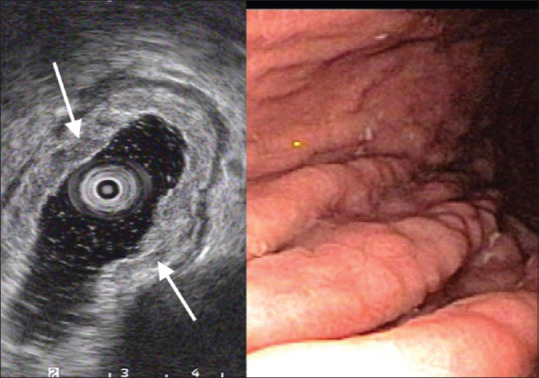
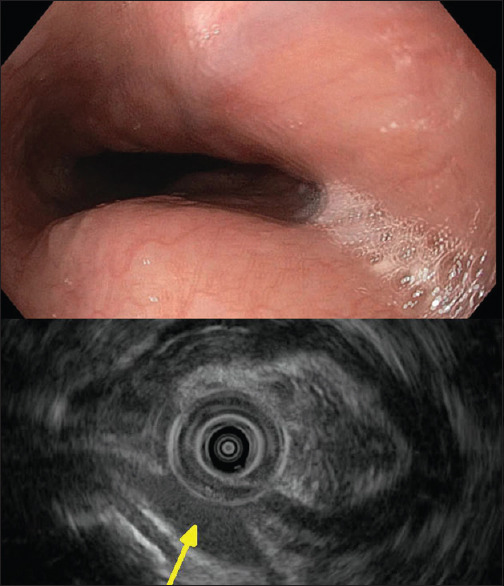
Figure 5.
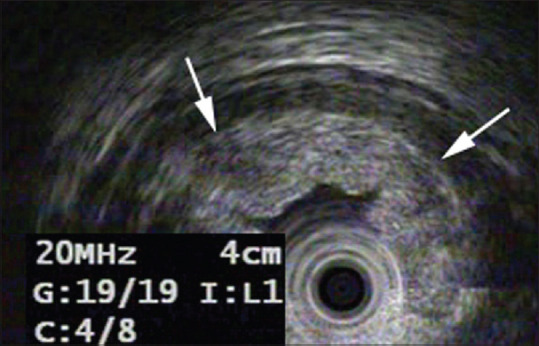
Early adenocarcinoma of the esophagus (Barrett's). The layers of the wall are maintained, especially the SM layer allowing ER. However, some hypoechoic broadening and small protrusions of the mucosal layers (arrows) are suspicious of SM invasion, primarily diagnosed as uSM2 or uSM3. Histologic category after ESD was pT1SM1
For advanced tumors [Figure 6], miniprobes correctly show fusion of the layers of the intestinal wall, but due to their limited penetration depth, differentiation of categories ≥T2 is often uncertain. On the other hand, EUS-MP may be of particular value in stenosing neoplasms that are not traversable with dedicated echoendoscopes.[56,57] However, in these advanced stenosing tumors (≥T3), EUS-determination of the T-category is of little importance. EUS-MP may in some cases be useful for determining the longitudinal extension of the tumor, especially at the GE junction pre neoadjuvant therapy or stenting.
Figure 6.
Advanced esophageal adenocarcinoma. Left panel: EUS-MP shows fusion of all layers of the esophageal wall and tumor extension beyond the boundaries of the organ (arrows). Right panel: Paraesophageal lymph node cranial of the tumor, suspicious for N1. Advanced large tumors > uT3 may sometimes be beyond the zone of high-resolution imaging with EUS-MP. However, even extreme stenoses can be passed without dilation allowing classification of tumor category ≥ uT3 and of longitudinal extension of the tumor by pull-through
N-category
Concerning lymph nodes, determining the N-category of esophageal cancer, conventional EUS was more sensitive and accurate than computed tomography (CT) in 2006.[25] Due to its limited penetration depth, EUS-MP is less sensitive (25%–73%) and accurate (56%–87%) for “N staging” than conventional EUS with 7.5-MHz echoendoscopes.[20,21,22] In some cases, during the first endoscopic examination of a suspected EEC or as part of a post-ESD-control, EUS-MP may identify enlarged periesophageal lymph nodes, thereby at least requiring further diagnostic steps such as EUS-guided puncture [Figure 7].
Figure 7.
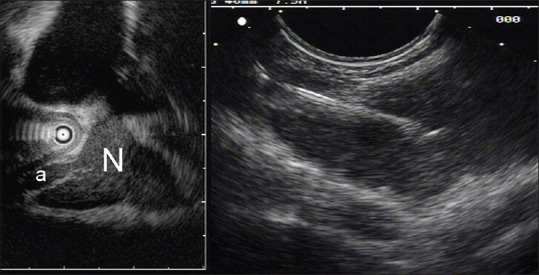
EUS-MP routinely shows the infracarinal lymph nodes (No. 107) en passent (left panel). Shown is a slightly enlarged LN with artery (a, left panel). Punctured under EUS guidance (PENTAX/Hitachi curved linear, 7.5 MHz. right panel). Benign cytology
Considering the ever-growing sophistication and sensitivity of other imaging techniques,[58,59] and, on the other hand, the week correlation of LN-size or shape with malignancy[60,61] and therefore unsatisfactory sensitivity of conventional EUS for malignant lymph nodes,[62] the role of EUS in defining the N category seems more than questionable. If malignant LN of 3 mm median size,[63] lymph node and bone marrow micrometastases,[61] vascular and lymphatic invasion, and tumor budding[55] define the prognosis of patients with pR0 SEC, sonomorphology of advanced tumors and lymph nodes becomes irrelevant. However, local pathological anatomy matters. It determines the therapeutic strategy and allows judgment on the probability of lymph node metastases. This may lead to a revival and technical improvement of high-frequency ultrasound as an adjunct to ME-NBI or other high-end endoscopy.
Gastric cancer
EGC is defined as a cancer confined to the mucosa or submucosa, regardless of LNM.[64] Diagnostic criteria for EGC by high-performance endoscopy such as ME with different techniques of virtual chromoendoscopy such as NBI have been established based on vascular and surface details (”VS classification”).[65,66,67,68,69,70,71] While differentiating benign gastric adenomas from malignant neoplasia is demanding[72,73,74,75] and even in Japan the miss rate of small gastric neoplasia was considerable,[74,76] determining invasion depth of early cancers by endoscopic criteria is at least as challenging.[14,51,67,71,72,77,78,79,80,81,82] Although many recent studies have been conducted to interpret the gastric mucosal surface structure and vascular characteristics under ME-NBI, invasion depth of EGC still cannot be accurately determined.[83]
Endoscopic mucosal resection (EMR) was reported in 1984, at this time modestly called “strip biopsy.”[84,85] Of the first 73 intramucosal gastric cancers resected using the new EMR-method since 1984, the intramucosal well-differentiated adenocarcinomas up to 1989 had no incidence of recurrence. In addition, from large numbers of operated patients with EGC, it was obvious that the risk of lymph node metastasis correlates with histologic features of the tumor.[86,87,88] The cumulative survival rate 5 years after gastrectomy for intramucosal EGC in 519 patients was almost 95%. According to these results, the criterion “early gastric cancer endoscopic surgery” was defined.[88,89] Moreover, the conclusion of Sano et al. in 1992 is still valid today, that “with a recently developed endoscopic technique small gastric tumors can be safely resected. The cut margin and depth of tumor invasion can be verified histologically […]. If an endoscopically removed tumor satisfies the [histologic] criteria, further surgical intervention may be optional as the outcome of ER is comparable to that of radical surgery in the absence of node involvement.”[90]
Formerly accepted indications for ER of EGC included resection of differentiated mucosal cancer measuring ≤2 cm without ulceration.[91] With the establishment of the ESD technique by Gotoda et al. in 1999,[92] the en bloc ER of large lesions became feasible. Based on data from large-scale studies on gastrectomies[86,87] and ER,[93,94] more expanded criteria for ER of EGC were accepted.[95] The “expanded criteria” for ER[94,95,96] now include the incipient (<500 μm) invasion of the submucosa (T1a = SM1), and it has been shown that after ESD of early gastric carcinomas according to the “expanded criteria,” the prognosis regarding tumor-free survival does not differ from that after surgical resection.[94,95] Several researchers have reported the feasibility and comparable outcomes of ESD in EGCs meeting the expanded indication by different criteria.[93,94,97,98,99,100]
The future perspectives and challenges of ER for EGC were clearly seen already 30 years ago: “The current problem, however, lies in the difficulty of accurately diagnosing preoperatively the depth of cancer invasion, and in discriminating mucosal cancer from the submucosal cancer by endoscopy or other methods.”[89] Therefore, early on with the start of ER, the use of EUS-MP for preresection assessment was established.[101] For many years, EUS-MP was considered the standard method for determining the depth of invasion by EGCs, because it provides superior imaging of different pathologic entities [Figures 8 and 9].
Figure 8.
Gastric ulcer. EUS-MP during primary diagnostic gastroscopy shows defect of M- and SM layers but intact PM-layer (arrow): Nor perforation or penetration. No malignant features
Figure 9.
Apparent mucosal thickening. Infiltration of the LPM and SM of the gastric corpus by slightly inhomogeneous hypoechoic infiltrates (arrows), well separated from PM layer. On white light endoscopy there are slightly edematous gastric folds. Snare biopsy shows mucosa associated lymphoid tissue B-cell lymphoma
There are numerous publications on the use of EUS-MP for the staging of EGC and determining the optimal treatment strategy, i.e., ER or surgery. At the times of the restrictive criteria for ER, but even in recent studies, the distinction of M (T1a) vs. SM (T1b) appeared paramount.[102,103] Later on, with the “expanded criteria” for ER, the ability to differentiate between mucosal (M) or microinvasive submucosal (SM1: Depth <500 μm) versus invasive submucosal (SM2: Depth ≥500 μm) cancer was decisive when choosing the method of treatment for EGC.[104] In previous reports, the diagnostic accuracies when determining the depth of invasion using ultrasound probes were similar to that of ED, 50%–95%.[105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120] In these articles, most authors divided the depth of superficial cancer into two subclassifications: M (T1a) and SM (T1b). However, the authors of four studies tried to distinguish M/SM1 from SM2.[111,113,114,116] The accuracy of EUS for the depth diagnosis of gastric cancers was relatively high in these studies.[121] The accuracy of EUS relatively decreased for lesions of depressed type, undifferentiated cancer,[107,110] concomitant ulceration, and lesions located in the upper third of the stomach and lesions with a large diameter.[107,109,111,114,116,122,123] In addition, overstaging of EGC with the 20-MHz probe was reported to occur in 19%–24% of patients due to peritumoral fibrosis mimicking deeper invasion.[105,124] However, when both the endoscopic appearance and EUS findings were applied together for tumor classification, a 92% overall accuracy rate could be achieved.[105]
The recently published retrospective study on the clinical benefit of EUS for the treatment strategy in gastric cancer in 6084 patients reports an accuracy of 89.4% of EUS in the classification of EGC.[103] Of 4818 cases with EGC, 94% were correctly assigned to the corresponding T-classification (T1a-b/M, SM) and 6.4% were overclassified as advanced (AGC). Out of 1201 cases classified as uT2 (AGC), 76% were correct and 24% (7% pT1a, 17% pT1b) were overestimated. In this study, 92% of patients with EGC were examined with conventional EUS (radial scanner), the others with 12-MHz EUS-MP. Since for the T-classification of intestinal early cancers, it is proven that EUS-MP is superior to conventional EUS, and EUS-MP with higher frequency (20 or even better 30 MHz) is superior to those with lower frequency (12 MHz);[125,126] these results would probably have been even better with 20 MHz or 30 MHz probes for all patients. Another study with 142 patients with early GC evaluated the diagnostic accuracy of three EUS-MPs of different frequencies in vertical margins. The results indicated that the accuracies of the early GC invasion depths of the M + SM1 group were 81.0%, 86.0%, and 92.3% as measured by the 12-, 20-, and 30-MHz probes, respectively.[125] Thus, it can be concluded that for the T-classification of EGC, 30-MHz EUS-MP might be optimal.[127]
IS EUS USEFUL FOR ASSESSING THE DEPTH OF SUPERFICIAL GASTRIC LESIONS?
Can EUS-MP be helpful for this purpose by improving the accuracy of endoscopic judgment alone?
Facing the heterogeneity of the published data, as stated by three meta-analyses,[83,128,129] Choi's conclusion in 2010 “EUS may not be necessary routinely, and conventional endoscopy may be sufficient for determining the optimal therapeutic strategy, especially in relation to endoscopic resection for early gastric cancer”[112] seems justified. The widely varying accuracies make it difficult to view the method as sufficiently reliable. It seems noteworthy that there is not even one study clearly demonstrating a significant improvement of staging accuracy through EUS-MP over ED or impact of EUS-MP on the treatment strategy.
Nevertheless, there is a number of positive or at least ambivalent voices accepting EUS-MP as a helpful complemental tool at least in single difficult cases[8,39,103,111,122,130] such as ulcerated EGC.[131] Although this technology did not change since almost 30 years, as opposed to the rapidly growing endoscopic image quality as well as pattern interpretation systems, many expert groups still are using EUS-MP in early gastrointestinal cancer. It seems that in most studies, EUS-MP performance is corresponding to the quality of ED. Considering that in general, the endosonographer is an expert knowing and interpreting the “VS-pattern” before ore while doing EUS, EUS-MP must always be understood as a complemental tool on top of endoscopic diagnosis. Furthermore, most of the criticisms questioning EUS-MP are based on studies focusing on differentiating M (T1a) from SM (T1b) or on precise preresectional classification, which is both of almost no consequence considering the new extended criteria for ER. There is much to suggest that histological criteria, especially lymphatic invasion, are the decisive prognostic predictors in the assessment of EGC.[95,132] They can only be obtained from histology based on high-quality endoscopic specimens obtained by ESD.
In the light of the good prognosis of EGC after ER according to the “expanded criteria” and in the absence of lymphatic invasion, even in SM2 tumors,[95,96] there is a general indication for ER in EGC. Only based on detailed histopathology can the prognosis and further therapeutic strategy be discussed.
The role of EUS-MP might thus be limited to the detection of T2 tumors that are not resectable endoscopically or only by full-wall resection. The latter are often obvious by ED, but differentiation between deeply invading SM2 and early T2 can be difficult [Figure 6]. For this purpose, some authors (HS, CFD) appreciate EUS-MP as a useful supplement to endoscopic diagnostics pre-ESD.
IS THERE A ROLE FOR EUS MINIPROBES IN N-STAGING IN EARLY GASTRIC CANCERS?
After obtaining the histology of the resected specimen, the probability of lymphatic dissemination may much more reliably than by imaging techniques (like conventional EUS[133]) just be predicted from a nomogram and scoring system derived from >10,000 Patients.[95,134,135,136] The therapeutic strategy after R0-ER of more advanced superficial cancers is by no means clear or easy. According to the recently proposed eCure scoring system, e.g., a patient with a T1bSM2 EGC without lymphatic or vascular invasion would have a risk of lymph node metastasis of around 5%.[134] Depending on the patient's characteristics such as comorbidities and age as well as his personal preferences, alternatives to surgery may as well be adjuvant chemotherapy or just nothing except regular controls.[95]
Sophisticated CT and magnetic resonance imaging or sentinel node mapping techniques[137,138] are being developed to high-resolution capacities at least as potent as the old conventional EUS.[139,140] However, none of them can capture micrometastases <5 mm.[141]
COLORECTAL CANCER
The classification of colorectal mucosal neoplasms has been improved in recent years based on defined endoscopic criteria proposed by the Japanese Narrow Band Imaging (NBI) Expert Team (JNET).[142] However, training is required even for experienced endoscopists to adopt the available classification systems properly.[143] In clinical routine practice, even when applying all currently available modalities for determining depth like the assessment of gross features, NBI, magnifying chromoendoscopy, based on the JNET or the NICE-system,[144] a perfect estimation of invasion depth is not possible.[145]
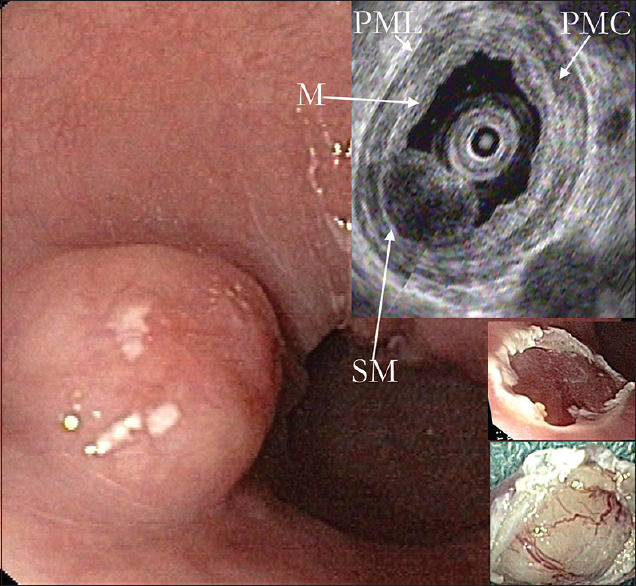
In addition to vessel and surface patterns, a third criterion can be obtained by EUS-MP during routine colonoscopy. Investigation with EUS-MP can determine the T category of colorectal cancer correctly in >80% of cases, based on the interpretation of the layered sonomorphology of the intestinal wall [Figure 10].[18]
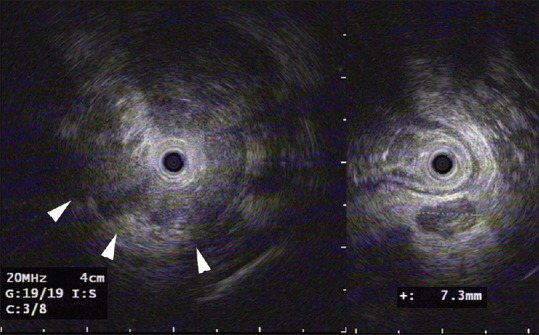
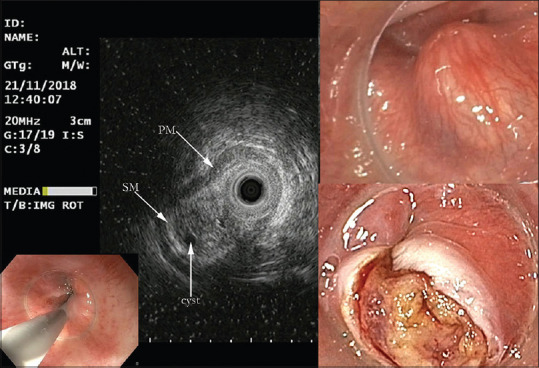
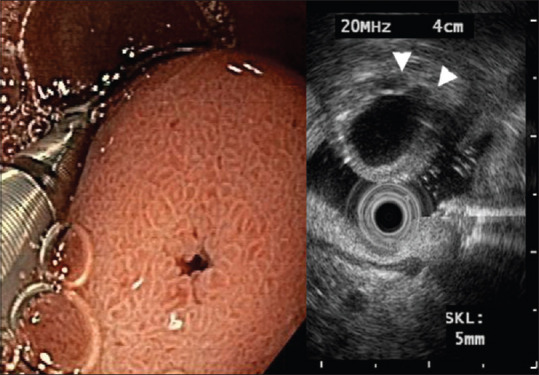
Figure 10.
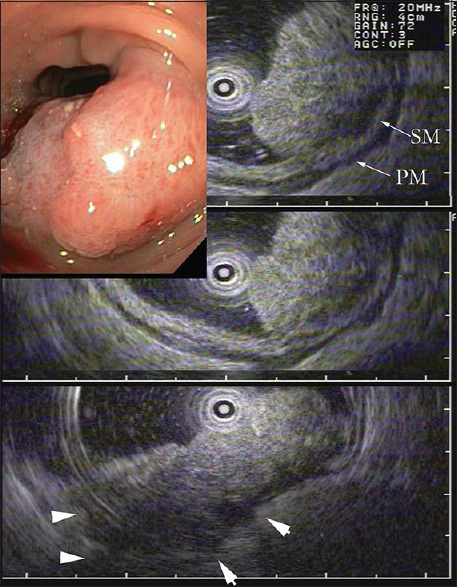
WLI-colonoscopy: Firm sigmoid polyp, highly suspicious for malignancy. EUS-MP 20 MHz shows a partially intact hyperechoic SM- and PM-layer (upper panel, arrows), but there is also fusion of all layers and hypoechoic invasion beyond the colonic wall corresponding to a tumor category uT3 (lower panel, arrowheads). Histopathology after surgery was pT2 pN0/L0 V0 – G2. A typical case of “overstaging” by EUS-MP probably taking edema for tumor. Nevertheless, the classification ≥ uT2 with indication for surgery was correct
In a prospective study, 131 consecutive patients with adenocarcinoma or broad-based polyps of the colon and rectum underwent 12.5-MHz miniprobe ultrasonography examinations conducted by a single endoscopist. Staging criteria for depth of tumor infiltration and nodal status were determined. Nodal disease was defined as the presence of a hypoechoic, round, defined boundary lesion larger than 10 mm in diameter. T0-T1 N0 lesions were resected using EMR, and patients with lesions staged as T2 N1 were referred for surgical resection. Tumor staging using endoscopic ultrasonography was compared with the histopathological specimens. The accuracy of T classification using EUS-MP was 96% in comparison with the histopathological specimen. Five (4%) lesions were overstated as T3 (pathology stage T2). Understaging occurred in three lesions (EUS stage was uT3, pathology stage was pT4). The overall accuracy of nodal classification using miniprobes was 87% (sensitivity, 0.95; specificity, 0.71; positive predictive value, 0.87; and negative predictive value, 0.88). One could assume from this study that miniprobes have high overall accuracy for both T staging and N staging of colorectal cancer and may have an important role in selecting patients suitable for minimally invasive resection techniques.[146]
A study from Korea showed that the overall accuracy with miniprobes for assessing the T-category in 90 patients with early colorectal cancer was 84%. It decreased with tumors larger than 2 cm and those infiltrating beyond the submucosa.[17] The meta-analysis of Gall[147] based on 642 cases leads to a positive evaluation of EUS-MP. In all but one of the included studies, miniprobes with 12 MHz (6 studies), 12.5 MHz (3 studies), or 15 MHz (1 study), i.e., nonoptimal resolution, were used. In addition, 52% of the investigated cases were in stage T3 or T4. Moreover, as in most studies, no distinction was made between rectal and colon carcinomas. Emmanuel et al.[148] reported recently on successful “Multimodal Endoscopic Assessment” including EUS-MP for rectal early neoplastic tumors to determine the appropriateness of ER or transanal endoscopic microsurgery.
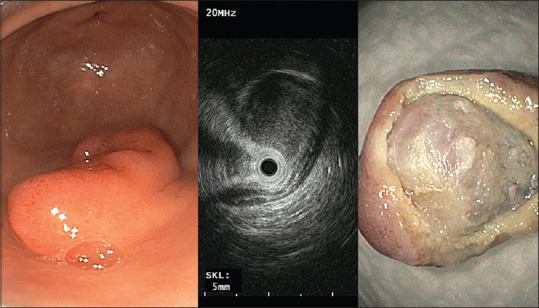
As diagnostic accuracy of EUS-MP depends on the macroscopic and growth type of the lesion and because all diagnostic methods have certain advantages and disadvantages, the JGES guidelines for colorectal ESD/EMR 2015 as well as 2020 recommend that appropriate diagnostic methods including EUS-MP should be combined, as the situation requires.[149,150] According to our own experience (HS, CFD), EUS-MP can for smaller suspicious neoplasia very precisely represent the relationship of the tumor to the layers 3 and 4 (submucosa and muscularis propria). As a supplement to the endoscopic diagnosis, it can support the therapeutic decision for or against ER. This is particularly true for recurrences and scars, where layer fusion in EUS-MP imaging can lead to the decision for full-wall resection. In very large and protruding polyps, however, EUS-MP sometimes is unreliable, due to its limited penetration and sometimes low image quality because of entrapped air in villous and multilobular neoplasias. For a critical evaluation of the EUS-MP, one would have to consider the respective pathological–anatomical situation, unlike in most studies. While discrimination of intraepithelial neoplasia from T1 (submucosal invasion) is difficult, differentiation between T1 and T2 might be easier. When the third layer (submucosa) looks preserved, ER is usually feasible [Figure 11].
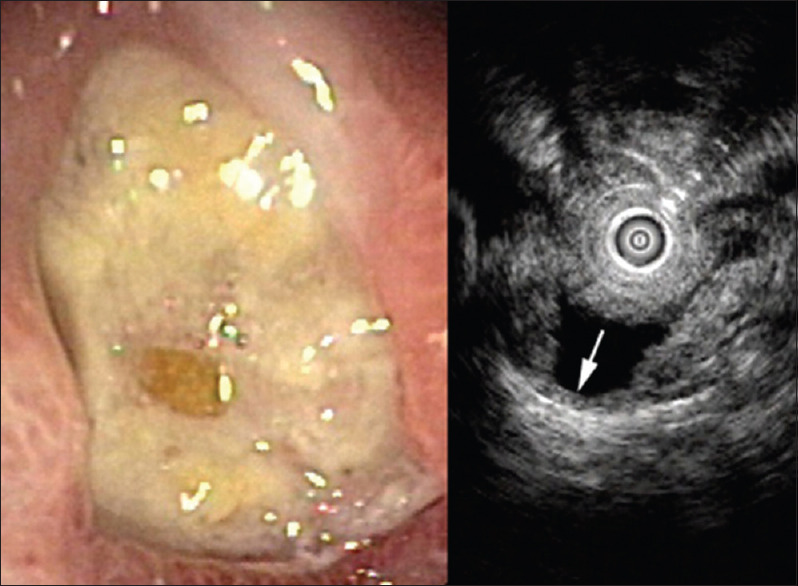
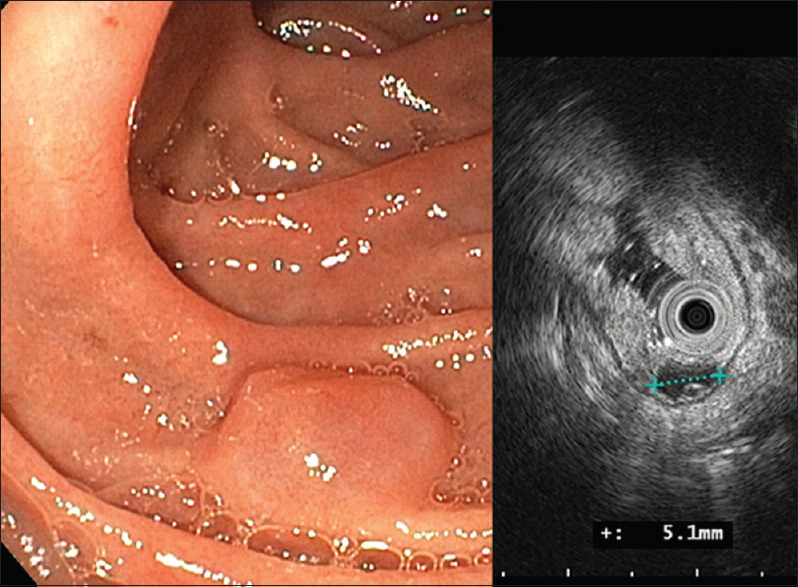
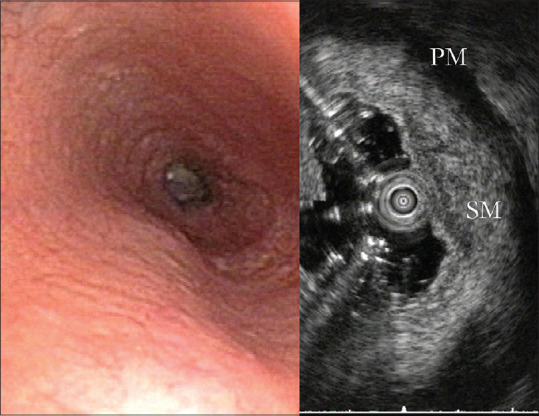
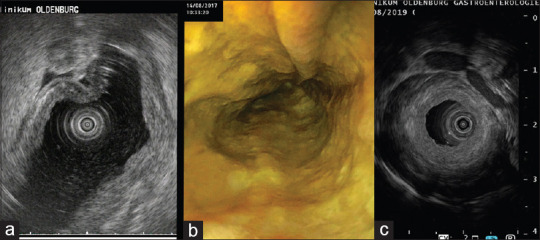
Figure 11.
WLI × 20 shows a rectal laterally spreading granular adenoma with branching slightly irregular surface pattern (Type V1) and in the flat nonprotruding area an irregularly meshed vessel pattern (arrow, JNET type 2B). HGIEN or superficially invasive cancer is suspected. EUS-MP (right panel) shows the hyperechoic SM-layer preserved (arrowhead) with intact PM-layer. After resection by ESD histology was HGIEN
Hypoechoic tissue extending through the submucosa into the muscularis propria (uT2) indicates that ER is inappropriate. If correct surgical resection according to oncological criteria is performed, the tendency of overstaging T2 as T3 Figure 10 and understaging T4 as T3 may be of little clinical relevance. The rectum allows the use of all EUS techniques, while in the colon, only miniprobes can be used. Moreover, the different consequences of rectal versus colonic surgical resections also require different therapeutic strategies. Thus, the clinical strategy requires high-quality histopathology after ESD or endoscopic en bloc resection.
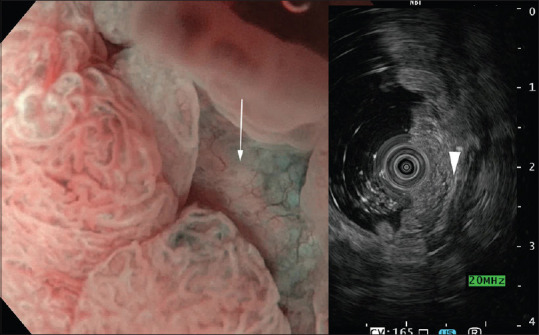
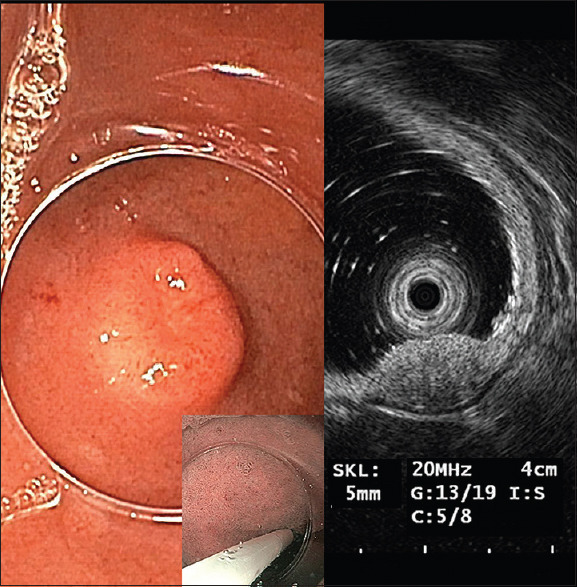
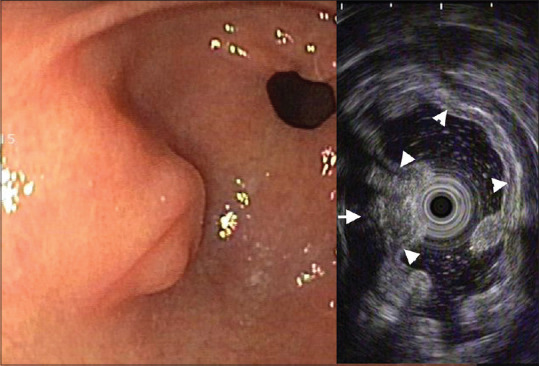
In summary, in the colon, there is no alternative to EUS-MP, if you wish fine resolution imaging of doubtful early neoplasms or other suspicious structures [Figure 12].
Figure 12.
WLI, routine colonoscopy, shows small firm SET covered by normal mucosa in the descending colon (left panel). EUS-MP 20 MHz reveals a firm subepithelial lesions (7.3 mm × 6.0 mm) with heterogeneous hypoechoic structure in continuity with the 4th layer (MM). There is a clear capsule margin. A gastrointestinal stroma tumors (GIST) is suspected. Histologic diagnosis after endoscopic resection is GIST, low risk (Ki-67 4%)
In the rectum, EUS-MPs are quick and efficient for small lesions but dedicated rectal probes or conventional EUS are good alternatives.
SUBEPITHELIAL LESIONS
Gastrointestinal submucosal tumors also termed subepithelial lesions (SELs) represent either nonneoplastic or neoplastic intramural submucosal, muscular, subserosal, or extramural masses[151] of various etiology [Figure 13] causing bulging of the intact mucosa.
Figure 13.
EGD shows an unexpected mass in the descending duodenum covered by intact mucosal structure (WLI, upper left, and NBI, lower left, both × 20). EUS-MP reveals bulging by a wide portal vein branch and intact layers of the duodenal wall (right panel). No resection
SELs comprise a variety of mesenchymal tumors such as GIST [Figure 12], leiomyomas [Figure 14], schwannomas, granular cell tumors, lipomas, vascular tumors (glomus tumors, hemangiomas), lymphangiomas, inflammatory fibroid tumors [Figure 15], mucosa-associated lymphoid tissue-lymphomas [Figure 9] or malignant lymphomas, epithelial tumors such as neuroendocrine tumors (NETs) [Figure 16], carcinomas, melanomas, metastases, congenital tumors such as aberrant pancreas, cysts [Figures 17 and 18], duplications, as well as Brunner's gland hamartomas, pneumatosis intestinalis [Figure 19], endometriosis, and finally impressions from outside.[152] Submucosal tumors are not rare, but since most of them are asymptomatic, the incidence rate is difficult to assess. It is estimated to be about 0.3%.[153]
Figure 14.
Submucosal esophageal tumor. Based on the clear characterization as well defined submucosal with intact layers by EUS-MP the endoscopic snare resection follows in the same session. Histology: Leiomyoma of the MM-layer, PM is intact)
Figure 15.
Defined asymptomatic antral tumor at white light endoscopy. EUS-MP reveals well-defined SET with intact M and PM layers: Snare resection is possible with minimal risk. Histology reveals a Vanek-tumor (inflammatory fibroid polyp)
Figure 16.
White light endoscopy shows a SEL in the descending duodenum. EUS-MP reveals a well-defined slightly hypoechoic nodule separating M and PM layer with intact PM layer. Snare resection was performed. Diagnosis: NET
Figure 17.
Submucosal nodule seen from the hypo pharyngeal position in the upper esophageal sphincter. EUS-MP shows submucosal position with intact PM- and SM-layer, heterogeneous echogenicity, small cystic structure. Water filling for optimal imaging was impossible because of the hypo pharyngeal position. Resection was difficult because of firm fibrous attachment; histology was multilocular cyst (benign)
Figure 18.
White light endoscopy shows a small SEL in the descending duodenum. EUS-MP shows submucosal cystic lesion without solid components, which was, therefore, not resected
Figure 19.
WLI-colonoscopy shows an atypical lesion in the ascending colon. EUS-MP 20 MHz reveals gas behind the intact mucosal layer (arrowheads). Diagnosis: Pneumatosis coli
The majority of SELs are asymptomatic and incidentally found during esophagogastroduodenoscopy or colonoscopy.[152] EUS-MP allows immediate delineation of bulging by extrinsic compression as well as allocation of intramural lesions to the respective layer of the intestinal wall.154 While diagnosis based on sonomorphology for some of these often small (1–10 mm) lesions like lipoma or Schwannoma[155] is highly reliable, for most lesions like GIST, NET [Figure 16] or ectopic pancreas [Figures 20 and 21] it is accurate in only 60%–70%.[156,157,158] Ectopic pancreas does not always show typical features. It is a chameleon with numerous differential diagnoses. In selected cases, EUS fine-needle aspiration (FNA) may help clarifying the diagnosis.[158]
Figure 20.
Ectopic pancreas in the antrum. EUS-MP shows submucosal position with heterogeneous echogenicity of the pancreatic tissue (arrow), intact M-layer (arrowheads), no extragastric extensions
Figure 21.
Ectopic pancreas in the duodenum pars II. Left panel: Bulging SEL with intact mucosa and porus of the duct of the aberrant pancreas. EUS-MP attached to the lesion. Right panel: Slightly hypoechoic SM-lesion (arrowheads) with cyst-like dilated duct in the SM-layer, thin underlying SM-layer, and intact hypoechoic PM-layer
If malignancy is suspected, several approaches of EUS-guided tissue acquisition[159,160,161,162,163,164,165] or direct endoscopic biopsy[166] could be applied.[167] This would usually require a scheduled second session using a curved-linear EUS with appropriate informed consent of the patient. Large symptomatic tumors are beyond the scale of EUS-MP but may as well be primarily characterized by EUS-MP during a first diagnostic endoscopy.
GISTs are the most common and because of their malignant potential[168] most controversially discussed SEL. Therefore, they deserve a more detailed commentary. The anatomic locations of GISTs are frequently the stomach (60%–65%), and small bowel (25%–30%), less commonly colon and rectum (5%–6%) [Figure 12], and other various locations (5%), rarely esophagus (<1%).[169,170] Minute GISTs were found to have a frequency in autopsy series of 22.5%[171] or 35%[172] with an unknown potential for malignancy. GISTs (40%) and leiomyomas (30%) are the most prevalent gastric SEL.[173]
When small GIST-like SELs are encountered during endoscopy and at once characterized using EUS-MP regarding their size, sonographic pattern, and location [Figure 12], what is the next step? In gastric GISTs, surgical resection is recommended when tumors are 20 mm or larger in size, or when they are growing or have signs of malignancy, such as irregular margin, ulceration, bleeding, cystic change, necrosis, or heterogeneous echogenicity in endoscopy and/or EUS.[174,175,176,177] Because the natural course of small gastric GISTs, including growth rate and metastatic potential, remains largely unknown, the treatment strategy for gastric GISTs <20 mm is controversial.[178] Most guidelines consider a conservative follow-up by EUS every 6–12 months acceptable.[174,175,177,179,180,181] However, there is some evidence for a malignant potential of even small GISTs[182,183] in favor of resection of all gastrointestinal GISTs irrespective of size.[180,181,183] Therefore, patients should be informed about the possibility of malignancy, even if the tumor is small.[184] For nongastric GISTs, on the other hand, surgical resection is recommended, regardless of tumor size or morphology.[181] If the tumor is strongly suggestive of GIST and is considered resectable, preoperative biopsy can be omitted.[177,181,185,186]
On the other hand, optimal histopathology of a sufficient amount of tumor tissue is needed to diagnose GIST with certainty. The methods of biopsy include EUS-FNA, core needle biopsy, and different approaches of endoscopic biopsy. However, the pathological diagnosis is sometimes limited because of the small amount of tissue obtained.[187] EUS-guided diagnosis by FNA or core needle biopsy in small lesions is difficult to obtain.[188,189,190] Therefore, routine biopsy or puncture is not recommended for GISTs that are completely resectable. Postoperative pathology assessment is essential to confirm the diagnosis after removal of any suspected GIST. According to the above-cited guidelines,[174,175,177,179,180,181] for small gastric as well as for all other GIST-like SELs by EUS criteria, primary ER would be a reasonable strategy. Instead of periodic follow-up of gastric GIST-like SEL <20 mm and EUS-FNB in case of growth, it might be preferable to primarily resect these lesions if they are small and completely resectable without risk. The further proceeding would then depend on the histology of the resectate.[191] According to recent evidence, most small GISTs cause dyspepsia like symptoms related to their origin in gastrointestinal Cajal pacemaker cells.[192,193,194] Therefore, with the development of different low-risk ER-techniques,[173,195,196,197,198,199,200,201,202,203,204,205] the preemptive or therapeutic uncomplicated ER of small SEL like GISTs and similar lesions might become accepted standard. Wang et al. reported on ER of 648 small gastric GISTs without major complications and 98.5% en bloc resections.[206] They and others[178] found a tumor diameter of 9.5–14.5[184,204,207] mm the best cutoff value to predict malignant potential. According to a recent report by Zhu et al., out of 289 small gastric GISTs (2–20 mm, average 10 mm), 87% presented with symptoms. ER by ESD was successful in 247/250 tumors with a complete resection rate of 98.8%. Small perforations (2–10 mm) occurring in 67 (26.8%) were all endoscopically managed.[173] Analogous to preventive ER of potentially malignant neoplasia, like intestinal adenomas, ER of all GISTs seems reasonable. ER of all GIST-like SEL would harvest also other potentially threatening lesions such as NETs, lymphomas, or Dieulafoy's lesions,[173] however, also benign leiomyomas. Whether these could or should be differentiated by preinterventional EUS-guided puncture seems questionable, especially in small lesions because of technical difficulty. However, contrast-enhanced EUS was reported to allow accurate discrimination of GIST from leiomyomas.[208,209,210,211]
ESOPHAGEAL STENOSES AND LESIONS
In patients with dysphagia, EUS-MP can often clarify the pathologic anatomy [Figures 22-26]. In contrast to standard echoendoscopes, EUS-MP can be negotiated across even subtotal stenoses and thus provide more information. The response to endoscopic dilatation is predictable by delineating the extent of esophageal wall involvement in benign strictures. A retrospective study described 24 patients with benign esophageal strictures (corrosive 11, peptic 5, postradiation 3, anastomotic 2, and others 3) who underwent investigation with EUS-MP before endoscopic dilatation. The strictures were mainly located in the middle and lower esophagus, with a mean length of 3.4 cm. Mucosa only was involved in 6, mucosa and submucosa in 4, and all layers were thickened in the remaining patients. It was shown that patients with only mucosal involvement required significantly fewer endoscopic sessions for effective dilatation as compared to patients with muscularis propria involvement (1.8 vs. 6.2 sessions, respectively; P = 0.0002).[212]
Figure 22.
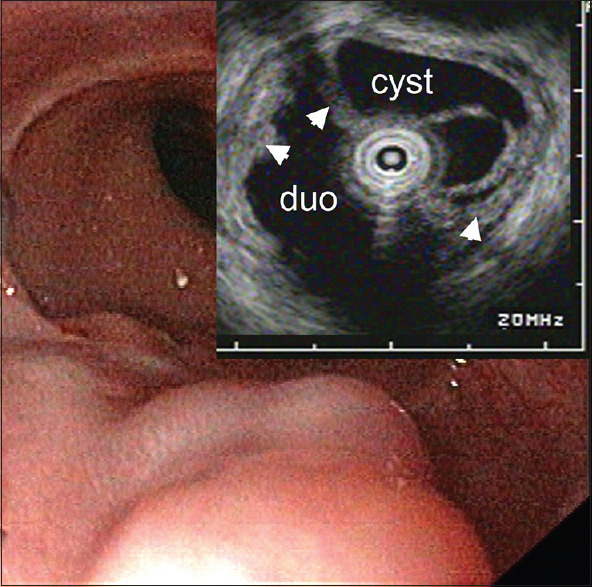
SEL in the lower esophagus. EUS-MP during routine EGD echo free submucosal cysts without any solid components. Esophageal lumen with water filling and intact mucosa (arrowheads), cyst: Anechoic contents of the cystic structure. Benign finding. duo: Duodenum
Figure 26.
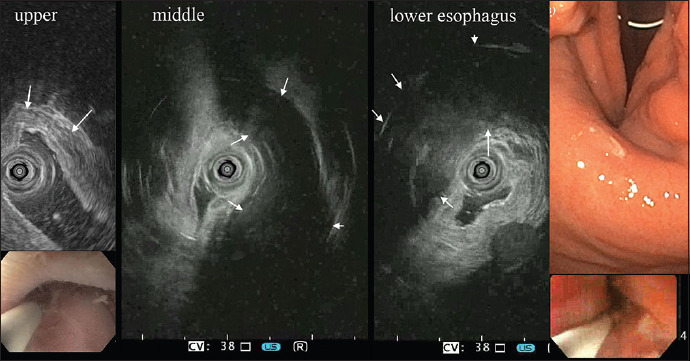
Dysphagia in a young female with Alport Syndrome. EUS-MP shows typical leiomyomatosis of the esophagus. M. propria (arrows) thickness increases from upper to lower esophagus. EGD in retroflexion shows the thick esophageal muscle at the cardia
Pathological changes of the esophageal muscular layers can be precisely analyzed by EUS-MP. Leiomyomatosis in patients with Alport syndrome shows characteristic thickening of the circular muscularis propria [Figure 26]. Thickening of the outer longitudinal muscle at the lower esophageal sphincter is associated with poor midterm treatment outcomes for achalasia patients treated with pneumatic dilatation.[213]
Figure 23.
A patient with unclear dysphagia. The endoscopic appearance of the esophagus is almost normal; the wall seems somewhat stiff without typical peristalsis. EUS-MP shows maintained layers with blurred separations and impressive widening of the SM-layer. PM is intact. Histology from snare biopsy revealed amyloidosis of the esophagus
Figure 24.
Smooth “SEL” in the middle esophagus. EUS-MP reveals external impression by an A. lusoria (arrow)
Figure 25.
A 64-year-old female with unclear esophageal stenosis and dysphagia. EUS-MP reveals ill-defined submucosal hypoechoic mass (arrowheads). M-layer seems intact; PM is lost within the lesion. Multiple biopsies revealed infiltration by a breast carcinoma that had been treated 16 years before. EUS-MP is not diagnostic but gives a clear picture of pathological anatomy
In cases of caustic ingestion, EUS-MP is useful to assess partial or full-wall damage in the acute or chronic stricture phase [Figure 27] and to predict the likelihood of stricture formation.
Figure 27.
(a) Acid ingestion, acute brake down of esophageal wall structure; colon interposition was performed. (b) Alkali ingestion, esophagus after 8 days with partial transmural necrosis. Conservative treatment led to a fibrotic asymmetric stricture with loss of wall architecture (c), requiring weekly bougienage (13 mm) until now. Only EUS-MP shows detailed pathological anatomy
Consecutive patients with esophagitis resulting from alkaline or acid chemical ingestion (n = 11) were evaluated prospectively by miniprobes between hospital days 4 and 12. Findings for the most severe lesion were classified according to the appearance of the muscular layers: distinct muscular layers without thickening (grade 0), distinct muscular layers with thickening (grade I), obscured muscular layers with indistinct margins (grade II), and muscular layers that could not be differentiated (grade III). Findings were also classified according to whether apparent damage to muscular layers in the worst appearing image involved part of the circumference (type a) or the whole circumference (type b). Implications of these findings for subsequent stricture formation were then evaluated. Stricture formation did not occur in patients with grade 0 or grade I lesions; transient stricture formation occurred in a patient showing grade IIa. Stricture requiring repeated bougie dilation occurred in a patient showing grade IIIb. It was hypothesized that EUS-MP images represented the damage to muscular layers (grades II to III), as opposed to only edema (grade I), thereby providing useful prognostic information.[214]
COMMON BILE DUCT DISORDERS
Fluoroscopy or wire-guided insertion of a miniprobe into the common bile duct during endoscopic retrograde cholangiopancreatography (ERCP) provides detailed visualization of the bile duct wall, periductal tissue, and bile duct content. Endoscopic sphincterotomy is not necessarily required before MP introduction. Pilot studies on autopsy specimens[215,216] have described a sonomorphological triple stratification of the normal bile duct. The potential importance of high-resolution imaging for small intraductal tumors of the pancreas and the periampullary region was recognized early on.[9,10,11,217,218]
Tamada et al. systematically evaluated the assessment of bile duct carcinomas by intraductal ultrasound (IDUS).[12,219,220,221,222,223,224,225] In distal and even in proximal bile duct carcinomas, invasion of the accompanying portal vein can be visualized.[226] An invasion of the pancreatic parenchyma could be visualized with a sensitivity of 100% (12/12 cases) by biliary IDUS (EUS: 78% and angiography: 61%). In the assessment of dignity of biliary strictures, the IDUS was most successful with an accuracy of 76%, inferior only to direct cholangioscopy (accuracy, 95%), and it was helpful for the targeted use of biopsy or cytology. An intact structure of the bile duct wall almost certainly ruled out malignancy.[227] In a small series of 10 patients with congenital cystic bile duct malformations, a cholangiographically invisible carcinoma of the bile duct was detected.[228] However, after Tamada's group, focused on biliary IDUS, was unable to reliably differentiate T1 from T2, the role of IDUS as a routine tool in biliary lesions was questioned.[220]
In a large cohort of 234 patients with indeterminate bile duct strictures, IDUS (91%) was superior to conventional EUS (74%), transpapillary biopsy (59%), and CT (73%) in detecting malignant lesions (P < 0.0001).[229] In a small series, wall thickening of the bile duct wall <7 mm at IDUS had high negative predictive value for differentiating malignant from benign biliary strictures.[230] In the absence of extrinsic compression, biliary wall thickness >7 mm had high positive predictive value for malignancy.[231] Other IDUS features suggestive of malignancy were disruption of wall echo layers, eccentric wall thickening, and hypoechoic masses with signs of vascular or surrounding tissue invasion [Figure 28].[232,233] Compared to surgical histopathology, preoperative miniprobe evaluation of 264 common bile duct strictures of unclear etiology resulted in correct diagnosis of malignancy with 93%–97% sensitivity, 79%–90% specificity, and 88%–92% accuracy.[234] However, IDUS could not reliably define longitudinal spread and surgical margins of bile duct cancer.[221,235,236] Accuracy for lymph node staging in bile duct carcinoma using IDUS (60%) was comparable to EUS (62.5%).[237] Prediction of resectability was correct in 82% of patients. On the other hand, in biliary stenoses caused by pancreatic cancer, lymph node staging with IDUS (13.3%) was significantly inferior to EUS (69.2%; P < 0.002).
Figure 28.
IDUS in a patient with CBD-obstruction shows the hypoechogenic invasive structure in the liver hilum penetrating the borders of the bile duct (arrow) with a small polyp like protrusion into the right hepatic duct
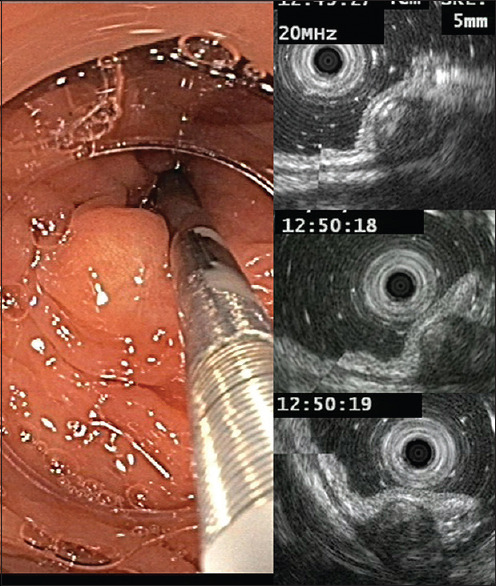
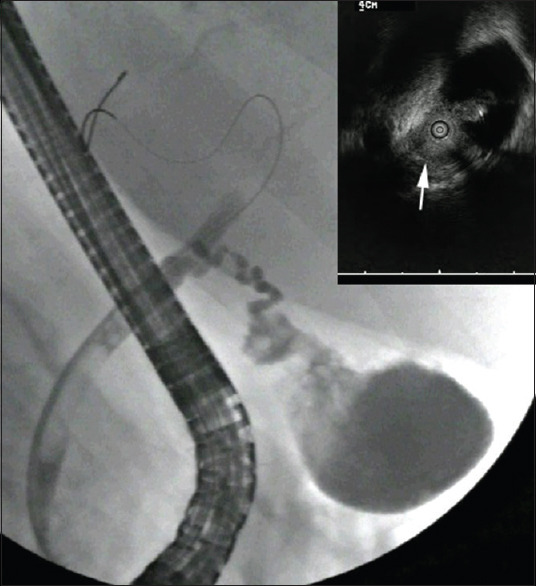
Extraductal ultrasound (EDUS) with a miniprobe at the level of the ampulla allows visualization of the distal common bile duct running close to the duodenal wall without the associated risks of post-ERCP pancreatitis [Figures 29 and 30].[238] In patients at intermediate risk of common bile duct stones, it is reasonable to perform EDUS first in order to proceeded to ERCP only when stones are present.[239] The diagnostic accuracy of standard EUS (sensitivity, 92%; specificity, 100%; PPV, 1.0; NPV, 0.93; and accuracy 95%) and EDUS (sensitivity, 90%; specificity, 98%; PPV, 0.99; NPV, 0.93; accuracy, 91%) was comparable for detecting stones in the distal common bile duct. Another study reported intraductal stones with EDUS in the absence of ductal dilatation with a sensitivity of 97% and a specificity of 98%.[240] It was also shown that EDUS of the common bile duct was safe in elderly patients with suspicion of choledocholithiasis after distal gastrectomy.[241]
Figure 29.
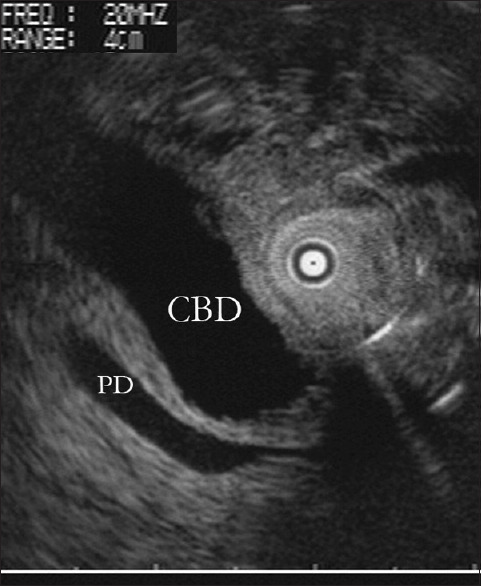
Extraductal ultrasound (extraductal EUS-MP) of the common bile duct (CBD) and the pancreatic duct (PD) shows the periampullary distal part of both ducts in their relation to the duodenal wall. The miniprobe is in the duodenal position just oral of the major papilla. Normal anatomy
Figure 30.
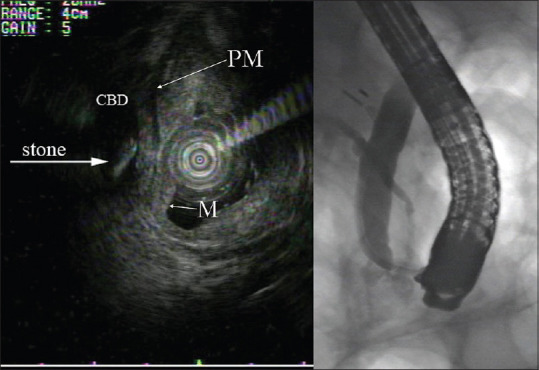
EDUS in a patient with suspected biliary pancreatitis without biochemical cholestasis and nondilated bile ducts. EDUS clearly detected a small floating stone in the common bile duct (CBD). The duodenal wall with M- and PM layers is clearly visible (left panel). The stone was not seen on the following ERC (right panel) but extracted after papillotomy
PANCREATIC DISORDERS
With curved-linear echoendoscopes even minute details of the pancreatic duct can be delineated and if adequate, sampled for cyto- or even histopath-ology. Without manipulating the papilla and the pancreatic duct,contrast-enhanced EUS[248,249,250,251,252] or elastography[253,255,256,257,258,259] are possible. The stiffness of miniprobes that makes it problematic to follow the angulated main duct prevents most endoscopists from performing IDUS of the pancreas.[242]
In some cases, IDUS was helpful to delineate small pancreatic cancers and NET.[243,244] Preoperative IDUS evaluating the extension of intraductal papillary mucinous neoplasm was accurate in up to 92%.[245,246,247]
SOLITARY PULMONARY NODULE [SPN]
Launched in 1999, the radial radial endobronchial ultrasound (EBUS) probe (Olympus Cooperation, Tokyo, Japan) probe employs a flexible catheter housing a rotating ultrasound transducer, which produces a 360° ultrasound image and was first used for guided transbronchial lung biopsy by Herth et al.[258] During the bronchoscopy, the 20-MHz mechanical probe is inserted through a guide sheath into the periphery of the lung. If a typical ultrasonographic image of a nodule appears, the probe is removed, and the guide sheath is left in place. Various groups have published their experience with EBUS-guided evaluation of SPNs. In a published meta-analysis by Steinfort et al.,[259] >1400 patients were evaluated. Radial EBUS-guided transbronchial biopsy showed a specificity of 1.00 and sensitivity of 0.73 for the diagnosis of lung cancer. Significant inter-study heterogeneity for sensitivity was seen, which does not allow direct comparison of studies. The results of the studies depend on the prevalence of malignancy, lesion size, probe placement within the lesion or next to, and the use of fluoroscopy.
Unfortunately, the radial EBUS probes are not steerable. Therefore, navigation support might be helpful, especially in lesions smaller than 2 centimeters. Eberhardt et al.[260] showed that combining EBUS with electromagnetic navigation bronchioscopy (ENB), gaining the benefits of real time control and the steer ability has an advantage over using one technique alone. The diagnostic yield of the combined procedure (88%) was greater than either endobronchial ultrasound (69%) or electromagnetic navigation alone. Comparable data have been published by Steinfort et al.[261] On the other hand, rEBUS is the most frequent technique used worldwide to confirm the lesion in real time during the procedure. Moving in the direction of endobronchial therapies of SPNs, rEBUS will be the most widely available method to confirm the probe placement before any therapeutic approach.
T classification: Invasion versus compression
In preoperative staging, rEBUS allows detailed analysis of intraluminal, submucosal and intramural tumor spread which can be essential for decisions on resection margins. EBUS has proved to be useful in the diagnosis of mediastinal tumor involvement in areas such as the large vessels and the esophageal wall, which is frequently impossible with conventional radiology. In a prospective study, it was shown that differentiation of external tumor invasion from compression of the tracheobronchial wall by EBUS is more reliable than CT imaging. Thus, many lesions considered to be non resectable by the radiologist due to supposed T4 tumors could be operated in a curative approach after EBUS.[262]
Carcinoma in situ
In small radiologically invisible tumors like carcinoma in situ, the decision for local endoscopic therapeutic intervention is dependent on their intraluminal and intramural extent within the multilayer structures of the bronchial wall and the adjacent structures. rEBUS is a very reliable tool in analyzing the extent of these small lesions. Especially for decisions in potentially curative endobronchial therapy such as photodynamic therapy or endoluminal high-dose radiation, rEBUS is superior to all other imaging procedures due to the detailed analysis of the layers of the bronchial wall.[263,264]
DISCUSSION AND SUMMARY
Longitudinally scanning EUS has despite the improvement of CT and MRI-technology firmly established its role due to the combination of relatively low cost, versatile use, high image quality and guidance of diagnostic and therapeutic transmural interventions. Nonetheless, EUS-MP, classic radial scanners with extremely high resolution, have defended their position in the bronchial system and also as a valuable adjunct to gastrointestinal endoscopy. While for biliary and pancreatic pathology their role is insignificant, they provide detailed characterization of all, even diminutive, mural lesions in upper and lower endoscopy. Unrivaled by any other diagnostic approach, EUS-MP allows imaging of details relevant for diagnosis and therapy. The possible impact on the detection of SEL during routine endoscopy and possibly full wall resection of all small colonic GISTs seems an important perspective. For good reasons, published images illustrating the sonomorphology of SEL, particularly GIST, generally show high-resolution EUS-MP pictures.[152,157,169,208,265,266] According to some of the authors, EUS-MP are therefore of great value for the ad hoc characterization of early carcinomas and SEL in the entire intestinal tract and, in individual cases, for periampullary lesions - with no more side effects than standard endoscopy and at potentially acceptable costs.One criterion for the assessment of a procedure is how it is used, if freely available, by busy endoscopists outside of studies in clinical routine. Our own experience shows that under such conditions the number of EUS-MP applications equals the number of classical EUS.[118] While the latter, with often only one or two instruments available, usually requires a separate additional session with the corresponding preparation, EUS-MP is performed in a few minutes. With a life span of 50-100 procedures EUS-MP should run at a figure comparable to one or two hemoclips. Especially regarding SEL that might often be overlooked EUS-MP could be attractive during routine endoscopies. Instead of dedicated echoendoscopes, EUS-MP could be the practitioner's quick-and-easy-EUS. Durability and price of EUS-MP as well as reimbursement should be adapted according to this perspective. The main weaknesses of miniprobes, namely their fragility at high cost, prevent their establishment in endoscopic routine and threaten their survival. Otherwise, they could become an endoscopic everyday standard, even outside of centers, like virtual chromoendoscopy.
Financial support and sponsorship
Nil.
Conflicts of interest
Anand V Sahai is the Honoary Editor-in-Chief of the journal. Christoph F. Dietrich is the Co-Editor-in-Chief of the journal. Pietro Fusaroli, Paolo Giorgio Arcidiacono and Adrian Săftoiu are Associate Editors of the journal. Felix Herth, Michael Hocke, and Alberto Larghi are Editorial Board Members of Endoscopic Ultrasound. The article was subject to the journal's standard procedures, with peer review handled independently of this Member and their research groups.
REFERENCES
- 1.Dietrich CF, Arcidiacono PG, Braden B, et al. What should be known prior to performing EUS? Endosc Ultrasound. 2019;8:3–16. doi: 10.4103/eus.eus_54_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dietrich CF, Arcidiacono PG, Braden B, et al. What should be known prior to performing EUS exams.(Part II)? Endosc Ultrasound. 2019;8:360–9. doi: 10.4103/eus.eus_57_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dietrich CF, Burmeister S, Hollerbach S, et al. Do we need elastography for EUS? Endosc Ultrasound. 2020;9:284–90. doi: 10.4103/eus.eus_25_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saftoiu A, Napoleon B, Arcidiacono PG, et al. Do we need contrast agents for EUS? Endosc Ultrasound. 2020;9:361–8. doi: 10.4103/eus.eus_20_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Testoni SG, Healey AJ, Dietrich CF, et al. Systematic review of endoscopy ultrasound-guided thermal ablation treatment for pancreatic cancer. Endosc Ultrasound. 2020;9:83–100. doi: 10.4103/eus.eus_74_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fusaroli P, Kypreos D, Alma Petrini CA, et al. Scientific publications in endoscopic ultrasonography: Changing trends in the third millennium. J Clin Gastroenterol. 2011;45:400–4. doi: 10.1097/MCG.0b013e3181fbde42. [DOI] [PubMed] [Google Scholar]
- 7.Fusaroli P, Kypraios D, Eloubeidi MA, et al. Levels of evidence in endoscopic ultrasonography: A systematic review. Dig Dis Sci. 2012;57:602–9. doi: 10.1007/s10620-011-1961-y. [DOI] [PubMed] [Google Scholar]
- 8.Yoshinaga S, Oda I, Nonaka S, et al. Endoscopic ultrasound using ultrasound probes for the diagnosis of early esophageal and gastric cancers. World J Gastrointest Endosc. 2012;4:218–26. doi: 10.4253/wjge.v4.i6.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Odegaard S, Kimmey MB, Martin RW, et al. The effects of applied pressure on the thickness, layers, and echogenicity of gastrointestinal wall ultrasound images. Gastrointest Endosc. 1992;38:351–6. doi: 10.1016/s0016-5107(92)70431-3. [DOI] [PubMed] [Google Scholar]
- 10.Herth F, Becker HD, Manegold C, et al. Endobronchial ultrasound (EBUS)-Assessment of a new diagnostic tool in bronchoscopy for staging of lung cancer. Onkologie. 2001;24:151–4. doi: 10.1159/000050303. [DOI] [PubMed] [Google Scholar]
- 11.Hürter T, Hanrath P. Endobronchial sonography: Feasibility and preliminary results. Thorax. 1992;47:565–7. doi: 10.1136/thx.47.7.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tamada K, Kanai N, Tomiyama T, et al. Prediction of the histologic type of bile duct cancer by using intraductal ultrasonography. Abdom Imaging. 1999;24:484–90. doi: 10.1007/s002619900545. [DOI] [PubMed] [Google Scholar]
- 13.Martin RW, Silverstein FE, Kimmey MB. A 20-MHz ultrasound system for imaging the intestinal wall. Ultrasound Med Biol. 1989;15:273–80. doi: 10.1016/0301-5629(89)90071-9. [DOI] [PubMed] [Google Scholar]
- 14.Akashi K, Yanai H, Nishikawa J, et al. Ulcerous change decreases the accuracy of endoscopic ultrasonography diagnosis for the invasive depth of early gastric cancer. Int J Gastrointest Cancer. 2006;37:133–8. doi: 10.1007/s12029-007-9004-9. [DOI] [PubMed] [Google Scholar]
- 15.May A, Günter E, Roth F, et al. Accuracy of staging in early oesophageal cancer using high resolution endoscopy and high resolution endosonography: A comparative, prospective, and blinded trial. Gut. 2004;53:634–40. doi: 10.1136/gut.2003.029421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chemaly M, Scalone O, Durivage G, et al. Miniprobe EUS in the pretherapeutic assessment of early esophageal neoplasia. Endoscopy. 2008;40:2–6. doi: 10.1055/s-2007-966958. [DOI] [PubMed] [Google Scholar]
- 17.Tsung PC, Park JH, Kim YS, et al. Miniprobe endoscopic ultrasonography has limitations in determining the T stage in early colorectal cancer. Gut Liver. 2013;7:163–8. doi: 10.5009/gnl.2013.7.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamanaka T. JGES consensus meeting report in DDW-Japan 2000, Kobe: Interpretation of the layered structure of the gastrointestinal wall with endoscopic ultrasonography. Dig Endosc. 2002;14:39–40. [Google Scholar]
- 19.Odegaard S, Nesje LB, Gilja OH, et al. High frequency ultrasonography of the gastrointestinal wall. Tidsskr Nor Laegeforen. 1996;116:1455–9. [PubMed] [Google Scholar]
- 20.Hasegawa N, Niwa Y, Arisawa T, et al. Preoperative staging of superficial esophageal carcinoma: Comparison of an ultrasound probe and standard endoscopic ultrasonography. Gastrointest Endosc. 1996;44:388–93. doi: 10.1016/s0016-5107(96)70086-x. [DOI] [PubMed] [Google Scholar]
- 21.Hünerbein M, Ulmer C, Handke T, et al. Endosonography of upper gastrointestinal tract cancer on demand using miniprobes or endoscopic ultrasound. Surg Endosc. 2003;17:615–9. doi: 10.1007/s00464-002-8622-3. [DOI] [PubMed] [Google Scholar]
- 22.Menzel J, Hoepffner N, Nottberg H, et al. Preoperative staging of esophageal carcinoma: Miniprobe sonography versus conventional endoscopic ultrasound in a prospective histopathologically verified study. Endoscopy. 1999;31:291–7. doi: 10.1055/s-1999-12. [DOI] [PubMed] [Google Scholar]
- 23.Pech O, Günter E, Dusemund F, et al. Value of high-frequency miniprobes and conventional radial endoscopic ultrasound in the staging of early Barrett's carcinoma. Endoscopy. 2010;42:98–103. doi: 10.1055/s-0029-1243839. [DOI] [PubMed] [Google Scholar]
- 24.Seifert H, Kikuchi D, Yahagi N. High-resolution endoscopic ultrasound: Clinical t-staging of superficial and subepithelial gastrointestinal neoplasias. In: Berr F, Oyama T, Ponchon T, Yahagi N, editors. Atlas of Early Neoplasias of the Gastrointestinal Tract. 2nd ed. Cham, Switzerland: Springer; 2019. [Google Scholar]
- 25.Pech O, May A, Günter E, et al. The impact of endoscopic ultrasound and computed tomography on the TNM staging of early cancer in Barrett's esophagus. Am J Gastroenterol. 2006;101:2223–9. doi: 10.1111/j.1572-0241.2006.00718.x. [DOI] [PubMed] [Google Scholar]
- 26.Japan Esophageal Society. Japanese Classification of Esophageal Cancer, 11th Edition: Part I. Esophagus. 2017;14:1–36. doi: 10.1007/s10388-016-0551-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murata Y, Napoleon B, Odegaard S. High-frequency endoscopic ultrasonography in the evaluation of superficial esophageal cancer. Endoscopy. 2003;35:429–35. doi: 10.1055/s-2003-38774. [DOI] [PubMed] [Google Scholar]
- 28.Meister T, Heinzow HS, Osterkamp R, et al. Miniprobe endoscopic ultrasound accurately stages esophageal cancer and guides therapeutic decisions in the era of neoadjuvant therapy: Results of a multicenter cohort analysis. Surg Endosc. 2013;27:2813–9. doi: 10.1007/s00464-013-2817-7. [DOI] [PubMed] [Google Scholar]
- 29.Dobashi A, Goda K, Yoshimura N, et al. Simplified criteria for diagnosing superficial esophageal squamous neoplasms using Narrow Band Imaging magnifying endoscopy. World J Gastroenterol. 2016;22:9196–204. doi: 10.3748/wjg.v22.i41.9196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goda K, Dobashi A, Yoshimura N, et al. Narrow-band imaging magnifying endoscopy versus lugol chromoendoscopy with pink-color sign assessment in the diagnosis of superficial esophageal squamous neoplasms: A randomised noninferiority trial. Gastroenterol Res Pract. 2015;2015:639462. doi: 10.1155/2015/639462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee CT, Chang CY, Lee YC, et al. Narrow-band imaging with magnifying endoscopy for the screening of esophageal cancer in patients with primary head and neck cancers. Endoscopy. 2010;42:613–9. doi: 10.1055/s-0030-1255514. [DOI] [PubMed] [Google Scholar]
- 32.Nagai K, Ishihara R, Ishiguro S, et al. Endoscopic optical diagnosis provides high diagnostic accuracy of esophageal squamous cell carcinoma. BMC Gastroenterol. 2014;14:141. doi: 10.1186/1471-230X-14-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ishihara R, Takeuchi Y, Chatani R, et al. Prospective evaluation of narrow-band imaging endoscopy for screening of esophageal squamous mucosal high-grade neoplasia in experienced and less experienced endoscopists. Dis Esophagus. 2010;23:480–6. doi: 10.1111/j.1442-2050.2009.01039.x. [DOI] [PubMed] [Google Scholar]
- 34.Asada-Hirayama I, Kodashima S, Fujishiro M, et al. Narrow band imaging with magnification can pick up esophageal squamous cell carcinoma more efficiently than lugol chromoendoscopy in patients after chemoradiotherapy. Diagn Ther Endosc. 2013;2013:256439. doi: 10.1155/2013/256439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goda K, Tajiri H, Ikegami M, et al. Magnifying endoscopy with narrow band imaging for predicting the invasion depth of superficial esophageal squamous cell carcinoma. Dis Esophagus. 2009;22:453–60. doi: 10.1111/j.1442-2050.2009.00942.x. [DOI] [PubMed] [Google Scholar]
- 36.Ebi M, Shimura T, Yamada T, et al. Multicenter, prospective trial of white-light imaging alone versus white-light imaging followed by magnifying endoscopy with narrow-band imaging for the real-time imaging and diagnosis of invasion depth in superficial esophageal squamous cell carcinoma. Gastrointest Endosc. 2015;81:1355–6100. doi: 10.1016/j.gie.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 37.Lee MW, Kim GH, IH, et al. Predicting the invasion depth of esophageal squamous cell carcinoma: Comparison of endoscopic ultrasonography and magnifying endoscopy. Scand J Gastroenterol. 2014;49:853–61. doi: 10.3109/00365521.2014.915052. [DOI] [PubMed] [Google Scholar]
- 38.Yu T, Geng J, Song W, et al. Diagnostic accuracy of magnifying endoscopy with narrow band imaging and its diagnostic value for invasion depth staging in esophageal squamous cell carcinoma: A systematic review and meta-analysis. Biomed Res Int. 2018;2018:8591387. doi: 10.1155/2018/8591387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim SJ, Choi CW, Kang DH, et al. Factors associated with the efficacy of miniprobe endoscopic ultrasonography after conventional endoscopy for the prediction of invasion depth of early gastric cancer. Scand J Gastroenterol. 2017;52:864–9. doi: 10.1080/00365521.2017.1315167. [DOI] [PubMed] [Google Scholar]
- 40.Tao Z, Yan C, Zhao H, et al. Comparison of endoscopic ultrasonography and magnifying endoscopy for assessment of the invasion depth of shallow gastrointestinal neoplasms: A systematic review and meta-analysis. Surg Endosc. 2017;31:4923–33. doi: 10.1007/s00464-017-5596-8. [DOI] [PubMed] [Google Scholar]
- 41.Arima M, Arima H, Tada M, et al. Diagnostic accuracy of tumor staging and treatment outcomes in patients with superficial esophageal cancer. Esophagus. 2007;4:145–53. [Google Scholar]
- 42.Shimura T, Ebi M, Yamada T, et al. Magnifying chromoendoscopy and endoscopic ultrasonography measure invasion depth of early stage colorectal cancer with equal accuracy on the basis of a prospective trial. Clin Gastroenterol Hepatol. 2014;12:662–80. doi: 10.1016/j.cgh.2013.06.022. [DOI] [PubMed] [Google Scholar]
- 43.Fu KI, Kato S, Sano Y, et al. Staging of early colorectal cancers: Magnifying colonoscopy versus endoscopic ultrasonography for estimation of depth of invasion. Dig Dis Sci. 2008;53:1886–92. doi: 10.1007/s10620-007-0104-y. [DOI] [PubMed] [Google Scholar]
- 44.Matsumoto T, Hizawa K, Esaki M, et al. Comparison of EUS and magnifying colonoscopy for assessment of small colorectal cancers. Gastrointest Endosc. 2002;56:354–60. doi: 10.1016/s0016-5107(02)70038-2. [DOI] [PubMed] [Google Scholar]
- 45.Yamada T, Shimura T, Ebi M, et al. Subset analysis of a multicenter, randomized controlled trial to compare magnifying chromoendoscopy with endoscopic ultrasonography for stage diagnosis of early stage colorectal cancer. PLoS One. 2015;10:e0134942. doi: 10.1371/journal.pone.0134942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mizumoto T, Hiyama T, Oka S, et al. Diagnosis of superficial esophageal squamous cell carcinoma invasion depth before endoscopic submucosal dissection. Dis Esophagus. 2018;31 doi: 10.1093/dote/dox142. [DOI] [PubMed] [Google Scholar]
- 47.Ishihara R, Arima M, Iizuka T, et al. Endoscopic submucosal dissection/endoscopic mucosal resection guidelines for esophageal cancer. Dig Endosc. 2020;32:452–93. doi: 10.1111/den.13654. [DOI] [PubMed] [Google Scholar]
- 48.Kim SJ, Kim GH, Lee MW, et al. New magnifying endoscopic classification for superficial esophageal squamous cell carcinoma. World J Gastroenterol. 2017;23:4416–21. doi: 10.3748/wjg.v23.i24.4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Park SY, Kim DJ, Suh JW, et al. Comparison of the 11(th) Japanese classification and the AJCC 7(th) and 8(th) staging systems in esophageal squamous cell carcinoma patients. J Thorac Dis. 2018;10:5039–46. doi: 10.21037/jtd.2018.07.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ishihara R, Goda K, Oyama T. Endoscopic diagnosis and treatment of esophageal adenocarcinoma: Introduction of Japan Esophageal Society classification of Barrett's esophagus. J Gastroenterol. 2019;54:1–9. doi: 10.1007/s00535-018-1491-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Goda K, Fujisaki J, Ishihara R, et al. Newly developed magnifying endoscopic classification of the Japan Esophageal Society to identify superficial Barrett's esophagus-related neoplasms. Esophagus. 2018;15:153–9. doi: 10.1007/s10388-018-0623-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oyama T, Inoue H, Arima M, et al. Prediction of the invasion depth of superficial squamous cell carcinoma based on microvessel morphology: Magnifying endoscopic classification of the Japan Esophageal Society. Esophagus. 2017;14:105–12. doi: 10.1007/s10388-016-0527-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Santi EG, Inoue H, Ikeda H, et al. Microvascular caliber changes in intramucosal and submucosally invasive esophageal cancer. Endoscopy. 2013;45:585–8. doi: 10.1055/s-0033-1344228. [DOI] [PubMed] [Google Scholar]
- 54.Inoue H, Kaga M, Ikeda H, et al. Magnification endoscopy in esophageal squamous cell carcinoma: A review of the intrapapillary capillary loop classification. Ann Gastroenterol. 2015;28:41–8. [PMC free article] [PubMed] [Google Scholar]
- 55.Seki M, Sano T, Yokoo S, et al. Tumour budding evaluated in biopsy specimens is a useful predictor of prognosis in patients with cN0 early stage oral squamous cell carcinoma. Histopathology. 2017;70:869–79. doi: 10.1111/his.13144. [DOI] [PubMed] [Google Scholar]
- 56.Khanna LG, Gress FG. Preoperative evaluation of oesophageal adenocarcinoma. Best Pract Res Clin Gastroenterol. 2015;29:179–91. doi: 10.1016/j.bpg.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 57.Castro-Pocas FM, Dinis-Ribeiro M, Rocha A, et al. Colon carcinoma staging by endoscopic ultrasonography miniprobes. Endosc Ultrasound. 2017;6:245–51. doi: 10.4103/2303-9027.190921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee HN, Kim JI, Shin SY, et al. Combined CT texture analysis and nodal axial ratio for detection of nodal metastasis in esophageal cancer. Br J Radiol. 2020;93:20190827. doi: 10.1259/bjr.20190827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee JY, Kim YH, Park YJ, et al. Improved detection of metastatic lymph nodes in oesophageal squamous cell carcinoma by combined interpretation of fluorine-18-fluorodeoxyglucose positron-emission tomography/computed tomography. Cancer Imaging. 2019;19:40. doi: 10.1186/s40644-019-0225-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wakita A, Motoyama S, Sato Y, et al. Evaluation of metastatic lymph nodes in cN0 thoracic esophageal cancer patients with inconsistent pathological lymph node diagnosis. World J Surg Oncol. 2020;18:111. doi: 10.1186/s12957-020-01880-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karstens KF, Ghadban T, Effenberger K, et al. Lymph node and bone marrow micrometastases define the prognosis of patients with pN0 esophageal cancer. Cancers (Basel) 2020;12:588. doi: 10.3390/cancers12030588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.van der Bogt RD, van der Wilk BJ, Poley JW, et al. Endoscopic ultrasound and fine-needle aspiration for the detection of residual nodal disease after neoadjuvant chemoradiotherapy for esophageal cancer. Endoscopy. 2020;52:186–92. doi: 10.1055/a-1065-1759. [DOI] [PubMed] [Google Scholar]
- 63.Aoyama J, Kawakubo H, Mayanagi S, et al. Discrepancy between the clinical and final pathological findings of lymph node metastasis in superficial esophageal cancer. Ann Surg Oncol. 2019;26:2874–81. doi: 10.1245/s10434-019-07498-2. [DOI] [PubMed] [Google Scholar]
- 64.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 65.Nakayoshi T, Tajiri H, Matsuda K, et al. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: Correlation of vascular pattern with histopathology (including video) Endoscopy. 2004;36:1080–4. doi: 10.1055/s-2004-825961. [DOI] [PubMed] [Google Scholar]
- 66.Yao K, Doyama H, Gotoda T, et al. Diagnostic performance and limitations of magnifying narrow-band imaging in screening endoscopy of early gastric cancer: A prospective multicenter feasibility study. Gastric Cancer. 2014;17:669–79. doi: 10.1007/s10120-013-0332-0. [DOI] [PubMed] [Google Scholar]
- 67.Doyama H, Nakanishi H, Yao K. Image-enhanced endoscopy and its corresponding histopathology in the stomach. Gut Liver. 2020 doi: 10.5009/gnl19392. doi: 10.5009/gnl19392. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Doyama H, Yoshida N, Tsuyama S, et al. The “white globe appearance” (WGA): A novel marker for a correct diagnosis of early gastric cancer by magnifying endoscopy with narrow-band imaging (M-NBI) Endosc Int Open. 2015;3:E120–4. doi: 10.1055/s-0034-1391026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kanesaka T, Uedo N, Yao K, et al. A significant feature of microvessels in magnifying narrow-band imaging for diagnosis of early gastric cancer. Endosc Int Open. 2015;3:E590–6. doi: 10.1055/s-0034-1392608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yao K, Anagnostopoulos GK, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy. 2009;41:462–7. doi: 10.1055/s-0029-1214594. [DOI] [PubMed] [Google Scholar]
- 71.Zhang Q, Wang F, Chen ZY, et al. Comparison of the diagnostic efficacy of white light endoscopy and magnifying endoscopy with narrow band imaging for early gastric cancer: A meta-analysis. Gastric Cancer. 2016;19:543–52. doi: 10.1007/s10120-015-0500-5. [DOI] [PubMed] [Google Scholar]
- 72.Maki S, Yao K, Nagahama T, et al. Magnifying endoscopy with narrow-band imaging is useful in the differential diagnosis between low-grade adenoma and early cancer of superficial elevated gastric lesions. Gastric Cancer. 2013;16:140–6. doi: 10.1007/s10120-012-0160-7. [DOI] [PubMed] [Google Scholar]
- 73.Muto M, Yao K, Kaise M, et al. Magnifying endoscopy simple diagnostic algorithm for early gastric cancer (MESDA-G) Dig Endosc. 2016;28:379–93. doi: 10.1111/den.12638. [DOI] [PubMed] [Google Scholar]
- 74.Yoshida N, Doyama H, Yano T, et al. Early gastric cancer detection in high-risk patients: A multicentre randomised controlled trial on the effect of second-generation narrow band imaging. Gut. 2021;70:67–75. doi: 10.1136/gutjnl-2019-319631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gotoda T, Uedo N, Yoshinaga S, et al. Basic principles and practice of gastric cancer screening using high-definition white-light gastroscopy: Eyes can only see what the brain knows. Dig Endosc. 2016;28(Suppl 1):2–15. doi: 10.1111/den.12623. [DOI] [PubMed] [Google Scholar]
- 76.Shimodate Y, Mizuno M, Doi A, et al. Gastric superficial neoplasia: High miss rate but slow progression. Endosc Int Open. 2017;5:E722–6. doi: 10.1055/s-0043-110076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yao K, Uedo N, Muto M, et al. Development of an e-learning system for the endoscopic diagnosis of early gastric cancer: An international multicenter randomized controlled trial. EBioMedicine. 2016;9:140–7. doi: 10.1016/j.ebiom.2016.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sumiyama K, Kaise M, Nakayoshi T, et al. Combined use of a magnifying endoscope with a narrow band imaging system and a multibending endoscope for en bloc EMR of early stage gastric cancer. Gastrointest Endosc. 2004;60:79–84. doi: 10.1016/s0016-5107(04)01285-4. [DOI] [PubMed] [Google Scholar]
- 79.Kato M, Kaise M, Yonezawa J, et al. Magnifying endoscopy with narrow-band imaging achieves superior accuracy in the differential diagnosis of superficial gastric lesions identified with white-light endoscopy: A prospective study. Gastrointest Endosc. 2010;72:523–9. doi: 10.1016/j.gie.2010.04.041. [DOI] [PubMed] [Google Scholar]
- 80.Hayee B, Inoue H, Sato H, et al. Magnification narrow-band imaging for the diagnosis of early gastric cancer: A review of the Japanese literature for the Western endoscopist. Gastrointest Endosc. 2013;78:452–61. doi: 10.1016/j.gie.2013.03.1333. [DOI] [PubMed] [Google Scholar]
- 81.Yao K. Clinical application of magnifying endoscopy with narrow-band imaging in the stomach. Clin Endosc. 2015;48:481–90. doi: 10.5946/ce.2015.48.6.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yao K, Uedo N, Muto M, et al. Development of an e-learning system for teaching endoscopists how to diagnose early gastric cancer: Basic principles for improving early detection. Gastric Cancer. 2017;20:28–38. doi: 10.1007/s10120-016-0680-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Luo M, Li L. Clinical utility of miniprobe endoscopic ultrasonography for prediction of invasion depth of early gastric cancer: A meta-analysis of diagnostic test from PRISMA guideline. Medicine (Baltimore) 2019;98:e14430. doi: 10.1097/MD.0000000000014430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tada M, Shimada M, Murakami F, et al. Development of the strip-off biopsy. (In Japanese with English abstracts. Cited after Sano T. et al., Br J Surg 1992) Gastroenterol Endosc. 1984;26:833–9. [Google Scholar]
- 85.Karita M, Tada M, Okita K. The successive strip biopsy partial resection technique for large early gastric and colon cancers. Gastrointest Endosc. 1992;38:174–8. doi: 10.1016/s0016-5107(92)70386-1. [DOI] [PubMed] [Google Scholar]
- 86.Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: Estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–25. doi: 10.1007/pl00011720. [DOI] [PubMed] [Google Scholar]
- 87.Hirasawa T, Gotoda T, Miyata S, et al. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12:148–52. doi: 10.1007/s10120-009-0515-x. [DOI] [PubMed] [Google Scholar]
- 88.Karita M, Tada M, Okita K, et al. Definition of the adaptation of endoscopic surgery for early gastric cancer.Special examination on the relationship between the histological differentiation of the intramucosal gastric cancer and the lymph node metastasis. Nihon Gan Chiryo Gakkai Shi. 1989;24:1572–84. [PubMed] [Google Scholar]
- 89.Inoue K, Tobe T, Kan N, et al. Problems in the definition and treatment of early gastric cancer. Br J Surg. 1991;78:818–21. doi: 10.1002/bjs.1800780717. [DOI] [PubMed] [Google Scholar]
- 90.Sano T, Kobori O, Muto T. Lymph node metastasis from early gastric cancer: Endoscopic resection of tumour. Br J Surg. 1992;79:241–4. doi: 10.1002/bjs.1800790319. [DOI] [PubMed] [Google Scholar]
- 91.Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma-2nd English Edition. Gastric Cancer. 1998;1:10–24. doi: 10.1007/s101209800016. [DOI] [PubMed] [Google Scholar]
- 92.Gotoda T, Kondo H, Ono H, et al. A new endoscopic mucosal resection procedure using an insulation-tipped electrosurgical knife for rectal flat lesions: Report of two cases. Gastrointest Endosc. 1999;50:560–3. doi: 10.1016/s0016-5107(99)70084-2. [DOI] [PubMed] [Google Scholar]
- 93.Ahn JY, Park HJ, Park YS, et al. Endoscopic resection for undifferentiated-type early gastric cancer: Immediate endoscopic outcomes and long-term survivals. Dig Dis Sci. 2016;61:1158–64. doi: 10.1007/s10620-015-3988-y. [DOI] [PubMed] [Google Scholar]
- 94.Lee S, Choi KD, Han M, et al. Long-term outcomes of endoscopic submucosal dissection versus surgery in early gastric cancer meeting expanded indication including undifferentiated-type tumors: A criteria-based analysis. Gastric Cancer. 2018;21:490–9. doi: 10.1007/s10120-017-0772-z. [DOI] [PubMed] [Google Scholar]
- 95.Hatta W, Gotoda T, Koike T, et al. History and future perspectives in Japanese guidelines for endoscopic resection of early gastric cancer. Dig Endosc. 2020;32:180–90. doi: 10.1111/den.13531. [DOI] [PubMed] [Google Scholar]
- 96.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition) Gastric Cancer. 2021;24:1–21. doi: 10.1007/s10120-020-01042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Park CH, Shin S, Park JC, et al. Long-term outcome of early gastric cancer after endoscopic submucosal dissection: Expanded indication is comparable to absolute indication. Dig Liver Dis. 2013;45:651–6. doi: 10.1016/j.dld.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 98.Hasuike N, Ono H, Boku N, et al. A non-randomized confirmatory trial of an expanded indication for endoscopic submucosal dissection for intestinal-type gastric cancer (cT1a): The Japan Clinical Oncology Group study (JCOG0607) Gastric Cancer. 2018;21:114–23. doi: 10.1007/s10120-017-0704-y. [DOI] [PubMed] [Google Scholar]
- 99.Fukunaga S, Nagami Y, Shiba M, et al. Long-term prognosis of expanded-indication differentiated-type early gastric cancer treated with endoscopic submucosal dissection or surgery using propensity score analysis. Gastrointest Endosc. 2017;85:143–52. doi: 10.1016/j.gie.2016.06.049. [DOI] [PubMed] [Google Scholar]
- 100.Kim YI, Kim YW, Choi IJ, et al. Long-term survival after endoscopic resection versus surgery in early gastric cancers. Endoscopy. 2015;47:293–301. doi: 10.1055/s-0034-1391284. [DOI] [PubMed] [Google Scholar]
- 101.Takemoto T, Yanai H, Tada M, et al. Application of ultrasonic probes prior to endoscopic resection of early gastric cancer. Endoscopy. 1992;24(Suppl 1):329–33. doi: 10.1055/s-2007-1010493. [DOI] [PubMed] [Google Scholar]
- 102.Choi J, Kim SG, Im JP, et al. Is endoscopic ultrasonography indispensable in patients with early gastric cancer prior to endoscopic resection? Surg Endosc. 2010;24:3177–85. doi: 10.1007/s00464-010-1112-0. [DOI] [PubMed] [Google Scholar]
- 103.Kim J, Kim SG, Chung H, et al. Clinical efficacy of endoscopic ultrasonography for decision of treatment strategy of gastric cancer. Surg Endosc. 2018;32:3789–97. doi: 10.1007/s00464-018-6104-5. [DOI] [PubMed] [Google Scholar]
- 104.Nagahama T, Yao K, Imamura K, et al. Diagnostic performance of conventional endoscopy in the identification of submucosal invasion by early gastric cancer: The “non-extension sign” as a simple diagnostic marker. Gastric Cancer. 2017;20:304–13. doi: 10.1007/s10120-016-0612-6. [DOI] [PubMed] [Google Scholar]
- 105.Yanai H, Matsumoto Y, Harada T, et al. Endoscopic ultrasonography and endoscopy for staging depth of invasion in early gastric cancer: A pilot study. Gastrointest Endosc. 1997;46:212–6. doi: 10.1016/s0016-5107(97)70088-9. [DOI] [PubMed] [Google Scholar]
- 106.Yasuda K. Endoscopic ultrasonic probes and mucosectomy for early gastric carcinoma. Gastrointest Endosc. 1996;43:S29–31. doi: 10.1016/s0016-5107(96)81511-2. [DOI] [PubMed] [Google Scholar]
- 107.Akahoshi K, Chijiwa Y, Hamada S, et al. Pretreatment staging of endoscopically early gastric cancer with a 15 MHz ultrasound catheter probe. Gastrointest Endosc. 1998;48:470–6. doi: 10.1016/s0016-5107(98)70087-2. [DOI] [PubMed] [Google Scholar]
- 108.Yanai H, Noguchi T, Mizumachi S, et al. A blind comparison of the effectiveness of endoscopic ultrasonography and endoscopy in staging early gastric cancer. Gut. 1999;44:361–5. doi: 10.1136/gut.44.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim JH, Song KS, Youn YH, et al. Clinicopathologic factors influence accurate endosonographic assessment for early gastric cancer. Gastrointest Endosc. 2007;66:901–8. doi: 10.1016/j.gie.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 110.Kim GH, Park DY, Kida M, et al. Accuracy of high-frequency catheter-based endoscopic ultrasonography according to the indications for endoscopic treatment of early gastric cancer. J Gastroenterol Hepatol. 2010;25:506–11. doi: 10.1111/j.1440-1746.2009.06111.x. [DOI] [PubMed] [Google Scholar]
- 111.Mouri R, Yoshida S, Tanaka S, et al. Usefulness of endoscopic ultrasonography in determining the depth of invasion and indication for endoscopic treatment of early gastric cancer. J Clin Gastroenterol. 2009;43:318–22. doi: 10.1097/MCG.0b013e3181775966. [DOI] [PubMed] [Google Scholar]
- 112.Choi J, Kim SG, Im JP, et al. Comparison of endoscopic ultrasonography and conventional endoscopy for prediction of depth of tumor invasion in early gastric cancer. Endoscopy. 2010;42:705–13. doi: 10.1055/s-0030-1255617. [DOI] [PubMed] [Google Scholar]
- 113.Okada K, Fujisaki J, Kasuga A, et al. Endoscopic ultrasonography is valuable for identifying early gastric cancers meeting expanded-indication criteria for endoscopic submucosal dissection. Surg Endosc. 2011;25:841–8. doi: 10.1007/s00464-010-1279-4. [DOI] [PubMed] [Google Scholar]
- 114.Yamamoto S, Nishida T, Kato M, et al. Evaluation of endoscopic ultrasound image quality is necessary in endosonographic assessment of early gastric cancer invasion depth. Gastroenterol Res Pract. 2012;2012:194530. doi: 10.1155/2012/194530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lee HH, Lim CH, Park JM, et al. Low accuracy of endoscopic ultrasonography for detailed T staging in gastric cancer. World J Surg Oncol. 2012;10:190. doi: 10.1186/1477-7819-10-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Mandai K, Yasuda K. Accuracy of endoscopic ultrasonography for determining the treatment method for early gastric cancer. Gastroenterol Res Pract. 2012;2012:245390. doi: 10.1155/2012/245390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Okamura S, Tsutsui A, Muguruma N, et al. The utility and limitations of an ultrasonic miniprobe in the staging of gastric cancer. J Med Invest. 1999;46:49–53. [PubMed] [Google Scholar]
- 118.Seifert H, Schütte A. Miniprobe EUS. Z Gastroenterol. 2008;46:909–16. doi: 10.1055/s-2008-1027569. [DOI] [PubMed] [Google Scholar]
- 119.Matsumoto Y, Yanai H, Tokiyama H, et al. Endoscopic ultrasonography for diagnosis of submucosal invasion in early gastric cancer. J Gastroenterol. 2000;35:326–31. doi: 10.1007/s005350050356. [DOI] [PubMed] [Google Scholar]
- 120.Sano T, Okuyama Y, Kobori O, et al. Early gastric cancer.Endoscopic diagnosis of depth of invasion. Dig Dis Sci. 1990;35:1340–4. doi: 10.1007/BF01536738. [DOI] [PubMed] [Google Scholar]
- 121.Yoshinaga S, Hilmi IN, Kwek BE, et al. Current status of endoscopic ultrasound for the upper gastrointestinal tract in Asia. Dig Endosc. 2015;27(Suppl 1):2–10. doi: 10.1111/den.12422. [DOI] [PubMed] [Google Scholar]
- 122.Tsuzuki T, Okada H, Kawahara Y, et al. Usefulness and problems of endoscopic ultrasonography in prediction of the depth of tumor invasion in early gastric cancer. Acta Med Okayama. 2011;65:105–12. doi: 10.18926/AMO/45269. [DOI] [PubMed] [Google Scholar]
- 123.Jung JI, Kim GH, IH, et al. Clinicopathologic factors influencing the accuracy of EUS for superficial esophageal carcinoma. World J Gastroenterol. 2014;20:6322–8. doi: 10.3748/wjg.v20.i20.6322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yanai H, Tada M, Karita M, et al. Diagnostic utility of 20-megahertz linear endoscopic ultrasonography in early gastric cancer. Gastrointest Endosc. 1996;44:29–33. doi: 10.1016/s0016-5107(96)70225-0. [DOI] [PubMed] [Google Scholar]
- 125.Ichikawa T, Kudo M, Matsui S, et al. Endoscopic ultrasonography with three miniature probes of different frequency is an accurate diagnostic tool for endoscopic submucosal dissection. Hepatogastroenterology. 2007;54:325–8. [PubMed] [Google Scholar]
- 126.Yasuda K, Kamaguchi M, Morikawa J, et al. Role of endoscopic ultrasonography in the diagnosis of early esophageal carcinoma. Gastrointest Endosc Clin N Am. 2005;15:93–9. doi: 10.1016/j.giec.2004.07.015. ix. [DOI] [PubMed] [Google Scholar]
- 127.Sabet EA, Okai T, Minamoto T, et al. Visualizing the gastric wall with a 30-MHz ultrasonic miniprobe: Ex vivo imaging of normal gastric sites and sites of early gastric cancer. Abdom Imaging. 2003;28:252–6. doi: 10.1007/s00261-002-0035-1. [DOI] [PubMed] [Google Scholar]
- 128.Mocellin S, Pasquali S. Diagnostic accuracy of endoscopic ultrasonography (EUS) for the preoperative locoregional staging of primary gastric cancer. Cochrane Database Syst Rev. 2015;2:CD009944. doi: 10.1002/14651858.CD009944.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Pei Q, Wang L, Pan J, et al. Endoscopic ultrasonography for staging depth of invasion in early gastric cancer: A meta-analysis. J Gastroenterol Hepatol. 2015;30:1566–73. doi: 10.1111/jgh.13014. [DOI] [PubMed] [Google Scholar]
- 130.Hünerbein M, Handke T, Ulmer C, et al. Impact of miniprobe ultrasonography on planning of minimally invasive surgery for gastric and colonic tumors. Surg Endosc. 2004;18:601–5. doi: 10.1007/s00464-003-8925-z. [DOI] [PubMed] [Google Scholar]
- 131.Park JS, Kim H, Bang B, et al. Accuracy of endoscopic ultrasonography for diagnosing ulcerative early gastric cancers. Medicine (Baltimore) 2016;95:e3955. doi: 10.1097/MD.0000000000003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sunagawa H, Kinoshita T, Kaito A, et al. Additional surgery for non-curative resection after endoscopic submucosal dissection for gastric cancer: A retrospective analysis of 200 cases. Surg Today. 2017;47:202–9. doi: 10.1007/s00595-016-1353-1. [DOI] [PubMed] [Google Scholar]
- 133.Chen J, Zhou C, He M, et al. A meta-analysis and systematic review of accuracy of endoscopic ultrasound for N staging of gastric cancers. Cancer Manag Res. 2019;11:8755–64. doi: 10.2147/CMAR.S200318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hatta W, Gotoda T, Oyama T, et al. A scoring system to stratify curability after endoscopic submucosal dissection for early gastric cancer: “eCura system”. Am J Gastroenterol. 2017;112:874–81. doi: 10.1038/ajg.2017.95. [DOI] [PubMed] [Google Scholar]
- 135.Tanabe S, Ishido K, Matsumoto T, et al. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: A multicenter collaborative study. Gastric Cancer. 2017;20:45–52. doi: 10.1007/s10120-016-0664-7. [DOI] [PubMed] [Google Scholar]
- 136.Kim SM, Min BH, Ahn JH, et al. Nomogram to predict lymph node metastasis in patients with early gastric cancer: A useful clinical tool to reduce gastrectomy after endoscopic resection. Endoscopy. 2020;52:435–43. doi: 10.1055/a-1117-3059. [DOI] [PubMed] [Google Scholar]
- 137.Mayanagi S, Takahashi N, Mitsumori N, et al. Sentinel node mapping for post-endoscopic resection gastric cancer: Multicenter retrospective cohort study in Japan. Gastric Cancer. 2020;23:716–24. doi: 10.1007/s10120-019-01038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wei J, Bu Z. Sentinel lymph node detection for gastric cancer: Promise or pitfall? Surg Oncol. 2020;33:1–6. doi: 10.1016/j.suronc.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 139.Nie RC, Yuan SQ, Chen XJ, et al. Endoscopic ultrasonography compared with multidetector computed tomography for the preoperative staging of gastric cancer: A meta-analysis. World J Surg Oncol. 2017;15:113. doi: 10.1186/s12957-017-1176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Renzulli M, Clemente A, Spinelli D, et al. Gastric cancer staging: Is it time for magnetic resonance imaging? Cancers (Basel) 2020;12:1402. doi: 10.3390/cancers12061402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Tavares A, Wen X, Maciel J, et al. Occult tumour cells in lymph nodes from gastric cancer patients: Should isolated tumour cells also be considered? Ann Surg Oncol. 2020;27:4204–15. doi: 10.1245/s10434-020-08524-4. [DOI] [PubMed] [Google Scholar]
- 142.Sano Y, Tanaka S, Kudo SE, et al. Narrow-band imaging (NBI) magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI Expert Team. Dig Endosc. 2016;28:526–33. doi: 10.1111/den.12644. [DOI] [PubMed] [Google Scholar]
- 143.Minoda Y, Ogino H, Chinen T, et al. Objective validity of the Japan Narrow-Band Imaging Expert Team classification system for the differential diagnosis of colorectal polyps. Dig Endosc. 2019;31:544–51. doi: 10.1111/den.13393. [DOI] [PubMed] [Google Scholar]
- 144.Puig I, López-Cerón M, Arnau A, et al. Accuracy of the narrow-band imaging international colorectal endoscopic classification system in identification of deep invasion in colorectal polyps. Gastroenterology. 2019;156:75–87. doi: 10.1053/j.gastro.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 145.Lee BI, Matsuda T. Estimation of invasion depth: The first key to successful colorectal ESD. Clin Endosc. 2019;52:100–6. doi: 10.5946/ce.2019.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hurlstone DP, Brown S, Cross SS, et al. Endoscopic ultrasound miniprobe staging of colorectal cancer: Can management be modified? Endoscopy. 2005;37:710–4. doi: 10.1055/s-2005-870142. [DOI] [PubMed] [Google Scholar]
- 147.Gall TM, Markar SR, Jackson D, et al. Mini-probe ultrasonography for the staging of colon cancer: A systematic review and meta-analysis. Colorectal Dis. 2014;16:O1–8. doi: 10.1111/codi.12445. [DOI] [PubMed] [Google Scholar]
- 148.Emmanuel A, Lapa C, Ghosh A, et al. Multimodal endoscopic assessment guides treatment decisions for rectal early neoplastic tumors. Dis Colon Rectum. 2020;63:326–35. doi: 10.1097/DCR.0000000000001587. [DOI] [PubMed] [Google Scholar]
- 149.Tanaka S, Kashida H, Saito Y, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015;27:417–34. doi: 10.1111/den.12456. [DOI] [PubMed] [Google Scholar]
- 150.Tanaka S, Kashida H, Saito Y, et al. Japan Gastroenterological Endoscopy Society guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2020;32:219–39. doi: 10.1111/den.13545. [DOI] [PubMed] [Google Scholar]
- 151.Wiech T, Walch A, Werner M. Histopathological classification of nonneoplastic and neoplastic gastrointestinal submucosal lesions. Endoscopy. 2005;37:630–4. doi: 10.1055/s-2005-870127. [DOI] [PubMed] [Google Scholar]
- 152.Nishida T, Kawai N, Yamaguchi S, et al. Submucosal tumors: Comprehensive guide for the diagnosis and therapy of gastrointestinal submucosal tumors. Dig Endosc. 2013;25:479–89. doi: 10.1111/den.12149. [DOI] [PubMed] [Google Scholar]
- 153.Nishida T, Holmebakk T, Raut CP, et al. Defining tumor rupture in gastrointestinal stromal tumor. Ann Surg Oncol. 2019;26:1669–75. doi: 10.1245/s10434-019-07297-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Vanek J. Gastric submucosal granuloma with eosinophilic infiltration. Am J Pathol. 1949;25:397–411. [PMC free article] [PubMed] [Google Scholar]
- 155.Park HC, Son DJ, Oh HH, et al. Endoscopic ultrasonographic characteristics of gastric schwannoma distinguished from gastrointestinal stromal tumor. Korean J Gastroenterol. 2015;65:21–6. doi: 10.4166/kjg.2015.65.1.21. [DOI] [PubMed] [Google Scholar]
- 156.Lim TW, Choi CW, Kang DH, et al. Endoscopic ultrasound without tissue acquisition has poor accuracy for diagnosing gastric subepithelial tumors. Medicine (Baltimore) 2016;95:e5246. doi: 10.1097/MD.0000000000005246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Khan S, Zhang R, Fang W, et al. Reliability of endoscopic ultrasound using miniprobes and grayscale histogram analysis in diagnosing upper gastrointestinal subepithelial lesions. Gastroenterol Res Pract. 2020;2020:6591341. doi: 10.1155/2020/6591341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gottschalk U, Dietrich CF, Jenssen C. Ectopic pancreas in the upper gastrointestinal tract: Is endosonographic diagnosis reliable.Data from the German Endoscopic Ultrasound Registry and review of the literature? Endosc Ultrasound. 2018;7:270–8. doi: 10.4103/eus.eus_18_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Moon JS. Endoscopic ultrasound-guided fine needle aspiration in submucosal lesion. Clin Endosc. 2012;45:117–23. doi: 10.5946/ce.2012.45.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Salah W, Faigel DO. When to puncture, when not to puncture: Submucosal tumors. Endosc Ultrasound. 2014;3:98–108. doi: 10.4103/2303-9027.131038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Rana A, Rana SS. Endoscopic ultrasound-guided tissue acquisition: Techniques and challenges. J Cytol. 2019;36:1–7. doi: 10.4103/JOC.JOC_146_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.de la Serna-Higuera C, Pérez-Miranda M, Díez-Redondo P, et al. EUS-guided single-incision needle-knife biopsy: Description and results of a new method for tissue sampling of subepithelial GI tumors (with video) Gastrointest Endosc. 2011;74:672–6. doi: 10.1016/j.gie.2011.05.042. [DOI] [PubMed] [Google Scholar]
- 163.Antonini F, Delconte G, Fuccio L, et al. EUS-guided tissue sampling with a 20-gauge core biopsy needle for the characterization of gastrointestinal subepithelial lesions: A multicenter study. Endosc Ultrasound. 2019;8:105–10. doi: 10.4103/eus.eus_1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Akahoshi K, Sumida Y, Matsui N, et al. Preoperative diagnosis of gastrointestinal stromal tumor by endoscopic ultrasound-guided fine needle aspiration. World J Gastroenterol. 2007;13:2077–82. doi: 10.3748/wjg.v13.i14.2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Mekky MA, Yamao K, Sawaki A, et al. Diagnostic utility of EUS-guided FNA in patients with gastric submucosal tumors. Gastrointest Endosc. 2010;71:913–9. doi: 10.1016/j.gie.2009.11.044. [DOI] [PubMed] [Google Scholar]
- 166.Lee HL. Advances in the management of upper gastrointestinal subepithelial tumor: Pathologic diagnosis using endoscopy without endoscopic ultrasound-guided biopsy. Clin Endosc. 2016;49:216–9. doi: 10.5946/ce.2016.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Dhaliwal A, Kolli S, Dhindsa BS, et al. Diagnostic yield of deep biopsy via endoscopic submucosal dissection for the diagnosis of upper gastrointestinal subepithelial tumors: A systematic review and meta-analysis. Ann Gastroenterol. 2020;33:30–7. doi: 10.20524/aog.2019.0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Akahoshi K, Oya M, Koga T, et al. Current clinical management of gastrointestinal stromal tumor. World J Gastroenterol. 2018;24:2806–17. doi: 10.3748/wjg.v24.i26.2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Søreide K, Sandvik OM, Søreide JA, et al. Global epidemiology of gastrointestinal stromal tumours (GIST): A systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39–46. doi: 10.1016/j.canep.2015.10.031. [DOI] [PubMed] [Google Scholar]
- 170.Liu X, Qiu H, Zhang P, et al. Prognostic factors of primary gastrointestinal stromal tumors: A cohort study based on high-volume centers. Chin J Cancer Res. 2018;30:61–71. doi: 10.21147/j.issn.1000-9604.2018.01.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Agaimy A, Wünsch PH, Hofstaedter F, et al. Minute gastric sclerosing stromal tumors (GIST tumorlets) are common in adults and frequently show c-KIT mutations. Am J Surg Pathol. 2007;31:113–20. doi: 10.1097/01.pas.0000213307.05811.f0. [DOI] [PubMed] [Google Scholar]
- 172.Kawanowa K, Sakuma Y, Sakurai S, et al. High incidence of microscopic gastrointestinal stromal tumors in the stomach. Hum Pathol. 2006;37:1527–35. doi: 10.1016/j.humpath.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 173.Zhu L, Khan S, Hui Y, et al. Treatment recommendations for small gastric gastrointestinal stromal tumors: Positive endoscopic resection. Scand J Gastroenterol. 2019;54:297–302. doi: 10.1080/00365521.2019.1578405. [DOI] [PubMed] [Google Scholar]
- 174.Landi B, Blay JY, Bonvalot S, et al. Gastrointestinal stromal tumours (GISTs): French Intergroup Clinical Practice Guidelines for diagnosis, treatments and follow-up (SNFGE, FFCD, GERCOR, UNICANCER, SFCD, SFED, SFRO) Dig Liver Dis. 2019;51:1223–31. doi: 10.1016/j.dld.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 175.von Mehren M, Randall RL, Benjamin RS, et al. Soft Tissue Sarcoma, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2018;16:536–63. doi: 10.6004/jnccn.2018.0025. [DOI] [PubMed] [Google Scholar]
- 176.Palazzo L, Landi B, Cellier C, et al. Endosonographic features predictive of benign and malignant gastrointestinal stromal cell tumours. Gut. 2000;46:88–92. doi: 10.1136/gut.46.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.von Mehren M, Kane JM, Bui MM. NCCN Guidelines Insights: SoftTissue Sarcoma, Version 1.2021. J Nat1 Copr Canc Netw. 2020;18:1604–12. doi: 10.6004/jnccn.2020.0058. [DOI] [PubMed] [Google Scholar]
- 178.Feng X, Yang Z, Zhang P, et al. Which size is the best cutoff for primary small gastric gastrointestinal stromal tumor? J Gastrointest Oncol. 2020;11:402–10. doi: 10.21037/jgo.2020.03.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Judson I, Bulusu R, Seddon B, et al. UK clinical practice guidelines for the management of gastrointestinal stromal tumours (GIST) Clin Sarcoma Res. 2017;7:6. doi: 10.1186/s13569-017-0072-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Casali PG, Abecassis N, Aro HT, et al. Gastrointestinal stromal tumours: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29:iv267. doi: 10.1093/annonc/mdy320. [DOI] [PubMed] [Google Scholar]
- 181.Koo DH, Ryu MH, Kim KM, et al. Asian consensus guidelines for the diagnosis and management of gastrointestinal stromal tumor. Cancer Res Treat. 2016;48:1155–66. doi: 10.4143/crt.2016.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Nakajima T, Ushijima T, Kihara A, et al. A gastrointestinal stromal tumor of the stomach demonstrating a stepwise progression from low- to high-grade malignancy. Case Rep Gastrointest Med. 2012;2012:606832. doi: 10.1155/2012/606832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Yang J, Feng F, Li M, et al. Surgical resection should be taken into consideration for the treatment of small gastric gastrointestinal stromal tumors. World J Surg Oncol. 2013;11:273. doi: 10.1186/1477-7819-11-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Gao Z, Wang C, Xue Q, et al. The cut-off value of tumor size and appropriate timing of follow-up for management of minimal EUS-suspected gastric gastrointestinal stromal tumors. BMC Gastroenterol. 2017;17:8. doi: 10.1186/s12876-016-0567-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Dumonceau JM, Polkowski M, Larghi A, et al. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2011;43:897–912. doi: 10.1055/s-0030-1256754. [DOI] [PubMed] [Google Scholar]
- 186.Li J, Ye Y, Wang J, et al. Chinese consensus guidelines for diagnosis and management of gastrointestinal stromal tumor. Chin J Cancer Res. 2017;29:281–93. doi: 10.21147/j.issn.1000-9604.2017.04.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Tu L, Hohenberger P, Allgayer H, et al. Standard approach to gastrointestinal stromal tumors-Differences between China and Europe. Visc Med. 2018;34:353–8. doi: 10.1159/000494347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Jenssen C, Barreiros AP, Will U, et al. German survey on EUS-guided diagnosis and management of gastrointestinal stromal tumors (GISTs)-Evidence or “Gut-Feeling”? Ultraschall Med. 2015;36:494–500. doi: 10.1055/s-0034-1398970. [DOI] [PubMed] [Google Scholar]
- 189.Eckardt AJ, Adler A, Gomes EM, et al. Endosonographic large-bore biopsy of gastric subepithelial tumors: A prospective multicenter study. Eur J Gastroenterol Hepatol. 2012;24:1135–44. doi: 10.1097/MEG.0b013e328356eae2. [DOI] [PubMed] [Google Scholar]
- 190.Akahoshi K, Oya M, Koga T, et al. Clinical usefulness of endoscopic ultrasound-guided fine needle aspiration for gastric subepithelial lesions smaller than 2 cm. J Gastrointestin Liver Dis. 2014;23:405–12. doi: 10.15403/jgld.2014.1121.234.eug. [DOI] [PubMed] [Google Scholar]
- 191.Nishida T, Blay JY, Hirota S, et al. The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer. 2016;19:3–14. doi: 10.1007/s10120-015-0526-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Furuzono S, Ohya S, Inoue S, et al. Inherent pacemaker function of duodenal GIST. Eur J Cancer. 2006;42:243–8. doi: 10.1016/j.ejca.2005.09.024. [DOI] [PubMed] [Google Scholar]
- 193.Kothari MS, Kosmoliaptsis V, Meyrick-Thomas J. Small bowel Gastrointestinal Stromal Tumors can physiologically alter gut motility before causing mechanical obstruction. Int Semin Surg Oncol. 2005;2:24. doi: 10.1186/1477-7800-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Yu QX, He ZK, Wang J, et al. Clinical presentations of gastric small gastrointestinal stromal tumors mimics functional dyspepsia symptoms. World J Gastroenterol. 2014;20:11800–7. doi: 10.3748/wjg.v20.i33.11800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Pang T, Zhao Y, Fan T, et al. Comparison of safety and outcomes between endoscopic and surgical resections of small (≤5 cm) primary gastric gastrointestinal stromal tumors. J Cancer. 2019;10:4132–41. doi: 10.7150/jca.29443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wang C, Gao Z, Shen K, et al. Safety and efficiency of endoscopic resection versus laparoscopic resection in gastric gastrointestinal stromal tumours: A systematic review and meta-analysis. Eur J Surg Oncol. 2020;46:667–74. doi: 10.1016/j.ejso.2019.10.030. [DOI] [PubMed] [Google Scholar]
- 197.Joo MK, Park JJ, Kim H, et al. Endoscopic versus surgical resection of GI stromal tumors in the upper GI tract. Gastrointest Endosc. 2016;83:318–26. doi: 10.1016/j.gie.2015.07.034. [DOI] [PubMed] [Google Scholar]
- 198.Tian X, Shi B, Chen WQ. Modified endoscopic full-thickness resection of gastric stromal tumor originating from the muscularis propria layer. J Gastrointest Oncol. 2020;11:461–6. doi: 10.21037/jgo.2020.03.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Meier B, Schmidt A, Glaser N, et al. Endoscopic full-thickness resection of gastric subepithelial tumors with the gFTRD-system: A prospective pilot study (RESET trial) Surg Endosc. 2020;34:853–60. doi: 10.1007/s00464-019-06839-2. [DOI] [PubMed] [Google Scholar]
- 200.Jiao R, Zhao S, Jiang W, et al. Endoscopic submucosal dissection of gastrointestinal stromal tumours: A retrospective cohort study. Cancer Manag Res. 2020;12:4055–61. doi: 10.2147/CMAR.S252459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Guo W, Yang Z, Wei Y, et al. Radical excision versus local resection for primary rectal gastrointestinal stromal tumors.Cohort study. Int J Surg. 2020;77:190–7. doi: 10.1016/j.ijsu.2020.03.068. [DOI] [PubMed] [Google Scholar]
- 202.Zheng XJ, Liu Y, Zhu JQ, et al. Submucosal tunneling endoscopic resection for submucosal tumors originating from muscularis propria layer at esophagogastric junction. Zhonghua Zhong Liu Za Zhi. 2019;41:129–34. doi: 10.3760/cma.j.issn.0253-3766.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 203.Zhang X, Modayil R, Criscitelli T, et al. Endoscopic resection for subepithelial lesions-pure endoscopic full-thickness resection and submucosal tunneling endoscopic resection. Transl Gastroenterol Hepatol. 2019;4:39. doi: 10.21037/tgh.2019.05.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Zhao Y, Pang T, Zhang B, et al. Retrospective comparison of endoscopic full-thickness versus laparoscopic or surgical resection of small (≤5 cm) gastric gastrointestinal stromal tumors. J Gastrointest Surg. 2020;24:2714–21. doi: 10.1007/s11605-019-04493-6. [DOI] [PubMed] [Google Scholar]
- 205.ASGE Technology Committee. Aslanian HR, Sethi A, et al. ASGE guideline for endoscopic full-thickness resection and submucosal tunnel endoscopic resection. VideoGIE. 2019;4:343–50. doi: 10.1016/j.vgie.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wang M, Xue A, Yuan W, et al. Clinicopathological features and prognosis of small gastric gastrointestinal stromal tumors (GISTs) J Gastrointest Surg. 2019;23:2136–43. doi: 10.1007/s11605-018-04070-3. [DOI] [PubMed] [Google Scholar]
- 207.Wang H, Tan Y, Huo J, Liu D. Submucosal 1-tunnel endoscopic resection for treating upper gastrointestinal multiple submucosal tumor originating from the muscularis propria layer: A report of 12 cases. Medicine (Baltimore) 2019;98:e14484. doi: 10.1097/MD.0000000000014484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Ignee A, Jenssen C, Hocke M, et al. Contrast-enhanced (endoscopic) ultrasound and endoscopic ultrasound elastography in gastrointestinal stromal tumors. Endosc Ultrasound. 2017;6:55–60. doi: 10.4103/2303-9027.200216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Pesenti C, Bories E, Caillol F, et al. Characterization of subepithelial lesions of the stomach and esophagus by contrast-enhanced EUS: A retrospective study. Endosc Ultrasound. 2019;8:43–9. doi: 10.4103/eus.eus_89_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Chhoda A, Jain D, Surabhi VR, et al. Contrast enhanced harmonic endoscopic ultrasound: A novel approach for diagnosis and management of gastrointestinal stromal tumors. Clin Endosc. 2018;51:215–21. doi: 10.5946/ce.2017.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Yang YT, Shen N, Ao F, et al. Diagnostic value of contrast-enhanced harmonic endoscopic ultrasonography in predicting the malignancy potential of submucosal tumors: A systematic review and meta-analysis. Surg Endosc. 2020;34:3754–65. doi: 10.1007/s00464-020-07585-6. [DOI] [PubMed] [Google Scholar]
- 212.Rana SS, Sharma R, Kishore K, et al. High-frequency miniprobe endoscopic ultrasonography in the management of benign esophageal strictures. Ann Gastroenterol. 2020;33:25–9. doi: 10.20524/aog.2019.0436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Li SW, Tseng PH, Chen CC, et al. Muscular thickness of lower esophageal sphincter and therapeutic outcomes in achalasia: A prospective study using high-frequency endoscopic ultrasound. J Gastroenterol Hepatol. 2018;33:240–8. doi: 10.1111/jgh.13816. [DOI] [PubMed] [Google Scholar]
- 214.Kamijo Y, Kondo I, Kokuto M, et al. Miniprobe ultrasonography for determining prognosis in corrosive esophagitis. Am J Gastroenterol. 2004;99:851–4. doi: 10.1111/j.1572-0241.2004.30217.x. [DOI] [PubMed] [Google Scholar]
- 215.Furukawa T, Naitoh Y, Tsukamoto Y, et al. New technique using intraductal ultrasonography for the diagnosis of diseases of the pancreatobiliary system. J Ultrasound Med. 1992;11:607–12. doi: 10.7863/jum.1992.11.11.607. [DOI] [PubMed] [Google Scholar]
- 216.Menzel J, Foerster EC, Ubrig B, et al. Ex vivo examination of the pancreas by intraductal ultrasonography (IDUS) Endoscopy. 1993;25:571–6. doi: 10.1055/s-2007-1010407. [DOI] [PubMed] [Google Scholar]
- 217.Furukawa T, Tsukamoto Y, Naitoh Y, et al. Differential diagnosis between benign and malignant localized stenosis of the main pancreatic duct by intraductal ultrasound of the pancreas. Am J Gastroenterol. 1994;89:2038–41. [PubMed] [Google Scholar]
- 218.Menzel J, Foerster EC, Domschke W. Adenoma of the papilla of Vater: A possible role for intraductal ultrasound (IDUS) Z Gastroenterol. 1995;33:539–42. [PubMed] [Google Scholar]
- 219.Tamada K, Ido K, Ueno N, et al. Assessment of hepatic artery invasion by bile duct cancer using intraductal ultrasonography. Endoscopy. 1995;27:579–83. doi: 10.1055/s-2007-1005761. [DOI] [PubMed] [Google Scholar]
- 220.Tamada K, Kanai N, Ueno N, et al. Limitations of intraductal ultrasonography in differentiating between bile duct cancer in stage T1 and stage T2: In-vitro and in-vivo studies. Endoscopy. 1997;29:721–5. doi: 10.1055/s-2007-1004296. [DOI] [PubMed] [Google Scholar]
- 221.Tamada K, Nagai H, Yasuda Y, et al. Transpapillary intraductal US prior to biliary drainage in the assessment of longitudinal spread of extrahepatic bile duct carcinoma. Gastrointest Endosc. 2001;53:300–7. doi: 10.1016/s0016-5107(01)70402-6. [DOI] [PubMed] [Google Scholar]
- 222.Tamada K, Ohashi A, Tomiyama T, et al. Comparison of intraductal ultrasonography with percutaneous transhepatic cholangioscopy for the identification of residual bile duct stones during lithotripsy. J Gastroenterol Hepatol. 2001;16:100–3. doi: 10.1046/j.1440-1746.2001.02384.x. [DOI] [PubMed] [Google Scholar]
- 223.Tamada K, Satoh Y, Tomiyama T, et al. Multiple bile duct biopsies using a sheath with a side port: Usefulness of intraductal sonography. AJR Am J Roentgenol. 2001;176:797–802. doi: 10.2214/ajr.176.3.1760797. [DOI] [PubMed] [Google Scholar]
- 224.Tamada K, Tomiyama T, Ohashi A, et al. Preoperative assessment of extrahepatic bile duct carcinoma using three-dimensional intraductal US. Gastrointest Endosc. 1999;50:548–54. doi: 10.1016/s0016-5107(99)70082-9. [DOI] [PubMed] [Google Scholar]
- 225.Tamada K, Ueno N, Tomiyama T, et al. Characterization of biliary strictures using intraductal ultrasonography: Comparison with percutaneous cholangioscopic biopsy. Gastrointest Endosc. 1998;47:341–9. doi: 10.1016/s0016-5107(98)70216-0. [DOI] [PubMed] [Google Scholar]
- 226.Tamada K, Ido K, Ueno N, et al. Assessment of portal vein invasion by bile duct cancer using intraductal ultrasonography. Endoscopy. 1995;27:573–8. doi: 10.1055/s-2007-1005760. [DOI] [PubMed] [Google Scholar]
- 227.Tamada K, Ido K, Ueno N, et al. Preoperative staging of extrahepatic bile duct cancer with intraductal ultrasonography. Am J Gastroenterol. 1995;90:239–46. [PubMed] [Google Scholar]
- 228.Tamada K, Yasuda Y, Tomiyama T, et al. Preoperative assessment of congenital bile duct dilatation using intraductal US. Gastrointest Endosc. 1999;49:488–92. doi: 10.1016/s0016-5107(99)70048-9. [DOI] [PubMed] [Google Scholar]
- 229.Heinzow HS, Kammerer S, Rammes C, et al. Comparative analysis of ERCP, IDUS, EUS and CT in predicting malignant bile duct strictures. World J Gastroenterol. 2014;20:10495–503. doi: 10.3748/wjg.v20.i30.10495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Krishna NB, Saripalli S, Safdar R, et al. Intraductal US in evaluation of biliary strictures without a mass lesion on CT scan or magnetic resonance imaging: Significance of focal wall thickening and extrinsic compression at the stricture site. Gastrointest Endosc. 2007;66:90–6. doi: 10.1016/j.gie.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 231.Chen L, Lu Y, Wu JC, et al. Diagnostic Utility of Endoscopic Retrograde Cholangiography/Intraductal Ultrasound (ERC/IDUS) in distinguishing malignant from benign bile duct obstruction. Dig Dis Sci. 2016;61:610–7. doi: 10.1007/s10620-015-3896-1. [DOI] [PubMed] [Google Scholar]
- 232.Ito Y, Shibutani S, Egawa T, et al. Utility of intraductal ultrasonography as a diagnostic tool in patients with early distal cholangiocarcinoma. Hepatogastroenterology. 2015;62:782–6. [PubMed] [Google Scholar]
- 233.Khashab MA, Fockens P, Al-Haddad MA. Utility of EUS in patients with indeterminate biliary strictures and suspected extrahepatic cholangiocarcinoma (with videos) Gastrointest Endosc. 2012;76:1024–33. doi: 10.1016/j.gie.2012.04.451. [DOI] [PubMed] [Google Scholar]
- 234.Meister T, Heinzow HS, Woestmeyer C, et al. Intraductal ultrasound substantiates diagnostics of bile duct strictures of uncertain etiology. World J Gastroenterol. 2013;19:874–81. doi: 10.3748/wjg.v19.i6.874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Tamada K, Kanai N, Wada S, et al. Utility and limitations of intraductal ultrasonography in distinguishing longitudinal cancer extension along the bile duct from inflammatory wall thickening. Abdom Imaging. 2001;26:623–31. doi: 10.1007/s002610000208. [DOI] [PubMed] [Google Scholar]
- 236.Tamada K, Yasuda Y, Nagai H, et al. Limitations of three-dimensional intraductal ultrasonography in the assessment of longitudinal spread of extrahepatic bile duct carcinoma. J Gastroenterol. 2000;35:919–23. doi: 10.1007/s005350070006. [DOI] [PubMed] [Google Scholar]
- 237.Menzel J, Poremba C, Dietl KH, et al. Preoperative diagnosis of bile duct strictures—comparison of intraductal ultrasonography with conventional endosonography. Scand J Gastroenterol. 2000;35:77–82. doi: 10.1080/003655200750024579. [DOI] [PubMed] [Google Scholar]
- 238.Seifert H, Wehrmann T, Hilgers R, et al. Catheter probe extraductal EUS reliably detects distal common bile duct abnormalities. Gastrointest Endosc. 2004;60:61–7. doi: 10.1016/s0016-5107(04)01523-8. [DOI] [PubMed] [Google Scholar]
- 239.Wehrmann T, Martchenko K, Riphaus A. Catheter probe extraductal ultrasonography vs.conventional endoscopic ultrasonography for detection of bile duct stones. Endoscopy. 2009;41:133–7. doi: 10.1055/s-0028-1103491. [DOI] [PubMed] [Google Scholar]
- 240.Dietrich C, Gouder S, Braden B, et al. Extraductal ultrasonography (EDUS) in the detection of choledocholithiasis. Gastrointest Endosc. 2002;55:W1532. [Google Scholar]
- 241.Togliani T, Pilati S, Lisotti A, et al. Catheter probe extraductal ultrasound (EDUS) exploration of the common bile duct is safe in elderly patients with suspicion of choledocholithiasis after distal gastrectomy. Abdom Radiol (NY) 2018;43:2987–90. doi: 10.1007/s00261-018-1580-6. [DOI] [PubMed] [Google Scholar]
- 242.Meister T, Heinzow H, Heinecke A, et al. Post-ERCP pancreatitis in 2364 ERCP procedures: Is intraductal ultrasonography another risk factor? Endoscopy. 2011;43:331–6. doi: 10.1055/s-0030-1256194. [DOI] [PubMed] [Google Scholar]
- 243.Yamao K, Okubo K, Sawaka A, et al. Endolumenal ultrasonography in the diagnosis of pancreatic diseases. Abdom Imaging. 2003;28:545–55. doi: 10.1007/s00261-002-0080-9. [DOI] [PubMed] [Google Scholar]
- 244.Ariyama J, Suyama M, Satoh K, et al. Endoscopic ultrasound and intraductal ultrasound in the diagnosis of small pancreatic tumors. Abdom Imaging. 1998;23:380–6. doi: 10.1007/s002619900365. [DOI] [PubMed] [Google Scholar]
- 245.Kobayashi G, Fujita N, Noda Y, et al. Lateral spread along the main pancreatic duct in branch-duct intraductal papillary-mucinous neoplasms of the pancreas: Usefulness of intraductal ultrasonography for its evaluation. Dig Endosc. 2011;23:62–8. doi: 10.1111/j.1443-1661.2010.01063.x. [DOI] [PubMed] [Google Scholar]
- 246.Cheon YK, Cho YD, Jeon SR, et al. Pancreatic resection guided by preoperative intraductal ultrasonography for intraductal papillary mucinous neoplasm. Am J Gastroenterol. 2010;105:1963–9. doi: 10.1038/ajg.2010.169. [DOI] [PubMed] [Google Scholar]
- 247.Furukawa T, Oohashi K, Yamao K, et al. Intraductal ultrasonography of the pancreas: Development and clinical potential. Endoscopy. 1997;29:561–9. doi: 10.1055/s-2007-1004259. [DOI] [PubMed] [Google Scholar]
- 248.Dietrich CF, Jenssen C. Modern ultrasound imaging of pancreatic tumors. Ultrasonography. 2020;39:105–13. doi: 10.14366/usg.19039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Ge N, Brugge WR, Saxena P, et al. An international, multi-institution survey of the use of EUS in the diagnosis of pancreatic cystic lesions. Endosc Ultrasound. 2019;8:418–27. doi: 10.4103/eus.eus_61_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Sãftoiu A, Bhutani MS, Itoi T, et al. Changes in tumor vascularity depicted by contrast-enhanced EUS as a predictor of prognosis and treatment efficacy in patients with unresectable pancreatic cancer (PEACE): A study protocol. Endosc Ultrasound. 2019;8:235–40. doi: 10.4103/eus.eus_16_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Dong Y, Jürgensen C, Puri R, et al. Ultrasound imaging features of isolated pancreatic tuberculosis. Endosc Ultrasound. 2018;7:119–27. doi: 10.4103/2303-9027.210901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Dietrich CF, Sahai AV, D'Onofrio M, et al. Differential diagnosis of small solid pancreatic lesions. Gastrointest Endosc. 2016;84:933–40. doi: 10.1016/j.gie.2016.04.034. [DOI] [PubMed] [Google Scholar]
- 253.Ignee A, Jenssen C, Arcidiacono PG, et al. Endoscopic ultrasound elastography of small solid pancreatic lesions: A multicenter study. Endoscopy. 2018;50:1071–9. doi: 10.1055/a-0588-4941. [DOI] [PubMed] [Google Scholar]
- 254.Hocke M, Braden B, Jenssen C, et al. Present status and perspectives of endosonography 2017 in gastroenterology. Korean J Intern Med. 2018;33:36–63. doi: 10.3904/kjim.2017.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Dong Y, D'Onofrio M, Hocke M, et al. Autoimmune pancreatitis: Imaging features. Endosc Ultrasound. 2018;7:196–203. doi: 10.4103/eus.eus_23_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Dietrich CF, Barr RG, Farrokh A, et al. Strain elastography-How to do it? Ultrasound Int Open. 2017;3:E137–49. doi: 10.1055/s-0043-119412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Dietrich CF, Dong Y, Jenssen C, et al. Serous pancreatic neoplasia, data and review. World J Gastroenterol. 2017;23:5567–78. doi: 10.3748/wjg.v23.i30.5567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Herth FJ, Ernst A, Becker HD. Endobronchial ultrasound-guided transbronchial lung biopsy in solitary pulmonary nodules and peripheral lesions. Eur Respir J. 2002;20:972–4. doi: 10.1183/09031936.02.00032001. [DOI] [PubMed] [Google Scholar]
- 259.Steinfort DP, Khor YH, Manser RL, et al. Radial probe endobronchial ultrasound for the diagnosis of peripheral lung cancer: Systematic review and meta-analysis. Eur Respir J. 2011;37:902–10. doi: 10.1183/09031936.00075310. [DOI] [PubMed] [Google Scholar]
- 260.Eberhardt R, Anantham D, Ernst A, et al. Multimodality bronchoscopic diagnosis of peripheral lung lesions: A randomized controlled trial. Am J Respir Crit Care Med. 2007;176:36–41. doi: 10.1164/rccm.200612-1866OC. [DOI] [PubMed] [Google Scholar]
- 261.Steinfort DP, Bonney A, See K, et al. Sequential multimodality bronchoscopic investigation of peripheral pulmonary lesions. Eur Respir J. 2016;47:607–14. doi: 10.1183/13993003.00786-2015. [DOI] [PubMed] [Google Scholar]
- 262.Herth F, Ernst A, Schulz M, et al. Endobronchial ultrasound reliably differentiates between airway infiltration and compression by tumor. Chest. 2003;123:458–62. doi: 10.1378/chest.123.2.458. [DOI] [PubMed] [Google Scholar]
- 263.Herth F, Becker HD, LoCicero J, 3rd, et al. Endobronchial ultrasound in therapeutic bronchoscopy. Eur Respir J. 2002;20:118–21. doi: 10.1183/09031936.02.01642001. [DOI] [PubMed] [Google Scholar]
- 264.Miyazu Y, Miyazawa T, Kurimoto N, et al. Endobronchial ultrasonography in the assessment of centrally located early-stage lung cancer before photodynamic therapy. Am J Respir Crit Care Med. 2002;165:832–7. doi: 10.1164/ajrccm.165.6.2108092. [DOI] [PubMed] [Google Scholar]
- 265.Ye LP, Mao XL, Zheng HH, et al. Safety of endoscopic resection for duodenal subepithelial lesions with wound closure using clips and an endoloop: An analysis of 68 cases. Surg Endosc. 2017;31:1070–7. doi: 10.1007/s00464-016-5065-9. [DOI] [PubMed] [Google Scholar]
- 266.Shen C, Chen H, Yin Y, et al. Endoscopic versus open resection for small gastric gastrointestinal stromal tumors: Safety and outcomes. Medicine (Baltimore) 2015;94:e376. doi: 10.1097/MD.0000000000000376. [DOI] [PMC free article] [PubMed] [Google Scholar]


