Abstract
Background and Objectives:
EUS-guided biliary drainage (EUS-BD) has recently been used for the treatment of not only malignant pancreaticobiliary diseases, but also for benign diseases. In most previous studies, EUS-BD was performed using a fully covered self-expandable metallic stent (SEMS), and data focusing on the usability of plastic stents for benign diseases are limited. We previously developed a plastic stent dedicated to EUS-guided hepaticoenterostomy (EUS-HES), and achieved favorable results in a feasibility study, although most of the patients had malignant diseases. Therefore, the aim of the present study was to evaluate the usability of dedicated plastic stents for EUS-HES in patients with benign pancreaticobiliary diseases.
Patients and Methods:
A total of 57 consecutive patients (28 men, median age: 68 years; range: 7–90 years) of normal and surgically altered anatomy with benign pancreaticobiliary diseases who underwent EUS-HES using the dedicated plastic stent between Jan. 2015 and Jun. 2020 were retrospectively analyzed.
Results:
The overall technical success rate of EUS-HES was 92.9% (53/57). Among the 4 cases of technical failure of plastic stent placement, a SEMS was placed in 1; percutaneous transhepatic biliary drainage was performed in 1; EUS-HES was reperformed 1 week later in 1; and observational management was selected in 1 patient. Adverse events associated with the procedure were seen in 15.7% (9/57) of the patients, namely, biliary peritonitis in 4, bleeding in 2, cholecystitis in 2, and pneumoperitoneum in 1 patient. Except for 1 patient who required blood transfusion owing to bleeding and 1 patient with cholecystitis who required percutaneous transhepatic gallbladder drainage, the other 7 patients were treated by conservative therapy. There were no intervention-associated deaths.
Conclusion:
Our results demonstrated that for patients with benign pancreaticobiliary diseases in whom conventional ERCP was unsuccessful, EUS-HES using a dedicated plastic stent was safe and feasible.
Keywords: EUS-guided hepaticoenterostomy, EUS-guided hepaticogastrostomy, EUS-guided hepaticojejunostomy, dedicated plastic stent, ERCP, bilioenteric anastomotic stricture, benign biliary stricture, common bile duct stone, intrahepatic bile duct stone, gastric outlet obstruction
INTRODUCTION
ERCP is presently the gold standard technique for biliary drainage. However, ERCP may not be successful in some specific situations, such as inaccessible papilla owing to gastric outlet obstruction (GOO), and surgically altered anatomy (SAA). Recently, EUS-guided biliary drainage (EUS-BD) has received attention as a novel alternative technique when fails ERCP and has been applied not only for malignant diseases but also for benign diseases, such as bilioenteric anastomotic strictures, intrahepatic bile duct (IHBD) stones, and/or common bile duct (CBD) stones, in patients with a SAA in whom balloon enteroscopy-assisted ERCP (BE-ERCP) was unsuccessful and in patients with a normal anatomy in whom conventional ERCP was unsuccessful.[1,2,3,4] We previously demonstrated the feasibility of EUS-guided antegrade intervention for the benign biliary diseases in SAA patients, and it appears to be a feasible and safe alternative procedure after unsuccessful BE-ERCP.[5] In general, a fully covered self-expandable metallic stent (SEMS) is commonly used for EUS-BD in patients with malignant diseases; however, in patients with benign diseases, whether a SEMS or a plastic stent should be used for EUS-BD has remained unclear. As the punctured IHBD is relatively thinner in patients with benign diseases than in those with malignant diseases, there may be a high risk of segmental obstructive cholangitis upon using a SEMS. From the above point, we considered that the use of a dedicated plastic stent is suitable for patients with benign pancreaticobiliary diseases. We previously developed a plastic stent dedicated to EUS-guided hepaticoenterostomy (EUS-HES) and achieved favorable results in a feasibility study, although most of the included patients had malignant diseases.[6] In fact, few studies have focused on the technical aspect and usability of dedicated plastic stents to perform EUS-HES for the creation of a temporal access route in patients with benign pancreaticobiliary diseases, including not only patients with a SAA but also those with a normal anatomy. Therefore, the aim of this study was to evaluate the outcomes of EUS-HES with using a dedicated plastic stent for patients with benign pancreaticobiliary diseases.
PATIENTS AND METHODS
A total of 57 consecutive patients (28 men; median age: 68 years; range: 7–90 years) with benign pancreaticobiliary diseases who underwent an attempt of EUS-HES using a dedicated plastic stent from January 2015 to June 2020 at our institution were retrospectively analyzed, and the clinical data as well as endoscopic procedure data were collected. Clinical data included the underlying disease, indication of EUS-HES, presence of cholangitis, anatomy, clinical success, and procedure-related adverse events (AEs). The size and branch of punctured IHBD, procedure time, type of needle, and dilator were also collected as endoscopic procedure data and compared between EUS-guided hepaticogastrostomy (EUS-HGS) and EUS-guided hepaticojejunostomy (EUS-HJS). General indications of EUS-HES for the benign pancreaticobiliary diseases were the presence of benign biliary stricture (BBS) or anastomotic stricture for which transpapillary or transanastomotic drainage was unsuccessful, IHBD or CBD stones in patients in whom conventional ERCP or BE-ERCP was unsuccessful, and inaccessible papilla owing to benign GOO. The primary outcome was technical success, which was defined as successful plastic stent placement in the IHBD. Secondary outcomes included clinical success and procedure-related AE rate. Generally, clinical success of EUS-HES has been defined as an improvement of jaundice or decrease of bilirubin level in patients with malignant biliary diseases.[7,8] In this study, target patients were those with benign pancreaticobiliary diseases, namely, although most patients had a past history of recurrent cholangitis or jaundice and had been having symptoms intermittently for a long period owing to the stricture or stones, many patients were symptom-free or had mild symptoms of cholangitis or jaundice, at the exact time of the intervention. In addition, many of the patients underwent EUS-HES, not for the drainage purposes, but for the creation of an access route for sequential antegrade intervention. For these reasons, clinical success was defined as being symptom-free or having no recurrence of cholangitis and additional drainage for 2 months after the EUS-HES. The reason for defining 2 months was that most of the patients were re-admitted within 2 months and received the sequential interventions with removal of the placed stent. AEs were graded in accordance with the severity grading system of the American Society for Gastrointestinal Endoscopy Lexicon.[9] The study protocol was approved by the Institutional Review Board of Tokyo Medical University (study approval No.: 4120).
EUS-guided hepaticoenterostomy procedure
All patients were hospitalized, and transverse section imaging, such as computed tomography scan and/or magnetic resonance cholangiopancreatography, was performed to determine the diameter of the IHBD and the patient's anatomy. Serum bilirubin level was measured together with another liver function test 1 day before the procedure. EUS procedures were performed with the patient in the supine position under conscious sedation using pentazocine with flunitrazepam. Prophylactic antibiotics were administered before and after the procedure. A curved linear array echoendoscope (GF-UCT 260, Olympus Medical Systems, Tokyo, Japan) was used under carbon dioxide insufflation. All procedures were performed in a setup comprising at least three physicians who were skilled endosonographers, an assistant with a high level of skill in guidewire manipulation, and another assistant who holds the scope during the procedure. Holding the scope in place and adjusting the EUS monitor so that the guidewire can be seen is important for successfully accomplishing the procedure. The IHBD (B2 or B3) was punctured by using a conventional sharp tip 19G needle (EZ Shot 3 Plus, Olympus Medical Systems, or Sono Tip, Medi-Globe, Tokyo, Japan) under EUS guidance after confirming no intervening vessels using the Doppler mode. In patients with thin IHBD or when the needle angle was not sufficient, a 22G needle was used. In patients with the presence of stomach, needle was punctured via stomach as EUS-HGS. In patients post-total gastrectomy with Roux-en-Y reconstruction (TGRY), the jejunum was punctured using a needle, i.e., EUS-HJS. After performing cholangiography, a 0.025-inch guidewire (VisiGlide 2, Olympus Medical Systems) was inserted into the IHBD. When using a 22G needle, a thinner guidewire was used (0.018-inch NovaGold, Boston Scientific, Natick, MA, USA, or 0.021-inch Metrowire, COOK Medical, Tokyo, Japan). In patients with a thin IHBD, it is difficult to penetrate the IHBD wall by slow puncture, even using a 22G needle, owing to the stiffness of the IHBD wall. In such cases, the IHBD wall was first deeply penetrated by fast puncture, and then, the tip of the needle was slowly pulled back with injecting contrast media into IHBD, such as like “Seldinger technique.” In cases of unsuccessful puncture even using the above technique owing to a thin peripheral IHBD, we used the “two-step puncture technique”.[10] First, the dilated IHBD was identified and punctured, and a sufficient amount of contrast media was injected, even if the position is inappropriate for EUS-HES. After the injection, a more dilated peripheral IHBD can be seen from a suitable position for EUS-HES. After advancing the guidewire sufficiently, tract dilation was performed using mechanical dilator (7-Fr, ES dilator, Zeon Medical, Tokyo, Japan) as a first choice. In the case of use of a 22G needle, after tract dilation using an ES dilator, the 0.018-inch guidewire was exchanged to a 0.025-inch guidewire to safely and reliably perform the subsequent devices exchange and stent insertion. 3-mm diameter of tapered tip balloon dilator (REN; Kaneka Medix Corp., Osaka, Japan), which is specificated to 0.025-inch guidewire, was also added in cases where the angle was tight or the IHBD wall was stiff. If all else fails, electrocautery dilator (6.5 Fr, Endoflex, Voerde, Germany) was used. In patients with anastomotic stricture, when the guidewire was passed through the anastomotic stricture site, anastomotic dilation was also performed by using balloon dilator. The diameter of the balloon dilator was selected according to the degree of stricture. A 6-mm or 8-mm diameter balloon dilator was mainly used for anastomotic stricture dilation. After the anastomotic dilation, the tip of the stent was deployed over the anastomotic stricture site. In patients with unsuccessful to pass the guidewire through the anastomotic stricture site, the tip of stent was deployed in the IHBD.
The EUS-HES–dedicated plastic stent is a single pigtail plastic stent with a total length of 20 cm and an effective length of 15 cm (Through and Pass, TYPE-IT, Gadelius Medical Co. Ltd., Tokyo, Japan) [Figure 1]. In Japan, the 8-Fr push-type stent, 7-Fr push-type stent, and 7-Fr modified consolidated repositionable-type stent are now commercially available. Both types of stents are made of polyethylene. The absence of holes in the middle part of the stent prevents bile juice leakage. Moreover, this stent has a straight and tapered tip and has the improved ability to penetrate the liver wall compared with a conventional standard biliary plastic stents.
Figure 1.
Images of the dedicated plastic stent (7-Fr modified consolidated repositionable-type stent). (a) Straight tip with single pigtail plastic stent; (b) the tip of stent and inner sheath; (c) endoscopic view of placed stent
Statistical analysis
All reported P values are two-sided, and P < 0.05 was considered to indicate a statistically significant difference between two groups. All statistical analyses were performed using SPSS (Version 20; SPSS, Chicago, IL, USA).
RESULTS
Baseline characteristics of the patients as well as the indications for EUS-HES, underlying diseases, and anatomy are summarized in Table 1. The largest number of indications for EUS-HES was unsuccessful BE-ERCP in patients with SAA (n = 44) [Figure 2], followed by primary EUS-HES owing to expected difficulties in the treatment by BE-ERCP in patients with a SAA (n = 7) [Figure 3], inaccessible papilla owing to benign GOO in patients with a normal anatomy (n = 4) [Figure 4], and unsuccessful ERCP in patients with a normal anatomy (n = 2). All seven patients' anatomy of primary EUS-HES was post-hepaticojejunostomy with Roux-en-Y (HJRY) reconstruction. Eight patients of TGRY with CBD stone were performed EUS-HJS [Table 2]. Among the 57 included patients, there were six patients with a normal anatomy [Table 3]. The overall technical outcomes of EUS-HES are shown in Table 4. A plastic stent was successfully deployed in 53 patients, and the technical success was achieved in 92.9% (53/57). The 8-Fr push-type stent was used in 35 patients, the 7-Fr push-type stent in 11 patients, and the 7-Fr consolidated repositionable-type stent in 9 patients, and there were no differences in technical success rates among the different stent types. All four patients of unsuccessful EUS-HES were achieved cholangiogram, although difficult to perform sequential procedures. The reasons of technical failure included that the inability to advance the guidewire owing to the stiff IHBD wall in 1; thin IHBD diameter of 1 mm and unsuccessful to advance the guidewire in 1; inability to place the plastic stent owing to the stiff liver in 1; and bleeding being seen during the procedure in 1. Instead of placing the plastic stent, a SEMS was deployed after adding the balloon dilation of the tract in 1; percutaneous transhepatic biliary drainage was performed in 1; EUS-HGS was re-performed 1 week later in 1; and observational management was selected in 1 patient because of the small CBD stone with no symptom at the time of intervention. The reason that a SEMS was placed in 1 patient instead of a dedicated plastic stent was over-dilation by the balloon dilator. In this patient, the placement of a consolidated repositionable-type plastic stent was first attempted; however, this was unsuccessful owing to the stiff liver wall. After removing the plastic stent, tract dilation was re-performed using a 4-mm dilating balloon to achieve sufficient tract dilation. However, when a 4-mm balloon dilator is used, the dedicated plastic stent is not wide enough for sufficient coverage and has the risk of bile leakage. To avoid such problems, we finally chose to use a SEMS. B2 was the predominant access route (32 patients) followed by B3 in 23 and B2/3 branch in 2 patients. The median bilirubin level was 0.78 mg/dL and cholangitis was seen in 12 patients. The median diameter of the punctured IHBD was 3.6 mm (range: 1.0–9.6 mm). The median IHBD diameter of the 27 patients in whom a 22G needle was used was 2.9 mm (range: 1.0–5.7 mm), and the median IHBD diameter of the 30 patients in whom a 19G needle was used was 4.4 mm (range: 2.7–9.6 mm). The minimum diameter of the IHBD that could be successfully punctured was 1.5 mm, and 1 patient with 1.0 mm of IHBD diameter was failed. In majority of patients (47/57), the ES dilator, which is a mechanical dilator with an ultra-tapered tip, was used as the first choice of tract dilation before the stenting. Balloon dilation and cautery dilation were added in 25 patients, owing to a stiff liver and IHBD wall. Passing of the guidewire through the anastomotic stricture site was achieved in 9 out of 28 patients of anastomotic stricture and was dilated using 6-mm or 8-mm balloon dilator, and the tip of stent was placed over the anastomotic stricture site. Antegrade stone removal simultaneous with EUS-HES was performed in 7 out of 23 patients with stones. However, the remaining majority patients were performed EUS-HES alone. The median procedure time was 22 min (range: 7–71 min). There were no significant differences between EUS-HGS and EUS-HJS, regarding the technical aspect. The clinical success and AEs are summarized in Table 5. The clinical success, which was defined as being symptom-free or having no recurrence of cholangitis without additional drainage for 2 months after the EUS-HES, was achieved in 91.2% (52/57, intention-to-treat analysis). The median duration of stent placement was 50 days (range: 15–90 days). One patient with clinical failure required additional insertion of a nasobiliary drainage tube owing to the recurrence of cholangitis, which was placed alongside the plastic stent on the postprocedure day 11. Moderate AEs were seen in 15.8% (9/57) of the patients, which included bleeding in 2, peritonitis owing to bile juice leakage in 4, cholecystitis in 2, and pneumoperitoneum in one patient. A 19G needle was used in both two patients in whom bleeding occurred, and one patient required a blood transfusion. This patient had been bleeding tendency owing to coagulopathy resulting from liver failure. Vitamin K2 was administered before the EUS-HES to prevent bleeding. However, owing to the stiff liver wall, this patient was required to use the multiple tract dilation, including cautery dilator. This patient vomited fresh blood and was in hypovolemic shock 6 h after the procedure, with a decrease of hemoglobin level from 10.9 to 7.8 g/dL; however, he responded to normal saline infusion and blood transfusion. The cause of the bleeding was thought to be a burn effect of cautery dilator. A nasogastric tube was placed to monitor the bleeding, and spontaneous hemostasis was achieved without the need for endoscopic procedures. In other patients in whom bleeding occurred during the procedure, immediately, after puncture with a 19G needle, EUS Doppler mode displayed bleeding on the surface of the liver, and the procedure was withdrawn. The reason for the bleeding was thought to be puncture of a blood vessel by the 19G needle. However, there were no changes in vital signs nor hematemesis, and EUS-HES was successfully performed 1 week later. One patient with cholecystitis required percutaneous drainage 2 days after the procedure. The other seven patients were treated by conservative therapy, including antibiotics. There were no intervention-associated deaths.
Table 1.
Patient characteristics (n=57)
| Characteristics | n |
|---|---|
| Age (years), median (range) | 68 (7–90) |
| Sex (male: female) | 28:29 |
| Underlying disease | |
| Bilioenteric anastomotic stricture | 28 |
| IHBD stones | 8 |
| CBD stones | 15 |
| Alcoholic chronic pancreatitis | 2 |
| WON | 1 |
| Idiopathic retroperitoneal fibrosis | 1 |
| Left lobe hepatic injury | 1 |
| Bile duct polyp | 1 |
| Indication for EUS-HGS | |
| Unsuccessful BE-ERCP in patients with a SAA | 44 |
| Primary EUS-HGS owing to expected difficulties in treatment by BE-ERCP in patients with a SAA | 7 |
| Inaccessible papilla owing to benign GOO in patients with a normal anatomy | 4 |
| Unsuccessful ERCP in patients with a normal anatomy | 2 |
| Anatomy | |
| SAA | 51 |
| Total gastrectomy with Roux-en-Y reconstruction | 8 |
| Distal gastrectomy with Roux-en-Y reconstruction | 4 |
| Distal gastrectomy with Billroth II reconstruction | 3 |
| Hepaticojejunostomy with Roux-en-Y reconstruction | 28 |
| Pancreaticoduodenectomy with Child reconstruction | 7 |
| Hepaticoduodenostomy | 1 |
| Normal anatomy | 6 |
IHBD: Intrahepatic bile duct; CBD: Common bile duct; WON: Walled-off necrosis; HGS: Hepaticogastrostomy; BE-ERCP: Balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography; SAA: Surgically altered anatomy; GOO: Gastric outlet obstruction
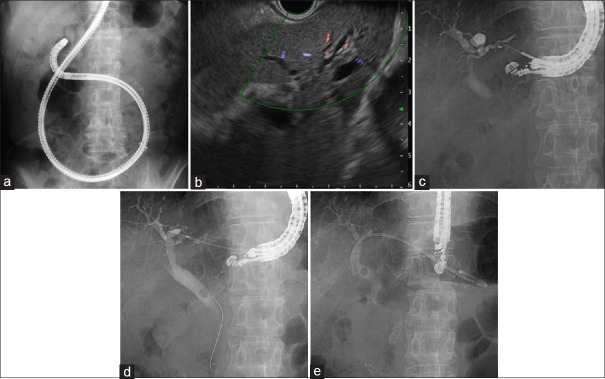
Figure 2.
EUS-guided hepaticogastrostomy for surgically altered anatomy patient with common bile duct stone. (a) Balloon enteroscope was reached into papilla, however biliary selective cannulation was unsuccessful; (b) EUS view of slightly dilated intrahepatic bile duct; (c) the intrahepatic bile duct was punctured using a 22G needle with a 0.018-inch guidewire; (d) the tract was dilated with mechanical dilator. The stone is located on the middle of common bile duct; (e) after exchanging to a 0.025-inch guidewire, the dedicated plastic stent was placed
Figure 3.
EUS-guided hepaticogastrostomy for surgically altered anatomy patient with bilioenteric anastomotic stricture. (a) The intrahepatic bile duct was punctured using a 22G needle with a 0.018-inch guidewire; (b) passing of the guidewire over the stricture site was achieved; (c) after exchanging to a 0.025-inch guidewire, the dedicated stent was inserted. The tip of stent was placed over the stricture site into the jejunum after the balloon dilation
Figure 4.
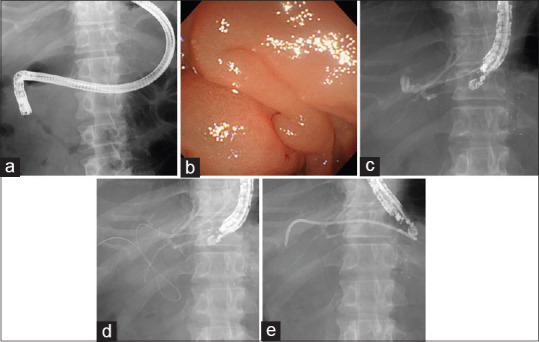
EUS-guided hepaticogastrostomy for normal anatomy patient with benign biliary stricture. (a) Insertion of duodenoscope was unsuccessful owing to the duodenal stricture results from walled-off necrosis. (b) Endoscopic view of duodenal stricture. (c) Intrahepatic bile duct was punctured with 19G needle. The previously placed biflanged metal stent for walled-off necrosis is recognized in the right side of the image. (d) 0.025-inch guidewire was advanced into the common bile duct. (e) Dedicated plastic stent was placed after the tract dilation
Table 2.
Characteristics of patients who underwent EUS-hepaticojejunostomy and their outcomes (n=8)
| Patient | Age (years)/sex | Underlying disease | Anatomy | Indication of EUS-HJS | Presence of cholangitis | Needle type | Diameter of IHBD (mm) | Procedure time (min) | Technical success | Adverse events |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 81/male | CBD stone | TGRY | Unsuccessful BE-ERCP | No | 22G | 3.0 | 35 | Yes | No |
| 2 | 74/female | CBD stone | TGRY | Unsuccessful BE-ERCP | No | 22G | 4.0 | 35 | Yes | No |
| 3 | 82/female | CBD stone | TGRY | Unsuccessful BE-ERCP | No | 22G | 2.2 | 15 | Yes | No |
| 4 | 79/female | CBD stone | TGRY | Unsuccessful BE-ERCP | No | 19G | 2.7 | 23 | Yes | No |
| 5 | 88/male | CBD stone | TGRY | Unsuccessful BE-ERCP | No | 22G | 5.7 | 45 | Yes | No |
| 6 | 68/male | CBD stone | TGRY | Unsuccessful BE-ERCP | No | 22G | 3.0 | 44 | Yes | No |
| 7 | 78/female | CBD stone | TGRY | Unsuccessful BE-ERCP | No | 19G | 4.2 | 10 | Yes | No |
| 8 | 78/male | CBD stone | TGRY | Unsuccessful BE-ERCP | No | 19G | 4.0 | 32 | Yes | No |
HJS: Hepaticojejunostomy; CBD: Common bile duct; TGRY: Total gastrectomy with Roux-en-Y reconstruction; BE-ERCP: Balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography; IHBD: Intrahepatic bile duct
Table 3.
Characteristics of normal anatomy patients who underwent EUS-hepaticogastrostomy and their outcomes (n=6)
| Patient | Age years/sex | Underlying disease | Indication of EUS-HGS | Presence of cholangitis | Diameter of IHBD (mm) | Needle type | Procedure time (min) | Technical success | Adverse events |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 48/male | WON | GOO and BBS with inaccessible papilla | Yes | 4.6 | 19G | 9 | Yes | No |
| 2 | 87/male | Chronic pancreatitis | GOO and BBS with inaccessible papilla | No | 4.1 | 19G | 21 | Yes | Cholecystitis |
| 3 | 85/male | Retroperitoneal fibrosis | GOO and BBS with inaccessible papilla | Yes | 3.8 | 19G | 20 | Yes | Bleeding |
| 4 | 55/male | Chronic pancreatitis | GOO and BBS with inaccessible papilla | Yes | 7.0 | 19G | 17 | Yes | No |
| 5 | 7/male | Traumatic hepatic injury | Complete BBS of left hepatic duct with unsuccessful ERCP | No | 2.8 | 22G | 23 | Yes | No |
| 6 | 82/male | IHBD stone | Left IHBD stone with unsuccessful ERCP | No | 3.0 | 19G | 19 | Yes | No |
HGS: Hepaticogastrostomy; WON: Walled-off necrosis; IHBD: Intrahepatic bile duct; GOO: Gastric outlet obstruction; BBS: Benign biliary stricture
Table 4.
Technical outcomes (n=57)
| Total (n=57) | EUS-HGS (n=49) | EUS-HJS (n=8) | P | |
|---|---|---|---|---|
| Success of plastic stent placement | 92.9% (53/57) | 91.8% (45/49) | 100% (8/8) | 0.411 |
| Punctured IHBD (B2/B3/branch of B2, 3) | 32/23/2 | 27/20/2 | 5/3/0 | 0.602 |
| Median bilirubin level (mg/dL), range | 0.78 (0.3–5.7) | 0.8 (0.3–5.7) | 0.53 (0.3–1.5) | 0.126 |
| Presence of cholangitis (presence/absence) | 12/57 | 12/49 | 0/8 | 0.119 |
| Median diameter of punctured IHBD (mm), range | 3.6 (1.0–9.6) | 3.7 (1.0–9.6) | 3.1 (2.2–5.7) | 0.305 |
| Needle used | ||||
| 19G | 30 | 27 | 3 | 0.364 |
| 22G | 27 | 22 | 5 | |
| Devices for tract dilation | ||||
| Mechanical dilator | 47 | 40 | 7 | 0.203 |
| Balloon dilator | 13 | 13 | 0 | |
| Electrocautery dilator | 12 | 10 | 2 | |
| Median procedure time (min), range | 22 (7–71) | 20 (7–71) | 33.5 (10–45) | 0.225 |
HGS: Hepaticogastrostomy; HJS: Hepaticojejunostomy; IHBD: Intrahepatic bile duct
Table 5.
Clinical outcomes and adverse events (n=57)
| Total (n=57) | EUS-HGS (n=49) | EUS-HJS (n=8) | P | |
|---|---|---|---|---|
| Clinical success rate | 91.2% (52/57) | 89.85% (44/49) | 100% (8/8) | 0.353 |
| Adverse events rate | 15.7% (9/57) | 18.45% (9/49) | 0% (0/8) | 0.193 |
| Peritonitis (bile juice leakage) | 4 | 4 | 0 | |
| Bleeding | 2 | 2 | 0 | |
| Cholecystitis | 2 | 2 | 0 | |
| Pneumoperitoneum | 1 | 1 | 0 | |
| Stent migration | 0% (0/57) | 0% (0/49) | 0% (0/8) | NA |
HGS: Hepaticogastrostomy; HJS: Hepaticojejnostomy; NA: Not available
DISCUSSION
EUS-BD was first reported in 2001, and since then, several investigators have addressed the feasibility of EUS-BD.[11,12,13,14] Recently, EUS-BD has been utilized for the treatment of benign pancreaticobiliary diseases.[2,15,16,17] We previously proposed the current treatment algorithm of benign biliary diseases in patients with SAA.[5] For nonlarge bile duct stones or nonsevere anastomotic strictures, one-step EUS-guided antegrade intervention is recommended. Otherwise, EUS-HES for the creation of a temporal access route with two-step antegrade intervention is recommended. In the present study, antegrade procedures, such as dilation of anastomotic stricture or antegrade removal of stone simultaneous with EUS-HES, were performed one-third of the patients, although the remaining majority patients were performed EUS-HES alone, as the most of the patients were difficult to treat by one session. Namely, preceding EUS-HES for the creation of a temporal access route for the sequential antegrade intervention is highly demanded in benign pancreaticobiliary diseases. In the present study, we focused on the technical aspect and usability of dedicated plastic stent of EUS-HES for benign pancreaticobiliary diseases. Regarding the stents, whether a SEMS or a plastic stent should be used for EUS-HES remains unclear.[18] An advantage of SEMS is its long duration of stent patency compared with a plastic stent. However, the disadvantages of SEMS are its high rate of stent shortening, which may cause unexpected inward stent migration, leading to fatal conditions, and stent-associated IHBD occlusion with segmental cholangitis owing to its width and cover. In addition, stent deployment in the appropriate position is technically difficult for SEMS compared with plastic stents, particularly for beginners of interventional EUS. On the other hand, the advantages of the plastic stent are the lack of a risk of stent shortening, ease of stent placement, and low cost. In the present study, we mainly evaluated the technical outcomes and usability of the plastic stent. The technical success was achieved in the majority of attempted patients. The obtaining of high technical success rate was thought to be achieved to the several following reasons.
One was the use of a dedicated plastic stent. In general, compared with patients with malignant diseases, patients with benign diseases tend to have a stiff liver and IHBD wall owing to their long period of suffering the recurrent cholangitis, resulting in secondary biliary cirrhosis. The stiffness of the liver and IHBD wall makes the EUS-HES procedure difficult. Therefore, the use of a stent that has high insertability and penetrability is mandatory. In the present study, regarding selection of the type of plastic stent (push-type or consolidated repositionable-type), there is a historical background. Initially, the 8-Fr push-type stent was developed as a dedicated plastic stent for EUS-HES. However, we thought that the 7-Fr is much easier to use for penetrating the liver wall, particularly in patients with benign diseases. Therefore, we changed to using the 7-Fr push-type stent. However, for push-type stent, there was no salvage procedure for when the stent could not penetrate the liver wall, and this was one of the biggest disadvantages of the push-type stent. Hence, the 7-Fr consolidated repositionable-type stent has been developed. If the stent cannot penetrate the liver wall owing to insufficient dilation of the tract or a stiff liver wall, salvage procedure such as pulling back the stent and re-dilating the tract while maintaining the guidewire placement is possible when using consolidated repositionable-type stent. However, at first, consolidated repositionable-type stent had a disadvantage of decreased insertability, owing to the gap between the inner sheath and the 0.025-inch guidewire, and the decreased rigidity of the stent. Therefore, most recently, modified 7-Fr consolidated repositionable-type stent has been developed. The stent was modified as specificated to 0.025-inch guidewire, the gap between guidewire and inner sheath has been reduced, and the tip of the stent became more tapered. Owing to these modifications, insertability has been improved. Considering safety and reliability, we recommend the use of the 7-Fr modified consolidated repositionable-type stent as an initial intervention for patients with benign diseases. The push-type stent may be recommended in cases of stent replacement or in patients with malignant diseases in whom the liver wall is not expected to be stiff. However, compared with SEMS, plastic stents have concerns regarding stent patency. In general, the stent patency of SEMS is better than that of plastic stents. In patients with malignant diseases, one of the priorities is the duration of stent patency. However, regarding patients with benign diseases, a long duration of stent patency is not the highest priority as the placed stent is removed within 1–2 months for the sequential antegrade intervention. Namely, the main purpose of EUS-HES for patients with benign diseases is the creation of temporal access route for sequential intervention, not for the long duration of drainage. In fact, in this study, the median duration of stent placement was 50 days, and none of the patients except for one developed stent occlusion with cholangitis during the waiting period of sequential intervention after the discharge. In addition, there were no cases of stent dislodgement or migration. Considering these points, the plastic stent appears to be suitable, with sufficient patency to perform EUS-HES for patients with benign diseases, and we recommend sequential antegrade intervention to be performed 1–2 months after the EUS-HES. However, it remains controversial so as to whether plastic stents or SEMSs are suitable for EUS-HES. Miranda-Garcia et al. demonstrated that technical success of EUS-HES with the use of a fully covered SEMS (80 mm × 10 mm) was achieved in 6 out of 7 SAA patientswith bilioenteric anastomotic strictures, as the first endoscopic step.[2] Nevertheless, outward migration of the SEMS after 4–9 weeks was seen in four patients owing to a minimally dilated IHBD; created fistula was enough dilated to replace double-pigtail stent with no consequences to the patients. Pizzicannella et al. demonstrated that all the 12 SAA patients with bilioenteric anastomotic strictures achieved technical and clinical success of EUS-guided SEMS (80 mm × 10 mm) placement.[15] Six of the patients in whom the guidewire has passed through the stenotic anastomosis had a transanastomotic double-pigtail plastic stent deployed, and the remaining six patients, in whom crossing the guidewire was impossible during the first procedure, had a double-pigtail plastic stent inside an SEMS deployed to decrease the risk of SEMS migration. Inward migration of the SEMS with cholangitis was seen in two patients although it was managed successfully by endoscopic procedures. The placement of a double-pigtail plastic stent inside an SEMS may decrease the risk of migration. However, these studies, as well as the present study, are retrospective studies performed at a single center, and there are no large-scale data comparing the plastic stent and SEMS. Therefore, further comparative studies are needed to reach a definite conclusion.
Another reason for the high technical success rate in our study may be attributable to the use of multiple dilators for the tract dilation. As shown in Table 4, in most patients, an ES dilator was the first choice for tract dilation. This plastic mechanical dilator has an extremely tapered and stiff tip, which enables easy penetration of the liver and IHBD wall.[19] However, in cases in which sufficient dilation is not obtained by the ES dilator alone, a balloon dilator and/or electrocautery dilator was also used. The combination of these dilators with step-by-step tract dilation is important for the success of the following stent placement, particularly for patients with a stiff liver.
The other reason for the high technical success rate in the present study may be the use of a 22G needle. Puncture using a 19G needle has been conventionally performed in EUS-HES. However, in recent years, owing to the development of various devices and techniques, puncture using a 22G needle has become possible. Theoretically, regarding the AE of bleeding, puncture using a 22G needle is much safer than that using a 19G needle, owing to the smaller needle diameter. As shown in Table 4, a 22G needle was used in half of the patients for the IHBD puncture. In this study, the median diameter of punctured IHBD was 3.6 mm, and the median bilirubin level was 0.78 mg/dL, which was smaller and lower, respectively, than those previously reported in patients with malignant diseases.[7] The median IHBD diameter of the patients in whom a 22G needle was used was 2.9 mm, and a high technical success rate was achieved. Based on these data, we recommend the use of a 22G needle in cases with insufficient dilation of the IHBD, for example, when it is less than 3 mm. Because a stiff liver and a thin IHBD are common features of patients with benign diseases, puncturing with a 22G needle appears suitable, as the thin needle is sharper and has higher operability than a 19G needle. However, puncture and thin guidewire manipulation using a 22G needle are technically challenging. There are concerns of kinking and peeling of the tip of the guidewire during guidewire manipulation.[18,20] Thus, gentle wire manipulation by a highly experienced assistant is mandatory. If a more flexible 0.018-inch guidewire with high-seeking ability is developed in the future, puncture using a 22G needle, which is less invasive and safer than a 19G needle, will become the standard for preventing bleeding, even for patients with a dilated IHBD and those with malignant diseases.
In the present study, we also included patients who underwent EUS-HJS. Generally, EUS-HJS is considered to be more difficult than EUS-HGS as the space of the jejunum lumen is limited. However, we achieved a high technical success rate using a dedicated plastic stent with no significant difference between EUS-HGS, as the stent deployment is easier than that of SEMS, even in the limited space of the jejunum lumen. James et al. also reported that five EUS-HJS procedures were successfully performed with the use of a SEMS.[21] They suggested that EUS-HJS may be the preferred approach in patients with a reduced stomach size, such as for partial gastrectomy and RY gastric bypass. However, there have been no studies to date comparing plastic stents with SEMS.
In the present study, most of the patients with SAA were first attempted to treat by BE-ERCP, but the procedure was unsuccessful. On the other hand, primary EUS-HES without BE-ERCP attempt was performed in seven HJRY patients. Most of these patients had undergone unsuccessful BE-ERCP in another institution and were referred to our institution. Generally, BE-ERCP for patients with HJRY is one of the technically challenging and time-consuming procedures, owing to the long length of limbs with the presence of a normal stomach and duodenum. Some retrospective studies demonstrated that the technical success of BE-ERCP for the patients with HJRY was 68%–93%, which is lower than that of other SAA patients.[22,23,24]. In this study, among these seven patients, EUS-HES was successfully performed in six patients with a median procedure time of 22 min. The advantage of EUS-HES is that the procedure time is shorter than that of BE-ERCP. One comparative study of BE-ERCP and EUS-BD demonstrated that EUS-BD procedures are significantly less time-consuming.[25] However, the AE rate of EUS-BD has been reported to be higher than that of BE-ERCP. Hence, for HJRY patients, primary EUS-BD might be a treatment option, if an institution has experts in interventional EUS. However, BE-ERCP should be the primary treatment for most SAA patients.
In the present study, we included not only SAA patients but also patients with a normal anatomy. There are limited data demonstrating the usefulness of EUS-HES for patients with a normal anatomy who have benign diseases. In general, EUS-guided rendezvous is performed in benign disease patients with a normal anatomy, in whom conventional ERCP was unsuccessful.[26] However, there are patients who are not indicated for EUS-guided rendezvous, such as those with benign GOO with biliary stricture owing to walled-off necrosis (WON) or chronic pancreatitis, and complete BBS owing to biliary injury, as guidewire passage and/or grabbing are impossible. Chronic pancreatitis and WON owing to necrotizing pancreatitis occasionally induce benign GOO with biliary stricture.[27] Duodenal stricture caused by WON is refractory, and complete GOO makes ERCP difficult or impossible. In such cases, EUS-HES is a useful and alternative approach to ERCP. There were four cases of benign GOO with biliary stricture in our study. All four of these patients first underwent ERCP, although scope insertion was unsuccessful. Subsequently, all of these patients underwent EUS-HES and achieved clinical success. Another two normal anatomy patients underwent EUS-HES for the BBS of left hepatic duct and B3 IHBD stones, as both were initially unsuccessfully treated by ERCP. In general, BBS is treated by transpapillary stenting.[28] However, complete BBS owing to biliary injury is occasionally refractory, and transpapillary stenting is technically challenging. B3 IHBD stones are also difficult to treat via transpapillary compared with B2 stones, as the B3 is an obtuse angle. In such cases, EUS-HES might be a useful alternative to ERCP for the creation of a temporal access route for the sequential antegrade stone removal and/or stricture dilation.
Our study demonstrates that the appropriate indications of EUS-HES and the recommended needle size for benign pancreaticobiliary diseases are as follows. Regarding patient symptoms and underlying diseases, most benign pancreaticobiliary diseases are indications, such as recurrent cholangitis, symptomatic CBD or IHBD stones, chronic pancreatitis, biliary strictures, and anastomotic strictures. Regarding technical and anatomical indications, papilla or anastomotic sites that are difficult or impossible to reach, and failed or difficult ERCP or BE-ERCP can be indications. Regarding endoscopic procedural indications, an IHBD diameter of at least 1.5 mm, with no bleeding tendency and no intervening vessels, is a good indication of EUS-HES. For IHBD diameters of less than 3 mm, the use of a 22G needle is recommended, and for those of more than 3 mm, a 19G needle can be used.
There are several limitations to this study. First, this is a retrospective study that was performed at a single center. Second, this study mainly focused on the technical aspect and details of EUS-HES with usability of the dedicated plastic stent for patients with benign pancreaticobiliary diseases, although the long-term outcomes of sequential intervention have not yet been evaluated. Hence, further evaluation, including long-term follow-up, is required in the future. In conclusion, our study demonstrated that EUS-HES using a plastic stent is feasible and safe for the treatment of patients with benign pancreaticobiliary diseases.
Financial support and sponsorship
Nil.
Conflicts of interest
Takao Itoi is an Associate Editor of Endoscopic Ultrasound and Shuntaro Mukai is an Editorial Board Member. The article was subject to the journal's standard procedures, with peer review handled independently of this Member and his research groups. Takao Itoi and Takayoshi Tsuchiya are consultants of Gadelius Medical Co. Ltd.
REFERENCES
- 1.Itoi T, Sofuni A, Tsuchiya T, et al. Endoscopic ultrasonography-guided transhepatic antegrade stone removal in patients with surgically altered anatomy: Case series and technical review (with videos) J Hepatobiliary Pancreat Sci. 2014;21:E86–93. doi: 10.1002/jhbp.165. [DOI] [PubMed] [Google Scholar]
- 2.Miranda-García P, Gonzalez JM, Tellechea JI, et al. EUS hepaticogastrostomy for bilioenteric anastomotic strictures: A permanent access for repeated ambulatory dilations.Results from a pilot study? Endosc Int Open. 2016;4:E461–5. doi: 10.1055/s-0042-103241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hosmer A, Abdelfatah MM, Law R, et al. Endoscopic ultrasound-guided hepaticogastrostomy and antegrade clearance of biliary lithiasis in patients with surgically-altered anatomy. Endosc Int Open. 2018;6:E127–30. doi: 10.1055/s-0043-123188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iwashita T, Nakai Y, Hara K, et al. Endoscopic ultrasound-guided antegrade treatment of bile duct stone in patients with surgically altered anatomy: A multicenter retrospective cohort study. J Hepatobiliary Pancreat Sci. 2016;23:227–33. doi: 10.1002/jhbp.329. [DOI] [PubMed] [Google Scholar]
- 5.Mukai S, Itoi T, Sofuni A, et al. EUS-guided antegrade intervention for benign biliary diseases in patients with surgically altered anatomy (with videos) Gastrointest Endosc. 2019;89:399–407. doi: 10.1016/j.gie.2018.07.030. [DOI] [PubMed] [Google Scholar]
- 6.Umeda J, Itoi T, Tsuchiya T, et al. A newly designed plastic stent for EUS-guided hepaticogastrostomy: A prospective preliminary feasibility study (with videos) Gastrointest Endosc. 2015;82:390–600. doi: 10.1016/j.gie.2015.02.041. [DOI] [PubMed] [Google Scholar]
- 7.Park DH, Jang JW, Lee SS, et al. EUS-guided biliary drainage with transluminal stenting after failed ERCP: Predictors of adverse events and long-term results. Gastrointest Endosc. 2011;74:1276–84. doi: 10.1016/j.gie.2011.07.054. [DOI] [PubMed] [Google Scholar]
- 8.Cho DH, Lee SS, Oh D, et al. Long-term outcomes of a newly developed hybrid metal stent for EUS-guided biliary drainage (with videos) Gastrointest Endosc. 2017;85:1067–75. doi: 10.1016/j.gie.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–54. doi: 10.1016/j.gie.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 10.Mukai S, Tsuchiya T, Itoi T. Endoscopic ultrasonography-guided hepaticogastrostomy with novel two-step puncture technique following peroral cholangioscopy-assisted stone removal. Dig Endosc. 2020;32:e32–3. doi: 10.1111/den.13556. [DOI] [PubMed] [Google Scholar]
- 11.Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: A new technique for biliary drainage. Endoscopy. 2001;33:898–900. doi: 10.1055/s-2001-17324. [DOI] [PubMed] [Google Scholar]
- 12.Wang K, Zhu J, Xing L, et al. Assessment of efficacy and safety of EUS-guided biliary drainage: A systematic review. Gastrointest Endosc. 2016;83:1218–27. doi: 10.1016/j.gie.2015.10.033. [DOI] [PubMed] [Google Scholar]
- 13.Itoi T, Sofuni A, Itokawa F, et al. Endoscopic ultrasonography-guided biliary drainage. J Hepatobiliary Pancreat Sci. 2010;17:611–6. doi: 10.1007/s00534-009-0196-1. [DOI] [PubMed] [Google Scholar]
- 14.Irisawa A, Miyoshi H, Itoi T, et al. Recent innovations in therapeutic endoscopy for pancreatobiliary diseases. Dig Endosc. 2020;32:309–15. doi: 10.1111/den.13473. [DOI] [PubMed] [Google Scholar]
- 15.Pizzicannella M, Caillol F, Pesenti C, et al. EUS-guided biliary drainage for the management of benign biliary strictures in patients with altered anatomy: A single-center experience. Endosc Ultrasound. 2020;9:45–52. doi: 10.4103/eus.eus_55_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakai Y, Kogure H, Isayama H, et al. Endoscopic ultrasound-guided biliary drainge for benign biliary diseases. Clin Endosc. 2019;52:212–9. doi: 10.5946/ce.2018.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogura T, Takenaka M, Shiomi H, et al. Long-term outcomes of EUS-guided transluminal stent deployment for benign biliary disease: Multicenter clinical experience (with videos) Endosc Ultrasound. 2019;8:398–403. doi: 10.4103/eus.eus_45_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Itoi T, Isayama H, Sofuni A, et al. Stent selection and tips on placement technique of EUS-guided biliary drainage: Transduodenal and transgastric stenting. J Hepatobiliary Pancreat Sci. 2011;18:664–72. doi: 10.1007/s00534-011-0410-9. [DOI] [PubMed] [Google Scholar]
- 19.Honjo M, Itoi T, Tsuchiya T, et al. Safety and efficacy of ultra-tapered mechanical dilator for EUS-guided hepaticogastrostomy and pancreatic duct drainage compared with electrocautery dilator (with video) Endosc Ultrasound. 2018;7:376–82. doi: 10.4103/eus.eus_2_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharma M, Toshniwal J, Vashistha C, et al. Shearing of the sheath of the guide wire: A complication of endoscopic ultrasound-guided rendezvous procedure. Endosc Ultrasound. 2013;2:171–2. doi: 10.7178/eus.06.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.James TW, Fan YC, Baron TH. EUS-guided hepaticoenterostomy as a portal to allow definitive antegrade treatment of benign biliary diseases in patients with surgically altered anatomy. Gastrointest Endosc. 2018;88:547–54. doi: 10.1016/j.gie.2018.04.2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Katanuma A, Isayama H. Current status of endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy in Japan: Questionnaire survey and important discussion points at Endoscopic Forum Japan 2013. Dig Endosc. 2014;26(Suppl 2):109–15. doi: 10.1111/den.12247. [DOI] [PubMed] [Google Scholar]
- 23.Parlak E, Ciçek B, Dişibeyaz S, et al. Endoscopic retrograde cholangiography by double balloon enteroscopy in patients with Roux-en-Y hepaticojejunostomy. Surg Endosc. 2010;24:466–70. doi: 10.1007/s00464-009-0591-3. [DOI] [PubMed] [Google Scholar]
- 24.Fujimoto T, Mori Y, Nakashima Y, et al. Endoscopic retrograde cholangiopancreatography in patients with surgically altered gastrointestinal anatomy: A retrospective study. Int Surg. 2018;103:184–90. [Google Scholar]
- 25.Khashab MA, El Zein MH, Sharzehi K, et al. EUS-guided biliary drainage or enteroscopy-assisted ERCP in patients with surgical anatomy and biliary obstruction: An international comparative study. Endosc Int Open. 2016;4:E1322–7. doi: 10.1055/s-0042-110790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iwashita T, Yasuda I, Mukai T, et al. EUS-guided rendezvous for difficult biliary cannulation using a standardized algorithm: A multicenter prospective pilot study (with videos) Gastrointest Endosc. 2016;83:394–400. doi: 10.1016/j.gie.2015.04.043. [DOI] [PubMed] [Google Scholar]
- 27.Bugiantella W, Rondelli F, Boni M, et al. Necrotizing pancreatitis: A review of the interventions. Int J Surg. 2016;28(Suppl 1):S163–71. doi: 10.1016/j.ijsu.2015.12.038. [DOI] [PubMed] [Google Scholar]
- 28.Coté GA, Slivka A, Tarnasky P, et al. Effect of covered metallic stents compared with plastic stents on benign biliary stricture resolution: A randomized clinical trial. JAMA. 2016;315:1250–7. doi: 10.1001/jama.2016.2619. [DOI] [PMC free article] [PubMed] [Google Scholar]