Abstract
Background
Opioid-related morbidity and mortality has increased during the COVID-19 pandemic, yet specific information about the communities most affected remains unknown. Our objective is to evaluate decedent-level associations with an opioid-related death following the implementation of stay-at-home orders in Los Angeles County.
Methods
This retrospective cohort study used data from the L.A. County Medical Examiner-Coroner to identify opioid-related deaths in 2019 and 2020. We used logistic regression to analyze the change in opioid-related deaths following a 30-day washout period after the start of stay-at-home orders. Independent variables included decedent age, gender, race and ethnicity, heroin or fentanyl present at the time of death, census tract-level education, and a scheduled drug prescription in the year before death.
Results
Opioid-related deaths in L.A. County are most common in census tracts where a small percentage of the population has a Bachelor’s degree. Following stay-at-home orders, Non-Hispanic Caucasian individuals had significantly more opioid-related deaths than Hispanic individuals (risk ratio (RR): 1.82 [95 % CI, 1.10–3.02]; P < 0.05) after adjusting for age, gender, and heroin or fentanyl use. Racial and ethnic differences in mortality were not explained by census tract-level education or recent scheduled drug prescriptions.
Discussion
There has been an alarming rise in opioid-related deaths in L.A. County during 2020. The increase in opioid-related overdose deaths following the onset of COVID-19 and related policies occurred most often among Non-Hispanic Caucasian individuals. Further research on this trend's underlying cause is needed to inform policy recommendations during these simultaneous public health crises.
Keywords: Opioid overdose, COVID-19, Mortality, Heroin, Fentanyl
1. Background
The United States is amid both a coronavirus disease 2019 (COVID-19) pandemic and an ongoing opioid epidemic. Their simultaneous occurrence poses a challenge for policymakers seeking to reduce infectious disease spread without exacerbating opioid use and overdose. Restrictions to the healthcare system, contraction of the economy, and general stress brought on by a deadly pandemic may have contributed to increases in licit and illicit opioid use and subsequent overdose--both fatal and non-fatal (Slavova et al., 2020; American Medical Association, 2020; Millenium Health, 2020; Alter and Yeager, 2020; Rodda et al., 2020). In the months following the introduction of state-mandated stay-at-home orders, there were increases in non-fatal and fatal drug overdoses across the United States (Alter and Yeager, 2020; Appa et al., 2021; Mason et al., 2021; U.S. Centers for Disease Control and Prevention, 2021b; Friedman and Akre, 2021; Ahmad et al., 2021). These policies seeking to reduce the spread of COVID-19 may have also exacerbated mental health issues that could trigger relapse and increased the risk of an isolated overdose without rescue (Khatri and Perrone, 2020).
As of March 2021, L.A. County has the largest number of confirmed COVID-19 cases and deaths nationwide, despite statewide stay-at-home orders in effect since March 19, 2020 (Dong et al., 2020; State of California, 2020). California has the 4th highest number of drug overdoses in the country, and L.A. County has historically had a higher prevalence of prescription opioid and misuse than the national average (County of Los Angeles Department of Public Health, 2018). From 2019–2020 the fentanyl-related mortality rate in L.A. County more than doubled (Shover et al., 2020). Therefore, understanding how the COVID-19 pandemic and opioid epidemic have impacted L.A. County provides useful information to prevent further exacerbation of the opioid crisis.
COVID-19 has disproportionately impacted historically marginalized groups and raised concerns about health disparities (Artiga et al., 2020). The COVID-19 and opioid epidemics are concentrated in different racial and ethnic groups. There are higher rates of infection, hospitalization, and death from COVID-19 among Black, Hispanic, Latino, American Indian, and Alaska Native individuals compared to Non-Hispanic Caucasian individuals (U.S. Centers for Disease Control and Prevention, 2021a). The opioid epidemic has been concentrated among low-income Non-Hispanic Caucasian individuals and people with lower educational attainment (Song, 2017; Friedman et al., 2019; Case and Deaton, 2015). Little is known about whether or not COVID-19 and its related policies have resulted in rising opioid-related deaths in some communities but not others. While aggregate level reports have shown an increase in opioid overdoses during this time, no study has evaluated decedent- and community-level socioeconomic characteristics. Our study's main objective is to identify factors associated with opioid-related overdose deaths following the implementation of stay-at-home orders in L.A. County.
2. Methods
2.1. Data sources
This retrospective cohort study relied upon data from the Los Angeles County Department of the Medical Examiner-Coroner autopsy reports, California Controlled Substance Utilization Review and Evaluation System (CURES), and the American Community Survey. All drug overdose deaths in L.A. County are investigated by the Department of the Medical Examiner-Coroner. Completed autopsy reports for deaths with opioid-related causes occurring in L.A. County between January 2019 and July 2020 were collected from an ongoing study with the L.A. County Medical Examiner-Coroner. Demographic characteristics included in the death record were collected. Using this decedent information, we queried CURES for the presence of a prescription for a scheduled drug written by a prescriber in Los Angeles County in the year before death. The California Controlled Substance Utilization Review and Evaluation System is the prescription drug monitoring program for the state. It stores Schedule II, III, and IV controlled substance prescription dispensing information, dates of a prescription fill, and quantities (California Department of Justice, 2020). The Medical Examiner-Coroner has the authority to use CURES to educate practitioners and others, following the California State's Health and Safety Code § 11165(c)(2). To capture census tract-level characteristics, we used the publicly available American Community Survey 2018 data. The survey is conducted monthly among various samples of the U.S. population. It collects current information on topics not reported in the U.S. Census, such as education, employment, internet access, and transportation (United States Census Bureau, 2020a).
2.2. Measures
Medical Examiner-Coroner death reports provided complete information regarding the decedent’s date of death, age, gender, race, ethnicity, and the presence of fentanyl or heroin at the time of death. The controlled-substance utilization review evaluation system provided each decedent's most recent address and scheduled drug prescriptions in the year before death. Addresses were linked to census tract-level variables using the Census Geocoder (United States Census Bureau, 2018a). For errors where the geocoder was unable to return results, street, zip code, and city received manual verification and updating. The American Community Survey identified the average percentage of adult residents aged 25 or older in the census tract with a Bachelor's degree or higher from 2013 to 2018. The Bachelor's degree was considered the relevant measure for educational attainment based on previous research identifying a large disparity in drug-related deaths between those with and without a Bachelor's degree (Case et al., 2020). For decedents with missing or unmatched address information, no tract-level education information could be collected from the American Community Survey. For those decedents, we used multiple imputation, a Monte Carlo technique, to estimate missing education values that reflect the uncertainty around the true value (Demirtas et al., 2008). We assumed education was missing at random and the variables by which it can be predicted have a joint multivariate normal distribution (Demirtas et al., 2008; Bhaskaran and Smeeth, 2014). We also evaluate the validity of this assumption (see Section 2.4). We selected the number of imputations similar to the percentage of cases with incomplete education data based on the equation put forth in Bodner’s conservative approach to estimating reliable point estimates, p-values, and standard errors (Bodner, 2008).
2.3. Outcomes
The outcome of interest was the change in the number of opioid-related deaths from February 2020 to April 2020 following the implementation of stay-at-home orders. Our post-period included deaths occurring on or before April 30th. The month of April was used as the post-period because it was the first full month of stay-at-home orders in L.A. County before requirements for businesses to reopen were eased (Kandel, 2020). Mobility patterns based on personal device data suggest that adherence to stay-at-home orders in L.A. County was greatest during April 2020, as demonstrated by the lowest average mobility since the onset of COVID-19 (Unacast, 2020). We selected a symmetric pre-period of one month. We did not include March 2020 data to account for differential time to implement and adhere to stay-at-home orders within the county. For example, many persons at risk of opioid overdose would not have a depleted supply of opioids or medication-assisted treatments within the first few weeks of stay-at-home orders. Secondary outcomes include the aggregate number of opioid-related deaths in January through April of 2019 compared to the same months in 2020, and the change in the number of deaths by ethnicity and race from February 2019 to April 2019 to examine seasonality.
2.4. Statistical analysis
Our primary model was the following logistic regression:
where Y is dichotomous for date of opioid-related death (April versus February), X1 is continuous for age, X2 is sex, X3 is the presence (or absence) of an illicit opioid in the death record, and X4 is categorical for race and ethnicity. Expanded models include main and interaction effects for the percentage of adults with a Bachelor’s degree in that census tract (continuous) and the presence (or absence) of a prescription for a scheduled drug from a prescriber in L.A. County in the year before the date of death. To validate the assumption that address data was missing at random and educational status could be imputed without bias, we ran a logistic regression with date of opioid-related death (April 2020 versus February 2020) as the outcome and a dichotomous variable for missing address data as the independent variable. We conducted our analyses and estimated risk ratios using Stata and its margins, mimrgns, and nlcom commands (StataCorp, 2019; Klein, 2014).
3. Results
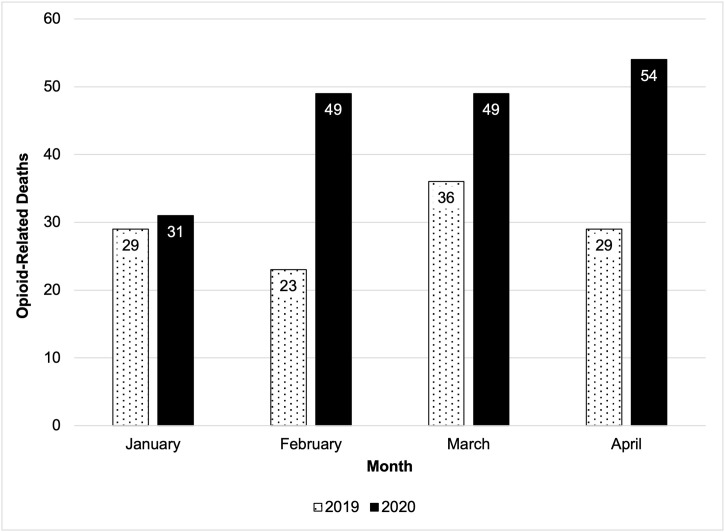
More opioid-related deaths per month occurred in 2020 compared to the same period in 2019 (Fig. 1 ). In total, there were 103 opioid-related deaths in February and April of 2020. The decedents were mostly male (81.6 %) and Non-Hispanic Caucasian (48.5 %). Illicit opioid use (i.e., heroin or fentanyl) was a contributing cause of death for most of the sample (95.1 %). There was no missing information regarding the decedent’s date of death, age, gender, race, ethnicity, and the presence of fentanyl or heroin at the time of death. Due to approximately 33 % of decedents having missing or unmatched address data, multiple imputation with 29 imputations estimated educational attainment. Across included census tracts, the mean prevalence of having a Bachelor's degree or higher among individuals 25 years or older was approximately 11 % lower in the sample than the average in L.A. County (20.9 % and 31.8 %, respectively) (United States Census Bureau, 2018b).Sample characteristics compared to L.A. County population characteristics based on ACS 2018 data are shown in Table 1 . The sample of decedents with opioid-related deaths consists of more males, non-Hispanic Caucasian individuals, and individuals residing in areas where a smaller share of the adult population has a Bachelor's degree or higher compared to the L.A. County population.
Fig. 1.
Unadjusted Number of Opioid-Related Deaths in 2019 and 2020. Dotted bars represent the number of opioid-related deaths in that month in 2019. Shaded bars represent the number of opioid-related deaths in that month in 2020.
Table 1.
Sample Characteristics.
| Sample N = 103 | Los Angeles County (2018) | |
|---|---|---|
| Age, mean (SD) | 36.0 (13.1) | Median = 36.2 |
| Male, No. (%) | 84 (81.6 %) | 49.3 % |
| Race, No. (%) | ||
| American Indian | 1 (1.0 %) | 1.6 % |
| Asian | 3 (2.9 %) | 16.2 % |
| Black | 14 (13.6 %) | 9.3 % |
| Hispanic or Latin American Ethnicity | 33 (32.0 %) | 48.5 % |
| Non-Hispanic Caucasian | 50 (48.5 %) | 26.3 % |
| Unknown | 2 (1.9 %) | |
| Bachelor’s degree or higher, mean (SD) | 20.9 % (11.7) | 31.8 % |
| Heroin or Fentanyl, No. (%) | 98 (95.1 %) |
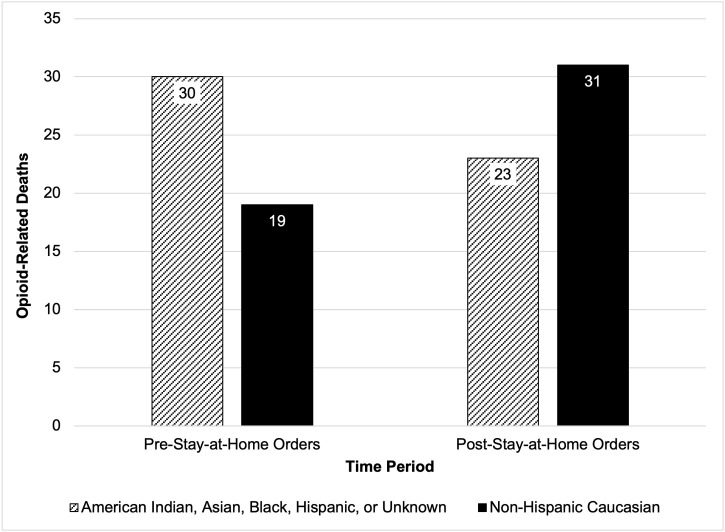
There was a statistically insignificant change in the probability of an opioid-related death in the post-period compared to the pre-period (probability difference: 4.85 percentage points [95 % CI, -4.76 to 14.3]; P > 0.05). Our main model results demonstrate that decedents were 82 % more likely to be Non-Hispanic Caucasian than Hispanic in the period following the implementation of stay-at-home orders (risk ratio (RR): 1.82 [95 % CI, 1.10–3.02]; P < 0.05), adjusting for age, gender, and heroin/fentanyl. These two ethnic groups had the largest share of deaths in both periods and were the only groups with significant differences between them. A histogram of opioid-related deaths by race or ethnicity and time is shown in Fig. 2 . Additional models controlled for education and prescription drug access. We were missing education data on 33.01 % of cases and used 29 imputations (Bodner, 2008). Missing address data was not significantly associated with death in the pre- versus post-period, consistent with data being missing at random (P > 0.05). Tract-level education was not statistically significant (RR for a 10 % increase in the mean percentage of adults with at least a Bachelor’s degree: 1.00 [95 % CI, 0.80–1.24]; P > 0.1) and did not modify the effect of race and ethnicity on death in the post-period (RR of Non-Hispanic Caucasians compared to Hispanic individuals: 1.82 [95 % CI, 1.06–3.09]; P < 0.05), adjusting for age, gender, and heroin/fentanyl. A prescription from a L.A. County prescriber for a scheduled drug in the year before death, when adjusting for age, gender, heroin/fentanyl, and education, was not statistically significant (RR: 0.71 [95 % CI, 0.45–1.11]; P > 0.1) and increased the association between race/ethnicity and death in the post-period (RR for Non-Hispanic Caucasians compared to Hispanic individuals: 1.98 [95 % CI, 1.15–3.41]; P < 0.05). Models controlling for the interactions between education and race/ethnicity as well as prescription drug access and race/ethnicity resulted in statistically insignificant coefficients, indicating that the impact of race and ethnicity on opioid-related deaths in the post-period is not dependent on tract-level education or prescription drug access. Regression results are displayed in Table 2 .
Fig. 2.
Opioid-related deaths by time period and race or ethnicity. Striped bars represent the number of opioid-related deaths in that time period among individuals of American Indian, Asian, Black, Hispanic, or Unknown race and ethnicity. Shaded bars represent the number of opioid-related deaths in that time period among Non-Hispanic Caucasian individuals.
Table 2.
Model Results.
| Variable | Primary Model |
Expanded Model with Education |
Expanded Model with Education & Scheduled Drug Prescription |
|||
|---|---|---|---|---|---|---|
| Risk Ratio | 95 % CI | Risk Ratio | 95 % CI | Risk Ratio | 95 % CI | |
| Age (5 year increase in mean age) | 1.00 | (0.93, 1.08) | 1.00 | (0.93, 1.08) | 1.01 | (0.94, 1.08) |
| Male | 1.09 | (0.62, 1.92) | 1.10 | (0.62, 1.94) | 1.11 | (0.63, 1.95) |
| Race/Ethnicity (Hispanic or Latin American Ethnicity as reference group) | ||||||
| American Indian | – | – | – | – | – | – |
| Asian | – | – | – | – | – | – |
| Black | 1.17 | (0.53, 2.60) | 1.18 | (0.53, 2.66) | 1.25 | (0.56, 2.81) |
| Non-Hispanic Caucasian | 1.82** | (1.10, 3.02) | 1.82** | (1.07, 3.12) | 1.98** | (1.15, 3.41) |
| Unknown | 1.37 | (0.31, 6.04) | 1.37 | (0.31, 6.00) | 1.56 | (0.39, 6.20) |
| Heroin or Fentanyl | 2.75 | (0.42, 17.84) | 2.66 | (0.40, 17.48) | 2.58 | (0.41, 16.34) |
| 10 % increase in mean % of adults in census tract with Bachelor’s degree or higher | – | – | 1.00 | (0.80, 1.24) | 1.01 | (0.81, 1.24) |
| Scheduled drug prescription in the year prior to death | – | – | – | – | 0.71 | (0.45, 1.11) |
| Intercept+ | 0.09* | (0.01, 1.50) | 0.09 | (0.00, 1.96) | 0.09 | (0.00, 1.97) |
Intercepts are displayed as baseline odds, *** p < 0.01, ** p < 0.05, * p < 0.1.
Opioid overdose deaths in April 2020 were 63 % higher than in February 2020 among Non-Hispanic Caucasians and 23 % lower among minority groups. In April 2019, there was a 46 % increase in opioid-related deaths among Non-Hispanic Caucasians and a 0% change in opioid-related deaths among minority groups compared to February 2019. However, we ran the main model on data from February and April of 2019 and did not find significant differences in deaths by race or ethnicity (RR of Non-Hispanic Caucasians compared to Hispanic individuals: 1.21 [95 % CI, 0.64–2.26]; P > 0.1; RR of Black individuals compared to Hispanic individuals: 1.33 [95 % CI, 0.65–2.72]; P > 0.1).
4. Discussion
There has been a concerning rise in opioid-related deaths from 2019–2020. Our analysis highlights that opioid-related deaths in L.A. County remain concentrated among individuals residing in areas where a smaller percentage of the population has a Bachelor’s degree or higher. These findings mirror previous findings that the most significant increase in mortality from suicide and poisonings is concentrated among individuals with less than a Bachelor’s degree (Case and Deaton, 2015).
Our analysis identifies the most significant risk of opioid-related death following stay-at-home orders among Non-Hispanic Caucasian individuals compared to Hispanic individuals. Past studies in the U.S. have identified increased morbidity and decreased mortality among Non-Hispanic Caucasians aged 45–54 years old, driven predominantly by the increase in pain and opioid use (Case and Deaton, 2015). The rise in mortality rate among middle-aged Non-Hispanic Caucasian individuals from self-inflicted deaths from guns, drug addiction, or alcohol are poignantly termed “deaths of despair”. Key drivers to deaths of despair among white working-class individuals in the last 50 years are external forces, such as declining wages, deterioration in job quality, and declining participation in organized religion, community groups, and unions (Case et al., 2020). Contrasting outcomes for non-whites may have to do with stronger community ties and social supports that arose out of generations of impoverished material conditions. Our findings suggest that COVID-19 has further exacerbated one type of deaths of despair, fatal opioid overdoses, among Non-Hispanic Caucasian individuals. The underlying reasons for this were not tract-level education or prescription drug access. Black, Asian, and Hispanic individuals experienced higher unemployment prior to the onset of COVID-19 (Williams, 2020). Perhaps Non-Hispanic Caucasians faced a greater change in the unemployment rate or responded more negatively to this change early in the pandemic. However, while the unemployment rate among minority groups was higher than for Non-Hispanic Caucasian groups in California before the pandemic, the unemployment rate increased least among Non-Hispanic Caucasian individuals from quarter 1 to quarter 2 of 2020 compared to Black, Hispanic, and Asian individuals (10.1 %, 12.3 %, 12.7 %, and 11.2 % respectively) (Williams, 2020). Therefore, it could be the coping response to this change to professional and social structures that is driving the difference in opioid-related mortality by race and ethnicity.
Alternatively, the increased risk of overdose among Non-Hispanic Caucasian individuals following the implementation of stay-at-home orders may reflect a decrease in access to face-to-face treatment, medications for addiction treatment, and formal support networks, such as Narcotics Anonymous. Narcotics Anonymous membership is predominantly Non-Hispanic Caucasian and medications for addiction treatment are provided less frequently to racial minority groups (Alexander et al., 2020; Wu et al., 2016; Narcotics Anonymous World Services, I. et al., 2018). Medication-assisted treatment for opioid use disorder may require daily clinic-based administration of methadone or 30-day appointments or refills of buprenorphine which could be disrupted during COVID-19 (Alexander et al., 2020; Substance Abuse and Mental Health Services Administration and Services, U.S.D.o.H.H., 2015). Individual-level data regarding opioid use disorder treatment linked with outcomes data would be necessary to evaluate this theorized decrease in medicine or support networks and increased relapse. The decline in face-to-face encounters with medical providers may have contributed to the decrease in opioid prescribing rates. A reduction in the supply of prescription opioids may have led to diversion to non-prescription opioids. Since COVID-19 became a state of emergency, illicit fentanyl use has increased (Millenium Health, 2020).
In our analysis of 2019 data, we do not find evidence of significantly more opioid-related deaths among Non-Hispanic Caucasians compared to Hispanic individuals in April versus February. The lack of seasonality in opioid-related deaths based on ethnicity and race in 2019 validates that our findings are specific to the time periods before and after stay-at-home orders in 2020.
A limitation of this study is its lack of decedent-level education data. While neighborhood educational achievement predicts an individual’s educational status, previous research has identified that an individual’s school, family socio-economic status, and parenting variables are also important factors (Nieuwenhuis and Hooimeijer, 2016). Additionally, educational attainment at the tract-level is given in 5-year estimates, which may not capture dynamic changes to education. Yet, one advantage of the 5-year estimates is its increased stability and reliability for less populated census tracts (United States Census Bureau, 2020b). Nevertheless, our analysis of 5-year estimates as point estimates does not take the distribution of each tract-level estimate into account. Another limitation is that this study was limited to drug overdoses involving opioids, so any shifts in all drug class utilization or overdose by race or ethnicity could not be measured. The generalizability of these findings may be limited to Los Angeles County. However, L.A. County is a diverse area of approximately 3% of the US population (United States Census Bureau, 2020c). Further analyses in other counties and in areas where the peak of the COVID-19 outbreak coincided with policy implementation would inform the generalizability of these results.
5. Conclusions
There has been a rise in opioid-related deaths in L.A. County during 2020 compared to 2019. Stay-at-home orders were associated with increased opioid-related deaths among Non-Hispanic Caucasians. One possibility is that changes to social and physical environments during lockdown led to increased opioid overdoses among Non-Hispanic Caucasians. Further research on this trend's underlying causes is needed to inform clinical and policy recommendations during these simultaneous public health crises.
Role of funding source
The National Institutes of Health National Institute on Aging (NIA) (R33AG057395; PI: Jason Doctor) and NIA Roybal Center for Behavioral Interventions (5P30AG024968-18) support this work.
Contributors
Marcella A. Kelley: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft; Jonathan Lucas: Data curation, Investigation, Writing – reviewing & editing; Emily Stewart: Investigation, Methodology, Writing – reviewing & editing; Dana Goldman: Conceptualization, Funding acquisition, Writing – reviewing & editing; Jason N. Doctor: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – reviewing & editing
Declaration of Competing Interest
Dr. Doctor is an independent consultant for Motley Rice LLC. Dr. Goldman reports research support from the National Institutes of Health and Blue Cross Blue Shield of Arizona, Bristol Myers Squibb, Cedars-Sinai Health System, Edwards Lifesciences, Gates Ventures, Genentech, Gilead Sciences, Johnson & Johnson, Kaiser Family Foundation, Novartis, Pfizer, and Roche. He serves as a paid scientific advisor to Biogen, GRAIL, and Precision Medicine Group.
Acknowledgements
All study procedures were approved by the University of Southern California Institutional Review Board (UP-19-00172).
References
- Ahmad F., Rossen L., Sutton P. 2021. Provisional Drug Overdose Death Counts: National Center for Health Statistics. Available at: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm (Accessed: 19 July 2021). [Google Scholar]
- Alexander G.C., Stoller K.B., Haffajee R.L., Saloner B. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19. Ann. Intern. Med. 2020;173(1):57–58. doi: 10.7326/M20-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alter A., Yeager C. 2020. COVID-19 Impact on US National Overdose Crisis: Overdose Detection Mapping Application Program. Available at: http://www.odmap.org/Content/docs/news/2020/ODMAP-Report-June-2020.pdf (Accessed: 25 January 2021) [Google Scholar]
- American Medical Association . 2020. Issue Brief: Reports of Increases in Opioid- and Other Drug-related Overdose and Other Concerns during COVID Pandemic. Available at: https://www.ama-assn.org/system/files/2020-11/issue-brief-increases-in-opioid-related-overdose.pdf (Accessed: 25 January 2021) [Google Scholar]
- Appa A., Rodda L.N., Cawley C., Zevin B., Coffin P.O., Gandhi M., Imbert E. Drug overdose deaths before and after shelter-in-Place orders during the COVID-19 pandemic in San Francisco. JAMA Network Open. 2021;4(5) doi: 10.1001/jamanetworkopen.2021.10452. e2110452-e2110452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artiga S., Garfield R., Orgera K. 2020. Communities of Color at Higher Risk for Health and Economic Challenges Due to COVID-19. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/communities-of-color-at-higher-risk-for-health-and-economic-challenges-due-to-covid-19/ (Accessed: 2 March 2021) [Google Scholar]
- Bhaskaran K., Smeeth L. What is the difference between missing completely at random and missing at random? Int. J. Epidemiol. 2014;43(4):1336–1339. doi: 10.1093/ije/dyu080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodner T.E. What Improves with Increased Missing Data Imputations? Struct. Equ. Model. A Multidiscip. J. 2008;15(4):651–675. [Google Scholar]
- California Department of Justice . 2020. Controlled Substance Utilization Review and Evaluation System. Available at: https://oag.ca.gov/cures 2020. (Accessed: 14 December 2020) [Google Scholar]
- Case A., Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. U. S. A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A., Deaton A., DeGruyter . Princeton University Press; Princeton, NJ: 2020. Deaths of Despair and the Future of Capitalism. [Google Scholar]
- County of Los Angeles Department of Public Health . 2018. Opioid Abuse Prevention and Treatment in Los Angeles County. [Google Scholar]
- Demirtas H., Freels S., Yucel R. Plausibility of multivariate normality assumption when multiply imputing non-Gaussian continuous outcomes: a simulation assessment. J. Stat. Comput. Simul. 2008;78(1):69–84. [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J., Akre S. COVID-19 and the drug overdose crisis: uncovering the deadliest months in the United States, January‒July 2020. Am. J. Public Health. 2021:e1–e8. doi: 10.2105/AJPH.2021.306256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J., Kim D., Schneberk T., Bourgois P., Shin M., Celious A., Schriger D.L. Assessment of Racial/Ethnic and income disparities in the prescription of opioids and other controlled medications in California. JAMA Intern. Med. 2019;179(4):469–476. doi: 10.1001/jamainternmed.2018.6721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel J. 2020. Timeline 2020: A Look Back at the Coronavirus Pandemic. NBC Los Angeles. Available at: https://www.nbclosangeles.com/news/coronavirus/2020-2021-california-coronavirus-pandemic-timeline-key-events/2334100/ (Accessed: 25 January 2021) [Google Scholar]
- Khatri U.G., Perrone J. Opioid use disorder and COVID-19: crashing of the crises. J. Addict. Med. 2020;14(4):e6–e7. doi: 10.1097/ADM.0000000000000684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein D. 2014. MIMRGNS: Stata Module to Run Margins after Mi Estimate. Statistical Software Components, Boston College Department of Economics. [Google Scholar]
- Mason M., Welch S.B., Arunkumar P., Post L.A., Feinglass J.M. Notes from the field: opioid overdose deaths before, during, and after an 11-Week COVID-19 stay-at-Home order - Cook County, Illinois, January 1, 2018-October 6, 2020. MMWR Morb. Mortal. Wkly. Rep. 2021;70(10):362–363. doi: 10.15585/mmwr.mm7010a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millenium Health . 2020. COVID-19 Special Edition: Significant Changes in Drug Use During the Pandemic: Millennium Health. Available at: https://resource.millenniumhealth.com/signalsreportCOVID (Accessed: 25 January 2021) [Google Scholar]
- Narcotics Anonymous World Services, I . 2018. 2018 Narcotics Anonymous Membership Survey. Available at: https://www.na.org/admin/include/spaw2/uploads/pdf/conference/project/2301_MS_2018_Nov19.pdf (Accessed: 16 February 2021) [Google Scholar]
- Nieuwenhuis J., Hooimeijer P. The association between neighbourhoods and educational achievement, a systematic review and meta-analysis. J. Hous Built Environ. 2016;31(2):321–347. doi: 10.1007/s10901-015-9460-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodda L.N., West K.L., LeSaint K.T. Opioid overdose-related emergency department visits and accidental deaths during the COVID-19 pandemic. J. Urban Health. 2020;97(6):808–813. doi: 10.1007/s11524-020-00486-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shover C.L., Falasinnu T.O., Dwyer C.L., Santos N.B., Cunningham N.J., Freedman R.B., Vest N.A., Humphreys K. Steep increases in fentanyl-related mortality west of the Mississippi River: recent evidence from county and state surveillance. Drug Alcohol Depend. 2020;216 doi: 10.1016/j.drugalcdep.2020.108314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Z. Mortality quadrupled among opioid-driven hospitalizations, notably within lower-income and disabled white populations. Health Aff (Millwood). 2017;36(12):2054–2061. doi: 10.1377/hlthaff.2017.0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC. [Google Scholar]
- State of California, Department, E., 2020. EXECUTIVE ORDER N-33-20.
- Substance Abuse and Mental Health Services Administration, Services, U.S.D.o.H.H . 2015. Federal Guidelines for Opioid Treatment Programs. [Google Scholar]
- U.S. Centers for Disease Control and Prevention . 2021. Risk for COVID-19 Infection, Hospitalization, and Death by Race/Ethnicity. Available at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (Accessed: 2 March 2021) [Google Scholar]
- U.S. Centers for Disease Control and Prevention . 2021. Suspected Nonfatal Drug Overdoses During COVID-19. [Google Scholar]
- Unacast . 2020. Unacast Social Distancing Dataset. Available at: https://www.unacast.com/covid19/social-distancing-scoreboard (Accessed: 4 March 2021) [Google Scholar]
- United States Census Bureau . 2018. Census Geocoder Documentation. Available at: https://www.census.gov/programs-surveys/geography/technical-documentation/complete-technical-documentation/census-geocoder.html 2020 (Accessed: 25 January 2021) [Google Scholar]
- United States Census Bureau . 2018. Table DP02: Selected Social Characteristics in the United States. Available at: https://data.census.gov/cedsci/table?q=ACSDP5Y2018.DP02%20Los%20Angeles%20County,%20California&g=0500000US06037&tid=ACSDP5Y2018.DP02&hidePreview=true (Accessed: 25 January 2021) [Google Scholar]
- United States Census Bureau . 2020. The Importance of the American Community Survey and the 2020 Census. Available at: https://www.census.gov/programs-surveys/acs/about/acs-and-census.html 2020 (Accessed: 25 January 2021) [Google Scholar]
- United States Census Bureau . 2020. American Community Survey 5-Year Data (2009-2019) Available at: https://www.census.gov/data/developers/data-sets/acs-5year.2018.html (Accessed: 19 July 2021) [Google Scholar]
- United States Census Bureau . 2020. U.S. and World Population Clock. Available at: https://www.census.gov/popclock/ (Accessed: 25 January 2021) [Google Scholar]
- Williams J. 2020. State Unemployment by Race and Ethnicity. Available at: https://www.epi.org/indicators/state-unemployment-race-ethnicity/ (Accessed: 25 January 2021) [Google Scholar]
- Wu L.T., Zhu H., Swartz M.S. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend. 2016;169:117–127. doi: 10.1016/j.drugalcdep.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]