Abstract
Background:
On average Black patients have longer LOS than comparable White patients. Longer hospital length of stay (LOS) may be associated with higher readmission risk. However, evidence suggests that the Hospital Readmission Reduction Program (HRRP) reduced overall racial differences in 30-day adjusted readmission risk. Yet, it is unclear whether the HRRP narrowed these LOS racial differences.
Objective:
We examined the relationship between Medicare-insured Black-White differences in average, adjusted LOS (ALOS) and the HRRP’s implementation and evaluation periods.
Methods:
Using 2009-2017 data from State Inpatient Dataset from New York, New Jersey, and Florida, we employed an interrupted time series analysis with multivariate generalized regression models controlling for patient, disease, and hospital characteristics. Results are reported per 100 admissions.
Results:
We found that for those discharged home, Black-White ALOS differences significantly widened by 4.15 days per 100 admissions (95% CI: 1.19 to 7.11, P < 0.001) for targeted conditions from before to after the HRRP implementation period, but narrowed in the HRRP evaluation period by 1.84 days per 100 admissions for every year-quarter (95% CI: −2.86 to −0.82, P < 0.001); for those discharged to non-home destinations, there was no significant change between HRRP periods, but ALOS differences widened over the study period. Black-White ALOS differences for non-targeted conditions remained unchanged regardless of HRRP phase and discharge destination.
Conclusion:
Increased LOS for Black patients may have played a role in reducing Black-White disparities in 30-day readmission risks for targeted conditions among patients discharged to home.
Keywords: hospital readmission reduction program, length of stay, disparities, social risk
Introduction
In well-studied inpatient conditions, there is growing evidence that patients who stay in hospital longer have a higher risk of risk-adjusted readmission.1-4 In the age of value-based payment models and increasing hospital consolidation, both patient length of stay (LOS) and readmission risk have significant operational and financial implications for hospitals.5 Operationally, longer LOS is associated with a higher risk of adverse health outcomes because of delays in discharge,6 emergency room boarding,7 and ambulance diversion.8 From a financial standpoint, longer LOS makes the management of hospital throughput and bed occupancy a challenge.
The Centers of Medicare and Medicaid Services (CMS) introduced its Hospital Readmission Reduction Program (HRRP) in 2013 to address growing concerns about readmission risk among Medicare beneficiaries. The HRRP compares hospitals based on risk-adjusted 30-day readmission rates of common inpatient conditions (initially heart failure, acute myocardial infarction, and pneumonia, and subsequently also total lower extremity joint replacement and chronic obstructive pulmonary disease). Hospitals with higher readmission rates are penalized through reduced reimbursements. Assessments of the HRRP by race suggest show mixed results, with either narrowing9 or stable trends10,11 in Black-White 30-day readmission rates for targeted conditions after its introduction. However, analyses focused on safety-net hospitals have demonstrated widening racial disparities in readmissions over time.10 These varied findings reflect both the patient heterogeneity in these studies as well as multitude of prehospitalization and hospital factors that affect readmission risk.12
Clinically meaningful differences in risk-adjusted LOS between Black and White patients have been well-described.13,14 These differences may be partially the result of unobserved patient social factors15 and disease severity16 of Black compared to White patients, and differential treatment in hospital. However, whether racial differences in LOS are associated with the HRRP’s introduction is unknown. Given that on average Black patients had longer LOS than comparable White patients prior to the HRRP, it is possible that Black-White differences in adjusted LOS may narrow after the HRRP’s introduction. One possible reason is because providers may seek to invest time and resources in better discharge planning and care coordination during hospitalization to prevent readmissions. Although not directly policy relevant in terms of value-based payment models, such findings may counter concerns that these payment models worsen disparities in important health outcomes.17,18
To test this hypothesis, we assessed whether trends of Black-White differences in average adjusted length of stay (ALOS) changed after the introduction of the HRRP among Medicare-insured beneficiaries in New York, New Jersey, and Florida over the period 2009-2017 using a segmented regression approach (also known as interrupted time series approach [ITS]) stratified by the patient’s discharge destination. We focus on Black-White ALOS differences related to the HRRP given Black-White differences in outcomes have been well-described in the literature.
Methods
Data Source and Study Population
We created an analytical file of Medicare-insured (Fee-for-service, and Medicare Advantage) inpatient discharges from years 2009 to 2017 using the New York, Florida, and New Jersey State Inpatient Databases from the Health Cost and Utilization Project. The study cohort was restricted to Black and White hospitalized Medicare-insured adults with a medical or surgical diagnosis group (using a methodology described elsewhere that utilized the Centers for Medicare and Medicaid Services diagnosis-related grouping categorization),14 with LOS greater than or equal to 1 day who were discharged alive. We excluded patients who died during their hospitalization because we stratified our analysis by discharge destination (i.e., home vs non-home). We excluded discharges at non-acute care hospitals, hospitals which admitted only White or Black patients, and critical access hospitals. Hospitalizations with missing quarter of the year in which the patient was discharged, sex, median household income for patient’s ZIP code also were excluded. A flow diagram describing the exclusions by category and number is provided in the Supplement (eFigure 1).
Outcome, Study Variables, and Model
Our outcome was adjusted average length of stay (ALOS) stratified by discharge destination (home vs non-home). Our model was informed by a previously described conceptual model of factors influencing LOS.14 This conceptual framework highlights how patient demographic characteristics such as age, sex, race/ethnicity, their condition (both diagnoses and severity), as well as admission-related characteristics such as time of day of admission and type of admission (i.e., elective vs non-elective), hospital characteristics, and discharge disposition all influence patient LOS.
We employed several control variables. Sociodemographic characteristics included age at admission, sex, race (Black or White), and SES (defined using median household income for patient’s ZIP code, in quartiles). Disease-related characteristics included the number of chronic diseases, the diagnosis-related group (DRG) and Elixhauser-related mortality score (ERMS).19 To ensure consistency of ERMS through the change from ICD-9-CM to ICD-10-CM diagnosis versions in October 2015, ICD-10-CM Elixhauser Comorbidity Software, version 2018 was used. Other admission-related characteristics included the year-quarter, admission type (elective, emergency, or other), whether admission occurred on a weekend, and the discharge destination (home vs non-home [acute rehabilitation, skilled nursing facilities, long-term acute care hospitals]). We stratified our analysis by admissions discharged to home vs non-home destinations because discharge to non-home destinations may be related to LOS if a patient deconditioned during their hospitalizations, and required rehabilitation to regain premorbid function.
The HRRP initially applied to 3 conditions, acute myocardial infarction, heart failure, and pneumonia, which we categorized as targeted conditions. And all others were categorized as nontargeted conditions. Targeted admissions were identified using primary ICD-9-CM, ICD-10-CM diagnosis codes (Supplement).
The ALOS was calculated using generalized estimating equation model accounting for clustering within hospital to estimate robust empirical standard errors. The distribution of LOS is non-negative and right-skewed, and therefore a gamma distribution with log-link was specified. The predicted ALOS was then derived for each specific race and year-quarter. Our final model controlled for patient race, age, sex, SES, DRG, number of chronic diseases, ERMS, weekend admission, admission type. Independent variables in the models were checked for multicollinearity using variation inflation factors.
Statistical Analysis
We first examined characteristics of patient stays by race and discharge destination for 3 periods: January 2007 to March 2010 (pre-Affordable Care Act period), April 2010 to September 2012 (HRRP implementation period), and October 2012 to December 2017 (HRRP evaluation period)—consistent with previous HRRP analyses.20-22
Next, we calculated the Black-White differences in ALOS for each year quarter stratified by targeted and non-targeted conditions, and separately by discharge destination. For ease of interpretation at the hospital-level, the ALOS differences were calculated per 100 admissions. Trend lines for Black-White ALOS differences were then plotted using values from variance weighted linear regression. We analyzed the changes in trend the 3 time periods (pre-Affordable Care Act period, HRRP implementation period, HRRP evaluation period) using an ITS model with linear splines at cutoff points for each of the periods (2010/Q2 and 2012/Q4). A sensitivity analysis was conducted for each targeted condition using the same approach.
Analyses were performed using SAS statistical software, version 9.4 (SAS Institute, Cary, NC) and Stata, version 16 (StataCorp, College Station, TX). A 2-sided α of 0.05 was used to assess statistical significance. This research was approved by the institutional review board of Weill Cornell Medical College.
Results
Characteristics of Study Cohort
Table 1 describes the characteristics of the cohort by race and HRRP period stratified by discharge destination. In comparison of Black and White patients discharged to home and non-home regardless of HRRP period, White patients were on average older, had lower ERMS but more chronic conditions, had higher proportions of individuals living in high-income neighborhoods, and fewer emergency conditions.
Table 1.
Characteristics of Medicare-Insured Patients’ discharge by Race, and Period of Hospital Readmission Reduction Program in New York, New Jersey, and Florida (2009-2017).
| A. Patients discharged home. | ||||||
| Pre-ACA Q1/2009-Q2/2010 |
Implementation Q3/2010-Q3/2012 | Evaluation Q4/2012-Q4/2017 | ||||
| White | Black | White | Black | White | Black | |
| Admissions, N | 1,658,915 | 300,995 | 2,690,835 | 517,128 | 5,263,087 | 1,062,205 |
| Age, mean (sd) | 73.6 (12.4) | 65.6 (15.9) | 73.2 (12.7) | 65.2 (16.0) | 72.9 (12.5) | 65.2 (15.8) |
| Female, % | 52.9 | 58.8 | 53.0 | 58.6 | 52.0 | 57.6 |
| Income, % | ||||||
| Q1 | 20.6 | 54.5 | 20.5 | 53.1 | 20.2 | 52.4 |
| Q2 | 28.3 | 20.2 | 28.4 | 20.4 | 27.7 | 22.8 |
| Q3 | 25.8 | 17.7 | 26.0 | 18.3 | 27.3 | 16.1 |
| Q4 | 25.2 | 7.7 | 25.2 | 8.2 | 24.8 | 8.7 |
| Elixhauser-related mortality score, mean (sd) | 4.5 (8.2) | 4.7 (8.4) | 4.8 (8.5) | 4.9 (8.7) | 5.1 (8.9) | 5.4 (9.2) |
| Number of chronic conditions, mean (sd) | 5.8 (2.8) | 5.6 (2.8) | 6.1 (2.9) | 5.8 (2.9) | 6.9 (3.5) | 6.8 (3.5) |
| LOS, median (IQR) | 3 (2-6) | 4 (2-7) | 3 (2-6) | 4 (2-6) | 3 (2-6) | 4 (2-6) |
| Proportion of medical admissions, % | 72.2 | 82.0 | 73.8 | 82.7 | 73.1 | 82.5 |
| Proportion of surgical admissions, % | 27.8 | 18.0 | 26.2 | 17.3 | 26.9 | 17.5 |
| Targeted conditions, % | 11.4 | 11.8 | 10.8 | 10.8 | 11.0 | 11.6 |
| % with specific condition (denominator = targeted conditions) | ||||||
| AMI | 20.2 | 13.2 | 21.7 | 14.5 | 23.0 | 15.5 |
| Heart Failure | 49.4 | 64.9 | 46.6 | 62.5 | 48.0 | 63.5 |
| Pneumonia | 30.4 | 21.9 | 31.7 | 23.0 | 29.0 | 21.1 |
| Admission type, % | ||||||
| Elective | 21.0 | 11.7 | 20.1 | 11.2 | 19.9 | 10.3 |
| Emergency | 65.7 | 79.0 | 67.7 | 80.7 | 70.8 | 83.2 |
| Other | 13.3 | 9.2 | 12.2 | 8.1 | 9.4 | 6.5 |
| Proportion of weekend admissions, % | 18.9 | 21.2 | 19.3 | 21.6 | 20.0 | 22.2 |
| State, % | ||||||
| NY | 35.9 | 40.3 | 35.0 | 39.0 | 33.1 | 37.7 |
| NJ | 15.5 | 17.3 | 15.1 | 16.6 | 14.2 | 15.1 |
| FL | 48.6 | 42.4 | 49.9 | 44.5 | 52.7 | 47.2 |
| B. Patients discharged to non-home destinations | ||||||
| Pre-ACA Q1/2009-Q2/2010 | Implementation Q3/2010-Q3/2012 | Evaluation Q4/2012-Q4/2017 | ||||
| White | Black | White | Black | White | Black | |
| Admissions, N | 870,571 | 135,162 | 1,441,617 | 230,585 | 2,856,841 | 471,112 |
| Age, mean (std) | 79 (11.3) | 72.5 (14) | 78.8 (11.5) | 72.4 (14) | 78.5 (11.6) | 72.1 (13.7) |
| Female, % | 60.3 | 57.6 | 59.7 | 57.8 | 57.9 | 56.7 |
| Income, % | ||||||
| Q1 | 21.2 | 50.2 | 21.3 | 49.6 | 20.9 | 48.6 |
| Q2 | 28.0 | 21.9 | 28.0 | 21.6 | 27.4 | 24.1 |
| Q3 | 25.8 | 18.9 | 25.7 | 19.1 | 27.4 | 17.3 |
| Q4 | 25.0 | 9.1 | 25.0 | 9.7 | 24.3 | 10.0 |
| Elixhauser-related mortality score, mean (sd) | 7.8 (10) | 8.4 (10.2) | 8.2 (10.3) | 8.9 (10.6) | 8.7 (10.6) | 9.5 (11) |
| Number of chronic conditions, mean (sd) | 6.6 (3) | 6.5 (2.9) | 7 (3.1) | 7 (3.1) | 8 (3.6) | 8.2 (3.7) |
| LOS, median (IQR) | 5 (3-9) | 6 (4-11) | 5 (3-9) | 6 (4-11) | 5 (3-9) | 6 (4-11) |
| Proportion of medical admissions, % | 69.9 | 76.6 | 70.4 | 76.5 | 70.4 | 75.8 |
| Proportion of surgical admissions, % | 30.1 | 23.4 | 29.6 | 23.5 | 29.6 | 24.2 |
| Targeted conditions, % | 11.9 | 10.2 | 11.1 | 9.7 | 10.6 | 9.5 |
| % with specific condition (denominator = targeted conditions) | ||||||
| AMI | 23.9 | 19.6 | 23.5 | 20.1 | 22.7 | 20.1 |
| Heart Failure | 44.8 | 53.4 | 44.2 | 52.4 | 48.1 | 55.6 |
| Pneumonia | 31.3 | 27.0 | 32.3 | 27.4 | 29.2 | 24.3 |
| B. Patients discharged to non-home destinations | ||||||
| Pre-ACA Q1/2009-Q2/2010 | Implementation Q3/2010-Q3/2012 | Evaluation Q4/2012-Q4/2017 | ||||
| White | Black | White | Black | White | Black | |
| Admission type, % | ||||||
| Elective | 14.6 | 10.3 | 14.6 | 10.5 | 13.4 | 10.2 |
| Emergency | 74.9 | 80.9 | 75.1 | 81.9 | 78.7 | 84.1 |
| Other | 10.5 | 8.8 | 10.4 | 7.6 | 7.9 | 5.7 |
| Proportion of weekend admissions, % | 21.4 | 21.2 | 21.5 | 21.2 | 22.2 | 22.0 |
| State, % | ||||||
| NY | 35.1 | 40.6 | 33.6 | 39.2 | 31.8 | 37.3 |
| NJ | 21.4 | 21.8 | 21.3 | 22.1 | 19.8 | 21.0 |
| FL | 43.5 | 37.5 | 45.1 | 38.8 | 48.4 | 41.7 |
Abbreviations: ACA: Affordable Care Act; IQR: Inter-quartile range; LOS: Length of stay; sd: standard deviation.
Results From Interrupted Time Series Models
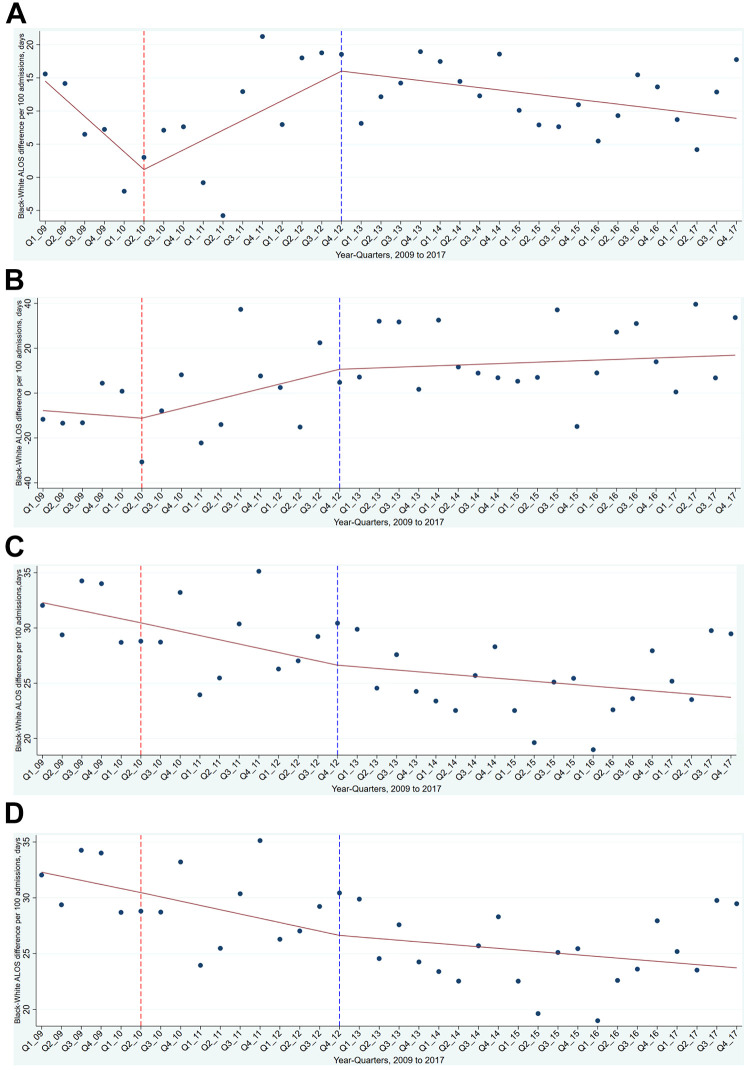
Table 2 shows trends in Black vs White ALOS differences over the 3 time periods of the HRRP. For patients with an HRRP-targeted condition discharged to home, pre-ACA trends suggest a significant decrease of 2.67 days per 100 admissions for each year-quarter (95% CI: −5.11 to −0.22, P = 0.03), implying that Black-White LOS disparities narrowed over this period. After the HRRP started, the trend increased to 1.48 days per 100 admissions (95% CI: 0.71 to 2.26, P < 0.001). Between the 2 periods, the change in slope was significant (Figure 1), representing a 4.15 day average adjusted LOS difference between Black and White patients per 100 admissions in each time quarter (95% CI: 1.19 to 7.11, P < 0.001). After the HRRP evaluation period began, Black-White differences decreased by 1.84 days per 100 admissions for every year-quarter (95% CI: −2.86 to −0.82, P < 0.001).
Table 2.
Rate of Change Over Year Quarters in Black-White Average Adjusted Length of Stay Differences per 100 Admissions for Targeted and Nontargeted Conditions, Stratified by Discharge Destination, 2009 to 2017, New York, New Jersey, and Florida.
| Outcome and time period1 | Targeted conditions | Non-targeted conditions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Home | Non-home | Home | Non-home | |||||||||
| Slope | 95% CI | P-value | Slope | 95% CI | P-value | Slope | 95% CI | P-value | Slope | 95% CI | P-value | |
| Pre-ACA | ||||||||||||
| Slope (95%CI) | −2.67 | −5.11 to −0.22 | 0.03 | −0.68 | −6.11 to 4.76 | 0.81 | −0.36 | −2.08 to 1.35 | 0.68 | −1.86 | −4.98 to 1.27 | 0.24 |
| Implementation | ||||||||||||
| Slope (95%CI) | 1.48 | 0.71 to 2.26 | <0.001 | 2.18 | 0.32 to 4.04 | 0.02 | −0.38 | −0.91 to 0.14 | 0.15 | 1.64 | 0.66 to 2.62 | <0.001 |
| Change in slope (Pre-ACA to Implementation period) | 4.15 | 1.19 to 7.11 | <0.001 | 2.86 | −3.85 to 9.58 | 0.40 | −0.02 | −2.08 to 2.04 | 0.99 | 3.50 | −0.28 to 7.27 | 0.07 |
| Evaluation period | ||||||||||||
| Slope (95%CI) | −0.36 | −0.71 to 0 | 0.05 | 0.31 | −0.55 to 1.18 | 0.48 | −0.15 | −0.4 to 0.1 | 0.26 | 0.01 | −0.47 to 0.48 | 0.98 |
| Change in slope (Implementation to Evaluation period) | −1.84 | −2.86 to −0.82 | <0.001 | −1.87 | −4.34 to 0.6 | 0.14 | 0.24 | −0.45 to 0.93 | 0.50 | −1.63 | −2.94 to −0.32 | 0.02 |
Abbreviation: ACA: Affordable Care Act.
1The pre-ACA period was from Q1 2009 through end of Q1 2010, the period of implementation of the HRRP was from start of Q2 2010 through end of Q2 2012, and the HRRP evaluation period was from start of Q3 2012 through end of Q4 2017.
Figure 1.
A, HRRP targeted conditions, discharge home. B, HRRP targeted conditions, discharge non-home. C, HRRP non-targeted conditions, discharge home. D, HRRP non-targeted conditions, discharge non-home. Trends in black-white average adjusted length of stay (ALOS) differences per 100 admissions for targeted and non-targeted conditions, stratified by discharge destination, 2009 to 2017, New York, New Jersey, and Florida. Points represent the average risk-adjusted length of stay (ALOS) differences between black and white patients during the yearly quarters. Solid lines represent the predicted ALOS differences calculated using weighted linear regression with linear splines at each change in time period: 2010/Q2, 2012/Q4. January 2007 through March 2010 was pre affordable care act period, April 2010 through September 2012 was the period of implementation, and October 2012 through December 2017 was evaluation period. Vertical lines indicate divisions between periods.
Among Medicare-insured patients with HRRP-targeted conditions discharged to non-home destinations, Black-White ALOS differences were not significantly different from the pre-ACA trend (2.86 days per 100 admissions in each year-quarter, 95% CI: −3.85 to 9.58). However, there was a 2.18 day difference (95% CI: 0.32 to 4.04, P = 0.02) in Black-White ALOS differences per 100 admissions during each year-quarter of HRRP implementation period. Furthermore, the change in trend between the HRRP implementation and evaluation periods was not statistically significant.
For HRRP non-targeted conditions, Black-White ALOS disparities for patients discharged home decreased over the 3 HRRP periods (Figure 1), with no statistically significant change in the slopes between either the pre-ACA and HRRP implementation period (−0.02 day difference per 100 admissions for each year-quarter, 95% CI: −2.08 to 2.04, P = 0.99) or the HRRP implementation to evaluation period (0.24 day difference per 100 admissions for each year-quarter, 95% CI: −0.45 to 0.93, P = 0.5). For discharges to non-home destinations with non-targeted conditions, the only significant difference in Black-White ALOS disparities was in the HRRP implementation period (1.64 day difference per 100 admissions for each year-quarter, 95% CI: 0.66 to 2.62, P < 0.001). There was a significant decrease in the change in slope between this period and the evaluation period (−1.63 day difference per 100 admissions for each year-quarter, 95% CI: −2.94 to −0.32, P = 0.02), suggesting that the effects on Black-White disparities were subsequently mitigated during the evaluation phase (Figure 1).
Results From Sensitivity Analysis
In sensitivity analyses for each of the 3 targeted conditions, the results for acute myocardial infarction and heart failure were consistent with our primary analysis. Patients with pneumonia who were discharged home had no significant change in trends between the 3 periods.
Discussion
In this study examining the effect of the HRRP on racial differences in ALOS from 2009 to 2017, we found that Black-White ALOS differences increased for patients with HRRP-targeted conditions who were discharged home after HRRP implementation, and then decreased to a lesser extent in the HRRP evaluation period. Overall, Black-White ALOS differences increased over the study period for patients admitted with HRRP-targeted conditions who were discharged to non-home destinations, and for those admitted with non-targeted conditions regardless of discharge destination.
This is the first study to explore the relationship between racial differences in LOS after the HRRP’s introduction. The 2 previous studies that examined this association found decreases in overall LOS after its introduction.23,24 Our findings contribute to the literature by identifying exacerbations of Black-White ALOS differences associated with the HRRP’s introduction for those admitted with targeted conditions. These differences were somewhat mitigated in the HRRP evaluation phase, although more so in patients who were discharged home. For patients with non-targeted conditions, Black-White ALOS differences continued to narrow across the 3 time periods for those discharged to home and non-home destinations (Figure 1C and 1D).
The ITS study design we employed exploits the quasi-experiment created by the introduction of HRRP, allowing for comparison of differences in LOS associated with race before and after the policy, that provides estimates indicative of changes in in-hospital treatment as a response to it. Furthermore, our model controlled for a number of demographic, disease, hospital, and admission-related factors which have been associated with LOS.14
There are 2 potential factors that may explain our findings. First, preventing readmissions require investment of time and resources in discharge planning in order to 1) achieve the necessary mobility and function to safely go home, 2) provide adequate follow-up, and 3) ensure a safe and supportive home environment. Therefore, the noted Black-White ALOS differences for HRRP-targeted conditions may have widened to account for appropriate discharge planning for Black patients compared to White patients. This may be especially relevant to patients discharged home compared to patients discharged to post-acute care settings such as skilled nursing facilities.
Second, the unobserved confounding related to individual social risk may explain these differences, particularly patients with targeted conditions who were discharged to non-home destinations. The addition of covariates reflecting increased social risk (e.g., income level, emergency Vs elective admissions) may explain greater variation in Black-White ALOS differences, leading to wider than expected differences. Critiques of the HRRP have demonstrated that hospitals serving higher numbers of non-White, rural, or dually eligible Medicare-Medicaid patients are disproportionately penalized.25,26 This led to peer-grouping as a method to stratify social risk by proportion of Medicare-Medicaid patients.27 However, further evaluation which explores racial differences in both adjusted LOS and adjusted readmission rates using Medicare fee-for-services claims data would be required to clarify this. In addition, an alternative explanation may be that our modeling strategy may not have adequately accounted for the variety of reasons why patients were discharged to non-home destinations compared to discharged to home, which include deconditioning28 and limited supports29 to allow for home-based convalescence.
It is important to note that for patients admitted with targeted conditions, trends in Black-White ALOS differences differed between the HRRP implementation and evaluation periods. The reasons for this are unclear and require further quantitative and qualitative research. As previously elsewhere, these observed changes may relate to hospitals’ inability to sustain improvements in readmission rates in the longer term for those discharged to home,22 but less so for those discharged to non-home destinations where continued engagement with post-acute care settings may be possible.30
There were 3 limitations to our study. First, our data are limited to 3 states. However, these are diverse states that represent over 10% of the US population. Second, we were unable to differentiate between Medicare FFS and Medicare Advantaged patients. The HRRP focused only on Medicare FFS patients. This may bias our results toward no effect. However, the results from a recent study suggest changes in readmission rates between these 2 groups are correlated in the context of the HRRP.31 Third, although the HCUP datasets have a rich source of variables describing disease, admission, hospital, and diagnosis-related factors of an individual admission, it is likely that other important socioeconomic factors that were not observed such as unemployment, social supports (e.g., marital status), and educational status contribute to role Black-White LOS differences.
Conclusions
In conclusion, we found widening LOS differences after the HRRP’s introduction, which narrowed somewhat in the evaluation phase, but only for HRRP-targeted conditions in patients discharged home. Given the growing literature on the association between longer LOS and increased risk of readmissions, future research should focus directly on whether the relative increase in LOS for Black Medicare patients admitted with targeted conditions limits or exacerbates their readmission risk.
Supplemental Material
Supplemental Material, sj-pdf-1-hme-10.1177_23333928211042454 for Association Between Racial Disparities in Hospital Length of Stay and the Hospital Readmission Reduction Program by Arnab K. Ghosh, Orysya Soroka, Martin Shapiro and Mark A. Unruh in Health Services Research and Managerial Epidemiology
Author Biographies
Arnab K. Ghosh, MD, MSc, MA, is an Assistant Professor of Medicine in the Department of Medicine at Weill Cornell Medical College.
Mark A. Unruh, PhD, MS, is an Associate Professor of Population Health Sciences in the Department of Population Health Sciences at Weill Cornell Medical College.
Orysya Soroka, MS, is a Senior Research Analyst in the Department of Medicine at Weill Cornell Medical College.
Martin Shapiro, MD, PhD, MPH, is a Professor of Medicine in the Department of Medicine at Weill Cornell Medical College.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr. Ghosh is supported by National Center for Advancing Translational Sciences (NCATS) grant KL2-TR-002385 of the Clinical and Translational Science Center at Weill Cornell Medical College.
ORCID iDs: Arnab K. Ghosh  https://orcid.org/0000-0002-5887-3301
https://orcid.org/0000-0002-5887-3301
Orysya Soroka  https://orcid.org/0000-0003-3282-2378
https://orcid.org/0000-0003-3282-2378
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Sud M, Yu B, Wijeysundera H C, et al. Associations between short or long length of stay and 30-day readmission and mortality in hospitalized patients with heart failure. JACC Heart Fail. 2017;5(8):578–588. [DOI] [PubMed] [Google Scholar]
- 2.Chopra I, Wilkins TL, Sambamoorthi U. Hospital length of stay and all-cause 30-day readmissions among high-risk Medicaid beneficiaries. J Hosp Med. 2016;11(4):283–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samsky MD, Ambrosy AP, Youngson E, et al. Trends in readmissions and length of stay for patients hospitalized with heart failure in Canada and the United States. JAMA Cardiol. 2019;4(5):444–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rachoin J-S, Aplin KS, Gandhi S, Kupersmith E, Cerceo E. Impact of length of stay on readmission in hospitalized patients. Cureus. 2020;12(9):e10669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blanchard JC, Rudin RS. Improving hospital efficiency through data-driven management: a case study of health first, Florida. Rand Health Q. 2016;5(4):2. [PMC free article] [PubMed] [Google Scholar]
- 6.Hauck K, Zhao X. How dangerous is a day in hospital? A model of adverse events and length of stay for medical inpatients. Med Care. 2011;49(12):1068–1075. [DOI] [PubMed] [Google Scholar]
- 7.Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605–611.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burke LG, Joyce N, Baker WE, et al. The effect of an ambulance diversion ban on emergency department length of stay and ambulance turnaround time. Ann Emerg Med. 2013;61(3):303–311.e1. [DOI] [PubMed] [Google Scholar]
- 9.Figueroa JF, Zheng J, Orav EJ, Epstein AM, Jha AK. Medicare program associated with narrowing hospital readmission disparities between black and white patients. Health Aff(Millwood). 2018;37(4):654–661. [DOI] [PubMed] [Google Scholar]
- 10.Chaiyachati KH, Qi M, Werner RM. Changes to racial disparities in readmission rates after Medicare’s hospital readmissions reduction program within safety-net and non–safety-net hospitals. JAMA Netw Open. 2018;1(7):e184154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandey A, Keshvani N, Khera R, et al. Temporal trends in racial differences in 30-day readmission and mortality rates after acute myocardial infarction among Medicare beneficiaries. JAMA Cardiol. 2020;5(2):136–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson S, Howie-Esquivel J, Vlahov D. Readmission risk factors after hospital discharge among the elderly. Popul Health Manag. 2012;15(6):338–351. [DOI] [PubMed] [Google Scholar]
- 13.Ghosh AK, Unruh MA, Soroka O, Shapiro M. Trends in medical and surgical admission length of stay by race/ethnicity and socioeconomic status: a time series analysis. Health Serv Res Manag Epidemiol. 2021;8:23333928211035581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghosh AK, Geisler BP, Ibrahim S. Racial/ethnic and socioeconomic variations in hospital length of stay: a state-based analysis. Medicine (Baltimore). 2021;100(20):e25976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8(6):621–628. [PubMed] [Google Scholar]
- 16.Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science. 2019;366(6464):447–453. [DOI] [PubMed] [Google Scholar]
- 17.Chen LM, Epstein AM, Orav EJ, Filice CE, Samson LW, Joynt Maddox KE. Association of practice-level social and medical risk with performance in the Medicare physician value-based payment modifier program. JAMA. 2017;318(5):453–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gu Q, Koenig L, Faerberg J, Steinberg CR, Vaz C, Wheatley MP. The Medicare hospital readmissions reduction program: potential unintended consequences for hospitals serving vulnerable populations. Health Serv Res. 2014;49(3):818–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fortin Y, Crispo JA, Cohen D, McNair DS, Mattison DR, Krewski D. External validation and comparison of two variants of the elixhauser comorbidity measures for all-cause mortality. PLoS One. 2017;12(3):e0174379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buhr RG, Jackson NJ, Kominski GF, Dubinett SM, Mangione CM, Ong MK. Readmission rates for chronic obstructive pulmonary disease under the hospital readmissions reduction program: an interrupted time series analysis. J Gen Intern Med. 2020;35(12):3581–3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salerno AM, Horwitz LI, Kwon JY, et al. Trends in readmission rates for safety net hospitals and non-safety net hospitals in the era of the US hospital readmission reduction program: a retrospective time series analysis using Medicare administrative claims data from 2008 to 2015. BMJ Open. 2017;7(7):e016149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543–1551. [DOI] [PubMed] [Google Scholar]
- 23.Mose JN, Kumar NK. The association between structural, performance, and community factors and the likelihood of receiving a penalty under the hospital readmissions reduction program (fiscal year 2013-2019). Health Equity. 2020;4(1):129–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayabakan S, Bardhan I, Zheng ZE. Triple aim and the hospital readmission reduction program. Health Serv Res Manag Epidemiol. 2021;8:2333392821993704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joynt Maddox KE, Reidhead M, Hu J, et al. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. Health Serv Res. 2019;54(2):327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaskin DJ, Zare H, Vazin R, Love D, Steinwachs D. Racial and ethnic composition of hospitals’ service areas and the likelihood of being penalized for excess readmissions by the Medicare program. Med Care. 2018;56(11):934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCarthy CP, Vaduganathan M, Patel KV, et al. Association of the new peer group-stratified method with the reclassification of penalty status in the hospital readmission reduction program. JAMA Netw Open. 2019;2(4):e192987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gill TM, Gahbauer EA, Han L, Allore HG. Functional trajectories in older persons admitted to a nursing home with disability after an acute hospitalization. J Am Geriatr Soc. 2009;57(2):195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewis ZH, Hay CC, Graham JE, Lin YL, Karmarkar AM, Ottenbacher KJ. Social support and actual versus expected length of stay in inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2016;97(12):2068–2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities. J Am Med Dir Assoc. 2017;18(1):30–34. [DOI] [PubMed] [Google Scholar]
- 31.Panagiotou OA, Voorhies KR, Keohane LM, et al. Association of inclusion of Medicare advantage patients in hospitals’ risk-standardized readmission rates, performance, and penalty status. JAMA Netw Open. 2021;4(2):e2037320. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-hme-10.1177_23333928211042454 for Association Between Racial Disparities in Hospital Length of Stay and the Hospital Readmission Reduction Program by Arnab K. Ghosh, Orysya Soroka, Martin Shapiro and Mark A. Unruh in Health Services Research and Managerial Epidemiology