Abstract
Background
There are global disparities in the provision of maternal health care, with women from rural communities and under‐resourced countries expecting poorer access to healthcare services. This potentially compounds the existing higher burden of maternal and neonatal morbidity within these populations. In this setting, point‐of‐care ultrasound (PoCUS) has the potential to improve outcomes while mitigating challenges and barriers associated with the introduction of new medical technology.
Objectives
To explore the availability and impact of PoCUS use for antenatal care (ANC) in under‐resourced settings.
Methods
Medline, Embase and Scopus were searched with no year limit. Studies were included if the participants were pregnant women undergoing ANC in a rural setting or developing country and if the intervention was PoCUS use or training.
Results
A total of 3863 unique articles were identified, with 17 meeting the inclusion criteria. Studies originated from Africa, Asia, Central America and Australia. All studies reported that POCUS use for ANC produced positive outcomes. PoCUS introduction into routine ANC resulted in higher antenatal attendance and reduced maternal and neonatal mortality rates. It was demonstrated that it was feasible to provide local healthcare workers with limited training to perform quality scanning and reporting in their clinics. Methods and measures of these three primary outcomes varied between studies.
Conclusion
Integration of PoCUS into ANC in the settings examined improved outcomes in under‐resourced areas. Further research should investigate the availability of PoCUS services at a country level, the clinical impact and economic feasibility.
Keywords: antenatal care, developing countries, obstetric ultrasound, point‐of‐care ultrasound (PoCUS), rural communities, under‐resourced
Introduction
Obstetric ultrasound has become an imperative component of ANC worldwide, with the World Health Organisation recommending that every pregnant woman should receive at least one ultrasound before 24 weeks of gestation.1 The Royal Australian and New Zealand College of Obstetrics and Gynaecology (RANZCOG) recommend for ultrasound examinations to be performed at 8–14 weeks, 18–20 weeks and 36 weeks.2 Best practice guidelines from the International Society of Ultrasound in Obstetrics and Gynaecology (ISUOG) advise ultrasound in the first trimester up to 13 + 6 weeks of gestation3 and mid‐trimester ultrasound between 18 and 22 weeks of gestation.4 Third‐trimester scans have become a part of a routine practice in some European countries as well.5 Antenatal ultrasound applications include gestational age, identification of multiple gestations, foetal development assessment, foetal anomaly detection and minimisation of labour induction..1, 2, 6
Despite the well‐documented benefits of antenatal care and ultrasound, there are global disparities in access. Women in under‐resourced countries are less likely to attend antenatal visits and access ultrasound services.6, 7, 8, 9 Disparities persist within countries, with rural communities less likely to access obstetric ultrasound compared to women living in urban settings.6, 7, 8, 9 These regions with reduced access to antenatal services are over represented in global burden of maternal and neonatal mortality, and therefore, service provision needs to be improved to allow equity in perinatal health outcomes.1, 9, 10 Ultrasound utilisation for women located in rural communities has the added benefit of aiding logistical arrangements.11 This may include allowing mothers to reach appropriate care in preparation for delivery or to be referred to a larger centre for pregnancy management in high‐risk cases.11
Barriers to women receiving adequate ANC in under‐resourced settings can be related to the service providers, the service users (pregnant women) and inequitable distribution of resources.12 Barriers include a large distance to services, scarcity of health professionals trained to use the services, a lack of cultural sensitivity by the service providers, limited accessibility to reach the services and the associated costs.12, 13, 14, 15 Common challenges to the introduction of new medical technology in under‐resourced settings can include the cost of the device, infrastructure such as a reliable electricity source, storage needs, ease of use and limited applications for use.11, 14 PoCUS has been demonstrated as a viable technology to mitigate these challenges due to the low outright and maintenance costs, portability, compact size, simple use, minimal requirements for use and the many potential applications.14, 16
The feasibility of PoCUS use in remote and under‐resourced settings has been demonstrated and intricacies reviewed.14, 16 Many studies in this area indicate that ANC is the most common use for PoCUS, and maternal care may improve significantly from the introduction of this technology.14, 15, 16, 17, 18, 19 The purpose of this scoping review is to examine the global scope of literature specifically regarding antenatal PoCUS in under‐resourced areas, such as developing countries and rural communities.
Methods
Identifying the research question
The research question developed to guide this scoping review was ‘What is the availability and impact of antenatal PoCUS services globally in low‐resource settings?’. This question was developed to produce a broad search strategy while remaining specific to antenatal services, PoC or compact ultrasound and low‐resource settings. The term ‘low resource’ was used to include communities disadvantaged due to rural location and communities in developing countries with transferable barriers to health care.
Identifying relevant studies
A systematic search was performed to identify the scope of the literature regarding availability, accessibility and utilisation of PoCUS for mothers undergoing ANC in regional and remote areas. The keywords used were ‘mother*’, ‘expectant’, ‘antenatal’, ‘maternal’, ‘pregan*’, ‘prenatal’, ‘obstetric’, ‘point of care ultrasound’, ‘PoCUS’, ‘point‐of‐care ultrasound’, ‘compact ultrasound’, ‘portable ultrasound’, ‘ultrasound’, ‘ultrasonography’, ‘sonography’, ‘availability’, ‘access’, ‘utilisation’, ‘impact’, ‘maternal health’, ‘neonatal health’, ‘developing countr*’, ‘regional’, ‘rural’, ‘remote’, ‘indigenous’, ‘limited resource’, ‘low resource’, ‘isolated’.
Keywords were applied in Medline, Embase and Scopus. The World Health Organization and other grey literature sources were searched, and a manual search of reference lists was undertaken; however, no additional studies were identified through this method. The last day of search was 18 August 2018.
Study selection
Studies were selected based on their participants, imaging equipment and outcomes.
Data were included if the participants were expectant mothers undergoing ANC in a regional, rural, remote or isolated setting. Studies were included if the type of antenatal imaging equipment used was described as point‐of‐care ultrasound, PoCUS, compact ultrasound and/or portable ultrasound. Studies were included if the outcomes addressed the impact on maternal and/or neonatal health, training, mortality, availability, accessibility or utilisation. Studies were excluded if they were not original publications or were not published in the English language.
From the initial search, duplicates were removed. Titles and abstracts were screened for eligibility based on the criteria above, and full texts of potentially included studies were retrieved and further assessed for eligibility. There were no exclusions due to the year of the study as the inclusion criteria yielded a small volume of relevant literature. Figure 1 details the selection process.
Figure 1.
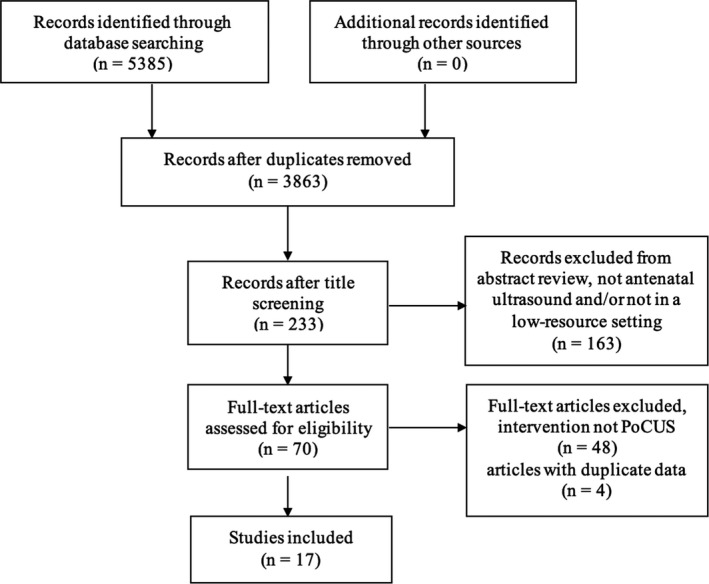
Flow Chart of Study Selection Assessing Antenatal PoCUS in a Low‐Resource Setting.
Charting the data
A purpose‐built Microsoft Excel sheet was used to extract relevant data from the selected studies including the authors, study design, setting, participants, type of PoCUS and the associated outcomes. This extracted data were further screened and were finally included if they addressed antenatal PoCUS use or antenatal PoCUS training in an under‐resourced setting. Table 1 provides an overview of the demographics of the 17 studies identified.
Table 1.
Characteristics of included studies
| Region | Study | Design | Setting | Participants | Aim |
|---|---|---|---|---|---|
| Africa | Amoah et al. (2017)36 | Survey preceding pilot project | Rural Ghana | Four communities | To evaluate the impact of mobile phones and POCUS implementation on ANC attendance |
| Cherniak et al. (2017)31 | Non‐blinded clustered randomised trial | Rural and isolated Uganda | Eight facilities | To determine the effectiveness of advertising POCUS on the uptake of ANC | |
| Mbuyita et al. (2015)24 | Prospective cohort | Rural Tanzania | 10 facilities | Determine the effects of introducing POCUS on the number of ANC visits | |
| Ross et al. (2014)30 | Retrospective data analysis pre‐post intervention | Rural Uganda | One facility | To determine the effect of introducing POCUS on ANC utilisation | |
| Kinnevey et al. (2016)28 | Prospective cross sectional | Rural Uganda | 12 midwives | Determine the cost of providing POCUS equipment and an antenatal POCUS training programme | |
| Greenworld et al. (2014)21 | Prospective cohort | Rural Mozambique | Nine nurses and clinical officers | To implement an obstetric ultrasound training programme | |
| Kimberly et al. (2009)22 | Prospective cohort | Rural Zambia | 21 midwives | To teach focused obstetric ultrasound to midwives using POCUS | |
| Vinayak et al. (2017)29 | Prospective cross sectional | Rural Kenya | Three midwives | To train midwives to perform basic obstetric POCUS | |
| Bentley, Hexom & Nelson (2015)26 | Prospective longitudinal | Urban Liberia | 31 midwives | To evaluate a POCUS curriculum | |
| Swanson et al. (2017)35 | Field action report | Rural Democratic Republic of the Congo | One facility | To identify the challenges of implementing antenatal POCUS in a rural study site | |
| Rulisa et al. (2016)25 | Prospective cross sectional | Urban Rwanda | 386 pregnant women | To evaluate the change in patient management with POCUS use for emergency obstetric conditions | |
| Central America | Crispin Milart et al. (2016)20 | Prospective cohort | Rural Guatemala | Three nurses | Impact of training and introducing POCUS on maternal and neonatal outcomes |
| Vyas et al. (2018)34 | Blinded investigational study | Rural Panama | Eight medical students (1st year) | Determine the feasibility of training medical students in ROUTE to perform POCUS | |
| Asia | Kozuki et al. (2016)23 | Prospective cohort | Rural Nepal | Three auxiliary nurse midwives | Determine the accuracy of training health workers to assess obstetric risk factors in homes using POCUS |
| Dalmacion et al. (2018)27 | Prospective cross sectional | Urban and rural Philippines | 20 community health workers | To determine the impact of POCUS on maternal and neonatal deaths | |
| Neufeld et al. (2009)33 | Randomised control trial | Rural Bangladesh | Nine paramedics | To determine the accuracy and precision of training paramedics to perform foetal biometry measurements using POCUS | |
| Australia | Glazebrook, Manahan & Chater (2005)32 | Pre‐post survey | Rural and remote Australia | 61 doctors | To evaluate a POCUS programme (obstetric and emergency medicine) |
Data collation, summary and reporting of findings
A total of 17 studies were included for content data analysis. Findings were categorised into continent regions and further analysed in terms of availability, accessibility, utilisation, patient and/or health professional perspectives, maternal outcomes, neonatal outcomes, mortality and training outcomes.
Results
The initial search yielded 3863 original results; however, 17 studies remained for inclusion after screening, as per the study protocol (see Figure 1). Majority of the results were observational studies, with 7 prospective cohort studies,20, 21, 22, 23, 24, 25, 26 3 cross‐sectional studies27, 28, 29 and 1 retrospective data analysis.30 Other study designs included a non‐blinded clustered randomised control trial,31 a pre‐post survey,32 a randomised control trial,33 a blinded investigational study,34 a field action report35 and a survey followed by a pilot project.36
Variables between studies included the country, setting, study design and the type of PoCUS used. Studies were categorised into continent regions for analysis to allow differences in results between country settings to be identified. The findings were further grouped and categorised by outcome. Table 2 summarises the outcomes of the included studies.
Table 2.
Summary of scoping review results
| Region | Type of POCUS for ANC intervention | Studies | Population | Outcomes | |||
|---|---|---|---|---|---|---|---|
| Knowledge and skills | Utilisation | Patient outcomes | Other outcomes | ||||
| Africa | Utilisation of ANC | Amoah et al. (2017)36 | Four communities | ↑ Antenatal attendance | Less likely to have a miscarriage or practice self ‐medication | ↑ Hospital deliveries | |
| Cherniak et al. (2017)31 | Eight facilities | ↑ Antenatal attendance | |||||
| Mbuyita et al. (2015)24 | 10 facilities |
= Attendance of ANC once ↑ Four or more antenatal visits |
↑ Referrals to higher facilities | ||||
| Ross et al. (2014)30 | One facility |
↑ Antenatal attendance ↑ Antenatal interventions provided |
|||||
| Training | Kinnevey et al. (2016)28 | 12 midwives | Minimal comfort levels in management of diagnoses pre‐training | Cost for providing a health facility with training and equipment is $6888 ‐$8288 | |||
| Greenworld et al. (2014)21 | Nine nurses and clinical officers | Equal detection rates of multiple conditions between trainees scanning alone and under supervision | |||||
| Kimberly et al. (2009)22 | 21 midwives |
↑ OSCE scores at 2 months ↑ OSCE scores at 6 months |
↑ Change in clinical management | ||||
| Vinayak et al. (2017)29 | Three midwives | High reporting accuracy | |||||
| Bentley, Hexom and Nelson (2015)26 | 31 midwives |
↑ Comfort levels ↑ OSCE scores ↑ Test scores immediately post‐training ↓ Test scores 1 year post‐training |
|||||
| Swanson et al. (2017)35 | One facility | Challenges include equipment security, electricity, servicing, ordering supplies and engaging health care workers | |||||
| Patient outcomes | Rulisa et al. (2016)25 | 386 pregnant women | ↑ Change in clinical management | ||||
| Central America | Training | Vyas et al. (2018)34 | Eight medical students (1st year) | High reporting accuracy | |||
| Patient outcomes | Crispin Milart et al. (2016)20 | Three nurses |
↓ Maternal mortality ↓ Neonatal mortality |
↑ Referrals to higher facilities | |||
| Asia | Training | Kozuki et al. (2016)23 | Three auxiliary nurse midwives |
High reporting accuracy High inter‐rater reliability |
|||
| Dalmacion et al. (2018)27 | 20 community health workers | High reporting accuracy |
↓ Maternal mortality ↓ Neonatal mortality |
||||
| Neufeld et al. (2009)33 | Nine paramedics | Acceptable intra‐ and inter‐ observer errors | |||||
| Australia | Training | Glazebrook, Manahan & Chater (2005)32 | 61 doctors |
↑ Test scores ↑ Self‐rated confidence and expertise |
|||
↑ statistically significant increase, ↓ statistically significant decrease, = no significant change.
Africa
Africa was the region with the largest volume of literature, with 11 studies identified.21, 22, 24, 25, 26, 28, 29, 30, 31, 35, 36 Common themes explored included the utilisation of ANC, clinical knowledge and skills and patient outcomes.
Utilisation of ANC
Four observational studies reporting on the utilisation of ANC demonstrated the association between the implementation of PoCUS services and ANC attendance.24, 30, 31, 36 These studies used variable measures of outcome such as ANC attendance, service utilisation or the number of ANC interventions administered.
Amoah et al.36 used a pilot test to evaluate the implementation of low‐cost mobile phones and PoCUS in four rural Ghana communities. At least, one community health worker (CHW) was equipped and trained in PoCUS use per community.36 One hundred women who had been pregnant in the previous 5 years completed an initial pre‐pilot survey to serve as a baseline for comparison, and 323 pregnant women were followed throughout their pregnancy as the pilot study.36 The implementation resulted in a statistically significant increase in ANC utilisation and hospital deliveries.36 It was also indicated that CHW's can be easily equipped with PoCUS as part of a prenatal care approach, allowing quality ANC to be accessible to women in rural communities.36
Cherniak et al.31 explored the relationship between advertising the availability of PoCUS and ANC attendance in a non‐blinded clustered randomised control trial. Eight rural sub‐counties of Uganda were included, with four rural sub‐counties of Uganda randomised to a control arm (advertisement of ANC without POCUS mention) and four sub‐counties randomised to different interventions (advertisements of ANC with PoCUS).31 The interventions included a PoCUS word of mouth advertisement, a PoCUS word of mouth advertisement with ANC radio advertisement, and word of mouth and radio advertisement of both ANC and PoCUS.31 The ANC attendance rate was highest when PoCUS was mentioned in both radio advertisement and word of mouth advertisement, and was significantly higher than in the control communities (rate of attendance was 65.1 per 1000 pregnant women compared to 11.1 per 1000 pregnant women in the control).31
Mbuyita et al.24 used a cohort study to investigate the effects of introducing PoCUS on the utilisation of ANC services and healthcare facility deliveries. Ten health facilities in a rural district of Tanzania were selected, with five as control facilities and five facilities receiving POCUS equipment and training.24 Two hundred and fifty‐seven pregnant women were surveyed across the ten facilities to generate comparative data.24 The introduction of PoCUS did not result in a statistically significant change among women attending ANC services at least once; however, an increase in the percentage of women attending ANC clinic four times or more (27.2% to 60.3%) was observed.24 There was also an increase in referrals made to higher facilities, due to the additional detection of abnormal conditions using PoCUS.24
Ross et al.30 retrospectively analysed the total number and rate of ANC interventions and attendance, prior to and after the implementation of PoCUS at a clinic in rural Uganda. Data of anti‐parasitic treatment, HIV testing, intermittent preventive therapy for malaria and iron and folate provision were used for analysis.30 The implementation of PoCUS was associated with an increase in ANC attendance and an increase in the number of antenatal interventions provided.30 The increase in antenatal interventions is potentially beneficial to the maternal and neonatal health of the community; however, longitudinal studies are required to validate this hypothesis.
Training‐ clinical knowledge and skills
Five observational studies from Africa reporting on PoCUS training were identified.21, 22, 26, 28, 29 These studies investigated the current clinical skills and/or outcomes of introducing antenatal PoCUS training and services in rural clinics. Variable measures of outcomes were used including the clinicians’ self‐rated knowledge, reporting accuracy compared to the trainers and observed structured clinical examinations (OSCE).
Kinnevey et al.28 used a cross‐sectional design to investigate the cost of providing 12 midwives from different rural Ugandan health facilities with PoCUS equipment and a 6‐week antenatal PoCUS training programme. The total cost of equipping a powered rural facility was $6888 USD ($3669 for training and $3219 for a Mindray DP‐10) and a non‐powered site was $8288, as additional costs were required to maintain the service using solar power.28 A pre‐training self‐assessment survey was administered to assess the prior ultrasound knowledge of the midwives and the nature of their clinics.28 The self‐assessed scores ranged between ‘not at all comfortable’ and ‘somewhat comfortable’ in 9 of 11 selected diagnoses, with higher scores in understanding the clinical significance than management of diagnoses.28 Combined the midwives managed over 6700 ANC visits with a low referral rate (3.2%), demonstrating that midwives were the primary physicians responsible for management of care28.
Greenworld et al.21 evaluated the effectiveness of an 8‐week obstetric ultrasound training programme using a cohort study in rural Mozambique. Nine nurses and clinical officers were trained using one week of lectures, 7 weeks of practical training and 10 months of remotely supported scanning.21 The study compared the results of the trainees scanning under supervision of the trainer and scanning alone.21 The detection rates of twin pregnancies, breech presentations, transverse presentations and placenta previa cases were similar between the two groups, while the detection of foetal anomalies was higher when the trainees were scanning under supervision.21
Kimberly et al.22 used a cohort study to evaluate an obstetric PoCUS training programme and the change in clinical management with PoCUS use in rural Zambia. Twenty‐one midwives were trained with 2 h of interactive teaching followed by 3 weeks of supervised scanning at the beginning of the programme, the 2‐month mark and the 6‐month mark.22 An OSCE demonstrated that the midwives had an improvement at both the 2‐month (69% improvement) and 6‐month mark (83%).22 About 16.5% of the total scans performed by the midwives prompted a change in a patient's clinical management, including increased antenatal visits and referral to a larger facility.22
Vinayak et al.29 assessed the feasibility of training rural midwives in obstetric PoCUS and mobile phone transmission technology, by conducting a cross‐sectional study in rural Kenya. Three midwives were trained over a 4‐week period utilising online modules, lectures, practical training and scanning under direct supervision.29 The midwives’ competency was assessed through a test upon completion of the online modules and an exit examination, where 100% was required to pass.29 Two hundred and seventy‐one pregnant women were independently scanned by the three midwives, and the images produced were electronically sent for evaluation.29 The reporting accuracy of the midwives’ images was 99.63%, and only one discrepancy was found between trainee and evaluator reporting.29
Bentley et al.26 evaluated an obstetric PoCUS training curriculum using a prospective cohort study in Liberia. Thirty‐one midwives underwent a 1‐week programme including a theoretical, practical and supervised scanning components.26 The training programme was evaluated using a pre‐post survey of comfort levels using PoCUS, a post‐training test to assess the midwives’ knowledge and an OSCE.26 Fourteen midwives were retained for a longitudinal evaluation at 1 year.26 There was a statistically significant increase in test scores, comfort levels using ultrasound and OSCE results between the pre‐workshop scores and post‐workshop scores; however, the test scores showed decreased knowledge at the one‐year evaluation (36.6% pre‐training, 90% post‐training and 66% 1‐year evaluation).26
Training—challenges
Swanson et al.35 was the only study identified to directly analyse the challenges associated with the implementation of antenatal PoCUS. The key challenges associated with training nurses, midwives and clinical officers in a 2‐week course and providing PoCUS equipment were identified in a field action report from the rural Demographic Republic of the Congo segment35 of the ‘First Look Ultrasound Study’.37 The security of the equipment and providing an electricity source were easily corrected challenges, using solutions such as locking the equipment and providing solar panels.35 Servicing the machines provided a greater challenge as the PoCUS unit needed to be shipped to the manufacturers to manage repairs, proving to be costly and timely.35 Limited supplies, such as ultrasound gel and paper towels for cleaning the gel, were required but necessitated bulk ordering and planning.35 Engaging healthcare workers for training and to provide PoCUS scanning in their clinic was a challenge as it required structural and workflow change.35 The challenge of ensuring ample patients were presenting to the clinic on days of training was negated by notifying women in advance.35
Patient outcomes
Two observational studies from Africa were identified which reported on the impact of antenatal PoCUS implementation on patient outcomes.25, 36 The intervention used, and outcome measures varied between both studies.
The study by Amoah et al.36 has been further described previously in terms of ANC attendance and the increase with the introduction of PoCUS. The survey also demonstrated that women who attended ANC were less likely to have a miscarriage or practice self‐medication and were more likely to have a hospital delivery.36
Rulisa et al.25 used a cohort study to prospectively review PoCUS use for emergency obstetric conditions in a Rwandan tertiary hospital and the impact on patient management. All obstetric patients admitted over a 4‐month period were categorised by their pre‐ and post‐PoCUS diagnosis severity.25 Three hundred and eighty‐six obstetric patients were admitted, and all received PoCUS assessment.25 Nine patients with an initially benign pre‐scan diagnosis were changed to a life‐threatening diagnosis post‐scan.25 Twelve patients’ classification changed from moderate to severe post‐scan.25 Six patients were scanned for analysis of foetal well‐being and were diagnosed with placenta previa post‐scan.25
Central America
Two of the identified studies were from Guatemala, Central America.20, 34 A prospective cohort study analysed the impact of antenatal PoCUS training on clinical outcomes,20 while a blinded investigational study evaluated the effectiveness of an antenatal PoCUS training programme.34
Crispin Milart et al.20 addressed the impact of training nurses in and introducing PoCUS on maternal and neonatal outcomes by conducting an observational study in the rural districts of Guatemala. Three nurses were trained using a 1‐week programme and provided with a prenatal care kit comprised of PoCUS equipment and dried blood screening tests.20 These nurses attended 762 pregnant women as the intervention group.20 A control group of 747 pregnant women received care from the community facilitator, as per common practice in this area.20 Five maternal deaths were reported in the control group (two from post‐partum haemorrhage and three due to external causes), whereas no maternal deaths were reported in the intervention group.20 A 64% reduction in neonatal mortality rate was observed in the intervention group in comparison with the control group.20 Seventy women were referred to higher facilities for management in the intervention group due to conditions detected by ultrasound, including foetal malpresentation (66%), multiple gestation, placenta previa and amniotic fluid problems.20
Vyas et al.34 used a blinded investigational study to train eight‐first‐year medical students from the University of California in the Rural Obstetrical Ultrasound Triage Exam (ROUTE), to perform ANC using PoCUS in rural Panama. Sixty pregnant women in their second or third trimesters were scanned in the study, where biparietal diameter, head circumference, foetal presentation and placental location were measured.34 Upon review by an experienced obstetric physician, the students correctly assessed biparietal diameter in 95.3% of cases and head circumference in 90.0% of cases.34 This suggests that healthcare workers with limited PoCUS training can utilise ROUTE to screen for high‐risk conditions in pregnant women in low‐resource settings.34
Asia
Three of the included studies were from Asia, all reporting on the effectiveness of training health workers from rural communities in obstetric PoCUS.23, 27, 33 All studies used a comparison between the trainees’ reporting and the reviewers’ reporting; however, the methods used and outcomes varied.23, 27, 33
Kozuki et al.23 evaluated the accuracy of training health workers in Nepal to assess obstetric risk factors using PoCUS in a cohort study. Three auxiliary nurse midwives were provided with two 1‐week ultrasound trainings one‐month apart, comprised of lectures, demonstrations and supervised scanning.23 No test of competency was used pre‐ or post‐training.23 Home visits were provided to 804 pregnant women in their third trimester, where two auxiliary nurse midwives examined each woman to calculate inter‐rater reliability.23 Sensitivity, specificity, positive and negative predictive values were between 90 and 100% for the three auxiliary nurse midwives.23 For cases of multiple gestation, there was 100% agreement with the auxiliary nurse midwives and the sonogram reviewers.23
Dalmacion et al.27 used a cross‐sectional study to analyse the maternal and neonatal outcomes associated with training 20 community healthcare workers (six doctors, five nurses and nine midwives) in antenatal PoCUS at an urban and rural site in the Philippines. Pre‐post tests were used to assess the training; however, the only results reported from this testing was that training outcomes did not differ between the two locations.27 Four hundred and sixty women were scanned, with 31.7% showing abnormal findings (most commonly foetal malpresentation 124/146).27 PoCUS utilisation potentially averted 6.3% maternal deaths and 14.6% neonatal deaths at the time of delivery.27 About 95% agreement was measured between the readings produced by the trainees and the trainers.27
As a component of a larger randomised intervention trial, Neufeld et al.33 investigated the accuracy and precision of training paramedics to perform foetal biometry measurements using PoCUS in rural Bangladesh. Nine paramedics from different clinics received a 6‐week training course consisting of general ultrasound theory, technique training and practical experience.33 One hundred and eighty women were scanned by the participants and then the study supervisor to determine accuracy and precision of the trainees’ results.33 Intraobserver error of the paramedics’ measurements ranged from 0.97 mm (mean standard deviation) for first‐trimester biparietal diameter to 7.25 mm for the abdominal circumference in the third trimester.33 Interobserver error ranged from 0.00 mm for femur diaphysis length to 3.36 mm for abdominal circumference in the third trimester.33 All measurement errors were within the specified acceptable range.33
Australia
One study specific to antenatal PoCUS in a rural setting was identified from Australia.32 Glazebrook et al.32 used a pre‐ and post‐workshop questionnaire to evaluate an obstetric and emergency medicine PoCUS programme provided to 61 rural or remote Australian doctors. A 2‐day workshop was provided in four Australian states consisting of lectures and practical experience with PoCUS use.32 The questionnaire consisted of a self‐rated confidence level section and a knowledge test section (multiple choice and true or false questions).32 A statistically significant increase in knowledge was observed by the test and the self‐rated confidence and expertise in intermediate obstetric ultrasound by the participants.32 All participants had varying degrees of previous knowledge and clinical experience in PoCUS; therefore, it is difficult to draw precise conclusions.32
Discussion
This is one of limited reviews to analyse antenatal PoCUS use in rural communities and under‐resourced settings. While there is a volume of literature regarding antenatal ultrasound implementation, the associated benefits and the barriers in developing countries, there is minimal literature specific to antenatal PoCUS.
All studies which addressed the utilisation of ANC demonstrated that the introduction of PoCUS produced a statistically significant increase in pregnant women attending and utilising ANC services.24, 30, 31, 36 Each study used different interventions and methods, with Cherniak et al.31 providing the most robust results exploring the effects of different methods of advertisement. The utilisation of PoCUS, and in turn ANC, was influenced by the mother's awareness of this technology, and therefore, the advertisement method largely influenced results produced. Increased ANC attendance and ANC interventions can improve maternal and neonatal outcomes, and therefore, PoCUS introduction can potentially produce benefits by association as well as primary outcomes from the scan (e.g. identification of anomalies). Longitudinal investigations of maternal and neonatal health of the community are required to validate this hypothesis.
The clinical skills and performance of healthcare workers following limited antenatal PoCUS training was the most commonly investigated outcome, with six studies from Africa,21, 22, 26, 28, 29, 35 one study from Central America,31 three studies from Asia23, 27, 33 and one from Australia.32 This totals 11 of the 17 included studies. There were many differences between the training provided including the participants, the duration of the training programme and the measurement tools (see Table 3).
Table 3.
Training programme differences
| Study | Participants | Training duration | Measurement tools |
|---|---|---|---|
| Kinnevey et al. (2016)28 | 12 midwives | 6 weeks | Pre‐training self‐assessment survey |
| Greenworld et al. (2014)21 | Nine nurses and clinical officers | 8 weeks | Compared detection rates of conditions when trainees scanning under supervision of the trainer and scanning alone (10 month period) |
| Kimberly et al. (2009)22 | 21 midwives | 9 weeks | OSCE to measure ultrasound ability and skill retention (at 2 months and 6 months) |
| Vinayak et al. (2017)29 | Three midwives | 4 weeks | Agreement between the readings produced by the trainees and the trainers |
| Bentley et al. (2015)26 | 31 midwives | 1 week |
Test and survey—pre, post and one year OSCE—post and one year |
| Crispin Milart et al. (2016)20 | Three nurses | 1 week | Maternal and neonatal morbidity rates |
| Vyas et al. (2018)34 | Eight medical students (1st year) | Not specified | Agreement between the readings produced by the trainees and the trainers |
| Kozuki et al. (2016)23 | Three auxiliary nurse midwives | 2 weeks | Sensitivity and specificity measures between two participants’ results of the same patient |
| Dalmacion et al. (2018)27 | 20 community health workers | 78 h | Agreement between the readings produced by the trainees and the trainers |
| Neufeld et al. (2009)33 | Nine paramedics | 6 weeks | Agreement between the readings produced by the trainees and the trainers |
| Glazebrook et al. (2005)32 | 61 doctors | 2 days | Pre‐post knowledge questionnaire |
A standardised method of training evaluation should be used in the future to allow accurate comparison of results. Some studies did not directly assess the participants knowledge post‐training, creating difficulties in accurate assessment of the effectiveness of the programme. In all instances, it would be beneficial to evaluate the training programme provided in addition to reporting the further outcomes associated with antenatal PoCUS implementation to contribute to increasing the literature on this topic. An OSCE would provide the most structured evidence; however, this may not be achievable in under‐resourced settings as it would require additional time and planning. A pre‐post survey provides less robust evidence; however, it can be a more feasible method. There is also the opportunity for qualitative feedback provided by the participants in a survey, in terms of what staff would prefer or require in the training specific to their practice. Follow‐up of the participants and evaluation of reporting is especially beneficial to ensure the post‐training outcomes are reflected in clinical practice.
It is evident on reflection of results that the sustainability of skills was associated with access to PoCUS equipment. In studies which provided the trainees with equipment, skills were maintained and developed upon follow‐up,22 whereas in studies where the trainees had limited access to equipment, skills were degraded26 (but still higher than pre‐training). The transient nature of staff posed an additional challenge, as when the trained staff move this resource was lost for the community.38 PoCUS training of permanent healthcare workers in these rural communities should be prioritised and include incentives to maintain these staff.38 This can include ensuring that the equipment is well functioning, adequate service pathways are in place, and there is support from larger centres.38
Further research should focus on the sustainability of skills and to longitudinally evaluate the impact on clinical outcomes as a result of the training and PoCUS introduction into routine ANC. All 11 studies provided evidence that training local healthcare workers to utilise POCUS for ANC was feasible and effective. The primary physicians responsible for the management and administration of ANC in the community should be the staff trained to provide the best utilisation of PoCUS. The value of antenatal PoCUS use should be maximised by providing a referral path for the management of mothers requiring a higher level of care.
There is no literature worldwide detailing the availability of PoCUS services within countries or the utilisation of these services. This review clearly demonstrates that PoCUS for ANC can directly influence the identification, diagnosis and treatment of conditions associated with maternal and neonatal morbidity in under‐resourced settings.20, 25, 27 As explained previously, women in rural communities and developing countries suffer worse pregnancy outcomes, and yet, these are the regions with the least provision of services.1, 9, 10 Implementation of PoCUS equipment, training and additional services to ensure sustainability is extremely cost‐effective (as explored by Kinnevey et al.) and does not present significant technical and logistical challenges (as explored by Swanson et al.). It is unacceptable that preventable maternal and neonatal deaths are occurring on a global scale, especially in countries where the funding for this simple and effective solution is available. Resource allocation and funding for PoCUS need to be addressed by governing bodies to improve the current inequitable health status. Further research may involve the availability of PoCUS or obstetric ultrasound services on a country level to document and highlight the inequities in service provision to provide evidence for government funding.
Conclusion
Antenatal PoCUS implementation in rural and under‐resourced communities can result in an increased uptake of ANC service utilisation and reduce maternal and neonatal morbidity. With limited training, local healthcare workers can accurately determine gestational age, number of gestations and identify foetal anomalies in all trimesters. Challenges for service implementation include electricity supply and establishing pathways for equipment servicing and maintenance. PoCUS is an exceptionally cost‐effective method of providing quality ANC to pregnant women to improve outcomes in areas with minimal facilities. Further studies should investigate producing an ideal standardised method of obstetric PoCUS training, longitudinally evaluating the maintenance of skills developed from training, evaluating the direct impact on clinical outcomes as a result of service provision, the availability of PoCUS services and an ideal method for increasing utilisation of PoCUS when the service is available.
Authorship declaration
The authorship listing conforms with the journal's authorship policy. All authors are in agreement with the content of the submitted manuscript.
Disclosure statement
No financial support was received for this review. There are no potential conflicts of interest.
Acknowledgements
This paper is component of a larger project funded by The Hospital Research Foundation. Many thanks to members of this project Eva Bezak PhD, FACPSEM and Amber Bidner BN, BMRS for their assistance in shaping the review.
References
- 1.World Health Organisation . WHO recommendations on antenatal care for a positive pregnancy experience. Luxembourg: WHO Press; 2016. [PubMed] [Google Scholar]
- 2.RANZCOG . Standards of maternity care in Australia and New Zealand. East Melbourne: RANZCOG Publications; 2016. p. 1–35. [Google Scholar]
- 3.Salomon LJ, Alfirevic Z, Bilardo CM, Chalouhi GE, Ghi T, Kagan KO, et al. ISUOG practice guidelines: performance of first‐trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 2013; 41: 102–13. [DOI] [PubMed] [Google Scholar]
- 4.Salomon LJ, Alfirevic Z, Berghella V, Bilardo C, Hernandez‐Andrade E, Johnsen SL, et al. Practice guidelines for performance of the routine mid‐trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 2010; 37: 116–26. [DOI] [PubMed] [Google Scholar]
- 5.Agence Nationale d'Evaluation et d'Accréditation en Santé . L’échographie obstétricale au cours de la grossesse en l'absence de facteur de risque. Service des Recommandations et Références Professionnelles, pp. 1–80, Décembre 1998. Paris. As quoted in: https://www.jogc.com/article/S1701-2163(16)34094-4/pdf
- 6.Sippel S, Muruganandan K, Levine A, Shah S. Review article: use of ultrasound in the developing world. Int J Emerg Med 2011; 4: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rijken MJ, Lee SJ, Boel ME, Papageorghiou AT, Visser GH, Dwell SL, et al. Obstetric ultrasound scanning by local health workers in a refugee camp on the Thai‐Burmese border. Ultrasound Obstet Gynecol 2009; 34: 395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finlayson K, Downe S. Why do women not use antenatal services in low‐ and middle‐income countries? A meta‐synthesis of qualitative studies. PLoS Med 2013; 10: e1001373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wanyonyi SZ, Mariara CM, Vinayak S, Stones W. Opportunities and challenges in realizing universal access to obstetric ultrasound in Sub‐Saharan Africa. Ultrasound Int Open 2017; 3: E52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stanton K, Mwanri L. Global maternal and child health outcomes: the role of obstetric ultrasound in low resource settings. World J Prev Med 2013; 1: 22–9. [Google Scholar]
- 11.Ahman A, Kidanto HL, Ngarina M, Edvardsson K, Small R, Mogren I. ‘Essential but not always available when needed’ – an interview study of physicians’ experiences and views regarding use of obstetric ultrasound in Tanzania. Glob Health Action 2016;9:31062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matsuoka S, Aiga H, Rasmey LC, Rathavy T, Okitsu A. Perceived barriers to utilization of maternal health services in rural Cambodia. Health Policy 2010; 95: 255–63. [DOI] [PubMed] [Google Scholar]
- 13.Reeve C, Banfield S, Thomas A, Reeve D, Davis S. Community outreach midwifery‐led model improves antenatal access in a disadvantaged population. Aust J Rural Health 2016; 24: 200–6. [DOI] [PubMed] [Google Scholar]
- 14.Harris RD, Marks WM. Compact ultrasound for improving maternal and perinatal care in low‐resource settings: review of the potential benefits, implementation challenges, and public health issues. J Ultrasound Med 2009; 28: 1067–76. [DOI] [PubMed] [Google Scholar]
- 15.Shah S, Bellows BA, Adedipe AA, Totten JE, Backlund BH, Sajed D. Perceived barriers in the use of ultrasound in developing countries. Crit Ultrasound J 2015; 7: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Becker DM, Tafoya CA, Becker SL, Kruger GH, Tafoya MJ, Becker TK. The use of portable ultrasound devices in low‐ and middle‐income countries: a systematic review of the literature. Trop Med Int Health 2016; 21: 294–311. [DOI] [PubMed] [Google Scholar]
- 17.Adler D, Mgalula K, Price D, Taylor O. Introduction of a portable ultrasound unit into the health services of the Lugufu refugee camp, Kigoma District, Tanzania. Int J Emerg Med 2008; 1: 261–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kolbe N, Killu K, Coba V, Neri L, Garcia KM, McCulloch M, et al. Point of care ultrasound (POCUS) telemedicine project in rural Nicaragua and its impact on patient management. J Ultrasound 2015; 18: 179–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rijken MJ, Mulder EJ, Papageorghiou AT, Thiptharakun S, Wah N, Paw TK, et al. Quality of ultrasound biometry obtained by local health workers in a refugee camp on the Thai‐Burmese border. Ultrasound Obstet Gynecol 2012; 40: 151–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crispin Milart PH, Diaz Molina CA, Prieto‐Egido I, Martinez‐Fernandez A. Use of a portable system with ultrasound and blood tests to improve prenatal controls in rural Guatemala. Reprod Health 2016; 13: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenwold N, Wallace S, Prost A, Jauniaux E. Implementing an obstetric ultrasound training program in rural Africa. Int J Gynaecol Obstet 2014; 124: 274–7. [DOI] [PubMed] [Google Scholar]
- 22.Kimberly HH, Murray A, Mennicke M, Liteplo A, Lew J, Bohan JS, et al. Focused maternal ultrasound by midwives in rural Zambia. Ultrasound Med Biol 2010; 36: 1267–72. [DOI] [PubMed] [Google Scholar]
- 23.Kozuki N, Mullany LC, Khatry SK, Ghimire RK, Paudel S, Blakemore K, et al. Accuracy of home‐based ultrasonographic diagnosis of obstetric risk factors by primary‐level health care workers in rural Nepal. Obstet Gynecol 2016; 128: 604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mbuyita S, Tillya R, Godfrey R, Kinyonge I, Shaban J, Mbaruku G. Effects of introducing routinely ultrasound scanning during Ante Natal Care (ANC) clinics on number of visits of ANC and facility delivery: a cohort study. Arch Public Health 2015; 73: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rulisa S, Rurangwa T, Lewis K, Small M. Point of care ultrasound use for emergency obstetric and gynecological conditions in a tertiary care hospital in Rwanda. Ultrasound Obstet Gynecol 2016; 48: 262–3. [Google Scholar]
- 26.Bentley S, Hexom B, Nelson BP. Evaluation of an obstetric ultrasound curriculum for midwives in Liberia. J Ultrasound Med 2015; 34: 1563–8. [DOI] [PubMed] [Google Scholar]
- 27.Dalmacion GV, Reyles RT, Habana AE, Cruz LMV, Chua MC, Ngo AT, et al. Handheld ultrasound to avert maternal and neonatal deaths in 2 regions of the Philippines: an iBuntis(R) intervention study. BMC Pregnancy Childbirth 2018; 18: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kinnevey C, Kawooya M, Tumwesigye T, Douglas D, Sams S. Addressing obstetrical challenges at 12 rural Ugandan health facilities: findings from an international ultrasound and skills development training for midwives in Uganda. IJMA 2016; 5: 46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vinayak S, Sande J, Nisenbaum H, Nolsoe CP. Training midwives to perform basic obstetric point‐of‐care ultrasound in rural areas using a tablet platform and mobile phone transmission technology‐a WFUMB COE project. Ultrasound Med Biol 2017; 43: 2125–32. [DOI] [PubMed] [Google Scholar]
- 30.Ross AB, DeStigter KK, Coutinho A, Souza S, Mwatha A, Matovu A, et al. Ancillary benefits of antenatal ultrasound: an association between the introduction of a low‐cost ultrasound program and an increase in the numbers of women receiving recommended antenatal treatments. BMC Pregnancy Childbirth 2014; 14: 424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cherniak W, Anguyo G, Meaney C, Kong LY, Malhame I, Pace R, et al. Effectiveness of advertising availability of prenatal ultrasound on uptake of antenatal care in rural Uganda: a cluster randomized trial. PLoS ONE 2017; 12: e0175440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Glazebrook R, Manahan D, Chater AB. Evaluation of an ultrasound program (intermediate obstetric and emergency medicine) for Australian rural and remote doctors. Aust J Rural Health 2005; 13: 295–9. [DOI] [PubMed] [Google Scholar]
- 33.Neufeld LM, Wagatsuma Y, Hussain R, Begum M, Frongillo EA. Measurement error for ultrasound fetal biometry performed by paramedics in rural Bangladesh. Ultrasound Obstet Gynecol 2009; 34: 387–94. [DOI] [PubMed] [Google Scholar]
- 34.Vyas A, Moran K, Livingston J, Gonzales S, Torres M, Duffens A, et al. Feasibility study of minimally trained medical students using the Rural Obstetrical Ultrasound Triage Exam (ROUTE) in rural Panama. World J Emerg Med 2018; 9: 216–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Swanson D, Lokangaka A, Bauserman M, Swanson J, Nathan RO, Tshefu A, et al. Challenges of implementing antenatal ultrasound screening in a rural study site‐ a case study from the Democratic Republic of the Congo. GHSP 2017; 5: 315–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Amoah B, Anto EA, Osei PK, Pieterson K, Crimi A. Boosting antenatal care attendance and number of hospital deliveries among pregnant women in rural communities: a community initiative in Ghana based on mobile phones applications and portable ultrasound scans. BMC Pregnancy Childbirth 2016; 16: 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McClure EM, Nathan RO, Saleem S, Esamai F, Garces A, Chomba E, et al. First look: a cluster‐randomized trial of ultrasound to improve pregnancy outcomes in low income country settings. BMC Pregnancy Childbirth 2014; 14: 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hayman NE, White NE, Spurling GK. Improving Indigenous patients’ access to mainstream health services: the Inala experience. MJA 2009; 190: 604–6. [DOI] [PubMed] [Google Scholar]


