Abstract
Background
The aim of this study was to assess the effects of loneliness, belongingness and other modifiable factors on psychological distress and wellbeing and whether the effects of COVID-19 modulated these relationships.
Methods
The current study reported on 1217 participants aged 18 years or older who completed an online survey from 28 to 31 March 2020. Survey measures included demographic characteristics; exposure to COVID-19; impact of COVID-19 on employment, finance, and work and social adjustment; loneliness, thwarted belongingness, and health behavior changes as modifiable factors. Outcome measures were psychological distress and wellbeing.
Results
Linear regression models revealed that COVID-19 related work and social adjustment difficulties, financial distress, loneliness, thwarted belongingness, eating a less healthy diet poorer sleep and being female were all associated with increased psychological distress and reduced wellbeing (p < 0.05). Psychological distress was more elevated for those with high difficulties adjusting to COVID-19 and high levels of thwarted belongingness (p < 0.005). Similarly, as COVID-19 related work and social adjustment difficulties increased, wellbeing reduced. This was more pronounced in those who felt lower levels of loneliness (p < 0.0001). Other interactions between COVID-19 impacts were observed with gender and poorer diet for psychological distress and cigarette use, age and gender for wellbeing (p < 0.05).
Limitations
The study was cross-sectional, preventing causal interpretation of the relationships.
Conclusion
Modifiable factors, age and gender had significant impacts on psychological distress and wellbeing. Public health and policy approaches to improving social, economic and lifestyle factors may mitigate the negative mental health effects of the pandemic and its restrictions.
Keywords: COVID-19, Belongingness, Health behaviors, Loneliness, Psychological distress, Wellbeing
1. Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has necessitated many practices to prevent or minimize viral transmission. Preventative measures to reduce infection included implementing good hygiene practices, physical distancing, quarantine measures and isolating those already infected (World Health Organization, 2020a). In addition, public health measures were enacted in many countries to minimize viral transmission including travel restrictions, shutting down non-essential services, stay-at-home orders or “lockdowns”, and the cancelation of social gatherings and events (Ritchie et al., 2020)). In Australia, these restrictions were gradually introduced between the 22nd and 30th March 2020. They included closing international borders and all non-essential services; however, essential services such as supermarkets, pharmacies, medical care, and restaurants and cafes that provided takeaway and home delivery could remain open (Campbell and Vines, 2021)(). Schools transitioned to online home learning, workplace distancing was introduced (e.g., working from home arrangements), and social gatherings were restricted to two people (Campbell and Vines, 2021, Storen and Corrigan, 2020)().
Whilst critical to reduce transmission, the strict measures employed to reduce the spread of COVID-19 have led to marked changes in modifiable health behaviors. Both positive and negative changes in sleep, physical activity, food intake, cigarette use, and alcohol consumption were self-reported in the early stages of COVID-19 lockdowns during April/May 2020 in Europe (Cancello et al., 2020; Rossinot et al., 2020). Similarly, an increase in alcohol consumption was found when compared to that of previous years in a US longitudinal survey of adults (Pollard et al., 2020). A UK based survey also found a 5.2% increase in high risk drinking during the lockdown period in May 2020 when compared with measures from 2016 to 2018 (Daly and Robinson, 2020). Many studies have also reported changes to other modifiable health behaviors such as reductions in physical activity (Cheval et al., 2020; Rossinot et al., 2020; Visser et al., 2020; Werneck et al., 2020) and dietary changes, with studies reporting mixed findings for the impact on diet (Rossinot et al., 2020; Visser et al., 2020).
The COVID-19 pandemic and associated lockdowns have resulted in significant social and economic consequences (Nicola et al., 2020). In particular, social connectedness is a factor that is highly likely to have been impacted by the enforced restrictions during the COVID-19 pandemic. Social connectedness is an overarching concept encompassing both belongingness and loneliness. Belongingness refers to the need to belong, based on experiences of social interactions, while loneliness is a subjective feeling of having less social contact than one wants. Some early evidence has emerged on the impact of lockdowns on social connectedness. For example, being under a stay-at-home order in the US was associated with increased perceptions of loneliness (Tull et al., 2020), while higher perceived loneliness in the early stages of the pandemic in Spain was associated with higher levels of psychological distress (Losada-Baltar et al., 2020).
Both health behaviors and social connectedness are strongly interconnected with mental health. Public health messaging during COVID-19 has focused on promoting protective factors and minimizing risk factors to promote and support mental health (World Health Organization, 2020b). There has been a dramatically greater focus on the mental health effects of COVID-19 in the literature compared with previous outbreaks of Ebola and H1N1 (Maalouf et al., 2021). Many studies including those using representative samples have shown that psychological distress, anxiety, worry, and depression were elevated at the start of the pandemic (Dawel et al., 2020; Ettman et al., 2020; Fisher et al. 2020; McGinty et al., 2020; Tull et al., 2020). A US study showed that symptoms of depression were three fold higher in April 2020 compared to pre-pandemic levels (Ettman et al., 2020). Increased psychological distress has also been observed, owing largely to the major personal, health, and other changes that have occurred due to the pandemic (Hollingue et al., 2020).
To date, most research has focused on mental health outcomes of the pandemic and the associated lockdowns, with fewer studies considering the potential impact that specific health behaviors performed during this time could have on mental health (Arora and Grey, 2020). During the pandemic, increased symptoms of depression and anxiety were associated with alcohol consumption in Australia (Tran et al., 2020), while a US study found that psychological distress was related to alcohol use being more evident in females (Rodriguez et al., 2020). Further, poorer mental health during COVID-19 was shown to be associated with negative changes in diet, sleep and physical activity (Rossinot et al., 2020), while increases in physical inactivity and TV viewing were associated with poorer mental health (Cheval et al., 2020; Werneck et al., 2020). These results are not surprising given the clear associations observed between health behaviors and mental health prior to COVID-19.
Prior to COVID-19, a wealth of research has shown associations between modifiable health behaviors and mental health. Clinical treatment guidelines for mood disorders recommend lifestyle interventions in addition to psychological therapies, medications and procedures to treat mental illness (Manger, 2019). Various lifestyle factors have been demonstrated to be associated with improved mental health outcomes (Velten et al., 2014). Evidence has shown that in non-clinical populations, depression and anxiety can be reduced by physical activity programs (Rebar et al., 2015). Results for dietary interventions are less conclusive with mixed effects on depression and anxiety symptoms (Firth et al., 2019). Further, the cessation of smoking is associated with improved mental health (Taylor et al., 2014).
Strong associations of social connectedness with mental health also exist. Perceptions of loneliness are associated with increased mortality (Leigh-Hunt et al., 2017), corresponding to a 26% increased likelihood of death (Holt-Lunstad et al., 2015). In addition, consistent evidence has shown that social isolation and loneliness are associated with depression, anxiety, phobias, suicide and dementia (Leigh-Hunt et al., 2017; Solmi et al., 2020). Similarly, in a longitudinal study social connectedness was a stronger predictor of mental health than mental health was of social connectedness, suggestive of a causative effect (Saeri et al., 2018).
The COVID-19 pandemic provides a unique time to investigate the association of health behaviors and social connections with mental health in the context of a universal stressor. Although few studies to date have used representative samples, it is clear that mental health has deteriorated during the early stages of COVID-19 and health behavior and social connections have been impacted. The current study intends to build on the existing research by investigating which specific health behaviors enacted during lockdowns promote or impede mental health using a representative sample. We were particularly interested in identifying modifiable factors, which could be used to guide public health messaging to support the mental health of the population during similar challenging times. Therefore, the aim of this study was to assess the effects of loneliness, feelings of belonging, physical activity, social activity, diet, sleep, cigarette use and alcohol consumption on the outcomes of psychological distress and wellbeing in a representative community sample. To determine which sub-groups were most affected by the direct and indirect impacts of COVID-19 we examined interactions between COVID-19 exposures with modifiable behaviors and demographic variables (age and gender) on psychological distress and wellbeing. The findings from this study will be useful in informing the development of interventions and strategies to improve mental health and wellbeing during the ongoing COVID-19 crisis and in other catastrophic events.
2. Methods
2.1. Participants and procedure
Participants were recruited between 28 and 31 March 2020. To contextualize this time period in Australia, physical distancing of 1.5 m between people was required and all non-essential gatherings were banned (20th March). During the week commencing 22nd March 2020 public venues (e.g., pubs/bars, sporting venues, cinemas) were closed with restaurants and cafes offering takeaway or home delivery only, schools were closed for all except children of essential workers and travelers encouraged to return and stay home. On 29th March 2020 mandatory quarantining for overseas travelers was enforced, on 30th March public gatherings were reduced to two people with everyone remaining at home unless shopping for essentials, exercising or traveling for work/education and public non-essential venues closed and on 30th March a payment was announced to support jobs and businesses affected by COVID-19 (Campbell and Vines, 2021)().
Participants were recruited through Qualtrics Research Service (QRS), which used quota sampling to obtain a representative sample of the Australian population on the basis of age group, gender, and geographical location (State/Territory). Participants received a detailed description of the study and provided written informed consent online prior to completing a survey that took approximately 30 min to complete. Ethical approval to conduct this survey was obtained from the Australian National University Human Research Ethics Committee (protocol: 2020/152). A total of 1217 participants were included in the current study. Table 1 reports on the sample characteristics. Participant characteristics aligned well with population data from the Australian Bureau of Statistics (Australian Bureau of Statistics, 2016), demonstrating that a representative sample of the Australian community was achieved.
Table 1.
Sample characteristics.
| Female (n = 613) | Male (n = 602) | Total (n = 1215) | Gender difference | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n (%) or M (SD) | n (%) or M (SD) | n (%) or M (SD) | χ2 or F | p | |||||
| COVID-19 impacts | COVID-19 employment impact | 158 | (25.8%) | 137 | (22.8%) | 295 | (24.3%) | 1.50 | 0.2200 |
| COVID-19 financial distress | 209 | (34.1%) | 186 | (30.9%) | 395 | (32.5%) | 1.42 | 0.2342 | |
| COVID-19 exposure | 11 | (1.8%) | 25 | (4.2%) | 36 | (3.0%) | 5.88 | 0.0154 | |
| WSAS score | 21.00 | (8.67) | 20.39 | (9.70) | 20.70 | (9.19) | 1.30 | 0.2544 | |
| Modifiable factors | Less physical activity | 320 | (52.2%) | 275 | (45.7%) | 595 | (49.0%) | 5.17 | 0.0230 |
| (More physical activity) | 126 | (20.6%) | 108 | (17.9%) | 234 | (19.3%) | |||
| Less social activity | 507 | (82.7%) | 465 | (77.2%) | 972 | (80.0%) | 5.67 | 0.0173 | |
| (More social activity) | 44 | (7.2%) | 60 | (10.0%) | 104 | (8.6%) | |||
| Poorer diet | 200 | (32.6%) | 114 | (18.9%) | 314 | (25.8%) | 29.70 | <0.0001 | |
| (Improved diet) | 117 | (19.1%) | 127 | (21.1%) | 244 | (20.1%) | |||
| Less sleep | 242 | (39.5%) | 156 | (25.9%) | 398 | (32.8%) | 25.37 | <0.0001 | |
| (More sleep) | 109 | (17.8%) | 130 | (21.6%) | 240 | (19.8%) | |||
| More alcohol | 107 | (17.5%) | 101 | (16.8%) | 208 | (17.1%) | 0.10 | 0.7539 | |
| (Less alcohol) | 104 | (17.0%) | 127 | (21.1%) | 231 | (19.0%) | |||
| (Non-drinker) | 202 | (33.0%) | 142 | (23.6%) | 344 | (28.3%) | |||
| More cigarettes | 39 | (6.4%) | 60 | (10.0%) | 99 | (8.1%) | 5.27 | 0.0217 | |
| (Fewer cigarettes) | 30 | (4.9%) | 54 | (9.0%) | 84 | (6.9%) | |||
| (Non-smoker) | 450 | (73.4%) | 397 | (65.9%) | 847 | (69.7%) | |||
| Loneliness | 2.93 | (1.85) | 2.96 | (1.77) | 2.95 | (1.81) | 0.10 | 0.7469 | |
| Thwarted belongingness | 3.05 | (1.28) | 3.22 | (1.25) | 3.13 | (1.27) | 5.04 | 0.0249 | |
| Demographics | Age | 42.53 | (15.60) | 49.01 | (18.13) | 45.74 | (17.20) | 44.67 | <0.0001 |
| Years of education | 14.59 | (1.77) | 14.62 | (1.76) | 14.60 | (1.77) | 0.10 | 0.7496 | |
| Have partner | 407 | (66.4%) | 396 | (65.8%) | 803 | (66.1%) | 0.05 | 0.8212 | |
| Live alone | 73 | (11.9%) | 73 | (12.1%) | 146 | (12.0%) | 0.01 | 0.9072 | |
| Outcomes | Psychological distress | 11.50 | (4.93) | 10.28 | (4.83) | 10.90 | (4.92) | 19.08 | <0.0001 |
| Wellbeing | 43.94 | (22.91) | 51.72 | (23.87) | 47.80 | (23.70) | 33.60 | <0.0001 | |
2.2. Measures
2.3.1. Psychological distress
A primary outcome of this study was psychological distress. This was measured using the Distress Questionnaire-5 (DQ5), a five-item self-rating scale reporting distress in the past 30 days (Batterham et al., 2016). An example of an item is ‘My worries overwhelmed me’. For the purpose of this study, we were interested in reports of distress over the last 2 weeks. Items were rated on a scale of 1–5 (‘Never’ to ‘Always’), generating a total score between 5 and 25, with higher scores indicating greater psychological distress. The scale had very good internal consistency in the current study sample (α = 0.92).
2.3.2. Wellbeing
The second primary outcome was subjective wellbeing measured using the 5-item World Health Organization Wellbeing Index (WHO-5) (Topp et al., 2015). It consists of 5 positively framed items assessing feelings of wellbeing over the past 2 weeks (e.g., ‘I have felt calm and relaxed’). Items were rated on a scale of 0–5 (‘At no time’ to ‘All of the time’), with total raw scale scores ranging between 0 and 25. These were multiplied by 4 to convert the scale from 0 (worst imaginable wellbeing) to 100 (best imaginable wellbeing), based on scoring guidelines (Topp et al., 2015). The scale had very good internal consistency (α = 0.91).
2.3.3. COVID-19 exposure and impact measures
Four separate measures were used to examine the direct impacts of COVID-19 on the sample. Firstly, exposure to SARS-CoV-2 was assessed through a series of yes/no items that assessed whether the respondent (i) had been diagnosed with COVID-19, (ii) was awaiting test results for COVID-19, (iii) knew of a family member that had been diagnosed with COVID-19, or (iv) had been in direct contact with someone diagnosed with COVID-19. Participants who endorsed any of these four items were classified as having exposure to COVID-19.
Second, the impact of COVID-19 on financial distress was assessed using the single item ‘Over the last 2 weeks, to what extent have you experienced financial distress related to COVID-19?’. Participants responded to this item on a 6-point Likert-type rating scale ranging from 1 ‘Not at all’ to 6 ‘Extremely’, with responses of 4 ‘Quite a lot’ or greater classified as in financial distress.
Third, the impact of COVID-19 on employment was determined by (i) being forced to reduce hours, (ii) losing their job as a result of COVID-19 (iii) being forced to take paid leave, or (iv) being forced to take unpaid leave. Participants who endorsed any of these four items were classified as having their employment adversely impacted due to COVID-19.
Fourth, to examine work and social impacts of COVID-19, scores on the Work and Social Adjustment Scale (WSAS) (Mundt et al., 2002) were used. For the WSAS, participants rated the level of impairment COVID-19 had caused (8-point Likert-type rating from 1 ‘Not at all impaired’ to 8 ‘Very severely impaired’) for five work and social domains (ability to work, home management, social leisure activities, private leisure activities, and ability to form and maintain close relationships). The scale had adequate internal consistency (α = 0.73).
2.3.4. Modifiable factors
Loneliness was measured over the past 2 weeks using the 6-item De Jong Gierveld Loneliness Scale (De Jong Gierveld and Van Tilburg, 2006). Items assessed emotional loneliness (e.g., ‘I experience a general sense of emptiness’) and social loneliness (e.g., ‘There are plenty of people I can rely on when I have problems’ (reverse coded)). Responses were recorded on a 5-point scale. Based on the scoring protocol, positive scores and negative scores were collapsed into a single category with the neutral response option counted as a positive for emotional loneliness and a negative for social loneliness. Higher scores indicated greater feelings of loneliness, ranging from 0 to 6, with adequate internal consistency (α = 0.72).
Feelings of belonging over the past 2 weeks were measured using the thwarted belongingness subscale of the Interpersonal Needs Questionnaire (Van Orden et al., 2012). The scale consists of 9 items (e.g., ‘I feel disconnected from other people’) that are rated on a 7-point Likert rating scale from 1 ‘Not at all true for me’ to 7 ‘Very true for me’. A total score was based on mean item response ranging from 1 to 7, with higher scores indicative of greater levels of thwarted belonging. The scale had very good internal consistency (α = 0.89).
Health behavior change over the past two weeks was assessed using the question ‘Over the last 2 weeks, how has the amount you did the following things changed?’, with respondents asked to indicate changes in being physically active, being social, eating a healthy diet, getting good quality sleep, drinking alcohol and smoking cigarettes. Response options were recorded on a 5-point scale (1 ‘I did a lot less’ to 5 ‘I did a lot more’) or not applicable. For the purposes of analysis, responses were collapsed into doing less (lot less/less) for the active, social, diet and sleep variables, and more (lot more/more) for the alcohol and cigarette variables. Those who did not report an increase or had a “not applicable” response for alcohol/cigarette use (non-users) were coded as not doing more of these behaviors.
2.3.5. Demographic factors
The following demographic factors were also measured: age (in years); gender (male/female/other/prefer not to say); years of education estimated from highest educational attainment; partner status (yes/no); and living alone (yes/no). Ethnicity was measured using 12 non-exclusive indicators, with the majority (73%) identifying only as Caucasian, similar to the Australian population.
2.4. Statistical analysis
Statistical analyses were conducted using SPSS v26 (IBM Corp, Chicago IL, USA) with alpha set at 0.05. In addition to descriptive analyses, linear regression analyses were performed to investigate the relationship between the independent variables and the two outcome measures, psychological distress (DQ-5) and wellbeing (WHO-5). Independent variables included in the model were the COVID-19 exposure and impact measures, demographic characteristics (age, gender, education, living alone and having a partner) and modifiable risk factors (loneliness, belonging and the six health behavior change items). Treatment coding was used to generate regression coefficients reported in the tables. Two-way interactions between COVID-19 impacts and each modifiable factor (and age and gender) were performed by adding interaction terms using a forward stepwise approach (from 44 candidate interaction terms, with continuous variables centered to ensure they were interpretable). Direction and relationship of significant interactions were determined graphically.
3. Results
3.1. Characteristics of the sample
The characteristics of the 1215 participants included in this study are reported in Table 1. Male participants were on average older than female participants (49 ± 18 vs 43 ± 16, respectively, p < .0001). There were no gender differences for the impact of COVID-19 on employment, financial distress or work and social adjustment; however more males reported exposure to COVID-19 (this included themselves or family member being diagnosed with COVID-19, awaiting test results or having been in direct contact with someone with COVID-19). Generally, the self-reported change toward less physical activity, less social activity, and less sleep was greater than the change toward healthier behaviors (more physical activity, more social activity, more sleep) during the past 2 weeks. More females than males reported reduced physical activity, social activity, diet and sleep over the past 2 weeks. Of those who drank alcohol, similar numbers reported an increase or decrease in consumption over the past 2 weeks. Most of the sample did not smoke. Of those who did, more males reported an increase in cigarette use over the past 2 weeks compared to females. Loneliness was similar for males and females while more males reported higher levels of thwarted belonging as compared to females.
3.2. Factors associated with psychological distress
Table 1 reports the mean for psychological distress in this sample. Linear regression was performed to investigate and adjust for the impacts of COVID-19 and modifiable factors on psychological distress. The final model (n = 1217) accounted for 51% of the variance in the sample (Table 2 ). COVID-19 variables alone explained 28% of variance, adding modifiable factors explained a further 20% of variance (Δ R2: p < .001), and demographic variables explained a further 3% of variance (Δ R2: p < .001) for a total of 51% of variance explained. Adding the interaction terms also significantly increased variance explained by 1%. Participants that were younger and female were more likely to have higher levels of psychological distress. Financial distress and difficulty adjusting to work and social life changes due to COVID-19 were significantly associated with elevated psychological distress.
Table 2.
Factors associated with psychological distress.
| Standard estimate | SE | p | ||
|---|---|---|---|---|
| COVID-19 impacts | COVID-19 employment impact | −0.0026 | 0.2629 | 0.9087 |
| COVID-19 financial distress | 0.2385 | 0.3178 | <0.0001 | |
| COVID-19 exposure | −0.0254 | 1.0613 | 0.4880 | |
| WSAS score | 0.1860 | 0.0151 | <0.0001 | |
| Modifiable factors | Less physical activity | 0.0290 | 0.2218 | 0.1995 |
| Less social activity | −0.0220 | 0.2815 | 0.3365 | |
| Poorer diet | 0.0491 | 0.2720 | 0.0428 | |
| Less sleep | 0.1325 | 0.2351 | <0.0001 | |
| More alcohol | 0.0379 | 0.2836 | 0.0816 | |
| More cigarettes | 0.0650 | 0.4082 | 0.0043 | |
| Loneliness | 0.2248 | 0.0772 | <0.0001 | |
| Thwarted belongingness | 0.2155 | 0.1088 | <0.0001 | |
| Demographics | Age | −0.1174 | 0.0068 | <0.0001 |
| Male gender | −0.0589 | 0.2495 | 0.0205 | |
| Years of education | −0.0310 | 0.0571 | 0.1311 | |
| Have partner | 0.0211 | 0.2373 | 0.3561 | |
| Live alone | −0.0424 | 0.3444 | 0.0628 | |
| Significant interaction terms | COVID-19 exposure x Gender | 0.0917 | 1.2826 | 0.0134 |
| (COVID-19 impact x other) | WSAS score x Thwarted belongingness | 0.0617 | 0.0086 | 0.0046 |
| WSAS score x Poorer diet | −0.0683 | 0.0261 | 0.0077 | |
| COVID-19 financial distress x Gender | −0.0760 | 0.4306 | 0.0161 |
Standard Error (SE); Work and Social Adjustment Scale (WSAS).
Increased loneliness and reduced feelings of belonging were significantly associated with increased levels of psychological distress. Other modifiable factors shown to be associated with increased psychological distress included eating a less healthy diet, reduced quality of sleep and smoking more cigarettes.
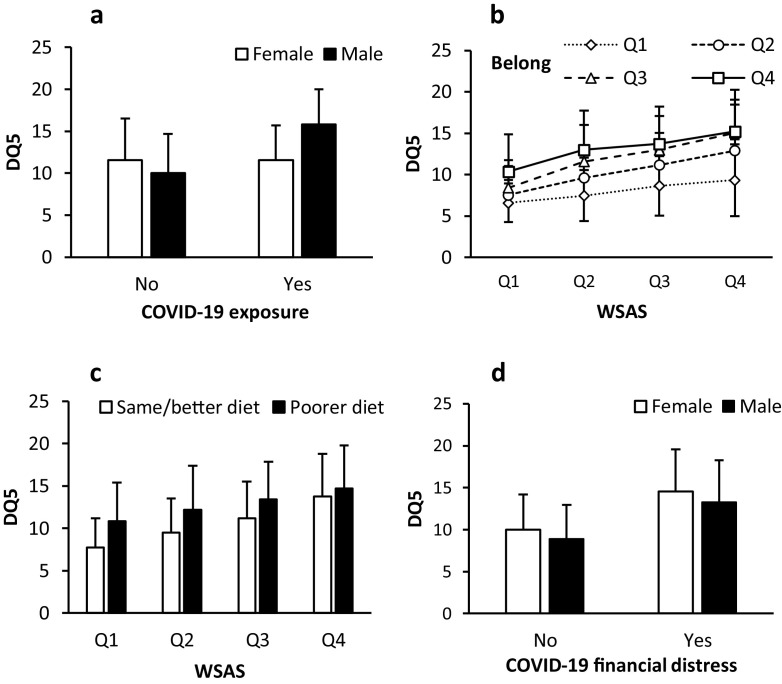
To investigate the effects of COVID-19 on psychological distress in greater detail and to determine which sub-populations were more likely to be affected, interactions between COVID-19 measures and modifiable factors, age and gender were tested. Table 2 displays the significant interactions that were revealed by the analyses. First, Fig. 1 a direct exposure to COVID-19, through self or family diagnosis, awaiting test results or direct contact with someone with the virus was associated with higher levels of psychological distress in males but not females. Second, psychological distress was most elevated for those with high WSAS scores and high thwarted belongingness. This is illustrated in Fig. 1b, based on quartiles for WSAS scores and thwarted belongingness for ease of interpretation. The relationship was less pronounced when minimal work and social adjustment difficulties were experienced or if participants felt reduced levels of thwarted belongingness. Also interacting with WSAS score was a less healthy diet, where poorer diet was associated with higher levels of psychological distress. This relationship was more pronounced in participants with fewer work and social adjustment difficulties (Fig. 1c). Finally, financial distress due to COVID-19 led to greater psychological distress in females than in males (Fig. 1d). It should be noted however that all interaction effects were small, with standardized effects <0.1.
Fig. 1.
Interaction of COVID-19 impacts with modifiable and demographic variables for psychological distress (DQ5) The mean ± standard deviation (SD) of psychological distress (DQ5) score plotted against COVID-19 impact and gender or modifiable factors. (a) Bar graph of direct exposure to COVID-19 with gender. (b) Quartiles (Q1-Q4) of Work and Social Adjustment Scale (WSAS) with thwarted belongingness (belong) in a line graph. (c) Quartiles of WSAS with diet in a bar graph. (d) Bar graph of COVID-19 financial distress and gender.
3.3. Factors associated with wellbeing
The mean for subjective wellbeing in our sample is reported in Table 1 with female participants reporting lower levels of wellbeing as compared to males.
To investigate COVID-19-related impacts on wellbeing after adjusting for background and modifiable factors, a linear regression was performed (Table 3 ). For the wellbeing model, the COVID-19 variables alone explained 10% of variance, adding modifiable factors explained a further 29% of variance (Δ R2: p < .001), and demographic variables explained a further 2% of variance (Δ R2: p < .001) for a total of 41% of variance explained (n = 1216). Adding the interaction terms also significantly increased variance explained by 2%. COVID-19-related work and social adjustment difficulties and financial distress were significantly associated with reduced feelings of subjective wellbeing. The effect of COVID-19 employment changes on wellbeing was positive in the full model, although the univariate effect of employment changes was negative, suggesting that the effects of employment on wellbeing may be dependent on other factors such as financial distress. Of the modifiable factors, increased feelings of loneliness as well as reduced feelings of thwarted belongingness were associated with reductions in subjective wellbeing. Participants who reported having a poorer diet or reduced sleep quality in the past 2 weeks were also more likely to experience reduced levels of wellbeing. After accounting for all factors, female participants and those with lower levels of education had lower mean levels of wellbeing.
Table 3.
Factors associated with wellbeing.
| Standard estimate | SE | p | ||
|---|---|---|---|---|
| COVID-19 impacts | COVID-19 employment impact | 0.0590 | 1.3800 | 0.0184 |
| COVID-19 financial distress | −0.1651 | 1.6674 | <0.0001 | |
| COVID-19 exposure | −0.0046 | 4.0236 | 0.8734 | |
| WSAS score | −0.0698 | 0.0697 | 0.0100 | |
| Modifiable factors | Less physical activity | 0.0005 | 1.1678 | 0.9841 |
| Less social activity | −0.0073 | 1.4688 | 0.7671 | |
| Poorer diet | −0.1082 | 1.3916 | <0.0001 | |
| Less sleep | −0.1874 | 1.2308 | <0.0001 | |
| More alcohol | −0.0057 | 1.4864 | 0.8093 | |
| More cigarettes | −0.0162 | 2.2147 | 0.5258 | |
| Loneliness | −0.1985 | 0.4005 | <0.0001 | |
| Thwarted belongingness | −0.2857 | 0.5565 | <0.0001 | |
| Demographics | Age | 0.0170 | 0.0360 | 0.5145 |
| Male gender | 0.0871 | 1.2979 | 0.0015 | |
| Years of education | 0.0569 | 0.2996 | 0.0109 | |
| Have partner | −0.0141 | 1.2421 | 0.5697 | |
| Live alone | 0.0086 | 1.8056 | 0.7284 | |
| Significant interaction terms | WSAS score x Loneliness | 0.0991 | 0.0318 | <0.0001 |
| (COVID-19 | COVID-19 exposure x More cigarettes | 0.0904 | 6.5402 | 0.0031 |
| impact x other) | WSAS score x Age | −0.0686 | 0.0038 | 0.0029 |
| COVID-19 financial distress x Gender | 0.0742 | 2.2622 | 0.0311 |
Standard Error (SE); Work and Social Adjustment Scale (WSAS).
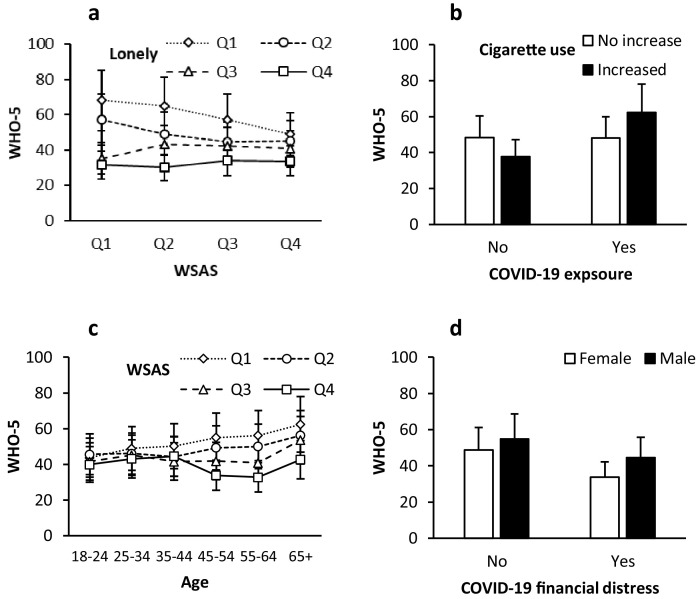
To further examine the relationship of COVID-19 impacts with modifiable risk factors for wellbeing, interaction effects were tested; all were small with standardized effects < 0.1. Significant interaction effects are illustrated in Fig. 2 , with scores of WSAS and loneliness reported as quartiles to aid interpretation. As work and social adjustment difficulties increased, wellbeing was reduced, but this was more pronounced in those who felt lower levels of loneliness. There was little change in wellbeing at each level of the WSAS for participants who felt high levels of loneliness (Q4) (Fig. 2a). Participants who experienced a direct contact with COVID-19 and increased their cigarette use reported increased levels of subjective wellbeing in the fully-adjusted model (Fig. 2b), although this outcome should be interpreted with caution given the low prevalence of direct COVID-19 contact. Work and social adjustment difficulties related to COVID-19 appeared to affect participants aged 45 or older to a greater extent, resulting in decreased levels of subjective wellbeing (Fig. 2c). Financial distress related to COVID was associated with greater reductions in the psychological wellbeing of females compared to males (Fig. 2d).
Fig. 2.
Interaction of COVID-19 impacts with modifiable and demographic variables for wellbeing (WHO-5) The mean ± standard deviation (SD) of subjective wellbeing (WHO-5) score plotted against COVID-19 impact and gender, age or modifiable factors. (a) Quartiles (Q1-Q4) of Work and Social Adjustment Scale (WSAS) with loneliness (lonely) in a line graph. (b) Bar graph of direct exposure to COVID-19 and cigarette use. (c) Quartiles (Q1-Q4) of WSAS with age groups in a line graph. (d) Bar graph of COVID-19 financial distress and gender.
4. Discussion
The implementation of measures to reduce social contact during the COVID-19 pandemic was likely to increase feelings of loneliness and decrease feelings of belonging at the time of the present study in late March 2020. Results from our study show that indirect exposures to COVID-19 (social, financial) had a considerable impact on mental health and wellbeing, and this was magnified for certain groups of the population such as those who were lonely, females and young people. Our results reinforce that increased psychological distress and poorer wellbeing were associated with increased loneliness and reduced feelings of belonging, similar to a Spanish study (Losada-Baltar et al., 2020). We further explicated these associations in relation to a range of COVID-19 exposures, demonstrating that difficulty with work and social adjustment to the pandemic interacted with both loneliness and thwarted belongingness. Overall, these outcomes suggest that loneliness and thwarted belongingness are likely to be associated with mental health outcomes differently for particular groups in the context of a pandemic. This knowledge may also guide other public health or environmental disasters.
Wellbeing in our sample was considerably lower than that seen in pre-pandemic European population based samples (Topp et al., 2015) and also lower than a Danish sample collected at a similar time point (Sønderskov et al., 2020). Similar to a Danish sample (Sønderskov et al., 2020) females had lower levels of wellbeing. In relationship with wellbeing, feelings of loneliness interacted with work and social adjustment difficulties to COVID-19. Subjective wellbeing was similar for participants with high feelings of loneliness at varying levels of work and social adjustment to COVID-19. However, participants with low levels of loneliness experienced greater decreases in wellbeing if they experienced difficulty adjusting to COVID-19. This could be because the enforced public health measures of social distancing, cancelation of events and social gathering restrictions may have had a greater impact on those for whom social interactions were more commonplace or highly valued. In contrast, participants who were already feeling lonely had lower wellbeing, but this state was less strongly related to work and social adjustment to COVID-19, suggesting that the public health measures had less impact on their wellbeing.
Overall, psychological distress in this sample was elevated compared to pre-pandemic healthy population samples (Batterham et al., 2018). Compared to males, females reported a higher level of psychological distress, as was observed in a sample of participants collected prior to COVID-19 (Batterham et al., 2016). The psychological distress in females was above the screening cut-point of 11 used to identify probable mental health conditions with high sensitivity and specificity (Batterham et al., 2016), which is indicative of the severity of distress in the sample. Difficulty adjusting to COVID-19 and feelings of belonging were related to psychological distress. The stress buffering model of Cohen and Wills (Cohen and Wills, 1985) suggests that social support can be protective in times of stress. Our results suggest that the increased social support likely to be associated with higher social connectedness is protective, however at higher levels of distress it may be less so.
The early stages of COVID-19 were associated with significant changes in work and lifestyle. Employment was affected in many ways, for example people started working from home, their hours may have reduced (voluntarily or forced), they may have changed their hours to allow for home schooling or they may have lost their job. All these changes are likely to create distress and disrupt normal day to day activities. Life rhythms, for example, sleeping, wake time, meals and social contacts have been shown to be important to mental health (Velten et al., 2014). The significant disruptions related to COVID-19 may have resulted in many participants having less healthy diets and lack of quality sleep, leading to reduced wellbeing and increased psychological distress. These findings may also indicate that the maintenance of healthy routines of daily living are important in supporting mental health.
There were also some gender differences to note. The findings suggest that females who encounter financial distress may be particularly vulnerable. This finding is concerning, as women are more prone to financial hardship and increased responsibilities during the pandemic (Workplace Gender Equality Agency, 2020). Ensuring that gender is not a barrier to equitable access to income support and related services in times of crisis should be a policy priority. In contrast, direct contact with the virus had a greater impact on increased distress in males. This finding may be related to the greater case fatality rate of COVID-19 in males (Chen et al., 2020), or gender differences associated with responses to infection (Davis et al., 2015; Sue, 2017). Our sample contained only 36 participants closely exposed to COVID-19 at the time of the study, therefore further research would be needed to confirm this. Consideration of diverse responses to risk communication should be accounted for in public messaging from Governments and health leaders (Vaughan and Tinker, 2009).
It is important for public health measures to focus on psychological wellbeing to reduce mental health problems. Feelings of loneliness and lack of belonging were significant problems in our sample. Loneliness was similar for males and females and was greater than a cut point of 2 suggesting participants were lonely (Van Tilburg and De Jong Gierveld, 2019), while more males reported higher levels of thwarted belonging as compared to females, this is in contrast to a previous community-based cohort (Christensen et al., 2014). Interventions that increase connection through technology or use educational social activity groups can improve social isolation and loneliness (Cattan et al., 2005; Chen and Schulz, 2016; Dickens et al., 2011). Promoting social connections through modalities that do not involve face-to-face interaction (e.g., video, phone and text technology) may mitigate some of the observed impacts on distress and reduced wellbeing identified in this study. Ensuring that vulnerable groups have adequate access to such technologies may be encouraged through policy mechanisms and community action. Individual activities that are adaptive and encourage engagement foster connection (Gardiner et al., 2018) and are important to consider in this environment. In addition, reduced sleep quality was associated with increased psychological distress and reduced wellbeing. Reduced sleep quality may again reflect changes in routine, such as working earlier or later in the day due to increased work demands or caring responsibilities, or a lack of a routine leading to later/less consistent bedtimes. Sleep disturbance and emotional regulation are considered to have a bidirectional relationship (Harvey et al., 2011), and sleep disturbance may also feed into social isolation (Chu et al., 2019). Therefore, public health measures to reduce sleep disturbance may consequently be beneficial during pandemics and other disasters.
The strengths of this study were that the sample was representative, and data were collected in late March, corresponding to the implementation of increased restrictions in Australia. It provides a unique snapshot of Australian life at the beginning of these changes. The limitations to the study include the use of self-report scales that may not reflect clinical states or objectively depict social connections. In addition, most scales included a reference period of the previous two weeks, which included the timeframe before the most severe restrictions of the lockdown were imposed. However, we note that in the two weeks before the survey was deployed, steps to minimize spread including physical distancing of 1.5 m, and regular handwashing were already being introduced by the federal government. Further, the cancelation of major public sporting events such as the Melbourne Grand Prix (13th March), and the suspension of the Australian Football League, (22nd March), and National Rugby League competitions (23rd March) were unprecedented events in Australia, signifying a major limitation on socialization and heralding to the population the severity of the pandemic. Another limitation is that the measurement of health behaviors was not able to distinguish whether changes were unhealthy or a reduction from an already healthy baseline. We were also limited in the number and length of scales that could be used, such that more in-depth measures and other constructs such as personality, or home schooling responsibilities may provide further insights into the relationships of interest. The interaction effects included in the models may have been different based on the model selection technique adopted. Nevertheless, the models explained more than 40% of variance in the outcomes, suggesting that key factors were accounted for adequately. Finally, this study was cross-sectional and therefore limits our ability to infer causality. Longitudinal research should be conducted to investigate how social connectedness changes over time in response to COVID-19.
In conclusion, social connectedness was significantly impacted by COVID-19 restrictions, and increased loneliness was associated with poorer mental health. Specific subgroups of the population, particularly women experiencing financial distress and men who are exposed to the virus, may require increased supports during the pandemic. Public health and policy approaches to improving social, economic and lifestyle factors may mitigate the negative mental health effects of the pandemic and its restrictions.
Funding
This study was funded by the ANU College of Health and Medicine, ANU Research School of Psychology, and ANU Research School of Population Health. ALC is supported by National Health and Medical Research Council (NHMRC) Fellowships 1122544 and 1173146. LMF is supported by an Australian Research Council Discovery Early Career Researcher Award (ARC DECRA) DE190101382. AG is supported by funding provided by the ACT Health Directorate for ACACIA: The ACT Consumer and Carer Mental Health Research Unit. YS is supported by ARC DECRA DE180100015. PJB is supported by NHMRC Fellowship 1158707.
CRediT authorship contribution statement
Sonia M. McCallum: Visualization, Conceptualization, Writing – original draft, Writing – review & editing. Alison L. Calear: Visualization, Conceptualization, Writing – original draft, Writing – review & editing. Nicolas Cherbuin: Visualization, Conceptualization, Writing – original draft, Writing – review & editing. Louise M. Farrer: Visualization, Conceptualization, Writing – original draft, Writing – review & editing. Amelia Gulliver: Visualization, Conceptualization, Writing – original draft, Writing – review & editing. Yiyun Shou: Visualization, Writing – original draft, Writing – review & editing. Amy Dawel: Data curation, Visualization, Writing – original draft, Writing – review & editing. Philip J. Batterham: Visualization, Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors are very grateful to the remaining team members involved in conducting The Australian National COVID-19 Mental Health, Behavior and Risk Communication Survey, including Dr Michelle Banfield, Professor Darren Gray, Dr Tambri Housen, Dr Alyssa Morse, Dr Eryn Newman, Dr Kristen Murray, Dr Rachael Rodney Harris and Professor Michael Smithson (listed alphabetically).
This study was funded by the ANU College of Health and Medicine, ANU Research School of Psychology, and ANU Research School of Population Health. ALC is supported by National Health and Medical Research Council (NHMRC) Fellowships 1122544 and 1173146. LMF is supported by an Australian Research Council Discovery Early Career Researcher Award (ARC DECRA) DE190101382. AG is supported by funding provided by the ACT Health Directorate for ACACIA: The ACT Consumer and Carer Mental Health Research Unit. YS is supported by ARC DECRA DE180100015. PJB is supported by NHMRC Fellowship 1158707.
References
- Arora T., Grey I. Health behavior changes during COVID-19 and the potential consequences: a mini-review. J. Health Psychol. 2020;25:1155–1163. doi: 10.1177/1359105320937053. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics, 2016. 2016 Census quickstats. https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/036 (Accessed 14 August 2020).
- Batterham P.J., Sunderland M., Carragher N., Calear A.L., Mackinnon A.J., Slade T. The distress questionnaire-5: population screener for psychological distress was more accurate than the K6/K10. J. Clin. Epidemiol. 2016;71:35–42. doi: 10.1016/j.jclinepi.2015.10.005. [DOI] [PubMed] [Google Scholar]
- Batterham P.J., Sunderland M., Slade T., Calear A.L., Carragher N. Assessing distress in the community: psychometric properties and crosswalk comparison of eight measures of psychological distress. Psychol. Med. 2018;48:1316–1324. doi: 10.1017/S0033291717002835. [DOI] [PubMed] [Google Scholar]
- Campbell, K., Vines, E., 2021. COVID-19: a chronology of Australian Government announcements (up until 30 June 2020). https://parlinfo.aph.gov.au/parlInfo/download/library/prspub/8027137/upload_binary/8027137.pdf (Accessed 31/08/2021).
- Cancello R., Soranna D., Zambra G., Zambon A., Invitti C. Determinants of the lifestyle changes during COVID-19 pandemic in the residents of northern Italy. Int. J. Environ. Res. Public Health. 2020;17:6287. doi: 10.3390/ijerph17176287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattan M., White M., Bond J., Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Soc. 2005;25:41–67. doi: 10.7748/nop.17.1.40.s11. [DOI] [PubMed] [Google Scholar]
- Chen Y.R.R., Schulz P.J. The Effect of Information Communication Technology Interventions on Reducing Social Isolation in the Elderly: a Systematic Review. J. Med. Internet Res. 2016;18:e18. doi: 10.2196/jmir.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J.a., Yu T., Zhang X., Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet North Am. Ed. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheval B., Sivaramakrishnan H., Maltagliati S., Fessler L., Forestier C., Sarrazin P., Orsholits D., Chalabaev A., Sander D., Ntoumanis N., Boisgontier M.P. Relationships between changes in self-reported physical activity, sedentary behavior and health during the coronavirus (COVID-19) pandemic in France and Switzerland. J. Sports Sci. 2020:1–6. doi: 10.1080/02640414.2020.1841396. [DOI] [PubMed] [Google Scholar]
- Christensen H., Batterham P.J., Mackinnon A.J., Donker T., Soubelet A. Predictors of the risk factors for suicide identified by the interpersonal-psychological theory of suicidal behavior. Psychiatry Res. 2014;219:290–297. doi: 10.1016/j.psychres.2014.05.029. [DOI] [PubMed] [Google Scholar]
- Chu C., Hom M.A., Gallyer A.J., Hammock E.A.D., Joiner T.E. Insomnia predicts increased perceived burdensomeness and decreased desire for emotional support following an in-laboratory social exclusion paradigm. J. Affect. Disord. 2019;243:432–440. doi: 10.1016/j.jad.2018.09.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- Daly M., Robinson E. High-risk drinking in midlife before versus during the COVID-19 Crisis: longitudinal evidence from the United Kingdom. Am. J. Prev. Med. 2020;60:294–297. doi: 10.1016/j.amepre.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis M.D.M., Stephenson N., Lohm D., Waller E., Flowers P. Beyond resistance: social factors in the general public response to pandemic influenza. BMC Public Health. 2015;15:436. doi: 10.1186/s12889-015-1756-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawel A., Shou Y., Smithson M., Cherbuin N., Banfield M., Calear A.L., Farrer L., Gray D., Gulliver A., Housen T., McCallum S.M., Morse A.R., Murray K., Newman E.J., Rodney Harris R.M., Batterham P. The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Front. Psychiatry. 2020;11:579985. doi: 10.3389/fpsyt.2020.579985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jong Gierveld J., Van Tilburg T. A 6-Item scale for overall, emotional, and social loneliness: confirmatory tests on survey data. Res. Aging. 2006;28:582–598. [Google Scholar]
- Dickens A.P., Richards S.H., Greaves C.J., Campbell J.L. Interventions targeting social isolation in older people: a systematic review. BMC Public Health. 2011;11:647. doi: 10.1186/1471-2458-11-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 Pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Marx W., Dash S., Carney R., Teasdale S.B., Solmi M., Stubbs B., Schuch F.B., Carvalho A.F., Jacka F., Sarris J. The effects of dietary improvement on symptoms of depression and anxiety: a meta-analysis of randomized controlled trials. Psychosom. Med. 2019;81:265–280. doi: 10.1097/PSY.0000000000000673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher J.T., TD, Hammarberg K., Sastry J., Nguyen H., Rowe H., Popplestone S., Stocker R., Stubber C., Kirkman M. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med. J. Aust. Prepr. 2020 doi: 10.5694/mja2.50831. 10 June 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardiner C., Geldenhuys G., Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc. Care Commun. 2018;26:147–157. doi: 10.1111/hsc.12367. [DOI] [PubMed] [Google Scholar]
- Harvey A.G., Murray G., Chandler R.A., Soehner A. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin. Psychol. Rev. 2011;31:225–235. doi: 10.1016/j.cpr.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holingue C., Badillo-Goicoechea E., Riehm K.E., Veldhuis C.B., Thrul J., Johnson R.M., Fallin M.D., Kreuter F., Stuart E.A., Kalb L.G. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: findings from American trend panel survey. Prev. Med. 2020;139 doi: 10.1016/j.ypmed.2020.106231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Losada-Baltar A., Jiménez-Gonzalo L., Gallego-Alberto L., Pedroso-Chaparro M.d.S., Fernandes-Pires J., Márquez-González M. We are staying at home.” Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J. Gerontol. Ser. B. 2020;76:e10–e16. doi: 10.1093/geronb/gbaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maalouf F.T., Mdawar B., Meho L.I., Akl E.A. Mental health research in response to the COVID-19, Ebola, and H1N1 outbreaks: a comparative bibliometric analysis. J. Psychiatr. Res. 2021;132:198–206. doi: 10.1016/j.jpsychires.2020.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manger S. Lifestyle interventions for mental health. Aust. J. Gen. Pract. 2019;48:670–673. doi: 10.31128/AJGP-06-19-4964. [DOI] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundt J.C., Marks I.M., Shear M.K., Greist J.H. The work and social adjustment scale: a simple measure of impairment in functioning. Br. J. Psychiatry. 2002;180:461–464. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rebar A.L., Stanton R., Geard D., Short C., Duncan M.J., Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol. Rev. 2015;9:366–378. doi: 10.1080/17437199.2015.1022901. [DOI] [PubMed] [Google Scholar]
- Ritchie, H., Mathieu, E., Rodés-Guirao, L., Appel, C., Giattino, C., Ortiz-Ospina, E., Hasell, J., Macdonald, B., Beltekian, D., Roser, M., 2020. Coronavirus Pandemic (COVID-19). https://ourworldindata.org/coronavirus (Accessed 31/08/2021).
- Rodriguez L.M., Litt D.M., Stewart S.H. Drinking to cope with the pandemic: the unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict. Behav. 2020;110 doi: 10.1016/j.addbeh.2020.106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossinot H., Fantin R., Venne J. Behavioral changes during COVID-19 confinement in France: a web-based study. Int. J. Environ. Res. Public Health. 2020;17:8444. doi: 10.3390/ijerph17228444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeri A.K., Cruwys T., Barlow F.K., Stronge S., Sibley C.G. Social connectedness improves public mental health: investigating bidirectional relationships in the New Zealand attitudes and values survey. Aust. N. Z. J. Psychiatry. 2018;52:365–374. doi: 10.1177/0004867417723990. [DOI] [PubMed] [Google Scholar]
- Solmi M., Veronese N., Galvano D., Favaro A., Ostinelli E.G., Noventa V., Favaretto E., Tudor F., Finessi M., Shin J.I., Smith L., Koyanagi A., Cester A., Bolzetta F., Cotroneo A., Maggi S., Demurtas J., De Leo D., Trabucchi M. Factors associated with loneliness: an umbrella review of observational studies. J. Affect. Disord. 2020;271:131–138. doi: 10.1016/j.jad.2020.03.075. [DOI] [PubMed] [Google Scholar]
- Sønderskov K.M., Dinesen P.T., Santini Z.I., Østergaard S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020;32:226–228. doi: 10.1017/neu.2020.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storen, R., Corrigan, N., 2020. COVID-19 a chronology of state and territory government announcements (up until 30 June 2020). https://parlinfo.aph.gov.au/parlInfo/download/library/prspub/7614514/upload_binary/7614514.pdf (Accessed 31/08/2021).
- Sue K. The science behind “man flu. BMJ. 2017;359:j5560. doi: 10.1136/bmj.j5560. [DOI] [PubMed] [Google Scholar]
- Taylor G., McNeill A., Girling A., Farley A., Lindson-Hawley N., Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ Br. Med. J. 2014;348:g1151. doi: 10.1136/bmj.g1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp C.W., Østergaard S.D., Søndergaard S., Bech P. The WHO-5 well-being index: a systematic review of the literature. Psychother. Psychosom. 2015;84:167–176. doi: 10.1159/000376585. [DOI] [PubMed] [Google Scholar]
- Tran T.D., Hammarberg K., Kirkman M., Nguyen H.T.M., Fisher J. Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia. J. Affect. Disord. 2020;277:810–813. doi: 10.1016/j.jad.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden K.A., Cukrowicz K.C., Witte T.K., Joiner T.E. Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the interpersonal needs questionnaire. Psychol. Assess. 2012;24:197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Tilburg, T., De Jong Gierveld, J., 2019. Cut-off points for the de Jong Gierveld loneliness scale. https://home.fsw.vu.nl/tg.van.tilburg/Cut-off%20points%20for%20the%20De%20Jong%20Gierveld%20loneliness%20scale.pdf (accessed 31 August 2020).
- Vaughan E., Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. Am. J. Public Health. 2009;99:S324–S332. doi: 10.2105/AJPH.2009.162537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velten J., Lavallee K.L., Scholten S., Meyer A.H., Zhang X.C., Schneider S., Margraf J. Lifestyle choices and mental health: a representative population survey. BMC Psychol. 2014;2:58. doi: 10.1186/s40359-014-0055-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser M., Schaap L.A., Wijnhoven H.A.H. Self-reported impact of the COVID-19 pandemic on nutrition and physical activity behavior in Dutch older adults living independently. Nutrients. 2020;12:3708. doi: 10.3390/nu12123708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werneck A.O., Silva D.R., Malta D.C., Souza-Júnior P.R., Azevedo L.O., Barros M.B., Szwarcwald C.L. Physical inactivity and elevated TV-viewing reported changes during the COVID-19 pandemic are associated with mental health: a survey with 43,995 Brazilian adults. J. Psychosom. Res. 2020 doi: 10.1016/j.jpsychores.2020.110292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Workplace Gender Equality Agency, 2020. Gendered impact of COVID-19. https://www.wgea.gov.au/topics/gendered-impact-of-covid-19 (Accessed 9 July 2020).
- World Health Organization, 2020a. Coronavirus disease (COVID-19) advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (Accessed 21 July 2020).
- World Health Organization, 2020b. Mental health and psychosocial considerations during the COVID-19 outbreak. https://www.who.int/publications/i/item/WHO-2019-nCoV-MentalHealth-2020.1 (Accessed 21 July 2020).