Abstract
Introduction
Obstetric sonography is a highly skilled diagnostic medical examination. Pregnant women like to socialise their ultrasound experience with family, introducing distractions for the sonographer. Our objective was to survey ultrasound practitioners to identify concerns regarding interruptions and their opinions about socialisation during the examination.
Methods
An online questionnaire was disseminated to study the views of Australian and New Zealand obstetric sonographers/sonologists. It was informed by a pilot study of possible distractors with quality and safety concerns and operator opinions regarding family bonding.
Results
The opinions of 393 obstetric sonographers/sonologists informed our results. Distractors with the most negative aspects included disruptive children (93.3%) and mobile phone conversations (84.3%). Most respondents (62%) believed that a distractor only had to be present for 5 min or less to have an impact. Small children were identified by 87.5% of respondents as safety risks to themselves, to the patient and to sonographers. Sonographers were concerned that distractors caused a loss of concentration, interruption to a systematic scanning approach and increased false negatives in screening, missing important diagnoses. Sonographers strongly agreed that obstetric sonography facilitated maternal–fetal bonding, but only 15% thought that siblings bond with the fetus during the scan.
Conclusion
Obstetric sonographers in our study are concerned that distractors pose a negative impact on the quality and safety of ultrasound. They also recognise the importance of family bonding. Strategies to bridge the medical and social components of obstetric sonography should be developed to reduce quality and safety threats.
Keywords: bonding, distractors, interruptions, obstetric ultrasound, sonographer attitudes
Introduction
Up to the mid‐20th century, obstetric care was dominated by efforts to improve maternal morbidity and mortality with major medical advances made by safe blood transfusions, antibiotics and effective anaesthesia.1 The 21st century, with the promulgation of antenatal ultrasound, has provided a visual and philosophical focus on the fetus. Medical sonography in Australia and New Zealand is routinely used in all trimesters of pregnancy to evaluate fetal and maternal health. It also provides an opportunity for women to view their unborn baby, which is often shared as a social event with their family members. The interplay between diagnostic medicine and socialisation in antenatal ultrasound provides fertile ground for competing interests.
It has become an expectation of pregnant women that time is allocated during the ultrasound examination for social enjoyment.2 The social aspect of ultrasound is identified as emotionally beneficial to pregnant women by providing ‘reassurance’ and reducing anxiety levels.3, 4, 5, 6 Obstetric ultrasound is therefore unique as an important medical procedure for diagnosis and screening with an additional social aspect postulated to facilitate ‘bonding’ and the transition to parenthood.7 Socialisation in obstetric ultrasound is recognised by professional bodies including The Royal College of Obstetricians and Gynaecologists (RCOG) which names ‘psychological support’ as one of the important objectives of a routine scan.8
Although sonographers are aware of their important role in the women's journey to motherhood, they are also charged with the task of identifying and monitoring fetal, placental and maternal abnormalities. The presence of family members during the obstetric ultrasound may result in distractions which sonographers view as a hindrance to their ability to perform the procedure professionally and effectively.9
Patients and their families have been identified as sources of interruptions, preventing healthcare professionals from successfully completing their tasks.10, 11, 12 An ‘interruption’ is defined as a break in the performance of a human activity by an internal (within the recipient) or external source, specific to a setting or a location.13 Interruptions may increase or overload mental tasks and thereby reduce the ability to cope with the task at hand, potentially impairing performance.14
A systematic review of interruptions and distractions in healthcare settings identified only 33 peer‐reviewed empirical data studies published in English.11 Only 7 (21%) of the studies examined outcomes related to interruptions, demonstrating a serious deficiency of literature in this area. Most studies on interruption in medical work‐practices were set in emergency departments, operating theatres, intensive care units or general wards across a range of healthcare professionals.
Literature relating to interruptions and distractions and their impact on clinical diagnostic imaging services is limited. To date, published studies15, 16, 17, 18 have focussed on diagnostic error in radiologists’ reports due to interruptions. To the best of our knowledge, the only published peer‐reviewed article on impacts of distractions in obstetrics ultrasound12 has found that active disruptive children decrease overall scanning time with sonographers ‘rushing’ their tasks. In contrast, a radiology study on interpretation of medical images with interruption by phone calls found that radiologists took longer to do the task, with increased time secondary to the cognitive cost of ‘switching’.18 The obstetric ultrasound work environment with the presence of children is likely to have unique distracting factors.
The frequency and impact of task interruption in the intensive care unit has been shown to have serious consequences for patient safety.19 Observational data revealed that 30% of nurse activities were interrupted. The consequences for task interruption were either abandoning its completion or omission of some of the task steps. This suggests there may be serious impact in obstetric ultrasound since it is ideally performed in a logical stepwise sequence (otherwise called ‘prospective memory tasking’19) with attention to not omitting any steps.
The effect of interrupted task performance is variable across different abilities of individuals to retain their working memory capacity.20 That is, some operators will be more susceptible to the negative effects of interruptions than others. In short, in the event of task interruption, ‘One size does not fit all’.20
As the first step in investigating the potential tensions between the social and diagnostic aspects of obstetric ultrasound, we sought the views of sonographers/sonologists to distractions or interruptions, any subsequent perceived threats to quality and safety, and their opinions on family bonding during the examination.
Methods
An online survey using closed‐ and open‐ended questions targeted at sonographers/sonologists in Australia and New Zealand was conducted from September to December 2015. Two professional bodies representing sonographers/sonologists (Australasian Sonographers Association & Australasian Society for Ultrasound in Medicine) supported the study and their respective online newsletters were used to distribute the survey. The exact number of actively practicing obstetric ultrasound practitioners in Australia and New Zealand is unknown. Guided by the sonographer accreditation professional bodies, we estimated the number to be 4000. A sample size calculator (Survey Monkey™) estimated that we would need 351 respondents for the results to be within a 95% confidence interval and 5% error tolerance. Pre‐approval for the study was obtained from the RWH (Royal Women's Hospital) Research Committee and RWH Human Research Ethics Committee as a quality assurance/audit project.
With no previous studies on cognitive factors in ultrasound to guide us, the authors who all have extensive experience in obstetric ultrasound scanning developed the questions for a pilot study. The pilot survey was distributed to actively practicing sonographers in various industry groups to seek feedback on the clarity and content of the content. Survey questions were subsequently grouped into the following categories: respondent's characteristics and work practice environments, number and types of scans performed per week, factors that were identified as possible distractors, quality and safety concerns relating to possible distractors and respondent's opinions on family bonding with the fetus. Demographics were sought in an attempt to determine if certain characteristics were associated with high or low working memory capacity and resilience to distractors.
Descriptive analysis of closed‐ and open‐ended questions was included. The response rate determined the use of chi‐square tests (R version 3.2.3, The R Foundation for Statistical Computing, 2015),21 Fisher Exact tests and/or simulated P‐values to test for significant associations between demographic and worksite sonographer characteristics and survey responses.22, 23
Ethics approval
Ethics Approval for the study was obtained from the Royal Women’s Hospital (RWH) Research Committee and the RWH Human Research Ethics Committee Melbourne, Victoria in 2015. The Committees were of the view that the study met the National Health and Medical Research Council requirements for quality assurance/audit projects and endorsed it as such.
Results
A total of 402 respondents registered for the survey, 6 were ineligible because they were not involved in obstetric scanning, providing the opinions of 393 obstetric sonographers/sonologists.
Sample characteristics
Tables 1 and 2 summarise the demographics of the respondents and their worksite environments.
Table 1.
Demographics of respondents
| Item (number of respondents) | Responses (n) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Gender (393) | Male | Female | |||||||
| 81 | 312 | ||||||||
| Age in years (393) | 20–30 | 31–40 | 41–50 | >50 | |||||
| 47 | 103 | 119 | 124 | ||||||
| Dependents (393) | Number of dependents (n = 261) | ||||||||
| Yes | No | 1 | 2 | 3 | 4 | 5 | >5 | ||
| 263 | 130 | 41 | 120 | 75 | 14 | 6 | 5 | ||
| Age of youngest dependent (261) | <0.5 | 0.5–1 | 1–1.5 | 1.5–2 | 2–4 | 4–6 | 6–12 | >12 | |
| 6 | 9 | 13 | 8 | 26 | 17 | 63 | 119 | ||
| Years of experience (358) | <2 | 2–5 | 6–10 | >10 | |||||
| 34 | 50 | 46 | 228 | ||||||
| Highest qualification (358) | Associate diploma | Diploma | Bachelor | Graduate certificate | Graduate diploma | Masters | PhD | DDU/COGUa | Other |
| 5 | 46 | 35 | 4 | 182 | 47 | 7 | 25 | 18 | |
Diploma of Diagnostic Ultrasound/Certification of Obstetrical and Gynaecological Ultrasound (RANZCOG).
Table 2.
Worksite environments of respondents
| Number of respondents | Responses (n) | ||||||
|---|---|---|---|---|---|---|---|
| Area of practice (358) | Inner metro | Outer metro | Rural | Remote | |||
| 204 | 137 | 57 | 9 | ||||
| Worksite (358) | Private practice | Public hospital | Tertiary referral centre | ||||
| 262 | 151 | 82 | |||||
| Types of scans performed in one week by sonographers (345) | Dating | FTS | Low‐risk morphology | High‐risk morphology | Third‐trimester growth | Third‐trimester high‐risk Doppler | Multiple gestation |
| 2460 | 1917 | 2370 | 705 | 2878 | 1358 | 611 | |
| Number of sonographers performing scans (345) | Dating | FTS | Low‐risk morphology | High‐risk morphology | Third‐trimester growth | Third‐trimester high‐risk Doppler | Multiple gestation |
| 336 | 311 | 326 | 272 | 328 | 296 | 292 | |
The majority of sonographers were female, qualified with a graduate diploma and had over 10 years of experience in sonography. There were differences (P < 0.001) in the proportion of low‐risk morphology, first‐trimester screening (FTS), third‐trimester and multiple pregnancy scans across different worksites. The proportion of dating and high‐risk morphology scans was similar across different worksites.
We collected data on years of experience, qualification and sonographer age, work environment, gender and number of dependents. Since there was an abundance of zero cell counts, Fisher Exact tests were utilised.22 Due to the sample size, exact P‐values were computationally intractable, so we calculated simulated P‐values (with 10,000 simulations per test).23 To control for Type 1 error with multiple tests, the Benjamini–Hochberg correction, with an overall family‐wise error rate of 5% was applied.23 Tests were performed using the ‘fisher.test’ function in the ‘stats’ library or the R statistical software package.21 A statistically significant association (adjusted P value <0.02) was found between operator gender and the distractor of ‘multiple questions asked by the patient or observers’, with a higher proportion of women responding that multiple questions were a distractor compared to males.
Events identified by sonographers as distractors in obstetric scanning
Table 3 summarises the percentage of respondents for each event identified as a distractor.
Table 3.
Identified distractors
| Factors identified as distractors | Respondents to this section = 345/393 (87%) |
|---|---|
| Active disruptive children (any age) | 93.30% |
| Mobile phone conversations by observers | 84.30% |
| Music or loud toys introduced by observers | 74.80% |
| Multiple questions from patient or observers | 70.70% |
| Background conversation | 69.90% |
| Video cameras filming the scan | 67.20% |
| Soiled nappy odour | 49.30% |
| Food and drink in the scan room | 43.50% |
| Adult observers | 40.90% |
| Staff interrupting the examination (physical presence or telephone) | 38.00% |
| Requirement for sonographers to provide a narration of the scan | 29.90% |
| Quiet Children – aged under 5 years/aged 5–12 years/aged 12–16 years | 9.90%/4.10%/2.60% |
| Don't experience distraction when scanning | 2.30% |
The most frequently identified distractors (and those having the most negative impact on scan performance) were active disruptive children (93.3%), mobile phone conversations (84.3%), music or loud toys (74.8%), multiple questions (70.7%) and background conversation (69.9%). Respondents also identified other distractions including the following: olfactory, observers standing directly behind them during the examination, noise from external sources and observer activities such as shuffling, texting and arguing.
Distractors identified as having the least negative impact on scan performance by respondents were adult observers in the room (40.9%), food and drink (43.5%) and quiet children (aged <5 years (9.9%), 5–12 years (4.1%) 12–16 years (2.6%)). Less than 3% of respondents reported that none of the predetermined distractors had a negative impact on their performance.
Most sonographers (85%) responded to the open‐ended question of how many quiet children they are comfortable being present in the scan room (in the presence of at least one adult, other than the patient). The most popular responses were that ‘2 children would be easily tolerated in these circumstances’ and ‘the number did not matter as long as the children were quiet’. There were frequent comments that the preferred number of children also depended on the size of the examination room, with many sonographers sceptical whether small children were likely to be quiet for the duration of a scan.
Quality and safety concerns relating to distractors
A total of 86.6% of respondents believed that distractors in the scanning room have a negative impact on scan quality (Table 4). Qualitative (‘free‐text’) responses revealed many additional quality and safety factors including the following: less commentary provided to the patient, less take‐home images provided and increased sonographer ‘stress’. Comments included ethical and practical difficulties when discussing newly diagnosed abnormalities with family members present. Some respondents were concerned at a diminution of the patient experience when the pregnant woman's focus shifted from observing the fetus to dealing with the distractions.
Table 4.
Quality factors that distractors impact negatively on
| Quality factors | Response percent (respondents = 271) |
|---|---|
| Scan interpretation (i.e. missing abnormalities) | 69.7 |
| Systematic scan | 68.60 |
| Client/patient communication | 67.90 |
| Client/patient experience | 66.80 |
| Image recording | 38.40 |
| Sonographer reporting/chart generation | 16.60 |
| Incorrect biometry | 13.70 |
| All of the above | 28.40 |
Sonographers were most concerned about the negative impact of distractors on multiple pregnancy and ‘high‐risk’ morphology scans requiring a significant level of focus and concentration, decisional latitude and diagnostic input. They were more tolerant of distractors on dating scans and third‐trimester growth scans. Some very experienced obstetric sonographers stated that due to the pressure of distraction‐rich environments they had either stopped performing second‐trimester morphology scans or were less willing to perform high‐risk scans in the presence of observers due to concerns about missing abnormalities.
Most sonographers (62%) believed that a distractor could be present for only 5 min or less to have a negative impact. Of concern, 40% of sonographers reported residual effects from one ‘distractor‐rich’ scan to the next. That is, the scan with the distractors may be resilient to any medical error but the next scan is compromised in quality. They reported a loss of concentration, irritation, frustration, anxiety, agitation, stress, annoyance, fatigue, headache, loss of confidence and difficulty in ‘switching off emotions’ in the subsequent scan. Many were concerned that after experiencing a ‘distraction‐rich’ examination, there was additional stress due to running behind in their schedule and a heightened fear of future distractions.
Many sonographers (70%) thought distractors increased the examination duration, while 23% thought it decreased the examination duration. The explanation for extended ultrasound scan duration included stopping the scan to control and diffuse distractions, particularly where children were interfering with equipment, or parents were disciplining children. It was frequently mentioned that concentration was interrupted and that extra time was needed to review recorded images to ensure the examination was complete, and of adequate quality. Common explanations for a decreased examination time were that the sonographers were less willing to engage in explanatory narrative and provide multiple take‐home images, or because they rushed the examination so that they didn't have to deal with the distractive environment.
Most sonographers believed that distractors posed safety risks to the patient, the sonographer or the person/child making the distraction. A high number of sonographers (87.5%) believed that there are risks due to the presence of children in the scanning room. Most comments related to safety risks to children and included physical risks from scanning equipment, electrical hazards and sharps disposal containers. There was also concern about children ‘playing’ around, under and on the examination couch. Strategies by sonographers to reduce safety risks for children included utilising laptops/electronic devices, toys, books, puzzles, games, drawing, engaging them in conversation and occasionally requesting that they were removed from the examination room. Sonographers frequently encouraged parents to provide entertainment for the child.
Safety risks to the pregnant woman included increased scanning time and misdiagnosis due to sonographer distractions. Safety concerns for sonographers included workplace stress, loss of concentration, risk of misdiagnosis, fear of complaints and exposure to medical litigation, forgetting to assess a structure and a future negative impact on a subsequent scan.
Sonographer views on family bonding with the fetus
Most sonographers agreed or strongly agreed that maternal and paternal bonding with the fetus was important (Figure 1). Additionally, sonographers identified that bonding was important for grandparents and same sex partners. Many also mentioned that bonding between the patient and sonographer was important. In contrast, few sonographers thought that sibling–fetal bonding was of any importance.
Figure 1.
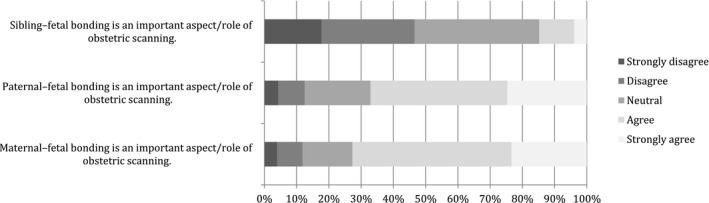
Sonographer rating of family bonding with the fetus at obstetric scan.
Discussion
In our study, the overall negative perceptions of the impact of distractors by sonographers were not affected by workplace or participant demographics. Sonographers identified that distractors often made it more challenging for them to perform a quality and safe examination. The presence of active and disruptive children was identified as a distractor by 93% of sonographers. Background noise, telephone conversations and multiple questions by observers were commonly identified distractors. Generally, sonographers are impacted by distractors within a short period of time.
Understanding and managing distractions in a healthcare setting is challenging. Healthcare settings can be hectic and demanding with time constraints. Healthcare professionals perform complex cognitive tasks that often require their undivided attention.24, 25 Obstetric sonographers have an important role to screen for, and monitor fetal and maternal pathology. They perform a series of tasks using a mental checklist and a systematic approach to ensure all aspects of the consultation is covered. ‘Prospective memory tasking’ relies on each step of the task informing the next step. When an interruption occurs, the sonographer may be momentarily deterred from the task at hand. Once this shift in attention occurs, memory of the series of tasks begins to decay to make room for processes required to deal with the interrupting task.26 The tasks can be resumed at any step but may not occur at the right step of the process. An error can occur with an incorrect resumption and missing steps in between that lead to an incomplete scan. The incorrect resumption of the task could result in errors with devastating consequences.10 The sonographers responding to our survey were very concerned that distractions impacted on the quality of the examination by interrupting their systematic approach, their ability to accurately interpret images and their ability to communicate effectively with the patients and observers.
Janelle S. Taylor a medical anthropologist in her book titled: The Public Life of the Fetal Sonogram 27 analyses the full socio‐cultural context of obstetric ultrasound. Taylor describes the entry of ultrasound into public consumer culture in the United States. Taylor's work raises the awareness of how obstetric ultrasound technology is now profoundly social in the developed world. The social aspect of obstetric scanning appears to be accepted by sonographers with most survey respondents agreeing that parental bonding with the fetus at the ultrasound examination is important. Sonographers facilitate bonding using a communicative approach, through their scan narrative.
The acceptance by sonographers and patients that the examination is a bonding event is at odds with distractors which can potentially decrease the diagnostic capability of the scan. For the patient and her family, distractive actions such as background conversations, repeated questions, photography or even phone conversations may be seen as the normal part of the bonding experience. The sonographer's anatomical narrative which may promote maternal–fetal bonding encourages observers’ perceptions that they are a part of this bonding journey.28 Most sonographers surveyed were happy to provide a narrative, and they did not see it as a threat to the quality of the scan. Additionally, they viewed it as a strategy to assist their mental checklist for systematic scanning, and also to mitigate multiple questions from observers that were seen as a greater threat to scan quality.
The presence of disruptive children in the scanning room was the most commonly identified distractor and many sonographers perceived them as safety risks for themselves and others. Furthermore, sonographers did not believe that the presence of young children assisted in bonding between the child and the fetus. In the presence of young children, sonographers were less willing to engage in explanatory narrative and some reported they rushed the examination so that they didn't have to deal with the distractive environment. The latter is supported by a previous study, where significantly shorter scan times were observed in the presence of disruptive children compared to distraction‐free scans.12
It is clear from this study that there is a need to manage the expectations of the patients and sonographers and bridge the social and medical considerations in obstetric sonography. Safety and quality is paramount, but so is the positive experience for the pregnant woman and her family. Sonographer and patient education would provide a good basis that could lead to development of policy or guidelines in this area.
Limitations of the study
An online survey can be limited by multiple factors including the following: participant self‐selection, the subjective nature of questions and responses and misunderstanding of questions by respondents. There is also the potential bias of researchers in the design of questions and interpretation of results. Our study did not attempt to discover the exact percentage of sonographers who were impacted by distractors. We aimed to explore the views of sonographers who were interested in discussing their perceptions with regard to distractors in order to inform future studies on medical error in obstetric sonography. Only the views of sonographers/sonologists are revealed in this study. Future studies could focus on patient perceptions and test the impact of distractors on quality factors such as error rates, examination duration and patient satisfaction.
Conclusion
Sonographers in our survey believe that distractors impact on the quality and safety of the obstetric ultrasound examination. Informed by this study, we believe there is a significant level of concern in this area. There is a need for further research to determine when and which distractions are a serious risk to the quality and safety of an obstetric ultrasound. One wonders if pregnant women would ever wish to decrease the diagnostic capability of obstetric scanning to fulfil their bonding expectations. Clearly, sonographers do not. Consideration should be given to developing strategies to bridge the social and medical aspects of obstetric sonography, aiming to eliminate any fear of a real threat to the quality of the examination while maintaining a safe working environment for sonographers and a positive experience for the pregnant woman.
Disclosure
The authors declare that they have no financial interests associated with their study or the publication of the manuscript and are not aware of any professional or personal conflicts of interest.
Authorship declaration
As the authors of the article (Najafzadeh, Woodrow and Thoirs), we declare that we have all made substantial contribution to the conception, design, acquisition, analysis and interpretation of data, drafting and revising of the article for intellectual content and approval of the final version offered for publication. We believe that our joint efforts conform to the journal's authorship policy and are in agreement with the content of the submitted manuscript.
Acknowledgements
We would like to thank the executives of the Australasian Society of Ultrasound in Medicine (ASUM) and the ASA (Australian Sonography Association) for their enthusiastic support in disseminating our survey to the membership. Mr Adam B Rohrlach, School of Mathematical Sciences, University of Adelaide, South Australia, for undertaking the statistical analysis for this study. Associate Professor Fabricio Costa, Monash Ultrasound for Women, Victoria, Australia for his encouragement in the release of the survey to ASUM members.
References
- 1.Chamberlain G. British maternal mortality in the 19th and early 20th centuries. J R Soc Med 2006; 99: 559–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chudleigh T. Scanning for pleasure. Ultrasound Obstet Gynecol 1999; 14: 369–71. [DOI] [PubMed] [Google Scholar]
- 3.Campbell S, Reading A, Cox D, Sledmere CM, Mooney R, Chudleigh P, et al. Ultrasound scanning in pregnancy: the short‐term psychological effects of early real‐time scans. J Psychom Obstet Gynecol 1982; 1: 57–61. [Google Scholar]
- 4.Reading A, Cox D, Sledmere C, Campbell S. Psychological changes over the course of pregnancy: a study of attitudes toward the fetus/neonate. Health Psychol 1984; 3: 211. [DOI] [PubMed] [Google Scholar]
- 5.Villeneuve C, Laroche C, Lippman A, Marrache M. Psychological aspects of ultrasound imaging during pregnancy. Canad J Psych 1988; 33: 530–6. [DOI] [PubMed] [Google Scholar]
- 6.Kovacevic M. The impact of fetus visualization on parents’ psychological reactions. J Prenat Perinat Psychol Health 1993; 8: 83–93. [Google Scholar]
- 7.Fletcher J, Evans M. Maternal bonding in early fetal ultrasound examinations. N Engl J Med 1983; 308: 392–3. [DOI] [PubMed] [Google Scholar]
- 8.RCOG . Report of the Royal College of Obstetrics and Gynaecology Working Party on Ultrasound Screening for Fetal Abnormalities, 1997.
- 9.Craig M. Family‐centered sonography. Part 2. Obstetric sonography. J Diag Med Sonog 1986;2:96–103. [Google Scholar]
- 10.Ratwani R, Hettinger Z, Brixey J, Rivera A, Colligan L. Managing interruptions in healthcare: from theory to practice. Proc Human Fact Ergonomics Soc Ann Meet 2014; 58: 624–8. [Google Scholar]
- 11.Rivera‐Rodriguez A, Karsh B. Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care 2010; 19: 304–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Najafzadeh A. Children accompanying their mothers during routine obstetric scans: effects on the mother's heart rate variations and on the sonographer's work practice. Soundeffects 2012; 4: 18–22. [Google Scholar]
- 13.Brixey J, Robinson D, Johnson C, Johnson T, Turley J, Zhang J. Concept analysis of the phenomenon interruption. Adv Nurs Sci 2007; 30: E26–42. [DOI] [PubMed] [Google Scholar]
- 14.Beasley J, Wetterneck T, Temte J, Lapin JA, Smith P, Rivera‐Rodriguez AJ, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med 2011; 24: 745–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balint B, Steenburg S, Lin H, Shen C, Steele J, Gunderman R. Do telephone call interruptions have an impact on radiology resident diagnostic accuracy? Acad Radiol 2014; 21: 1623–8. [DOI] [PubMed] [Google Scholar]
- 16.Schemmel A, Lee M, Hanley T, Pooler BD, Kennedy T, Field A, et al. Radiology workflow disruptors: a detailed analysis. J Am Coll Radiol 2016; 13: 1210–4. [DOI] [PubMed] [Google Scholar]
- 17.Sogge S. Nature of Phone Call Interruptions in a Neuroradiology Reading Room during a Typical Workday: An Observational Study. In: Proceedings of Conference Nature of Phone Call Interruptions in a Neuroradiology Reading Room during a Typical Workday: An Observational Study.
- 18.Williams L, Drew T. Distraction in diagnostic radiology: how is search through volumetric medical images affected by interruptions? Cogn Res 2017; 2: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Drews F. The frequency and impact of task interruptions in the ICU, Proceedings of the Human Factors and Ergonomics Society 51st Annual Meeting 2007: 683–6.
- 20.Drews FA, Musters A. Individual differences in interrupted task performance: one size does not fit all. Int. J Human‐Computer Studies 2015; 79: 97–105. [Google Scholar]
- 21.R Core Team . A language and environment for statistical computing. Vienna: Foundation for Statistical Computing, 2014. Available from: https://www.gbif.org/tool/81287/r-a-language-and-environment-for-statistical-computing. [Google Scholar]
- 22.Liu I, Agresti A. The analysis of ordered categorical data: an overview and a survey of recent developments. Test 2005; 14: 1–73. [Google Scholar]
- 23.Hochberg Y, Benjamini Y. More powerful procedures for multiple significance testing. Stat Med 1990; 9: 811–8. [DOI] [PubMed] [Google Scholar]
- 24.Manning D, Gale A, Krupinski E. Perception research in medical imaging. Br J Radio 2005; 78: 683–5. [DOI] [PubMed] [Google Scholar]
- 25.Johnson M, Sanchez P, Langdon R, Manias E, Levett‐Jones T, Weidemann G, et al. The impact of interruptions on medication errors in hospitals: an observational study of nurses. J Nurs Manag 2017; 25: 498–507. [DOI] [PubMed] [Google Scholar]
- 26.Altmann EM, Trafton JG. Task interruption: Resumption lag and the role of cues, 2004. Available from: https://www.interruptions.net/literature/Altmann-CogSci04.
- 27.Taylor JS. The public life of the fetal sonogram. New Brunswick, NJ: Rutgers University; 2008. [Google Scholar]
- 28.Draper J. ‘It was a real good show’: the ultrasound scan, fathers and the power of visual knowledge. Sociol Health Illn 2002; 24: 771–95. [Google Scholar]


