Abstract
Point‐of‐care ultrasound, or PoCUS, where imaging is undertaken at the bedside, clinic or emergency department (ED) by the clinician overseeing treatment, is a rapid form of assessment that may be undertaken alongside or as an alternative to traditional, formal ultrasound performed by a radiology service. PoCUS reduces the time to diagnosis, thus allowing lifesaving treatment to be initiated. This is particularly relevant in Obstetrics and Gynaecology (OBGYN), where delayed diagnosis of pregnancy complications is often fatal or highly debilitating to the mother or fetus. The literature suggests that PoCUS is particularly useful in areas that are inadequately resourced, as it is relatively cheap and accessible. High‐quality training is essential to ensure that the staff performing the scans are adequately qualified to deliver the service. Clinicians who perform PoCUS in their practice should be aware of the appropriate indications, as well as when to refer for formal imaging.
Keywords: obstetrics and gynaecology, PoCUS, ultrasound, women's health
Introduction
PoCUS is different to conventional ultrasound in that it is a rapid, limited study performed at the bedside for a specific diagnostic or therapeutic outcome. The study is being performed by the clinician making the treatment decisions, with the advantage of having an insight into their patient's symptoms and background that the sonographer does not.1 The scope of clinical questions that may be addressed with PoCUS is less than with formal imaging2; however, PoCUS has revealed itself to be of use in a wide range of clinical scenarios. Areas of medicine where PoCUS seem to be especially useful are Emergency Medicine, Obstetrics and Gynaecology and Rural and Remote medicine, where intervention is time critical and access to formal imaging is limited. There is a growing body of literature looking at the different ways in which it can be used, the benefits and limitations of PoCUS and the practicalities of training medical and support staff in the use of bedside ultrasound.
Definition of PoCUS
In 2017, the Australasian Journal of Ultrasound in Medicine (AJUM) published a discussion paper on the definition of PoCUS, and how to differentiate it from other modalities such as comprehensive and limited diagnostic ultrasound.3 The reason for this delineation was to streamline medicare‐billing practices and limit the number of studies being billed inappropriately. The Australasian Society for Ultrasound in Medicine (ASUM) acknowledge that the PoCUS is difficult to define and have recommended that confusing definitions such as ‘bedside’ and ‘point of care’ should be substituted for ‘focused, limited and comprehensive’. Australasian Journal of Ultrasound in Medicine states that PoCUS is a study that is ‘performed by a medical practitioner who uses ultrasound equipment to enhance and extend their own clinical examination of the patient’3 and should be considered an extension of the physical examination. The PoCUS is not a structured examination that adheres to a protocol, nor are images typically stored or reports generated. The information gathered is for the use of the clinician in real time, to influence management decisions.3 PoCUS is seen an increase in uptake by clinicians due to its portability, ease of use and accessibility and may be especially useful in remote or resource‐limited areas; however, it should not be considered a substitute for formal diagnostic ultrasound.
Advantages of PoCUS
Ultrasound has many advantages over other imaging modalities making it well suited to the acute care setting. The equipment can be relatively affordable and portable, the images may be obtained and interpreted in real time, and is believed to be safe, involving no ionising radiation.2 This is particularly relevant in the field of obstetrics, with the highest potential for reduction in morbidity and mortality.2
An additional benefit of PoCUS is the option of keeping the patient near medical staff and resuscitation equipment whilst performing the study, allowing a potentially unstable patient to receive treatment in a timely manner.4 Alternatively, a negative study may allow patients to be discharged from ED, reducing the waiting times and thus increasing patient satisfaction, as well as resource allocation. This has been noted when looking at women presenting to a West Indian emergency department with first trimester bleeding.4, 5
PoCUS can be used to influence the management of certain conditions, such as tubo‐ovarian abscess (TOA), the management of which depends on ultrasound findings such as size and locularity. It has been shown that ultrasound‐guided drainage has a lower complication rate; thus, PoCUS can potentially reduce the incidence of surgery‐related complications, as well as being used for the therapy itself (Figure 1).6
Figure 1.
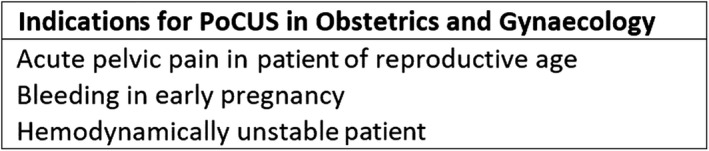
Indications for PoCUS.
There is much interest in the use of PoCUS in remote and poorly resourced areas, as a means of screening at‐risk patients for tertiary follow‐up.7, 8, 9 Many studies have looked at training of healthcare workers such as midwives in the use of PoCUS, which strongly support the practice.10, 11, 12 It is important to understand, however, that PoCUS is a limited, focused exam that aims to answer a specific question, for example, ‘is there a fetal heartbeat’, or ‘is there free fluid?’ It cannot be stressed enough that PoCUS should not be viewed as an alternative to formal ultrasound.2
PoCUS training in Australia and worldwide
Ultrasound is a highly user dependent tool.13, 14 The quality of ultrasound images is dependent on several factors, including operator understanding of ultrasound physics and familiarity with the ultrasound machine controls, as well as on their skills and competency in performing the examination.15 Sonography is a complex skill to master and requires considerable training and many hours of practice to become competent.2 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) training (revised in 2016) includes ultrasound training. The training consists of online modules and on‐site contact hours amounting to at least 80 h in the first 92 weeks of the programme. There is also a logbook requirement of at least 25 transabdominal (TA) and 25 transvaginal (TV) scans, 25 s or third trimester biometry evaluations and 75 third trimester assessments. Furthermore, trainees are required to undertake a RANZCOG‐approved course or workshop during their training. A properly qualified practitioner at the training site must carry out the in‐hospital assessment of the ultrasound module. Two assessments of procedural and surgical skills (APSS) are required, a 1st and 3rd Trimester APSS by the end of Year 2 and a Biometry APSS by Year 4.16 In a statement by the Australasian Journal of Ultrasound in Medicine on the Use of Ultrasound by Medical Practitioners they acknowledge the increased uptake of ultrasound by non‐sonologists and emphasise the recommendation that PoCUS should only be performed by properly credentialled clinicians, and only for the studies for which they are credentialled. There are two postgraduate programmes for ultrasound, the Diploma in Diagnostic Ultrasound (DDU) and the Certificate in Clinician Performed Ultrasound (CCPU), which are aimed at clinicians wishing to incorporate PoCUS in to their practice.17 The training outcomes for the CCPU are outlined in Figure 2.
Figure 2.
Learning Objectives for CCPU.
The Australasian College of Emergency Medicine (ACEM) encourages trainees to be competent in the key areas of ultrasound: abdominal aortic aneurysm, EFAST, procedural guidance and echo in life support. Of the specific clinical indications for PoCUS in the emergency department, identification of intrauterine pregnancy is the only obstetric and gynaecologic indication the ACEM supports.18
In the United States, emergency medicine is the only discipline that has formal requirements for its ultrasound training and credentialing, the Council for Graduate Medical Education (ACGME).19 The training of emergency physicians is governed by the ACGME in accordance with guidelines set out by the American College of Emergency Medicine (ACEP). The governing body in the United Kingdom is the Consortium for the Accreditation of Sonographic Education (CASE).20 There is no such governing body in Europe, and thus, training requirements and assessment of competency differ from country to country.21
Many studies have shown that clinicians are uncomfortable with their level of skill using PoCUS and would be interested in improving their skills.22, 23, 24 Moreover, confidence in the use of ultrasound appears to wane over time, possibly from lack of use or ongoing training.22 The efficacy of training programmes for students, residents and non‐clinicians such as nurses and midwives in the use of PoCUS has been explored extensively in the literature. The results are largely positive, suggesting that the training programmes result in increased confidence and improved performance in the use of ultrasound.25, 26 The courses described from many countries worldwide are highly variable in nature, duration and in the assessment of competency. It is thus impossible to compare the level of expertise reached by the participants, as there is no standardised assessment protocol. This variation in the level of competency has been identified and addressed by Jensen with a ‘mastery‐based’ learning protocol, by which trainees’ practice until they complete a predefined level of competency. This differs from traditional volume‐based programmes where a certain number of patients are examined, or hours of study are logged before the clinician is considered competent. It was shown by Jensen that the level of competency varied considerably using the volume type training.27 This approach has been studied among internal medicine residents.28 The obstetric units of the CCPU currently adopt a combination of contact hours in lectures and practical learning, formative and summative assessments supervised by a qualified clinician or sonologist and 25‐50 logged cases, depending on the unit.29, 30, 31 This is similar to the RANZCOG format and is typical of a volume‐based protocol.
There is paucity in the literature regarding the experiences of obstetric specialists and their experiences with PoCUS. Based on survey results from other specialties such as paediatrics and internal medicine, there is a chance that obstetricians feel unable to maintain their skills due to their existing workload and may suffer from lack of access to ongoing training and support from their hospital. Further research into PoCUS for obstetrics to address this issue would be useful. Similarly, there are a few studies looking at the use of PoCUS among gynaecology specialists. Acute pelvic pain is a common presenting complaint, with a differential diagnosis including ovarian cysts, which may be haemorrhagic, actively bleeding or torted, ruptured ectopic pregnancy, pelvic inflammatory disease and tubo‐ovarian abscess.32, 33, 34 PoCUS is highly utilised by emergency physicians in North America, and it has been suggested that it should be considered first line, as ultrasound lends itself well to the diagnosis of gynaecologic disorders.34 Transvaginal ultrasound has been shown to be useful for confirming high probability pre‐diagnoses, but not so much those with a low probability.35
A lack of confidence in PoCUS, of consulting obstetric and gynaecologic specialist, appears to extend to the studies performed by emergency clinicians. One survey from the United States showed that OBGYN specialists had a lower level of confidence in the scans performed by emergency physicians, compared to the Internal Medicine specialists who were surveyed. This lack of trust was especially prevalent where images were not available for review, and was less so for trauma scans, which are typically performed with consulting services present. This was thought to be due to a lack of awareness on the part of the consulting clinicians on the rigorous training and quality control for PoCUS in Emergency Medicine. This includes the sonographic assessment of pelvic pain relating to early pregnancy, though it is not specified if gynaecologic indications, other than ectopic pregnancy, are included in their training.21 The authors suggested that a better understanding of the training undergone by the emergency physicians may inspire more trust and confidence in the results, so that they may be better used in the decision‐making process.23
Examples of PoCUS from obstetrics and gynaecology
Listed below are several examples of how PoCUS has been used to reach a diagnosis in obstetrics and gynaecology.
Case 1
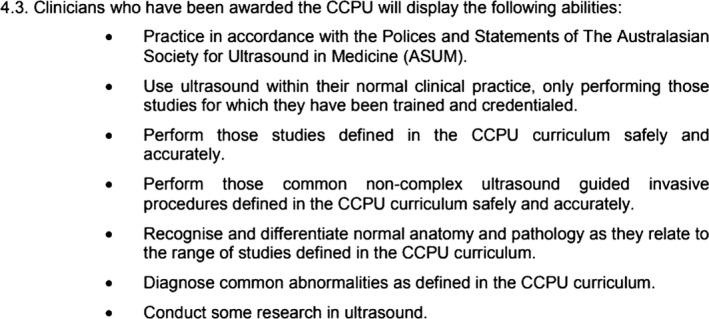
36/40 pregnant females seen in clinic with increased fundal height. PoCUS reveals polyhydramnios with a single deepest pocket 8 and above. Extreme changes in the amniotic fluid levels are a good indicator of fetal well‐being (Figure 3).36, 37
Figure 3.
Graph Indicating Polyhydramnios (Max Deep Pocket >99 percentile Tile as Seen on Ultrasound) Maximum Deepest Pocket 8 cm.
Case 2
Emergency Department presentation with abdominal pain and bleeding in early pregnancy (9W1D). PoCUS reveals no fetal heartbeat. Colour Doppler confirms fetal demise with no heart movement or flow seen within the fetal pole (Figure 4).
Figure 4.
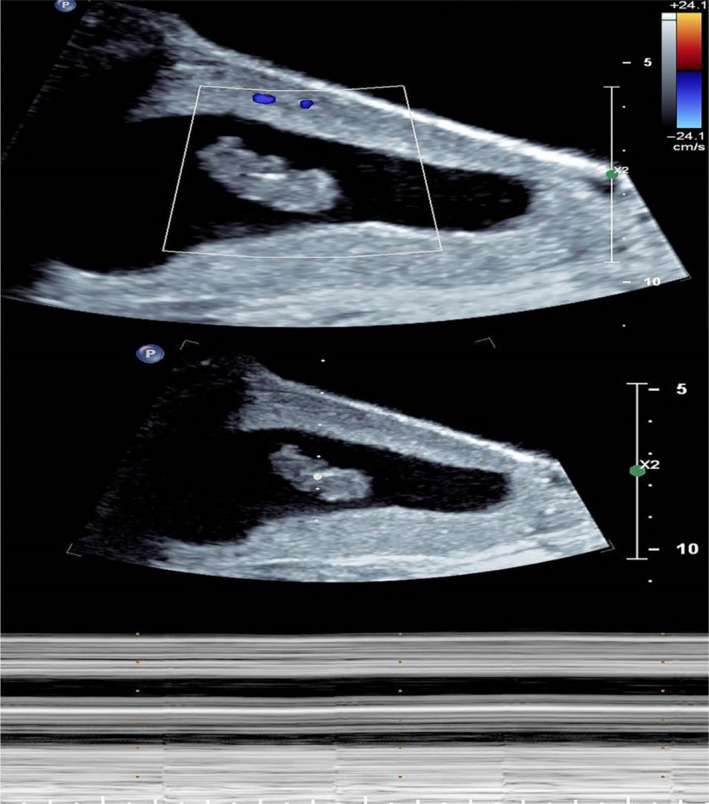
Colour Doppler Confirming Foetal Demise with no Flow Seen Within the Foetal Pole.
Case 3
Emergency Department scan of haemodynamically unstable female with an early pregnancy. PoCUS reveals no obvious intrauterine gestation with extensive free fluid (FF) and haematoma (open arrows) throughout the pelvis. Although not seen with PoCUS, a ruptured ectopic pregnancy is suspected and confirmed at the emergency surgery. Ovarian cyst (C) noted (Figure 5).
Figure 5.
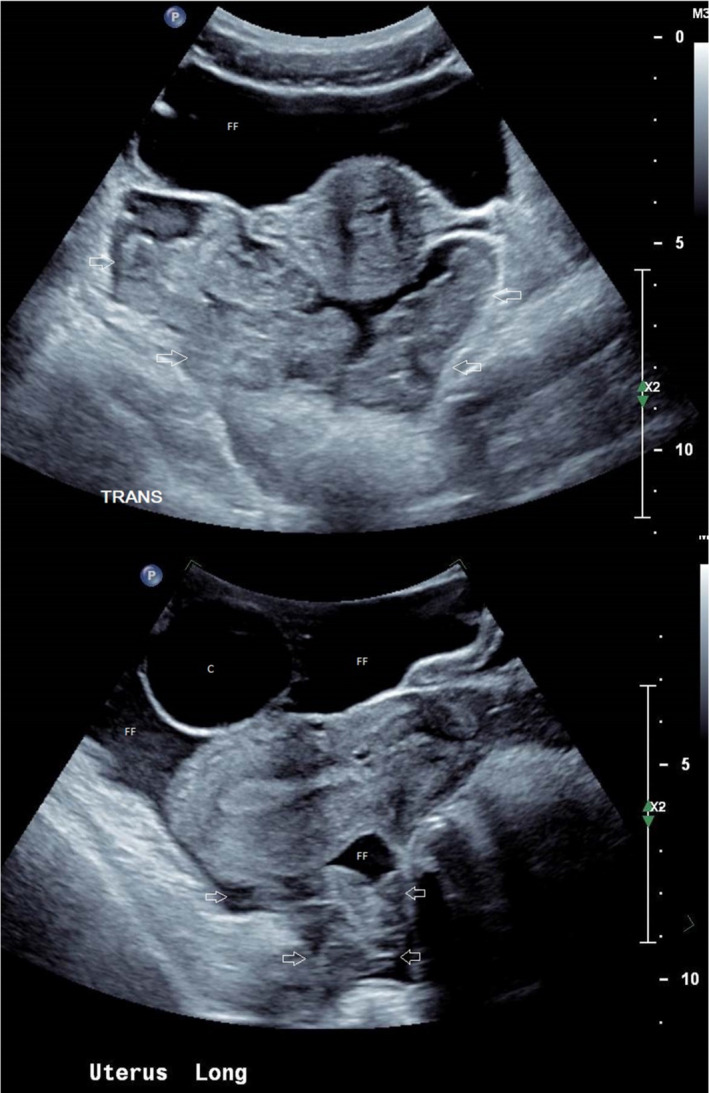
Ultrasound Demonstrating Free Fluid Throughout Pelvis and Haematoma. Ovarian Cyst Noted.
Case 4
22/40 pregnant females seen in ED with pelvic pain and contractions. PoCUS shows fluid within the cervix (open arrows). Departmental formal transvaginal scan confirms shortened cervix (Figure 6).
Figure 6.
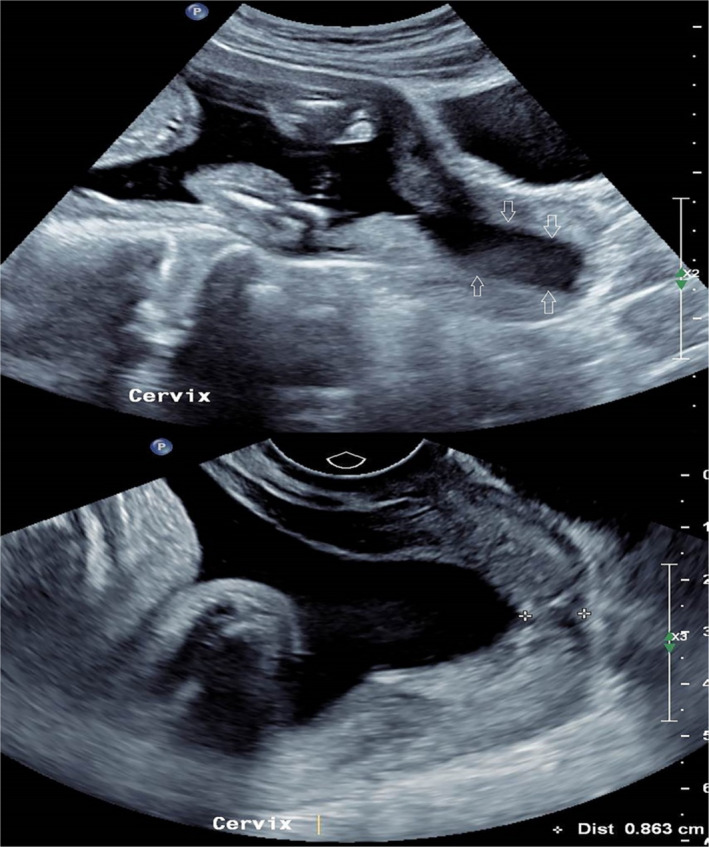
Trans‐abdominal Image Showing Fluid Within the Cervix, Indicating a Shortened Cervix.
Scope of practice
PoCUS examinations are limited, focused examinations, for answering specific questions. It has been said that PoCUS should be viewed as a rule – in modality – but a negative finding should not eliminate a diagnosis.38 It is thus crucial that the scope of practice for PoCUS should be discussed at a hospital or facility level. It is also widely acknowledged that guidelines are needed to ensure that PoCUS is performed safely, and to good effect.38, 39, 40
There are a significant number of case reports in the literature, which describe the use of PoCUS in exceptional circumstances. Examples of this include the diagnosis of uterine rupture, cervical ectopics, DVTs and pulmonary oedema associated with pre‐eclampsia, and fetal abnormalities and abnormal dopplers.41, 42, 43, 44, 45, 46, 47 This can be misleading as it suggests that clinician in the emergency or outpatient settings will be able to make these diagnoses themselves. These are rare clinical scenarios and require considerable training and experience. An average clinician would not get adequate exposure to these conditions to be able to identify the signs on ultrasound with confidence. It is therefore extremely important that clinicians understand the purpose of using PoCUS. For example, the ACEP guidelines support the use of PoCUS for assessing vaginal bleeding in early pregnancy but indicate that any bleeding occurring outside of this requires assessment by formal radiology services.21 Matthews and Zwank identified the lack of guidelines for the use of PoCUS in the hospital setting, but proposed that the existing emergency medicine guidelines may be used as a template.40
The bulk of the literature available examines the use of PoCUS in the emergency setting, and by ancillary staff such as midwives and nurses, but very little has been reported on PoCUS among obstetric clinicians. A study from 2004 identified that only 20% of obstetric trainees was planning on using PoCUS in their practice, although this figure may have significantly changed in the recent years, as PoCUS has become more widespread in its use.48
Limitations
The published literature on ultrasound training programmes for clinicians and non‐clinicians may be slightly misleading in suggesting that a short course, online or in person, and a completed logbook may be the only requirement to get appropriately trained in the delivery of PoCUS. Sonography is highly complex, takes rigorous training and assessment to master.21, 49 Ultrasound must also be practiced regularly in order to maintain competency. This may be an unrealistic undertaking for a previously unskilled, or busy clinician, regardless of their motivation to provide the service.50
The possibility of litigious action being taken against the clinician has been cited as a barrier to the uptake of PoCUS among emergency physicians.51 In favour of using PoCUS, a retrospective study looking at lawsuits relating to PoCUS in an emergency department showed only one case of medico‐legal action by a patient, and no cases of sexual assault were brought against the clinicians. The conclusion drawn by the authors was that legal action is more likely to take place due to failure to perform imaging at the bedside, resulting in delayed or missed diagnoses, than by performing the imaging.52
Another barrier to the implementation of PoCUS is the difficulty to use the ultrasound equipment. The ultrasound machine that a clinician must use in an emergency may be a different make or model that they may have trained on.53 There are a number of features required for image optimisation such as gain, depth, focal zone, zoom and technical aspects such as measuring callipers, mode and Doppler which may be difficult to navigate on an unfamiliar machine.54
Access to equipment has been identified as a barrier in rural settings, and the equipment that is available must be portable and robust enough to withstand potentially harsh environments and heavy wear.53, 55
An important consideration for any clinician undertaking a high volume of sonography as part of their practice is the risk of occupational musculoskeletal injuries. According to one study, it was found that 83% of physicians from a variety of specialties had experienced work‐ related musculoskeletal disorders. The most common sites affected with the spine, shoulder and wrist thought to be due to abnormal posture and asymmetric use of muscle groups.56
Conclusion
PoCUS is the use of ultrasound by the treating clinician as an extension of the physical exam to provide information in real time that can influence management. It is not a comprehensive examination and provides only limited information. Rigorous ongoing training and assessment are required of clinicians performing PoCUS, such that an adequate level of skill in the modality is maintained. The protocol for gaining credentialing in obstetrics and gynaecology is currently based on the volume of cases, where perhaps a mastery‐based programme would produce more skilled clinicians. Limitations to implementing PoCUS include time required to properly train and credential clinicians, lack of access to up to date equipment in rural areas, lack of standardisation of equipment and the risk of occupational injuries. Little research has been conducted into the use of PoCUS among OBGYN specialists, particularly the level of proficiency and confidence in the use of PoCUS, and the efficacy of training practices, which deserve further research.
Acknowledgements
The authors wish to thank Tina Hamlyn (Redcliffe QLD) for assisting with the manuscript.
References
- 1.Sporea I. Ultrasound for everyone – is it the right time? Med Ultrasonogr 2014; 16(1): 3–4. [DOI] [PubMed] [Google Scholar]
- 2.Dietrich CF, Goudie A, Chiorean L, Cui XW, Gilja OH, Dong Y, et al. Point of care ultrasound: a WFUMB position paper. Ultrasound Med Biol 2017; 43(1): 49–58. [DOI] [PubMed] [Google Scholar]
- 3.Australasian Society for Ultrasound in Medicine (ASUM) . Discussion Paper: Definition of Point of Care Ultrasound (POCUS), 2017, available from https://www.asum.com.au/standards-of-practice/.
- 4.Morgan BB, Kao A, Trent SA, Hurst N, Oliveira L, Austin AL, et al. Effect of emergency physician‐performed point‐of‐care ultrasound and radiology department‐performed ultrasound examinations on the emergency department length of stay among pregnant women at less than 20 weeks’ gestation. J Ultrasound Med 2018; 37(11): 2497–250. [DOI] [PubMed] [Google Scholar]
- 5.French S, Henry T, Williams EW. Evaluation of waiting times and sonographic findings in patients with first trimester vaginal bleeding at the university hospital of the West Indies. Can emergency department ultrasound make a difference?. West Indian Med J 2014;63(3):247–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Inal ZO, Inal HA, Gorkem U. Experience of tubo‐ovarian abscess: a retrospective clinical analysis of 318 patients in a single tertiary center in middle Turkey. Surg Infect (Larchmt) 2018; 19(1): 54–60. [DOI] [PubMed] [Google Scholar]
- 7.Becker DM, Tafoya CA, Becker SL, Kruger GH, Tafoya MJ, Becker TK. The use of portable ultrasound devices in low‐ and middle‐income countries: a systematic review of the literature. Tropical Med Int Health 2016; 21(3): 294–311. [DOI] [PubMed] [Google Scholar]
- 8.Dalmacion GV, Reyles RT, Habana AE, Cruz LMV, Chua MC, Ngo AT, et al. Handheld ultrasound to avert maternal and neonatal deaths in 2 regions of the Philippines: an iBuntis® intervention study. BMC Pregn Childbirth 2018; 18: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reynolds TA, Amato S, Kulola I, Chen CJ, Mfinanga J, Sawe HR. Impact of point‐of‐care ultrasound on clinical decision‐making at an urban emergency department in Tanzania. PLoS ONE 2018; 13(4): e0194774–e0194774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bentley S, Hexom B, Nelson BP. Evaluation of an obstetric ultrasound curriculum for midwives in Liberia. J Ultrasound Med 2015; 34(9): 1563–8. [DOI] [PubMed] [Google Scholar]
- 11.Kimberly HH, Murray A, Mennicke M, Liteplo A, Lew J, Bohan JS, et al. Focused maternal ultrasound by midwives in rural Zambia. Ultrasound Med Biol 2010; 36(8): 1267–72. [DOI] [PubMed] [Google Scholar]
- 12.Vinayak S, Sande J, Nisenbaum H, Nolsøe CP. Training midwives to perform basic obstetric point‐of‐care ultrasound in rural areas using a tablet platform and mobile phone transmission technology‐A WFUMB COE project. Ultrasound Med Biol 2017; 43(10): 2125–32. [DOI] [PubMed] [Google Scholar]
- 13.Filly RA. Is it time for the sonoscope? If so, then let's do it right!. J Ultrasound Med 2003; 22(4): 323–5. [DOI] [PubMed] [Google Scholar]
- 14.Tolsgaard MG. Assessment and learning of ultrasound skills in Obstetrics & Gynecology. Dan Med J 2018;65(2):pii: B5445. [PubMed] [Google Scholar]
- 15.Abuhamad A, Minton KK, Benson CB, Chudleigh T, Crites L, Doubilet PM. Obstetric and gynecologic ultrasound curriculum and competency assessment in residency training programs: consensus report. Am J Obstet Gynecol 2018; 218(1): 29–67. [DOI] [PubMed] [Google Scholar]
- 16.RANZCOG . Ultrasound Training – Revised. 12 December 2016. Available from: https://www.ranzcog.edu.au/Training/Specialist-Training/Online-portfolio-assessments/Ultrasound-Training [16th August 2018].
- 17.The Australasian Society of Ultrasound in Medicine . (ASUM). Minimum education & training requirements for ultrasound practitioners. Australas J Ultrasound Med 2017; 20(3): 132–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Australian College of Emergency Medicine (ACEM) . Policy on the use of focussed ultrasound in emergency medicine 2006; 21(4). [Google Scholar]
- 19.Beal EW, Sigmond BR, Sage‐Silski L, Lahey S, Nguyen V, Bahner DP, et al. Point‐of‐care ultrasound in general surgery residency training: a proposal for milestones in graduate medical education ultrasound. J Ultrasound Med 2017; 36(12): 2577–84. [DOI] [PubMed] [Google Scholar]
- 20.Harrison G. Summative clinical competency assessment: a survey of ultrasound practitioners’ views. Ultrasound 2015; 23(1): 11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whitson MR, Mayo PH. Ultrasonography in the emergency department. Critical Care (London, England) 2016; 20(1): 227–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Acar Y, Tezel O, Salman N, Cevik E, Algaba‐Montes M, Oviedo‐García A, et al. 12th WINFOCUS world congress on ultrasound in emergency and critical care. Critical Ultrasound J 2016; 8(Suppl 1): 12–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hansen W, Mitchell CE, Bhattarai B, Ayutyanont N, Stowell JR. Perception of point‐of‐care ultrasound performed by emergency medicine physicians. J Clin Ultrasound JCU 2017; 45(7): 408–15. [DOI] [PubMed] [Google Scholar]
- 24.Henwood PC, Beversluis D, Genthon AA, Wilson CN, Norwood B, Silva D, et al. Characterizing the limited use of point‐of‐care ultrasound in Colombian emergency medicine residencies. Int J Emerg Med 2014; 7(1): 7–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah S, Adedipe A, Ruffatto B, Backlund BH, Sajed D, Rood K, et al. BE‐SAFE: bedside sonography for assessment of the fetus in emergencies: Educational intervention for late‐pregnancy obstetric ultrasound. Western J Emerg Med 2014; 15(6): 636–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stolz LA, Muruganandan KM, Bisanzo MC, Sebikali MJ, Dreifuss BA, Hammerstedt HS, et al. Point‐of‐care ultrasound training for non‐physician emergency care practitioners in rural Uganda. Trop Med Int Health 2015; 20(8): 1067–72. [DOI] [PubMed] [Google Scholar]
- 27.Jensen JK, Dyre L, Jørgensen ME, Andreasen LA, Tolsgaard MG. Simulation‐based point‐of‐care ultrasound training: a matter of competency rather than volume. Acta Anaesthesiol Scand 2018; 62(6): 811–9. [DOI] [PubMed] [Google Scholar]
- 28.Schnobrich DJ, Mathews BK, Trappey BE, Muthyala BK, Olson APJ. Entrusting internal medicine residents to use point of care ultrasound: towards improved assessment and supervision. Med Teach 2018; 00: 1–6. [DOI] [PubMed] [Google Scholar]
- 29.ASUM , Advanced Pregnancy Ulktrasondf, in Certificate in Clinician Performed Ultrasound (CCPU).
- 30.ASUM , Basic Early Pregnancy Ultrasound, in Certificate in Clinician Performed Ultrasound (CCPU).
- 31.ASUM , Basic First and Second Trimester Screening, in Certificate in Clinician Performed Ultrasound (CCPU).
- 32.Valentin L. Characterising acute gynaecological pathology with ultrasound: an overview and case examples. Best Pract Res Clin Obstet Gynaecol 2009; 23(5): 577–93. [DOI] [PubMed] [Google Scholar]
- 33.Cilotti A, Weiss C, Bagnolesi P, Campassi C, Bimbi M, Bartolozzi C. Echography in gynecologic emergencies. Radiol Med 1992; 83(5): 630–5. [PubMed] [Google Scholar]
- 34.Cicchiello LA, Hamper UM, Scoutt LM. Ultrasound evaluation of gynecologic causes of pelvic pain. Obstet Gynecol Clin North Am 2011; 38(1): 85–114, viii. [DOI] [PubMed] [Google Scholar]
- 35.Sayrac N, Bektas F, Soyuncu S, Sayrac V. The impact of goal‐directed transvaginal ultrasonography on clinical decision‐making for emergency physicians. Am J Emerg Med 2015; 33(7): 895–8. [DOI] [PubMed] [Google Scholar]
- 36.Magann EF, Sanderson M, Martin JN, Chauhan S. The amniotic fluid index, single deepest pocket, and two‐diameter pocket in normal human pregnancy. Am J Obstet Gynecol 2000; 182(6): 1581–8. [DOI] [PubMed] [Google Scholar]
- 37.Moore TR. The role of amniotic fluid assessment in evaluating fetal well‐being. Clin Perinatol 2011; 38(1): 33–46, v. [DOI] [PubMed] [Google Scholar]
- 38.Marin JR, Lewiss RE. Point‐of‐care ultrasonography by pediatric emergency physicians. Policy statement. Ann Emerg Med 2015; 65(4): 472–8. [DOI] [PubMed] [Google Scholar]
- 39.Blans MJ, Bosch FH. Ultrasound in acute internal medicine; time to set a European standard. Eur J Intern Med 2017; 45: 51–3. [DOI] [PubMed] [Google Scholar]
- 40.Mathews BK, Zwank M. Hospital medicine point of care ultrasound credentialing: an example protocol. J Hosp Med 2017; 12(9): 767–72. [DOI] [PubMed] [Google Scholar]
- 41.Ferrazzi E, Zullino S, Stampalija T, Vener C, Cavoretto P, Gervasi MT, et al. Bedside diagnosis of two major clinical phenotypes of hypertensive disorders of pregnancy. Ultrasound Obstet Gynecol 2016; 48(2): 224–31. [DOI] [PubMed] [Google Scholar]
- 42.Sehgal A, Crispi F, Skilton MR, deBoode WP . Clinician performed ultrasound in fetal growth restriction: fetal, neonatal and pediatric aspects. J Perinatol 2017; 37(12): 1251–8. [DOI] [PubMed] [Google Scholar]
- 43.Herman A, Dreazen E, Herman AM, Batukan CE, Holzgreve W, Tercanli S. Bedside estimation of Down syndrome risk during first‐trimester ultrasound screening. Ultrasound Obst Gynecol 2002; 20(5): 468–75. [DOI] [PubMed] [Google Scholar]
- 44.Pachtman S, Koenig S, Meirowitz N. Detecting pulmonary edema in obstetric patients through point‐of‐care lung ultrasonography. Obstet Gynecol 2017; 129(3): 525–9. [DOI] [PubMed] [Google Scholar]
- 45.Zieleskiewicz L, Pierrou C, Ragonnet B, Tourret M, Chau C, Craighero F, et al. Role of whole‐body ultrasound in severe pre‐eclampsia and post‐partum hemorrhage. Canadian J Anesthesia 2013; 60(8): 796–802. [DOI] [PubMed] [Google Scholar]
- 46.Avula R, Niemann M, Dorinzi N, Robinson K, Sharon M, Minardi J. Occult iliac deep vein thrombosis in second trimester pregnancy: clues on bedside ultrasound. Clin Pract Cases Emerg Med 2017; 1(3): 183–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee SH, Ryu S, Choi SW, Kim HJ, Kang TK, Chan OhS, et al. Acute type A aortic dissection in a 37‐week pregnant patient: an unusual clinical presentation. J Emerg Med 2017; 52(4): 565–8. [DOI] [PubMed] [Google Scholar]
- 48.Lee W, Hodges AN, Williams S, Vettraino IM, McNie B. Fetal ultrasound training for obstetrics and gynecology residents. Obstet Gynecol 2004; 103(2): 333–8. [DOI] [PubMed] [Google Scholar]
- 49.Salmon M, Landes M, Hunchak C, Paluku J, Malemo Kalisya L, Salmon C, et al. Getting it right the first time: defining regionally relevant training curricula and provider core competencies for point‐of‐care ultrasound education on the African continent. Ann Emerg Med 2017; 69(2): 218–26. [DOI] [PubMed] [Google Scholar]
- 50.Gold DL, Marin JR, Haritos D, Melissa Skaugset L, Kline JM, Stanley RM, et al. Pediatric emergency medicine physicians’ use of point‐of‐care ultrasound and barriers to implementation: a regional pilot study. AEM Educ Train 2017; 1(4): 325–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Austin Terry JBLB. PoCUS – Where do I begin?, 2017. Available from: https://www.aci.health.nsw.gov.au/networks/eci/clinical/clinical-resources/clinical-tools/ultrasound-in-the-ed/pocus—where-do-i-begin (16th August 2018).
- 52.Blaivas M, Pawl R. Analysis of lawsuits filed against emergency physicians for point‐of‐care emergency ultrasound examination performance and interpretation over a 20‐year period. Am J Emerg Med 2012; 30(2): 338–41. [DOI] [PubMed] [Google Scholar]
- 53.Anticona Huaynate CF, Pajuelo Travezaño MJ, Correa M, Mayta Malpartida H, Oberhelman R, Murphy LL, et al. Diagnostics barriers and innovations in rural areas: insights from junior medical doctors on the frontlines of rural care in Peru. BMC Health Services Res 2015; 15: 454–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Enriquez JL, Wu TS. An introduction to ultrasound equipment and knobology. Crit Care Clin 2014; 30(1): 25–45, v. [DOI] [PubMed] [Google Scholar]
- 55.Nelson BP, Melnick ER, Li J. Portable ultrasound for remote environments, Part I: feasibility of field deployment. J Emerg Med 2011; 40(2): 190–7. [DOI] [PubMed] [Google Scholar]
- 56.Wareluk P, Jakubowski W. Evaluation of musculoskeletal symptoms among physicians performing ultrasound. J Ultrason 2017; 17(70): 154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]