Abstract
Approximately 25% of cancer patients suffer from chronic cancer-related fatigue (CCRF), which is a complex, multifactorial condition. While there are evidence-based interventions, it remains unclear what treatment works best for the individual patient. Psychological network models can offer a schematic representation of interrelations among fatigue and protective and perpetuating factors for the individual patient. We explored whether feedback based on these individual fatigue networks can help personalize psychological care for CCRF. A 34-year old woman with CCRF was referred to our mental healthcare institute for psycho-oncology. During the waitlist period, she filled out an experience sampling app for 101 days, including five daily assessments of fatigue, pain, mood, activity and fatigue coping. The interplay between items was visualized in network graphs at the moment-level and day-level, which were discussed with the patient. For example, acceptance of fatigue in the past three hours was associated with less hopelessness and less fatigue in the following moment. At the day-level, acceptance was also being associated with less fatigue, less hopelessness, a better mood, and more motivation to do things. The patient recognized these patterns and explained how unexpected waves of fatigue can make her feel hopeless. This started a dialogue on how cultivating acceptance could potentially help her handle the fatigue. The patient would discuss this with her therapist. Feedback based on individual fatigue networks can provide direct insight into how one copes with CCRF and subsequently offer directions for treatment. Further research is needed in order to implement this in clinical practice.
Keywords: chronic cancer-related fatigue, personalized medicine, network approach, case study, experience sampling method, acceptance, clinical practice
Introduction
Fatigue is one of the most prevalent and disrupting side effects of cancer and its treatment. It is characterized by feelings of weakness, exhaustion, and lack of energy. This fatigue differs from typical tiredness as it is not alleviated by rest or sleep, nor is it proportional to recent exertion (Berger et al., 2015). In approximately 25% of patients, fatigue persists for months to years after completion of cancer treatment (Thong et al., 2020). This persisting fatigue is defined as chronic cancer-related fatigue (CCRF). The unpredictable nature of CCRF with sudden drops in energy makes it difficult for patients to live their lives. CCRF is associated with reduced quality of life and heightened distress (Arndt et al., 2006; Thong et al., 2020). It interferes with patients’ ability to work, their daily life activities and social relationships (Bootsma et al., 2020; Duijts et al., 2014).
Despite its prevalence and disrupting effects, the etiology of CCRF remains poorly understood. Evidence suggests CCRF is a complex multifactorial condition, affected by a range of physiological (e.g., inflammation), clinical (e.g., comorbidities, cancer treatment), and psychosocial factors (e.g., distress) (Thong et al., 2020; Wagner & Cella, 2004). For example, during cancer treatment fatigue often co-occurs with symptoms such as pain, sleep problems, loss of appetite and withdrawal, collectively known as cytokine-induced sickness behaviors (Dantzer et al., 2008). Sickness behavior is an adaptive response to inflammation and is believed to preserve energy resources to fight illness and promote healing processes (Dantzer et al., 2008), which is very helpful during cancer treatment. Due to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis and other underlying physiological mechanisms, fatigue can persist long after completion of cancer treatment (Yang et al., 2019). While before cancer, patients had a general sense of how much rest was needed after exertion, now they have no idea whether and when they will recover from CCRF, making it very difficult to determine when to be active and when to rest.
So far, qualitative research has provided some insight into the unpredictable nature of fatigue throughout the day and from day to day (Bootsma et al., 2020; Levkovich et al., 2017). Patients suffering from CCRF usually report a continuous level of fatigue throughout the day with sudden appearances of exhaustion, often forcing the patient to lie down until the fatigue passes (Borneman et al., 2012; Levkovich et al., 2017). Patients also experience changes in fatigue at the day-level, with some days of energy, while on others there is none (Bootsma et al., 2020). While these studies provide some understanding of the course of CCRF, in order to help patients to get more grip on their fatigue we need to gain more insight into what factors affect CCRF, both throughout the day and from day to day.
Following the multifactorial etiology of CCRF, several types of treatments have proven effective in coping better with CCRF. These include both psychosocial interventions (e.g., cognitive behavioral therapy, mindfulness-based cognitive therapy) as well as physical activity interventions (e.g., exercise interventions, activity coaching) (Bruggeman-Everts et al., 2017; Kessels et al., 2018; Mustian et al., 2017). While these interventions have proven to be effective in reducing CCRF, it is unknown what intervention is most suitable for the individual patient. In order to unravel what treatment works best for whom, we need to help patients gain more insight into the factors that worsen or relieve their CCRF (Thong et al., 2020).
Based on the literature, our clinical experience, and qualitative and quantitative research on CCRF (Bootsma et al., 2020; Schellekens et al., 2019), we developed an experience sampling app, termed ‘Energy inSight’, to unravel the perpetuating and protective factors of the individual patient’s CCRF. The experience sampling method (ESM) is a structured diary technique, in which a participant receives questions multiple times a day for multiple days on end about their thoughts, feelings, activities and context in their daily living environment (Csikszentmihalyi & Larson, 1987; Delespaul, 1995). This results in an intensive longitudinal dataset, making it possible to examine the interactions between symptoms, cognitions, emotions, and behavior in a detailed, ecologically valid manner at the level of the individual patient (Csikszentmihalyi & Larson, 1987). Such a rich dataset provides the opportunity to examine the interaction between fatigue and related factors on different time frames, allowing more insight into the elusive course of fatigue throughout the day and from day to day.
Despite concerns about the burden this method puts on patients, ESM has already shown promising first results concerning feasibility and usefulness in psycho-oncology research (Kampshoff et al., 2019). On a small scale, ESM has already found its way into clinical practice as a personalized screening tool in the field of depression and psychosis research (Bos et al., 2019; van Os et al., 2017). Research suggests that as patients are actively involved in collecting data and gain insight into the personal, contextualized dynamics of their daily life, ESM contributes to self-management and patient empowerment (Bos et al., 2019; Simons et al., 2015; Wichers et al., 2011).
A new way to make sense of this intensive longitudinal data and to gain insight into an individual’s symptom dynamics is the network approach. The network approach to mental disorders theorizes disorders as causally connected symptoms in a network structure (Borsboom & Cramer, 2013). Thus, rather than viewing symptoms as manifestations of a common cause (e.g., you feel depressed because you have a depressive disorder), symptoms are conceptualized as elements of a complex dynamical system (e.g., sleep problems can trigger fatigue and concentration problems, resulting in feelings of worthlessness and loss of enjoyment, which in turn can trigger a depressed mood). Consequently, such a network of strongly interconnected symptoms can fulfill the criteria of a mental disorder (Borsboom, 2017). Due to the self-sustaining nature, it can be difficult to get out of such a malfunctioning state, potentially explaining the chronic nature of certain disorders. Next to symptom measures, other theoretically relevant nodes can be included in the network to reveal the nature of the complex relationships and core mechanisms involved in disorders (van der Lee & Schellekens, 2020). As such, the network approach seems very well suited to apply to a complex, multi-factorial condition such as CCRF. By adding perpetuating and protective factors of CCRF to the network, we can gain more insight into what worsens or relieves a person’s fatigue. The network approach is supported by network analyses that offer a visual display of (causal) relationships between symptoms, cognitions, emotions, and behavior (Epskamp et al., 2017). These visualized person-specific networks are rather intuitive and easy to understand for researchers, therapists and laypersons alike, and therefore have the potential to be used in providing personalized feedback as well as supporting personalized interventions.
Only a handful of studies have explored the application and effectiveness of ESM-derived personalized feedback on daily life dynamics (Bak et al., 2016; Bos et al., 2020; Kramer et al., 2014; Kroeze et al., 2017; Van Roekel et al., 2017). For example, Van Roekel and colleagues (2017) demonstrated that personal lifestyle advice (based on descriptives and network graphs of daily life activities, social context, and pleasure ratings) resulted in higher positive affect and pleasure ratings among anhedonic young adults, compared to those not receiving feedback. Two case studies also explored the potential of providing feedback on symptom dynamics by using network analysis to inform treatment. Bak and colleagues (2016) showed how the dynamic symptom network of a patient with schizophrenia provided increased insight into relapse and recovery, facilitating the patients’ treatment. Moreover, Kroeze and colleagues (2017) described how the symptom network of a patient with treatment-resistant anxiety and depressive symptoms provided increased insight into the patient’s symptom dynamics, which was valued as useful by the patient and therapist and facilitated a new direction in treatment. In sum, adding ESM-derived feedback to standard care seems feasible and has the potential to improve treatment in psychological healthcare.
Aim of the Present Study
This case study aimed to explore the usability of providing feedback on symptom networks to a patient who sought help for CCRF in a mental health care institute for psycho-oncology. We explored whether the network provided new insights into CCRF and whether these insights helped to personalize treatment. To gain more insight into how symptom dynamics change over time, based on reported changes throughout the day and from day to day (Bootsma et al., 2020; Levkovich et al., 2017), we explored moment-level as well as day-level networks.
Methods
Design and Procedure
This case study was part of an n=5 proof-of-concept study in which we developed the experience sampling app Energy InSight, assessed its feasibility, and explored whether it contributed to psychological care for CCRF. This study was approved by our ethical review board METC Brabant (P1935). Patients suffering from CCRF who were referred to the Helen Dowling Institute, a mental healthcare institute for psycho-oncology in the Netherlands, were invited to participate. After providing written informed consent, patients received instructions and installed the ESM app on their own smart phone. They filled out the app while they were on the waitlist for psychological care. During the 21-day ESM period, patients received notifications at five quasi-random time intervals (i.e., three hour time windows) a day, and two questionnaires at a fixed time point in the morning and evening. The timing of the measurements was adjusted to the patients’ sleep-wake schedule. Patients had to fill out the measurements within 30 minutes after the notification, otherwise, it was considered missing. During the first or second treatment session patients discussed the fatigue networks with their therapist. In our proof-of-concept study, we have described in more detail how patients and therapists experience the ESM app Energy InSight and the resulting network reports (Bootsma et al., 2021).
One of these participants, who we will name Sylvia, was motivated to fill out the app for 100 days. This provided enough power to explore not only how fatigue and other factors affect each other from moment to moment, but also from day to day. Assessments for 100 days were deemed sufficient as simulation studies have shown adequate performance for estimating eight-node networks using 50 observations (e.g., Epskamp et al., 2017). With 100 assessments and a 15% dropout rate, which is common in ESM studies among cancer patients (Kampshoff et al., 2019), we expected to be able to estimate reliable networks of Sylvia’s ESM data. Like the other participants in the proof-of-concept study, Sylvia received the 21-day feedback at the first meeting with her therapist. Before the second meeting with her therapist she finished filling out the app for 100 days. After 100 days, the first and second author discussed with Sylvia the moment-level and day-level networks, which she later discussed with her therapist.
Case presentation
Sylvia was a 34 year old woman who was referred to the Helen Dowling Institute, a mental healthcare institute for psycho-oncology. She suffered from severe fatigue (score of 49, which is way above the severe fatigue cut-off of ≥35 on Checklist Individual Strength – Fatigue Severity subscale (Vercoulen et al., 1994)) for over a year by then. Two years prior she was diagnosed with ovarian cancer with bone metastases. The tumor was removed through surgery. Next, she received four rounds of chemotherapy, followed by two surgeries to remove the affected rib and vertebra. After one year of curative treatment, leading to chemotherapy-induced kidney failure, she received medical follow-up consultations every few months by an oncologist. She also suffered from inflammatory bowel disease and inflammatory rheumatism since her teenage years. She lived together with her partner, had a university education, and was fully incapacitated for work since her cancer diagnosis. Previously, she worked fulltime as a project leader.
While she had always struggled with fatigue due to her comorbidities, throughout her cancer treatment the fatigue worsened dramatically. Sylvia described she had particular trouble concentrating when she felt tired. When she tried to read a newspaper or do her administration, she could get headaches and become nauseous. This severely limited her daily life activities. Her experience of fatigue was rather similar from day to day. Usually, she had trouble starting the day, which usually took her a few hours. Fatigue increased throughout the day, with a dip in the late afternoon. She usually took a nap by then because she was unable to do any of her activities. She did, however, also experience unexpected waves of extreme fatigue that did not seem to be related to previous activities. During those moments, it was difficult to get through the day. Furthermore, when she had a particularly busy activity, for example when she went to a party, she had trouble dealing with all the stimuli and social interactions at once. As a result, she would be extra fatigued for the following two to three days.
ESM assessment
Based on quantitative (i.e., network analysis on group-level) and qualitative research findings (i.e., meta-ethnography) we developed the ESM app Energy InSight. For example, based on group-level networks (Schellekens et al., 2019; Wolvers et al., 2021), we decided to include items on acceptance of fatigue and a sense of control over fatigue in the app. Moreover, based on patients’ experiences of fatigue being intertwined with emotions (e.g., guilt) and pain, as shown in the meta-ethnography (Bootsma et al., 2020) we added items on emotions and pain to the app. This resulted in a selection of 24 items that were assessed 5 times a day in a period of 100 days. For the network modeling items on social context (location, company, type of company) were excluded, resulting in 21 items (see Table 1 for an overview of the items).
Table 1.
The selected nodes from the ESM app (n=447) per network
| Item | Scale options | M | (SD) | NW* | |
|---|---|---|---|---|---|
| Fatigue | Physically I feel | 0 = Exhausted; 100 = Energetic | 39.68 | 20.15 | 1 - 2 |
| Concentration | I am able to concentrate | 0 = Not at all; 100 = Very well | 48.22 | 26.72 | 1 - 2 |
| Motivation | I feel like doing fun things | 0 = Not at all; 100 = A lot | 65.71 | 23.96 | 1 - 2 |
| Pain | I am in pain | 0 = Not at all; 100 = A lot | 40.96 | 31.04 | 1 - 2 |
| Positive mood | 1 | ||||
| - Happy | I feel happy | 0 = Not at all; 100 = A lot | 74.06 | 20.28 | 2 |
| - Enthusiastic | I feel enthusiastic | 0 = Not at all; 100 = A lot | 76.56 | 21.02 | 2 |
| - Relaxed | I feel relaxed | 0 = Not at all; 100 = A lot | 59.17 | 31.65 | 2 |
| - Curious | I feel curious | 0 = Not at all; 100 = A lot | 86.22 | 15.22 | 2 |
| - Content | I feel content | 0 = Not at all; 100 = A lot | 45.08 | 25.56 | 2 |
| Negative mood | 1 | ||||
| - Frustrated | I feel frustrated | 0 = Not at all; 100 = A lot | 39.20 | 28.93 | 2 |
| - Agitated | I feel agitated | 0 = Not at all; 100 = A lot | 40.96 | 31.04 | 2 |
| - Down | I feel down | 0 = Not at all; 100 = A lot | 24.03 | 21.44 | 2 |
| - Insecure | I feel insecure | 0 = Not at all; 100 = A lot | 42.89 | 25.96 | 2 |
| - Guilty | I feel guilty | ||||
| In the past three hours… | 0 = Not at all; 100 = A lot | 25.82 | 26.69 | 2 | |
| Physically active | I was physically active | 0 = Not at all; 100 = A lot | 47.02 | 37.04 | 1 |
| Mentally active | I was mentally active | 0 = Not at all; 100 = A lot | 46.80 | 34.96 | 1 |
| Pondering | I thought about my energy level | 0 = Not at all; 100 = A lot | 84.22 | 25.40 | 1 |
| Allowing rest | I took into account my energy level by allowing myself rest (other than sleeping) | 0 = Not at all; 100 = A lot | 69.27 | 32.27 | 1 |
| Accepting | I thought “my energy level is okay right now” | 0 = Not at all; 100 = Strongly | 41.90 | 24.78 | 1 |
| Hopeless | I had the idea “my energy level will never improve” | 0 = Not at all; 100 = Strongly | 46.05 | 25.52 | 1 |
| Control | I had the idea “I could influence my energy level” | 0 = Not at all; 100 = Strongly | 57.37 | 28.92 | 1 |
NW1 = Network 1. Contemporaneous network; NW2 = Network 2. Temporal network.
Fatigue. Three items were used to assess different dimensions of fatigue: the physical level of fatigue (“Physically I feel… [exhausted to energetic]”), mental fatigue in the form of concentration difficulties (“I am able to concentrate”), and the motivation to do things (“I feel like doing fun things”). The item on physical fatigue was reverse scored such that a higher score reflected more fatigue.
Pain. Pain was assessed with the item “I am in pain”.
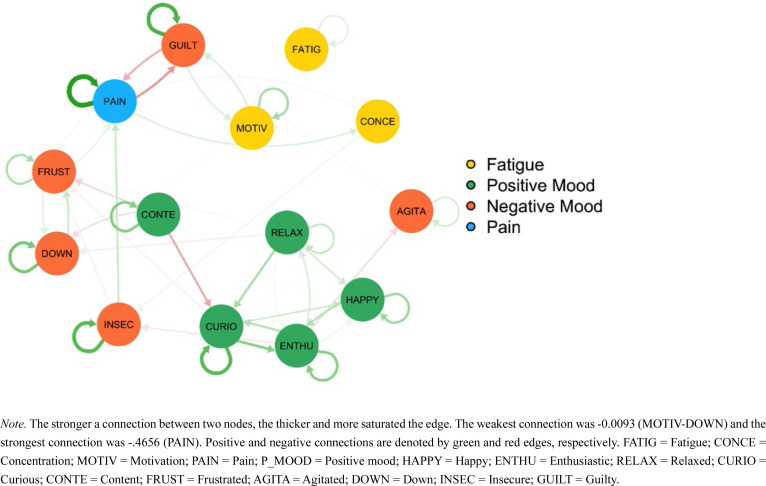
Mood. Mood was assessed with 10 affect items. Example items were “I feel content” and “I feel agitated”. In order to improve the interpretability of the contemporaneous network, which included all 21 items, affect items were aggregated into ‘positive mood’ (happy, enthusiastic, relaxed, curious, content) and ‘negative mood’ (frustrated, agitated, down, insecure, guilty).
Activity. Activity was assessed with two items: “In the past three hours I was physically active” and “In the past three hours I was mentally active”. Items were phrased in terms of ‘the past three hours’ because the average time between assessments was three hours.
Coping with fatigue. Five items assessed thoughts and behaviors concerning fatigue. These included pondering about the fatigue (“In the past three hours I thought about my energy level”), allowing oneself to rest when fatigued (“In the past three hours I took into account my energy level by allowing myself rest (other than sleeping) ”), accepting the level of fatigue as is (“In the past three hours I thought ‘my energy level is okay right now’”), feeling hopeless about one’s fatigue (“In the past three hours I had the idea ‘my energy level will never improve’”), and feeling in control of the fatigue (“In the past three hours I had the idea I could influence my energy level”). Items were phrased in terms of ‘in the past three hours’ because the average time between beeps was three hours.
Statistical Analysis
The data analysis plan was pre-registered online at Open Science Framework at the start of data collection (https://osf.io/wf8vc/). We estimated two moment-level network models: (1) A contemporaneous network model including all variables. To improve the readability of the contemporaneous network, we summarized the 10 mood items into two aggregated mood variables: positive mood and negative mood. (2) A temporal network model including the fatigue, pain and mood variables. See Table 1 for an overview of the variables per network. The temporal network model only contained fatigue, pain and mood variables as these items relate to the present moment. To prevent confusion regarding the interpretation, we left out items referring to the past three hours (i.e., coping with fatigue and activity variables).
Besides these moment-level network models, we also ran these network models at the day-level. For these network models, we used the average scores per day of each variable. Variables for the network models were selected based on sufficient variability (i.e., Mean Squared Successive Difference (MSSD) >50). In this case, the variability of all 21 variables proved sufficient. In the moment-level temporal networks we did not allow the first response of the day to regress on the last response of the previous day.
Network estimation
The contemporaneous and temporal networks were estimated using the R package graphicalVAR. In the contemporaneous network, ‘‘nodes’’ represent the selected variables while ‘‘edges’’ (i.e., links connecting two nodes) represent the partial contemporaneous correlations. In partial correlation networks the association between two nodes is estimated while controlling for all other nodes. This means that when an edge is present between two nodes, they are conditionally dependent given all other nodes.
A temporal network is based on partial directed correlations. In this model, a variable at a certain time point is predicted by the same variable at the previous time point (autoregressive effects) and all other variables at the previous time point (cross-lagged effects). The connections between nodes are depicted with arrows. An arrow from one node to another depicts a cross-lagged effect while an arrow directing to the same node depicts an autoregressive effect.
The graphicalVAR package uses penalized maximum likelihood estimation to estimate model parameters, while simultaneously controlling for parsimony (Abegaz & Wit, 2013; Rothman et al., 2010). The graphical-VAR package estimates 2,500 different models, varying 50 levels of parsimony in the contemporaneous network and 50 levels of parsimony in the temporal network. Bayesian information criterion (BIC) model selection is used to select the best fitting model. This means that edges that are likely to be spurious are removed from the model, leading to networks that are simpler to interpret (Epskamp et al., 2018; Epskamp & Fried, 2017).
The estimated models are displayed in network graphs. The stronger a connection between two nodes, the thicker and more saturated the edge. Based on the strongest connection, we have set a maximum edge strength of .55 for all network models to ensure that the thickness of the edges is comparable between models. Positive and negative connections are denoted by green and red edges, respectively. The networks were visually inspected and interpreted based on the strongest connections among variables.
Results
In a detailed personalized feedback report, the course of fatigue, moment-level and day-level network plots were presented to the patient and discussed with her by the first two authors after 101 days. Sylvia explained how she had no trouble filling out the app. She filled out 445 of the 501 assessments (88.8% compliance). Sylvia described how filling out the app for 101 days helped her to become more aware of her body. By answering the items every three hours, she actively monitored her energy level and sensed her boundaries more easily. This awareness allowed her to choose to rest in time and not overexert herself.
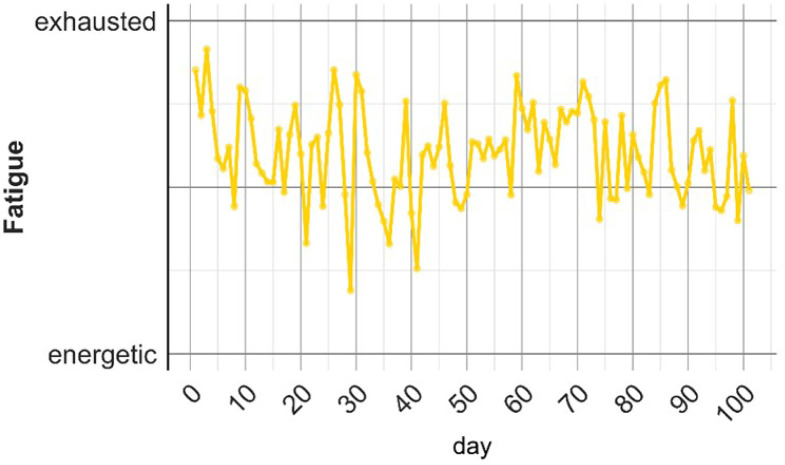
Course of Fatigue
On average, the level of fatigue increased throughout the day with a peak in the evening. Sylvia recognized this. She described how she often woke up tired and that the fatigue worsened with every activity she did. The average level of fatigue varied greatly from day to day with a majority of “fatigue” days and some days of “energy” (Figure 1).
Figure 1.
Average fatigue level from day to day
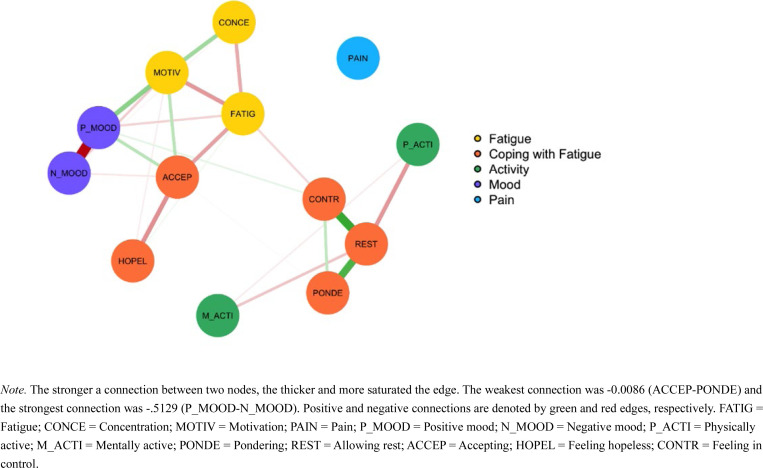
Moment-Level Contemporaneous Network
The contemporaneous moment-level network (Figure 2) included three items that were strongly connected to other items: Motivation, Acceptance and Allowing Rest. Regarding Motivation, there were connections with Fatigue, Concentration and Positive Mood. This suggests that when Sylvia was looking forward to doing fun things, she felt less fatigued, was better able to concentrate and experienced more positive emotions at that moment. Sylvia recognized this pattern in the sense that when she felt less fatigued she could undertake more and felt happier and more content.
Figure 2.
Moment-level contemporaneous network
Acceptance was connected to Fatigue and Hopelessness. This suggests that when she thought “the fatigue will never get better” in the past three hours, she was less okay with her energy level in the past three hours, and she experienced more fatigue in the following moment. Sylvia described how unexpected waves of fatigue could make her feel hopeless. She found it interesting that acceptance connected hopelessness with fatigue. Sylvia saw this as an opportunity. Becoming more aware of the changes in her fatigue, and being okay with her energy level for what it was, could help her deal more effectively with the fatigue and potentially decrease it.
Allowing Rest (other than sleep) was connected to Pondering about one’s fatigue level, having a sense of Control over one’s fatigue level and Physical Activity. Sylvia explained how filling out the app already helped her to relax more. For example, she usually would rest by doing the dishes. Now she realized that taking a good rest by doing nothing, just drinking a cup of tea, helped her to relax more, which gave her a sense of control over her fatigue. Interestingly, Allowing Rest was not directly related to Fatigue.
At the first meeting with her therapist, Sylvia had received feedback from the 21-day report. The connections in the moment-level contemporaneous network model based on the first 21 days were similar to the 101-day report, with the exception of Acceptance. In the 21-day report no connection was found between Acceptance and Fatigue.
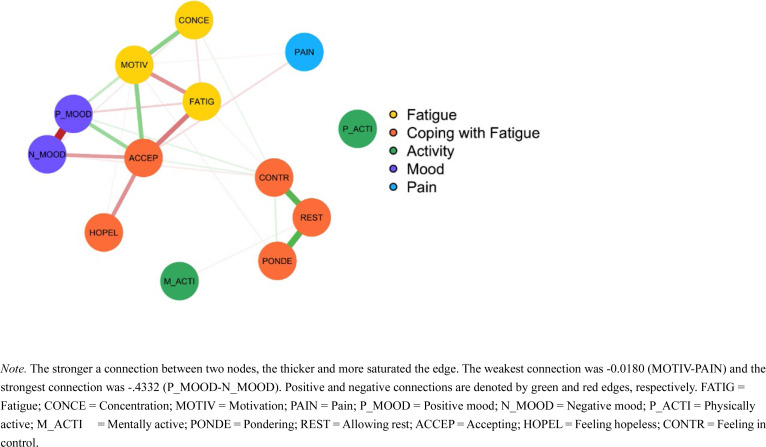
Day-Level Contemporaneous Network
The day-level contemporaneous network (Figure 3) was rather similar to the moment-level contemporaneous network. When visually inspecting the strongest connections among symptoms, the main difference concerned the connections of Acceptance with other nodes. Similar to the moment-level networks, Acceptance was connected to Hopelessness and Fatigue. In addition, the day-level network also showed connections of Acceptance with Negative Mood, Positive Mood and Motivation. This suggests that when Sylvia accepted her fatigue level for what it was on a certain day, she felt less hopeless regarding her fatigue, was in a less negative and more positive mood, felt more motivated to do things and experienced less fatigue that day. Sylvia recognized this and explained that when she was okay with her fatigue level, she generally felt better throughout the day.
Figure 3.
Day-level contemporaneous network
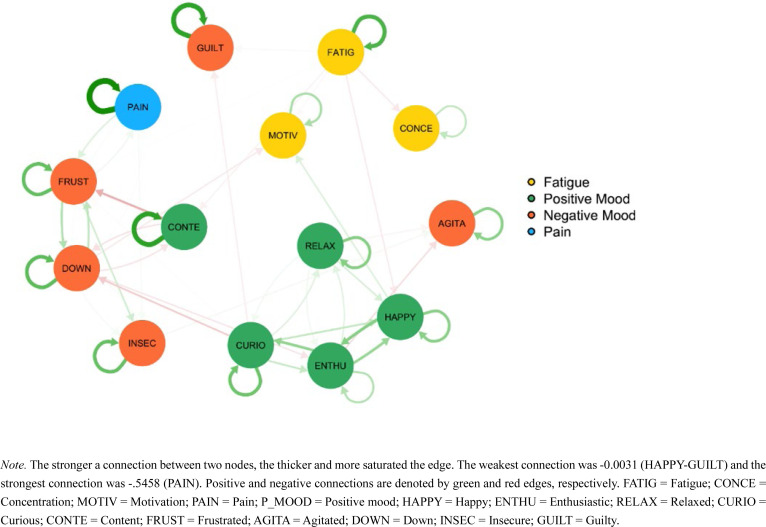
Moment-Level Temporal Network
The temporal network (Figure 4) included autoregressive effects of Fatigue, Pain, feeling Guilty and feeling Content. This means that, for example, when Sylvia was fatigued at one moment, she was more likely to be fatigued in the next moment (i.e., approximately 3 hours later). Sylvia described how fatigue and pain were the two main chronic symptoms she suffered from. She also recognized the feelings of guilt. She explained that when she was fatigued or in pain, she felt guilty about not taking good care of herself.
Figure 4.
Moment-level temporal network including Fatigue, Pain and Mood.
The connections of the moment-level temporal network of the 21-day report were similar to the connections found in the 101-day report, with the exception of pain. As pain did not show sufficient variability (MSSD <50) in the first 21 days, it was not included in the network.
Day-Level Temporal Network
Similar to the moment-level network, Pain and Guilt showed strong autoregressive effects in the day-level network (Figure 5). In addition, also feeling Curious and feeling Insecure showed autoregressive effects. At the day level, this means that, for example, when Sylvia experienced pain one day, she was likely to feel pain the next day. In contrast with the moment-level network, fatigue did not show a strong autoregressive effect at the day-level. This suggests that yesterday’s fatigue was not a strong predictor of today’s fatigue. Sylvia did not immediately recognize this and explained how attending a party could leave her tired for multiple days on end.
Figure 5.
Day-level temporal network
Experiences with feedback
While the temporal networks did not show connections between nodes over time, they portrayed some autoregressive effects. The contemporaneous network models provided insight into how we could create the best circumstances to help Sylvia handle her fatigue better throughout the day. Helping her to accept her fatigue level may help her handle her fatigue better and improve her wellbeing. Sylvia thought the network models were useful as they provided a deeper insight into what factors were important to her fatigue. All in all, she thought the networks were easy to understand and experienced the process of filling out the app and receiving feedback on the networks as positive.
Sylvia had already started cognitive behavioral therapy (CBT) with her therapist when she received feedback on the 101-days report. Based on the 21-day network report, feeling guilty about not taking good care of herself was already one of the main targets in treatment. The 100-day report confirmed these findings. In contrast to the 21-day report, both the moment-level and day-level contemporaneous network models of the 101-day report showed the importance of accepting her fatigue. Sylvia thought that a practice that helped her to become more aware of her fatigue level could help her accept her fatigue level better. Sylvia would take this up with her therapist.
Discussion
This case study showed how personalized feedback based on network graphs of ESM data can provide insight into the symptom dynamics of CCRF and provide opportunities for personalizing psychological treatment. From clinical practice and qualitative research we know that fatigue changes throughout the day but also from one day to the next (Bootsma et al., 2020; Levkovich et al., 2017). Sylvia also experienced this and was therefore motivated to fill out the ESM app for 100 days. This allowed us to assess both moment-level and day-level networks, gaining more insight into the elusive course of fatigue.
Filling out the ESM app for 101 days was feasible for our severely fatigued patient. She became more aware of her body and her boundaries. Sylvia thought the network models based on ESM data were useful as they provided insight into what factors were important to her fatigue. Interestingly, the moment-level networks based on 101 days provided additional insight beyond the networks based on the initial 21 days. Including more assessments helps estimating more reliable networks (Epskamp et al., 2017), potentially revealing connections that are not visible with less assessments. In Sylvia’s case, we found a connection between acceptance and fatigue after 101 days, which was not present after 21 days. Feeling more acceptant of her fatigue in the past three hours was associated with less fatigue in the following moment. The day-level network models were rather similar to the moment-level network models, suggesting that the factors were robustly associated with fatigue. That is, at the day-level, more acceptance was also associated with less fatigue and less hopelessness, as well as with a more positive mood and more motivation to do things. These findings suggested that Sylvia could benefit from treatment that helps cultivate acceptance.
One difference between the moment-level and day-level temporal networks was the autoregressive effect of fatigue. While fatigue from three hours ago predicted present-moment fatigue, yesterday’s fatigue was not such a strong predictor of today’s fatigue. The day-level network did not provide other insights beyond the moment-level network. More research is needed to examine whether the additional insight provided by day-level networks outweigh the burden of filling out the app for 100 rather than 21 days in clinical practice.
The present study provided insight into changes in CCRF throughout the day and from day to day. Although CCRF is chronic and experienced as continuously present, in this case fatigue appeared to increase over the course of a day and varied from day to day. Sylvia even experienced a few days of energy. However, in order to gain more insight into the course and symptom dynamics of CCRF we need to explore what time lag is the most optimal to study CCRF. The currently chosen time lag of approximately three hours between assessments was roughly based on our clinical experience with changes in CCRF and the burden of a maximum number of 5 assessments per day. Newly developed statistical methods can help determine the optimal time lag (Bringmann et al., 2017; Jacobson et al., 2019). A large-scale ESM study is needed with more assessments per day, allowing us to determine the optimal time lag, and to assess the extent of inter-individual differences.
The idiographic findings on the central role of acceptance are in line with recent findings from our cross-sectional group-level network model among 342 cancer patients seeking psychological care (Schellekens et al., 2019). In this study, we examined the interconnectedness among symptoms (anxiety, depression, fatigue) and risk and protective factors, showing that acceptance of illness appeared to be the most centrally embedded factor in the network, meaning it had more and stronger connections with other symptoms (e.g., less anxiety) and factors (e.g., less helplessness) in the network than other factors. Moreover, a recent meta-analysis of 78 studies demonstrated how acceptance of cancer is related to lower distress, anxiety and depression (Secinti et al., 2019). These findings emphasize the importance of coming to terms with one’s illness in the adjustment to cancer. Acceptance involves a non-judgmental and compassionate attitude towards one’s experiences (Hayes et al., 2004), thereby reducing the struggle with the realities of the illness and actively soothing one’s stress system (Lindsay et al., 2018).
Methodological issues
While this case study demonstrates a successful portrayal of how network models can facilitate personalizing psychological treatment for CCRF, the following methodological issues should be taken into account. First, as in any case study, the generalizability of the findings is limited as the network models are specific for this patient. It should be noted that the participant was a highly educated woman very motivated to gain insight in her CCRF. However, the present findings did show that the network models can provide interpretable and useful information, which is generalizable to other patients. By going beyond the usual severity scores, studying the unique patterns of connectivity among symptoms can facilitate the development of a personalized treatment plan.
Furthermore, the selection of relevant nodes is highly important for network models as results may differ depending on which symptoms are chosen for inclusion in network analyses. We might not have included all potentially relevant variables for this person, using the standardized questions of the Energy inSight ESM app. However, the selection of the Energy inSight items was based on patients’ experiences with CCRF (Bootsma et al., 2020), group-level network models in fatigued cancer patients (Schellekens et al., 2019) and the CCRF literature. More-over, Sylvia considered the items in the network as highly relevant. Offering patients the opportunity to add an item they consider relevant for their CCRF might be a valuable next step in using personalized feedback of network models in clinical practice (van Os et al., 2017).
Unfortunately, not all items could be included in the temporal networks as some items referred to the present moment (fatigue, mood, pain) while others referred to the past three hours (coping with fatigue, activity). A good alternative would be to only include items that can be framed in terms of the present moment. For example, the item on acceptance refers to the past three hours in the present study but could also be framed in terms of the present moment (i.e., “I consider my energy level as okay right now”). This will allow us to include the coping with fatigue items into the temporal network. Moreover, it makes full use of the in-the-moment reports that are unique to ESM and prevent memory bias (Delespaul, 1995).
Conclusion
Network models of the symptom dynamics of a single patient provided recognition of important factors (e.g., allowing rest, feelings of guilt) and new insight into coping with CCRF (e.g., acceptance of fatigue) that can be helpful in treatment. Furthermore, filling out the ESM app for 100 days was feasible for our patient, who suffered from severe CCRF, and provided additional insight on top of the feedback based on the initial 21 days. Further research is needed to determine whether the benefit of day-level networks outweighs the burden of prolonged ESM assessment.
Acknowledgements
We would like to thank Sylvia for her motivation to fill out the app for 101 days and her interest in receiving personalized feedback.
Author contributions
All authors designed the study. MS carried out the statistical analysis and drafted the manuscript. TB organized the data collection. RW helped with data collection and statistical analysis and drafted the personalized feedback reports. All authors helped to revise the manuscript and read and approved the final manuscript.
Declaration of interests
The authors declare that there are no conflicts of interests.
Funding
This study was funded by the Dutch Cancer Society (10761).
Action editor
Lars-Gunnar Lundh served as action editor for this article.
Open access
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
References
- Abegaz, F., & Wit, E. (2013). Sparse time series chain graphical models for reconstructing genetic networks. Biostatistics, 14(3), 586–599. 10.1093/biostatistics/kxt005 [DOI] [PubMed] [Google Scholar]
- Arndt, V., Stegmaier, C., Ziegler, H., & Brenner, H. (2006). A population-based study of the impact of specific symptoms on quality of life in women with breast cancer 1 year after diagnosis. Cancer, 107(10), 2496–2503. 10.1002/cncr.22274 [DOI] [PubMed] [Google Scholar]
- Bak, M., Drukker, M., Hasmi, L., & Van Jim, O. S. (2016). An n=1 clinical network analysis of symptoms and treatment in psychosis. PLoS ONE, 11(9), 1–15. 10.1371/journal.pone.0162811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger, A. M., Mooney, K., Alvarez-Perez, A., Breitbart, W. S., Carpenter, K. M., Cella, D., Cleeland, C., Dotan, E., Eisenberger, M. A., Escalante, C. P., Jacobsen, P. B., Jankowski, C., LeBlanc, T., Ligibel, J. A., Loggers, E. T., Mandrell, B., Murphy, B. A., Palesh, O., Pirl, W. F., … Smith, C. (2015). Cancer-related fatigue, Version 2.2015. Journal of the National Comprehensive Cancer Network, 13(8), 1012–1039. 10.6004/jnccn.2015.0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bootsma, T. I., Schellekens, M. P. J., van Woezik, R. A. M., Slatman, J., & van der Lee, M. L. (2021). Evaluation of an Experience Sampling app (Energy inSight) to help personalize behavioral interventions for chronic cancer-related fatigue: a proof-of-concept study [Unpublished Manuscript]. Scientific Research Department, Helen Dowling Institute. [Google Scholar]
- Bootsma, T. I., Schellekens, M. P. J., van Woezik, R. A. M., van der Lee, M. L., & Slatman, J. (2020). Experiencing and responding to chronic cancer-related fatigue: A meta-ethnography of qualitative research. Psycho-Oncology, 29(2), 241–250. 10.1002/pon.5213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borneman, T., Piper, B. F., Koczywas, M., Munevar, C. M., Sun, V., Uman, G. C., & Ferrell, B. R. (2012). A qualitative analysis of cancer-related fatigue in ambulatory oncology. Clinical Journal of Oncology Nursing, 16(1), E26–E32. 10.1188/12.CJON.E26-E32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13. 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, D., & Cramer, A. O. J. (2013). Network analysis: An Integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9(1), 91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Bos, F. M., Snippe, E., Bruggeman, R., Doornbos, B., Wichers, M., & van der Krieke, L. (2020). Recommendations for the use of long-term experience sampling in bipolar disorder care: a qualitative study of patient and clinician experiences. International Journal of Bipolar Disorders, 8(1), 38. 10.1186/s40345-020-00201-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos, F. M., Snippe, E., Bruggeman, R., Wichers, M., & van der Krieke, L. (2019). Insights of patients and clinicians on the promise of the experience sampling method for psychiatric care. Psychiatric Services (Washington, D.C.), 70(11), 983–991. 10.1176/appi.ps.201900050 [DOI] [PubMed] [Google Scholar]
- Bringmann, L. F., Hamaker, E. L., Vigo, D. E., Aubert, A., Borsboom, D., & Tuerlinckx, F. (2017). Changing dynamics: Time-varying autoregressive models using generalized additive modeling. Psychological Methods, 22(3), 409–425. 10.1037/met0000085 [DOI] [PubMed] [Google Scholar]
- Bruggeman-Everts, F. Z., Wolvers, M. D. J., van de Schoot, R., Vollenbroek-Hutten, M. M. R., & Van der Lee, M. L. (2017). Effectiveness of two web-based interventions for chronic cancer-related fatigue compared to an active control condition: Results of the “Fitter na kanker” randomized controlled trial. Journal of Medical Internet Research, 19(10), e336. 10.2196/jmir.7180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csikszentmihalyi, M., & Larson, R. (1987). Validity and reliability of the experience-sampling method. The Journal of Nervous and Mental Disease, 175(9), 526–536. 10.1097/00005053-198709000-00004 [DOI] [PubMed] [Google Scholar]
- Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness and depression: when the immune system subjugates the brain. Nature Reviews Neuroscience, 9(1), 46–56. 10.1038/nrn2297.From [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delespaul, P. A. E. G. (1995). Assessing schizophrenia in daily life. The Experience Sampling Method. Maastricht University Press. [Google Scholar]
- Duijts, S. F. A., van Egmond, M. P., Spelten, E., van Muijen, P., Anema, J. R., & van der Beek, A. J. (2014). Physical and psychosocial problems in cancer survivors beyond return to work: a systematic review. Psycho-Oncology, 23(5), 481–492. 10.1002/pon.3467 [DOI] [PubMed] [Google Scholar]
- Epskamp, S., Borkulo, C. D. Van, Date, C., Veen, V. Der, Servaas, M. N., Isvoranu, A., Riese, H., & Cramer, A. O. J. (2018). Personalized Network Modeling in Psychopathology: The Importance of Contemporaneous and Temporal Connections. 10.1177/2167702617744325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp, S., Borsboom, D., & Fried, E. I. (2017). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50, 195-212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp, S., & Fried, E. I. (2017). A Tutorial on Regularized Partial Correlation Networks. 10.1103/PhysRevB.69.161303 [DOI] [PubMed] [Google Scholar]
- Hayes, S. C., Follette, V. M., & Linehan, M. M. (2004). Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. Guilford Press. [Google Scholar]
- Jacobson, N. C., Chow, S. M., & Newman, M. G. (2019). The differential time-varying effect model (DTVEM): A tool for diagnosing and modeling time lags in intensive longitudinal data. Behavior Research Methods, 51(1), 295–315. 10.3758/s13428-018-1101-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampshoff, C. S., Verdonck‐de Leeuw, I. M., Oijen, M. G., Sprangers, M. A., & Buffart, L. M. (2019). Ecological momentary assessments among patients with cancer: A scoping review. European Journal of Cancer Care, 28(3), e13095. 10.1111/ecc.13095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessels, E., Husson, O., & van der Feltz-Cornelis, C. M. (2018). The effect of exercise on cancer-related fatigue in cancer survivors: a systematic review and meta-analysis. Neuropsychiatric Disease and Treatment, 14, 479–494. 10.2147/NDT.S150464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer, I., Simons, C. J. P., Hartmann, J. A., Menne-Lothmann, C., Viechtbauer, W., Peeters, F., Schruers, K., van Bemmel, A. L., Myin-Germeys, I., Delespaul, P., van Os, J., & Wichers, M. (2014). A therapeutic application of the experience sampling method in the treatment of depression: a randomized controlled trial. World Psychiatry, 13(1), 68–77. 10.1002/wps.20090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroeze, R., van der Veen, D. C., Servaas, M. N., Bastiaansen, J. A., Voshaar, R. C. O., Borsboom, D., Ruhe, H. G., Schoevers, R. A., & Riese, H. (2017). Personalized feedback on symptom dynamics of psychopathology: A proof-of-principle study. Journal for Person-Oriented Research, 3(1), 1-10. 10.17505/jpor.2017.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levkovich, I., Cohen, M., & Karkabi, K. (2017). The experience of fatigue in breast cancer patients 1–12 month post-chemotherapy: A qualitative study. Behavioral Medicine, 45(1), 7-18. 10.1080/08964289.2017.1399100 [DOI] [PubMed] [Google Scholar]
- Lindsay, E. K., Young, S., Smyth, J. M., Brown, K. W., & Creswell, J. D. (2018). Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology, 87, 63–73. 10.1016/j.psyneuen.2017.09.015 [DOI] [PubMed] [Google Scholar]
- Mustian, K. M., Alfano, C. M., Heckler, C., Kleckner, A. S., Kleckner, I. R., Leach, C. R., Mohr, D., Palesh, O. G., Peppone, L. J., Piper, B. F., Scarpato, J., Smith, T., Sprod, L. K., & Miller, S. M. (2017). Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: A meta-analysis. JAMA Oncology, 3(7), 961–968. 10.1001/jamaoncol.2016.6914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman, A. J., Levina, E., & Zhu, J. (2010). Sparse multivariate regression with covariance estimation. Journal of Computational and Graphical Statistics, 19(4), 947–962. 10.1198/jcgs.2010.09188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schellekens, M. P. J., Wolvers, M. D. J., Schroevers, M. J., Bootsma, T. I., Cramer, A. O. J., & van der Lee, M. L. (2019). Exploring the interconnectedness of fatigue, depression, anxiety and potential risk and protective factors in cancer patients: a network approach. Journal of Behavioral Medicine, 43, 553–563. 10.1007/s10865-019-00084-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secinti, E., Tometich, D. B., Johns, S. A., & Mosher, C. E. (2019). The relationship between acceptance of cancer and distress: A meta-analytic review. Clinical Psychology Review, 71, 27–38. 10.1016/j.cpr.2019.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons, C. J. P., Hartmann, J. A., Kramer, I., Menne-Lothmann, C., Höhn, P., van Bemmel, A. L., Myin-Germeys, I., Delespaul, P., van Os, J., & Wichers, M. (2015). Effects of momentary self-monitoring on empowerment in a randomized controlled trial in patients with depression. European Psychiatry, 30(8), 900–906. https://doi.org/DOI: 10.1016/j.eurpsy.2015.09.004 [DOI] [PubMed] [Google Scholar]
- Thong, M. S. Y., van Noorden, C. J. F., Steindorf, K., & Arndt, V. (2020). Cancer-related fatigue: Causes and current treatment options. Current Treatment Options in Oncology, 21(2), 17. 10.1007/s11864-020-0707-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Lee, M. L., & Schellekens, M. P. J. (2020). Capturing the complexity of mental disorders in the medically ill: the network approach on behavioral medicine. Translational Behavioral Medicine, 10(3), 812–816. 10.1093/tbm/ibz019 [DOI] [PubMed] [Google Scholar]
- van Os, J., Verhagen, S., Marsman, A., Peeters, F., Bak, M., Marcelis, M., Drukker, M., Reininghaus, U., Jacobs, N., Lataster, T., Simons, C., Lousberg, R., Gülöksüz, S., Leue, C., Groot, P. C., Viechtbauer, W., & Delespaul, P. (2017). The experience sampling method as an mHealth tool to support self-monitoring, self-insight, and personalized health care in clinical practice. Depression and Anxiety, 34(6), 481–493. 10.1002/da.22647 [DOI] [PubMed] [Google Scholar]
- Van Roekel, E., Vrijen, C., Heininga, V. E., Masselink, M., Bos, E. H., & Oldehinkel, A. J. (2017). An exploratory randomized controlled trial of personalized lifestyle advice and tandem skydives as a means to reduce Anhedonia. Behavior Therapy, 48(1), 76–96. 10.1016/j.beth.2016.09.009 [DOI] [PubMed] [Google Scholar]
- Vercoulen, J. H. M. M., Swanink, C. M. A., Fennis, J. F. M., Galama, J. M. D., van der Meer, J. W. M., & Bleijenberg, G. (1994). Dimensional assessment of chronic fatigue syndrome. Journal of Psychosomatic Research, 38(5), 383–392. 10.1016/0022-3999(94)90099-X [DOI] [PubMed] [Google Scholar]
- Wagner, L. I., & Cella, D. (2004). Fatigue and cancer: Causes, prevalence and treatment approaches. British Journal of Cancer, 91(5), 822–828. 10.1038/sj.bjc.6602012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichers, M., Simons, C. J. P., Kramer, I. M. A., Hartmann, J. A., Lothmann, C., Myin-Germeys, I., van Bemmel, A. L., Peeters, F., Delespaul, P., & van Os, J. (2011). Momentary assessment technology as a tool to help patients with depression help themselves. Acta Psychiatrica Scandinavica, 124(4), 262–272. 10.1111/j.1600-0447.2011.01749.x [DOI] [PubMed] [Google Scholar]
- Wolvers, M. D. J., Schellekens, M. P. J., Bruggeman-Everts, F. Z., Vollenbroek-Hutten, M. M. R., Bootsma, T. I., Cramer, A. O. J., & van der Lee, M. L. (2021). How are cancer-related fatigue symptoms interrelated with mental health and behavioral factors? A network approach [Unpublished Manuscript]. Scientific Research Department, Helen Dowling Institute. [Google Scholar]
- Yang, S., Chu, S., Gao, Y., Ai, Q., Liu, Y., Li, X., & Chen, N. (2019). A narrative review of cancer-related fatigue (CRF) and its possible pathogenesis. Cells, 8(7), 738. 10.3390/cells8070738 [DOI] [PMC free article] [PubMed] [Google Scholar]