It is an exciting time to be a heart failure (HF) physician. After decades of stagnation in the development of effective treatments for HF, we are now enjoying a surge in new medical therapies, greater insights into pathophysiology, and extraordinary innovation in percutaneous and surgical interventions. However, simultaneously, the number of individuals living with and dying from HF continues to grow, with widening racial disparities in HF-related deaths. In this landscape, the growth of a highly skilled, diverse, and agile advanced heart failure and transplant cardiology (AHFTC) workforce is essential.
It may be surprising, then, to those of us who are passionate about the HF field, that in the three years since AHFTC fellowship programs began participating in the Electronic Residency Application Service (ERAS) and the two years since joining the National Resident Matching Program (NRMP), the number of applications to AHFTC programs has plateaued, and a significant number of programs have gone unfilled. For the 2020 matriculation year, 84 individuals applied to AHFTC fellowships through the NRMP, filling 80 of 115 (70%) positions (4 applicants did not match), leaving 30 of 63 (48%) programs with vacancies. For the 2021 matriculation year, 77 applicants applied through the NRMP, filling only 75 of 118 (64%) positions, and leaving 35 of 70 (50%) programs unfilled.1 Of those applications submitted through ERAS but not entered into the Match, 106 were submitted for appointment year 2019, 129 were submitted for 2020, and only 120 were submitted for 2021.2 These data also reveal disappointing progress in enhancing the diversity of our AHFTC workforce: in 2020, the proportions of women and trainees who are underrepresented in medicine (UIM) entering AHFTC programs were just 35% (from 36% in 2014) and 9% (from 15% in 2014), respectively. Despite the beneficial impacts of physician-patient gender and racial/ethnic concordance, women comprised only 25.5% of board certified HF cardiologists in 2016, and UIM physicians comprised only 10%,3 a significant underrepresentation of the HF patient population.
Although it is possible that these trends are partly attributable to the official recognition of AHFTC as a cardiovascular disease (CVD) subspecialty only in 2013, its recent entry into the Match, or professional uncertainty and stress owing to the coronavirus disease 2019 (COVID-19) pandemic, a comparison with another cardiac subspecialty — namely, Clinical Cardiac Electrophysiology — suggests otherwise. Since its entry into the Match in 2019, Clinical Cardiac Electrophysiology has seen a steady increase in filled positions, from 81 of 130 positions (62%) in 2019, to 115 of 135 (85%) in 2020, to 124 of 129 (96%) in 2021.1 Similarly, Clinical Cardiac Electrophysiology received 91 ERAS applications for appointment year 2019, 129 for 2020, and 151 for 2021.2
Clearly, there are mismatches among the emerging workforce demands for AHFTC physicians, the HF community’s enthusiasm for the field, and trainees’ interest in and motivation to join this subspecialty. Herein we explore several factors that may deter trainees, especially women and UIM, from pursuing careers in AHFTC and discuss strategies for stimulating and sustaining HF career interest among the next generation of CVD specialists.
A Career in AHFTC: Perceived and Real Challenges
Several factors likely contribute to the high numbers of vacant AHFTC training slots. First, although learning to care for patients with HF is a foundational skill in CVD training, for many fellows, this knowledge is acquired without exposure to AHFTC physicians, to therapies such as ventricular assist device (VAD) and heart transplant (HT), or to accredited AHFTC programs. Currently, there are 268 Accreditation Council for Graduate Medical Education (ACGME)-accredited CVD programs but only 83 ACGME-accredited AHFTC fellowship programs. Additionally, although the number of centers performing HT (146) and VAD implantation (183) is increasing, a number of institutions with general CVD fellowships do not offer these therapies. Thus, CVD fellows encounter significant variability in access and exposure to AHFTC. Moreover, this heterogeneity leads to a dearth of potential mentors and sponsors in AHFTC, and this lack of role models may disproportionately impact UIM trainees.
Concerns about family planning and work-life integration, both during and after AHFTC fellowship, may also contribute to the reticence to pursue HF careers. A recent survey of 236 international HF cardiologists revealed that more than 45% of respondents perceived AHFTC to have a worse work-life balance than other CVD subspecialties. Respondents cited the complexity of the care of HF patients and frequent night and weekend responsibilities as sources of burnout.4 Trainees may feel that the rigorous AHFTC fellowship and practice are not compatible with early parenthood or that taking parental leave during the one-year fellowship may engender stigma or lead to deficiencies in skills and requirements. In fact, compared with men, a significantly greater proportion of AHFTC women physicians suffered negative career consequences for taking parental leave.3 These perceptions and realities continue to be genuine barriers to trainees considering AHFTC careers.
Job availability is also of paramount importance to trainees. Those who hope to pursue academic careers may perceive that VAD/HT faculty positions are already saturated. Of the 465 individuals who completed ACGME-accredited AHFTC training from 2014 to 2019, 60.2% do not currently have a faculty appointment at a U.S. medical school.5 Although this finding may reflect the growth and need for HF physicians outside of traditional academia, trainees who wish to work at academic institutions may instead pursue niches with a greater likelihood of attaining a faculty appointment. Alternatively, trainees who wish to work with medically underserved populations or in private practice settings may fear that the skills acquired during AHFTC fellowship may not translate to HF careers in which VAD/HT are not the focus or that their career paths may not be supported. Among physicians who completed AHFTC training between 2014 and 2019, 25.5% are practicing in federally designated medically underserved areas.5 Importantly, this factor may be of particular concern to UIM trainees, who are more likely to practice in underserved communities.
Strategies for Strengthening the Future AHFTC Workforce
The challenges described in this article are surmountable but will require intentional efforts by local and national AHFTC leadership. The following are suggested strategies to foster interest and recruitment into AHFTC training programs (Figure):
Figure.
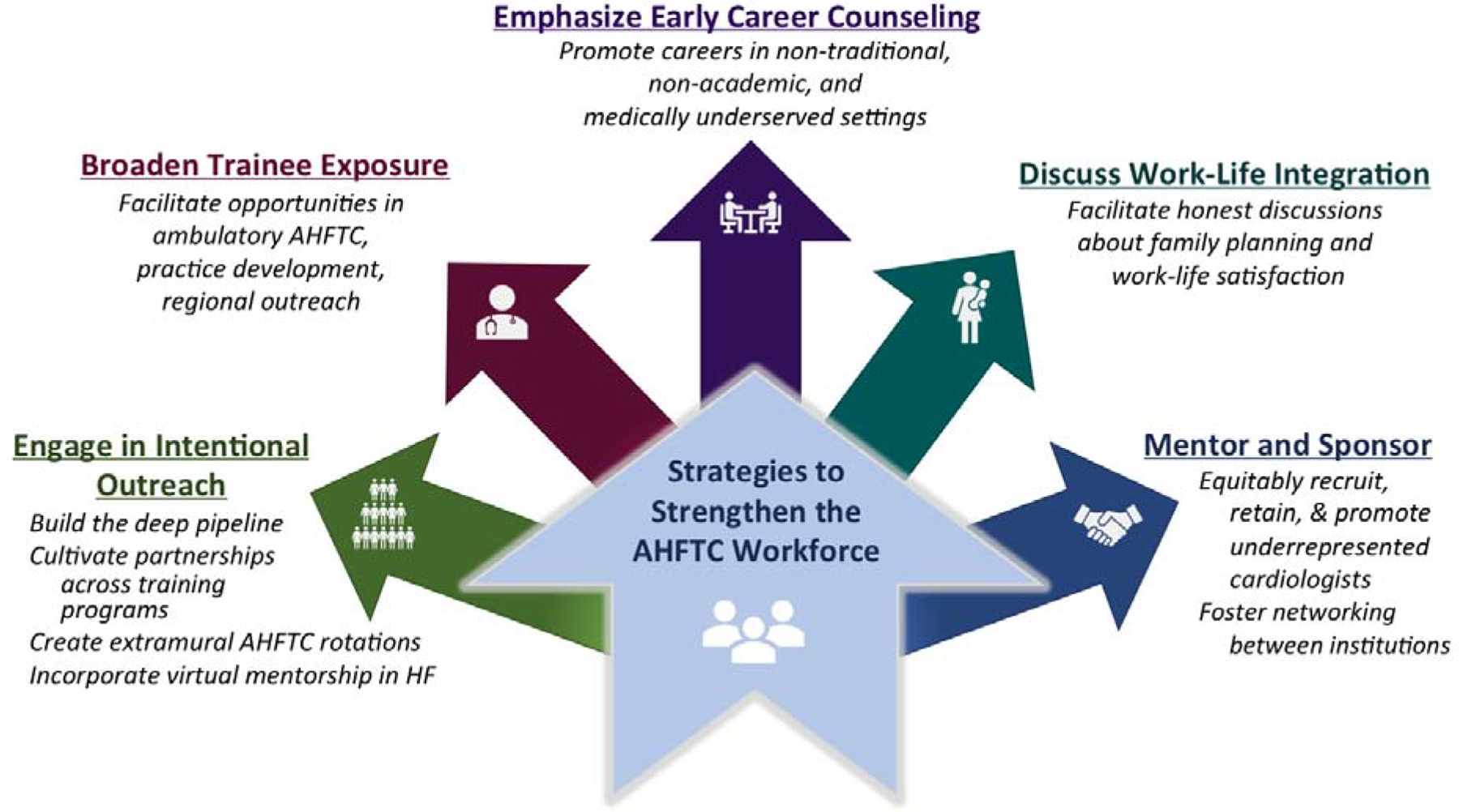
Strategies to Foster Interest and Increase Recruitment into Advanced Heart Failure and Transplant Cardiology Training Programs. Abbreviations: HF = heart failure; AHFTC = advanced heart failure and transplant cardiology.
Engage in intentional outreach: Professional CVD societies should develop and implement robust outreach campaigns to engage the deep pipeline with special attention to UIM students and general fellows at institutions without AHFTC fellowships. At the institutional level, general CVD fellowship program directors at institutions without AHFTC programs should cultivate partnerships with centers and programs that do offer these services and vice versa. Opportunities for general CVD fellows to electively rotate at AHFTC institutions should be widely explored and incentivized. Although the logistics of extramural rotations can be complicated, such experiences have been described as feasible and valuable.6 With the remarkable innovation in virtual education spurred by the coronavirus disease 2019 pandemic, general CVD programs without strong AHFTC curricula should consider incorporating virtual didactics from external HF experts. It is imperative for us to cultivate a diverse and inclusive workforce that is representative of the patients for whom we care.
Broaden trainee exposure: Trainees’ clinical HF exposure largely occurs in the inpatient setting. Although cardiogenic shock, mechanical circulatory support, and acute decompensated HF are foundational aspects of AHFTC, isolated experience with inpatient HF care may lead to a skewed vision of an AHFTC career. Many trainees are drawn to cardiac critical care and others are attracted to the fulfilling longitudinal patient relationships and other outpatient practice skills, such as the titration of guideline-directed medical therapies. Program leaders should facilitate ambulatory AHFTC opportunities for trainees. Exposure to outpatient AHFTC medicine allows trainees to appreciate the periods of clinical diastole in between intense inpatient service time.
Emphasize early career counseling: Trainees with AHFTC backgrounds are invaluable in a variety of practice settings and may pursue non-traditional career paths. Academic institutions and professional societies should foster relationships with clinicians in rural, medically underserved, private practice, and other non-academic settings and promote their perspectives on the value of AHFTC training to their careers. Career counseling must begin earlier in medical training, and we suspect this will help fellows better conceptualize their futures and connect with appropriate mentors.
Normalize discussions about extraprofessional life: AHFTC physicians should be transparent and honest with trainees regarding obstacles in family planning and work-life integration. Faculty should offer their perspectives on these topics and share their “survival strategies” even if unsolicited, because trainees may be hesitant to ask owing to a fear of being stigmatized. Similarly, AHFTC programs should ensure that their parental leave policies are fair, equitable, and easily accessible.
Mentor and sponsor early and often: Mentorship and sponsorship take many forms, from research partnerships to clinical training to the provision of local and national leadership opportunities, and can change the trajectory of a trainee’s career. AHFTC physicians should feel empowered and motivated to mentor trainees, especially those underrepresented in AHFTC and from outside their institutions. Gender and race/ethnicity concordance in mentoring relationships is associated with positive outcomes, and the AHFTC community should explore new and innovative ways to foster these networks, recognize and rectify existing disparities in AHFTC leadership, and equitably recruit, retain, and promote the next generation of HF cardiologists.
Conclusions
Decreasing the morbidity and mortality of HF in the current era relies upon the efforts of a diverse, competent, and vibrant AHFTC workforce. However, emerging data on recruitment into AHFTC fellowships signal a threat to the endurance of a clinician workforce that is sufficient to meet the rapidly evolving scientific, clinical, and leadership needs of the field of AHFTC. These challenges are daunting; however, our proposed strategies illuminate the path forward. There is great, untapped potential to attract CVD trainees to careers in AHFTC, and we must extend dedicated energy, enthusiasm, and resolve now to secure the future of our field.
Funding:
N.R. is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number KL2TR001879. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.National Resident Matching Program. Results and data: Available at: https://www.nrmp.org/main-residency-match-data/. AccessedMarch 9, 2021.
- 2.Association of American Medical Colleges. Electronic Residency Application Service Statistics: Available at: https://www.aamc.org/data-reports/interactive-data/eras-statisticsdata/. AccessedMarch 9, 2021.
- 3.Mehta LS, Fisher K, Rzeszut MA, et al. Current Demographic Status of Cardiologists in the United States. JAMA Cardiol. 2019;4(10):1029–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moayedi Y, Hershman SG, Ross HJ, Khush KK, Teuteberg JJ. Perceived Generational, Geographic, and Sex-Based Differences in Choosing a Career in Advanced Heart Failure: An International Survey. Circulation: Heart Failure. 2019;12(7):e005754. [DOI] [PubMed] [Google Scholar]
- 5.Association of American Medical Colleges. Electronic residency application service report on residents. Available at: https://www.aamc.org/data-reports/students-residents/interactive-data/table-c2-number-individuals-who-completed-residency-and-are-practicing-medically-underserved-areas. AccessedMarch 9, 2021.
- 6.Sivagnanam K, Mendes Lisa A, Schlendorf Kelly H, Damp JB, Stevenson LW, Ramu V, et al. Bridge to transplantation: advanced heart failure and transplant cardiology training for cardiovascular disease fellows. J Am Coll Cardiol 2017;70:1413–6. [DOI] [PubMed] [Google Scholar]


