Abstract
Caregivers are responsible for the care of another, such as a young adult, disabled child, elderly parent, or sick spouse. Individuals who have caregiving responsibilities must blend the often-contradictory behavioral expectations from the different roles in which they reside. Building on the theoretical foundations of Conservation of Resources theory, this study tests a mediational model explicating the process through which caregiver burden impacts mental health through work-family conflict among a community sample of 1,007 unpaid caregivers in the greater Chicago area who responded to a mail survey at three time points. Structural equation modeling analyses indicate strain-based conflict as being a consistent mediator between caregiver burden and mental health at baseline and two years later. These findings can inform practice and policy for workers with caregiving responsibilities.
Keywords: Caregiver burden, Work-family conflict, Family-work conflict, Depression, Anxiety, Conservation of Resources Theory
Introduction
According to the “Aging in the US” report from the Population Reference Bureau (2015), the number of Americans who are 65 years old or older is projected to more than double from 46 million to over 98 million by 2060. This will shift the 65-and-older age group’s share of the total population to nearly 24 percent (a 9 percent increase). These statistics are in line with global trends as well. According to World Health Organization (WHO), the proportion of the world’s population over 60 years old will nearly double from 12% to 22% between 2015 and 2050 (WHO, 2018, February 5). As individuals get older and experience limitations in performing their daily activities, they increasingly rely on assistance from others for their daily living and/or medical tasks. Another noteworthy trend is women’s substantial growth in the labor market. As the workforce becomes more balanced with respect to gender, and as women traditionally play a more important role in family caregiving (Smith, 2004), the informal caregiving role is becoming an increasingly important private and public issue.
Although some care recipients receive assistance from formal caregivers who are paid to provide care at home or in a care setting, the majority of care recipients’ assistance is provided by unpaid individuals, such as family or close friends. These informal, or unpaid, caregivers are defined as providing care to (1) a relative or friend at least 18 years old who cannot care for themselves or (2) a child under the age of 18 because of a medical, behavioral, or other condition or disability at any time in the last 12 months (National Alliance for Caregiving [NAC] & American Association for Retired Persons [AARP], 2015, p. 3). Currently, an estimated 43.5 million people in the United States provide unpaid care to an adult or a child (NAC & AARP, 2015).
It has also been noted that many individuals in the United States are expected to assume the role of an informal caregiver during their lives (Rospenda, Minich, Milner, & Richman, 2010). This is, in part, due to healthcare innovations that have led to longer life expectancies, pressures to keep individuals living in the community rather than in institutionalized homes, and the cost of formal in-home care (Rospenda et al., 2010). This inflation poses a particular threat to U.S. business as the current cost of informal caregiving, in terms of lost productivity to the U.S. economy, is estimated to be $25.2 billion annually (Gallup-Healthways Well-Being Survey, 2011). This is in line with research that has found that 69% of employed caregivers report having to adjust their work in order to meet their caregiving responsibilities (Feinberg, Reinhard, Houser, & Choula, 2011). Despite this trend, there has been relatively little research on the work-family dynamics of these caregivers (e.g., Li, Shaffer, & Bagger, 2015; Marks, 1998; Peng, Jex, Zhang, Ma, & Matthews, 2020). Quite understandably, keeping a balance between caregiving responsibilities and work can be highly demanding (Li et al., 2015). Such a task might require the diversion of personal resources such as time, energy, and finances from normal activities to caregiving responsibilities. Although some employers may provide flexible work arrangements to accommodate the needs of the caregivers, not all employees are lucky in that sense due to a host of personal factors (Lahaie, Earle, & Heymann, 2013) or organizational constraints. At the same time, people have different levels of personal resources to cope with the demands of caregiving, so the same level of caregiving may create greater burden for certain individuals, and as such may lead to greater conflict between work and family roles that both require the same resources. Thus, caregiver burden deserves further research in terms of its impact on both work-family dynamics and the health of employed caregivers.
Furthermore, while caregivers’ psychological and physical health issues are documented in various studies (e.g., Bainbridge, Cregan, & Kulik, 2006; McDonald, Poertner, & Pierpont, 1999; Rosenzweig, Brennan, & Ogilvie, 2002), there is not much research that has documented the prevalence and health consequences of caregiving among U.S. employees. Interestingly, the caregiving literature has tended to isolate the caregiving role from other roles (Gordon, Pruchno, Wilson-Genderson, Marcinkus, & Rose, 2012; Stephens & Franks, 1999). This is astounding as 60% of caregivers were also employed at some point in the past year (NAC & AARP, 2015). Furthermore, as detailed later, although the caregiving literature is extensive, much of it is published in the gerontological and family literature that is based on cross-sectional analyses of relatively small opportunity samples (i.e., only eldercare, childcare, or disabled care). These samples are typically based on non-representative samples that often include only women caregivers (Glavin & Peters, 2015; Gordon et al., 2012; Halinski, Duxbury, & Stevenson, 2020; Li et al., 2015; Marks, 1998; Schulz & Sherwood, 2008; Zuba & Schneider, 2013) and treat work-family conflict as a unidimensional construct, although there is evidence that indicates cross-domain and matching domain effects between family and work domains (Ford, Heinen, & Langkamer, 2007; Gordon et al., 2012; Huang, Hammer, Neal, & Perrin, 2004; Pearlin, Mullan, Temple, & Skaff, 1990).
While these studies contribute to our understanding of caregiving processes, researchers call for longitudinal studies that would help us understand the evolution of caregiving experiences over time and how they impact work-family dynamics (Calvano, 2013; Clancy et al., 2020; Griggs, Lance, Thrasher, Barnes-Farrell, & Baltes, 2020; Li et al., 2015).
To address these gaps in the literature, we extend research exploring the relationship between caregiver burden, work-family conflict processes, and employee mental health (i.e., depression and anxiety) over two years. First, we examine whether caregiver burden is associated with poorer mental health among a large community sample of employees. Then, we examine an unexplored mechanism that may explain the relationship between caregiver burden and mental health, namely the extent that processes related to the work-family interface contribute to this relationship. Testing this exploratory mechanism is important for both theory and practice. As such, it is a key issue of concern for the larger work-family literature (Peng et al., 2020) and for organizations. Prior research indicates that when caregivers are well supported at work and in community, the difficulties they experience are offset (Brown & Pitt-Catsouphes, 2016; NAC & AARP, 2015).
Caregiver Mental Health
According to the World Health Organization (WHO), mental health is “a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively, and is able to make a contribution to his or her community” (WHO, 2018, March 30). Depression and anxiety are the most common mental health issues in the world (WHO, 2017), and have been the most frequently examined consequences of caregiving (Barnett, 2015; McDaniel & Allen, 2012; Schulz & Sherwood, 2008; Stenberg, Ruland, & Miaskowski, 2010). Because caregivers often deal with a time-extensive, stressful, and high-pressure roles, they are more likely to experience depression and anxiety.
A compelling body of evidence suggests that caregivers are prone to higher rates of mental health problems than non-caregivers (Dekel, Solomon, & Bleich, 2005; Duxbury, Higgins, & Smart, 2011; Ho, Gilbert, Mason, Goodman, & Barker, 2009; Zacker, Jimmieson, & Winter, 2012). In a meta-analysis of 84 studies, Pinquart and Sorensen (2003) showed that caregivers experience more mental health problems and lower levels of general subjective well-being than those without caregiving responsibilities. They cited difficult caregiving tasks, restrictions in personal life, and illness-specific problems of the care recipient as common reasons that may impair caregivers’ mental and physical health. As such, acting as an informal caregiver may place individuals at increased risk to experience caregiver burden, stress, and role overload in addition to compassion fatigue or caregiver burnout (Honea et al., 2008; Nguyen, 2009; Whitebird et al., 2013). Overall, this line of research has consistently shown relatively large effects, which are moderated by various factors such as age, socioeconomic status, and availability of social support (Schulz & Sherwood, 2008).
Caregiver Burden and Mental Health
As caregiving is becoming an increasingly important private and public concern, the constructs related to caregiving have begun to attract the attention of organizational researchers as well as employers and policymakers. Of these constructs, caregiver burden is one of the most commonly examined, especially in medical and family journals that rely on samples with discrete care recipient populations; however, less has been published among employed populations (Hopps, Ladeluca, McDonald, & Makinson, 2017). Accordingly, caregiver burden has been studied as both a predictor and outcome in caregiver literature (Gordon et al, 2012; Savundranayagam & Montgomery, 2010) and is recognized as a negative effect of caregiving (Werner, Mittelman, Goldstein, & Heinik, 2012). Caregiver burden is defined as “the physical, psychological or emotional, social, and financial problems that can be experienced by family members caring for impaired older adults” (George & Gwyther, 1986, p. 253). It also has been argued that caregiver burden and general well-being are opposite sides of the same coin (George & Gwyther, 1986). As such, caregiver burden is associated with mental health problems (Lee, Walker, & Shoup, 2001; Savundranayagam, Montgomery, & Kosloski, 2011; Schulz & Sherwood, 2008; Pinquart & Sorensen, 2003).
Given that poor mental health has been linked to caregiving responsibilities and caregiver burden, understanding the mechanisms through which caregiving impacts mental health is critical (Barnett, 2015; McCann, Hebert, Bienias, Morris, & Evans, 2004), especially among the employed population. While the relationship between caregiving and mental health has been well-established, few studies have studied how caregiver mental health may be related to caregivers’ diverse life experiences and other life roles over time (Barnett, 2015; Pearlin et al., 1990) and the extent to which work-family processes are related to or influenced by caregiving (Glavin & Peters, 2015; Marks, 1998; Stephens et al., 2001). More specifically, work-family dynamics of caregivers have not received much attention in caregiving research despite its obvious relevance (Peng et al., 2020).
Work-family conflict (WFC) is defined as “a form of interrole conflict in which the role pressures from the work and family domains are mutually incompatible in some respect” (Greenhaus & Beutell, 1985, p. 77). In their review, Greenhaus and Beutell (1985) conceptualized WFC as a function of both the interference of work with family and family with work. As WFC is impacted by various factors, different forms of conflict have been proposed in the literature, the most commonly distinguished ones being strain-based and time-based conflict (Carlson, Kacmar, & Williams, 2000; La-pierre & Allen, 2006). Time-based conflict is experienced when time pressures associated with one role prevent one from fulfilling the expectations of a separate role, while strain-based conflict is experienced when strain in one role affects performance in a separate role (Kelloway, Gottlieb, & Barham, 1999, p. 338).
There is a consensus in prior research that WFC is associated with indicators of poorer psychological health (Amstad, Meier, Fasel, Elfering, & Semmer, 2011; Davis, Gere, & Sliwinski, 2017; Frone, 2000; Frone, Russell, & Barnes, 1996; Kinnunen, Geurts, & Mauno, 2004). As employed caregivers have increased family demands (i.e., caregiver burden), caregivers might face increased conflict between work and family roles as they are forced to make accommodations to respond to both caregiver and employee responsibilities. As such, these accommodations might have potential costs for both the caregiver and the employer. One study indicates that 70% of employed caregivers suffer work-related problems due to their dual roles (NAC & AARP, 2015). In that sense, the burden of caregiving has the potential to create significant role overload and conflict (McDaniel & Allen, 2012), which might ultimately result in mental health problems.
Theoretical Model and Development of Hypotheses
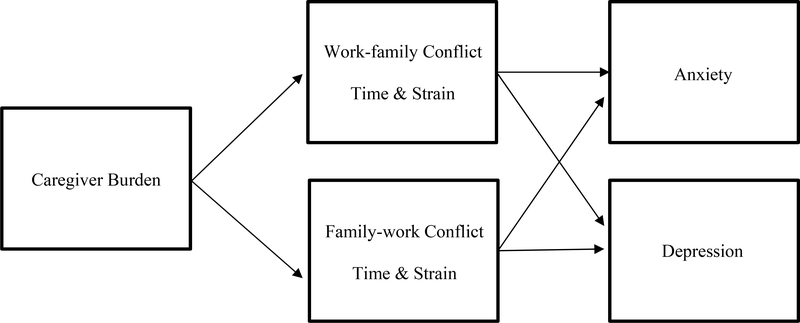
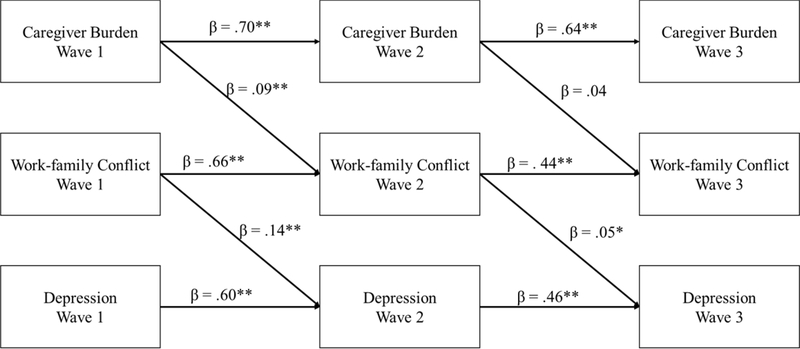
We hypothesize a theoretical model with WFC/FWC as the mediators of the relationship between caregiver burden and mental health (i.e., anxiety and depression; Figure 1). Prior research has indicated that role conflict mediates the relationship between various work-family demands and outcomes (Andrade & Mikula, 2014; Demerouti, Bakker, & Schaufeli, 2005; Frone, Russell, & Cooper, 1992; Hall, Dollard, Tuckey, Winefield, & Thompson, 2010; Judge & Colquitt, 2004). Overall, the literature indicates that demands in each domain are a threat to the work-family balance as these demands promote role conflict in each domain (La-pierre & Allen, 2006; Michel, Kotrba, Mitchelson, Clark, & Baltes, 2011). However, as noted before, while childcare has been primarily examined as family demand in the literature (Lee, Foos, & Clow, 2010), there has been relatively little research on how caregiving, an important family demand, is associated with work-family dynamics. Furthermore, while caregiver strain, stress, and demands have been the most frequently examined antecedents in the caregiving literature (Löckenhoff, Duberstein, Friedman, & Costa, 2011; Pearlin et al., 1990; Peng et al., 2020; Stephens, Townsend, Martire, & Druley, 2001), caregiver burden, as a broad multidimensional construct, has more rarely been studied (Gordon et al., 2012; Savundranayagam & Montgomery, 2010). We believe that this multidimensional construct (i.e., caregiver burden) can facilitate a better understanding of the various challenges facing informal caregivers.
Figure 1.
The Proposed Mediation Model.
Theoretically, there are several reasons why caregiver burden may contribute to interrole conflict and subsequent mental health problems. In line with previous research (Gordon & Rouse, 2013; Li et al., 2015; Peng at al., 2020; Zacher et al., 2012), we use the Conservation of Resources theory (COR; Hobfoll, 1989, 2002) as the theoretical framework for our study. Briefly, the theory posits that when an individual’s resources become exhausted, that individual will experience psychological strain, which may affect an individual’s general health (Hobfoll & Shirom, 2000). According to COR theory, interrole conflict leads to stress because resources are lost in the process of juggling multiple roles, which might lead to dissatisfaction, depression, anxiety, or physiological tension (Gordon & Rouse, 2013; Grandey & Cropanzano, 1999). In other words, engaging in one role might cause the individual to become less involved in the other role due to the shortage of resources and eventually result in interrole conflict (Gordon & Rouse, 2013; Greenhaus & Parasuraman, 1994). Thus, in line with COR theory, caregiver burden might inflict significant resource demands on employed caregivers, who must simultaneously deal with two different and demanding responsibilities. Consequently, from the perspective of cross-domain model of work-family conflict, employed caregivers might experience higher levels of interrole conflict, more specifically FWC, than non-caregivers (Li et al., 2015), which ultimately might lead to mental health problems.
A few notable studies on caregivers have examined the interrole conflict in the caregiving process in varying models. For example, Gordon et al (2012) examined the influence of caregiving and work demands as well as instrumental caregiving support and workplace emotional support on caregiving burden and work burden through role conflict in a sample of middle-aged employed women in a cross-sectional design. They found that WFC acted as a partial mediator between work burden and workplace support, a finding that is consistent with other cross-sectional research (Glavin & Peters, 2015; Stephens et al., 2001; Zuba & Schneider, 2013). In one notable longitudinal study, Marks (1998) found that the positive relationship between certain caregiving types (i.e., parent care, disabled childcare) and mental health is mediated by interrole conflict. In a more recent cross-sectional study, Peng et al. (2020) found that FWC mediates the relationship between eldercare demands and each partner’s time theft in a sample of Chinese dual-earner couples in a weekly diary design. Overall, the literature indicates that employed caregivers must meet demands beyond those facing non-caregivers and/or the unemployed; and interrole conflict transmits the effects of caregiving, often resulting in negative outcomes. However, as noted earlier, these prior studies are limited in several ways. Most are cross-sectional studies of specific sub-populations of caregivers (i.e., only eldercare, childcare, disabled care; caregivers over the age of 55; or only women caregivers), and focus on different aspects of caregiving (i.e., caregiver strain, caregiver stress) rather than caregiver burden, which is defined as the overall impact of the demands associated with caregiving. Furthermore, most of these studies have been characterized by small sample sizes with limited generalizability (Duxbury et al., 2011), treat WFC as a unidimensional construct while not accounting for FWC, and mostly utilize only the matching perspective (Ford et al., 2007; Gordon et al., 2012; Huang et al., 2004; Pearlin et al., 1990; Smoktunowicza et al., 2017).
As such, drawing upon COR theory, and in line with literature on caregivers (Gordon & Rouse, 2013; Peng at al., 2020; Stephens et al., 2001; Zacher et al., 2012), we propose that caregiving burden in the family domain depletes the resources (which may include time and energy as well as emotional, physical, financial, and other resources) of employed caregivers, which, in turn, lead to family-work conflict, which ultimately lead to mental health problems. As such, the following hypotheses are posited:
Hypothesis 1: FWC mediates the relationship between caregiver burden and anxiety.
Hypothesis 2: FWC mediates the relationship between caregiver burden and depression.
Evidence indicates that not only cross-domain but also matching domain effects between family and work domains may exist (Ford et al., 2007; Gordon et al., 2012, Huang et al., 2004; Pearlin et al., 1990; Smoktunowicza, Cieslak, & Demerouti, 2017). That is, FWC might have antecedents and consequences in the work domain while WFC might have antecedents and consequences in the family domain (Gordon et al., 2012). A review of the literature suggests that demands of the caregiving role and the employee role frequently interfere with each other (Gignac, Kelloway, & Gottlieb, 1996; Pearlin et al., 1990; Stephens et al., 2001; Stephens, Franks, & Atienza, 1997). Accordingly, caregiving and employment responsibilities may create interrole conflict in both family and work domains. Thus, we suggest that caregivers might experience increases in not only FWC but also WFC. More specifically, caregiver burden might carry over into not only work but also the family domain while various job demands might carry over into not only family but also the work domain. This is in line with Pearlin and colleagues’ research (1990), which suggests that caregivers “frequently experience cross-pressures and dilemmas at the junctures of caregiving and occupation” (p. 588). The above arguments give rise to the following hypotheses:
Hypothesis 3: WFC mediates the relationship between caregiver burden and anxiety.
Hypothesis 4: WFC mediates the relationship between caregiver burden and depression.
In sum, we respond to the call of previous scholars (Barnett, 2015; Chappel & Reid, 2002; Clancy et al., 2020; Gordon et al., 2012; Marks, 1998; Peng et al., 2020; Schulz & Sherwood, 2008) to explore the caregiving process and how the combination of multiple roles is associated with caregiver mental health over time, which has been identified as inherently complex and in need of more study. We address the limitations of previous research in the following ways: 1) we utilize three-wave longitudinal data from a large, diverse community-based sample of employed caregivers with varied caregiving responsibilities, 2) we examine mediating effects of both WFC and FWC, in line with matching and cross-domain perspectives, and 3) we assess mental health by assessing symptoms of both anxiety and depression.
Method
Data were collected between 2006 and 2010 in a three-wave survey of a community sample of adults (≥ 18 years) who had been employed at least 20 hours per week at some point in the past 12 months and who provided unpaid caregiving to one or more individuals. Random digit dial methodology was used to recruit participants who met these inclusion criteria from numbers randomly selected from block groups in the Chicago metropolitan area. In households with more than one eligible respondent, the Troldahl-Carter-Bryant method (Bryant, 1975; Troldahl & Carter, 1964) was used to select who would participate. A mailed self-report survey was sent to those who agreed to participate. Participants were resurveyed at 12-month intervals from when their first questionnaire was received. A 12-month lag was chosen because 1) 12 months allows for meaningful change in measured variables to take place; 2) the measures of depression and anxiety used here have demonstrated sensitivity to change over a 12-month time frame in our prior research; 3) the variables studied here were part of a fairly lengthy questionnaire, and in order to better control respondent burden, we limited requests for response to once per year. Participants received a $30 American Express gift card compensation for completing each wave of the questionnaire.
In Wave 1, 1,007 individuals completed the survey while 713 (70.8%) individuals completed Wave 2, and 689 (68.4%) completed Wave 3. To test for selective dropout at Waves 2 and 3, we examined if respondents who completed the questionnaire at that wave differed from those who did not complete a questionnaire at that wave on each study variable. Differences were found only for age, in that older respondents were more likely to complete a survey at Wave 2 (β=.035, s.e.=.007, p<.001) and Wave 3 (β=.031, s.e.=.007, p<.001), the average age being 43 years old (SD = 9.9). No significant differences were found between the completers and the dropouts in terms of gender, race/ethnicity, caregiver burden, WFC time or strain, FWC time or strain, or mental health at Wave 2 or Wave 3. Therefore, we concluded that with the exception of age, the dropouts were comparable to the completers at each wave and that no serious selection problems due to dropout had occurred.
Of the participants who completed all three questionnaires, 43.7% of the participants were white, 34.8% were African American, 15.7% were Latino/a, 4.9% were “other” race/ethnicity, and .9% was missing. Approximately 46% were male while roughly 54% were female. This sample consisted of caregivers who were responsible for children under the age of 18 (75.7%), children over the age of 18 (15.4%), a spouse/partner (24.1%), parents (21.5%), and/or siblings, aunts or uncles, and grandparents (less than 6% each). It is important to note that, although these percentages do not reflect the actual ratio in the US population (while eldercare is much more common in the population, childcare is predominant in our sample), the previous research indicates that eldercare providers report similar types of role conflict as childcare providers and caregiving recipient type is not associated with caregiver burden (Halinski et al., 2020; Lee et al., 2010).
Measures
Burden.
Caregiver burden was measured using a modified 23-item version of the Caregiver Burden Inventory (CBI; Novak & Guest, 1989) which measures burden in 6 areas: time-dependence (e.g., “I don’t have a minute’s break from my caregiving chores when I’m not at work”), developmental (e.g., “I feel that I am missing out on life because of caregiving”), physical (e.g., “My health has suffered because of caregiving”), social (e.g., “I’ve had problems with my spouse/partner because of caregiving”), and emotional (e.g., “I resent my care recipient(s)”). Each scale was measured by 4-items except for physical burden (3-items) and scored on a scale from 1 (not descriptive at all) to 4 (very descriptive). Alpha reliabilities for the overall burden scale were α = .87 or greater at each wave of the study (see Table 1 for details).
Table 1.
Descriptive statistics, correlations, and reliability scores.
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|
| ||||||||
| 1. Burden | 1.59 (.44) | (.88) | ||||||
| 2. WFC-Time | 2.34 (.79) | .29** | (.89) | |||||
| 3. WFC-Strain | 2.33 (.68) | .33** | .66** | (.84) | ||||
| 4. FWC-Time | 1.94 (.72) | .45** | .50** | .54** | (.82) | |||
| 5. FWC-Strain | 1.94 (.68) | .44** | .49** | .60** | .70** | (.89) | ||
| 6. Anxiety | 1.86 (.68) | .32** | .30** | .43** | .31** | .42** | (.87) | |
| 7. Depression | 1.60 (.64) | .32** | .29** | .41** | .29** | .40** | .68** | (.87) |
|
| ||||||||
| M (SD) | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|
| ||||||||
| 8. Burden | 1.63 (.42) | (.87) | ||||||
| 9. WFC-Time | 2.33 (.71) | .27** | (.87) | |||||
| 10. WFC-Strain | 2.35 (.61) | .32** | .64** | (.82) | ||||
| 11. FWC-Time | 1.98 (.69) | .39** | .46** | .49** | (.83) | |||
| 12. FWC-Strain | 1.99 (.64) | .39** | .47** | .59** | .65** | (.89) | ||
| 13. Anxiety | 1.90 (.72) | .29** | .28** | .40** | .27** | .40** | (.90) | |
| 14. Depression | 1.63 (.62) | .36** | .31** | .42** | .27** | .41** | 69** | (.85) |
|
| ||||||||
| M (SD) | 15 | 16 | 17 | 18 | 19 | 20 | 21 | |
|
| ||||||||
| 15. Burden | 1.62 (.42) | (.87) | ||||||
| 16. WFC-Time | 2.35 (.73) | .23** | (.88) | |||||
| 17. WFC-Strain | 2.36 (.63) | .36** | .64** | (.83) | ||||
| 18. FWC-Time | 1.95 (.70) | .48** | .47** | .49** | (.83) | |||
| 19. FWC-Strain | 1.99 (.66) | .49** | .44** | .55** | .70** | (.89) | ||
| 20. Anxiety | 1.90 (.72) | .36** | .27** | .44** | .26** | .41** | (.90) | |
| 21. Depression | 1.64 (.65) | .39** | .22** | .39** | .30** | .43** | .67** | (.87) |
|
| ||||||||
| Wave 1 – Wave 2 | Wave 1 – Wave 3 | Wave 2 – Wave 3 | ||||||
|
| ||||||||
| 22. Burden | .65** | .65** | .73** | |||||
| 23. WFC-Time | .57** | .61** | .59** | |||||
| 24. WFC-Strain | .63** | .59** | .63** | |||||
| 25. FWC-Time | .58** | .59** | .68** | |||||
| 26. FWC-Strain | .58** | .58** | .62** | |||||
| 27. Anxiety | .57** | .55** | .67** | |||||
| 28. Depression | .58** | .59** | .60** | |||||
Note. WFC is work-family conflict and FWC is family-work conflict. 1–7 (n ranges from 788–939) are at Wave 1, 8–14 (n ranges from 495–655) are at Wave 2, 15–21 are at Wave 3 (n ranges from 424–581). 22–28 compare each construct between waves as indicated (n ranges from 430–653).
is significant at p < .01. Alpha reliability levels are provided in bolded parentheses along the diagonal.
WFC/FWC.
The 22-item Work-Family Conflict Scale (Kelloway et al., 1999) was used to assess the conflict between work and family roles in one’s current job. The scale contains subscales for time-based WFC (5-items; e.g. “job demands keep me from spending the amount of time I would like with my family”), strain-based WFC (6-items; e.g., “I think about work when I am home”), time-based FWC (5-items; e.g., “My family demands interrupt my workday”), and strain-based FWC (6-items; “When I am at work, I am distracted by family demands”). All items were scored on a scale from 1 (never) to 4 (almost always). Alpha reliabilities of each subscale were α = .82 or greater at each wave of the study (Table 1).
Depression.
Depression was measured with 7-items from the Center for Epidemiologic Studies Depression Scale (Radloff, 1977). Items include, “In the last seven days, did you have trouble sleeping” and “In the last seven days, did you feel lonely.” All items were scored on a scale from 1 (rarely or none of the time; less than 1 day) to 4 (most or all of the time; 5–7 days). Alpha reliabilities were α = .85 or greater at each wave of the study (Table 1).
Anxiety.
Anxiety was measured using the 9-item tension-anxiety factor from the Profile of Mood States scale (McNair, Lorr, & Droppleman, 1981). Items include, “In the last seven days, did you feel anxious” and “In the last seven days, did you feel panicky.” Alpha reliabilities were α = .87 or greater at each wave of the study (Table 1).
Controls.
For consistency with previous research on caregiving (Barrah, Shultz, Baltes, & Stolz, 2004; Clancy et al., 2020; Gordon & Rouse, 2013; Halinski et al., 2020; Lee et al., 2010; Stephen at al., 2001; Pinquart & Sörensen, 2011), we controlled for various sociodemographic characteristics. Individuals were asked seven different demographic questions that were used as control variables. Respondents were asked to report their gender, age, the number of care-recipients, hours worked per week, and ethnicity by answering single item questions in relation to each. Individuals were also asked if they cared for an individual with an illness and/or a disability. As such, those who said yes were coded as 1, and those who said no were coded as 0. Respondents selected their income level from seven categories: (1) $10,000 or less, (2) $10,001 to $20,000, (3) $20,001 to $30,000, (4) $30,001 to $50,000, (5) $50,001 to $70,000, (6) $70,001 to $90,000, and (7) above $90,000.
Results
Table 1 contains descriptive statistics, correlations, and Alpha reliability coefficients. Correlation analyses indicate that all study variables were significantly correlated within each wave of data and that measures within each construct were more highly correlated with other measures within that construct than with measures of other constructs (e.g., WFC and FWC variables were more strongly correlated with each other than with burden or mental health variables), providing evidence of convergent and discriminant validity.
To test the relationship between caregiver burden and WFC/FWC and burden and mental health, we performed hierarchical linear regressions. The relationship between caregiver burden and each variable of interest (i.e., WFC, FWC, anxiety, and depression) was tested (Table 2 and Table 3). For each analysis, hours worked per week, the number of care-recipients cared for, gender, age, ethnicity, household income, and whether the individual(s) being cared for had a disability or illness were controlled. Additionally, the variable of interest (i.e., WFC, FWC, anxiety, and depression) at Wave 1 was controlled. As such, caregiver burden at Wave 1 predicted increases in WFC-time and WFC-strain at Wave 2 but not Wave 3. Additionally, caregiver burden at Wave 1 predicted increases in FWC-time and FWC-strain at Wave 2 and Wave 3. Lastly, caregiver burden predicted increases in anxiety for only Wave 2 and increases in depression for both Wave 2 and Wave 3.
Table 2.
Unstandardized regression results of caregiver burden predicting outcome variables.
| Variable | WFC-Time (W2; n = 512) | WFC-Time (W3; n = 451) | WFC-Strain (W2; n = 501) | WFC-Strain (W3; n = 442) | FWC-Time (W2; n = 501) | FWC-Time (W3; n = 444) | FWC-Strain (W2; n = 470) | FWC-Strain (W3; n = 415) |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | |
| Hours worked | .004 (.002)* | .000 (.002) | .001 (.001) | .000 (.002) | .001 (.002) | .001 (.002) | .001 (.002) | .001 (.002) |
| Care-recipients | .006 (.017) | .039 (.019)* | −.003 (.014) | .006 (.017) | −.004 (.017) | .005 (.018) | −.024 (.017) | .008 (.020) |
| Gender | −.079 (.053) | −.016 (.058) | .026 (.044) | −.029 (.050) | .143 (.017)** | .046 (.055) | .006 (.046) | −.002 (.056) |
| Age | .001 (.003) | −.001 (.003) | −.001 (.002) | −.003 (.003) | −.004 (.003) | −.005 (.003) | −.002 (.002) | −.003 (.003) |
| Ethnicity | .040 (.028) | .040 (.030) | .069 (.023)** | .053 (.026)* | .043 (.026) | .019 (.028) | .077 (.026)** | .050 (.029) |
| Household Income | .014 (.016) | .041 (.017)* | −.002 (.013) | .035 (.015)* | .035 (.015)* | .050 (.017)** | −.010 (.015) | .008 (.017) |
| Disability/Illness | −.030 (.048) | −.077 (.064) | .026 (.040) | .091 (.056) | .086 (.046) | −.054 (.061) | .050 (.045) | .041 (.063) |
| WFC-Time (W1) | .479 (.034)** | .511 (.038)** | ---- | ---- | ---- | ---- | ---- | ---- |
| WFC-Strain (W1) | ---- | ---- | .573 (.033)** | .500 (.038)** | ---- | ---- | ---- | ---- |
| FWC-Time (W1) | ---- | ---- | ---- | ---- | .503 (.038)** | .507 (.043)** | ---- | ---- |
| FWC-Strain (W1) | ---- | ---- | ---- | ---- | ---- | ---- | .477 (.039)** | .490 (.045)** |
| Caregiver Burden | .172 (.064)** | .089 (.067) | .122 (.053)* | .056 (.059) | .174 (.063)** | .213 (.070)** | .291 (.064)** | .164 (.072)* |
Note. Care-recipients is the number of individuals being cared for, and disability/illness is whether an individual being cared for has a disability/ illness. W means wave, WFC is work-family conflict, FWC is family-work conflict, and β are unstandardized.
is significant at p < .05
is significant at p < .01.
Table 3.
Unstandardized regression results of caregiver burden predicting outcome variables.
| Variable | Anxiety (W2; n = 505) | Anxiety (W3; n = 484) | Depression (W2; n = 517) | Depression (W3; n = 496) |
|---|---|---|---|---|
|
| ||||
| β (SE) | β (SE) | β (SE) | β (SE) | |
| Hours worked | .001 (.002) | −.001 (.002) | .001 (.001) | .000 (.002) |
| Care-recipients | .003 (.019) | −.004 (.020) | −.011 (.016) | −.029 (.017) |
| Gender | .016 (.055) | −.002 (.057) | −.015 (.045) | .094 (.050) |
| Age | −.003 (.003) | −.003 (.003) | .003 (.002) | .000 (.003) |
| Ethnicity | .095 (.030)** | .059 (.030)* | .006 (.024) | .023 (.026) |
| Household Income | −.039 (.016)* | −.033 (.016)* | −.026 (.013) | −.013 (.015) |
| Disability/Illness | .004 (.051) | .082 (.064) | −.005 (.042) | .066 (.056) |
| Anxiety (W1) | .559 (.040)** | .544 (.041) | ---- | ---- |
| Depression (W1) | ---- | ---- | .516 (.036)** | .528 (.040)** |
| Caregiver Burden | .219 (.068)** | .094 (.070) | .314 (.055)** | .147 (.060)** |
Note. Care-recipients is the number of individuals being cared for, and disability/illness is whether an individual being cared for has a disability/illness. W means wave and β are unstandardized.
is significant at p < .05
is significant at p < .01.
Next, a cross-lagged panel model examining mediation via AMOS, an SPSS macro for structural equation modeling (SEM), was used to test the mediational effects of WFC and FWC on the relationship between caregiver burden and mental health (i.e., anxiety or depression). Again, for each analysis, hours worked per week, number of care-recipients, gender, age, ethnicity, household income, and whether care recipient(s) had a disability or illness were treated as controls. Missing data were imputed using regression imputation from AMOS. For bootstrapping, 5,000 cases, and 95% confidence interval (CI) was utilized.
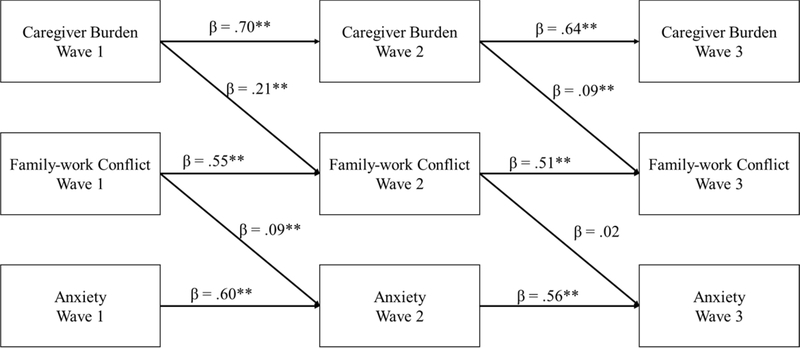
Hypothesis 1 predicted that FWC would mediate the relationship between caregiver burden and anxiety (Figure 2). The model fit indices suggested an acceptable model fit n = 1,007, χ2 = 219.63, df = 19, CFI = .97, TLI = .82, RMSEA = .10, CI95% [.091,.115], SRMR = .03). Neither the direct effect of caregiver burden (W1) on anxiety (W3; β = −.00, CI95% [−.06, .05], p > .05) nor the indirect effect of caregiver burden (W1) on anxiety (W3; β = .00, CI95% [−.01, .01], p > .05) was significant. Therefore, hypothesis 1 is not supported.
Figure 2.
The cross-lagged panel for mediational effects of family-work conflict on the caregiver burden and anxiety relationship.
Note: Standardized direct effects are shown. n = 1,007. ** is p < .01 and * is p < .05. Hours worked for each week, number of care-recipients who were cared for, gender, age, ethnicity, household income, and whether the individual(s) being cared for had a disability or illness were covariates.
Supplemental analysis for FWC-strain and FWC-time were run. For FWC-strain, the model fit indices were acceptable (n = 1,007, χ2 = 226.78, df = 19, CFI = .97, TLI = .81, RMSEA = .10, CI95% [.092,.117], SRMR = .04). The direct effect of caregiver burden (W1) on anxiety (W3) was not significant (β = −.02, CI95% [−.08, .03], p > .05) but the indirect effect was significant (β = .02, CI95% [.01, .03], p < .01). For FWC-time, the model fit indices were acceptable (n = 1,007, χ2 = 191.91, df = 19, CFI = .97, TLI = .84, RMSEA = .10, CI95% [.083,.108], SRMR = .03). Neither the direct effect of caregiver burden (W1) on anxiety (W3; β = −.00, CI95% [−.06, .06], p > .05) nor the indirect effect were significant (β = −.00, CI95% [−.01, .01], p > .05). Unlike the aggregate FWC, FWC-strain was found to mediate the relationship.
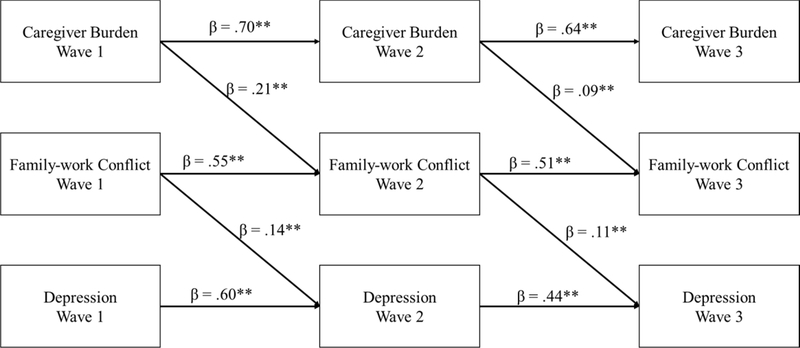
Hypothesis 2 predicted that FWC would mediate the relationship between caregiver burden and depression (Figure 3). The model fit indices suggested an acceptable model fit n = 1,007, χ2 = 239.70, df = 19, CFI = .97, TLI = .81, RMSEA = .11, CI95% [.097,.120], SRMR = .04). The direct effect of caregiver burden (W1) on depression (W3) was not significant (β = −.04, CI95% [−.09, .02], p > .05) but the indirect effect of caregiver burden (W1) on depression (W3) was significant (β = .02, CI95% [.01, .04], p < .01). Hypothesis 2 was supported.
Figure 3.
The cross-lagged panel for mediational effects of family-work conflict on the caregiver burden and depression relationship.
Note: Standardized direct effects are shown. n = 1,007. ** is p < .01 and * is p < .05. Hours worked for each week, number of care-recipients who were cared for, gender, age, ethnicity, household income, and whether the individual(s) being cared for had a disability or illness were covariates.
Supplemental analysis for FWC-strain and FWC-time were run. For FWC-strain, the model fit indices were acceptable (n = 1,007, χ2 = 261.28, df = 19, CFI = .96, TLI = .77, RMSEA = .11, CI95% [.101,.125], SRMR = .04). The direct effect of caregiver burden (W1) on depression (W3) was not significant (β = −.03, CI95% [−.09, .03], p > .05) but the indirect effect was significant (β = .03, CI95% [.02, .05], p < .01). For FWC-time, the model fit indices were acceptable (n = 1,007, χ2 = 218.64, df = 19, CFI = .97, TLI = .81, RMSEA = .10, CI95% [.090,.115], SRMR = .04). While the direct effect of caregiver burden (W1) on depression was not significant (W3; β = −.01, CI95% [−.07, .04], p > .05), the indirect effect was significant (β = .01, CI95% [.00, .02], p <.05). As such, it seems that both FWC-strain and FWC-time are mediating mechanisms.
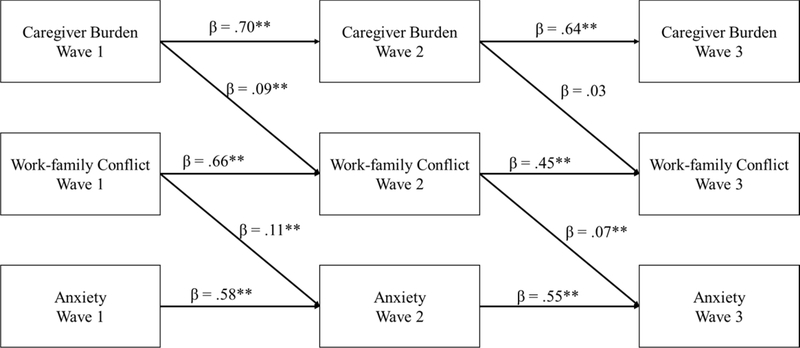
Hypothesis 3 predicted that WFC would mediate the relationship between caregiver burden and anxiety (Figure 4). The model fit indices suggested an acceptable model fit (n = 1,007, χ2 = 204.98, df = 19, CFI = .97, TLI = .83, RMSEA = .10, CI95% [.087,.111], SRMR = .03). The direct effect of caregiver burden (W1) on anxiety (W3) was not significant (β = −.01, CI95% [−.06, .05], p > .05) but the indirect effect was significant (β = .01, CI95% [.00, .02], p < .01). This supports hypothesis 3.
Figure 4.
The cross-lagged panel for mediational effects of work-family conflict on the caregiver burden and anxiety relationship.
Note: Standardized direct effects are shown. n = 1,007. ** is p < .01 and * is p < .05. Hours worked for each week, number of care-recipients who were cared for, gender, age, ethnicity, household income, and whether the individual(s) being cared for had a disability or illness were covariates.
Supplemental analysis for WFC-strain and WFC-time were run. For WFC-strain, the model fit indices were acceptable (n = 1,007, χ2 = 224.49, df = 19, CFI = .97, TLI = .81, RMSEA = .10, CI95% [.092,.116], SRMR = .04). The direct effect of caregiver burden (W1) on anxiety (W3) was not significant (β = −.01, CI95% [−.06, .04], p > .05) but the indirect effect was significant (β = .01, CI95% [.00, .01], p < .01). For WFC-time, the model fit indices were acceptable (n = 1,007, χ2 = 152.45, df = 19, CFI = .98, TLI = .87, RMSEA = .08, CI95% [.072,.096], SRMR = .03). Neither the direct effect of caregiver burden (W1) on anxiety (W3; β = .00, CI95% [−.05, .06], p > .05) nor the indirect effect were significant (β = −.00, CI95% [−.00, .01], p > .05). As such, it seems that WFC-strain is the true mediating mechanism.
Hypothesis 4 predicted that WFC would mediate the relationship between caregiver burden and depression (Figure 5). The model fit indices suggested an acceptable model fit (n = 1,007, χ2 = 227.03, df = 19, CFI = .97, TLI = .81, RMSEA = .10, CI95% [.092,.117], SRMR = .04). The direct effect of caregiver burden (W1) on depression (W3) was not significant (β = .00, CI95% [−.05, .06], p > .05) but the indirect effect approached significance (β = .01, CI95% [−.00, .01], p = .077). As such, this does not support hypothesis 4.
Figure 5.
The cross-lagged panel for mediational effects of work-family conflict on the caregiver burden and depression relationship.
Note: Standardized direct effects are shown. n = 1,007. ** is p < .01 and * is p < .05. Hours worked for each week, number of care-recipients who were cared for, gender, age, ethnicity, household income, and whether the individual(s) being cared for had a disability or illness were covariates.
Supplemental analysis for WFC-strain and WFC-time were run. For WFC-strain, the model fit indices were acceptable (n = 1,007, χ2 = 238.81, df = 19, CFI = .97, TLI = .79, RMSEA = .11, CI95% [.095,.120], SRMR = .04). The direct effect of caregiver burden (W1) on anxiety (W3) was not significant (β = −.00, CI95% [−.06, .05], p > .05) but the indirect effect was significant (β = .01, CI95% [.002, .013], p < .01). For WFC-time, the model fit indices were acceptable (n = 1,007, χ2 = 178.94, df = 19, CFI = .98, TLI = .84, RMSEA = .09, CI95% [.079,.104], SRMR = .04). Neither the direct effect of caregiver burden (W1) on anxiety (W3; β = .01, CI95% [−.05, .06], p > .05) nor the indirect effect were significant (β = .00, CI95% [−.00, .01], p > .05). As such, it seems that WFC-strain mediates the relationship while WFC-time does not.
Discussion
Understanding the consequences of assuming a caregiver role is becoming an increasingly important private and public issue (Marks, 1998). The growing number of caregivers in the US, the documented mental and physical health problems experienced by caregivers, as well as the impact of the potentially highly intrusive and demanding nature of the caregiver role on work-family dynamics create a compelling case for research, particularly in light of the COVID-19 pandemic, which has placed unprecedented demands on working parents who have been faced with balancing childcare, children’s school demands, and their own work demands. Additionally, the fact that most caregivers are also employed makes it imperative to understand the extent to which the demands and stress of caregiving and employment contribute to mental health as to help pinpoint what resources are needed to support healthy management of multiple role demands.
To our knowledge, this is the first study of its kind to examine the process through which caregiver burden impacts WFC and FWC, which, in turn, influences mental health over time for U.S. employees. The study allows us to examine not only the short-term variations among the constructs but also the way they relate to each other over time, thus addressing an important limitation of the caregiving literature. Besides, the present study relied on a more heterogeneous and larger sample than previous studies that have focused on relatively small opportunity samples (i.e., only eldercare, childcare, or disabled care), and non-representative samples that often include only women caregivers.
Our findings lend partial support to our research hypotheses. The findings indicate the strain-based WFC and FWC as being a consistent mediator between caregiver burden and mental health at baseline and two years later. Our findings extend previous cross-sectional research (Gignac et al., 1996; Glavin & Peters, 2015; Gordon et al., 2012; Stephens et al., 2001; Zuba & Schneider, 2013) by distinguishing WFC and FWC, and by demonstrating that mental health problems of employed caregivers are experienced primarily through strain-based conflict.
To begin, we note that informal caregivers are often engaged in a stressful and demanding family role. Our results suggest that there is a substantial burden associated with the caregiving role, which affects the caregivers with time-dependence, developmental, physical, social, and emotional aspects. Caregiving, indeed, has all the aspects of a chronic stressor with high levels of unpredictability and uncontrollability (Schulz & Sherwood, 2008). When this role is combined with another role, a high level of role conflict, indeed, comes as no surprise. In line with COR theory (Hobfoll, 1989, 2002), the findings support the idea that as caregiving burden increases, the limited amount of time and energy available to spend on work role will decrease. So, the domains will be perceived as conflicting, which can produce significant strain, creating time and strain-based WFC and FWC, ultimately resulting in mental health problems. As the focus of our study, the caregiver burden of employed caregivers might initiate a loss of psychological resources, which, in turn, interferes with work and family responsibilities.
Besides, it seems likely that job strains exhaust employee’s physical and/or mental energy as well as other resources (Gordon et al., 2012), resulting in WFC; similarly, caregiving burden exhaust caregiver’s mental and/or physical energy as well as other resources, resulting in FWC, which, ultimately, result in the deterioration of mental health over time. This is in line with previous conceptualizations of strain-based WFC/FWC. As such, strain-based conflict, which is understood to be a crossover type of strain from one role that affects an individual’s performance in another domain (Greenhaus & Beutell, 1985), can be seen to be more related to mental health issues than time-based conflict (Shang, O’Driscoll, & Roche, 2016). This indicates that it is the emotional or psychological aspects of balancing work and family that is most important for mental health, particularly depressive symptoms, rather than the degree of time involved in balancing work and family responsibilities. One possible explanation could be the interpretation of the time and strain demands differently by different caregiving providers. The cognitive appraisal of the situation is an important issue in understanding how an individual will respond to a stressor (Lazarus, 1967). Although caregiving recipient type is not associated with caregiver burden (Halinski et al., 2020; Lee et al., 2010), it is possible that eldercare and childcare providers may interpret the time and strain demands of caregiving in a different way. Our sample mainly consists of employed childcare providers (75.7%). As work might allow employees access to better quality childcare by receiving job benefits such as a subsidy for childcare costs or employer-supported on-site child center, employed childcare providers might experience less time-based conflict.
Another possible explanation could be that caregivers might have better opportunities to manage their time commitments than their strain in caregiving responsibilities. For example, telecommuting provides an opportunity to fulfill work demands and simultaneously conserve time with family members (Brough & O’Driscoll, 2005), thereby potentially enhancing work-life balance and reducing conflict. Thus, strain-aspect of caregiving, rather than time-aspect might conceivably affect the degree of conflict experienced and subsequent mental health problems for caregivers. Furthermore, it is possible that time-based conflict would be more likely to lead to task and work-related deficits like daily interruptions, lack of attentiveness, lowered performance, and other performance-related costs (Gordon & Rouse, 2013) rather than having an impact on mental health. Additional research measuring both mental health and performance-related outcomes is needed to further explore possible differential effects of WFC and FWC time and strain-based conflict on various outcome domains.
These findings contribute to the literature by extending the work-family conflict research to the growing population of employed caregivers and utilizing tests of mediation in a longitudinal study, which helps address concerns about causality in caregiving research. Second, we have expanded COR theory to the issue of employed caregivers, yielding new information on WFC and FWC as underlying strain-based processes that explain how caregiver burden is associated with mental health, contributing to the debate on matching and cross-domain effects of work-family conflict (Ford et al., 2007; Gordon et al., 2012; Pearlin et al., 1990).
In addition to its theoretical contributions, this research has significant practical implications. Given that caregiver burden has deleterious effects on the mental health of employees through its impact on strain-based conflict, these findings further reinforce the need for organizations to offer and implement benefits/programs that help employees ease the strain of simultaneously inhabiting caregiving and employee roles. These benefits/programs act as resources that could help reduce the strain of balancing work and family roles. This is also consistent with COR theory which proposes that individuals might be able to offset resource loss with the addition of other personal resources (Hobfoll & Lilly, 1993). Otherwise, if the strain from multiple roles is not mitigated, caregiver burden may spill over into the workplace by affecting the employee’s quality and/or quantity of work, which may ultimately impact employer productivity and profitability. Moreover, organizations must approach the issue of caregiving through the lens of talent management (Fuller & Raman, 2017). By supporting and providing resources to employees with caregiving responsibilities, it may be easier to retain experienced, educated, and trained employees in an organization as well as attract new talent. Finally, in line with suggestions by Li and colleagues (2015), family counselors may also be an invaluable resource to reduce employee strain by helping caregivers adjust to their responsibilities and to serve as a mediator to resolve family disputes around issues of caregiving.
As with all research, this study is not without its limitations. Firstly, caregiver burden is treated as an aggregate total rather than a combination of different facets. Thus, a multifaceted concept consisting of distinct components (i.e., time-dependence, developmental, physical, social, and emotional burden) that elaborate on the subjective and objective burden (Novak & Guest, 1989; Rospenda et al., 2010) could be used in future studies. Because in this study some facets were below acceptable levels of reliability, this approach was necessary. Secondly, in terms of work-family conflict forms, we adopted the viewpoint of Kelloway et al. (1999), who asserted that behavior-based WFC is difficult to operationalize, and consequently, there is not much empirical evidence for the existence of it. Accordingly, we used their scale in our analysis which measures only time-based and strain-based WFC. However, there is also research in the literature that found that each of the three forms of WFC could be reliably measured and had a unique set of antecedents (Carlson, 1999; Matthews, Kath, & Barnes-Farrell, 2010). Future research should incorporate all forms of WFC and FWC. As one reviewer noted, it would be interesting to adopt Carlson et al. (2000)’s approach and scale in which they incorporated all forms of WFC. Thirdly, the data were all self-report. Thus, common-method bias cannot be totally discounted. However, given the nature of perceived caregiver burden, role conflict, and mental health, self-report measures seem to be more appropriate than other forms of measurement (Peng et al., 2020).
Also, like most work-family research, we have focused on the negative aspects of caregiving. Providing caregiving can have positive effects as well, such as work enrichment, evoking a sense of purpose, and strengthening the bond (e.g., Boerner, Schulz, & Horowitz, 2004; Cohen, Colantonio, & Vernich, 2002; Greenhaus & Powell, 2006; Redmond & Richardson, 2003). However, some research suggests that occupying multiple roles may be beneficial (e.g., Barnett & Hyde, 2001; Greenhaus & Powell, 2006; Grzywacz & Marks, 2000). Role enhancement theory (Sieber, 1974) posits that multiple roles are indeed beneficial for well-being because they increase feelings of purpose, belonging and self-efficacy (Castro & Gordon, 2012; Barnett & Hyde, 2001; Sieber, 1974). In line with this theory, there is some evidence that providing caregiving might involve rewarding aspects as well, enabling the caregiver to feel happy and important (Boerner et al., 2004; Cohen et al., 2002; Marks, 1998). However, while we might expect to see such positive aspects much more in certain role combinations such as being a parent and a volunteer at a child’s school, we argue that these beneficial effects are likely less common for the combination of employment and caregiving roles, which were our focus in this study. Because both roles imply special restrictions more or less constantly in daily lives of people, caregiving might become more burdensome and uncertain over time as caregivers are faced with blending the often contradictory expectations of both roles (Azarnoff & Scharlach, 1988; Gordon et al., 2012; Keeling & Davey, 2008; Marks, 1998; Pinquart & Sorensen, 2003). Thus, we did not examine the positive aspects of informal caregiving in our study. Future longitudinal research designed to integrate both positive and negative aspects of caregiving would contribute to a more multifaceted understanding of the complex mental health effects of caregiving while employed. Furthermore, previous literature has found that caregivers with a strong social support network report less burden (Li et al., 2015; Rospenda et al., 2010). Similarly, satisfaction with caregiving tasks has been found to be an important coping resource that helps employed caregivers (Zacher et al., 2012). Thus, consistent with COR theory, it might be expected that similar kinds of resources such as perceived social support, supervisor and workplace support, role clarity, autonomy, access to community support services, and relationship satisfaction would mitigate the relationship between caregiver burden and potential negative outcomes by serving as resources that may help the caregivers manage the burden associated with caring. Avenues for future research in this area should include the examination of such individual and organizational resources individually or in combination as possible boundary conditions.
Notwithstanding the foregoing limitations, this 3-wave longitudinal study extends previous research by serving as an initial investigation into the nature of the associations between caregiver burden, role conflict, and mental health over time. Findings from this study deepen our understanding by underlining that the burden of providing caregiving exerts its harmful effects on the mental health of informal caregivers through interrole conflict. Collectively, these results provide a foundation for future research studies and should help to inform practice and policy for a large subset of the working population who are both employed and have caregiving responsibilities.
Acknowledgments
This research was made possible by a Grant (R01 AA015766) from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) to the third author.
Contributor Information
Alper Kayaalp, Department of Psychology, South Dakota State University, 857 11th St., 029B Hansen Hall, Brookings, SD 57007.
Kyle J. Page, American Family Insurance, 6000 American Parkway, Madison, WI 53783.
Kathleen M. Rospenda, Department of Psychiatry, University of Illinois at Chicago, Chicago, IL 60612.
References
- Amstad FT, Meier LL, Fasel U, Elfering A, & Semmer NK (2011). A meta-analysis of work–family conflict and various outcomes with a special emphasis on cross-domain versus matching-domain relations. Journal of Occupational Health Psychology, 16, 151–169. [DOI] [PubMed] [Google Scholar]
- Andrade C, & Mikula G (2014). Work–family conflict and perceived justice as mediators of outcomes of women’s multiple workload. Marriage & Family Review, 50, 285–306. [Google Scholar]
- Azarnoff RS, & Scharlach AE (1988). Can Employees Carry the Elder Care Burden? Personnel Journal, 60–76. [Google Scholar]
- Bainbridge HTJ, Cregan C, & Kulik CT (2006). The effect of multiple roles on caregiver stress outcomes. Journal of Applied Psychology, 91, 490–497. [DOI] [PubMed] [Google Scholar]
- Barnett A (2015). Adult child caregiver health trajectories and the impact of multiple roles over time. Research on Aging, 37, 227–52. [DOI] [PubMed] [Google Scholar]
- Barnett RC, & Hyde JS (2001). Women, men, work, and family. American Psychologist, 56, 781–796. [DOI] [PubMed] [Google Scholar]
- Barrah J, Shultz K, Baltes B, & Stolz H (2004). Men’s and women’s eldercare-based work family conflict: Antecedents and work-related outcomes. Fathering, 2, 305–330. [Google Scholar]
- Boerner K, Schulz R, & Horowitz A (2004). Positive Aspects of Caregiving and Adaptation to Bereavement. Psychology and Aging, 19(4), 668–675. [DOI] [PubMed] [Google Scholar]
- Brough P, & O’Driscoll M (2005). Work–family conflict and stress. In Antoniou A, & Cooper C (Eds.), A research companion to organizational health psychology (pp. 346–365). Cheltenham, UK: Edward Elgar. [Google Scholar]
- Brown M, & Pitt-Catsouphes M (2016). A mediational model of workplace flexibility, work-family conflict, and perceived stress among caregivers of older adults. Community Work & Family, 19, 379–395. [Google Scholar]
- Bryant B (1975). Respondent selection in a time of changing household composition. Journal of Marketing Research, 12, 129–135. [Google Scholar]
- Calvano L (2013). Tug of War: Caring for Our Elders While Remaining Productive at Work, Academy of Management Perspectives, 27, 204–218. [Google Scholar]
- Carlson DS (1999). Personality and role variables as predictors of three forms of work–family conflict. Journal of Vocational Behavior, 55, 236–253. [Google Scholar]
- Carlson DS, Kacmar KM, & Williams LJ (2000). Construction and initial validation of a multidimensional measure of work–family conflict. Journal of Vocational Behavior, 56, 249–276. [Google Scholar]
- Castro Y, & Gordon KH (2012). A review of recent research on multiple roles and women’s mental health. In Lundberg-Love PK, Nadal KL, & Paludi MA (Eds.), Women and mental disorders (Vol. 1–4, pp. 37–54). [Google Scholar]
- Chappel NL, & Reid RC (2002). Burden and well-being among caregivers: Examining the distinction. Gerontologist, 42, 772–780. [DOI] [PubMed] [Google Scholar]
- Clancy RL, Fisher GG, Daigle KL, Henle CA, McCarthy J, & Fruhauf CA (2020). Eldercare and work among informal caregivers: A multidisciplinary review and recommendations for future research. Journal of Business and Psychology, 35, 9–27. [Google Scholar]
- Cohen CA, Colantonio A, & Vernich L (2002). Positive aspects of caregiving: Rounding out the caregiver experience. International Journal of Geriatric Psychiatry, 17, 184–188. [DOI] [PubMed] [Google Scholar]
- Davis KD, Gere J, & Sliwinski MJ (2017). Investigating the work–family conflict and health link: Repetitive thought as a mechanism. Stress and Health, 33, 330–338. [DOI] [PubMed] [Google Scholar]
- Dekel R, Solomon Z, & Bleich A (2005). Emotional distress and marital adjustment of caregivers: Contribution of level of impairment and appraised burden. Anxiety, Stress, and Coping, 18, 71–82. [Google Scholar]
- Demerouti E, Bakker AB, & Schaufeli WB (2005). Spillover and crossover of exhaustion and life satisfaction among dual-earner parents. Journal of Vocational Behavior, 67, 266–289. doi: 10.1016/j.jvb.2004.07.001 [DOI] [Google Scholar]
- Duxbury L, Higgins C, & Smart R (2011). Elder care and the impact of caregiver strain on the health of employed caregivers. Journal of Prevention Assessment & Rehabilitation, 40, 29–40. [DOI] [PubMed] [Google Scholar]
- Feinberg L, Reinhard SC, Houser A, & Choula R (2011). Valuing the Invaluable: 2011 Update the Growing Contributions and Costs of Family Caregiving. https://assets.aarp.org/rgcenter/ppi/ltc/i51-caregiving.pdf
- Ford MT, Heinen BA, & Langkamer KL (2007). Work and family satisfaction and conflict: A meta-analysis of cross-domain relations. Journal of Applied Psychology, 92, 57–80. [DOI] [PubMed] [Google Scholar]
- Frone MR (2000). Work–family conflict and employee psychiatric disorders: The national comorbidity study. Journal of Applied Psychology, 85, 888–895. [DOI] [PubMed] [Google Scholar]
- Frone MR, Russell M, & Barnes GM (1996). Work–family conflict, gender, and health-related out-comes: A study of employed parents in two community samples. Journal of Occupational Health Psychology, 1, 57–69. [DOI] [PubMed] [Google Scholar]
- Frone MR, Russell M, & Cooper ML (1992). Antecedents and outcomes of work-family conflict: Testing a model of the work-family interface. Journal of Applied Psychology, 77, 65–78. [DOI] [PubMed] [Google Scholar]
- Fuller J & Raman M (2017). Dismissed by Degrees: How degree inflation is undermining U.S. competitiveness and hurting America’s middle class. https://www.hbs.edu/managing-the-future-of-work/Documents/dismissed-by-degrees.pdf
- Gallup-Healthways Well-Being Surveys (2011, July 27). Caregiving Costs U.S. Economy $25.2 Billion in Lost Productivity. https://news.gallup.com/poll/148670/caregiving-costs-economy-billion-lost-productivity.aspx [Google Scholar]
- George LK, & Gwyther LP (1986). Caregiver well-being: A multidimensional examination of family caregivers of demented adults. The Gerontologist, 26, 253–259. [DOI] [PubMed] [Google Scholar]
- Gignac MA, Kelloway EK, & Gottlieb BH (1996). The impact of caregiving on employment: A mediational model of work-family conflict. Canadian Journal on Aging/La Revue Canadienne du Vieillissement, 15, 525–542. [Google Scholar]
- Glavin P, & Peters A (2015). The costs of caring: Caregiver strain and work–family conflict among Canadian workers. Journal of Family and Economic Issues, 36, 5–20. [Google Scholar]
- Gordon JR, Pruchno RA, Wilson-Genderson M, Marcinkus MW, & Rose M (2012). Balancing caregiving and work: Role conflict and role strain dynamics. Journal of Family Issues, 33, 662–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon JR, & Rouse ED (2013). The relationship of job and elder caregiving involvement to work-caregiving conflict and work costs. Research on Aging, 35, 96–117. [Google Scholar]
- Grandey AA, & Cropanzano R (1999). The conservation of resources model applied to work-family conflict and strain. Journal of Vocational Behavior, 54, 1–21. [Google Scholar]
- Greenhaus JH, & Beutell NJ (1985). Sources of conflict between work and family roles. Academy of Management Review, 10, 76–88. [Google Scholar]
- Greenhaus JH, & Parasuraman S (1994). Work-family conflict, social support, and well-being. In Davidson MJ & Burke RJ (Eds.) Women in management: Current research issues (pp. 213–229). London: Chapman. [Google Scholar]
- Greenhaus JH, & Powell GN (2006). When Work and Family Are Allies: A Theory of Work-Family Enrichment. Academy of Management Review, 31, 72–92. [Google Scholar]
- Griggs TL, Lance CE, Thrasher G, Barnes-Farrell J, & Baltes B (2020). Eldercare and the psychology of work behavior in the twenty-first century. Journal of Business and Psychology, 35, 1–8. [Google Scholar]
- Grzywacz JH, & Marks NF (2000). Family, work, work family spillover, and problem drinking during midlife. Journal of Marriage and the Family, 62, 336–348. [Google Scholar]
- Halinski M, Duxbury L, & Stevenson M (2020). Employed caregivers’ response to family-role overload: The role of control-at-home and caregiver type. Journal of Business and Psychology, 35, 99–115. [Google Scholar]
- Hall GB, Dollard MF, Tuckey MR, Winefield AH, &Thompson BM (2010). Job demands, work-family conflict, and emotional exhaustion in police officers: A longitudinal test of competing theories. Journal of Occupational and Organizational Psychology, 83, 237–250. [Google Scholar]
- Ho AK, Gilbert AS, Mason SL, Goodman AO, & Barker RA (2009). Health-related quality of life in Huntington’s disease: which factors matter most? Movement Disorders, 24, 574–578. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44, 513–524. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE (2002). Social and psychological resources and adaptation. Review of General Psychology, 6, 307–324. [Google Scholar]
- Hobfoll SE, & Lilly RS (1993). Resource conservation as a strategy for community psychology. Journal of Community Psychology, 21, 128–148. [Google Scholar]
- Hobfoll SE, & Shirom A (2000). Conservation of resources theory: Applications to stress and management in the workplace. In Golembiewski RT (Ed.), Handbook of organization behavior (2nd ed., pp. 57–81). NewYork: Dekker. [Google Scholar]
- Honea NJ, Britnall R, Given B, Sherwood P, Colao DB, Somers SC, & Northouse LL (2008). Putting evidence into practice: Nursing assessment and interventions to reduce family caregiver strain and burden. Clinical Journal of Oncology Nursing, 12, 507–516. [DOI] [PubMed] [Google Scholar]
- Hopps M, Iadeluca L, McDonald M, & Makinson GT (2017). The burden of family caregiving in the United States: Work productivity, health care resource utilization, and mental health among employed adults. Journal of Multidisciplinary Healthcare, 10, 437–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang YH, Hammer LB, Neal MB, & Perrin NA (2004). The relationship between work-to-family conflict and family-to-work conflict: A longitudinal study. Journal of Family and Economic Issues, 25, 79–100. [Google Scholar]
- Judge TA, & Colquitt JA (2004). Organizational justice and stress: The mediating role of work–family conflict. Journal of Applied Psychology, 89, 395–404. [DOI] [PubMed] [Google Scholar]
- Keeling S, & Davey J (2008). Working careers in New Zealand: Zones of care and contested boundaries. In Martin-Matthews A & Phillips JE (Eds.), Aging and caring at the interaction of work and home life: Blurring the boundaries (pp. 129–146). New York, NY: Lawrence Erlbaum [Google Scholar]
- Kelloway EK, Gottlieb BH, Barham L (1999). The source, nature, and direction of work and family conflict: A longitudinal investigation. Journal of Occupational Health Psychology, 4, 337–346. [DOI] [PubMed] [Google Scholar]
- Kinnunen U, Geurts S, & Mauno S (2004). Work-to-family conflict and its relationship with satisfaction and well-being: a one-year longitudinal study on gender differences. Work and Stress, 18, 1–22. [Google Scholar]
- La-pierre LM, and Allen TD (2006). Work-supportive family, family-supportive supervision, use of organizational benefits, and problem-focused coping: implications for work-family conflict and employee well-being. Journal of Occupational Health Psychology, 11, 169–181. [DOI] [PubMed] [Google Scholar]
- Lahaie C, Earle A, & Heymann J (2013). An uneven burden: Social disparities in adult caregiving responsibilities, working conditions, and caregiver outcomes. Research on Aging, 35, 243–274. [Google Scholar]
- Lazarus AA (1967). In support of technical eclecticism. Psychological Reports, 21, 415–416. [DOI] [PubMed] [Google Scholar]
- Lee JA, Foos PW, & Glow GL (2010). Caring for one’s elders and family-to-work conflict. Psychologist-Manager Journal, 23, 15–39. [Google Scholar]
- Lee JA, Walker M, & Shoup R (2001). Balancing elder care responsibilities and work: The impact on emotional health. Journal of Business and Psychology, 16, 277–289. [Google Scholar]
- Li A, Shaffer J, & Bagger J (2015). The psychological well-being of disability caregivers: Examining the roles of family strain, family-to-work conflict, and perceived supervisor support. Journal of Occupational Health Psychology, 20, 40–49. [DOI] [PubMed] [Google Scholar]
- Löckenhoff CE, Duberstein PR, Friedman B, & Costa PT (2011). Five-Factor personality traits and subjective health among caregivers: The role of caregiver strain and self-efficacy. Psychology and Aging, 26, 592–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks NF (1998). Does it hurt to care? Caregiving, work–family conflict, and midlife well-being. Journal of Marriage and the Family, 60, 951–966. [Google Scholar]
- Matthews RA, Kath LM, & Barnes-Farrell JL (2010). A short, valid, predictive measure of work–family conflict: Item selection and scale validation. Journal of Occupational Health Psychology, 15, 75–90. [DOI] [PubMed] [Google Scholar]
- McCann JJ, Hebert LE, Bienias JL, Morris MC, & Evans DA (2004). Predictors of beginning and ending caregiving during a 3-year period in a biracial community population. American Journal of Public Health, 94, 1800–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDaniel KR, & Allen DG (2012). Working and care-giving: The impact on caregiver stress, family-work conflict, and burnout. Journal of Life Care Planning, 10, 21–32. [Google Scholar]
- McDonald TP, Poertner J, & Pierpont J (1999). Predicting caregiver stress: An ecological perspective. American Journal of Orthopsychiatry, 69, 100–109. [DOI] [PubMed] [Google Scholar]
- McNair DM, Loor M, & Droppleman LF (1981). Profile of Mood States. San Diego, CA: Educational and Industrial Testing Service. [Google Scholar]
- Michel JS, Kotrba LM, Mitchelson JK, Clark MA, & Baltes BB (2011). Antecedents of work-family conflict: a meta-analytic review. Journal of Organizational Behavior, 32, 689–725. [Google Scholar]
- National Alliance for Caregiving (NAC) & American Association for Retired Persons (AARP) (2015). Caregiving in the U.S. Report. https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf
- Nguyen M (2009). Nurse’s assessment of caregiver burden. Medsurg Nursing, 18, 147–51. [PubMed] [Google Scholar]
- Novak M, & Guest C (1989). Application of a multidimensional caregiver burden inventory. The Gerontologist, 29, 798–803. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Temple SJ, & Skaff MM (1990). Caregiving and the Stress Process: An Overview of Concepts and Their Measures. Gerontologist, 30, 583–94. [DOI] [PubMed] [Google Scholar]
- Peng Y, Jex S, Zhang W, Ma J, & Matthews RA (2020). Eldercare demands and time theft: Integrating family-to-work conflict and spillover-crossover perspective. Journal of Business and Psychology, 35, 45–58. [Google Scholar]
- Pinquart M, & Sorensen S (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychological Aging, 18, 250–67. [DOI] [PubMed] [Google Scholar]
- Pinquart M, & Sörensen S (2011). Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychology and Aging, 26, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Population Reference Bureau (2015). Population Bulletin. Aging in the US. https://www.prb.org/wp-content/uploads/2016/01/aging-us-population-bulletin-1.pdf
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Rosenzweig JM, Brennan EM, & Ogilvie AM (2002). Work–family fit: Voices of parents of children with emotional and behavioral disorders. Social Work, 47, 415–424. [DOI] [PubMed] [Google Scholar]
- Rospenda KM, Minich LM, Milner LA, & Richman JA (2010). Caregiver burden and alcohol use in a community sample. Journal of Addictive Diseases, 29, 314–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savundranayagam MY, & Montgomery R (2010). Impact of role discrepancies on caregiver burden among spouses. Research on Aging, 32, 175–199. [Google Scholar]
- Savundranayagam MY, Montgomery RJ, & Kosloski K (2011). A dimensional analysis of caregiver burden among spouses and adult children. Gerontologist, 51, 321–31. [DOI] [PubMed] [Google Scholar]
- Schulz R, & Sherwood P (2008). Physical and mental health effects of family caregiving. The American Journal of Nursing, 108(9 Suppl.), 23–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang S, O’Driscoll PM, & Roche M (2017). Moderating role of acculturation in a mediation model of work–family conflict among Chinese immigrants in New Zealand. Stress and Health, 33, 55–68 [DOI] [PubMed] [Google Scholar]
- Sieber SD (1974). Toward a theory of role accumulation. American Sociological Review, 39, 567–578. [Google Scholar]
- Smith PR (2004). Elder care, gender, and work: The work–family issue of the 21st century. Berkeley Journal of Employment & Labor Law, 25, 351–398. [Google Scholar]
- Smoktunowicz E, Cieślak R, & Demerouti E (2017). Interrole conflict and self-efficacy to manage work and family demands mediate the relationships of job and family demands with stress in the job and family domains. Anxiety Stress Coping, 30, 485–497. 10.1080/10615806.2017.1329932 [DOI] [PubMed] [Google Scholar]
- Stenberg U, Ruland CM, & Miaskowski C (2010). Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology, 19, 1013–1025. [DOI] [PubMed] [Google Scholar]
- Stephens MAP, & Franks MM (1999). Parent care in the context of women’s multiple roles. Current Directions in Psychological Science, 8, 149–152. [Google Scholar]
- Stephens MA, Franks MM, & Atienza AA (1997). Where two roles intersect: Spillover between parent care and employment. Psychology and Aging, 12, 30–37. [DOI] [PubMed] [Google Scholar]
- Stephens MA, Townsend AL, Martire LM, & Druley JA (2001). Balancing parent care with other roles: interrole conflict of adult daughter caregivers Journals of Gerontology, 56, 24–34. [DOI] [PubMed] [Google Scholar]
- Troldahl C, & Carter R (1964). Random selection of respondents within households in phone surveys. Journal of Marketing Research, 1, 71–76. [Google Scholar]
- Werner P, Mittelman MS, Goldstein D, & Heinik J (2012). Family stigma and caregiver burden in Alzheimer’s disease. The Gerontologist, 52, 89–97. [DOI] [PubMed] [Google Scholar]
- Whitebird RR, Kreitzer M, Crain AL, Lewis BA, Hanson LR, & Enstad CJ (2013). Mindfulness-Based Stress Reduction for Family Caregivers: A Randomized Controlled Trial. The Gerontologist, 53, 676–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Report (WHO) (2017). Depression and Other Common Mental Disorders. Global Health Estimates. https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf?sequence=1 [Google Scholar]
- World Health Organization (2018, February 5). Ageing and health. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
- World Health Organization (2018, March 30). Mental health: strengthening our response https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
- Zacher H, Jimmieson NL, & Winter G (2012). Eldercare demands, mental health, and work performance: The moderating role of satisfaction with eldercare tasks. Journal of Occupational Health Psychology, 17, 52–64. [DOI] [PubMed] [Google Scholar]
- Zuba M, & Schneider U (2013). What helps working informal caregivers? The role of workplace characteristics in balancing work and adult-care responsibilities. Journal of Family and Economic Issues, 34, 460–469. [Google Scholar]