Abstract
Insufficient scientific evidence about electronic cigarettes (e-cigarettes) has led to conflicting recommendations (CRs) by credible scientific organizations, creating a public health debate that could prove especially difficult to reconcile as current and former smokers make decisions about whether to use e-cigarettes. To investigate how CRs about e-cigarettes may affect intentions to engage in healthy behaviors, 717 former and current smokers were randomly exposed to one of five conditions (varying in the level of conflict in recommendations) in this between-subject experiment. Our results indicated a significant interaction between the message level of conflict and individuals’ information avoidance, employed to maintain hope and deniability. These results suggest the effects of CRs stemming from scientific uncertainty vary with subgroups of people, pointing to several pressing theoretical and practical implications.
Keywords: uncertainty, conflicting recommendations, confusion, carryover effects, information avoidance, electronic cigarettes
Despite the human drive to reduce uncertainty and to explain the world (Berger & Calabrese, 1975), achieving complete certainty or predictability is often not plausible, especially in a context where scientific inquiry surrounding the topic is preliminary and still developing (Bradac, 2001). Defined as the “subjective perception of ignorance” (Han et al., 2011, p. 830), uncertainty arises in individuals confronted with circumstances involving probability and without access to sufficient and reliable information (Babrow et al., 1998). To better understand, co-exist with, and manage uncertainty, multiple theories have been proposed across contexts from health information to interpersonal relationships, highlighting the phenomenon’s complexity (Afifi & Weiner, 2004; Berger & Calabrese, 1975; Brashers & Babrow, 1996; Ellsberg, 1961).
More recently, decision-making in the face of scientific uncertainty has found a new case study in the booming market of electronic cigarettes (e-cigarettes). Since the introduction of e-cigarettes as an alternative nicotine delivery device to the U.S. market in 2007, the popularity and sales of e-cigarettes have been consistently on the rise. For example, the popular JUUL brand increased sales by 641% from 2016 (2.2 million) to 2017 (16.2 million; King et al., 2018). The e-cigarette market totaled $2.5 billion in 2014 (Mickle, 2015), projecting e-cigarette sales to surpass traditional cigarette sales by 2047 (Robehmed, 2013).
Despite their growing popularity, the health consequences of e-cigarettes remain a topic for scientific debate among credible health organizations. Whereas some organizations acknowledge the lack of sufficient scientific evidence, others frame e-cigarettes in either a negative or positive light by selectively emphasizing their potential risks (e.g., long-term health effects, second hand vaping; American Academy of Pediatrics [AAP], 2015, 2019; Food and Drug Administration [FDA], 2020) or benefits (e.g., harm reduction, smoking cessation; Royal College of Physicians [RCP], 2016; Truth Initiative, 2019a; World Health Organization [WHO], 2019). Thus, in the face of unresolved uncertainty about the health effects of e-cigarettes, credible organizations have introduced conflicting recommendations (CRs)—messages providing competing claims about e-cigarette use that cannot simultaneously be true—into the information environment.
Not only do CRs from credible public health institutions complicate individual decision-making about whether using e-cigarettes is a healthy or undesirable behavior, but this perceived uncertainty may spill over to other health behaviors where recommendations are clear and certain. For example, exposure to contradictory health information often creates public confusion about health behavior in cancer- and nutrition-related literature (e.g., Johnson-Taylor et al., 2007; Nagler, 2014). As credible public health sources advocate for health behaviors that reduce ones’ risk of cancer—including smoking cessation, daily fruit and vegetable consumption, routine exercise, and limited alcohol consumption—CRs about e-cigarettes for smoking cessation may activate beliefs about these off-target behaviors, artificially creating perceived uncertainty for consensus health recommendations. This carryover of confusion stemming from CRs about e-cigarettes and smoking cessation to other health recommendations may be differential based on individual strategies for managing uncertainty, yet only a few studies have investigated these potential interactions (Brashers, 2001; Carcioppolo et al., 2016).
The current study used an experiment including 717 former and current smoker participants to investigate the interaction between CRs and individuals’ information avoidance tendency (IAT)— which can change based on personal characteristics, communication experiences, and contextual factors— on both confusion about e-cigarettes and carryover effects on other health behaviors considered by the Centers for Disease Control and Prevention (CDC) as essential for lowering individual cancer risk (CDC, 2018): healthy diet, exercise, and alcohol intake. The findings of the study shed light on the decision theory of processing uncertainty (Ellsberg, 1961) and the UMT literature (Barbour et al., 2012; Brashers, 2001, 2007; Brashers et al., 2000), as well as inform practical interventions to alleviate the potential adverse effects of CRs about e-cigarettes on smokers, particularly those with low level of health IAT.
Conflicting Recommendations (CRs) about E-cigarettes
E-cigarette use continues to rise in the U.S. among adults, with the highest prevalence among youth and young adults (McMillen et al., 2015; Syamlal et al., 2016). Over a quarter of high school students use e-cigarettes, and young adults are more likely to initiate e-cigarettes than older adults (Cullen et al., 2019; Truth Initiative, 2019b). Despite the prevalence of e-cigarette use, the potential risks (e.g., long-term health effects, secondhand vaping) and benefits (e.g., harm reduction, cessation aid) associated with these devices remain unclear. Although the association between vaping and recent outbreaks of pulmonary illness was established, the public health community has yet to specify exactly which products or chemical substances in e-cigarettes cause lung injuries, exacerbating existing uncertainty, debate, and even panic about the long-term health effects (CDC, 2019).
In light of insufficient scientific evidence about e-cigarettes, contradictory information and recommendations were published by credible health organizations and professional associations. Whereas some of these statements acknowledge the lack of scientific evidence, others undermine uncertainty by framing e-cigarettes in either a positive or negative light by emphasizing the potential benefits or risks of e-cigarettes. Specifically, some emphasize that electronic nicotine delivery systems (ENDS) can be a tool for harm reduction as a potential smoking cessation aid, as several credible organizations state (e.g., RCP, 2016; Truth Initiative, 2019a; WHO, 2019). For example, Public Health England has reiterated its claim in a new campaign that “vaping is at least 95% safer than smoking” and “the devices have helped thousands of people to quit smoking” (Kmietowicz, 2018, p. 1).
At the same time, other professional groups concluded that the current evidence is insufficient to recommend ENDS for tobacco cessation among adults (Campaign for Tobacco-free Kids, 2019; National Institute on Drug Abuse [NIDA], 2019). Although some organizations have made statements about the negative long-term consequences of e-cigarettes, such as AAP (2015), who stated “ENDS have the potential to addict a new generation of youth to nicotine and reverse more than 50 years of progress in tobacco control” (p. 1), others have pointed out that the long-term consequences remain unclear (e.g., NIDA, 2019). Conflicting messages were disseminated also about the second- and third-hand effects of vaping, such as the statement from the American Academy of Pediatric Dentistry (2015) that “unrestricted access to smoking of e-cigarettes not only poses health risks to the user, but also may pose health risks to people nearby due to second hand exposure of the vapors” (p. 67), with disagreements from other organizations stressing insufficient evidence of second- and third-hand vaping (e.g., Truth Initiative, 2019a).
Adverse Outcomes and Decision Theory of Processing Uncertainty
Scientific uncertainty about e-cigarettes contributes to an information environment rife with contradictions, as evident in studies showing exposure to overall e-cigarette information is strongly and positively correlated with recall of contradictory e-cigarette information (Tan et al., 2015). Contradictory e-cigarette information from credible organizations may lead to adverse outcomes, which were documented in previous literature over a variety of health behaviors. First and foremost, exposure to contradictory health information may directly result in public confusion about the health behavior (e.g., Johnson-Taylor et al., 2007; Nagler, 2014), with ambiguity theorized as the link between contradictory information exposure and confusion (Ellsberg, 1961). According to Ellsberg’s (1961) decision theory of uncertainty, when conflicting opinions and evidence are present, individuals will experience high ambiguity and have low confidence in conclusions derived from that information, “even where there is ample quantity of information, [and] where there are questions of reliability and relevance of information” (p. 659). As a result, confusion or considerable ignorance may result from exposure to contradictory information, making individuals feel they know little about the issue or cannot respond given the available information (Ellsberg, 1961). Since CRs about the potential risks and relative benefits of e-cigarettes compared to combustible cigarettes is more relevant and salient to former and current smokers than those who have never smoked, the first hypothesis was proposed as follows.
H1: Exposure to CRs about e-cigarettes is positively associated with confusion about the health effects of using e-cigarettes among former and current smokers.
The decision theory of uncertainty processing has been applied to understand the effects of processing uncertain health-related information. In cancer-related research, people were averse to ambiguity about cancer prevention recommendations and manifested this ambiguity aversion through pessimistic or even fatalistic beliefs about the preventability of cancer (Han et al., 2006; Niederdeppe & Levy, 2007). Uncertainty about cancer prevention also predicts cancer information overload which, like fatalistic beliefs, lowers intentions to engage in cancer prevention behaviors and consequently increases cancer risk (Niederdeppe et al., 2014; Niederdeppe & Levy, 2007).
In addition to confusion and negative beliefs about a health behavior, contradictory message exposure could also have important carryover effects to other health behaviors. For example, Nagler (2014) found that natural media exposure to contradictory nutrition information was positively associated with confusion. This led people to doubt not only nutrition recommendations but also other health recommendations not subject to conflict and contradiction (e.g., exercise), making them less likely to adhere to general healthy behaviors. Therefore, people who feel confused about e-cigarettes might be less receptive to subsequent health recommendations, particularly for health behaviors similarly recommended for cancer risk reduction. If CRs about e-cigarettes for smoking cessation activate confusion about consensus recommendations to reduce cancer risk, they may also undermine health campaigns and interventions targeting other health behaviors. Thus, the second hypothesis was proposed:
H2: Former and current smokers’ confusion about e-cigarettes is negatively associated with their intention to adhere to other healthy lifestyle recommendations.
Based on this line of reasoning, we also hypothesized an indirect effect of CRs about e-cigarettes on intentions to adhere to healthy lifestyle recommendations through confusion:
H3: Former and current smokers’ confusion about e-cigarettes mediates the relationship between their exposure to CRs about e-cigarettes and their intention to adhere to healthy lifestyle recommendations.
Uncertainty Management and Information Avoidance
In recent years, uncertainty scholars have witnessed a paradigm shift from defining uncertainty as a necessarily undesirable state that motivates people to reduce it (e.g., uncertainty reduction theory; Berger & Calabrese, 1975; Gudykunst, 1995), to acknowledging that people could evaluate uncertainty as either positive or negative, an appraisal that then determines how they manage that uncertainty, as posited by uncertainty management theory (UMT) (Babrow & Kline, 2000; Brashers, 2001). Diverging from conceptualizations of uncertainty as risk that needs to be avoided (Berger & Calabrese, 1975; Gudykunst, 1995), Brashers and colleagues argued, in the framework of UMT, that individuals could at times evaluate uncertainty as a source of opportunity (Brashers, 2001; Brashers & Babrow, 1996; Brashers et al., 2000). Specifically, UMT claims that when uncertainty is appraised as a source of danger, anxiety, and fear, individuals attempt to reduce it; when uncertainty is appraised as an opportunity, associated with hope or optimism, individuals seek to maintain or increase it (Brashers & Babrow, 1996). Individuals increase or reduce uncertainty by seeking or avoiding information. For example, Brashers and colleagues (2000) found that participants with HIV/AIDS strategically deployed both information seeking and avoidance to manage uncertainty about their prognosis. Here, information avoidance can not only exacerbate uncertainty, as it does not resolve uncertainty with more information, but it also reduces uncertainty by allowing individuals to avoid potentially distressing knowledge or retreat from overwhelming information (Brashers et al., 2000).
Although information avoidance is a prominent communicative response to uncertainty, it has received less scholarly attention than other coping strategies like information seeking. Previous research tends to oversimplify information avoidance as a strategy deployed when information is perceived as unpleasant and may cause “mental discomfort or dissonance” (Case et al., 2005, p. 354). However, UMT maintains that individuals may also avoid information when they appraise their state of uncertainty as an opportunity for hope and optimism (Brashers et al., 2000; Brashers, 2001). Drawing on a mixed-method of survey and content analysis, Barbour and colleagues (2012) derived six reasons for individuals’ information avoiding behaviors: (a) maintain hope or deniability, b) resist overexposure, (c) accept limits of action, (d) manage flawed information, (e) maintain boundaries, and (f) continue with life or activities. This formative research also showed that strategies for avoiding information include removing or ignoring stimuli (e.g., avoiding people who might provide health advice) and controlling conversations (e.g., withholding information, changing the subject), providing in-depth qualitative evidence for generalizing uncertainty management research to other health contexts.
To quantitatively assess how uncertainty management influences individuals’ communication and decision-making, four uncertainty preference scales were proposed (Carcioppolo et al., 2016): (a) avoiding information to maintain uncertainty, (b) avoiding insufficient information, (c) seeking information to increase uncertainty, and (d) seeking information to reduce uncertainty. When people avoid information to maintain uncertainty, they appraise uncertainty as an opportunity and consider the information as scary. For instance, individuals diagnosed with a serious illness (e.g., terminal cancer, severe depression) may actively avoid information about unanimously high mortality of their diseases. By avoiding such information, they can maintain hope and deniability through desirable uncertainty (Barbour et al., 2012). In contrast, when avoiding information considered as insufficient, such as health information from questionable sources (e.g., a high school student’s Facebook post, a website without information about the author), people believe the information is overwhelming or flawed, causing undesirable uncertainty (Carcioppolo et al., 2016).
People differ in their tendency to avoid or approach information under distressful and overwhelming information environments (Brashers, 2001). Specifically, exposed to the same amount of e-cigarette information, individuals with high avoidance are likely to process and be influenced by less information than those with low avoidance, by filtering out certain amount of information that is undesirable to either maintain or reduce uncertainty. Thus, individuals’ level (high vs. low) of information avoidance tendencies (IAT) may moderate their exposure to CRs and consequently influence their level of confusion about e-cigarettes. To contribute to understudied information avoidance behaviors and better understand how individuals’ level (high vs. low) of IAT may interact with the effects of exposure to CRs, we only focused on information avoidance strategies in the current study and thus proposed two research questions:
RQ1: Do levels (high vs. low) of IATs of former and current smokers moderate the positive association between CRs about e-cigarettes and confusion?
RQ2: Does the indirect effect of CRs about e-cigarettes on intentions to adhere to healthy lifestyle recommendations through confusion depend upon the levels (high vs. low) of IATs of former and current smokers?
Method
Participants
Current (n = 408) and former (n = 309) adult smokers from the United States were recruited from online surveys conducted by Survey Sampling International (now Dynata) in April 2018 and were compensated directly by Dynata. Current and former smokers were examined because CRs about the potential harms and comparative benefits of e-cigarettes as a smoking cessation tool are most salient to this population. Participants’ smoking status was determined by lifetime smoking of at least 100 cigarettes. Those who had not smoked at least 100 cigarettes in their lifetime were ineligible for the current study. We also excluded the responses from those who failed the attention check questions.
Participants ranged in age from 21 to 99 with an average age of 52.4 years (SD = 15.4). The majority of participants were female (55.5%) and White (87.7%).1 Approximately half of the participants indicated that they had ever tried vaping (n = 354, 49.4%), among whom 29.1% (n = 103) were daily vapers, 30.5% (n = 108) were occasional vapers, and 40.4% (n = 143) were non-vapers by the time the study was conducted. Regarding their highest level of education, 12.7% (n = 91) reported holding a college degree or above, 29.3% (n = 210) completed some college or technical school, 44.1% (n = 316) graduated from high school, and 13.9% (n = 100) had less than a high school education.
Procedure
To test the hypotheses and examine the interaction between CRs and individuals’ IAT, a five condition (conflicting recommendations) between-subjects experiment was employed. IAT—an exogenous variable measured prior to random assignment—was treated as an individual characteristic moderator. The approval of the study protocol was obtained by the university’s Institutional Review Board.
Participants were first asked to answer two eligibility questions about age and smoking status. Adult participants who had smoked at least 100 cigarettes then answered two questions about their vaping behaviors and seven questions measuring their IAT. Next, participants were randomly assigned to one of five conditions, including (1) a treatment condition containing CRs about e-cigarette use for smoking cessation, and four control conditions not including any CRs about e-cigarette use: (2) recommendations favoring (pro-) e-cigarette use for cessation, (3) recommendations discouraging (anti-/con) e-cigarette use for cessation, (4) a general description of e-cigarettes without recommendations, and (5) a no-message control.
The one-sided control conditions were designed to understand the unique role of two-sided CRs, such as the role of motivated reasoning among motivated subgroups of former and current smokers. We also included both the no-recommendation control and the no-message control conditions so that we could isolate the effect of even being exposed to any e-cigarette information, which likely activates an individual’s previous exposure and its sentiment more so than the no-message control.2 After randomization and message exposure for the four message conditions—the treatment condition and three message control conditions (2 – 4)—subjects responded to questions measuring their confusion towards e-cigarettes and intention to adhere to healthy lifestyle recommendations as the outcome variables. Participants randomly assigned to the no-message control condition (condition 5) skipped any e-cigarette-related recommendation and proceeded directly to the outcome measure questions (i.e., confusion, intention to adhere to healthy behaviors). Upon completion, all participants were directed to the debriefing page, where the purpose of the study was detailed, accurate and timely information about e-cigarettes was presented, and they were thanked for their participation.
Stimuli
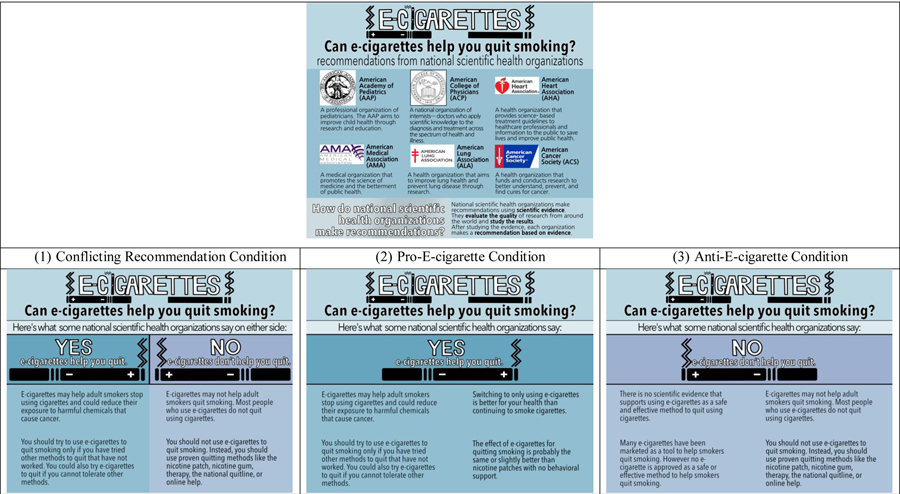
Messages were adapted from publicly available statements by credible national scientific health organizations about e-cigarettes and designed as infographics to increase readability. Across the four message conditions, we presented information from six credible scientific health organizations (see Figure 1 for details), from which we collected the recommendations or statements. However, we did not attribute each individual recommendation or statement to any of the listed organizations in order to avoid any potential negative consequence toward any particular source when individuals processed and appraised those messages during the study.
Figure 1.
Stimuli for the Recommendation Conditions (Condition 1–3)
All four message conditions contained four propositions, providing answers to the question “Can e-cigarettes help you quit smoking?” for the three recommendation conditions (conditions 1–3), and the question “What are e-cigarettes?” for the message control condition (condition 4). The treatment CRs condition (condition 1) contained two arguments endorsing the use of e-cigarettes for smoking cessation, and another two emphasizing the potential risks and discouraging the use of e-cigarettes. The two recommendation control conditions (conditions 2 and 3) presented one-sided recommendations only. Specifically, the pro-e-cigarette and the anti-e-cigarettes conditions included four arguments endorsing or discouraging e-cigarettes use respectively. The message control condition only provided introductory information about e-cigarettes, without providing any recommendation about using or not using e-cigarettes. No information was presented to participants randomized to the no-message control condition. Details of the stimuli for conditions 1–3 can be found in Figure 1.
Measures
Vaping Behavior
Participants’ vaping status was evaluated with two questions. The first question asked whether they have ever used e-cigarettes in their entire life, with three options provided (i.e., “I have never tried them,” “I have tried them, but not in the past 30 days,” and “I used them at least once in the past 30 days”). The second question was only shown to those who selected the third option, asking whether they were currently using e-cigarettes on a 3-point scale (1 = not at all, 2 = some days, 3 = every day).
Information Avoidance Tendencies (IAT)
Questions evaluating individuals’ IAT were measured exogenously prior to stimuli exposure and adapted from the uncertainty preference scale validated by Carcioppolo et al. (2016). Participants indicated their answers on a 7-point Likert scale (1 = strongly disagree, 7 = strongly agree). According to a confirmatory factor analysis (CFA), IAT that includes two factors (i.e., information avoidance to maintain uncertainty, avoidance of insufficient information to reduce uncertainty) fit the data very well as a second-order latent construct, χ2 (12) = 21.74, p = .04; CFI = .99, TLI = .97, RMSEA = 0.050 90% CI [0.010, 0.084], SRMR = 0.035. We then conducted CFAs on these two factors separately, which were analyzed as potential moderators individually. Information avoidance to maintain uncertainty was measured under a stem question “I tend to AVOID health information because” followed by four statements: “It can be depressing,” “I get anxious when I think about my health,” “Being constantly reminded of it makes me nervous about my own health condition,” and “It can be scary to think about” (α = .86, M = 4.52, SD = 1.47, Mdn = 4.75). A CFA yielded good model fit to the data, χ2 (2) = .39, p > .05; CFI = 1.00, TLI = 1.00, RMSEA = 0.000 90% CI [0.000, 0.066], SRMR = 0.004, with item loadings ranging from .77 to .89. The same stem question was used to measure avoidance of insufficient information to reduce uncertainty, followed by three statements: “There’s a lot of misinformation out there, so it’s difficult to know which is truthful,” “The recommendations are always changing,” and “The amount of information out there can be overwhelming” (α = .77, M = 5.03, SD = 1.29, Mdn = 5.00). Given a just-identified (or saturated) latent construct, a CFA yielded perfect model fit with item loadings ranging from .77 to .88. The normality assumption was met for all items. Two average scores were calculated for these two IAT factors respectively, and later dichotomized using a median split to prepare for the inferential statistical analyses. We analyzed the IATs as dichotomous moderators because (a) the operationalization is consistent with our RQs, and (b) categorizing participants into two groups not only adds to the interpretability of the results, but also provides more useful insights to the targeting strategies in message design for future interventions.
E-cigarette Confusion
To understand participants’ confusion about e-cigarettes after being exposed to the stimuli (or general confusion about e-cigarettes for participants in the no-message control condition without any message exposure), three reverse-coded statements were implemented on a 5-point Likert scale that ranged from 1 = strongly disagree to 5 = strongly agree (Nagler, 2014). Statements included “E-cigarette research findings make sense to me,” “I have the knowledge I need about tobacco products (regular cigarettes, e-cigarettes, etc.) to stay healthy,” and “I understand scientists’ recommendations about how risky tobacco products (regular cigarettes, e-cigarettes, etc.) are” (M= 2.00, SD = .74, α = .62). All questions met the normality assumption and were reverse coded in analyses, with higher values indicating higher level of confusion about e-cigarettes. Since the CFA model for e-cigarette confusion is saturated, the model produced perfect fit with item loadings ranging from .62 to .81. These three statements measuring individuals’ e-cigarette confusion were averaged to form an index for statistical analyses.
Intentions to Adhere to Healthy Lifestyle Recommendations
Participants were asked to indicate their intention to adhere to three healthy lifestyle recommendations (i.e., consumption of fruits and vegetables, exercising, and limited alcohol intake) using a 5-point Likert scale that ranged from 1 = very unlikely to 5 = very likely (Nagler, 2014). Items provided specific recommendations for each healthy lifestyle behavior, including “Science shows that having five or more servings of fruits and vegetables most days is a healthy choice. How likely is it that you will have five or more servings of fruits and vegetables most days in the next year?” (M = 3.52, SD = 1.16); “Science shows that exercising at least three times in most weeks is a healthy choice. How likely is it that you will exercise at least three times in most weeks over the next year?” (M = 3.57, SD = 1.23); and “Science shows that limiting the alcohol you drink (up to 1 drink per day for women and up to 2 drinks per day for men) is a healthy choice. How likely is it that you will limit the alcohol you drink in the next year?” (M = 3.90, SD = 1.19).3
Analysis
Prior to hypotheses testing, all variables were carefully screened to ensure the assumptions of normality, linearity, and homoscedasticity. Bivariate associations among all variables are reported in Table 1. No correlation coefficient was higher than .40,4 which is well below the recommended threshold of .70 (Tabachnick et al., 2001) and suggested multicollinearity was of little concern. Since randomization guaranteed the statistical independence between condition indicators and other independent variables, we proceeded with our primary analyses.
Table 1.
Bivariate Correlations and Descriptive Statistics for All Continuous Variables (N = 717).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Avoid info to maintain uncertainty | -- | |||||||
| 2. Avoid insufficient information | .58*** | -- | ||||||
| 3. E-cigarette confusion | −.08* | −.10* | -- | |||||
| 4. Intention to maintain healthy diet | .08* | .04 | −.19*** | -- | ||||
| 5. Intention to exercise | .04 | .07 | −.18*** | .40*** | -- | |||
| 6. Intention to limit alcohol intake | .08* | .07 | −.22*** | .17*** | −.22*** | -- | ||
| 7. Age | −.28*** | −.13** | .03 | −.15*** | −.20*** | .04 | -- | |
| 8. Vaping days | −.06 | .04 | −.05 | .00 | .07 | .21** | .09 | -- |
|
| ||||||||
| Mean | 4.52 | 5.03 | 2.00 | 3.52 | 3.57 | 3.90 | 52.42 | 18.09 |
| SD | 1.47 | 1.29 | .74 | 1.16 | 1.23 | 1.19 | 15.44 | 10.64 |
Note.
p< .05,
p< .01,
p< .001.
One-way and two-way analyses of variance (ANOVA) were employed to test H1 and RQ1 respectively, with e-cigarette confusion as the outcome variable and planned contrasts between the treatment group with CR exposure and each of the control conditions. The two measures derived from IAT (i.e., information avoidance to maintain uncertainty, avoidance of insufficient information to reduce uncertainty) were analyzed as moderators individually. To test H2, hierarchical linear regressions were obtained, controlling for individuals’ age, gender, and vaping status. H3 was tested by three mediation analyses for each control condition. We then examined whether the indirect effects—CR exposure leads to e-cigarette confusion, which further predicts intention to adhere to healthy lifestyle recommendations—were conditioned on participants’ IAT. To achieve this goal, moderated mediation analyses were performed. The mediation and the moderated mediation analyses were conducted using Model 4 and Model 7, respectively, in PROCESS (Hayes, 2017). To examine indirect effects, bootstrapping was implemented to obtain bias-corrected and accelerated 95% confidence intervals (CIs) for each indirect effect (Preacher & Hayes, 2008), with the number of replications set to 10,000 to improve the precision of bias-corrected CIs (MacKinnon et al., 2004). All analyses were performed in SPSS v.25.
Results
Main and Moderating Effects
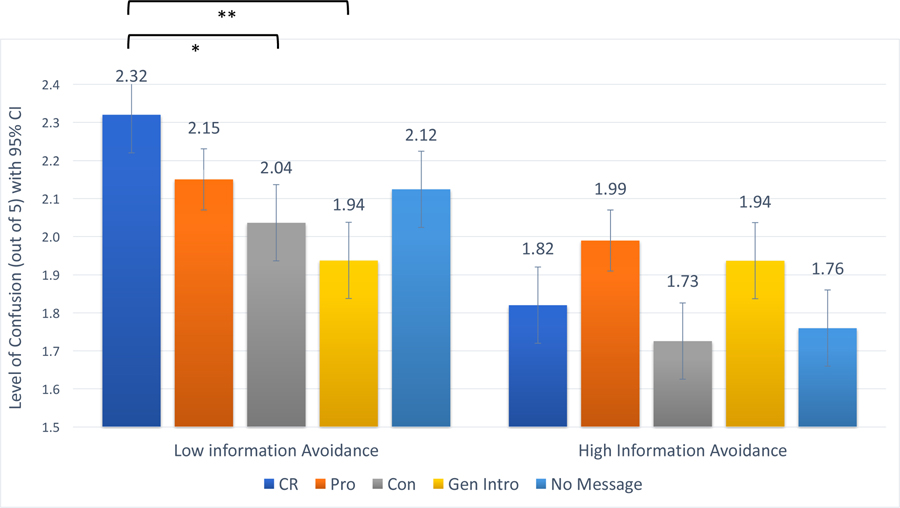
No main effect was observed for the experimental condition on confusion, F (4, 712) = 2.038, p = .087, which failed to support H1. To test the moderating effects of IAT levels on the association between CRs about e-cigarettes and confusion of CRs (addressing RQ1), we conducted a two-way ANOVA and found a significant interaction between the condition and information avoidance to maintain uncertainty on e-cigarette confusion, F(4, 707) = 2.564, p = .037, η2 = .014. Post-hoc analyses, both with and without Bonferroni correction, showed that participants presented with CRs had significantly more confusion than participants presented with one-sided anti-e-cigarette (p = .017) or general control messages (p = .001) only among those with low level of information avoidance to maintain uncertainty (see Figure 2). We observed no significant interaction effect between condition and (high vs. low) avoidance of insufficient information on confusion, F(4, 707) = 1.486, p = .205.5
Figure 2.
Interaction Effect between Experimental Condition and Information Avoidance to Maintain Uncertainty on Confusion about Electronic Cigarettes (E-Cigs)
Note. CR = conflicting recommendations about e-cig use for smoking cessation, Pro = recommendations favoring e-cig use for cessation, Con = recommendations discouraging e-cig use for cessation, Gen Intro = general introduction of e-cigs without recommendations. *p < .05; **p < .01.
Three hierarchical linear regressions were obtained to examine whether e-cigarette confusion reduces individuals’ intentions to adhere to healthy behaviors (H2). More confusion was associated with lower intentions to follow all three healthy behavior recommendations: to consume fruits and vegetable (b* = −.18, p < .001), exercise (b* = −.18, p < .001), and limit alcohol intake (b* = −.23, p < .001) (see Table 2 for details). Thus, H2 was supported.
Table 2.
Hierarchical Linear Regression Models of the Relationship between E-Cigarette Confusion and Individuals’ Intentions to Adhere to Healthy Behaviors.
| DV: healthy diet | DV: exercise | DV: limit alcohol | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| b * | SE | t | b * | SE | t | b * | SE | t | |
| Model 1 | |||||||||
| Age | −.16*** | .00 | −3.91 | −.18*** | .00 | −4.55 | .03 | .00 | .74 |
| Female | −.05 | .09 | −1.25 | −.03 | .09 | −.87 | −.01 | .09 | −.36 |
| Vaping | −.02 | .09 | −.52 | .04 | .10 | .86 | −.02 | .10 | −.38 |
| R 2 | .03 | .04 | .00 | ||||||
| Model 2 | |||||||||
| Age | −.15*** | .00 | −3.82 | −18*** | .00 | −4.47 | .04 | .00 | .95 |
| Female | −.04 | .09 | −1.07 | −.03 | .09 | −.70 | −.01 | .09 | −.12 |
| Vaping | −.02 | .09 | −.41 | .04 | .10 | 1.00 | −.01 | .10 | −.24 |
| Confusion | −.18*** | .06 | −4.96 | −.18*** | .06 | −4.84 | −.23*** | .06 | −6.15 |
| R 2 | .06 | .07 | .05 | ||||||
| ∆R2 | .03*** | .03*** | .05*** | ||||||
Note.
p < .05
p < .01
p < .001.
Indirect Effects and Moderated Mediation
H3 predicted that the relationship between CR exposure about e-cigarettes and healthy lifestyle intentions is mediated by individuals’ confusion. Mediation analysis indicated that e-cigarette confusion did not significantly mediate the relationship between exposure to CRs and individuals’ intention to consume fruits and vegetables, exercise, or limit alcohol intake, when compared to each of the four control conditions, which were dummy coded (CRs condition coded as 1 and the four control conditions as 0 for each dummy variable). Table 3 presents a summary of all Hs and RQs. Given the null indirect effects, which failed to support H3, we proceeded to examine whether the indirect effects were moderated by IATs.
Table 3.
Summary of Analyses of Hypotheses and Research Questions
| Hs or RQs | Analysis | Result |
|---|---|---|
| 1. H1: E-cig CRs → confusion (main effect) | Presented in manuscript | Not supported |
|
| ||
| 2. H2: E-cig confusion → adherence to healthy lifestyle recommendations | Presented in manuscript | Supported |
|
| ||
| 3. H3: E-cig CRs → confusion → adherence to healthy lifestyle recommendations | Not supported | |
| → adherence to consumption of fruits and vegetable | −.056 (95% CIs [−.144, .005]) | |
| → adherence to exercise | −.046 (95% CIs [−.115, .005]) | |
| → adherence to limited alcohol intake | −.056 (95% CIs [−.140, .007]) | |
|
| ||
| 4. RQ1: E-cig CRs × level of IAT to maintain uncertainty→ confusion (moderating effect) | F (4, 707) = 2.564, p = .037 | Effect found for IAT to maintain uncertainty |
| E-cig CRs × level of IAT to reduce uncertainty→ confusion (moderating effect) | F (4, 707) = 1.486, p = .205 | |
|
| ||
| 5. RQ2: E-cig CRs × level of IAT to maintain uncertainty → confusion→ adherence to healthy lifestyle recommendations (moderated indirect effect) | Effect found for IAT to maintain uncertainty | |
| → adherence to consumption of fruits and vegetable |
.178 (95% CIs [.059, .330]) | |
| → adherence to exercise |
.148 (95% CIs [.027, .319]) | |
| → adherence to limited alcohol intake |
.178 (95% CIs [.041, .365]) | |
Note. The analyses for H3 and RQ2 presented were the comparisons between the experiment and non-cessation message control condition. The indirect effects of pairwise comparison between the experiment and all other conditions were not significant. The full moderated mediation analyses are presented in Table 4. E-cig = electronic cigarettes. IAT = info avoidance tendency. The level of IAT to reduce uncertainty was not a significant moderator in answering RQ1 and therefore not analyzed in testing RQ2.
To address RQ2, two dimensions of individuals’ IAT were median-split and dummy coded. Given the non-significant interaction between condition and avoidance of insufficient information to reduce uncertainty, only information avoidance to maintain uncertainty was analyzed as a potential moderator. The indirect effects of experimental condition on intention to adhere to health lifestyle recommendations mediated by e-cigarette confusion were tested at two levels of participants’ information avoidance to maintain uncertainty (below or above the median)6 in consistency with the two-way ANOVA. Condition was also dummy coded, with the CRs condition coded as 1 and the four control conditions as 0 for each dummy variable. The detailed moderated mediation results are presented in Table 4.
Table 4.
Moderated Mediation Analyses Conditional on Information Avoidance Preference
| Conditional Indirect Effects on Intention to Maintain Healthy Diet | |||||
|---|---|---|---|---|---|
|
| |||||
| Control Condition | Index of Moderated Mediation | IAT | b | SE | BC CIs |
| One-sided Pro | .134 (95% CIs [.027, .266]) | L | −.067 | .048 | [−.158, −.001] |
| H | .067 | .050 | [−.011, .153] | ||
| One-sided Con | .049 (95% CIs [−.027, .144]) | L | −.074 | .047 | [−.159, −.012] |
| H | −.025 | .036 | [−.086, .026] | ||
| Non-cessation message | .178 (95% CIs [.059, .330]) | L | −.136 | .065 | [−.254, −.048] |
| H | .042 | .043 | [−.028, .121] | ||
| No message | .048 (95% CIs [−.054, .159]) | L | −.069 | .048 | [−.155, −.002] |
| H | −.021 | .043 | [−.094, .044] | ||
|
| |||||
| Conditional Indirect Effects on Intention to Exercise | |||||
|
| |||||
| Control Condition | Index of Moderated Mediation | IAT | b | SE | BC CIs |
| One-sided Pro | .144 (95% CIs [.006, .312]) | L | −.072 | .051 | [−.182, .021] |
| H | .072 | .056 | [−.027, .194] | ||
| One-sided Con | .049 (95% CIs [−.047, .164] | L | −.073 | .043 | [−.173, −.004] |
| H | −.024 | .036 | [−.107, .041] | ||
| Non-cessation message | .148 (95% CIs [.027, .319] | L | −.113 | .056 | [−.237, −.023] |
| H | .035 | .040 | [−.034, .127] | ||
| No message | .044 (95% CIs [−.060, .186]) | L | −.064 | .047 | [−.172, .010] |
| H | −.020 | .040 | [−.103, .060] | ||
|
| |||||
| Conditional Indirect Effects on Intention to Limit Alcohol | |||||
|
| |||||
| Control Condition | Index of Moderated Mediation | IAT | b | SE | BC CIs |
| One-sided Pro | .112 (95% CIs [.002, .268] | L | −.056 | .042 | [−.150, .014] |
| H | .056 | .047 | [−.024, .163] | ||
| One-sided Con | .058 (95% CIs [−.050, .198] | L | −.086 | .051 | [−.200, −.006] |
| H | −.029 | .041 | [−.120, .047] | ||
| Non-cessation message | .178 (95% CIs [.041, .365] | L | −.136 | .062 | [−.273, −.035] |
| H | .042 | .046 | [−.039, .144] | ||
| No message | .037 (95% CIs [−.056, .145]) | L | −.053 | .040 | [−.145, .010] |
| H | −.016 | .036 | [−.097, .049] | ||
Note. ES= Indirect effect size. BC CIs= Bias-corrected bootstrapping confidence intervals. L= Low level of information avoidance to maintain uncertainty. H= High level of information avoidance to maintain uncertainty.
When comparing the CRs condition with the no-cessation message condition, there is a clear pattern that the mediation path—exposure to CRs increasing confusion, and confusion in turn reducing intention to adhere to three healthy behaviors—was significantly moderated by participants’ level of IAT to maintain uncertainty. The overall significant index for moderated mediation suggests that this mediational path was clearer and stronger in magnitude among those with lower levels of IAT to maintain uncertainty. In fact, the 95% CIs of this mediational path fell below zero only among those below the median point of the moderator, but not among those above. Regarding the pairwise comparison between the CRs condition and other control conditions, the overall index for moderated mediation pointed to similar patterns in the comparison with the one-sided pro-e-cigarette condition. As for the contrast with the one-sided anti-e-cigarette condition, although the overall indices did not reach significance, sub-group analyses revealed that the 95% CIs of the mediation path fell below zero only among those with low information avoidance to maintain uncertainty, consistently across three health behaviors. No clear pattern of moderated mediation was observed for the comparison with the no-message control.
Discussion
Given the nature of the scientific process, decision-making in an environment filled with uncertainty is the norm rather than the exception, not only in health contexts but in all societal contexts driven by the scientific enterprise. In this study, we contributed to and extended theories of uncertainty processing (Ellsberg, 1961) and management (Brashers, 2001; Brashers & Babrow, 1996; Brashers et al., 2000) by investigating the influence of exposure to CRs about e-cigarettes on confusion about using these products, the carryover effects of e-cigarette CRs on other health behaviors, and the moderating role of IAT. Although the effects we identified were small in magnitude, the prevalence of CRs in today’s information environment means that even modest effects may have meaningful and socially significant implications (Glanz et al., 2008). Thus, our findings have both theoretical and practical implications worth noting.
First, the non-significant overall effect of CR exposure on confusion (H1) was at odds with previous research that pointed to negative effects in the context of nutrition messages (Lee et al., 2018; Nagler, 2014). However, when analyzing participants based upon their IATs, we did find the aforementioned negative effect (RQ1), but only among individuals with a lower IAT to maintain uncertainty. Thus, we have reason to speculate that the non-significant effect of CRs among participants with high levels of IAT may offset the effect among their counterparts, which contributed to the non-significant overall effect. It should be noted that our second factor of IAT (i.e., avoiding insufficient information to reduce uncertainty), which is often used to measure avoidance of misinformation from sources less credible than the ones used in the current study, did not significantly moderate the effects of CR exposure on confusion.
Beyond the total effects, we also found concerning carryover effects of confusion in congruence with prior research (Nagler, 2014; Niederdeppe & Levy, 2007), which mediated the relationships between CR exposure and lower intention to adhere to healthy behaviors among participants with low IAT. When exposed to CRs, individuals may not only feel confused, but hold fatalistic and overloaded beliefs discouraging their adherence to other risk-reducing behaviors (Jensen et al., 2014; Niederdeppe & Levy, 2007). The indirect effects were also conditional on individuals’ IAT to maintain uncertainty, with robust results obtained when comparing the CRs experimental condition and the no-cessation message condition. Because people with high IAT to maintain uncertainty perceive information as scary, they are able to remain optimistic by resisting that undesirable information and less likely to hold fatalistic beliefs about healthy behaviors. However, such conditional effects were not found between the CRs experimental condition and other control conditions. One plausible explanation is that with the public communication environment rife with pro- and anti-e-cigarette information, which would influence individuals’ cognitions and behavior through information seeking behavior (Yang et al., 2019), the one-sided recommendation stimuli may activate participants’ recall of e-cigarette exposure prior to the experiment. Should the naturalistically acquired information be contradictory to the manipulated one-sided recommendation, participants may also feel confused, which mitigates the comparative effects between the CRs and one-sided control conditions.
These findings provide an important contribution to research on scientific uncertainty in the context of emerging controversial public health issues. Prior research in this area focused on correlational data (Dieckmann et al., 2015; Han et al., 2006; Jensen et al., 2014; Lee et al., 2018; Nagler, 2014; Niederdeppe & Levy, 2007; Tan et al., 2015), and thus, the need to establish causality through experiments was stressed (Carpenter et al., 2015; Nagler, 2014). Our study fills this gap by establishing the causal influence of exposure to e-cigarette CRs on smokers’ cognitions and behavioral intentions, and by examining the conditions under which this effect is triggered, by incorporating individual’s IAT as a moderator for a closer investigation of this mechanism.
Theoretical Implications
The detection of the conditional indirect effects is of theoretical importance from four perspectives. First, our findings echo the arguments of UMT (Brashers, 2001; Brashers & Babrow, 1996; Brashers et al., 2000) that, at times, uncertainty may not be perceived as a risk but as an opportunity, showing divergence from the early uncertainty literature (Berger & Calabrese, 1975; Gudykunst, 1995). Since UMT originated in cancer information literature, the applicability of UMT in other behaviors that was supported by the current findings further extended the theory by developing a deeper and nuanced understanding of the concepts. Although (active) avoidance of information was previously considered to be a passive uncertainty management strategy, labeled as a maladaptive fear control response (Witte, 1992), participants actually benefited from their IAT to maintain uncertainty in this study and were less likely to exhibit the adverse cognitive and behavioral outcomes resulting from exposure to CRs, adding to the “perceived” opportunity of uncertainty theorized in UMT.
Second, our results extend the decision theory of processing uncertainty (Ellsberg, 1961), which laid a theoretical foundation for the cognitive effects of CR exposure including confusion, by demonstrating the moderating role of individual differences in managing uncertainty. The moderating effects of IAT to maintain uncertainty highlight the heterogeneity of the population in processing and coping with uncertainty and emphasize the necessity of segmenting the population at deeper levels (e.g., cognition), above and beyond demographic differences when studying uncertainty management. Third, our results support trends shifting the social norm favoring information seeking as more beneficial than information avoidance (Lapinski & Rimal, 2005) by demonstrating CRs may not have negative consequences on the population homogeneously, and by recognizing individual-level differences in managing uncertainty through information avoidance. Such a paradigm shift indicates the complex and multi-faceted nature of communication in the face of scientific uncertainty. Finally, when processing health information and making consequential health decisions, the uncertainty associated with complex scientific issues could be deeply personal. Prior UMT studies have focused primarily on the relationship between appraisal of uncertainty and communicative management strategies, with limited delving into the cognitive process of the appraisal. The current study points to extending UMT by considering the role of confusion and other relevant cognitive factors, such as need for closure (Sweeny et al., 2010).
In addition, the other dimension of IAT—avoiding insufficient information to reduce uncertainty, measuring individual’s negative appraisal of uncertainty and operationalized as the avoidance of misinformation (Carcioppolo et al., 2016)—was not significant in moderating the direct and indirect effects in this study. Although Barbour and colleagues (2012) qualitatively conceptualized the different objectives of information seeking in the uncertainty management framework and conjectured that “increasing or maintaining uncertainty through avoiding information may be functional” (p. 225), the current study is among the first to provide quantitative evidence to support the functional differentiation between the two IAT dimensions; that the uncertainty management strategy may have an effect on individuals’ health behaviors and outcomes (Barbour et al., 2012). The findings also add evidence to the discriminant validity of these two constructs as discrete measures of information avoidance, both in the scientific uncertainty context (Carcioppolo et al., 2016) and beyond, including communicating about health, science, crisis, the environment, and risk. Given that the IAT is not trait-based and contingent on the context and messages, future research is encouraged to explore how both IAT factors moderate the effects of receiving CRs in other contexts on individuals’ confusion and other cognitive and behavioral reactions.
Although seeking and avoiding information were identified as the two primary behaviors individuals perform when managing uncertainty, the IAT has received considerably less scholarly attention or been presumed as less beneficial than the seeking behavior. Furthermore, according to UMT (Brashers, 2001; Brashers et al., 2000), when uncertainty is appraised as opportunity associated with optimism, individuals may employ both information seeking and avoidance strategies to maintain uncertainty, a positive correlation supported in previous research (Carcioppolo et al., 2016). Therefore, the current findings not only highlight the importance and potential positive effects on protective behaviors in response to scientific uncertainty, but also point to a future direction of uncertainty management scholarship that information seeking behaviors are worth studying in tandem with information avoidance.
Practical Implications
The practical implications of the findings are two-fold: one for the public and consumers of information and one for educators and message designers. There have been heated and lingering discussions surrounding the health effects of e-cigarettes, catalyzed in part by the recent confirmed deaths and probable cases of fatal pulmonary illness linked to vaping across the U.S. (Lovelace, 2019). The increased attention to the topic in the media could overwhelm those relying on e-cigarettes as quitting devices. Our findings suggest that individuals who wish to avoid the adverse effects of CRs should try to avoid excessive consumption of information before scientific consensus emerges. Simply put, when knowledge is still preliminary and developing, for example during the early stages of epidemics (e.g., COVID-19), attempting to solve the distress of uncertainty by consuming as much information as possible from a wide variety of sources could be detrimental. Instead, one should take cautionary steps and avoid reaching conclusions before empirical data solidify.
As for public educators and message designers, the identification of moderation effects demonstrates that some sub-populations (e.g., individuals with low levels of IAT) are more vulnerable to CR effects. Dismissing the adverse effects of CRs around scientific uncertainty due to the lack of a main effect is thus not only misleading, but potentially dangerous. Based on our findings, we recommend that future campaigns or interventions educate the public by (a) clearing the misunderstanding that more information is always favorable, (b) informing the potential benefits of information avoidance, and (c) giving suggestions of not processing— or at least cautiously processing— CRs while the scientific evidence is insufficient. Such campaigns or interventions should be explicitly designed to minimize carryover effects and increase self-efficacy, particularly among vulnerable populations. It is worth noting that this recommendation holds for our definition of CRs, where uncertain evidence produces competing claims that cannot simultaneously be true. Other problems rooted in conflict (e.g., where information about known harms and benefits produces conflict over what decision to make) require their own strategy for handling information avoidance.
Limitations and Future Research
Several limitations should be noted. First, although we adopted an established confusion measure (Nagler, 2014), the scale reliabilities in both the current and previous studies were not high. Since Cronbach’s α is a function of the number of items, with more items producing higher α with a certain average item intercorrelations (Cortina, 1993), that the confusion scale was measured by three items may explain the low α. Relatedly, the experimental conditions and confusion were e-cigarette-specific, whereas the IAT was operationalized by a global measure. Therefore, we encourage future research to develop a more reliable confusion measure, and replicate this study to examine whether the results would differ if a behavior-specific operationalization of IAT is used. Second, it is also worth noting that we only measured participants’ intention, rather than the actual implementation, of conducting other health behaviors, which future studies are encouraged to investigate. Third, our study used a single message (infographic designed to increase readability of CRs) within each condition, but this approach is not immune from case-category confounding (Jackson et al., 1989). For instance, participants’ (un)familiarity with harmful chemicals or listed health organizations might influence their answers. Further inquiry should consider multiple cases of CRs covering a wider range of arguments in regards to using e-cigarettes for smoking cessation (e.g., secondhand and third-hand aerosol exposure, long-term consequences, etc.) to contribute a greater understanding of this mechanism.
Despite these limitations, this study experimentally tested how individual differences in IATs moderate the effects of exposure to CRs on increased confusion and lowered intentions to adhere to healthy behaviors in general. The specification of the moderated mediation models shed theoretical and practical light on the potential adverse effects of CRs for those with lower levels of information avoidance to maintain uncertainty, which should be taken into account when designing future public messages. It points to the advantage of accounting for individual differences in the acceptance of, and processing of, uncertain scientific information when designing tailored interventions to ameliorate the adverse effects caused by scientific uncertainty.
Acknowledgments
Research reported in this publication was supported by the National Cancer Institute (NCI) of the National Institutes of Health (NIH) and FDA Center for Tobacco Products (CTP) under Award Number P50-CA179546-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration (FDA). We thank Dr. Paul Schrodt and three anonymous reviewers for their constructive feedback in the peer review process.
Footnotes
Our sample, although predominantly being White, showed consistency with the demographics of tobacco and e-cigarette users in nationally representative samples. According to the latest Health Information National Trends Survey (HINTS; National Cancer Institute, 2019) dataset, 80.8% and 80.6% tobacco users and e-cigarette users respectively reported as White.
The information level across conditions might be different, which future research is encouraged to take into account. Specifically, the stimuli in the two-sided condition may be perceived as more informative than those in the one-sided or no recommendation control conditions.
Based on the conceptualization of the carryover effects and previous literature (e.g., Nagler, 2014), the healthy lifestyle intention should not be treated as a latent variable measured by three specific behaviors, because the intention for healthy lifestyle is not a global measure, and the three specific behaviors examined in the current study are not inherent scale for healthy lifestyle. For instance, it is not uncommon that one individual adheres to healthy dieting but does not conduct enough physical activity (or goes to gym frequently but consumes a high volume of alcohol). Therefore, the three behaviors (i.e., fruit and vegetable intake, exercise, and limited alcohol intake) should be analyzed individually to provide a clear picture of the moderated mediating mechanism.
Although the two information avoidance constructs (i.e., avoid to maintain uncertainty and avoid insufficient information) were correlated at the magnitude of r = .58, they were analyzed in separate statistical models, and therefore did not cause multicollinearity.
According to the a priori power analysis using G*power (Faul et al., 2009), when the power (1 − β) was set at .95 (α = .05), 470 subjects are needed in order to detect a small effect size (.20). Therefore, we believe our design is well-powered.
When median splitting the sample based on participants’ score of IAT to maintain uncertainty, 44 participants with the median score were categorized in the low information avoidance group. Acknowledging that assigning the participants in the median IAT level (n = 44) to the low information avoidance group may introduce arbitrariness, we conducted further analyses of splitting the participants into three groups (i.e., low [M − SD], median [M], high [M + SD]) based on their IAT and obtained similar results. The detailed results of additional analyses are available upon request.
References
- Afifi WA, & Weiner JL (2004). Toward a theory of motivated information management. Communication Theory, 14(2), 167–190. 10.1111/j.1468-2885.2004.tb00310.x [DOI] [Google Scholar]
- American Academy of Pediatric Dentistry. (2015). Policy on electronic cigarettes. Reference Manual, 38(6), 67–69. Retrieved from https://www.aapd.org/assets/1/7/P_ElectronicCig.pdf [Google Scholar]
- American Academy of Pediatrics. (2015). Electronic nicotine delivery systems. Pediatrics, 136(5), 1018–1026. 10.1542/peds.2015-3222 [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. (2019). AAP policy statements: E-cigarettes need stronger regulations to prevent youth access and use. Retrieved from https://www.aap.org/en-us/about-the-aap/aap-press-room/Pages/AAP-Policy-Statement-E-Cigarettes-Need-Stronger-Regulations-to-Prevent-Youth-Access-and-Use.aspx
- Babrow AS, & Kline KN (2000). From “reducing” to “coping with” uncertainty: Reconceptualizing the central challenge in breast self-exams. Social Science and Medicine, 51(12), 1805–1816. 10.1016/S0277-9536(00)00112-X [DOI] [PubMed] [Google Scholar]
- Babrow AS, Kasch CR, & Ford LA (1998). The many meanings of uncertainty in illness: Toward a systematic accounting. Health Communication, 10(1), 1–23. 10.1207/s15327027hc1001_1 [DOI] [PubMed] [Google Scholar]
- Barbour JB, Rintamaki LS, Ramsey JA, & Brashers DE (2012). Avoiding health information. Journal of Health Communication, 17(2), 212–229. 10.1080/10810730.2011.585691 [DOI] [PubMed] [Google Scholar]
- Berger CR, & Calabrese RJ (1975). Some explorations in initial interaction and beyond: Toward a developmental theory of interpersonal communication. Human Communication Research, 1(2), 99–112. 10.1111/j.1468-2958.1975.tb00258.x [DOI] [Google Scholar]
- Bradac JJ (2001). Theory comparison: Uncertainty reduction, problematic integration, uncertainty management, and other curious constructs. Journal of Communication, 51(3), 456–476. 10.1093/joc/51.3.456 [DOI] [Google Scholar]
- Brashers DE (2001). Communication and uncertainty management. Journal of Communication, 51(3), 477–497. 10.1111/j.1460-2466.2001.tb02892.x [DOI] [Google Scholar]
- Brashers DE (2007). A theory of communication and uncertainty management. In Whaley B & Samter W (Eds.), Explaining communication: Contemporary theories and exemplars (pp. 2001–2218). Erlbaum. [Google Scholar]
- Brashers DE, & Babrow AS (1996). Theorizing communication and health. Communication Studies, 47(3), 243–251. 10.1080/10510979609368479 [DOI] [Google Scholar]
- Brashers DE, Neidig J, Haas SM, Dobbs LK, Cardillo LW, & Russell JA (2000). Communication in the management of uncertainty: The case of persons living with HIV or AIDS. Communication Monographs, 67(1), 63–84. 10.1080/03637750009376495 [DOI] [Google Scholar]
- Campaign for Tobacco-free Kids. (2019). Electronic cigarettes and youth. Retrieved from https://www.tobaccofreekids.org/assets/factsheets/0382.pdf
- Carcioppolo N, Yang F, & Yang Q (2016). Reducing, maintaining, or escalating uncertainty? The development and validation of four uncertainty preference scales related to cancer information seeking and avoidance. Journal of Health Communication, 21(9), 979–988. 10.1080/10810730.2016.1184357 [DOI] [PubMed] [Google Scholar]
- Carpenter DM, Geryk LL, Chen AT, Nagler RH, Dieckmann NF, & Han PK (2015). Conflicting health information: A critical research need. Health Expectations, 19(6), 1173–1182. 10.1111/hex.12438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case DO, Andrews JE, Johnson JD, & Allard SL (2005). Avoiding versus seeking: The relationship of information seeking to avoidance, blunting, coping, dissonance, and related concepts. Journal of the Medical Library Association, 93(3), 353–362. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018, August9). Cancer Prevention and Control: Healthy Choices. Retrieved October 12, 2019, from https://perma.cc/ZU4T-S5RU
- Centers for Disease Control and Prevention. (2019, October11). Outbreak of lung injury associated with e-cigarette user, or vaping. Retrieved October 11, 2019, from https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html
- Cortina JM (1993). What is coefficient alpha? An examination of theory and applications. Journal of Applied Psychology, 78(1), 98–104. 10.1037/0021-9010.78.1.98 [DOI] [Google Scholar]
- Cullen KA, Gentzke AS, Sawdey MD, Chang JT, Anic GM, Wang TW, Creamer MR, Jamal A, Ambrose BK, & King BA (2019). E-Cigarette use among youth in the United States, 2019. JAMA, 322(21), 2095–2103. 10.1001/jama.2019.18387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieckmann NF, Johnson BB, Gregory R, Mayorga M, Han PK, & Slovic P (2015). Public perceptions of expert disagreement: Bias and incompetence or a complex and random world? Public Understanding of Science, 26(3), 325–338. 10.1177/0963662515603271 [DOI] [PubMed] [Google Scholar]
- Ellsberg D (1961). Risk, ambiguity, and the Savage axioms. Quarterly Journal of Economics, 75(4), 643–669. 10.2307/1884324 [DOI] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, & Lang A-G (2009). Statistical power analyses using G*power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41, 1149–1160. 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration. (2020). FDA finalizes enforcement policy on unauthorized flavored cartridge-based e-cigarettes that appeal to children, including fruit and mint. Retrieved from https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children
- Glanz K, Rimer BK, & Viswanath K (Eds). (2008). Health behavior and health education: Theory, research, and practice. John Wiley & Sons. [Google Scholar]
- Gudykunst WB (1995). The uncertainty reduction and anxiety-uncertainty reduction theories of Berger, Gudykunst, and associates. In Cushman DP & Kovacic B (Eds.), Watershed research traditions in human communication theory (pp. 67–100). State University of New York Press. [Google Scholar]
- Han PK, Klein WM, & Arora NK (2011). Varieties of uncertainty in health care: A conceptual taxonomy. Medical Decision Making, 31(6), 828–838. 10.1177/0272989X10393976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PK, Moser RP, & Klein WM (2006). Perceived ambiguity about cancer prevention recommendations: Relationship to perceptions of cancer preventability, risk, and worry. Journal of Health Communication, 11(Suppl. 1), 51–69. 10.1080/10810730600637541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Publications. [Google Scholar]
- Jackson S, O’Keefe DJ, Jacobs S, & Brashers DE (1989). Messages as replications: Toward a message‐centered design strategy. Communication Monographs, 56(4), 364–384. 10.1080/03637758909390270 [DOI] [Google Scholar]
- Jensen JD, Carcioppolo N, King AJ, Scherr CL, Jones CL, & Niederdeppe J (2014). The cancer information overload (CIO) scale: Establishing predictive and discriminant validity. Patient Education and Counseling, 94(1), 90–96. 10.1016/j.pec.2013.09.016 [DOI] [PubMed] [Google Scholar]
- Johnson-Taylor WL, Yaroch AL, Krebs-Smith SM, & Rodgers AB (2007). What can communication science tell us about promoting optimal dietary behavior? Journal of Nutrition Education and Behavior, 39(Suppl. 1), S1–S4. 10.1016/j.jneb.2006.05.011 [DOI] [PubMed] [Google Scholar]
- King BA, Gammon DG, Marynak KL, & Rogers T (2018). Electronic cigarette sales in the United States, 2013–2017. JAMA, 320(13), 1379–1380. 10.1001/jama.2018.10488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kmietowicz Z (2018). Public Health English insists e-cigarettes are 95% safer than smoking. BMJ, 363, k5429. 10.1136/bmj.k5429 [DOI] [PubMed] [Google Scholar]
- Lapinski MK, & Rimal RN (2005). An explication of social norms. Communication Theory, 15(2), 127–147. 10.1111/j.1468-2885.2005.tb00329.x [DOI] [Google Scholar]
- Lee CJ, Nagler RH, & Wang N (2018). Source-specific exposure to contradictory nutrition information: Documenting prevalence and effects on adverse cognitive and behavioral outcomes. Health Communication, 33(4), 453–461. 10.1080/10410236.2016.1278495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovelace B Jr. (2019, October 3). Vaping illness outbreak surpasses 1,000 cases, 18 deaths with no sign of slowing, CDC says. CNBC. Retrieved October 8, 2019, from https://www.cnbc.com/2019/10/03/vaping-lung-cases-surge-to-more-than-1000-with-at-least-18-deaths-cdc-says.html [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99–128. 10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillen RC, Gottlieb MA, Shaefer RMW, Winickoff JP, & Klein JD (2015). Trends in electronic cigarette use among US adults: Use is increasing in both smokers and nonsmokers. Nicotine & Tobacco Research, 17(10), 1195–1202. 10.1093/ntr/ntu213 [DOI] [PubMed] [Google Scholar]
- Mickle T (2015, November 17). E-cigarette sales rapidly lose steam. The Wall Street Journal. Retrieved from http://www.wsj.com/articles/e-cigsales-rapidly-lose-steam-1447798921 [Google Scholar]
- Nagler RH (2014). Adverse outcomes associated with media exposure to contradictory nutrition messages. Journal of Health Communication, 19(1), 24–40. 10.1080/10810730.2013.798384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. (2019). HINTS 5, Cycle 2 (2018) dataset, updated November 2018 [Data file, code book, methods report and user’s directions]. Retrieved from http://hints.cancer.gov/
- National Institute on Drug Abuse. (2019). Vaping devices (Electronic cigarettes). Retrieved from https://www.drugabuse.gov/publications/drugfacts/vaping-devices-electronic-cigarettes
- Niederdeppe J, & Levy AG (2007). Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiology and Prevention Biomarkers, 16(5), 998–1003. 10.1158/1055-9965.EPI-06-0608 [DOI] [PubMed] [Google Scholar]
- Niederdeppe J, Lee T, Robbins R, Kim H, Kresovich A, Kirshenblat D, Standridge K, Clarke CE, Jensen J, & Fowler EF (2014). Content and effects of news stories about uncertain cancer causes and preventive behaviors. Health Communication, 29(4), 332–346. 10.1080/10410236.2012.755603 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Contemporary approaches to assessing mediation in communication research. In Hayes AF, Slater MD, & Snyder LB (Eds.), The Sage sourcebook of advanced data analysis methods for communication research (pp. 13–54). Sage. [Google Scholar]
- Robehmed N (2013, November 17). E-cigarette sales surpass $1 billion as big tobacco moves in. Forbes. Retrieved from http://www.forbes.com/sites/natalierobehmed/2013/09/17/e-cigarette-sales-surpass-1-billion-as-big-tobacco-moves-in/#5e500aaa548e [Google Scholar]
- Royal College of Physicians. (2016). Nicotine without smoke: Tobacco harm reduction. Retrieved from https://www.rcplondon.ac.uk/projects/outputs/nicotine-without-smoke-tobacco-harm-reduction-0
- Sweeny K, Melnyk D, Malone W, & Shepperd JA (2010). Information avoidance: Who, what, when, and why. Review of General Psychology, 14(4), 340–353. 10.1037/a0021288 [DOI] [Google Scholar]
- Syamlal G, Jamal A, King BA, Mazurek JM (2016). Electronic cigarette use among working adults— United States, 2014. Morbidity and Mortality Weekly Report, 65(22), 557–561. 10.15585/mmwr.mm6522a1 [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS, & Osterlind SJ (2001). Using multivariate statistics. Allyn & Bacon. [Google Scholar]
- Tan AS, Lee CJ, & Bigman CA (2015). Public support for selected e-cigarette regulations and associations with overall information exposure and contradictory information exposure about e-cigarettes: Findings from a national survey of US adults. Preventive Medicine, 81, 268–274. 10.1016/j.ypmed.2015.09.009 [DOI] [PubMed] [Google Scholar]
- Truth Initiative. (2019a). Action needed: E-cigarettes. Retrieved from https://truthinitiative.org/sites/default/files/media/files/2019/11/Truth-Initiative-E-Cigarette-Fact-Sheet-Nov-11.pdf
- Truth Initiative. (2019b). E-cigarettes, Facts, stats and regulations. Retrieved from https://truthinitiative.org/research-resources/emerging-tobacco-products/e-cigarettes-facts-stats-and-regulations
- Witte K (1992). Putting the fear back into fear appeals: The extended parallel process model. Communication Monographs, 59(4), 329–349. 10.1080/03637759209376276 [DOI] [Google Scholar]
- World Health Organization. (2019). WHO study group on tobacco product regulation. Report on the scientific basis of tobacco product regulation: Seventh report of a WHO study group (WHO Technical Report Series, No. 1015). Retrieved from https://apps.who.int/iris/bitstream/handle/10665/329445/9789241210249-eng.pdf?ua=1 [PubMed]
- Yang Q, Liu J, Lochbuehler K, & Hornik R (2019). Does seeking e-cigarette information lead to vaping? Evidence from a national longitudinal survey of youth and young adults. Health Communication, 34(3), 298–305. 10.1080/10410236.2017.1407229 [DOI] [PMC free article] [PubMed] [Google Scholar]