Abstract
Background
The coronavirus disease 2019 (COVID-19) outbreak impacted the lives of worldwide people with epilepsy (PWE) in various aspects, particularly in those countries most significantly affected by this pandemic, such as Brazil. We aimed to investigate the prevalence of depressive symptoms in PWE and their correlation with epilepsy features and access to treatment.
Methods
PWE were invited to answer a cross-sectional online-based survey to assess and rate depressive symptoms using the NDDI-E during the first year of the COVID-19 pandemic and its relation to multiple lifestyles epilepsy clinical aspects.
Results
A total of 490 PWE were recruited. The prevalence of depressive symptoms during the COVID-19 pandemic was 35.3% (cutoff score > 15 on NDDI-E). The factors associated with higher NDDI-E scores were: female sex, increased seizure frequency, barriers to access to their treating physician and antiseizure medication, and unemployment. Regarding the pandemic impact on PWE healthcare, 29.2% reported restricted access to their medication, 46.1% barriers to access their physicians, 94.2% had their consultations canceled due to the pandemic, and 28.4% had seizure worsening in this period.
Conclusion
The COVID-19 pandemic affected PWE access to the healthcare system. Depressive symptoms were more severe in patients with higher seizure frequency who had difficulties obtaining proper medical care. The COVID-19 pandemic may impact the healthcare and mental wellbeing of patients with chronic diseases such as epilepsy. Nevertheless, prospective studies on epilepsy and COVID-19 are still lacking.
Keywords: COVID-19, Depression, Epilepsy, Healthcare, Antiseizure medication
1. Introduction
Epilepsy is a chronic non-communicable neurological disease that affects around 50 million people worldwide [1] and has social, psychological, and cognitive repercussions [2]. People with epilepsy (PWE) have a higher risk of associated psychiatric comorbidities [3], depression being one of the most prevalent. Depression is 3–10 times more frequent in those with epilepsy [4], [5], with an estimated overall active disorder prevalence of 23.1% and an estimated odds ratio (OR) compared with individuals without epilepsy, of 2.77 [5]. Although depressive disorder and symptoms can impact the quality of life and epilepsy outcomes, it is frequently overlooked in PWE [3], [4].
Furthermore, since late 2019, the coronavirus disease (COVID-19) pandemic has brought several challenges and restrictions to people’s lives, possibly decreasing mental health status and comprehensive care for PWE. Some studies found depression rates ranging from 39% to 47% in PWE during the pandemic [3], [6], [7], [8]. The majority of them conducted in high-income countries documented that PWEs’ rates presented higher depressive symptoms than the general population [3], [6]. Even though the authors could not establish a direct correlation, one might hypothesize that lowered healthcare access and social and economic impacts of the pandemic could be implicated [7], [8].
Brazil, and its 210 million inhabitants, is a country with profound social and economic disparities and has been significantly impacted by the COVID-19 pandemic, with high death and transmissibility rates. According to the World Health Organization (WHO), 2–3% of its population may have epilepsy [9], [10], and depression prevalence is estimated to be 5.8%, according to the World Health Organization (WHO), one of the highest in the world [11]. Considering the Brazilian populational scenario and challenges, further investigation into depression and the pandemic’s impact on PWEs is necessary. To the best of our knowledge, scarce data focus on the effects of the pandemic in Brazil [12].
Therefore, we conducted an online-based survey to assess and rate depressive symptoms among PWE in Brazil during the COVID-19 pandemic and its relation to multiple lifestyles and clinical aspects of PWE.
2. Material and methods
This is a cross-sectional study, conducted via an online survey (Google Forms) and by means of phone-based interviews with one of the researchers (RMC), from March 2020 to January 2021, during the first year of the COVID-19 pandemic in Brazil. The survey could be answered by PWE or their caregivers (for minor aged PWE or those with any neurological disability, needing assistance).
2.1. Participants
Patients were identified from secondary and tertiary epilepsy center databases and through patient associations from all Brazilian territory, from both public and private practices. Patients were reassured that their treatment was not related to this study and that healthcare follow-up would be provided despite their willingness to participate. The anonymity of the data was guaranteed, and the personal information (i.e., name) not relevant to the study was not included in the central database for analysis.
All respondents had a minimum age of 16 years, patients had a definite diagnosis of active epilepsy, under treatment with antiseizure medication (ASM), and were regularly followed up in specialized epilepsy centers.
The exclusion criteria comprised patients with functional seizures and a history of intellectual disability that would prevent them from answering the survey. We also excluded patients with a current major psychiatric disorder or with an acute deterioration unable to understand the questionnaire's nature.
2.2. Instruments
Patients were invited to participate in the study by phone and social media, with the aid of announcements through a patient organization (Associação Brasileira de Epilepsia – ABE). The nature and length of the questionnaire were primarily explained, and afterward, they received an online form. One researcher could help those who needed assistance through telephone calls or their caregivers. The questionnaire was custom designed for this study to collect demographic and clinical information:
-
1.
Demographics: age, sex, educational level, employment status (before and during the pandemic), financial circumstances, and family members;
-
2.
Epilepsy-related factors: age at epilepsy onset, duration of disease, use of ASMs;
-
3.
Routine and habits during the pandemic: changes in their daily routine, such as willingness to adhere to social isolation, face masks, and personal hygiene measures;
-
4.
Healthcare access: the status of medical appointments, contact and guidance provided by the healthcare center, and access to medical prescription and ASM itself;
-
5.
Depressive symptoms assessment: we used the Neurological Disorders Depression Inventory for Epilepsy (NDDI-E), a 6-item questionnaire that allows for rapid identification of major depressive symptoms in epilepsy. The NDDI-E is a 4‐point Likert assessment, ranging from 1 to 4, and its maximum score is 24. Scores higher than 15 indicate symptoms that are compatible with major depressive disorder [13].
2.3. Statistical analysis
Statistical analysis was performed using IBM SPSS® Statistics Grad Pack software premium version 27.0. Variables were tested for normality using the Kolmogorov–Smirnov test. Subsequent non-parametric tests Spearman's correlation and Mann–Whitney U were applied accordingly to compare NDDI-E means between two groups. Variables with a normal distribution are shown as the mean ± standard deviation (SD; minimum–maximum), while variables with a non-normal distribution were reported as the median with an interquartile range (IQR). To identify factors associated with depression the authors first performed univariate analyses, followed by a multiple linear regression with the five factors showing a trend of association (p < 0.20) to investigate the independent predictors of depression that were statistically significant.
2.4. Ethics
This study was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki, 2014). The institutional review boards and ethics committees of each site approved the study protocol (CEPSH/UFSC Protocol No. 4.059.818 and CEP/FMUSP 15093). All subjects signed an informed consent form and voluntarily agreed to participate.
3. Results
A total of 490 subjects were assessed during the study. People from all Brazilian regional divisions answered the questionnaire (Fig. 1 ). No response was obtained from only three (from 26 + 1 federal district) Brazilian states. Many of the respondents were from São Paulo state with 261 (53.8%) answers, followed by the states of Santa Catarina 41 (8.4%), Rio de Janeiro 25 (5.1%), and Rio Grande do Sul 24 (4.5%). Most individuals [351 (71.6%)] were women, and their mean age was 37.3 ± 13.33 (1–89) years. Overall, individuals had an average of 15.8 ± 13.20 (0–66) years of epilepsy.
Fig. 1.
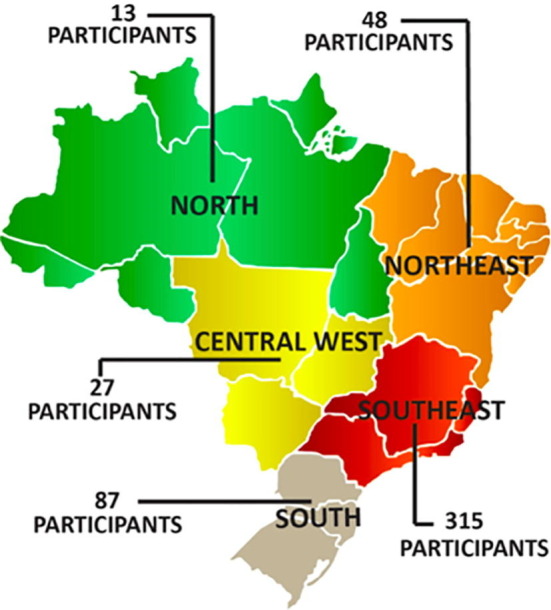
Brazilian respondents from all its geographical regions (Brazil is the fifth largest country globally, with a total area of 8 million km2 and 210 million inhabitants).
Most of the patients answered the questionnaire themselves [320 (65.3%)], and those who were unable to answer had it done by their caregiver on the patient’s behalf. Regarding education, 219 (44.7%) of the subjects had university degrees. Individuals’ demographic data are detailed in Table 1 .
Table 1.
Respondents’ demographics and clinical characteristics.
| Characteristics | Total (N = 490) |
|---|---|
| Age, years a | 37.3 ± 13.33 (1–89) |
| Sex, n (%) | 351 (71.6) Women |
| Subjects, n (%) | Patients 320 (65.3%) |
| Family and/or caregivers 170 (34.7%) | |
| Educational status, n (%) | No formal education 19 (3.9%) |
| Elementary school 81 (16.5%) | |
| High school 171 (34.9%) | |
| Graduate 138 (28.2%) | |
| Post-graduate 81 (16.5%) | |
| Disease duration, years a | 15.8 ± 13.20 (0–66) |
aMean ± SD (minimum–maximum).
Regarding epilepsy, 99% (485) of the respondents were on ASM, and 10.6% (52) were also receiving the ketogenic diet. When asked about the effect of the pandemic on their seizure frequency, 55.7% of respondents reported changes in frequency along the period – most of them noticed increased seizures [139 (28.4%)].
Although most cities were in lockdown, subjects reported they did not have difficulties obtaining their ASM [347 (70.8%)]. The 29.2% (143) who had such difficulties reported, in open-answers, that their significant obstacles were: no access to medical prescription (65 subjects), medication availability in pharmacies and drug stores (25 subjects), no financial resources to buy the medication (25 subjects), and 14 could not access government-subsidized drugs. Individual epilepsy data are detailed in Table 2 .
Table 2.
Epilepsy characteristics.
| Epilepsy versus Pandemic | Total (N = 490) |
|---|---|
| Did pandemics change your seizure frequency? | No 330 (67.4%) |
| Yes 160 (32,6%) | |
| 139 (28.3%) increased seizures | |
| 21 (4.2%) reduced seizures | |
| Epilepsy treatment | Pharmacological 485 (99%) |
| Ketogenic diet 52 (10.6%) | |
| Handmade cannabidiol or DBS 14 (2.9%) | |
| Epilepsy surgery 5 (1%) | |
| Did you have any difficulties buying/obtaining your medication during pandemics? | No 347 (70.8%) |
| Yes 143 (29.2%) | |
| Did you have any difficulties contacting your physician? | No 262 (53.4%) |
| Yes 226 (46.1%) | |
| Did you keep in touch with your doctor during the pandemic? | No 262 (53.4%) |
| Yes 226 (46.1%) |
DBS = deep brain stimulation.
Nearly half, 46.1% (226), of the individuals had difficulties contacting their physicians during the pandemic. Four hundred and fifty-eight (93.5%) patients used the internet or their smartphones to access doctors, and 6.1% (30) contacted by telephone.
Regarding difficulties to access doctors, 94.2% (213) reported having their appointments canceled; 6.5% (17) chose not to go to their appointment because of fear of contamination by Sars-Cov-2, and 5% (13) lived in a different city and did not have transportation to their medical appointment. Ten (2.7%) patients answered that the healthcare provider in charge was on the risk group (advanced age or comorbidities) and could not meet their patients personally, and five did not have financial conditions to pay for medical consultation.
As to occupation before the pandemic, only 38.3% (188) individuals were employed. The unemployed group (302 individuals) included several characteristics: 70.8% (143/302) were already unemployed before the pandemic, 30.7% (62/302) were retired, 12.9% (26/302) received government aid, and 11.9% (24/302) alleged they sometimes have informal or temporary jobs (not subject to Brazilian national labor legislation, income taxation, social protection, or entitlement to certain employment benefit). Twenty-two were students, and 25 have never been employed or sought employment. Due to the pandemic, only 5.5% (27) experienced job loss.
The self-assessed NDDI-E was performed only among patients with epilepsy (N = 320). The NDDI-E median score was 12.0 [interquartile range (IQR) = 8–18]. According to the Mann–Whitney test for independent samples, NDDI-E scores were found to be significantly higher among women (p < 0.001), in those patients who had increased seizure frequency (p = 0.002), who had difficulty in contacting their neurologist (p = 0.031), those who had some impediment to buy or maintain antiseizure medications (p < 0.001) during the pandemic, and those who were unemployed before the pandemic (p = 0.028).
Multiple linear regression [F(5,314) = 9.622; p < 0,001; R 2 = 0.346], confirmed that NDDI-E could be predicted by four variables, gender (women) (β = 0.236; t = 4.488; p < 0.001), any impediment to buy or maintain antiseizure medications (β = 0.184; t = 3.379; p < 0.001), increase on seizure frequency (β = 0.143; t = 2.746; p = 0.006) and unemployment (β = −0.105; t = −2.005; p = 0.046). The only variable not significant in the final model was difficulty in contacting the neurologist (β = 0.061; t = 1.137; p = 0.256).
According to Mann–Whitney test for independent samples, NDDI-E scores were found to be significantly higher among Brazilian Southeastern population (p < 0.001). The regions South (p = 0.051), Central-West (p = 0.589), Northeast (p = 0.790), and North results (p = 0.149) were not significantly different (Table 3. ).
Table 3.
Factors leading to depression according to NDDI-E (N = 320).
| Ua | NDDI-E (N) medianb | p | |
|---|---|---|---|
| NDDI and changes in seizure frequency | 9254.0 | no change (N = 208) 12.0 | 0.002* |
| changed (N = 112) 14.5 | |||
| NDDI and difficulties to access anti-seizure medication | 6391.0 | no difficulties (N = 240) 12.0 | <0.001* |
| had difficulties (N = 80) 16.0 | |||
| NDDI and impaired access to usual physician | 1084.0 | no difficulties (N = 180) 12.0 | 0.031* |
| had difficulties (N = 140) 14.0 | |||
| NDDI and sex | 5607.5 | men (N = 75) 9.0 | <0.001* |
| women (N = 245) 14.0 | |||
| NDDI and job loss during the pandemic | 1963.0 | lost job (N = 16) 17.0 | 0.192 |
| kept job (N = 304) 12.0 | |||
| NDDI and unemployment before the pandemic | 10719.0 | employed (N = 136) 12.0 | 0.028* |
| unemployed (N = 184) 13.5 |
aMann–Whitney’s U.
b(N = number of subjects) Median.
NDDI-E = Neurological Disorders Depression Inventory for Epilepsy.
*p < 0.05.
4. Discussion
Brazil is a vast country with a complex social, political, and economic situation. The COVID-19 pandemic outbreak has further affected not only a lifestyle but also access to the healthcare system. Social isolation measures contain the virus from spread but prevented patients from accessing their physicians and health services. Telemedicine was quickly implemented, medication delivery systems were affected, and ASM's supply maintenance is of great concern. The summation of these circumstances imposed new challenges to epilepsy care regarding seizure control and mental health, a component of great importance for treatment outcome [4].
Our results showed that the median NDDI-E score was set below the cutoff point for major depressive disorder [13] (median = 12; IQR 8–18), but 113 (35.3%) patients presented a score higher than 15. We could not assess whether the pandemic increased these rates due to the timing of data collection, although a Chinese longitudinal study has suggested increased rates of depression during the period of the epidemic, compared with the period before and after the outbreak [8]. Nevertheless, these data are essential to delineate better care provisions for patients and understand which factors may influence mental health at this moment. Current literature has indicated that, during the pandemic, PWE had higher levels of distress than controls [14] and that depression prevalence seems to be higher in PWE than in general population [3], indicating more significant mental health impacts on PWE. Factors such as barriers to healthcare access and social and economic impacts of the pandemic could all be stressing factors [7].
Indeed, our analysis showed that mean NDDI-E scores were significantly higher for those who had difficulties accessing their physicians and those who could not obtain ASM. In consonance, Van Hees et al. showed higher odds for depression in those with impaired ASM access [3]. Not being able to access healthcare or medication could potentially generate insecurity, especially when fear of seizure worsening walks alongside a pandemic. The healthcare team is directly involved in these patients' mental well-being by identifying potential risks, treating them accordingly, and providing security and information. The significant influx and obsessive pursuit of information on the pandemic (infodemics) were pointed out as a risk for severe psychological distress among PWE [14]; when so-called fake news is considered, the population may be even more vulnerable. Therefore, regular accompaniment by the healthcare team may be crucial to maintain PWE and their caregivers calm, supported, and appropriately informed. Additionally, physicians also play an essential role in ASM access since they issue prescriptions and can change the medication if needed due to unavailability, costs, or maladaptation to the medication.
Seizure frequency was altered in 55.7% of individuals, which increased to 28.4% of respondents. Several studies have reported an increase in seizures during this pandemic [6], [7], [12], [15], [16], pointing to factors such as income reduction, insomnia, pharmacoresistant epilepsy [16], difficulties to obtain ASM, impaired access to healthcare, and emotional stress [6]. Our results indeed indicate that, in addition to poor access to healthcare and ASM, median NDDI-E scores were significantly higher than those who experienced an exacerbation of seizures amidst the pandemic. Several factors could be related to it; a possibility is that the insecurity caused by the pandemic and increased social isolation could worsen mental health and lead to seizure exacerbation, as depression may facilitate the development of epileptic activity [5]. Conversely, seizure exacerbation due to other factors, such as no access to proper treatment, could also affect the development of depression, as already pointed by literature [5]. Many other factors within this pandemic, alongside previous aspects of the disease, may be involved, and further studies and deepened analysis are needed to comprehend causality [12].
In the face of these results, healthcare assistance needs to continue during the pandemic to guarantee seizure control and mental well-being. Several studies have suggested telemedicine as one solution to maintaining contact between healthcare teams, PWE, and caregivers [7], [12], [15], [16], [17], [18]. Accessible technologies, such as WhatsApp – an online messaging platform – have had high acceptance rates for this purpose [18], and telephone calls have also been used [7], [16], [18]. Teleconferences are also crucial for the physicians' assessment, and the visual contact could help reduce patients' anxiety and concerns [16]. Indeed, implementing such interventions needs to contemplate regional challenges and patients' accessibility to the internet or phones. Brazil's national health system (SUS - Sistema Único de Saúde or Unified Health System) is free and has an established telehealth program in the early 2000s [19]. However, a significant portion of patients is socially and economically vulnerable. Thus solutions, as mentioned earlier, may not be feasible for most. Indeed, 44.7% of our respondents had at least a university degree, which an online survey could assess. In the face of these challenges, customization of healthcare delivery, education of patients on the use of technology, and provision of devices and internet support could all be measures that aid in telemedicine, preventing healthcare accessibility issues and COVID-19 spread [17], [18]. Telehealth could assist in maintaining access to healthcare professionals, follow-ups, provide online prescriptions and information, and, most importantly, detect mental health issues as depression and aid patients and caregivers to cope with fears and challenges imposed by the pandemic.
This study has some limitations that must be addressed. First, the use of online self-assessed surveys has inherent bias limitations. For a significant portion of respondents, we could not assure epilepsy diagnosis, as preconized by the ILAE (International League Against Epilepsy) [2], nor that the entire survey was indeed fully answered by the PWE or caregiver. Additionally, this is a cross-sectional study. Therefore, we could not assess causality between challenges imposed by the pandemic and depression. We did not have the NDDI-E scores from each patient before the installation of the pandemic. Accordingly, we could not attest to how and whether the event has changed these scores. At last, 44.7% of our respondents had university degrees, an educational status that may represent those with internet access in Brazil, but may not be generalizable to the Brazilian population in all its territories. Also, we do not have a control group for comparison of the impact of COVID-19 on PWE versus the general population.
5. Conclusion
The healthcare and mental wellbeing of patients with chronic diseases such as epilepsy seems to be more impacted by the COVID-19 pandemic. To reduce this psychosocial impact, ensuring strategies for the continuous access to medical treatment is essential, for example, telemedicine, uninterrupted delivery of ASM, financial aid, and delivery of evidence-based information.
6. Declarations of interest
None.
Acknowledgments
The authors: KL holds a CNPq (Brazilian Council for Scientific and Technologic Development, Brazil) PQ2 Research Fellowship (Process No. 313205/2020-5), KL is supported by PRONEM (Programa de Apoio a Nucleos Emergentes – KETODIET – SC Project – Process No 2020TR736) from FAPESC/CNPq, Santa Catarina Brazil.
References
- 1.Who.int. 2021. Epilepsy, https://www.who.int/news-room/fact-sheets/detail/epilepsy/; 2019 [accessed 11 February 2021].
- 2.Fisher R.S., Acevedo C., Arzimanoglou A., Bogacz A., Cross J.H., Elger C.E., et al. ILAE Official Report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475–482. doi: 10.1111/epi.12550. [DOI] [PubMed] [Google Scholar]
- 3.Van Hees S, Siewe Fodjo JN, Wijtvliet V, Van den Bergh R, Faria de Moura Villela E, da Silva CF, et al. Access to healthcare and prevalence of anxiety and depression in persons with epilepsy during the COVID-19 pandemic: a multicountry online survey. Epilepsy Behav 2020;112:107350. 10.1016/j.yebeh.2020.107350. [DOI] [PMC free article] [PubMed]
- 4.Josephson C.B., Jetté N. Psychiatric comorbidities in epilepsy. Int Rev Psychiatry. 2017;29:409–424. doi: 10.1080/09540261.2017.1302412. [DOI] [PubMed] [Google Scholar]
- 5.Fiest K.M., Dykeman J., Patten S.B., Wiebe S., Kaplan G.G., Maxwell C.J., et al. Depression in epilepsy: a systematic review and meta-analysis. Neurology. 2013;80:590–599. doi: 10.1212/WNL.0b013e31827b1ae0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Millevert C, Van Hees S, Siewe Fodjo JN, Wijtvliet V, Faria de Moura Villela E, Rosso B, et al. Impact of COVID-19 on the lives and psychosocial well-being of persons with epilepsy during the third trimester of the pandemic: Results from an international, online survey. Epilepsy Behav 2021;116:107800. 10.1016/j.yebeh.2021.107800. [DOI] [PMC free article] [PubMed]
- 7.Conde Blanco E., Manzanares I., Centeno M., Khawaja M., Betrán O., Donaire A., et al. Epilepsy and lockdown: a survey of patients normally attending a Spanish centre. Acta Neurol Scand. 2021;143:206–209. doi: 10.1111/ane.13354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun L, Mo Q, Sun H, Niu Y, Si Y. Depression in patients with epilepsy during the COVID-19 pandemic based on longitudinal self-reporting. Epileptic Disord 2021. [Epub ahead of print]. 10.1684/epd.2021.1263. [DOI] [PMC free article] [PubMed]
- 9.Neto J.G., Marchetti R.L. Epidemiologic aspects and relevance of mental disorders associated with epilepsy. Rev Bras Psiquiatr. 2005;27:323–328. doi: 10.1590/s1516-44462005000400013. [DOI] [PubMed] [Google Scholar]
- 10.Fiest K.M., Sauro K.M., Wiebe S., Patten S.B., Kwon C.-S., Dykeman J., et al. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017:296–303. doi: 10.1212/WNL.0000000000003509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Estimated population-based prevalence of depression. Who.int. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/estimated-population-based-prevalence-of-depression/; 2021 [accessed 12 February 2021].
- 12.Kuroda N. Epilepsy and COVID-19: updated evidence and narrative review. Epilepsy Behav. 2021;116 doi: 10.1016/j.yebeh.2021.107785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilliam F.G., Barry J.J., Hermann B.P., Meador K.J., Vahle V., Kanner A.M. Rapid detection of major depression in epilepsy: a multicentre study. Lancet Neurol. 2006;5:399–405. doi: 10.1016/S1474-4422(06)70415-X. [DOI] [PubMed] [Google Scholar]
- 14.Hao X., Zhou D., Li Z., Zeng G., Hao N., Li E., et al. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia. 2020;61:1166–1173. doi: 10.1111/epi.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Assenza G., Lanzone J., Brigo F., Coppola A., Di Gennaro G., Di Lazzaro V., et al. Epilepsy care in the time of COVID-19 pandemic in Italy: risk factors for seizure worsening. Front Neurol. 2020;11:1–11. doi: 10.3389/fneur.2020.00737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fonseca E., Quintana M., Lallana S., Luis Restrepo J., Abraira L., Santamarina E., et al. Epilepsy in time of COVID-19: a survey-based study. Acta Neurol Scand. 2020;142:545–554. doi: 10.1111/ane.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Subotic A., Pricop D.F., Josephson C.B., Patten S.B., Smith E.E., Roach P. Examining the impacts of the COVID-19 pandemic on the well-being and virtual care of patients with epilepsy. Epilepsy Behav. 2020;113 doi: 10.1016/j.yebeh.2020.107599. [DOI] [PubMed] [Google Scholar]
- 18.Semprino M., Fasulo L., Fortini S., Martorell Molina C.I., González L., Ramos P.A., et al. Telemedicine, drug-resistant epilepsy, and ketogenic dietary therapies: a patient survey of a pediatric remote-care program during the COVID-19 pandemic. Epilepsy Behav. 2020;112 doi: 10.1016/j.yebeh.2020.107493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CONASS-Conselho Nacional de Secretários de Saúde. Para Entender A Gestão Do SUS. 20th ed. Brasília: CONASS; 2011, p. 79 - 81.


