Abstract
Background
The outbreak of COVID-19 and the physical isolation measures taken by the governments to reduce its propagation might have negative psychological consequences on the population. In this study, we aimed to explore, for the first time, how mental health status fluctuated along the weeks of the emergency state in Portugal, and to identify which factors may shape these changes in mental health outcomes.
Methods
To this end, we conducted an online survey to evaluate demographic, lifestyle and mental health variables (DASS-21 and quality of life) in the Portuguese population at three different time-points. 748 participants (mean age = 39.52, % females = 79.95) provided data at all time-points.
Results
We observed that depression, anxiety and stress symptoms seemed to improve as the weeks passed during the state of emergency, while the perception of quality of life and sleep got worse. In particular, being female, younger, actively working, and extroverted appear to be protective factors of mental health adaptability during this particular period. On the contrary, having a psychiatric diagnosis or physical illness, and higher neuroticism seem to be risk factors for mental health worsening.
Limitations
The lack of a more diverse sample could limit the generalizability of our results, and other factors that were not considered in our analysis might also have a significant impact on mental health.
Conclusions
Our results provide relevant and novel insights about the course of mental health changes and its predictors during the outbreak of COVID-19, which may help identify potential vulnerability groups.
Keywords: Mental health, Quality of life, Resilience, Isolation, COVID-19, Longitudinal
1. Introduction
The outbreak of the coronavirus disease 2019 (COVID-19) has originated a worldwide crisis with dramatic consequences for health, economy and society (Holmes et al., 2020). To reduce the propagation of the disease, most governments initially imposed a period of compulsory confinement, where the movements and contact between people were severely restricted. The Portuguese government declared the emergency state, including compulsory confinement and social distancing measures, on the 19th of March. While these measures play a critical role for the promotion of public health safety, they also challenge our ability to adapt. In such an unprecedent scenario, people are restricted of maintaining contact with loved ones, their daily routines are dramatically changed, and their working activities need profound adjustments (Brooks et al., 2020). Moreover, with the closure or restriction of business activities, several people face the risk of unemployment, further intensifying the experience of negative feelings (Rossi et al., 2020). These factors together with the uncertainty, distress and fear related to the progression of the disease are likely to increase the psychological burden, including the appearance of symptoms of anxiety (James Rubin and Wessely, 2020), stress or depression (Brooks et al., 2020; Holmes et al., 2020).
Studies from previous outbreaks, as well as initial COVID-19 research, highlight that the psychological impact of compulsory confinement is substantial and may persist in the long-term across different populations (Brooks et al., 2020; Cao et al., 2020; Holmes et al., 2020; Paulino et al., 2020; Wang et al., 2020). Despite this, the adverse mental health effects of the pandemic do not have an equal impact on everyone, and it becomes of relevance to identify which groups present higher vulnerability (Ferreira dos Santos et al., 2020). In this line, recent studies within the Portuguese population during the COVID-19 outbreak showed that mental health status may depend on several protective and risk factors (Antunes et al., 2020; Moreira et al., 2021), and pointed to females, younger adults, and people not doing exercise, among others, as potential vulnerability groups. Moreover, psychological symptoms could be amplified by pre-existing depressive and anxiety disorders (Zhu et al., 2020), so people with previous psychiatric diagnosis deserve special attention.
One limitation of most previous research is its cross-sectional design. Understanding the shifts in the population's mental health status during the pandemic, and the factors that may be influencing these changes, is relevant to understanding public responses to the on-going pandemic, planning for subsequent management of COVID-19, and preparing for future pandemics. In this line, some potential beneficial factors have been identified at the cross-sectional level, and recommendations have been proposed by the World Health Organization (2020). Despite this, due to the scarcity of longitudinal studies, it remains to be explored whether these same factors are also predictors of changes in mental health status, and thus predictors of adaptability and resilience.
To answer this question, we conducted the first longitudinal investigation in Portugal exploring mental health status along the emergency state. Our aims were (i) to explore how mental health status fluctuates along the weeks of the emergency state; and (ii) to gain insights into the influence of various sociodemographic and clinical factors that may shape changes in mental health outcomes across the course of the pandemic. To the best of our knowledge, this is the first study longitudinally exploring the psychological impact of compulsory confinement due to COVID-19 in the Portuguese population, with a thorough characterization of potential protector and risk factors.
2. Methods
2.1. Procedure
An online survey using Google Forms was applied to the general adult Portuguese population from the 23rd of March to the 31st of May 2020, starting less than one week after the state of emergency was declared by the Portuguese Government (19th of March), which included lockdown and compulsory confinement. Social media and national newspapers were used to advertise and recruit possible volunteers. Based on previous studies from the team and our communication capability, we were aiming to reach a sample between 1500 and 2000 participants. Since the recruitment was made mainly through online sources (and online access to the Google Forms was a requirement to participate), the representativity of the study sample to the whole adult Portuguese population was thus limited. Electronic informed consent was obtained from all participants. Ethical approval was obtained from the Ethical Committee for Life Sciences of the University of Minho (Braga, Portugal), following the recommendations of the Declaration of Helsinki.
The survey assessed sociodemographic information (age, sex, employment status), data about the living conditions (the existence of green space and balcony, and the presence of children, teenagers, or elders in the current housing), and clinical data (presence of psychiatric or physical diagnoses, and weekly substance consumption – alcohol, tobacco, cannabis, or other). Data regarding the amount of time spent daily doing exercise, and looking for COVID-19-related information, was also collected.
Additionally, the survey measured depression, anxiety, and stress levels with the Depression, Anxiety and Stress Scale (DASS-21; Lovibond and Lovibond, 1995; Pais-Ribeiro et al., 2004). The DASS-21 scale evaluates symptoms of depression, anxiety, and stress experienced in the prior week, on a four-point scale, ranging from 0 (“Did not apply to me at all”), to 3 (“Applied to me very much, or most of the time”). Participants were also asked about their quality of life self-evaluation, satisfaction, and quality of sleep using a 5-point Likert scale ranging from “Very bad/Very unsatisfied” to “Very good/Very satisfied”. These measures were collected at a first time-point (that will be referred as Week 0 from now on), after 4 weeks, and after 8 weeks. The Week 0 questionnaire was collected between the 23rd of March and the 5th of April. The last time-point was collected after the state of emergency ended (2nd of May 2020), with the lockdown and confinement measures beginning to be slowly removed. Finally, in order to evaluate personality differences, participants also completed the NEO Five-Factor Inventory (NEO-FFI; Bertoquini and Pais-ribeiro, 2006; Costa and McCrae, 1992). The five personality factors are represented with the five subscales of the questionnaire: neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness.
2.2. Statistical analyses
The statistical analyses were conducted with the JASP software (version 0.13.0.0; JASP Team, University of Amsterdam, the Netherlands). P values under 0.05 were considered statistically significant.
Normality of continuous variables was assessed with Shapiro-Wilk's test. When data were non-parametric, the Friedman test was used to test longitudinal changes in the DASS-21 subscales and quality of life (QoL) measures along the three time-points, and effect sizes were reported using Kendall's W (0.2 small effect, 0.5 moderate effect, >=0.8 strong effect). Conover's post-hoc test with Holm correction was used to check the differences between every two time-points.
Next, multiple linear regression models were used to study which variables predicted changes from Week 0 to the last time-point in the DASS-21 subscales and the QoL variables. To this end, we computed the subtraction between these two time-points for the different variables of interest (dependent variables). In order to always get a positive predictive value as an indicative of improvement and a negative predictive value as an indicative of worsening (for ease of interpretation), and taking into account that for the DASS-21 subscales the higher the score the worse, but for the QoL measures the higher the better, the data from the last time-point was subtracted from the data at Week 0 in the DASS-21 subscales, and the other way around for the QoL measures. Next, since we wanted to remove the confounding effect of potential differences at baseline, for each of our computed subtracted variables of interest the effect of the variable at Week 0 was regressed out. Thus, the dependent variables included in the models were the subtracted variables residualized by their baseline scores. Finally, the following predictors were tested in multivariate models for each of the dependent variables: age, sex (male – 0; female - 1), employment status (unemployed – 0; studying – 1; working – 2), house balcony and/or terrace (no – 0; yes - 1), living with children (no – 0; yes - 1), living with teenagers (no – 0; yes - 1), living with elderly (no – 0; yes - 1), having a diagnosis of a psychiatric disorder (no – 0; yes - 1), having a diagnosis of a physical disorder (no – 0; yes - 1), consumption of substances several times a week (no – 0; yes – 1), daily amount of time dedicated to sport (less than 1 h – 0; more than 1 h – 1), daily amount of time looking for COVID-19 related news (less than 1 h – 0; more than 1 h – 1), and the NEO-FFI subscales. Normality, linearity, and homoscedasticity assumptions were visually checked with Q-Q plots and residuals vs. predicted plots. Multicollinearity was examined with the tolerance and variance inflation factor (VIF) values.
3. Results
We obtained answers from 1743 participants at Week 0, but due to dropout the final sample size included for the analyses was of 748. Table 1 presents the descriptive statistics of the main variables for the final sample used, while Supplementary Table 1 shows a comparison of these variables between the dropout sample and the final sample.
Table 1.
Descriptive statistics of the dependent and independent variables used in the different models.
| Variable | Week 0 | Week 4 | Week 8 |
|---|---|---|---|
| DASS-21, Mean (SD) | Median (IQR) | |||
| Depression | 3.52 (3.87) | 2 (4) | 3.49 (4.3) | 2 (4) | 3.29 (4.43) | 1.5 (4.25) |
| Anxiety | 2.49 (3.23) | 1 (4) | 1.88 (2.95) | 1 (3) | 1.8 (3.18) | 0 (2) |
| Stress | 5.94 (4.3) | 5 (5) | 5.64 (4.61) | 5 (6) | 5.26 (4.88) | 4 (6) |
| QoL, Mean (SD) | Median (IQR) | |||
| Self-Evaluation | 3.04 (0.67) | 3 (0) | 2.82 (0.68) | 3 (1) | 2.83 (0.67) | 3 (1) |
| Satisfaction | 2.99 (0.88) | 3 (1) | 2.83 (0.85) | 3 (0) | 2.84 (0.81) | 3 (0) |
| Quality of Sleep | 2.46 (1.02) | 3 (1) | 2.31 (0.95) | 2 (1) | 2.36 (0.96) | 3 (1) |
| Age, Mean (SD) | Median (IQR) | 39.52 (12.47) | 38 (18) | - | - |
| Sex, N (%) | |||
| Female | 598 (79.95) | - | - |
| Male | 150 (20.05) | - | |
| Employment Status, N (%) | |||
| Unemployed | 148 (19.79) | - | - |
| Studying | 74 (9.89) | ||
| Working | 526 (70.32) | ||
| Balcony/Terrace, N (%) | |||
| No | 87 (11.63) | - | - |
| Yes | 661 (88.37) | ||
| Living with Children, N (%) | |||
| No | 579 (77.41) | - | - |
| Yes | 169 (22.59) | ||
| Living with Teenagers, N (%) | |||
| No | 657 (87.83) | - | - |
| Yes | 91 (12.17) | ||
| Living with Elderly, N (%) | |||
| No | 631 (84.36) | - | - |
| Yes | 117 (15.64) | ||
| Psychiatric Disorder, N (%) | |||
| No | 655 (87.57) | - | - |
| Yes | 93 (12.43) | ||
| Physical Disorder, N (%) | |||
| No | 472 (63.1) | - | - |
| Yes | 276 (36.9) | ||
| Substances, N (%) | |||
| No | 514 (68.72) | - | - |
| Yes | 234 (31.28) | ||
| Sport Time, N (%) | |||
| No | 621 (83.02) | - | - |
| Yes | 127 (16.98) | ||
| COVID-19 Time, N (%) | |||
| No | 447 (59.76) | - | - |
| Yes | 301 (40.24) | ||
| NEO-FFI, Mean (SD) | Median (IQR) | |||
| Neuroticism | 7.6 (3.33) | 8 (5) | - | - |
| Extraversion | 8.85 (2.8) | 9 (4) | ||
| Openness to Experience | 10.54 (3.55) | 11 (5) | ||
| Agreeableness | 10.55 (2.98) | 11 (4) | ||
| Conscientiousness | 11.64 (2.6) | 12 (3) | ||
DASS-21, Depression, Anxiety and Stress Scale; SD, Standard Deviation; IQR, Interquartile Range; QoL, Quality of Life; NEO-FFI, NEO Five-Factor Inventory.
3.1. Repeated-measures analyses
The Shapiro-Wilk test was statistically significant for all 6 dependent variables (the quality of life variables were negatively skewed, while the DASS-21 subscales were positively skewed, which can be expected in a general non-clinical population). Thus, the non-parametric Friedman test was used for all variables, which proven to be statistically significant for all of them.
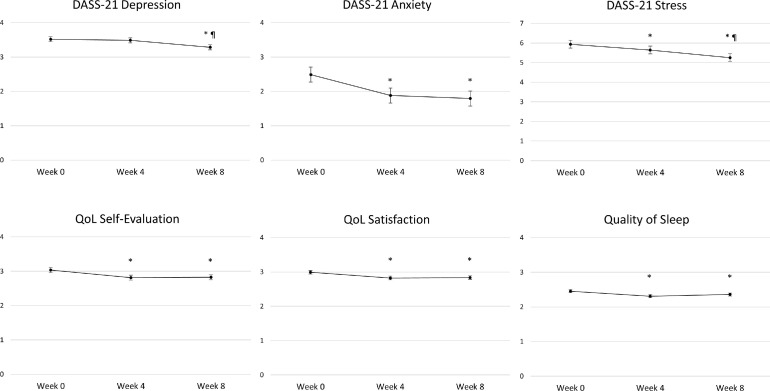
The DASS-21 Depression subscale resulted in a χ2 F(2)=23.19, p < .001, Kendall's W = 0.793, and presented a decrease across the weeks, more pronounced between Weeks 4 and 8 than between Weeks 0 and 4, as it is shown with Conover's post-hoc tests (Week 0 vs. Week 4: T-Stat=1.87, pholm=.062; Week 0 vs. Week 8: T-Stat=4.78, pholm<.001; Week 4 vs. Week 8: T-Stat=2.91, pholm=.007), and in Fig. 1 . The DASS-21 Anxiety subscale had a χ2 F(2)=97.04, p < .001, Kendall's W = 0.745, and also showed a decrease, in this case more pronounced between Weeks 0 and 4 (Week 0 vs. Week 4: T-Stat=7.45, pholm<.001; Week 0 vs. Week 8: T-Stat=9.31, pholm<.001; Week 4 vs. Week 8: T-Stat=1.86, pholm=.063), Fig. 1. The DASS-21 Stress subscale resulted in a χ2 F(2)=35.11, p < .001, Kendall's W=0.788, and showed the more consistent decrease across the weeks (Week 0 vs. Week 4: T-Stat=2.15, pholm=.032; Week 0 vs. Week 8: T-Stat=5.86, pholm<.001; Week 4 vs. Week 8: T-Stat=3.71, pholm<.001), Fig. 1.
Fig. 1.
Plots representing the mean values and standard error of the variables of interest on the three time-points studied. *Significant difference in the Conover's post-hoc test in comparison to Week 0. ¶Significant difference in the Conover's post-hoc test in comparison to Week 4. DASS-21: Depression, Anxiety and Stress Scale; QoL: Quality of Life.
Regarding the QoL variables, QoL self-evaluation had a χ2 F(2)=140.4, p < .001, Kendall's W = 0.749, and presented an initial decrease that was later maintained between Weeks 4 and 8 (Week 0 vs. Week 4: T-Stat=10.46, pholm<.001; Week 0 vs. Week8: T-Stat=10.08, pholm<.001; Week 4 vs. Week 8: T-Stat=0.38, pholm=.705), Fig. 1. QoL satisfaction resulted in a χ2 F(2)=82.02, p < .001, Kendall's W = 0.765, and showed a similar pattern than QoL self-evaluation (Week 0 vs. Week 4: T-Stat=7.74, pholm<.001; Week 0 vs. Week 8: T-Stat=7.96, pholm<.001; Week 4 vs. Week 8: T-Stat=0.22, pholm=.827), Fig. 1. Finally, quality of sleep resulted in a χ2 F(2)=23.5, p < .001, Kendall's W = 0.796, and presented an initial decrease with a later slight increase which did not reach significance (Week 0 vs. Week 4: T-Stat=4.73, pholm<.001; Week 0 vs. Week 8: T-Stat=3.3, pholm=.002; Week 4 vs. Week 8: T-Stat=1.44, pholm=.151), Fig. 1.
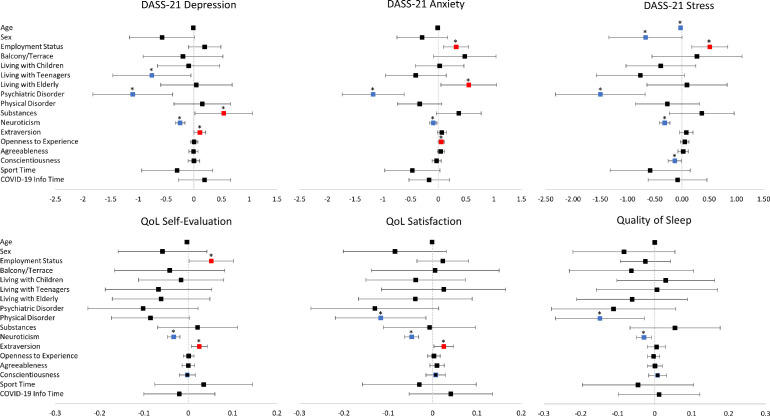
3.2. Multiple regression analyses
All multiple regression models were statistically significant. For the DASS-21 Depression subscale change (F(17,730)=6.53; p < .001; R2 = 0.132), consumption of substances and higher extraversion scores were significant positive predictors, while living with teenagers, having a psychiatric disorder diagnosis, and higher neuroticism scores were significant negative predictors. Regarding the DASS-21 Anxiety subscale change (F(17,730)=5.12; p < .001; R2 = 0.106), being working, living with elderly, and higher openness to experience scores were significant positive predictors, while having a psychiatric disorder diagnosis and higher neuroticism scores were significant negative predictors. Regarding improvement in the DASS-21 Stress subscale (F(17,730)=7.16; p < .001; R2 = 0.143), being working was a significant positive predictor, while being older, male, having a psychiatric disorder diagnosis, and higher neuroticism and conscientiousness scores were significant negative predictors.
With regards to the QoL variables, for QoL self-evaluation improvement (F(17,730)=5.8; p < .001; R2 = 0.119), being working and higher extraversion scores were significant positive predictors, while higher neuroticism was a negative predictor. Regarding QoL satisfaction change (F(17,730)=6.9; p < .001; R2 = 0.138), higher extraversion scores was a significant positive predictor, while having a physical disorder diagnosis and higher neuroticism scores were significant negative predictors. Finally, for quality of sleep (F(17,730)=1.98; p = .01; R2 = 0.044) there were no positive predictors, and having a physical disorder diagnosis and higher neuroticism were significant negative predictors.
The unstandardized beta and the standard error for the significant predictors of each model are presented in Table 2 , and a representation of the models can be found in Fig. 2 . The tolerance and VIF values for all models pointed to an absence of multicollinearity, and the Q-Q plots and residuals vs. predicted plots suggested that the assumptions were not violated. Finally, the interaction of these significant factors across time for the different dependent variables is shown in Supplementary Figure 1, for visualization purposes and ease of interpretation.
Table 2.
Statistical results for the significant predictors of the different multiple linear regression models.
| Dependent variable | Predictors | B ± SE B | p-value |
|---|---|---|---|
| DASS-21 depression subscale | Substances | 0.540 ± 0.260 | .038 |
| NEO-FFI Extraversion subscale | 0.109 ± 0.053 | .040 | |
| Living with Teenagers | -0.756 ± 0.352 | .032 | |
| Psychiatric Disorder | -1.1 ± 0.36 | .002 | |
| NEO-FFI Neuroticism subscale | -0.246 ± 0.042 | <.001 | |
| DASS-21 anxiety subscale | Employment Status | 0.321 ± 0.113 | .004 |
| Living with Elderly | 0.549 ± 0.251 | .029 | |
| NEO-FFI Openness to Experience subscale | 0.053 ± 0.027 | .048 | |
| Psychiatric Disorder | -1.175 ± 0.28 | <.001 | |
| NEO-FFI Neuroticism subscale | -0.09 ± 0.033 | .006 | |
| DASS-21 stress subscale | Employment Status | 0.511 ± 0.165 | .002 |
| Age | -0.024 ± 0.012 | .045 | |
| Sex | -0.668 ± 0.335 | .047 | |
| Psychiatric Disorder | -1.496 ± 0.411 | <.001 | |
| NEO-FFI Neuroticism subscale | -0.316 ± 0.048 | <.001 | |
| NEO-FFI Conscientiousness subscale | -0.131 ± 0.061 | .031 | |
| QoL self-evaluation | Employment Status | 0.052 ± 0.025 | .036 |
| NEO-FFI Extraversion subscale | 0.025 ± 0.009 | .007 | |
| NEO-FFI Neuroticism subscale | -0.033 ± 0.007 | <.001 | |
| QoL satisfaction | NEO-FFI Extraversion subscale | 0.025 ± 0.011 | .018 |
| Physical Disorder | -0.117 ± 0.051 | .021 | |
| NEO-FFI Neuroticism subscale | -0.047 ± 0.008 | <.001 | |
| Quality of sleep | Physical Disorder | -0.148 ± 0.06 | .013 |
| NEO-FFI Neuroticism subscale | -0.029 ± 0.01 | .003 |
B, unstandardized beta; SE B, standard error; DASS-21, Depression, Anxiety and Stress Scale; QoL, Quality of Life; NEO-FFI, NEO Five-Factor Inventory. For all predictors, positive B = positive predictive value (improvement related to increased values of the predictor) and negative B = negative predictive value (worsening related to increased values of the predictor). Categorical predictors codification: sex (male – 0; female - 1), employment status (unemployed – 0; studying – 1; working – 2), living with teenagers (no – 0; yes - 1), living with elderly (no – 0; yes - 1), having a diagnosis of a psychiatric disorder (no – 0; yes - 1), having a diagnosis of a physical disorder (no – 0; yes - 1), consumption of substances several times a week (no – 0; yes – 1).
Fig. 2.
Representation of the multiple linear regression models. Each separate plot represents the estimates of a single regression model for each dependent variable. The vertical line corresponds to the boundary of statistical significance (i.e., no effect). Each row represents each of the predictors shown on the left. The squares represent the regression coefficients, i.e., the estimated change in the outcome variable for each unit increase in the predictor; significant effects are marked with an asterisk (red and blue correspond to positive and negative effects); and the 95% confidence interval for each coefficient is represented as the segment line. Categorical predictors codification: sex (male – 0; female - 1), employment status (unemployed – 0; studying – 1; working – 2), house balcony and/or terrace (no – 0; yes - 1), living with children (no – 0; yes - 1), living with teenagers (no – 0; yes - 1), living with elderly (no – 0; yes - 1), having a diagnosis of a psychiatric disorder (no – 0; yes - 1), having a diagnosis of a physical disorder (no – 0; yes - 1), consumption of substances several times a week (no – 0; yes – 1), daily amount of time dedicated to sport (less than 1 h – 0; more than 1 h – 1), daily amount of time looking for COVID-19 related news (less than 1 h – 0; more than 1 h – 1). DASS-21: Depression, Anxiety and Stress Scale; QoL: Quality of Life. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article).
4. Discussion
In the first longitudinal study during the emergency state in the Portuguese population, we have found an improvement of depression, anxiety and stress symptoms along the weeks, together with a worsening in the perception of quality of life and sleep. Our results were in line with previous longitudinal studies in populations from other countries (Bendau et al., 2021; Fancourt et al., 2021; Zhou et al., 2020), with the 3 subscales of the DASS-21 linearly decreasing across time. This symptoms’ decrease point to our ability to adapt to new and challenging situations, even when facing such an unprecedented scenario. Despite this, participants rated worse their quality of life and sleep as the weeks passed. This suggests that even though participants were able to adapt to the situation in terms of psychological symptoms, the sacrifices and limitations derived from the confinement had an impact on their quality of life. In this line, it would be relevant to study how this maintained worsening in quality of life affects mental health in the longer term. Indeed, some studies suggest there are negative psychological effects months or years after confinement (Brooks et al., 2020).
With regards to the factors found to predict symptom change, some discrepancies were found in comparison to previous cross-sectional studies. Specifically, previous studies pointed to female sex and younger age as risk factors for higher depression, anxiety and stress symptomatology (Antunes et al., 2020; Ferreira et al., 2020; Huang and Zhao, 2020; Moreira et al., 2021; Rossi et al., 2020). Moreover, pre-pandemic studies already described that women and younger individuals have a higher risk for mental disorders, including anxiety and mood disorders (Alonso et al., 2004b, 2004a). On the other hand, in this study we found that being older and male seemed to be risk factors for a lack of improvement of stress symptomatology, and similar results were found in Salfi et al. (2020) with regards to sex differences. Although these findings could seem contradictory at first, they probably point to greater long-term resilience and ability to adapt during the lockdown in women and younger individuals, which is not incompatible with their general worse mental health reported both in pre-pandemic studies and cross-sectional studies performed during the COVID-19 pandemic. As Salfi et al. (2020) noted, from a sociocultural perspective our results could reflect deep-rooted differences in gender roles within western societies, where women have traditionally held a prominent position in the domestic environment compared to men. In this regard, the extended lockdown would have largely compromised each individual's public life, preserving and emphasizing the domestic one at the same time. This highlights the importance of performing longitudinal studies for addressing questions of adaptability, that would otherwise remain unnoticed with a cross-sectional design.
On the other hand, our findings regarding employment status agree with past cross-sectional research showing that working at home or working without restrictions when compared to not working was associated with better mental health and life satisfaction during the COVID-19 pandemic (Moreira et al., 2021; Paulino et al., 2020; Zhang et al., 2020). This finding is probably linked to economic effects but could also be related to disruption of social networks and loss of leisure activities (Brooks et al., 2020). It should be noted that unemployed individuals represent thus an important vulnerability group, because not only they present worse mental health at Week 0, but they also adapt worse to the situation along the weeks. Measures should be implemented to prevent employment’ loss due to the COVID-19 pandemic, and to protect unemployed individuals.
With regards to house composition, in the longitudinal study from Fancourt et al. (2021), the authors found that individuals living with children had higher levels of anxiety and depressive symptoms initially than individuals living with other adults, but a faster rate of improvement as weeks passed. The authors mention that this improvement could be related to the growing public awareness of research suggesting that children were less affected by COVID-19. In our case, we did not find any significant effect regarding living with young children, but we had a significant negative association with living with teenagers. Thus, this factor seems to have a negative influence with regards to parents’ mental health resilience across time. On the other hand, concerning living with elderly, in the longitudinal study of Canet-Juric et al. (2020) in the Argentinian population, they found the exact same pattern of results than ours with regards to anxiety symptoms. That is, despite initial higher anxiety levels in people living with elderly, probably due to this population being an at-risk population, their decrease of anxiety across time was larger. It could be that after the initial negative impact, they have felt more in control of the situation by reducing exposure to the virus and developed better coping strategies.
Regarding clinical data, previous studies have shown that individuals with organic diseases had higher risk for insomnia, depression, and obsessive-compulsive symptoms during the pandemic (Zhang et al., 2020), and chronic diseases were associated with reduced life satisfaction (Zhang et al., 2020) and enhanced levels of anxiety, depression, and stress (Paulino et al., 2020; Wang et al., 2020). Moreover, a recent systematic review of the mental health consequences of the COVID-19 pandemic also points to the worsening of psychiatric symptoms in patients with preexisting psychiatric disorders (Vindegaard and Benros, 2020). These results are in agreement with our findings regarding the diagnosis of a psychical or psychiatric disorder as a risk factor for mental health worsening across time, pointing thus to another vulnerability group that would need extra support during compulsory confinement (Brooks et al., 2020). Regarding substance consumption, alcohol was the substance reported to be consumed more often, in accordance to other studies (Chodkiewicz et al., 2020). Alcohol consumption has been shown to increase in contexts of economic crisis (Bor et al., 2013; Mucci et al., 2016), and some reports are already available regarding increased alcohol consumption due to the COVID-19 pandemic (Chodkiewicz et al., 2020; Wardell et al., 2020). Our results in this regard could point to alcohol consumption as a coping strategy that would lead to an initial decrease in depressive symptoms (Khantzian, 1997). But as previous research has shown, this is a maladaptive strategy with severe negative consequences in the long run (Khantzian, 1997; Merrill et al., 2014; Stevenson et al., 2019), so attention should be given to people at risk of developing alcohol dependence or abuse in this context.
With regards to personality data, the association between neuroticism and mental health problems is a well-established one, as well as the opposite association with extraversion (Hengartner, 2015; Kuranova et al., 2020; Sadeq and Molinari, 2018; Wilks et al., 2020). Furthermore, within the context of the COVID-19 pandemic, there are already some cross-sectional studies pointing to the risk effect of neuroticism and the protective effect of extraversion on mental health (Gubler et al., 2020; Morales-Vives et al., 2020), which are now further supported by our findings from a longitudinal perspective. Moreover, we also found conscientiousness to be specifically associated with stress symptomatology worsening, and openness to experience with improvement of anxiety symptoms. Thus, individual personality differences seem to be another reliable factor for identifying people more vulnerable of developing mental health problems under this situation.
This study is not without limitations. Firstly, our Week 0 measurement took place almost a week after the state of emergency was declared by the Portuguese Government, so we do not have an actual pre-pandemic baseline. Instead, our first time-point data should probably be interpreted as the peak of mental health worsening, that then progressively improved as we adapted to the new situation. Having a pre-pandemic measurement would have allowed to determine if the different symptoms reported went back to pre-pandemic levels after 8 weeks, but because of the particularities of the situation, this was impossible to get (even if a measurement could have been taken before the state of emergency was declared in Portugal, people were already influenced by the COVID-19 situation at other countries). Secondly, other factors that were not considered in our analysis might have a significant impact on mental health, for example, the workload, history of psychiatric disorders, and the use of coping strategies (e.g. exercise and mindfulness). Additionally, due to convenience sampling, our sample ended up being younger and with more proportion of females than the average Portuguese adult population (www.ine.pt). The lack of a more diverse sample could limit the generalizability of our results, and the ability to explore how other demographic characteristics (e.g., socioeconomic status) may have affected mental health during the pandemic. In this line, there were some differences between those participants that dropped out from the study and those who continued participating. Interestingly though, there were no differences in the NEO-FFI Neuroticism subscale, and in the proportion of participants with psychiatric disorders, which are the two more consistent predictors identified. Finally, our results derive from self-report measures and symptom dimensions were not evaluated by a professional, which could have also introduced a source of bias.
In conclusion, our results provide relevant and novel insights about the course of mental health changes and its predictors during the outbreak of COVID-19 in the Portuguese population. In general, depression, anxiety and stress symptoms seem to improve as the weeks passed during the state of emergency, while the perception of quality of life and sleep got worse. In particular, being female, younger, actively working, and extroverted appear to be protective factors of mental health improvement during this particular period. On the contrary, having a psychiatric diagnosis or physical illness, and higher neuroticism seem to be risk factors for mental health worsening. Our findings help identify vulnerability groups that deserve special attention in this exceptional scenario.
Role of the funding source
The funding sources had no involvement in study design, the collection, analysis and interpretation of data, the writing of the report, or the decision to submit the article for publication.
CRediT authorship contribution statement
Maria Picó-Pérez: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Visualization. Sónia Ferreira: Conceptualization, Methodology, Investigation, Data curation, Writing – review & editing. Beatriz Couto: Conceptualization, Investigation, Data curation. Catarina Raposo-Lima: Conceptualization, Investigation. Mafalda Machado-Sousa: Conceptualization, Investigation. Pedro Morgado: Conceptualization, Methodology, Resources, Writing – review & editing, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Acknowledgments
We would like to thank all participants for their time and availability.
This work has been funded by National funds, through the Foundation for Science and Technology (FCT) - project UIDB/50026/2020, UIDP/50026/2020, and 110_596697345 (Research 4 COVID); and by the projects NORTE-01-0145-FEDER-000013 and NORTE-01-0145-FEDER-000023, supported by Norte Portugal Regional Operational Programme (NORTE 2020), under the PORTUGAL 2020 Partnership Agreement, through the European Regional Development Fund (FEDER).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.08.150.
Appendix. Supplementary materials
References
- Alonso J., Angermeyer M.C., Bernert S., Bruffaerts R., Brugha T.S., Bryson H., De Girolamo G., De Graaf R., Demyttenaere K., Gasquet D., Haro J.M., Katz S.J., Kessler R.C., Kovess Y., Lépine J.P., Ormel J., Polidori G., Russo L.J., Vilagut G., Almansa J., Arbabzadeh-Bouchez S., Autonell J., Bernal M., Buist-Bouwman M.A., Codony M., Domingo-Salvany A., Ferrer M., Joo S.S., Martínez-Alonso M., Matschinger H., Mazzi F., Morgan Z., Morosini P., Palacín C., Romera B., Taub N., Vollebergh W.A.M. Prevalence of mental disorders in Europe: results from the European Study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr. Scand. 2004 doi: 10.1111/j.1600-0047.2004.00327.x. Suppl. [DOI] [PubMed] [Google Scholar]
- Alonso J., Angermeyer M.C., Lépine J.P. The European Study of the Epidemiology of Mental Disorders (ESEMeD) project: an epidemiological basis for informing mental health policies in Europe. Acta Psychiatr. Scand. 2004 doi: 10.1111/j.1600-0047.2004.00325.x. Suppl. [DOI] [PubMed] [Google Scholar]
- Antunes R., Frontini R., Amaro N., Salvador R., Matos R., Morouço P., Rebelo-Gonçalves R. Exploring lifestyle habits, physical activity, anxiety and basic psychological needs in a sample of Portuguese adults during COVID-19. Int. J. Environ. Res. Public Health. 2020;17:1–13. doi: 10.3390/ijerph17124360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain Behav. 2021;11 doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertoquini, V., Pais-ribeiro, J., 2006. Estudo de formas muito reduzidas do modelo dos cinco factores da personalidade.
- Bor J., Basu S., Coutts A., Mckee M., Stuckler D. Alcohol use during the great recession of 2008-2009. Alcohol Alcohol. 2013;48:343–348. doi: 10.1093/alcalc/agt002. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canet-Juric L., Andrés M.L., del Valle M., López-Morales H., Poó F., Galli J.I., Yerro M., Urquijo S. A longitudinal study on the emotional impact cause by the COVID-19 pandemic quarantine on general population. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.565688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chodkiewicz J., Talarowska M., Miniszewska J., Nawrocka N., Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int. J. Environ. Res. Public Health. 2020;17:1–11. doi: 10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa P.T., McCrae R.R. Psychological Assessment Resources; 1992. Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira dos Santos C., Picó-Pérez M., Morgado P. COVID-19 and mental health—what do we know so far? Front. Psychiatry. 2020 doi: 10.3389/fpsyt.2020.565698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira S., Sousa M.M., Moreira P.S., Sousa N., Picó-Pérez M., Morgado P. A wake-up call for burnout in Portuguese physicians during the COVID-19 outbreak: a national survey study. JMIR Public Heal. Surveill. 2020 doi: 10.2196/24312. (Preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubler D.A., Makowski L.M., Troche S.J., Schlegel K. Loneliness and well-being during the COVID-19 pandemic: associations with personality and emotion regulation. J. Happiness Stud. 2020;1 doi: 10.1007/s10902-020-00326-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hengartner M.P. The detrimental impact of maladaptive personality on public mental health: a challenge for psychiatric practice. Front. Psychiatry. 2015;6 doi: 10.3389/fpsyt.2015.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: who will be the high-risk group? Psychol. Heal. Med. 2020 doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- James Rubin G., Wessely S. The psychological effects of quarantining a city. BMJ. 2020 doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- Khantzian E.J. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv. Rev. Psychiatry. 1997 doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kuranova A., Booij S.H., de Jonge P., Jeronimus B., Lin A., Wardenaar K.J., Wichers M., Wigman J.T.W. Do not worry, be happy: protective factors to buffer against distress associated with psychotic experiences. Schizophr. Res. 2020 doi: 10.1016/j.schres.2020.05.019. [DOI] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. 0005-7967(94)00075-1. [DOI] [PubMed] [Google Scholar]
- Merrill J.E., Wardell J.D., Read J.P. Drinking motives in the prospective prediction of unique alcohol-related consequences in college students. J. Stud. Alcohol Drugs. 2014;75:93–102. doi: 10.15288/jsad.2014.75.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales-Vives F., Dueñas J.M., Vigil-Colet A., Camarero-Figuerola M. Psychological variables related to adaptation to the COVID-19 lockdown in Spain. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.565634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira P.S., Ferreira S., Couto B., Machado-Sousa M., Fernández M., Raposo-Lima C., Sousa N., Picó-Pérez M., Morgado P. Protective elements of mental health status during the COVID-19 outbreak in the Portuguese population. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18041910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucci N., Giorgi G., Roncaioli M., Perez J.F., Arcangeli G. The correlation between stress and economic crisis: a systematic review. Neuropsychiatr. Dis. Treat. 2016 doi: 10.2147/NDT.S98525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pais-Ribeiro J.L., Honrado A., Leal I. Contribuição para o estudo da adaptação portuguesa das escalas de ansiedade, depressão e stress (EADS) de 21 items de Lovibond e Lovibond. Psicol. Saúde Doenças. 2004;5:229–239. [Google Scholar]
- Paulino M., Dumas-Diniz R., Brissos S., Brites R., Alho L., Simões M.R., Silva C.F. COVID-19 in Portugal: exploring the immediate psychological impact on the general population. Psychol. Heal. Med. 2020 doi: 10.1080/13548506.2020.1808236. [DOI] [PubMed] [Google Scholar]
- Rossi, R., Socci, V., Talevi, D., Mensi, S., Niolu, C., Di Marco, A., Rossi, A., Siracusano, A., Di, G., 2020. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N=18147 web-based survey. medRxiv 2020.04.09.20057802. 10.1101/2020.04.09.20057802. [DOI] [PMC free article] [PubMed]
- Sadeq N.A., Molinari V. Personality and its relationship to depression and cognition in older adults: implications for practice. Clin. Gerontol. 2018 doi: 10.1080/07317115.2017.1407981. [DOI] [PubMed] [Google Scholar]
- Salfi F., Lauriola M., Amicucci G., Corigliano D., Viselli L., Tempesta D., Ferrara M. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: a longitudinal study on the Italian population. Neurobiol. Stress. 2020 doi: 10.1016/j.ynstr.2020.100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson B.L., Dvorak R.D., Kramer M.P., Peterson R.S., Dunn M.E., Leary A.V., Pinto D. Within- and between-person associations from mood to alcohol consequences: the mediating role of enhancement and coping drinking motives. J. Abnorm. Psychol. 2019;128:813–822. doi: 10.1037/abn0000472. [DOI] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain. Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell J.D., Kempe T., Rapinda K.K., Single A., Bilevicius E., Frohlich J.R., Hendershot C.S., Keough M.T. Drinking to cope during COVID-19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol. Clin. Exp. Res. 2020;44:2073–2083. doi: 10.1111/acer.14425. [DOI] [PubMed] [Google Scholar]
- Wilks Z., Perkins A.M., Cooper A., Pliszka B., Cleare A.J., Young A.H. Relationship of a big five personality questionnaire to the symptoms of affective disorders. J. Affect. Disord. 2020;277:14–20. doi: 10.1016/j.jad.2020.07.122. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2020. Mental health and psychosocial considerations during the COVID-19 outbreak. Geneva, Switzerland.
- Zhang S.X., Wang Y., Rauch A., Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W.R., Wang K., Yin L., Zhao W.F., Xue Q., Peng M., Min B.Q., Tian Q., Leng H.X., Du J.L., Chang H., Yang Y., Li W., Shangguan F.F., Yan T.Y., Dong H.Q., Han Y., Wang Y.P., Cosci F., Wang H.X. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Macgeorge E.L., Myrick J.G. Mental health and its predictors during the early months of the COVID-19 pandemic experience in the United States. Int. J. Environ. Res. Public Health. 2020;17:1–19. doi: 10.3390/ijerph17176315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Chen L., Ji H., Xi M., Fang Y., Li Y. The risk and prevention of novel coronavirus pneumonia infections among inpatients in psychiatric hospitals. Neurosci. Bull. 2020 doi: 10.1007/s12264-020-00476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.