Abstract
Pandemics such as the Covid-19 pandemic have shown to impact our physical and mental well-being, with particular challenges for children and families. We describe data from 43 adults (31♀, ages = 22–51; 21 mothers) and 26 children (10♀, ages = 7–17 years) including pre-pandemic brain function and seven assessment points during the first months of the pandemic. We investigated (1) changes in child and adult well-being, (2) mother–child associations of mental well-being, and (3) associations between pre-pandemic brain activation during mentalizing and later fears or burden. In adults the prevalence of clinically significant anxiety-levels was 34.88% and subthreshold depression 32.56%. Caregiver burden in parents was moderately elevated. Overall, scores of depression, anxiety, and caregiver burden decreased across the 11 weeks after Covid-19-onset. Children’s behavioral and emotional problems during Covid-19 did not significantly differ from pre-pandemic levels and decreased during restrictions. Mothers’ subjective burden of care was associated with children’s emotional and behavioral problems, while depression levels in mothers were related to children’s mood. Furthermore, meeting friends was a significant predictor of children’s mood during early restrictions. Pre-pandemic neural correlates of mentalizing in prefrontal regions preceded later development of fear of illnesses and viruses in all participants, while temporoparietal activation preceded higher subjective burden in mothers.
Subject terms: Psychology, Human behaviour
Introduction
The global onset of the coronavirus disease 2019 (Covid-19) pandemic has been recognized as a significant threat to our physical and mental well-being. Worldwide efforts have been implemented including protective health measures to slow down or prevent the direct physical effects of the virus. In Switzerland these restrictions included school closure, work-from-home orders, and travel restrictions. Past and accumulating evidence indicates that restrictions (e.g., school closure, lockdown, social distancing) may have a significant effect on individuals’ psychosocial functioning, possibly through increases in emotional distress1,2. Evidence indicates that mental health consequences include an increase in neuropsychiatric symptoms of affect and behavior3,4. Such increases in negative effects (e.g., stress, anxiety, depression, or somatic complaints) associated with Covid-19 and restrictions are reported globally1,2,5,6. The duration of lockdown and restrictions have been linked to increased distress5. Negative effects tend to be higher in younger individuals, those with chronic disease or pre-existing health conditions, females and those living alone or in socioeconomic adversity1,2,7.
Children’s, parents’, and families’ lives may be particularly impacted by Covid-19-related restrictions8. A sudden decrease in social contacts is opposite to the human social nature and our existing routines9,10. For children and adolescents, positive peer-relationships, the ability to pursue hobbies and educational opportunities are affected11. For parents, an increased burden may result from a disrupted work-life balance. Parental exhaustion, irritability, and mental health symptoms (e.g., depression and anxiety) have been reported to increase during pandemics12,13. Moreover, parents’ psychological distress can affect children’s ability to adjust to novel situations and may therefore promote the development of behavioral and emotional problems14. High anxiety or depressive symptoms in parents have been associated with an increase in harsh parenting and child abuse potential15, indicating urgent consideration for policymakers to provide resources and support for at-risk families.
Notably, reports on increases in emotional distress are complemented by reports of a smaller, but significant, proportion of individuals who describe no changes or increases in well-being during restrictions. Such data indicates that interindividual differences in the effect of restrictions on mental health should be considered2. For example, restrictions may bring some families closer together, increase parent–child bonding and joint experiences7. An increased understanding of interindividual differences that protect or increase risk for psychopathologies holds the potential to inform personalized support associated with pandemics.
The identification of potential precursors for psychosocial functioning during challenging life events is crucial for the development and implementation of prevention and intervention measures. Socioemotional abilities represent different skill sets of social and emotional functioning16 which may serve as potential antecedents of psychosocial functioning during challenging life events17. Successful socioemotional skill development in children is positively linked to present and future well-being18 and a disruption of these has been linked to externalizing and internalizing problems19. Furthermore, socioemotional skill development strongly relies on caregiver-child relationships and dyadic learning20.
A fundamental ability for many later-emerging socioemotional abilities is mentalizing, a sociocognitive skill enabling the understanding of emotions, thoughts or motives of others and oneself (enabled by our so-called Theory of Mind and impacted by parenting behaviors21). Having a well-developed Theory of Mind has been associated with higher social competences, psychological and physiological functioning22. Contrariwise, impaired mentalizing abilities have been linked to stress and depression23, potentially serving as a predictor of these17. On a neural level, the functional brain network associated with mentalizing typically includes areas such as the bilateral temporoparietal junction, precuneus, medial prefrontal cortex and right superior temporal sulcus24, with the temporoparietal junction and prefrontal cortex particularly relevant when thinking about others’ and one’s own mental states10. The right temporoparietal junction has been the area most consistently activated during different types of fMRI mentalizing tasks24. The right dorsolateral prefrontal cortex is similarly involved during mentalization and perspective taking, but also plays a key role in emotion regulation, which is strongly associated with mental well-being25,26. A disrupted ability to mentalize, including associated neural alterations, can be found in clinical disorders, such as borderline personality disorder, conduct disorder or alexithymia27,28.
Increasing evidence highlights the urgent need to consider the indirect consequences of the pandemic on physical and psychological well-being. Children’s, parents’, or families’ lives may be particularly affected, and parental well-being is suggested to be intertwined with that of children. Past evidence further indicates that well-being and stress are moderated by sociocognitive skills. In this study, we aimed (1) to investigate the effects of Covid-19 and associated restrictions on child and adult well-being as measured repeatedly during the first months after Covid-19 onset; (2) to assess associations of mental well-being (e.g., anxiety, depression, caregiver burden) in mothers with children’s emotional and behavioral problems or mood; (3) to examine the association between the neural correlates of mentalizing as measured prior to Covid-19 and later development of fear of contamination and illnesses in all participants, or caregiver burden in mothers. In line with prior work2,29, we expect reports of negative effects on mental well-being (e.g., general health, anxiety, distress, depression), with possible changes over time. Emotional and behavioral problems in children may vary over time. Furthermore, we suggest that variations in emotional and behavioral problems or mood in children are positively associated with variables of mental well-being of their mothers. In everyday life, increased mentalizing skills are linked to improved socioemotional functioning22. However, studies have shown that particularly during challenging life circumstances an elevated tendency to mentalize may also be negatively associated with our well-being (e.g., higher anxiety in those with better mentalization skills17). In line with this observation, we suggest that neural correlates of mentalizing are positively associated with later caregiver burden or the development of higher anxiety and fears associated with viruses.
Methods
Participants
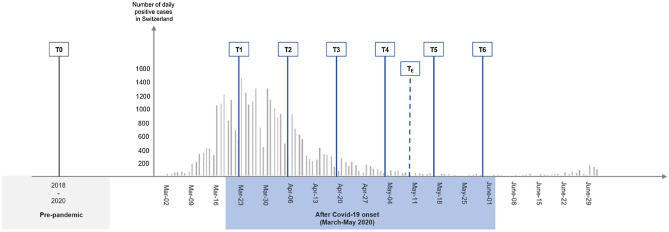
Ninety-eight European participants (60 adults and 38 children) of a previous cross-sectional neuroimaging study investigating socioemotional development between 2018 and 2020 were asked to participate in the Covid-19 online follow-up assessments. Pre-pandemic assessments included behavioral tests and functional magnetic resonance imaging (fMRI) during mentalizing; see study description in30. We here describe data from the first 3 months after the first implementation of stringent restrictions following Covid-19 onset in Switzerland and include seven assessments time points across this time period (Fig. 1). Sixty-nine participants (43 adults: 31 females; average age = 35.14 years; age range 22–51 years; 26 children: 10 females; average age = 10.69 years; age range 7–17 years) agreed to take part in the follow-up study; retention rate per time point for these 69 individuals were as follows: T3 (41 adults [95.35%], 24 children [92.31%],); T4 (39 adults [90.70%], 23 children [88.46%],); TE (40 adults [93.02%], 24 children [92.31%]); T5 (29 adults [67.44%], 15 children [57.69%]); T6 (37 adults [86.05%], 23 children [88.46%]).
Figure 1.
Study design and overview of assessment time points conducted prior to (T0) and during the pandemic and associated restrictive measures in Switzerland (T1–T6).
All adults and children were previously recruited from the general community and schools for a study on the behavioral and neural correlates of socioemotional skill development. More specifically, participants took part in an evaluation study for a novel cognitive and affective Theory of Mind cartoon task (specifics may be found in30). Furthermore, 21 women and 26 children were related (mother–child dyads). Parents of the children reported no known clinical diagnosis for 23 of the children, for three children a clinical diagnosis of ADHD was indicated and for one of these three children the parents further noted a possible developmental delay. In line with guidelines and approval by the local ethics board (Ethikkomission Nordwest- und Zentralschweiz) all participants signed an informed consent form. Additionally, in case of children, verbal assent of the child and written informed consent from a parent and/or legal guardian was collected. All research presented here was performed in accordance with the relevant guidelines and regulations of the Ethikkomission Nordwest- und Zentralschweiz.
Assessments
Overall, eight testing time points are included, with the first (T0) reporting data obtained during the two years prior to the pandemic. Seven assessments were conducted across 75 days (11 weeks) after Covid-19 onset in Switzerland. The online assessment started following nationwide restrictions implemented in Switzerland on March 16th, 2020, including the ban of events, school closure, closure of all non-essential and hardware stores, garden centers, markets, museums, zoos, nightclubs, closure of hairdresser, restaurants, ban of gatherings (maximum of five people) and home-office orders, etc. Schools were re-opened on May 11th, 2020, resulting in more parents returning to work. Only assessments relevant to the present analyses are described below. Further details, including information for all assessments conducted prior to Covid-19 onset (T0) and during restrictions (T1–T6) may be found in the Supplementary Methods.
Testing prior to Covid-19 (T0) took place between March 2018 and February 2020 and included functional neuroimaging during mentalizing. Online assessments after Covid-19 onset were conducted from March to May 2020. Participants filled out six biweekly online questionnaires (labelled as T1, T2, T3, T4, T5, T6 in Fig. 1). For adults, these targeted anxiety (State-Trait Anxiety Inventory or STAI-6; a self-report questionnaire to assess anxiety level as state31), depression (Center for Epidemiologic Studies Depression Scale or CESD-R, German version32; assessing symptoms in the last 1–2 weeks relating dysphoria, anhedonia, appetite, sleep, thinking, guilt, fatigue, movement and suicidal ideation), general health (General Health Questionnaire or GHQ-12, German version; a self-report instrument to screen for psychosocial well-being33), distress (questionnaire adapted from the Kessler Psychological Distress Scale, but answer format was modified allowing participants to indicate their emotional state in relation to their usual emotional state34) and subjective burden of caregiving for mothers (the Burden Scale for Family Caregivers or BSFC-s35; a self-report questionnaire assessing subjective burden of family caregivers, which was adapted to capture increased burden in parental responsibilities during restrictions). In children emotional and behavioral problems were assessed using the Strengths and Difficulties Questionnaire (SDQ36) and subjective mood ratings (children had to choose between 5 different smileys in order to indicate their mood in the last days. Ratings included 1: very happy, 2: happy, 3: unsure, 4: unhappy, 5: very sad). Children were further asked whether they had met any friends in the previous week. News consumption (adults only) and time spent outside (all participants) were assessed by asking participants to indicate the amount of time spent on these activities on a 5-point Likert scale. Adults reported their daily news consumption across all forms of media through the following scale: 1: no time, 2: approximately 15 min, 3: approximately 30 min, 4: approximately 1 h, 5: more than an hour of time spent consuming news). Adults and children indicated the average duration of spending time outside per day in the past week (1: no time, 2: half an hour, 3: 1 h, 4: 1–2 h, 5: more than 2 h of time spent outside).
One extra questionnaire (TE, between T4 and T5) was added before a first ease in restrictions was introduced by the government. This extra testing consisted of the Child Behavior Checklist (CBCL37) evaluating child behavior and the Fear of Illness and Virus Evaluation (developed by Professor Jill Ehrenreich-May, https://adaa.org/node/5168). CBCL was also acquired at T0 allowing a pre-/post-comparison. Of the six biweekly assessments, the last two (T5, T6) were conducted after schools reopened.
Behavioral data analyses
Mental well-being during Covid-19-related restrictions
First, adults’ scores in anxiety depression, and caregiver burden were screened. STAI-6 total scores above 40 were considered as an indicator of clinically significant levels of anxiety, according to38. Depression scores were screened to detect subthreshold depression symptoms according to the CESD total score (CESDtotal ≥ 16) or meeting criteria for a major depressive episode (description of the algorithm for calculation may be found at: https://cesd-r.com/cesdr/). Next, we calculated the 11-week prevalence of clinically significant anxiety, subthreshold depression and major depression (i.e., the proportion of participants surpassing relevant cut-off scores and fulfilling criteria at least once during the assessment period). Finally, parental burden was classified as “low”, “moderate” or “high” according to the classification suggested by Pendergrass and colleagues39 (BSFC-s scores of 0–4 are considered as low; 5–14 as moderate; 15–30 as high).
We investigated the effect of Covid-19 and related restrictions on mental well-being using linear mixed-effect models in R (https://www.r-project.org/). As a first step, missing data points were evaluated to assess whether these were missing at random (MAR). In case of no violation of MAR assumption missing data was replaced by Multivariate Imputation by Chained Equations MICE package in R40 employing the predictive mean matching method. Overall, 14.41% of the testing time points reported in the present analyses were imputed (12.79% in adults, 16.03% in children).
Linear mixed-effects models were employed to analyze the relationship between length since Covid-19 onset and continuous outcome measures (depression, anxiety, general health, distress, caregiver burden, and emotional and behavioral problems in children) using lme441. Duration (in weeks) was entered as a fixed effect. Subjects were entered as a random effect and the model allowed for random intercepts and random slopes accounting for non-independence of datapoints (same person answering multiple times). Furthermore, a different response of the subjects was expected (each person might react differently to duration of restrictions). P values were obtained by the Satterthwaite approximation as recommended by Luke et al.42 for small group sizes using the lmerTest package43. This pipeline was adjusted for the analysis of depression, caregiver burden and emotional and behavioral problems in children for the following reasons: Depression scores (CESD-R) and children’s emotional problems, conduct problems, hyperactivity, peer problems and total scores (SDQ) were log-transformed after a visual inspection of the data revealing a right skew. For caregiving burden (BSFC-s), and children’s peer problems and total score of emotional and behavioral problems (SDQ), the full model (including random intercepts and slopes for each subject) indicated an overfit. Consequently, a simplified model excluding random slopes by subject was implemented.
For the analysis of categorical, non-parametric data (i.e., clinically relevant threshold for depression reached [yes/no], time spent outside, news consumption and mood in children), Friedman tests were used. Significant main effects were followed up using post-hoc pairwise comparisons and adjusted using Holm-Bonferroni correction. Finally, one-way analysis of variance was employed to test whether emotional and behavioral problems (SDQ and CBCL) in children differed prior to and during Covid-19-related restrictions. For the score during Covid-19 all time points of SDQ were averaged to build one score (average of five online assessments). CBCL was only assessed once at TE.
Mother–child associations
To test whether mental well-being in mothers (anxiety, depression, and caregiver burden) explained variability in children’s emotional or behavioral problems a multiple regression analysis was implemented corrected for children’s age and sex. Since emotional and behavioral problems in children were assessed through parental reports, parental bias may impact findings. Therefore, we repeated the multiple regression analysis by using mood scores provided by the children as a dependent variable.
Post-hoc follow-up assessment
Mental well-being and the development of negative symptoms during stressful life events have been suggested to be influenced by further variables of interest, including sex and parenting44, news exposure2 or time spent outside45. For adult participants, multiple regression analysis controlling for age was conducted to assess whether variation in mental well-being (i.e., anxiety, depression, or distress) were explained by sex, news consumption, time spent outside or parenthood. For children, we assessed whether children’s well-being (self-report for mood) during restrictions was explained by time spent outside or meeting friends (yes/no) using multiple regression analyses, controlling for age and sex of the children.
Children’s subjective reports
Children were asked two open-ended questions: At T1–T4, these were “What do you like about spending more time at home now?” and “What do you like less about spending more time at home now?”. At T5 (after the first week of school opening) and T6 (3 weeks after school reopened) these were changed to “What do you like about going back to school?” and “What do you like less or think, is a bit annoying, about going back to school?” Subcategories based on topics mentioned were built and coded by two independent reviewers (Supplementary Methods).
fMRI data analyses
fMRI data was analyzed using SPM12 running on MATLAB R2020b (www.fil.ion.ucl.ac.uk/spm). Neural correlates of mentalizing were tested using the CAToon task30 (see30 and Supplementary Methods). fMRI was acquired for all participants between 2018 and 2020. In short, fMRI during mentalization was acquired using a cartoon-based Theory of Mind task [experimental condition: affective (AT) and cognitive (CT) Theory of Mind; control condition: physical causality (PC)]. The neural correlates of mentalizing were based on a regressor of interest including both cognitive and affective Theory of Mind as compared to physical causality ((AT|CT) > PC). Whole-brain T2-weighted echo-planar images were collected using a 20-channel head coil on a Siemens 3T Prisma MR scanner (specifics in Supplementary Methods). Group analyses included age and sex as covariates and all findings were corrected for multiple comparisons using whole brain family-wise error correction (FWE).
For the present purpose mean parameter estimates were extracted for areas of interest consistently recruited during mentalizing24, including right temporoparietal junction (TPJ) and dorsolateral prefrontal cortex (dlPFC), using the MarsBar toolbox46. More specifically, right TPJ was selected as a region of interest since it is most consistently recruited during mentalizing tasks and perspective taking in both children and adults47. A 7 mm sphere was extracted for the right TPJ, because the group activation cluster extended beyond the area of interest (spanning over 5860 voxels reaching from temporal pole to occipital areas). The right dlPFC was selected as a region of interest, because of its involvement during mentalization and perspective taking, but also because of its key role in emotion regulation, which is in turn strongly associated with mental well-being25, including the development of stress-related burden, depression and anxiety26,48. To test whether these regions were significant predictors of fears about contamination and illness, or caregiver burden, we employed multiple regression analyses controlling for age and sex when applicable. For the multiple regression analysis including caregiver burden we calculated one score averaging all BSFCtotal scores. In-scanner data collection was only evaluated to assure task compliance (i.e., no more than 10% missing in all trials; Supplementary Table S1).
Results
Behavioral findings
Descriptive statistics
A summary of the behavioral data collected prior to and during the early weeks following Covid-19 onset is included in Table 1 (in children scores prior to and scores averaged over the 11-weeks online assessment are reported. For adults only averaged scores are reported; Fig. 2).
Table 1.
Group characteristics of adults and children prior to and during the first months after Covid-19 onset.
| Adults (n = 43, 31 females) | Children (n = 26, 10 females) | |||||||
|---|---|---|---|---|---|---|---|---|
| First pandemic months | M ± SD | Pre-pandemic | M ± SD | First pandemic months | M ± SD | |||
| Age | In years | 35.14 ± 9.20 | Age | In years | 9.58 ± 2.39 | Age | In years | 10.69 ± 2.52 |
| Time s. 1st test | In months | 18.76 ± 7.03 | IQ | Verbal | 13.88 ± 8.94 | Time s. 1st test | In months | 13.64 ± 7.01 |
| ISCED | 4.84 ± 1.75 | Non-verbal | 12.88 ± 4.48 | SDQa | Emotional problems | 1.21 ± 1.62 | ||
| BSFCab | Subjective burden of care | 8.32 ± 4.42 | SDQ | Emotional problems | 1.73 ± 2.24 | Conduct problems | 1.64 ± 1.49 | |
| STAI-6a | Anxiety | 38.85 ± 8.57 | Conduct problems | 1.69 ± 1.72 | Hyperactivity | 2.88 ± 1.93 | ||
| Distressac | Distress | 4.09 ± 0.56 | Hyperactivity | 2.81 ± 1.86 | Peer problems | 1.64 ± 1.44 | ||
| GHQa | Mental health | 5.15 ± 2.57 | Peer problems | 0.92 ± 1.41 | Prosocial | 6.56 ± 1.53 | ||
| CESD-Rb | Depression | 9.96 ± 10.60 | Prosocial | 7.35 ± 1.67 | Total | 7.38 ± 4.87 | ||
| Total | 7.15 ± 4.97 | CBCL | Withdrawn | 54.58 ± 5.38 | ||||
| News | [1] no time | 1.89% | CBCL d | Withdrawn | 54.27 ± 5.50 | Somatic problems | 56.54 ± 7.46 | |
| Consumptiona | [2] 15 min | 36.04% | Somatic problems | 55.46 ± 5.57 | Anxious/depressed | 55 ± 8.32 | ||
| (daily) | [3] 30 min | 30.76% | Anxious/depressed | 56.73 ± 8.49 | Social problems | 53.13 ± 4.78 | ||
| [4] 1 h | 21.82% | Social problems | 53.65 ± 4.63 | Schizoid-compulsive | 54.13 ± 6.49 | |||
| [5] > 1 h | 9.49% | Schizoid-compulsive | 54.35 ± 6.36 | Attention problems | 55 ± 5.82 | |||
| Attention problems | 55.19 ± 5.84 | Delinquent behaviour | 52.38 ± 4.43 | |||||
| Time outsidea | [1] No time | 1.25% | Delinquent behaviour | 52.69 ± 3.90 | Aggressive behaviour | 53.29 ± 5.29 | ||
| (daily) | [2] 30 min | 21.78% | Aggressive behaviour | 55.38 ± 6.83 | Total | 51 ± 9.36 | ||
| [3] 1 h | 19.77% | Total | 53.81 ± 8.45 | FIVE | Fears about contamination and illness | 12.38 ± 2.78 | ||
| [4] 1–2 h | 34.93% | Fears about social distancing | 15.17 ± 4.27 | |||||
| [5] > 2 h | 22.28% | Behaviors related to illness and viruses | 29.63 ± 5.32 | |||||
| FIVE | Fears about contamination and illness | 13.53 ± 2.94 | Impact of illness and virus fears | 2.83 ± 1.01 | ||||
| Fears about social distancing | 15.10 ± 3.63 | Total | 30.38 ± 6.76 | |||||
| Behaviors related to illness and viruses | 30.55 ± 4.85 | Time outsidea | [1] No time | 0.72% | ||||
| Impact of illness and virus fears | 2.98 ± 1.05 | (daily) | [2] 30 min | 12.79% | ||||
| Total | 31.6 ± 6.11 | [3] 1 h | 18.49% | |||||
| [4] 1–2 h | 32.90% | |||||||
| [5] > 2 h | 35.10% | |||||||
| Mooda | [1] Very happy | 31.34% | ||||||
| [2] Happy | 46.07% | |||||||
| [3] Unsure | 15.44% | |||||||
| [4] Unhappy | 5.70% | |||||||
| [5] Very sad | 1.45% | |||||||
Time s. 1st test time since first testing, ISCED international standard classification of education, BSFC burden scale for family caregivers, STAI-6 state-trait anxiety inventory, GHQ general health questionnaire, CESD-R center for epidemiologic studies depression scale, FIVE fear of illness and virus evaluation, SDQ strengths and difficulties questionnaire, CBCL child behavior checklist.
aAverage score.
bIn mothers only.
cDistress: 1—much less than usual, 2—quite less than usual, 3—a little less than usual, 4—as much as usual, 5—a little more than usual, 6—quite a bit more than usual, 7—much more than usual.
dN = 25 (out of a total N pre-/during confinement of 26).
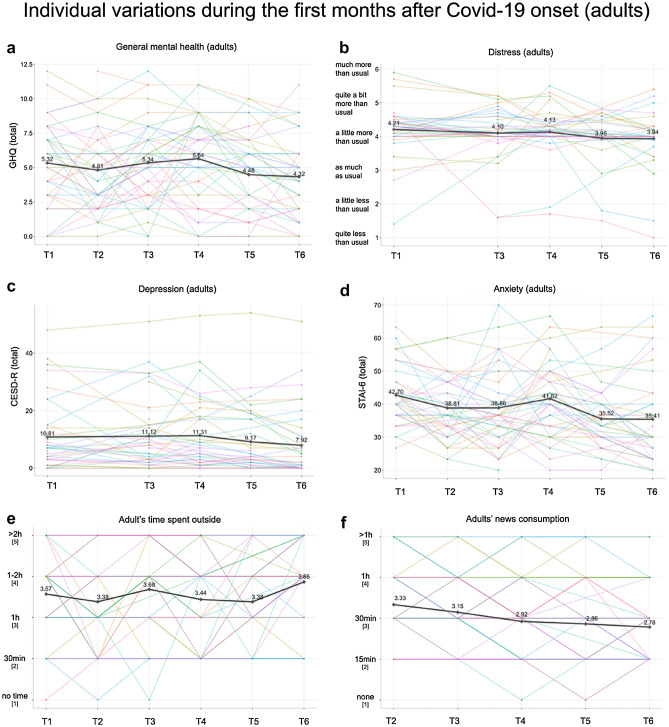
Figure 2.
Variations of group mean (bold) and individual (colorful) scores in mental well-being across the first months after Covid-19 onset in adults. (a) Variation in scores of general mental health. (b) Variation in distress scores. (c) Variation in depression scores. (d) Variation in anxiety scores. (e) Variation in time spent outside. (f) Variation in news consumption.
Well-being during Covid-19 in adults
32.56% of all adults reported increased depression scores indicating the presence of subthreshold depressive symptoms (CESDtotal ≥ 16) with 4.65% meeting the criteria for a major depressive episode at least once. The prevalence of clinically significant anxiety was 34.88%. Group average scores reached clinically significant levels of anxiety at T1 (mean = 42.70, SD = 8.952) and T4 (mean = 41.62, SD = 8.798). Group average scores of subjective burden were in the moderate range (BSFC-s scores of 5–1439) throughout the whole assessment period (Fig. 3).
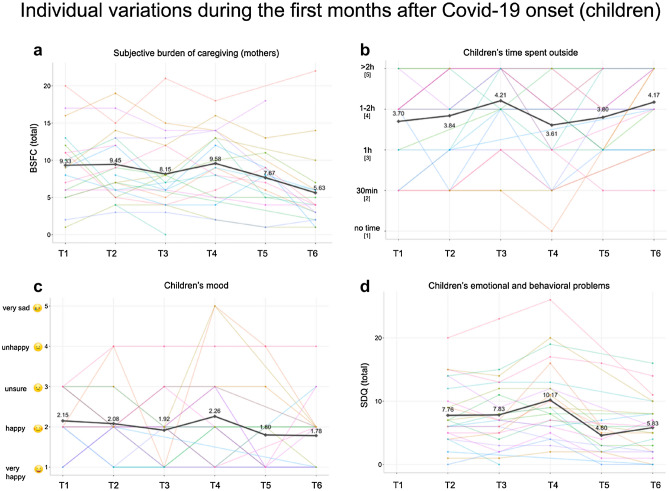
Figure 3.
Variations of group mean (bold) and individual (colorful) scores in mental well-being across the first months of Covid-19 onset in children and mothers. (a) Variation in mothers' subjective burden. (b) Variation in children’s time spent outside. (c) Variation in children’s mood. (d) Variation in children’s emotional and behavioral problems.
When estimating the effect of restrictions on mental health longitudinally, linear mixed-effect models revealed a small but significant decrease in depression (β = − 0.04), anxiety (β = − 0.61), and burden of caregiving (β = − 0.26) scores with each week passing by. There was a non-significant decrease in general health (β = − 0.06) and distress (β = − 0.02) scores. A detailed summary of all models is included in Table 2.
Table 2.
Linear mixed models in adults estimating the effect of time after Covid-19 onset on mental health indices.
| Predictors | CESD (log) | STAI | BSFC | GHQ | Distress | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | |
| Intercept | 2.05 (0.17) | 1.72–2.37 | 42.58 (1.41) | 39.82–45.33 | 10.07 (0.97) | 8.16–11.98 | 5.49 (0.43) | 4.65–6.34 | 4.22 (0.12) | 3.99–4.46 | |||||
| Duration (weeks) | − 0.04 (0.02) | − 0.07 to − 0.01 | 0.012 | − 0.61 (0.16) | − 0.93 to − 0.29 | 0.001 | − 0.26 (0.08) | − 0.42 to − 0.09 | 0.003 | − 0.06 (0.04) | − 0.13 to 0.02 | 0.162 | − 0.02 (0.02) | − 0.05 to 0.01 | 0.218 |
| ICC | 0.78 | 0.59 | 0.56 | 0.59 | 0.67 | ||||||||||
| N | 215/43 | 258/43 | 132/22 | 258/43 | 215/43 | ||||||||||
CESD center of epidemiologic studies depression scales, STAI state and trait anxiety inventory (state anxiety sum scores), BSFC-s burden scale for family caregivers (sum score), GHQ General Health Questionnaire (sum score), Distress modified Kessler psychological distress scale (mean), SE standard error, CI confidence interval, Duration (weeks) fixed effect, weeks passed since restrictions have been introduced, ICC intraclass correlation coefficient, N number of observations)/(number of participants), p values have been estimated using Satterthwaite approximation, significant effects in bold.
For the categorical variables Friedman test of differences revealed significant variations in time spent outside (χ2 = 18.422, p = 0.002) and news consumption (χ2 = 25.177, p < 0.001). Follow-up Bonferroni-corrected pairwise comparisons showed no significant differences for time spent outside between timepoints. For news consumption, follow-up pairwise comparisons showed significant differences between timepoints T2 and T6 (Fig. 2).
Well-being during Covid-19 in children
Linear mixed-effects models indicated a significant decrease in children’s scores of conduct problems (β = − 0.04), hyperactivity (β = − 0.03), peer problems (β = − 0.03) and overall emotional and behavioral problems (β = − 0.04; total score of SDQ), whereas there was a non-significant decrease in emotional problems (β = − 0.003) and increase in prosocial behavior (β = 0.08). A detailed summary of all models is included in Table 3. Friedman test revealed a significant variation in time spent outside (χ2 = 21.002, p < 0.001), with significant differences between timepoints T1 and T3. A significant variation over time was also revealed in mood ratings (χ2 = 13.425, p = 0.020), however, post-hoc pairwise comparisons remained non-significant. One-way analysis of variance indicated no significant difference in behavioral and emotional problems in children when comparing pre-Covid-19 scores with average scores obtained during Covid-19 (Supplementary Table S2).
Table 3.
Linear mixed models estimating the effect of time after Covid-19 onset on children’s behavioral and emotion problems.
| Predictors | Conduct problems (log) | Emotional problems (log) | Hyperactivity (log) | Peer problems (log) | Prosocial behavior | Total (log) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | Estimates (SE) | CI (95%) | p | |
| Intercept | 1.02 (0.15) | 0.73–1.32 | 0.55 (0.17) | 0.23–0.88 | 1.38 (0.14) | 1.10–1.67 | 1.04 (0.14) | 0.77–1.31 | 5.96 (0.46) | 5.06–6.86 | 2.20 (0.15) | 1.91–2.49 | ||||||
| Duration (weeks) | − 0.04 (0.01) | − 0.07 to − 0.01 | 0.012 | − 0.003 (0.02) | − 0.03 to 0.03 | 0.834 | − 0.03 (0.01) | − 0.05 to − 0.00 | 0.047 | − 0.03 (0.01) | − 0.06 to − 0.01 | 0.016 | 0.08 (0.05) | − 0.00 to 0.17 | 0.075 | − 0.04 (0.01) | − 0.07 to − 0.02 | 0.001 |
| ICC | 0.77 | 0.49 | 0.72 | 0.56 | 0.58 | 0.66 | ||||||||||||
| N | 130/26 | 130/26 | 130/26 | 130/26 | 130/26 | 130/26 | ||||||||||||
SE standard error, CI confidence interval, Duration (weeks) fixed effect, weeks passed since restrictions have been introduced, ICC intraclass correlation coefficient, N (number of observations)/(number of participants), p values have been estimated using Satterthwaite approximation, significant effects in bold.
Mother–child associations
The multiple regression analyses including age and sex of the children revealed that the full model for mothers’ subjective burden of caregiving explained 52.7% (ß = 0.763, t(22) = 4.762, p < 0.001) of the variance in children’s emotional and behavioral problems (complete model: F(3,22) = 8.173, p < 0.001; R2 = 0.527 [adjusted R2 = 0.463]). Anxiety and depression in mothers did not enter the model. Children’s self-reported mood was best predicted by mothers’ depression scores (ß = 0.660, t(22) = 4.136, p < 0.001). Depression scores explained 45.2% of variance in children’s mood (complete model including depression, age and sex: F(3,22) = 6.037, p = 0.004; R2 = 0.452 [adjusted R2 = 0.377]). Mothers’ experienced burden of caregiving and anxiety did not enter the final model.
Post-hoc follow-up assessments
Post-hoc multiple regression analyses revealed no impact of sex, news consumption, time spent outside or parenthood on variations in scores of anxiety, depression or distress in adults, as neither entered into the prediction model. For children, meeting friends (yes/no) explained 35.5% of the variation and entered into the model as a significant predictor of mood (ß = − 0.601, t(22) = − 3.551, p = 0.002). Mood was negatively coded (lowest score representing the best mood and highest scores representing lowest mood/sadness), indicating that meeting friends was positively linked to a better mood. The model including meeting friends controlling for age and sex was established as a significant predictor of mood with an R2 = 0.380 (adjusted R2 = 0.294; F(3, 22) = 4.499, p = 0.013).
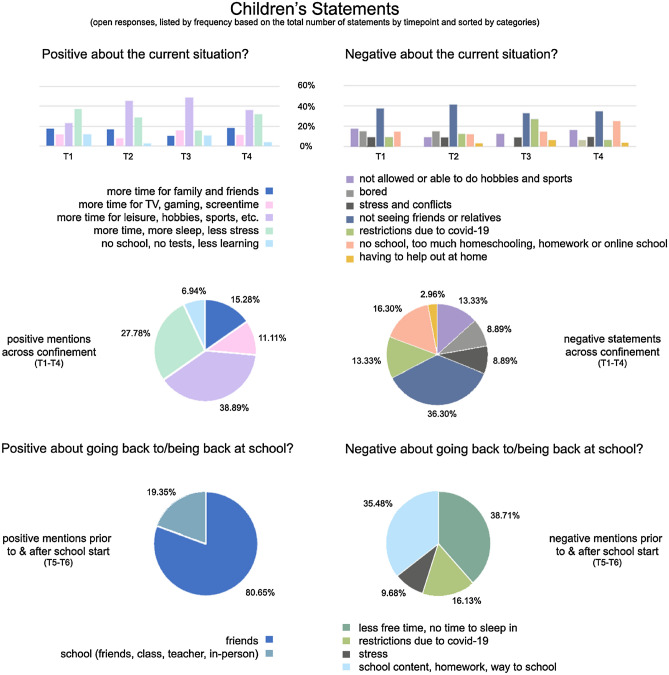
Children’s qualitative reports
An overview about children’s subjective statements is given in Fig. 4.
Figure 4.
Qualitative measures of positive and negative associations with school closure or opening in children.
Neuroimaging findings
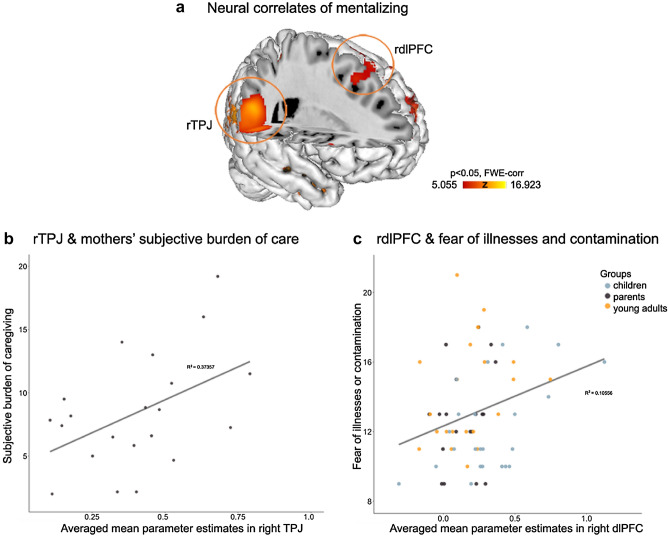
Across all participants, the neural correlates of mentalizing corresponded to brain regions previously associated with Theory of Mind24, including bilateral temporoparietal and prefrontal regions or precuneus (see peak activation reports and figure in Supplementary Table S3, Supplementary Figure S2). The multiple regression analysis revealed that activation assessed prior to Covid-19 during mentalizing in right dorsolateral prefrontal cortex was a predictor of later development of fear about illness or contamination (ß = 0.334, t(60) = 2.661, p = 0.010) constituting a significant model where dlPFC activation explained 13.9% of the variance in later reports of fear about illness or contamination (R2 = 0.139; adjusted R2 = 0.096; F(3,60) = 3.221, p = 0.029; including the covariates age and sex). Right temporoparietal junction did not enter the model as a significant predictor. When assessing the relationship between mentalizing-related activation and subjective burden, the right temporoparietal junction emerged as a significant predictor of burden (ß = 0.623, t(18) = 3.276, p = 0.004), while the dorsolateral cortex did not enter into the model. The complete model explained 41.9% of the variation in subjective burden (R2 = 0.419; adjusted R2 = 0.355; F(2,18) = 6.493, p = 0.008; including age as a covariate; Fig. 5).
Figure 5.
Functional brain correlates of mentalizing as assessed prior to Covid-19 onset and their associations with subjective burden and fear of illnesses and contamination reported during the early months of Covid-19. (a) Brain rendering for the neural correlates of mentalizing (Theory of Mind > control) across all participants (corrected for age and sex and whole brain FWE-corrected; regions of interest in right TPJ and dlPFC are circled in red). (b) Association between mean parameter scores during mentalizing in right TPJ and subjective burden of caregiving in mothers and (c) association of mean parameter scores in right dlPFC and fear of illnesses and contamination across all participants.
Discussion
We describe data on a small, but extensively characterized group of children and adults (N = 69, 41♀, age range = 7–51 years, including 26 children and their mothers), with reports across eight waves of testing, including seven assessment timepoints during the early months after Covid-19 onset in Switzerland and one assessment prior to the pandemic onset. Our findings report on mental well-being and psychosocial functioning in children and adults. The prevalence of clinically significant anxiety was 34.88%, and a 32.56% prevalence of subthreshold depression symptoms was observed across the 11 weeks. Caregiver burden was in the moderate ranges. Overall, scores of depression, anxiety and caregiver burden decreased over the course of the 11 weeks investigated. In children pre-pandemic levels of emotional and behavioral problems did not differ significantly from the average of the 11-week period during restrictions. Scores of conduct problem, hyperactivity, peer problems and overall emotional and behavioral problems in children decreased across time after Covid-19 onset. Well-being in mothers predicted mood and emotional and behavioral problems in children. In children meeting friends was a significant predictor of mood during restrictions. Additionally, neural correlates of mentalizing in prefrontal, but not temporoparietal regions, preceded the development of fear about contamination and illness across all participants. In mothers, higher neural activation in temporoparietal, but not frontal, regions during mentalizing preceded higher reports of subjective burden of care during restrictions. This may indicate that higher tendency to mentalize, usually considered beneficial for social interactions49 and favorable when present in mother–child dyads50, can be negatively associated with socioemotional functioning during prolonged stress.
Child behavior as measured by the SDQ or CBCL showed no difference when comparing pre-pandemic scores to those during restrictions, which is in line with longitudinal reports7 observing a relatively stable level of problem behaviors after Covid-19 onset. Based on parental reports conduct problems, hyperactivity, peer problems and the overall level of emotional and behavioral problems decreased across time in the child group studied here. Emotional problems and prosocial behavior showed no significant changes during the 11-weeks assessment period. Additionally, children’s time spent outside, and mood varied significantly. Variations in mood scores may be explained by several public holidays (Easter) around mid-restrictions. It may be possible that time spent outside during vacation allowed the meeting of friends, which was a relevant variable for increases in mood in children. Prior evidence highlights that prolonged school closure or restrictive measures are detrimental to children’s physical and mental health and can have long-lasting consequences14. Conversely, the present study did not identify significant changes for emotional and behavioral problems of the children comparing pre- and post-pandemic onset levels. Our findings further indicate that meeting friends predicted better mood, which is in line with prior evidence emphasizing the importance of friendships and peer relationships in developmental groups11,45.
Quantitative measures obtained were further supported by qualitative reports, which provide a unique insight into children’s values and further highlight sources of resilience. More specifically, children mentioned more time for leisure, sleep, family, and friends or less stress or exams as positive attributes of school closure. Negative mentions centered around restrictions affecting social contacts, prohibiting hobbies or sports, or increased stress and conflict. Interestingly, across two time points, positive mentions about returning to schools across all children solely focused on social domains (e.g., meeting friends, class, teachers again or in-person schooling), whereas negative mentions included less sleep, less free time or increased stress and homework, or restrictions. Themes reported were in line with findings of qualitative reports during Covid-1911,45.
Anxiety, depression and caregiver burden was high amongst adults with scores decreasing across the 11-week assessment period. Clinically significant levels of anxiety were reached at the beginning and after 7 weeks of restrictions. Furthermore, the 11-week prevalence of anxiety was 34.88%. An increase in anxiety due to Covid-19 and related restrictions has been reported previously2,5,8,51, however, missing pre-pandemic scores hindered a direct investigation in the present group. Mixed-effects models reflected a decrease of anxiety scores across the first months after Covid-19 onset, which is in line with similar longitudinal studies indicating a decrease following a significant early impact in affect2,51. Similarly, a decrease in depressive symptomatology was observed. While group average scores of depression were in the normal range, it is notable that 32.56% of all adults reported heightened depressive symptoms and 4.65% qualified for a major depressive episode at least once. These observations mirror reports of heightened depression scores in the general population during Covid-19 (e.g., retrospective reports2 or longitudinal data6). Mothers reported elevated levels of subjective burden of care (in the moderate range), which is in line with similar studies investigating parental burden during Covid-1952. Notably, a moderate burden of care has been associated with elevated risk for physical, psychosomatic, or mental health problems39,52, indicating the need for parental programs mitigating possible stress-related health consequences. The experienced subjective burden of care decreased across the early months of investigation. Distress and general health, however, did not significantly change. Longitudinal studies to date have either reported a decrease or stagnation of depression or anxiety levels for the early months following Covid-19 onset across different countries2,29,53. Loosen et al.29 for example suggest that such decreases in stress-related symptoms can partly be explained by adaptation, a phenomenon well-described in stress research54. Overall, first meta-analyses of studies compiling pre-/post mental health data report significant, but only small effects on anxiety and depression in adults55. Participant reports reflected significant changes in news consumption, reporting a higher amount of news consumed at the beginning and lower scores towards the end of the assessment period. Sex, news consumption, time spent outside or parenthood were not associated with variations in scores of anxiety, depression or distress in adults. This is somewhat surprising given prior evidence of the impact of each of these variables on mental well-being during Covid-19 (gender and parenting44; news consumption2; time spent outside45).
In the present study, mother–child variables were positively associated. Subjective burden of caregiving in mothers predicted emotional and behavioral problems in children, while anxiety and depression did not. This indicates that higher burden in mothers was linked to more problem behaviors in children. It is important to mention though that emotional and behavioral problems in the child were reported by the mother, thus reporting bias can’t be excluded. We further investigated the effect of the mothers’ well-being on children’s self-reported mood, demonstrating that elevated depression in mothers was associated with children’s mood ratings. Dyadic relationships are a primary vehicle for children’s learning9. While commonly a driver of positive effects, it may also lead to negative consequences, as demonstrated in the example of vicarious conditioned fear learning in parent–child dyads56. We thus hypothesize, that negative mental health in adults may negatively impact children’s well-being, possibly through learnt maladaptive coping or contagion. Increased parental stress and anxiety may lead to parental burnout13 or increased aggression15. Intergenerational care during early years lays the foundation for healthy social skill development57 and systemic mental health intervention programs commonly draw from this relationship58. Our data point towards a support of programs investing in increased parental support, which are expected to influence children’s well-being positively.
The neural correlates of mentalizing as measured prior to the pandemic in prefrontal, but not temporoparietal brain regions, preceded the development of fear about contamination and illness in all participants. In mothers, higher neural activation during mentalizing in temporoparietal, but not frontal regions was associated with higher burden of caregiving during restrictions. Activation increases in the right temporoparietal junction are commonly reported as a response to tasks of mentalizing, as this area selectively responds to observed social interactions59 and is part of the so-called paternal caregiver brain network60. Prefrontal areas are similarly engaged during tasks of mentalizing and are crucial for cognitive control processes10. Our data indicate that neural activation during mentalization in prefrontal cortex prior to Covid-19 may precede the development of fear of contamination and illnesses in both children and adults. The assessment of fear about contamination and illness required participants to make statements relating to the likelihood of oneself, a parent, a pet, or someone else in the world becoming sick and/or dying because of a virus or illness. Activation increases in prefrontal cortex have been linked to psychological state attributions, independent of whether they affect oneself, a relative, imagined people or animals61 or cognitive control (i.e., emotion regulation). A higher tendency to think about other people’s well-being, as reflected by higher mentalization-related activation in the prefrontal cortex, may thus be linked to the likelihood of developing fear about contamination and illness affecting ourselves and others.
Overall, better mentalizing has been associated with higher social competence, psychological and physiological functioning22, while impairments have been associated with stress and depression23. Increased mentalizing skills in caregivers are beneficial for child development. For example, parental mentalization has been positively associated with regulatory skills in children62,63, which may be protective during stressful life events43. However, the opposite effect may occur during stressful situations17. Higher levels of empathy in parents have for example been linked to better psychological and physiological health of their children, but also higher levels of inflammatory markers in the parents63. Moreover, higher levels of mentalizing abilities were shown to be associated with higher cortisol and heart rate reactivity in stressful situations64. This may temporarily be beneficial but may have a long-term negative impact depending on the intensity and duration of negative events. Our data indicate that mentalization can be negatively associated with increased burden and fear development in prolonged stressful situations.
In the present example, extensive phenotyping within individuals allow a comprehensive view and an opportunity to assess effects of time within individuals. Although the presented findings mostly align with Covid-19 literature they should be considered with caution due to the relatively small group size and less comprehensive pre-pandemic health measures. Research on the existence of potential subgroups will have to be further examined using larger and more diverse populations. An indication for possible subgroups reacting differently to stressful life events as associated with pandemics include reports of children that may in fact benefit or even thrive during restrictions7. A more detailed understanding of subgroups of individuals that are differently affected may increase opportunities to select the best fitting individualized treatments or prevention. Assessing direct subjective experience of the severity of impact by Covid-19 and associated restrictions would have been a valuable addition. Moreover, as the pre-pandemic assessment did not include comparable measures of mental health in the adult group, it is difficult to disentangle the effect of Covid-19 and related restrictions from pre-existing mental health symptoms. It remains to be investigated how far-reaching the herein observed negative effects on well-being are. Past work has indicated that early adversities can have an impact for life, with effects potentially being most significant in younger age and depending on the intensity of the experience65. An increased understanding of protective and/or risk factors and mechanisms leading to the development of stress-related psychopathologies may ultimately hold the potential to facilitate more personalized prevention and treatment strategies.
Supplementary Information
Acknowledgements
This study was funded through a Jacobs Foundation Early Career Research Grant (NMR; Nr. 2016201713). PD and NMR received funds through the Zurich Neuroscience Network. None of the authors have any disclosure/conflict of interest to report. We would like to express our gratitude to all the families, children and adults that have participated in our research.
Author contributions
N.M.R conceived the experiments. N.M.R., L.V.F., P.D. and R.B. designed, implemented, and conducted the experiments. R.B., A.N., J.A., L.V.F., and N.M.R. analyzed the results. N.M.R, R.B. and C.B.S. wrote the manuscript and each author reviewed the manuscript. All authors have made an important scientific contribution to the manuscript.
Data availability
Behavioral mean scores are included in the manuscript and neuroimaging data is provided through NeuroVault (https://identifiers.org/neurovault.collection:9780). Further information or data may be obtained from the corresponding author.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-96852-0.
References
- 1.Kwong AS, et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. British J Psychiatry. 2021;218:334–343. doi: 10.1192/bjp.2020.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Quervain, D. et al. The Swiss Corona Stress Study. (2020).
- 3.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J. Health Soc. Behav. 1981;22:337–356. doi: 10.2307/2136676. [DOI] [PubMed] [Google Scholar]
- 4.Shanahan L, et al. Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020;1:1–10. doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saude Publica. 2020;36:e00054020. doi: 10.1590/0102-311x00054020. [DOI] [PubMed] [Google Scholar]
- 6.Ettman CK, et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3:e2019686–e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Achterberg M, Dobbelaar S, Boer OD, Crone EA. Perceived stress as mediator for longitudinal effects of the COVID-19 lockdown on wellbeing of parents and children. Sci. Rep. 2021;11:1–14. doi: 10.1038/s41598-021-81720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atzil S, Gao W, Fradkin I, Barrett LF. Growing a social brain. Nat. Hum. Behav. 2018;2:624–636. doi: 10.1038/s41562-018-0384-6. [DOI] [PubMed] [Google Scholar]
- 10.Blakemore S-J. The social brain in adolescence. Nat. Rev. Neurosci. 2008;9:267–277. doi: 10.1038/nrn2353. [DOI] [PubMed] [Google Scholar]
- 11.Chu, K., Schwartz, C., Towner, E., Kasparian, N. A. & Callaghan, B. Parenting under pressure: A mixed-methods investigation of the impact of COVID-19 on family life. J Affect Disord R, 100161 (2021). [DOI] [PMC free article] [PubMed]
- 12.Nolvi, S. et al. Parental depressive and anxiety symptoms as a response to the COVID-19 pandemic: A birth cohort follow-up study. (2020).
- 13.Marchetti D, et al. Parenting-related exhaustion during the Italian COVID-19 lockdown. J. Pediatr. Psychol. 2020;45:1114–1123. doi: 10.1093/jpepsy/jsaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgül E, Kallitsoglou A, Essau CAE. Psychological effects of the COVID-19 lockdown on children and families in the UK. Revista de Psicología Clínica con Niños y Adolescentes. 2020;7:42–48. [Google Scholar]
- 15.McRae, C., Henderson, A. M., Low, R., Chang, V. & Overall, N. Parents’ distress and poor parenting during COVID-19: The buffering effects of partner support and cooperative coparenting. (2020). [DOI] [PubMed]
- 16.Thompson, R. A. Socioemotional development. Vol. 36 (U of Nebraska Press, 1990).
- 17.Sharp C, Fonagy P, Allen JG. Posttraumatic stress disorder: A social-cognitive perspective. Clin. Psychol. Sci. Pract. 2012;19:229–240. doi: 10.1111/cpsp.12002. [DOI] [Google Scholar]
- 18.Coyl-Shepherd DD, Hanlon C. Family play and leisure activities: Correlates of parents' and children's socio-emotional well-being. Int. J. Play. 2013;2:254–272. doi: 10.1080/21594937.2013.855376. [DOI] [Google Scholar]
- 19.Eisenberg N, et al. The relations of regulation and emotionality to children's externalizing and internalizing problem behavior. Child Dev. 2001;72:1112–1134. doi: 10.1111/1467-8624.00337. [DOI] [PubMed] [Google Scholar]
- 20.Calkins, S. D. & Hill, A. Caregiver influences on emerging emotion regulation. Handb. Emot. Regul.229248 (2007).
- 21.Frith C, Frith U. Theory of mind. Curr. Biol. 2005;15:R644–R645. doi: 10.1016/j.cub.2005.08.041. [DOI] [PubMed] [Google Scholar]
- 22.Devine RT, White N, Ensor R, Hughes C. Theory of mind in middle childhood: Longitudinal associations with executive function and social competence. Dev. Psychol. 2016;52:758. doi: 10.1037/dev0000105. [DOI] [PubMed] [Google Scholar]
- 23.Fischer-Kern M, et al. Mentalizing in female inpatients with major depressive disorder. J. Nerv. Ment. Dis. 2013;201:202–207. doi: 10.1097/NMD.0b013e3182845c0a. [DOI] [PubMed] [Google Scholar]
- 24.Molenberghs P, Johnson H, Henry JD, Mattingley JB. Understanding the minds of others: A neuroimaging meta-analysis. Neurosci. Biobehav. Rev. 2016;65:276–291. doi: 10.1016/j.neubiorev.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Tugade MM, Fredrickson BL. Regulation of positive emotions: Emotion regulation strategies that promote resilience. J. Happiness Stud. 2007;8:311–333. doi: 10.1007/s10902-006-9015-4. [DOI] [Google Scholar]
- 26.Megreya AM, Al-Attiyah AA, Moustafa AA, Hassanein EE. Cognitive emotion regulation strategies, anxiety, and depression in mothers of children with or without neurodevelopmental disorders. Res. Autism Spectr. Disord. 2020;76:101600. doi: 10.1016/j.rasd.2020.101600. [DOI] [Google Scholar]
- 27.Moriguchi Y, et al. Impaired self-awareness and theory of mind: An fMRI study of mentalizing in alexithymia. Neuroimage. 2006;32:1472–1482. doi: 10.1016/j.neuroimage.2006.04.186. [DOI] [PubMed] [Google Scholar]
- 28.Fonagy P, Bateman A. The development of borderline personality disorder—A mentalizing model. J. Pers. Disord. 2008;22:4–21. doi: 10.1521/pedi.2008.22.1.4. [DOI] [PubMed] [Google Scholar]
- 29.Loosen AM, Skvortsova V, Hauser TU. Obsessive–compulsive symptoms and information seeking during the Covid-19 pandemic. Transl. Psychiatry. 2021;11:1–10. doi: 10.1038/s41398-021-01410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borbás R, Fehlbaum LV, Rudin U, Stadler C, Raschle NM. Neural correlates of theory of mind in children and adults using CAToon: Introducing an open-source child-friendly neuroimaging task. Dev. Cogn. Neurosci. 2021;49:100959. doi: 10.1016/j.dcn.2021.100959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI) Br. J. Clin. Psychol. 1992;31:301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 32.Schmitt, A. German version of the Center for Epidemiologic Studies Depression Scale Revised (CESD-R). (2016).
- 33.Schrnitz N, Kruse J, Tress W. Psychometric properties of the General Health Questionnaire (GHQ-12) in a German primary care sample. Acta Psychiatr. Scand. 1999;100:462–468. doi: 10.1111/j.1600-0447.1999.tb10898.x. [DOI] [PubMed] [Google Scholar]
- 34.Kessler R, Mroczek D. Final versions of our non-specific psychological distress scale. Memo Dated March. 1994;10:199. [Google Scholar]
- 35.Abler B, Kessler H. Emotion regulation questionnaire–Eine deutschsprachige Fassung des ERQ von Gross und John. Diagnostica. 2009;55:144–152. doi: 10.1026/0012-1924.55.3.144. [DOI] [Google Scholar]
- 36.Goodman R. The strengths and difficulties questionnaire: A research note. J. Child Psychol. Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 37.Achenbach TM, Ruffle TM. The child behavior checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr. Rev. 2000;21:265–271. doi: 10.1542/pir.21-8-265. [DOI] [PubMed] [Google Scholar]
- 38.Emons W, Habibović M, Pedersen S. Prevalence of anxiety in patients with an implantable cardioverter defibrillator: Measurement equivalence of the HADS-A and the STAI-S. Qual. Life Res. 2019;28:3107–3116. doi: 10.1007/s11136-019-02237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pendergrass A, Malnis C, Graf U, Engel S, Graessel E. Screening for caregivers at risk: Extended validation of the short version of the burden scale for family caregivers (BSFC-s) with a valid classification system for caregivers caring for an older person at home. BMC Health Serv. Res. 2018;18:1–9. doi: 10.1186/s12913-018-3047-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buuren SV, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2010;45:1–68. [Google Scholar]
- 41.Bates, D., Maechler, M. & Bolker, B. (Vienna, 2012).
- 42.Luke SG. Evaluating significance in linear mixed-effects models in R. Behav. Res. Methods. 2017;49:1494–1502. doi: 10.3758/s13428-016-0809-y. [DOI] [PubMed] [Google Scholar]
- 43.Kuznetsova, A., Brockhoff, P. & Christensen, R. (2014).
- 44.Huebener M, Waights S, Spiess CK, Siegel NA, Wagner GG. Parental well-being in times of Covid-19 in Germany. Rev. Econ. Househ. 2020;19:1–32. doi: 10.1007/s11150-020-09529-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Idoiaga Mondragon N, Berasategi Sancho N, Dosil Santamaria M, Eiguren Munitis A. Struggling to breathe: A qualitative study of children’s wellbeing during lockdown in Spain. Psychol. Health. 2021;36:179–194. doi: 10.1080/08870446.2020.1804570. [DOI] [PubMed] [Google Scholar]
- 46.Brett, M., Anton, J.-L., Valabregue, R. & Poline, J.-B. in 8th international conference on functional mapping of the human brain. 497 (Sendai).
- 47.Fehlbaum, L., Borbás, R., Paul, K. & Raschle, N. Early continuity in neuronal correlates of mentalizing: ALE meta-analyses in adults, children and youths. (2020). [DOI] [PMC free article] [PubMed]
- 48.Riaz M, Abid M, Bano Z. Psychological problems in general population during covid-19 pandemic in Pakistan: Role of cognitive emotion regulation. Ann. Med. 2021;53:189–196. doi: 10.1080/07853890.2020.1853216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Caputi M, Lecce S, Pagnin A, Banerjee R. Longitudinal effects of theory of mind on later peer relations: The role of prosocial behavior. Dev. Psychol. 2012;48:257. doi: 10.1037/a0025402. [DOI] [PubMed] [Google Scholar]
- 50.Camoirano A. Mentalizing makes parenting work: A review about parental reflective functioning and clinical interventions to improve it. Front. Psychol. 2017;8:14. doi: 10.3389/fpsyg.2017.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. The Lancet Psychiatry . 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Russell B, Hutchison M, Tambling R, Tomkunas A, Horton A. Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent–child relationship. Child Psychiatry Hum. Dev. 2020;51:671–682. doi: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.O'Connor RC, et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health and Wellbeing study. Br. J. Psychiatry. 2021;218:326–333. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lazarus, R. S. Psychological stress and the coping process. (1966).
- 55.Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021;51:1–11. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marin M-F, et al. Vicarious conditioned fear acquisition and extinction in child–parent dyads. Sci. Rep. 2020;10:1–10. doi: 10.1038/s41598-020-74170-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bridgett DJ, Burt NM, Edwards ES, Deater-Deckard K. Intergenerational transmission of self-regulation: A multidisciplinary review and integrative conceptual framework. Psychol. Bull. 2015;141:602. doi: 10.1037/a0038662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marcus BA, Swanson V, Vollmer TR. Effects of parent training on parent and child behavior using procedures based on functional analyses. Behav. Interv. 2001;16:87–104. doi: 10.1002/bin.87. [DOI] [Google Scholar]
- 59.Saxe, R. The right temporo-parietal junction: a specific brain region for thinking about thoughts. Handbook of theory of mind, 1–35 (2010).
- 60.Feldman R, Braun K, Champagne FA. The neural mechanisms and consequences of paternal caregiving. Nat. Rev. Neurosci. 2019;20:205–224. doi: 10.1038/s41583-019-0124-6. [DOI] [PubMed] [Google Scholar]
- 61.Baetens K, Ma N, Steen J, Van Overwalle F. Involvement of the mentalizing network in social and non-social high construal. Soc. Cogn. Affect. Neurosci. 2014;9:817–824. doi: 10.1093/scan/nst048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Senehi N, Brophy-Herb HE, Vallotton CD. Effects of maternal mentalization-related parenting on toddlers’ self-regulation. Early Child. Res. Q. 2018;44:1–14. doi: 10.1016/j.ecresq.2018.02.001. [DOI] [Google Scholar]
- 63.Manczak EM, DeLongis A, Chen E. Does empathy have a cost? Diverging psychological and physiological effects within families. Health Psychol. 2016;35:211. doi: 10.1037/hea0000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tollenaar MS, Overgaauw S. Empathy and mentalizing abilities in relation to psychosocial stress in healthy adult men and women. Heliyon. 2020;6:e04488. doi: 10.1016/j.heliyon.2020.e04488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nelson CA, et al. Adversity in childhood is linked to mental and physical health throughout life. BMJ. 2020;371:m3048. doi: 10.1136/bmj.m3048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Behavioral mean scores are included in the manuscript and neuroimaging data is provided through NeuroVault (https://identifiers.org/neurovault.collection:9780). Further information or data may be obtained from the corresponding author.