Abstract
Recent studies have shown reduced physical activity at early stages of the COVID-19 pandemic. However, there is a lack of investigation on longitudinal changes in physical activity beyond lockdowns and stay-at-home orders. Moreover, it is unclear if there is heterogeneity in physical activity growth trajectories. This study aimed to explore longitudinal patterns of physical activity and factors associated with them. Data were from the UCL COVID-19 Social Study. The analytical sample consisted of 35,915 adults in England who were followed up for 22 weeks from 24th March to 23rd August 2020. Data were analysed using growth mixture models. Our analyses identified six classes of growth trajectories, including three stable classes showing little change over time (62.4% in total), two classes showing decreasing physical activity (28.6%), and one class showing increasing physical activity over time (9%). A range of factors were found to be associated the class membership of physical activity trajectories, such as age, gender, education, income, employment status, and health. There is substantial heterogeneity in longitudinal changes in physical activity during the COVID-19 pandemic. However, a substantial proportion of our sample showed persistent physical inactivity or decreasing physical activity. Given the well-established link between physical activity and health, persistent or increased physical inactivity is likely to have both immediate and long-term implications for people’s physical and mental health, as well as general wellbeing. More efforts are needed to promote physical activity during the pandemic and beyond.
Subject terms: Risk factors, Public health
Introduction
There is extensive evidence on the positive impacts of physical activity for both physical and mental health. For example, regular physical activity is associated with reduced rates of all-cause mortality, obesity, cancer, cardiovascular disease, stroke, and diabetes, among other physical conditions, as well as depression, anxiety, and other mental health problems1–4. Regular physical activity also leads to improvements in cardiorespiratory and muscular fitness, functional health, cognitive function, wellbeing, and quality of life1,3,5. However, levels of physical inactivity are rising in many countries3. Physical inactivity is the fourth leading risk factor for global mortality6, causing 9% of premature mortality worldwide7. Physical inactivity is also one of the most important risk factors for chronic diseases globally8–11. Even short-term physical inactivity, over a period of 1–4 weeks, has been associated with negative changes in cardiovascular function and increased cardiovascular risk factors12,13.
Since December 2019, there has been an outbreak of coronavirus disease (COVID-19). Lockdowns and stay-at-home orders have been announced globally to control the spread of the disease, disrupting people’s usual behaviours. In many countries, this has involved the closure of non-essential businesses, including gyms, outdoor sports amenities, and playgrounds, as well as limits placed on how often people could leave their homes each day. However, how this has affected physical activity levels has been complex. Large cross-sectional surveys in many western countries have suggested decreases in overall physical activity when comparing self-reports of activity levels before to during lockdowns14–25. The majority of longitudinal studies to date also show an initial drop in physical activity levels at the start of lockdown restrictions14,26–31, as do data from wearable fitness trackers in a number of countries32–35. However, some wearable fitness tracker studies suggest that activity levels may not have uniformly decreased across populations32–35. Further, following an initial decrease in activity levels as lockdowns first came in, population-level data on the frequency of google searches for terms related to ‘exercise’ compared to ‘television show’ significantly increased in some countries such as the UK even after adjusting for increased interest in television shows36. This suggests that the effects of lockdowns and broader social restrictions on physical activity may be more nuanced.
Additionally, studies examining longer-term impacts on physical activity have provided mixed findings on whether physical activity returned to pre-lockdown levels with the initial easing of restrictions in the UK26,27,30,31. To our knowledge, no studies have investigated changes in physical activity after further easing of restrictions in the UK in July 2020. The longer term impacts of lockdown measures on physical activity therefore remains unclear, yet it is a crucial question to identify whether short-term disruptions to physical activity behaviours lead to long-term changes that could have adverse effects on health. Moreover, studies to date have assumed one homogeneous trajectory of physical activity, without exploring the heterogeneous patterns of longitudinal changes. This is also vital to understand, as different people may have reacted differently to the pandemic and lockdown measures and therefore be at a higher or lower risk of sustained changes to their physical activity levels. Some studies have been exploring factors likely to influence physical activity levels. Being women, younger, single, a parent, and from an ethnic minority group as well as having poor health, lower education and income, and no access to outside space have been associated with lower physical activity during lockdowns27,28,31,32,37–43. There is also some evidence that physical activity habits prior to the onset of the COVID-19 pandemic are associated with changes in physical activity at the start of lockdown14,26,29,38,44–48. However, some findings have been inconsistent, and many studies have only examined physical activity at one point early in the pandemic. It therefore remains unclear whether similar factors are associated with the subsequent trajectories of physical activity throughout lockdown and the easing of restrictions.
Consequently, this study set out to examine the heterogeneity in the longitudinal changes of physical activity in England, using a large sample of 35,915 adults tracked across 22 weeks from the 24th March to 23rd August 2020 encompassing a strict lockdown followed by the easing of restrictions. Further, it sought to explore sociodemographic and health-related factors that might be associated with different patterns of longitudinal changes in physical activity. Given the well-established health benefits of physical activity, understanding changes in physical activity habits, and predictors of these changes, is essential for informing healthcare policy in the aftermath of COVID-19.
Method
Study design and participants
This study analysed data from the COVID-19 Social Study, a longitudinal study run by University College London (UCL) that focuses on the psychological and social experiences of adults living in the UK during the COVID-19 pandemic. The study commenced on 21st March 2020 and involved weekly online data collection from participants until 23rd August 2020, followed by monthly data collection for the duration of the pandemic. The study did not use a random sample design, but it does contain a heterogeneous sample that was recruited using three primary approaches. First, convenience sampling was used, including promoting the study through existing networks and mailing lists (including large databases of adults who had previously consented to be involved in health research across the UK), print and digital media coverage, and social media. Second, more targeted recruitment was undertaken focusing on (1) individuals from a low-income background, (2) individuals with no or few educational qualifications, and (3) individuals who were unemployed. Third, the study was promoted via partnerships with third sector organisations to vulnerable groups, including adults with pre-existing mental health conditions, older adults, carers, and people experiencing domestic violence or abuse. A full protocol for the study is available online at www.COVIDSocialStudy.org.
To examine trajectories of physical activity in relation to specific lockdown measures, we focused solely on participants who lived in England (N = 56,428). We included participants who had at least three repeated measures between 24th March 2020, the day after the first lockdown started in the UK, and August 23rd 2020, when the survey switched to monthly follow-up and the relevant measure was discontinued. This period encompasses the first national lockdown followed by the easing of restrictions allowing unlimited outdoor exercises (13th May 2020), reopening outdoor gyms and playgrounds (4th July 2020) and indoor gyms and swimming pools (25th July 2020). These criteria provided us with data from 38,917 participants who were followed up for a maximum of 22 weeks. After excluding participants with missing values (8%), our final analytic sample size was 35,915.
Measures
In the UCL COVID-19 Social Study, participants were asked weekly how long they had spent on the last working day (1) going out for a walk or other gentle physical activity, (2) going out for moderate or high intensity activity (e.g. running, cycling or swimming), (3) exercising inside their home or garden (e.g. doing yoga, weights or other indoor exercise). Responses were recorded on a five-point frequency scale: did not do, < 30 min, 30 min–2 h, 3–5 h and ≥ 6 h. We generated a composite physical activity measure by using the highest response across these three questions, which was recoded into four categories: (1) did not do, (2) < 30 min, (3) 30 min–2 h and (4) ≥ 3 h. For instance, if a participant walked for ≥ 3 h, did high intensity activity for 30 min–2 h, and did not exercise at home, they would be coded as ≥ 3 h. As the physical activity questions referred to the last working day, and the first national lockdown started on 23rd March 2020, we included responses from 24th March 2020 onwards.
A range of socio-demographic and health-related factors were considered as potential predictors of physical activity trajectories. These included gender (women, men), ethnicity (white, ethnic minorities), age groups (18–29, 30–45, 46–59, 60+ years), education (General Certificate of Secondary Education (GCSE) or below, Advanced Level qualifications (A-levels) or equivalent, and university degree or above), household income (< £30,000, ≥ £30,000 per annum), employment status (employed throughout, employed at baseline but lost job during the follow-up, unemployed or economically inactive), living arrangement (living alone, living with others but no children, living with others including children), and area of living (city, large town, small town, rural). Health-related factors were self-reported diagnosis of any long-term physical health condition, including disability (yes, no), and self-reported diagnosis of any long-term mental health condition (yes, no).
Statistical analysis
Data were analysed using the growth mixture modelling (GMM) approach. The conventional growth modelling approach assumes one homogeneous growth trajectory, allowing individual growth factors to vary randomly around the overall mean. GMM relaxes this assumption and enables researchers to explore different patterns of change (latent trajectory classes)49.
We included a polynomial time function to allow for nonlinear growth trajectories informed by the data. Starting with the unconditional GMM, we compared models with different number of classes on the basis of the Bayesian information criterion (BIC) and sample-size adjusted Bayesian information criterion (ABIC), along with the Vuong-Lo-Mendell-Rubin likelihood ratio (LMR-LR) test and Adjusted Lo-Mendell-Rubin likelihood ratio (ALMR-LR) test. After identifying the optimal number of classes, we introduced predictors to explain the observed heterogeneity between classes.
Weights were applied throughout the analyses. The final analytical sample was weighted to the proportions of gender, age, ethnicity and education in the English population obtained from the Office for National Statistics17. The main analyses were implemented in Mplus Version 8.
Ethics approval and consent to participate
The COVID-19 Social Study was approved by the UCL Research Ethics Committee [12467/005]. All methods were performed in accordance with the relevant guidelines and regulations, and all participants gave informed consent.
Results
Descriptive
The analytical sample comprised 35,915 participants of whom 75.6% were women, and there was an over-representation of people with a degree or above (70.3%) and an underrepresentation of people from ethinic minority backgrounds (5%; Table 1). Younger adults under 30 years of age were also underrepresented in the sample. After weighting, the sample reflected population proportions, with 51% women, 34.7% participants with a degree or above, 14.5% participants being ethnic minortiy and 19.5% aged under 30.
Table 1.
Characteristics of the sample (N = 35,915).
| Raw data | Weighted data | |||
|---|---|---|---|---|
| Percent (%) | N | Percent (%) | N | |
| Gender | ||||
| Women | 75.9 | 27,245 | 51.0 | 18,330 |
| Men | 24.1 | 8670 | 49.0 | 17,585 |
| Ethnicity | ||||
| Minority | 5.0 | 1796 | 14.5 | 5223 |
| White | 95.0 | 34,119 | 85.5 | 30,692 |
| Age | ||||
| 18–29 | 7.4 | 2656 | 19.5 | 7012 |
| 30–45 | 29.0 | 10,431 | 26.4 | 9483 |
| 46–59 | 33.0 | 11,858 | 24.1 | 8657 |
| 60 + | 30.5 | 10,970 | 30.0 | 10,763 |
| Education | ||||
| GCSE or below | 12.9 | 4636 | 32.5 | 11,656 |
| A-levels or equivalent | 16.8 | 6031 | 32.9 | 11,807 |
| Degree or above | 70.3 | 25,248 | 34.7 | 12,452 |
| Household income | ||||
| < 30 k | 36.7 | 13,193 | 46.0 | 16,519 |
| ≥ 30 k | 63.3 | 22,722 | 54.0 | 19,396 |
| Employment status | ||||
| Employed | 55.7 | 19,988 | 49.0 | 17,587 |
| Employed to unemployed | 10.4 | 3724 | 10.1 | 3636 |
| Unemployed/economically inactive | 34.0 | 12,203 | 40.9 | 14,692 |
| Living status | ||||
| Alone | 19.8 | 7100 | 18.3 | 6577 |
| With others (not children) | 53.2 | 19,106 | 56.2 | 20,168 |
| With others (including children) | 27.0 | 9709 | 25.5 | 9169 |
| Area of living | ||||
| City | 35.4 | 12,717 | 34.8 | 12,503 |
| Large town | 19.1 | 6859 | 21.8 | 7817 |
| Small town | 24.8 | 8916 | 24.4 | 8770 |
| Rural area | 20.7 | 7423 | 19.0 | 6825 |
| Long term physical illness | ||||
| Yes | 39.2 | 14,086 | 40.8 | 14,651 |
| No | 60.8 | 21,829 | 59.2 | 21,264 |
| Long term mental illness | ||||
| Yes | 18.3 | 6578 | 20.0 | 7186 |
| No | 81.7 | 29,337 | 80.0 | 28,729 |
Figure 1 shows how the proportion of the sample in each physical activity category changed over the course of 22 weeks from the start of lockdown in March 2020. We observed a steady increase in the percentage of people who reported not having done any physical activity. The percentage of people who exercised for three hours or more also slightly increased in the first 10 weeks, but this then decreased and stablised. Notably, there is little evidence that the prevalence of physical activity as a whole showed sudden, concurrent changes with major adjustments in lockdown measures (as indicated by the vertical lines and dates in Fig. 1).
Figure 1.
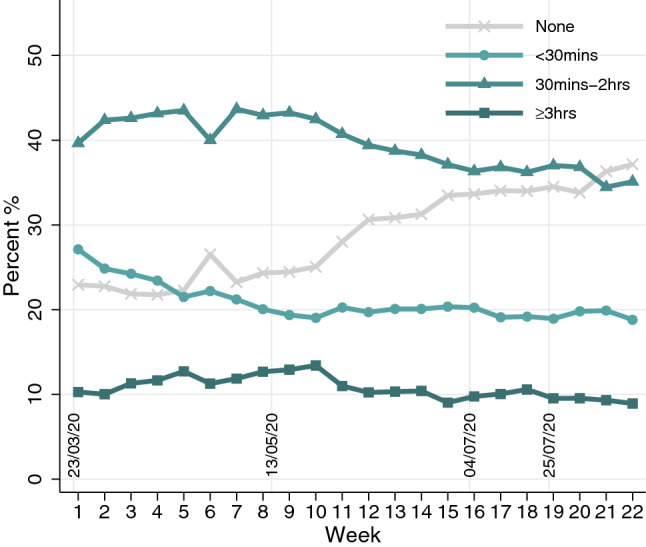
Descriptive changes of physical activity over 22 weeks. On March 23, 2020, the first lockdown commenced in England. All non-essential businesses, including gyms, outdoor sports amenities, and playgrounds were closed. On May 10, 2020, it was announced that strict lowdown was being eased, with unlimited outdoor exercise being allowed from May 13, 2020. On July 4, further public amenities were reopened, including outdoor gyms and playgrounds. On July 25, 2020, indoor gyms and swimming pools reopened.
Latent trajectory classes
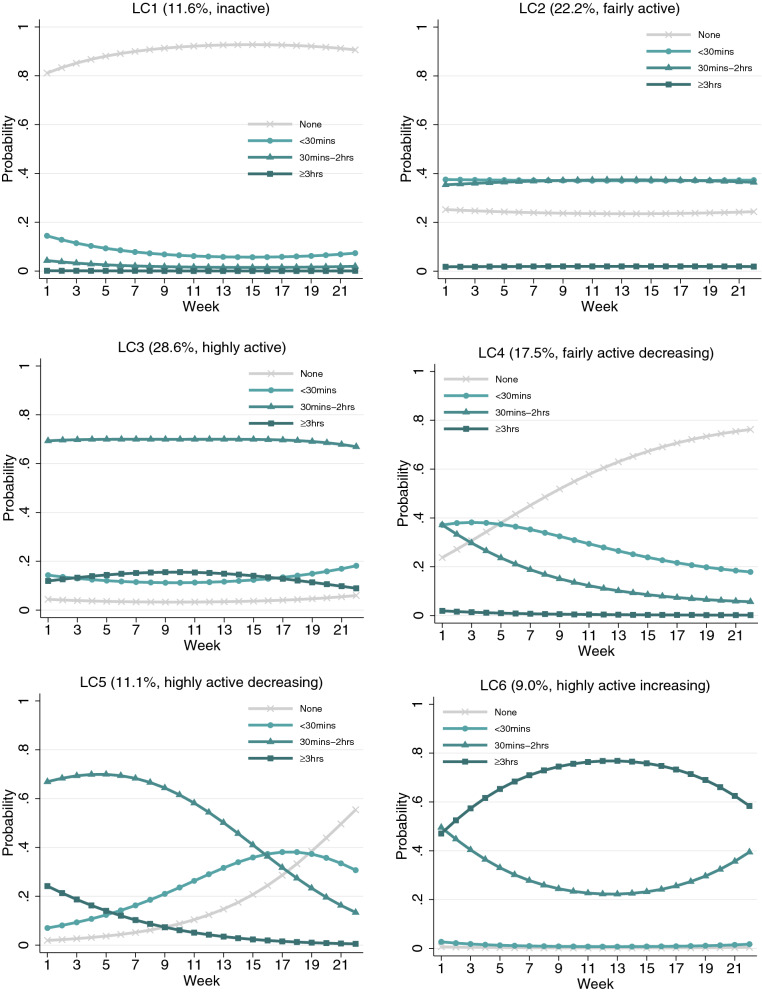
To determine the optimal number of latent trajectory classes, we estimated and compared across unconditional GMMs with different numbers of classes. Although the BIC and ABIC decreased with each additional class being added to the model, the ALMR-LR test of the seven-class GMM did not reject the six-class model (Table S1). Therefore, the six-class GMM model was chosen. It had an adequate quality of class membership classification (entropy = 0.72). The estimated probability of each physical activity category for each latent class (LC) is presented in Fig. 2.
Figure 2.
Estimated growth trajectories for different classes.
The first three classes (LC1–3) were static, with little change observed over the 22-week period, making up 62.4% of the sample. The first class (LC1 = 11.6%) was marked by a high probability of physical inactivity (“inactive”). Participants in the second class (LC2 = 22.2%) had a moderate probability of doing physical activity for short (under 30 min) and medium (30 min to 2 h) durations (“fairly active”). The third class (LC3 = 28.6%) was the largest class, which consisted of people with a high probability of exercising for 30 min–2 h (“highly active”).
The last three classes (LC4–6) were dynamic, showing substantial changes over time. Both class four and five, together forming 28.6% of the sample, showed decreasing physical activity over time. The fourth class (LC4 = 17.5%) started from a moderate level of physical activity, very similar to LC2 when the lockdown started. In this class, the probability of being inactive increased rapidly over time, which was accompanied by declines in the short (< 30 min) and medium-duration (30 min–2 h) categories (“fairly active decreasing”). In contrast, participants in LC5 (11.1%) started from a high probability of exercising for 30 min–2 h, similar to LC3 at the beginning of lockdown. This probability was stable over the first few weeks but was followed by a rapid decline in subsequent weeks (“highly active decreasing”). This decline translated into an increased probability of being in the inactive or short duration (< 30 min) categories. The sixth class (LC6 = 9.0%) was the smallest and the most active, showing a high probability of exercising for medium (30 min–2 h) and long (≥ 3 h) durations. It was the only class that showed an overall increase in physical activity over time (“highly active increasing”). More specifically, the probability of exercising for a long duration (≥ 3 h) increased in the first 13 weeks, which was followed by a decrease when lockdown measures were substantially eased in June 2020. The growth trajectory of the long duration category (≥ 3 h) was the opposite of that for the category of medium duration (30 min–2 h), indicating exclusive transition between these two categories. Notably, this class had a very low probability of exercising for a short duration (< 30 min) or being physically inactive, which did not change over time.
Factors associated with latent trajectory classes
We fitted a conditional GMM to examine how individual characteristics were related to class membership of physical activity trajectories, using LC1 (“inactive”) as the reference (Table 2). Young adults had higher odds of being “fairly active” (LC2) than people aged 30 to 45 (OR = 1.48, 95% CI 1.03–2.13), as did individuals with a degree or above compared to those with lower education (OR = 2.06, 95% CI 1.66–2.56). People living with children also had higher odds of being “fairly active” than those living alone (OR = 1.54, 95% CI 1.18–2.00). However, people with long-term physical (OR = 0.83, 95% CI 0.69–1.00) and mental (OR = 0.57, 95% CI 0.46–0.71) health conditions had lower odds of being “fairly active”.
Table 2.
Results from the Growth mixture model with predictors of latent classes (LC) (LC1 as the reference, N = 35,915).
| LC2 (vs. LC1) | LC3 (vs. LC1) | LC4 (vs. LC1) | LC5 (vs. LC1) | LC6 (vs. LC1) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Woman (vs man) | 1.02 | [0.85–1.23] | 0.96 | [0.81–1.14] | 1.19 | [0.98–1.46] | 1.19 | [0.94–1.49] | 0.71 | [0.58–0.87] |
| Ethnic minority (vs white) | 0.82 | [0.57–1.17] | 0.89 | [0.62–1.29] | 0.99 | [0.66–1.48] | 0.83 | [0.52–1.31] | 1.04 | [0.68–1.59] |
| Age 18–29 (vs. 30–45) | 1.48 | [1.03–2.13] | 1.24 | [0.85–1.80] | 1.32 | [0.86–2.03] | 2.01 | [1.33–3.04] | 1.62 | [1.02–2.57] |
| Age 46–59 (vs. 30–45) | 0.83 | [0.67–1.03] | 1.32 | [1.07–1.63] | 0.83 | [0.65–1.06] | 0.94 | [0.72–1.22] | 1.19 | [0.89–1.59] |
| Age 60 + (vs. 30–45) | 1.22 | [0.93–1.59] | 2.23 | [1.72–2.89] | 1.18 | [0.87–1.60] | 1.75 | [1.25–2.45] | 2.07 | [1.47–2.92] |
| A-levels or equivalent (vs. GCSEs or below) | 1.09 | [0.87–1.36] | 1.25 | [1.01–1.54] | 1.12 | [0.87–1.43] | 1.44 | [1.09–1.90] | 1.08 | [0.83–1.41] |
| Degree or above (vs. GCSEs or below) | 2.06 | [1.66–2.56] | 2.36 | [1.93–2.90] | 1.35 | [1.06–1.72] | 1.78 | [1.34–2.35] | 1.27 | [0.97–1.68] |
| Household income < 30 k (vs ≥ 30 k) | 0.82 | [0.67–1.02] | 0.54 | [0.44–0.65] | 0.80 | [0.64–1.01] | 0.46 | [0.36–0.60] | 0.66 | [0.52–0.84] |
| Employed to unemployed (vs employed) | 1.25 | [0.90–1.73] | 1.68 | [1.24–2.26] | 1.52 | [1.08–2.13] | 1.79 | [1.26–2.56] | 1.77 | [1.27–2.48] |
| Unemployed/inactive (vs employed) | 0.86 | [0.69–1.08] | 1.06 | [0.87–1.29] | 0.77 | [0.61–0.99] | 0.70 | [0.52–0.94] | 0.94 | [0.72–1.21] |
| Living with others, but no children (vs alone) | 1.20 | [0.98–1.48] | 1.37 | [1.13–1.67] | 1.04 | [0.83–1.30] | 1.60 | [1.21–2.11] | 1.29 | [1.01–1.64] |
| Living with others, including children (vs alone) | 1.54 | [1.18–2.00] | 1.51 | [1.17–1.95] | 1.28 | [0.95–1.74] | 1.60 | [1.13–2.26] | 1.62 | [1.17–2.23] |
| Large town (vs city) | 0.83 | [0.65–1.04] | 0.87 | [0.69–1.09] | 1.06 | [0.81–1.38] | 0.83 | [0.61–1.13] | 0.91 | [0.67–1.22] |
| Small town (vs city) | 0.92 | [0.74–1.15] | 1.03 | [0.82–1.29] | 0.93 | [0.71–1.20] | 0.91 | [0.68–1.21] | 1.00 | [0.75–1.33] |
| Rural (vs city) | 0.87 | [0.67–1.12] | 1.17 | [0.92–1.48] | 1.30 | [0.97–1.74] | 1.32 | [0.97–1.80] | 1.27 | [0.96–1.67] |
| Long-term physical illness (vs none) | 0.83 | [0.69–1.00] | 0.49 | [0.41–0.58] | 0.86 | [0.70–1.04] | 0.55 | [0.44–0.69] | 0.61 | [0.49–0.75] |
| Long-term mental illness (vs none) | 0.57 | [0.46–0.71] | 0.48 | [0.39–0.60] | 0.70 | [0.56–0.88] | 0.49 | [0.36–0.66] | 0.55 | [0.43–0.72] |
LC1 inactive, LC2 fairly active, LC3 highly active, LC4 fairly active decreasing, LC5 highly active decreasing, LC6 highly active increasing.
p < 0.05 in bold text.
Older adults had higher odds of being “highly active” (LC3) than those aged 30 to 45 (OR = 1.32–2.23), as did people with higher levels of education (OR = 1.25–2.36), those who lost their job (OR = 1.68, 95% CI 1.24–2.26), and people living with others (OR = 1.37–1.51). People from low-income households (OR = 0.54, 95% CI 0.44–0.65), and those with physical (OR = 0.49, 95% CI 0.41–0.58) and mental (OR = 0.48, 95% CI 0.39–0.60) health conditions had lower odds of being “highly active”.
For the dynamic classes, individuals with a degree or above (OR = 1.35, 95% CI 1.06–1.72) and those who lost their job (OR = 1.52, 95% CI 1.08–2.13) had higher odds of “fairly active decreasing” activity (LC4). People who were already unemployed or economically inactive at the start of lockdown (OR = 0.77, 95% CI 0.61–0.99) and those with mental health conditions (OR = 0.70, 95% CI 0.56–0.88) had lower odds of being in LC4.
Young adults under 30 (OR = 2.01, 95% CI 1.33–3.04) and older adults aged 60+ (OR = 1.75, 95% CI 1.25–2.45) had higher odds of “highly active decreasing” activity (LC5) than those aged 30–45. Also more likely to be in this class were people who: had higher levels of education (OR = 1.44–1.78); lost their job (OR = 1.79, 95% CI 1.26–2.56); and were living with others (OR = 1.60–1.60). Conversely, people who were from low-income households (OR = 0.46, 95% CI 0.36–0.60), unemployed or economically inactive (OR = 0.70, 95% CI 0.52–0.94), and had physical (OR = 0.55, 95% CI 0.44–0.69) and mental (OR = 0.49, 95% CI 0.36–0.66) health conditions had lower odds of being in LC5.
Finally, young adults under 30 (OR = 1.62. 95% CI 1.02–2.57), older adults aged 60+ (OR = 2.07, 95% CI 1.47–2.92), people who lost their job (OR = 1.77, 95% CI 1.27–2.48) and those living other others (OR = 1.29–1.62) had higher odds of “highly active increasing” activity (LC6). In contrast, women (OR = 0.71, 95% CI 0.58–0.87), people from low-income households (OR = 0.66, 95% CI 0.52–0.84) and those with physical (OR = 0.61, 95% CI 0.49–0.75) and mental (OR = 0.55, 95% CI 0.43–0.72) health conditions had lower odds of being in LC6, the only class where physical activity increased over time.
Given the similarities between LC4 (“fairly active decreasing”) and LC2 (“fairly active”), and between LC5 (“highly active decreasing”) and LC3 (“highly active”) at the beginning of the lockdown, we compared factors associated with these trajectories using alternative reference classes (Table S2). Individuals who had a degree or above (vs GCSEs or below), those who were unemployed or economically inactive (vs employed), and people aged 46–59 (vs 30–45) had lower odds of being in a class with decreasing physical activity. In contrast, people living in rural areas (vs cities) and aged 18–29 (vs 30–45) had higher odds of decreasing physical activity throughout the pandemic.
We carried out sensitivity analyses excluding keyworkers (n = 8651) who might have had a different experience during the lockdown due to still being able to go to work (analytical sample N = 27,264). The results were materially consistent with the main analysis, returning the same number of classes and very similar patterns of growth trajectories (Fig. S1). Other sensitivity analyses using piecewise growth models to reflect changes in lockdown measures also yielded similar results (Fig. S2).
Discussion
This study is the first to examine the heterogeneity in longitudinal changes of physical activity during the COVID-19 pandemic. Building on recent longitudinal studies, which reported a general decline in physical activity at the start of the pandemic14,26–31, our analyses identified six unique classes of growth trajectories of physical activity. Three of these classes were stable, showing little change over time, including the inactive (11.6%), the fairly active (22.2%) and the highly active (28.6%). There were two classes showing declines in physical activity or increased physical inactivity, making up 28.6% of all participants. In contrast, 9% of participants showed an upward trend in physical activity over the observational period. These differing trajectories may explain the inconsistent findings to date from longitudinal studies testing whether physical activity returned to pre-lockdown levels with the easing of restrictions in the UK26,27,30,31.
This study further examined sociodemographic and health-related predictors of the patterns of physical activity growth trajectories. When comparing the three stable classes (inactive, fairly active, and highly active; LC1–3), we found no gender, ethnic, or urban/rural differences between them. However, people who were older, more educated, had a higher income, shared a household with others, and those without long-term physical and mental health problems, were more likely to be in a more active class. This is consistent with previous evidence that age, education, income, health status, and social support are associated with physical activity during lockdown27,31,32,37–40,42,43. In contrast, our findings are not consistent with prior evidence that women and people of non-white ethnicity were less active during lockdown28,31,38–40,42,43, but consistent with a review of reviews suggesting that gender and ethnicity are correlates but not determinants of physical activity50. Previous studies have also found that differences in physical activity between genders and ethnic groups are very small4.
A similar set of factors were found to predict the difference between the three dynamic classes (LC4–LC6) relative to the inactive (LC1). The dynamic classes were either fairly active or highly active at the start of lockdown, followed by decreases or increases in physical activity during lockdown. As with the stable classes, people who had higher education and income, lived with others, and did not have long-term health problems were more likely to be in the dynamic fairly or highly active classes than the inactive class. Additionally, individuals who became unemployed were more likely to be in the highly active or dynamic classes. It is possible that this group was unique in having to adjust how they spent their time during lockdown after becoming unemployed, compared to those who were employed or economically inactive throughout this period. Further research with this group may enable us to identify opportunities to increase physical activity and understand barriers that prevent this behaviour change51.
There were very few sociodemographic or health-related differences in the dynamic compared to stable classes that started at similar levels of physical activity (fairly active decreasing vs fairly active, and highly active decreasing vs highly active). However, those with decreasing levels of physical activity (i.e. in dynamic classes) were younger, more likely to be employed, living in rural areas, and had lower levels of education. Understanding why these factors were associated with decreasing physical activity is important for the development of interventions. Although younger people were generally more physically active before the pandemic50, several other studies have found that younger adults were more likely to report changes (both increases and decreases) in physical activity during lockdown than older adults39,41,52. This could be because younger adults were generally confined to smaller homes with no outdoor space and less space to exercise, meaning motivation to remain physically active reduced over time. Levels of physical activity in younger adults may also have decreased as restrictions eased and they replaced time previously spent on physical activity with more sedentary leisure activities, such as socialising. Additionally, being younger and having lower educational attainment are associated with higher levels of anxiety, depression, and loneliness during lockdown53,54, as well as increasing loneliness throughout lockdown55, all of which could have contributed to reductions in physical activity. It is also possible that decreasing physical activity was associated with being employed because individuals struggled to maintain levels of physical activity alongside working from home, decreased work-life balance, and increased stress and burnout throughout the lockdown56,57.
This study has a number of strengths including its large sample size, repeated weekly follow-up of the same participants over 22 weeks since the first UK lockdown, and robust statistical approaches. Although the UCL COVID-19 Social Study did not use a random sample, it does have a large sample size with wide heterogeneity, including good stratification across all major socio-demographic groups. In addition, analyses were weighted on the basis of population estimates of core demographics, with the weighted data showing good alignment with national population statistics and another large scale nationally representative social survey53. Despite all efforts to make our sample inclusive and representative of the adult population in England, we cannot rule out the possibility of potential biases due to omitting other demographic factors that could be associated with survey participation in the weighting process. Further, our analyses relied on self-reported time spent on physical activity which is subject to recall and reporting bias. We also lack data on people’s physical activity before the start of the COVID-19 pandemic, so it remains unknown how change or stability in physical activity observed in this study compare to usual levels in our sample before the pandemic. Finally, this study only has data during and post the first UK lockdown. Future studies could extend our analyses to explore whether, and to what extent, the longitudinal patterns of physical activity persist after the COVID-19 pandemic.
Conclusions
Although there may have been a decline in physical activity in the general population at the start of the COVID-19 pandemic, it is important to acknowledge the heterogeneity in people’s longitudinal changes in physical activity. Our analyses have shown that over 62% of people experienced little change and another 9% increased their physical activity between March and August 2020. However, it should be highlighted that nearly 29% of people experienced reduced physical activity during the same period. Moreover, amongst the people with little change in physical activity, 12% were consistently inactive. Both of these groups call for attention and action. Given the well-established link between physical activity and health1–5, persistent or increased physical inactivity is likely to have both immediate and long-term implications for people’s physical and mental health, as well as general wellbeing 58. More public health efforts should be made to promote physical activity for the general population, and in particular for groups that are at a higher risk of inactivity or of reduced physical activity, during the COVID-19 pandemic and beyond.
Supplementary Information
Acknowledgements
The researchers are grateful for the support of a number of organisations with their recruitment efforts including: the UKRI Mental Health Networks, Find Out Now, UCL BioResource, SEO Works, FieldworkHub, and Optimal Workshop. The study was also supported by HealthWise Wales, the Health and Care Research Wales initiative, which is led by Cardiff University in collaboration with SAIL, Swansea University.
Abbreviations
- ABIC
Sample-size adjusted Bayesian information criterion
- ALMR-LR
Adjusted Lo-Mendell-Rubin likelihood ratio
- BIC
Bayesian information criterion
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
- GCSE
General certificate of secondary education
- GMM
Growth mixture modelling
- LC
Latent classes
- LMR-LR
Vuong-Lo-Mendell-Rubin likelihood ratio
- OR
Odds ratio
- UCL
University College London
- UK
United Kingdom
Author contributions
F.B., A.S. and D.F. developed the study idea and the analysis plan. F.B. analysed the data. J.B. and J.M. did the literature review. F.B., J.B. and J.M. wrote the first draft. F.B., J.B. and J.M. had accessed and verified the underlying data. All authors provided critical revisions. All authors read and approved the submitted manuscript.
Funding
This Covid-19 Social Study was funded by the Nuffield Foundation [WEL/FR-000022583], but the views expressed are those of the authors and not necessarily the Foundation. The study was also supported by the MARCH Mental Health Network funded by the Cross-Disciplinary Mental Health Network Plus initiative supported by UK Research and Innovation [ES/S002588/1], and by the Wellcome Trust [221400/Z/20/Z]. DF was funded by the Wellcome Trust [205407/Z/16/Z].
Data availability
Anonymous data will be made publicly available following the end of the pandemic.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-97065-1.
References
- 1.Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Curr. Opin. Psychiatry. 2005;18:189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Saint-Maurice PF, Troiano RP, Bassett DR, Graubard BI, Carlson SA, Shiroma EJ, Fulton JE, Matthews CE. Association of daily step count and step intensity with mortality among US adults. JAMA. 2020;323:1151–1160. doi: 10.1001/jama.2020.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Global Recommmendations on Physical Activity for Health. World Health Organization; 2010. [Google Scholar]
- 4.Rhodes RE, Lubans DR, Karunamuni N, Kennedy S, Plotnikoff R. Factors associated with participation in resistance training: A systematic review. Br. J. Sports Med. 2017;51:1466–1472. doi: 10.1136/bjsports-2016-096950. [DOI] [PubMed] [Google Scholar]
- 5.Mandolesi L, Polverino A, Montuori S, Foti F, Ferraioli G, Sorrentino P, Sorrentino G. Effects of physical exercise on cognitive functioning and wellbeing: Biological and psychological benefits. Front. Psychol. 2018;9:1–11. doi: 10.3389/fpsyg.2018.00509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. World Health Organization; 2009. [Google Scholar]
- 7.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 9.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384:45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 10.Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circ. Res. 2019;124:799–815. doi: 10.1161/CIRCRESAHA.118.312669. [DOI] [PubMed] [Google Scholar]
- 11.Booth FW, Roberts CK, Thyfault JP, Ruegsegger GN, Toedebusch RG. Role of inactivity in chronic diseases: Evolutionary insight and pathophysiological mechanisms. Physiol. Rev. 2017;97:1351–1402. doi: 10.1152/physrev.00019.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carter S, Hartman Y, Holder S, Thijssen DH, Hopkins ND. Sedentary behavior and cardiovascular disease risk: Mediating mechanisms. Exerc. Sport Sci. Rev. 2017;45:80–86. doi: 10.1249/JES.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 13.Nosova EV, Yen P, Chong KC, et al. Short-term physical inactivity impairs vascular function. J. Surg. Res. 2014;190:672–682. doi: 10.1016/j.jss.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balanzá-Martínez V, Kapczinski F, de AzevedoGardoso T, Atienza-Carbonell B, Rosa AR, Mota JC, De Boni RB. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Rev. Psiquiatr. Salud. Ment. 2021;14:16–26. doi: 10.1016/j.rpsm.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bourdas DI, Zacharakis ED. Evolution of changes in physical activity over lockdown time: Physical activity datasets of four independent adult sample groups corresponding to each of the last four of the six COVID-19 lockdown weeks in Greece. Data Br. 2020;32:106301. doi: 10.1016/j.dib.2020.106301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Đogaš Z, Kalcina LL, Dodig IP, Demirović S, Madirazza K, Valić M, Pecotić R. The effect of COVID-19 lockdown on lifestyle and mood in Croatian general population: A cross-sectional study. Croat. Med. J. 2020;61:309–318. doi: 10.3325/cmj.2020.61.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knell G, Robertson MC, Dooley EE, Burford K, Mendez KS. Health behavior changes during covid-19 pandemic and subsequent “stay-at-home” orders. Int. J. Environ. Res. Public Health. 2020;17:6268. doi: 10.3390/ijerph17176268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qin F, Song Y, Nassis GP, Zhao L, Dong Y, Zhao C, Feng Y, Zhao J. Physical activity, screen time, and emotional well-being during the 2019 novel coronavirus outbreak in China. Int. J. Environ. Res. Public Health. 2020;17:1–16. doi: 10.3390/ijerph17145170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deschasaux-Tanguy M, Druesne-Pecollo N, Esseddik Y, et al. Diet and physical activity during the COVID-19 lockdown period (March–May 2020): Results from the French NutriNet-Santé cohort study. Medrxiv. 2020 doi: 10.1101/2020.06.04.20121855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duncan GE, Avery AR, Seto E, Tsang S. Perceived change in physical activity levels and mental health during COVID-19: Findings among adult twin pairs. PLoS ONE. 2020;15:e0237695. doi: 10.1371/journal.pone.0237695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Faulkner J, O’Brien WJ, McGrane B, et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: A multi-country cross-sectional analysis. J. Sci. Med. Sport. 2020 doi: 10.1016/j.jsams.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mutz M, Gerke M. Sport and exercise in times of self-quarantine: How Germans changed their behaviour at the beginning of the COVID-19 pandemic. Int. Rev. Sociol. Sport. 2020 doi: 10.1177/1012690220934335. [DOI] [Google Scholar]
- 23.Schnitzer M, Schöttl SE, Kopp M, Barth M. COVID-19 stay-at-home order in Tyrol, Austria: Sports and exercise behaviour in change? Public Health. 2020;185:218–220. doi: 10.1016/j.puhe.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Violant-Holz V, Gallego-Jiménez MG, González-González CS, Muñoz-Violant S, Rodríguez MJ, Sansano-Nadal O, Guerra-Balic M. Psychological health and physical activity levels during the COVID-19 pandemic: A systematic review. Int. J. Environ. Res. Public Health. 2020;17:1–19. doi: 10.3390/ijerph17249419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caputo EL, Reichert FF. Studies of physical activity and COVID-19 during the pandemic: A scoping review. J. Phys. Act. Heal. 2020;17:1275–1284. doi: 10.1123/jpah.2020-0406. [DOI] [PubMed] [Google Scholar]
- 26.Janssen X, Fleming L, Kirk A, Rollins L, Young D, Grealy M, MacDonald B, Flowers P, Williams L. Changes in physical activity, sitting and sleep across the COVID-19 National Lockdown Period in Scotland. medRxiv. 2020 doi: 10.1101/2020.11.05.20226381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCarthy H, Potts H, Fisher A. Physical activity behaviour before, during and after COVID-19 restrictions: Longitudinal smartphone-tracking study of adults in the United Kingdom. J. Med. Internet Res. 2021;23:e23701. doi: 10.2196/23701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Zhang Y, Bennell K, et al. Physical distancing measures and walking activity in middle-aged and older residents in Changsha, China, during the COVID-19 epidemic period: Longitudinal observational study. J. Med. Internet. Res. 2020 doi: 10.2196/21632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maltagliati, S. et al. Evolution of physical activity habits after a context change: The case of COVID-19 lockdown. British Journal of Health Psychology.10.1111/bjhp.12524 (2020). [DOI] [PMC free article] [PubMed]
- 30.Tison GH, Avram R, Kuhar P, Abreau S, Marcus GM, Pletcher MJ, Olgin JE. Worldwide Effect of COVID-19 on physical activity: A descriptive study. Ann. Intern. Med. 2020;173:767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mata, J. et al. Health behaviors and mental health during the COVID-19 pandemic: A longitudinal population-based survey in Germany. Social Science & Medicine. 10.1016/j.socscimed.2021.114333 (2020). [DOI] [PMC free article] [PubMed]
- 32.Ong JL, Lau TY, Massar SAA, Chong ZT, Ng BKL, Koek D, Zhao W, Yeo BTT, Cheong K, Chee MWL. COVID-19 related mobility reduction: Heterogenous effects on sleep and physical activity rhythms. Sleep. 2021;44:zsaa179. doi: 10.1093/sleep/zsaa179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.FitBit Staff. The impact of coronavirus on global activity. https://blog.fitbit.com/covid-19-global-activity/ (2020).
- 34.Garmin. How garmin users prioritize movement in a global pandemic. https://www.garmin.com/en-US/blog/health/how-garmin-users-prioritized-movement-in-a-global-pandemic/ (2021).
- 35.Giuntella O, Hyde K, Saccardo S, Sadoff S. Lifestyle and mental health disruptions during COVID-19. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3666985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ding D, Del Pozo CB, Green MA, Bauman AE. Is the COVID-19 lockdown nudging people to be more active: A big data analysis. Br. J. Sports Med. 2020;54:2019–2020. doi: 10.1136/bjsports-2020-102575. [DOI] [PubMed] [Google Scholar]
- 37.Smith L, Jacob L, Butler L, et al. Prevalence and correlates of physical activity in a sample of UK adults observing social distancing during the COVID-19 pandemic. BMJ Open Sport Exerc. Med. 2020;6:1–5. doi: 10.1136/bmjsem-2020-000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herbec, A. et al. Correlates of and changes in aerobic physical activity and strength training before and after the onset of COVID-19 pandemic in the UK. Findings from the HEBECO study. medRxiv. 10.1101/2021.01.16.21249925 (2021). [DOI] [PMC free article] [PubMed]
- 39.Rogers NT, Waterlow NR, Brindle H, Enria L, Eggo RM, Lees S, Roberts CH. Behavioral change towards reduced intensity physical activity is disproportionately prevalent among adults with serious health issues or self-perception of high risk during the UK COVID-19 lockdown. Front. Public Heal. 2020;8:1–12. doi: 10.3389/fpubh.2020.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vogel EA, Zhang JS, Peng K, Heaney CA, Lu Y, Lounsbury D, Hsing AW, Prochaska JJ. Physical activity and stress management during COVID-19: A longitudinal survey study. Psychol. Health. 2021 doi: 10.1080/08870446.2020.1869740. [DOI] [PubMed] [Google Scholar]
- 41.Rhodes RE, Liu S, Lithopoulos A, Zhang CQ, Garcia-Barrera MA. Correlates of perceived physical activity transitions during the COVID-19 pandemic among Canadian Adults. Appl. Psychol. Heal. Well-Being. 2020;12:1157–1182. doi: 10.1111/aphw.12236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dunton GF, Wang SD, Do B, Courtney J. Early effects of the COVID-19 pandemic on physical activity locations and behaviors in adults living in the United States. Prev/ Med. Rep. 2020;20:101241. doi: 10.1016/j.pmedr.2020.101241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robinson E, Boyland E, Chisholm A, Harrold J, Maloney NG, Marty L, Mead BR, Noonan R, Hardman CA. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite. 2021;156:104853. doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brand R, Timme S, Nosrat S. When pandemic hits: exercise frequency and subjective well-being during COVID-19 pandemic. Front. Psychol. 2020;11:1–10. doi: 10.3389/fpsyg.2020.570567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chang YK, Hung CL, Timme S, Nosrat S, Chu CH. Exercise behavior and mood during the COVID-19 pandemic in Taiwan: Lessons for the future. Int. J. Environ. Res. Public Health. 2020;17:1–17. doi: 10.3390/ijerph17197092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lesser IA, Nienhuis CP. The impact of COVID-19 on women’s physical activity behavior and mental well-being. Int. J. Environ. Res. Public Health. 2020;17:1–12. doi: 10.3390/ijerph17113899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meyer J, McDowell C, Lansing J, Brower C, Smith L, Tully M, Herring M. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int. J. Environ. Res. Public Health. 2020;17:1–13. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.de la Cámara MÁ, Jiménez-Fuente A, Pardos-Sevilla AI. Confinement time due to the COVID-19 disease: An opportunity to promote and engage people in regular physical exercise? Transl. Sport Med. 2021;4:3–5. doi: 10.1002/tsm2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Muthén B, Asparouhov T. Growth mixture modeling: Analysis with non-Gaussian random effects. In: Fitzmaurice G, Davidian M, Verbeke G, Molenberghs G, editors. Longitud. Data. Anal. CRC Press; 2008. pp. 143–165. [Google Scholar]
- 50.Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: Why are some people physically active and others not? Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 51.Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:1–11. doi: 10.1186/1748-5908-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alomari MA, Khabour OF, Alzoubi KH. Changes in physical activity and sedentary behavior amid confinement: The BKSQ-COVID-19 project. Risk Manag. Healthc. Policy. 2020;13:1757–1764. doi: 10.2147/RMHP.S268320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–34. doi: 10.1016/j.puhe.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bu F, Steptoe A, Fancourt D. Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc. Sci. Med. 2020;265:113521. doi: 10.1016/j.socscimed.2020.113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weber C, Golding S, Ratcliffe E, Yarker J, Lewis R, Munir F. Homeworking during COVID-19 lockdown: Relationships between the physical and social environments at home, work-related burnout, and musculoskeletal pain. Heal. Psychol. Updat. 2020;29:55–56. [Google Scholar]
- 57.Anderson D, Kelliher C. Enforced remote working and the work-life interface during lockdown. Gend. Manag. 2020;35:677–683. [Google Scholar]
- 58.Pinho CS, Caria ACI, Aras Júnior R, Pitanga FJG. The effects of the COVID-19 pandemic on levels of physical fitness. Rev. Assoc. Med. Bras. 2020;66:34–37. doi: 10.1590/1806-9282.66.s2.34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymous data will be made publicly available following the end of the pandemic.