Abstract
Objectives
To identify mental health prospective trajectories before and after a second lockdown during the COVID-19 pandemic and their associations with somatic symptoms.
Design
Prospective Study.
Setting
Population-based study drawn from a probability-based internet panel of over 100 000 Israelis.
Participants
Adults aged 18 years or more, representative of the adult Israeli population. The participants were measured at two time points (time 1 (T1) pre-second lockdown N=1029; response rate=76.17%; time 2 (T2) post-second lockdown N=764; response rate=74.24%).
Main outcome measures
Trajectories of anxiety and adjustment disorder based on clinical cut-off score for probable diagnoses across T1-T2, somatic symptoms at T2. The four trajectories: stable-low, (no probable diagnosis), stable-high (stable probable diagnosis), exacerbation (no probable diagnosis at T1, probable diagnosis at T2), recovery (probable diagnosis at T1, no probable diagnosis at T2).
Results
Three anxiety trajectories predicted probable somatic symptoms (stable-high OR=6.451; exacerbation OR=5.379; recovery OR=2.025) compared with the stable-low trajectory. The three adjustment disorder trajectories also predicted somatic symptoms (stable-high OR=4.726; exacerbation OR=6.419; recovery OR=4.666) compared with the stable-low trajectory.
Conclusions
Our data show elevated somatic symptoms among those whose mental health trajectories were poor, exacerbated and those who recovered following the second lockdown. The presentation of somatic symptoms may mask psychological vulnerabilities, even among those who appear to have recovered from the stressor. This indicates that lockdown may be a double-edged sword and should be carefully administered given these populations vulnerabilities.
Keywords: COVID-19, epidemiology, anxiety disorders, mental health
Strengths and limitations of this study.
To our knowledge, this is the first study to address the association between mental health trajectories and somatic symptoms before and after a second lockdown.
The survey used a robust quota sampling method representative of the Israeli adult population based on age and sex.
Findings are based on a large longitudinal national sample enabling identification of mental health trajectories.
The use of unrelated robust and validated measures of adjustment disorder, anxiety and somatisation allows us to report those trajectories of adjustment disorder and anxiety at higher risk of increased somatic symptoms.
The main weaknesses of this study are potential selection bias and the lack of measurement of somatic symptoms and mental health indices before the COVID-19 pandemic.
Introduction
From a mental health perspective, the COVID-19 pandemic can be viewed as a highly stressful event likely to lead to anxiety and stress-related disorders.1 Particularly interesting, are the specific stressors associated with a lockdown, given that such restrictions play such an important role in preventing COVID-19 outbreaks.2 Several studies have pointed to an association between a single lockdown and poorer mental health.3 4 However, in some countries, there was more than one lockdown. Israel was one of the first countries to apply a second lockdown, as a result of a rapid infection increase (18 September to 8 November 2020). The current study explored trajectories of mental health,5 and the associations between these trajectories and somatic symptoms over time.
Despite the plethora of studies examining mental health during COVID-19, few studies have addressed adjustment disorder.6 7 Furthermore, studies regarding the association between mental health and somatic symptoms are scarce among the general population,8 9 although these are commonly reported by patients in both general population and clinical settings.8 Somatic symptom burden has been related to higher age, lower education, social and economic status, and unemployment.10–12 Huang et al 9 in China reported a prevalence of 7.59% somatic symptoms in the general population following the COVID-19 outbreak. A high somatic symptom burden has also been associated with reduced subjective health and quality of life, increased psychological distress and use of healthcare services.12 Only a few studies have assessed the prevalence of adjustment disorder during the COVID-19 pandemic.6 7 However, no study thus far has examined a lockdown-related adjustment disorder trajectory and its relation to somatic symptoms. Distinguishing this specific disorder is crucial in understanding the relative importance of such a stressor compared with general anxiety during the pandemic. Moreover, to date, no study has examined mental health symptoms before and after lockdowns and tested their accumulated burden. As a result, the aforementioned studies lack the prospective perspective of any change and fluctuations that might follow lockdowns.
Empirical research on how mental health and health-related behaviours have changed throughout the COVID-19 pandemic remains limited and is largely based on cross-sectional data or very narrow prospective data collected before and during the pandemic. Increasing attention has been made to different groupings of responses to this global crisis. A trajectories approach used in longitudinal studies of mental health following potential stressors has identified four main outcome patterns or trajectories over time, namely chronic, recovered, delayed onset and resilient.13 14 Cross-sectional diagnostic classification can easily overlook these trajectories. For example, recovery may be conflated with resilience or chronic stress depending on when it is assessed. To understand the peri-implication and postimplication of the COVID-19 crisis, and lockdowns in particular, prospective studies which comprise large national samples are required. Based on the trajectories approach, the current study suggests four trajectories: a ‘stable-low trajectory’ which included participants who did not reach the clinical cut-off of anxiety and adjustment disorder at either time 1 (T1) or time 2 (T2), a ‘recovery trajectory’ which included participants that reached full criteria of probable anxiety/probable adjustment disorder at T1, but recovered at T2 and did not reach the clinical cut-offs of anxiety/adjustment disorder; a ‘stable-high trajectory’ which included participants that reached full criteria of probable anxiety/probable adjustment disorder at both T1 and T2, and an ‘exacerbation trajectory’, which includes participants that did not reach criteria of probable anxiety/adjustment disorder at T1 but reached full criteria of probable anxiety/probable adjustment disorder at T2. To date, we know of no prospective studies that examined the impact of trajectories of mental health on somatic symptoms before and after a second lockdown.
This study has several novel characteristics. First, it is the first study to assess mental health before and after a second lockdown. Second, this is one of the first studies to measure trajectories of adjustment disorder based on the International Classification of Diseases 11th Revision (ICD-11). Third, this is one of the first studies to measure the association between trajectories of mental health and somatic symptoms.
The present study aims to: (1) identify prospective trajectories of anxiety and adjustment disorder before and after the second lockdown; (2) examine the associations of anxiety and adjustment disorder during the COVID-19 crisis with somatic symptoms and probable somatic symptoms after the second lockdown.
We hypothesised that lockdown-related stable-high and exacerbation trajectories will be associated with greater somatic symptoms, compared with ‘recovery’ and ‘stable-low’ trajectories.
Methods
Recruitment and eligibility
Data were collected from 3 August to 30 August 2020 for T1 and 15 November to 3 December for T2. Eligibility criteria specified that participants should be: aged 18 or over; Israeli residents at the time the survey was conducted; able to give informed consent; fluent in their native language.
Sample size
As a minimum, we estimated that 610 participants would be required to detect low-medium effect sizes of 0.20, with 90% power and a 5% significance level based on inclusion of 12 explanatory variables (6 background variables and 6 trajectories that were compared with the reference group), in a logistic regression model. For the two-way analysis of variance (ANOVA) we detected a need for a 523 minimum sample size, on the basis of 16 groups (4 adjustment disorder trajectories×4 anxiety trajectories), low-medium effect sizes of 0.20, with 90% power and a 5% significance level. Overall, for logistic regression, a simulation study recommended a minimum sample size of 500 to derive statistics that can represent the parameters in the targeted population.15
Sampling and procedures
The study was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for observational studies.
We used Israel’s iPanel company to deploy the COVID-19 Mental Health Survey. This panel is a probability-based panel with over 100 000 members.16 The panels consist of adults aged 18–85 who have given their consent to be contacted about surveys. Panel recruitment is dynamic and constant using a range of online methods.
iPanel adheres to the stringent standards of the world association for market, social and opinion researchers (ESOMAR). From this panel, we recruited participants aged 18–71.
A quota sampling approach was used with quotas meeting the Israeli national census data on age and sex, as specified by the Israeli Bureau of Statistics census data. The use of this approach ensured that a good representation of the adult population in Israel. After the quotas and required sample size were reached, the survey was closed.
The final data set was weighted according to these factors (age and sex) to enable the study to be considered representative of the internet-using participants of 18–71 years living in Israel.
At T1, out of 1351 invitations sent, 1029 responded (response rate=76.17%); at T2, out of 1029 participants in T1 (baseline), 764 responded (response rate=74.24%). We conducted a set of sensitivity analyses at T1 comparing those who did answer the survey to those who did not (n=322) on the following key demographic factors age (t(1049)=1.10; p=0.271), sex (χ²(1)=2.65; p=0.104), marital status (χ²(4)=1.33; p=0.856), income (χ²(4)=2.77; p=0.594) and education (χ²(5)=6.84; p=0.145). No differences were found between the groups.
Measurements
Demographic variables were age (mean=40.75; SD=14.75; range 18–71), sex coded men as ‘1’ women as ‘2’ (50.5% of the sample, n=520). Most of the participants were in a committed relationship (58.3% of the sample, n=600) coded as ‘1’ for single, ‘2’ for committed relationship, ‘3’ for divorced, ‘4’ for separated and ‘5’ for widowed. Education was coded as ‘1’ for elementary school, ‘2’ for high school without diploma, ‘3’ for high school graduate with diploma, ‘4’ for higher education with no diploma, ‘5’ for undergraduate diploma and ‘6’ for postgraduate diploma. Income was measured by the following question: ‘the average monthly income in Israel in August 2020 was 13 558 NIS (2570 GBP). Please rate your income in comparison’. The rating was done on a 5-point Likert scale coded as ‘1’ much below average, ‘2’ a little below average, ‘3’ about the average, ‘4’ a little above the average and ‘5’ much above average.
Risk group for COVID-19 was measured by the following question: ‘do you suffer from one of the following medical conditions: (hypertension, diabetes, cardiovascular disease, chronic respiratory disease, chronic obstructive pulmonary disease and cancer)’. The list was composed according to the WHO and US Centers for Disease Control and Prevention (CDC). Being in a risk group for COVID-19 was coded as ‘1’ for being in risk group for COVID-19 and ‘2’ for being in non-risk group for COVID-19. For elaborated demographics, see table 1.
Table 1.
Participant demographics (n=1029) and Israeli population values
| Participants (n=1029) | Israel population (N=9 291 000) |
|
| n (%) | n (%) | |
| Sex | ||
| Male | 509 (49.5) | 49.7 |
| Female | 520 (50.5) | 50.3 |
| Age groups (years) | ||
| 18–22 | 180 (13.3) | 10.1 |
| 23–29 | 218 (16.1) | 15.9 |
| 30–39 | 291 (21.5) | 24 |
| 40–49 | 240 (17.8) | 20 |
| 50+ | 422 (31.2) | 30 |
| Education | ||
| Elementary school | 9 (0.7) | 1.9 |
| High school no diploma | 132 (9.2) | 8 |
| Graduate high school with diploma | 312 (23.1) | 22 (graduate high school/with diploma 42) |
| Higher education with no diploma | 292 (21.6) | 17 |
| Undergraduate diploma | 386 (28.6) | 20 (higher diploma—academic/not academic 50.9%) |
| Postgraduate diploma | 220 (16.3) | 11 |
| Income | Mean income 13 558 NIS (2570 GBP) | |
| Much below average | 281 (21.1) | 26.9 |
| A little below average | 237 (17.8) | N/A |
| About average | 332 (24.9) | 34.1 (based on incomes from all resources to a household) |
| A little above average | 355 (26.7) | N/A above average—28 |
| Much above average | 127 (9.5) | N/A |
| Marital status | ||
| Single | 431 (31.9) | 30 |
| Married | 796 (58.9) | 61 |
| Divorced | 107 (7.9) | 6 |
| Separated | 9 (0.7) | 1 |
| Widowed | 8 (0.6) | 2 |
| COVID-19 risk group according to the WHO criteria | ||
| Yes | 240 (23.3) | N/A |
| No | 789 (76.7) | N/A |
Israel population estimates from Office for National Statistics, end year estimates 2018.
Anxiety was measured using the Generalised Anxiety Disorder 7-item Scale (GAD-7).17 Participants indicated how often they had been bothered by each symptom over the last 2 weeks on a 4-point Likert scale (0=not at all, to 3=nearly every day). The reliability as measured by Cronbach’s alpha was high for both times: T1 (α=0.92) and T2 (α=0.91). Higher scores indicated higher level of anxiety (ranged score 0–21) and were divided into two categories of anxiety severity (0–9 no probable anxiety; 10–21 probable anxiety).
Adjustment disorder in the form of ICD-11 probable adjustment disorder was measured using the International Adjustment Disorder Questionnaire 19-item (IADQ).18 The IADQ comprises two parts. First is a checklist of a stressors list covering different aspects of life. The second IADQ component assesses adjustment disorder core symptoms (six-items) tapping into two symptoms clusters (‘preoccupation’ and ‘failure to adapt’), functional impairment (three-items) rated on 5-point Likert scale (0=not at all, to 4=extremely). The 10th question assesses when the symtpoms has begun (coded as 0 for no (not within the first month of the stressful event) and 1 for yes (within the first month of the stressful event)). The algorithm for a probable diagnosis of ICD-11 adjustment disorder requires the presence of a psychosocial stressor (score ≥1 on the IADQ stressor list), at least one preoccupation symptom rated ≥2, at least one failure-to-adapt symptom rated ≥2, and evidence of functional impairment rated ≥2. The reliability as measured by Cronbach’s alpha in T1 (α=0.93) and T2 (α=0.94) were excellent.
Somatic symptoms severity was measured using the Somatic Severity Scale 8-item Scale (SSS-8).19 Respondents rated how much they were bothered by common somatic symptoms within the last seven days on a 5-point Likert scale (0=not at all to 4=very much). Higher scores indicated higher level of somatic symptoms (ranged score 0–32) and were divided into five categories of somatic severity (0–3 none-minimal; 4–7 low; 8–11 medium; 12–15 high; 16–32 very high). For the purpose of this study, we used the cut-off score of ≥12 and above for indicating high somatic symptoms severity. The reliability as measured by Cronbach’s alpha in T2 (α=0.83) was good.
Statistical methods
The analytic plan included a descriptive epidemiological approach to depict mental health trajectories across the two assessments, before and after the second lockdown. We used the GAD-7 and IADQ cut-offs in order to determine the trajectories in the current study. Four trajectory groups were generated: (1) participants with no probable anxiety/adjustment disorder at both T1-T2 (‘stable-low trajectory’); (2) participants with probable anxiety/adjustment disorder at both T1-T2 (‘stable-high trajectory’); (3) participants with no probable anxiety/adjustment disorder at T1 and probable anxiety/adjustment disorder at T2 (‘exacerbation trajectory’); (4) participants with probable anxiety/adjustment disorder at T1 and no probable anxiety/adjustment disorder at T2 (‘recovery trajectory’). The rates of each trajectory were identified for both anxiety and adjustment disorder. In order to show the differences between the trajectories which relied on cut-offs (dichotomous scores), we present the descriptive information in figures—means of the anxiety and adjustment disorder in the continuous scores of the scales used. Then, we tested the rates of probable somatic symptoms in the different mental health trajectories. In order to characterise the trajectories with respect to demographic data, a multinomial regression on anxiety and adjustment disorder trajectories by background variables was performed.
Second, we addressed the differences between the trajectory groups for both adjustment disorder and anxiety, as well as the combination between them along with their impact on the severity of somatic symptoms in T2. A two-way ANOVA was conducted. The main effects as well as the interaction effect were calculated.
Third, a logistic regression model examined the outcome variable of probable dichotomous somatic symptoms severity (T2). In the first step, age, sex, relationship status, income and education were included in the model. Risk group membership for COVID-19 was also added to the model. In the second step, we added the trajectories ΔT1-T2 of anxiety severity categories and ICD-11 probable adjustment disorder. We tested whether the trajectories would significantly contribute to somatic symptoms severity, compared with the stable-low trajectory (reference group).
Role of sponsor
The study sponsor did not play a role in the study design, collection; analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Patient and public involvement
No patient involved.
Results
Cohort characteristics
Table 1 summarises the main characteristics of the participants, alongside comparative data on Israeli population where available.
Descriptive information
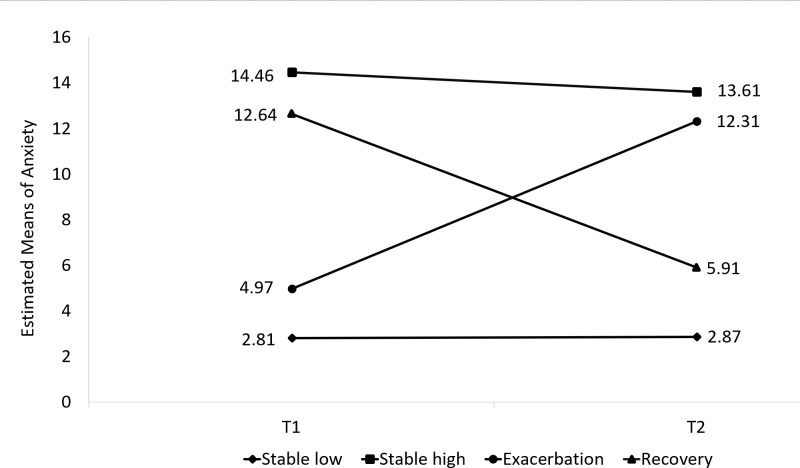
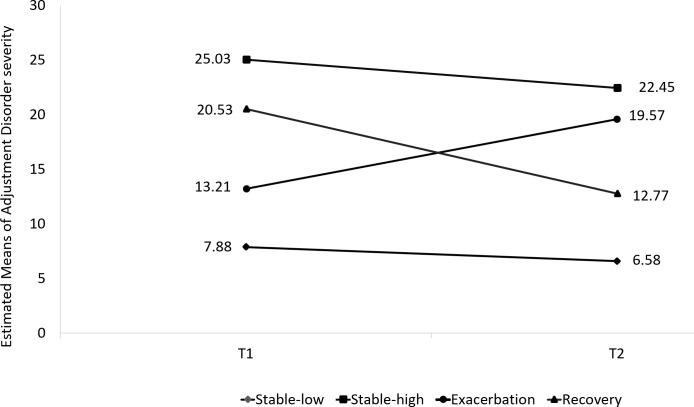
Prevalence of high somatic severity symptoms was 18.8% (n=144). Four different trajectories were identified on the basis of cut-off scores for probable anxiety and probable adjustment disorder. The ‘stable-low trajectory’ included the majority of the sample in both anxiety (78.1%) and adjustment disorder (71.3%). A second trajectory had the ‘recovery’ course (9.0% and 8.9%, respectively). Of the entire sample, 5.4% and 11.8% belonged to the ‘stable-high’ trajectory of anxiety and adjustment disorder. A fourth trajectory—the ‘exacerbation’ trajectory—included 7.5% and 8.0% in the anxiety and adjustment disorder, respectively. The trajectories of anxiety and adjustment disorder are presented in figures 1 and 2.
Figure 1.
Trajectories of anxiety symptoms over time. Four different trajectories were identified for probable anxiety.
Figure 2.
Trajectories of adjustment disorder symptoms over time. Four different trajectories were identified for probable anxiety.
The prevalence rates of the probable somatic severity symptoms in the anxiety trajectories were 11.1%, 61.0%, 49.1% and 36.2% among the ‘stable-low’, ‘stable high’, ‘exacerbation’ and ‘recovery’ trajectories, respectively. The prevalence rates of the probable somatic severity symptoms in the adjustment disorder trajectories were 8.8%, 48.9%, 44.3% and 36.8% among the ‘stable-low’, ‘stable high’, ‘exacerbation’ and ‘recovery’ trajectories, respectively.
Predicting trajectories by background variables
A multinomial regression on anxiety trajectories by background variables showed trajectories to be predicted significantly by sex, age and risk group. Younger age was significantly associated with the exacerbation group (b=−0.032, SE=0.014, Wald=5.571, p=0.018, OR 0.969, 95% CI 0.943 to 0.995) and stable-high group (b=−0.040, SE=0.015, Wald=6.705, p=0.010, OR 0.961 95% CI 0.932 to 0.990) compared with the stable-low group. High risk for COVID-19 contributed significantly to the high-stable trajectory group (b=0.81, SE=0.08, Wald=4.54, p=0.033, OR 0.446, 95% CI 0.212 to 0.937), compared with the stable-low group. There were more women in the recovery group, compared with the stable-low group (b=−0.66, SE=0.28, Wald=5.42, p=0.033, OR 0.519, 95% CI 0.298 to 0.901).
Adjustment disorder were predicted predominantly by sex and risk group. The COVID-19 risk group contributed significantly to belonging to the stable high (b=0.58, SE=0.27, Wald=4.67, p=0.030, OR 0.56, 95% CI 0.331 to 0.947) and to the exacerbation groups (b=0.70, SE=0.31, Wald=5.09, p=0.024, OR 0.50, 95% CI 0.272 to 0.912) compared with the stable-low group serving as the reference group. There were more women in the trajectory of stable high (b=−0.87, SE=0.25, Wald=12.51, p<0.001, OR 0.417, 95% CI 0.257 to 0.677), and recovery groups (b=−0.66, SE=0.22, Wald=9.25, p=0.003, OR 0.52, 95 CI 0.338 to 0.791) compared with the stable-low group.
Differences between the trajectories and severity of somatic symptoms
A two-way ANOVA showed significant main effects and non-significant interaction effects. A main effect for the anxiety trajectories demonstrated significant differences between the anxiety trajectories in the severity of somatic symptoms F(3, 748)=16.723, p<0.001, η²=0.04. The stable-low trajectory (M=8.19, SD=0.34) reported significantly lower severity of somatic symptoms compared with the stable-high (M=13.38, SD=0.93), exacerbation (M=12.34, SD=0.69) and recovery (M=10.02, SD=0.60) trajectories. The differences between the stable-low and both the stable-high (mean difference=−5.19, p<0.001) and exacerbation trajectories (mean difference=−4.15, p<0.001) were greater than the difference between the stable-low and the recovery trajectory (mean difference=−1.89, p=0.050).
An ANOVA for the adjustment disorder trajectories showed significant differences between the trajectories in the severity of somatic symptoms F(3, 760)=17.623, p<0.001, η²=0.05. The stable-low trajectory (M=8.04, SD=0.47) reported significantly lower severity of somatic symptoms compared with the stable-high (M=12.99, SD=0.53), exacerbation (M=12.07, SD=0.82) and recovery (M=10.83, SD=0.80) trajectories. The differences between the stable-low and both the stable-high (mean difference=−4.96, p<0.001) and exacerbation trajectories (mean difference=−4.03, p<0.001) were greater than the difference between the stable-low and the recovery trajectory (mean difference=−2.79, p=0.016).
The interaction between the trajectories of adjustment disorder and the trajectories of anxiety was not significant F(9, 748)=1.467, p=0.156, η²=0.01.
Role of mental health trajectories in predicting risk for probable somatic symptoms
A logistic regression found that trajectories of both the anxiety and adjustment disorder were associated with somatic symptoms at T2 (see table 2). Participants with a stable high trajectory, exacerbation trajectory or recovery trajectory had substantially higher odds of having somatic symptoms at T2, compared with participants with a low-stable trajectory.
Table 2.
Logistic regression of factors predicting somatic symptoms burden by SSS-8 (score ≥12)
| n (%) | b | SE | Wald | P value | OR (95% CI) | |
| Age | −0.00 | 0.01 | 0.49 | 0.486 | 0.994 (0.978 to 1.011) | |
| Sex (reference group: men) | 365 (48.8) | 0.45* | 0.23 | 4.02 | 0.045 | 1.574 (1.010 to 2.454) |
| Relationship status (reference group: not in a committed relationship) | 299 (39.1) | −0.42 | 0.25 | 2.92 | 0.088 | 0.654 (0.402 to 1.065) |
| Education | 0.16 | 0.10 | 2.62 | 0.105 | 1.170 (0.968 to 1.416) | |
| Income (monthly average: 2570 GBP) (reference group: much lower than average)a (n= 1014), b (n= 756) | 157 (20.5) | |||||
| A little below average | 126 (16.5) | −0.10 | 0.34 | 0.09 | 0.764 | 0.903 (0.463 to 1.759) |
| About average | 193 (25.3) | −0.52 | 0.33 | 2.51 | 0.113 | 0.594 (0.312 to 1.131) |
| A little above average | 203 (26.6) | −0.24 | 0.33 | 0.52 | 0.469 | 0.790 (0.418 to 1.494) |
| Much higher than average | 77 (10.1) | −0.28 | 0.43 | 0.43 | 0.513 | 0.754 (0.323 to 1.760) |
| Being in risk group for COVID-19 (reference group: not in risk) | 581 (76.0) | −0.27 | 0.26 | 1.08 | 0.298 | 0.761 (0.454 to 1.274) |
| Trajectories over T1-T2 | ||||||
| GAD-7 Anxiety (reference group: stable-low trajectory) | 597 (78.0) | 41.291 | ||||
| Stable high trajectory | 41 (5.4) | 1.864*** | 0.389 | 22.993 | 0.000 | 6.451 (3.011 to 13.822) |
| Exacerbation trajectory | 57 (7.5) | 1.682*** | 0.333 | 25.575 | 0.000 | 5.379 (2.802 to 10.325) |
| Recovery trajectory | 69 (9.0) | 0.705* | 0.329 | 4.591 | 0.032 | 2.025 (1.062 to 3.861) |
| ICD-11 probable adjustment disorder by IADQ (reference group: stable-low trajectory) | 545 (71.3) | 52.853 | ||||
| Stable high trajectory | 90 (11.8) | 1.553*** | 0.303 | 26.306 | 0.000 | 4.726 (2.611 to 8.555) |
| Exacerbation trajectory | 61 (8.0) | 1.859*** | 0.329 | 31.988 | 0.000 | 6.419 (3.370 to 12.227) |
| Recovery trajectory | 68 (8.9) | 1.540*** | 0.320 | 23.161 | 0.000 | 4.666 (2.492 to 8.739) |
*p≤0.05; **p≤0.01; ***p≤0.001. aActual n=1014; bactual n=756.
GAD, General Anxiety disorder; IADQ, International Adjustment Disorder Questionnaire; ICD-11, International Classification of Diseases 11th Revision; SSS, Somatic Severity Scale.
The OR shows that participants with an exacerbation trajectory in adjustment disorder had the highest odds (OR 6.419) of experiencing somatic symptoms at T2, compared with the other trajectories (high stable OR 4.726 and recovery OR 4.666), all as compared with the stable-low trajectory. The statistical difference between the strength of the coefficients of the trajectories was not significant (p value ranged from 0.490 to 0.690).
As for the anxiety trajectories, the stable-high trajectory (OR 6.451) and the exacerbation trajectory (OR 5.379) had the highest OR for experiencing somatic symptoms at T2, compared with the recovery trajectory that showed lower odds ratio (OR 2.025), all compared with the group-stable-low trajectory. This was reflected further in the statistical difference between the stable-high and the recovery trajectory t(1508)=2.27, p=0.02 and between the exacerbation and the recovery trajectories t(1508)=2.09, p=0.036.
Discussion
Several studies have suggested that mental health has deteriorated over time in many countries during the pandemic.20–22 We explored trajectories of anxiety and adjustment disorder before and after the second lockdown during the COVID-19 pandemic in Israel. In line with the existing literature on responses to mass trauma, four types of mental health trajectories were identified: stable-low, stable-high, exacerbation and recovery groups. These trajectories, with similarities in distribution, have been reported for other disorders namely Post Traumatic Stress Disorder (PTSD),23 depression and anxiety,24 25 in different populations.5
To date, we know of one, UK-based study that has examined trajectories of anxiety and depression over the course of the COVID-19 pandemic.26 However, this UK study focused on the first lockdown measuring changes in anxiety and depression. Our analysis of multiple events underscored the complex and non-homogenous reactions to lockdowns. Several demographic variables predicted trajectories of response. Being female was a risk factor for more psychopathological trajectories of anxiety and adjustment disorder symptoms for the stable-high trajectory of adjustment disorder and the recovery trajectory of anxiety and adjustment disorder. Older age was associated with lower odds of belonging to the stable-high or exacerbation trajectories compared with the stable-low trajectory. Risk group membership was associated with higher odds of belonging to the stable-high group of anxiety and adjustment disorder and to the exacerbation group of adjustment disorder.
The current study showed the association between poor mental health (anxiety and adjustment disorder trajectories) and elevated risk of somatic symptoms. For both anxiety and adjustment disorder, affiliation to the stable-high, exacerbation and the recovery T1-T2 trajectories were significantly associated with higher risk for somatic symptoms at T2, compared with the stable-low trajectory. It is important to note that for adjustment disorder the three trajectories were associated with somatic symptoms at T2 in a similar magnitude. However, for anxiety, the association between the recovery trajectory and somatic symptoms at T2 was significantly lower than the associations between stable-high and exacerbation trajectories and somatic symtpoms. Adjustment disorder refers to a specific stressor of the lockdown and was reflected in all the three trajectories which differed from the stable-low trajectory. However, trajectories of anxiety suggested a more general anxiety construct that is global and not stressor specific. Thus, the findings show that adjustment disorder manages to capture the consequences of lockdowns more than anxiety.
In line with our hypotheses, the groups with stable-high and exacerbation trajectories (before and after a second lockdown) of anxiety were associated with higher somatic symptoms at T2, compared to the stable-low group. Huang and his colleagues9 found that during the COVID-19 outbreak in China, anxious people were more likely to have somatic symptoms than people without anxiety symptoms. This was also observed through somatic symptoms burden among those with higher vulnerability to anxiety.26 Thus, stress can be expressed over time through emotional and somatic roots, implying that researchers and clinicians should remain open minded regarding the course of symptoms of anxiety and screen for both anxiety and somatisation. High stable anxiety and elevated levels of arousal which accompany such stress conditions may change bodily sensations and produce physiological changes that may have manifestations in various conditions and diseases.27 Moreover, the COVID-19 pandemic seemed to trigger specific somatic schemata and thoughts of health/illness in particular among high anxious people with a more vulnerable anxiety trajectory.27 Finally, among highly anxious individuals with a chronic and exacerbated course, worries may switch between the fear of COVID-19 and the fear of other diseases (somatisation).
A similar finding emerged with regard to trajectories of adjustment disorder; as expected, groups with stable-high and exacerbation trajectories (before and after a second lockdown) of adjustment disorder reported higher levels of somatic symptoms in T2 compared to the stable-low group. One possible explanation may be related to multifaceted changes people experienced during cumulative lockdown periods. Adaptability to such rapid and profound change has been undoubtedly a challenging process, suggesting increase in stress levels of many individuals that are associated with somatic symptoms. In line with this notion, it was found that cumulative psychosocial stressors predict greater somatic symptoms. Despite the high correlation between somatic symptoms with depression and anxiety, stressors predicted somatic symptoms even when controlling the above variables.28 In the current study, items for each of the variables namely adjustment disorder, anxiety and somatic symptoms were distinct, with no overlap between them.
Surprisingly, the recovery group-participants with probable mental health problems (anxiety or adjustment disorder at T1 and no probable anxiety or adustment disorder at T2), was associated with elevated risk for a somatic symptoms, compared to the resilient/stable-low trajectory. One possible explanation may be related to the difference between recovery and resilient/stable-low trajectories.13 While recovery implies a healthy pattern, it suggests a less adaptive coping as compared to the resilient/stable-low trajectory. The recovery trajectory was found to be a vulnerability pattern that is stress-related and associated with somatic symptoms. In line with this notion, it might be that the recovery trajectory group was able to cope better in comparison to the exacerbation and stable-high groups following the second lockdown.
Overall, the findings of the study show the association between anxiety and adjustment disorder trajectories with somatic symtpoms following a second lockdown during the COVID-19 pandemic. The global crisis of COVID-19 pandemic challenges countries with potential lockdowns. The healthcare system that administered the lockdown, politicians and public health officials who mandated it should carefully consider the need for such action given the costs to vulnerable parts of the population. Our data emphasise the importance of supporting individuals during lockdowns in order to reduce psychological distress, and the different types of trajectories evident in response to this continuous stressor. Moreover, the present findings may point to the importance of identifying and targeting somatic symptoms as indicators of mental health problems. This may be done by general practitioners who can include a brief somatic symptoms screening as part of a patient’s visit, especially during a crisis period. This may facilitate the management of mental health problems during uncertain times such as the COVID-19 pandemic, and in doing so may reduce costs and burden on the healthcare system. From a clinical perspective, interventions should be specific to vulnerable populations and take into consideration the specific burden that comes with stress among specific groups during the lifespan of a continuous stressor such as the global COVID-19 pandemic.
Discussion of methodology
We employed an online survey using quota sampling from a probability-based internet panel of the Israeli population. This had several advantages
First, internet penetration in Israel as of January 2021 is 88.0% (7.68 million out of 8.72 million) and percentage of mobile connections in Israel as of January 2021 is 116.9% (10.2 million out of 8.72 million) as some people have more than one mobile phone (https://datareportal.com/reports/digital-2021-israel).
Second, online surveys have become important during the COVID-19 pandemic as traditional survey methods were less feasible.29
Third, obtaining high-quality behavioural data or mental health data in a longitudinal design during COVID-19 pandemic is still uncommon.29
Fourth, an online survey enabled us to collect real-time data regarding health and mental health.29
Fifth, online surveys can be created and deployed in very short time in comparison to traditional surveys.29 This is particularly important during an ongoing pandemic where a number of external factors (eg, infection rates and governmental response) change rapidly.
Sixth, people feel less reluctant to disclose sensitive information in an online format.30
However, all these benefits come with a price tag of selection bias. Selection bias can be reduced by using probability panels in countries with high internet penetration and high mobile connectivity. Using an online survey taken from a probability panel will have higher external validity and better generalisation of the general population in comparison to online surveys taken from non-probabilistic panel and countries with low internet penetration and mobile connectivity.
To sum, during COVID-19 pandemic, online surveys proved their value in collecting medical and mental health data. While the problem of selection bias still exists, the benefits and potential solutions to reduce this bias are justifying the use of online surveys.
Limitations
The findings of this study should be considered in the light of several limitations. The first and foremost is selection bias. However, using a probability-based internet panel that is weighted and dynamically adjusted to meet the Israeli Bureau of Statistics in terms of age and sex in a country with high internet penetration and mobile connections is one way to reduce selection bias. Second, while random stratified sampling is often preferable in comparison to quota sampling, the use of robust quota sampling enables a high response rate based on probability-based internet panel of the Israeli internet user population. This is highly valuable in longitudinal designs. Contrary to this, the use of random stratified sampling tends to yield lower response rates. A previous study based on the same probability-based internet panel using a random stratification sampling led to 31.00% response rate16 versus 76.17% response rate in the current study. We note that a probability sampling with low response rate suffers from the same potential bias as a non-probability sampling and therefore enjoys no clear advantage over a quota sampling.31
Study design considerations related to probability panels and real-time assessments can potentially reduce bias and increase the rigour of online surveys.
Moreover, quota sampling reflects the general population can be deployed when time constraints exist such as lockdowns during COVID-19 pandemic. Using stratified random samples before and after a second lockdown could lead to the miss of time window for sampling. In addition, the COVID-19 pandemic increased the homogeneity in the population related to the shared experience of the pandemic. In such conditions wherein homogeneity increases, quota sampling has further advantages, and it was found to have similar estimates compared with probability sampling.32
However, we did not have pre-COVID-19 assessments of mental health conditions. We did not measure somatic symptoms before the second lockdown was applied (T1). It could be that somatic symptoms exacerbated the mental health symptoms. Earlier somatisation symptoms may serve as marker of later stress reactions. Finally, reliance on self-report data may be liable to recall bias when assessing the occurrence of mental health symptoms.
In conclusion, lockdowns should be viewed as multifaceted by impacting health and mental health. While lockdowns prevent the spread of an infection, this may be at the cost of health and mental health. Our study strengthens the argument that a lockdown during a pandemic is a double-edged sword.
Supplementary Material
Acknowledgments
The authors thank Ariel University Research Authority for the continuous support for basic research.
Footnotes
Contributors: MB-E, RG, YH-R and YL designed the study concept. MB-E, RG, YH-R, EL, YL wrote the paper. MB-E, YH-R, EL collected the data. MB-E and YL conducted the analyses. MB-E, YH-R, YL drafted the first version of the manuscript. RG, YH-R, EL critically reviewed the manuscript and had a significant intellectual contribution. Authors read and approve the final manuscript. MB-E and YL had full access to all data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: YH-R was funded by Ariel’s University Research Authority internal grant (RA2000000302).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by the Ethics Committee of Ariel University (AU-SOC-YHR-20200616). The sample was administered online, and all participants signed an electronic informed consent.
References
- 1.Kazlauskas E, Quero S. Adjustment and coronavirus: how to prepare for COVID-19 pandemic-related adjustment disorder worldwide? Psychol Trauma 2020;12:S22–4. 10.1037/tra0000706 [DOI] [PubMed] [Google Scholar]
- 2.Atalan A. Is the lockdown important to prevent the COVID-19 pandemic? Effects on psychology, environment and economy-perspective. Ann Med Surg 2020;56:38–42. 10.1016/j.amsu.2020.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ben-Ezra M, Sun S, Hou WK, et al. The association of being in quarantine and related COVID-19 recommended and non-recommended behaviors with psychological distress in Chinese population. J Affect Disord 2020;275:66–8. 10.1016/j.jad.2020.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goodwin R, Hou WK, Sun S, et al. Psychological and behavioural responses to COVID-19: a China-Britain comparison. J Epidemiol Community Health 2021;75:189–92. 10.1136/jech-2020-214453 [DOI] [PubMed] [Google Scholar]
- 5.Galatzer-Levy IR, Huang SH, Bonanno GA. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin Psychol Rev 2018;63:41–55. 10.1016/j.cpr.2018.05.008 [DOI] [PubMed] [Google Scholar]
- 6.Dragan M, Grajewski P, Shevlin M. Depression and anxiety in Poland during an early phase of the COVID-19 pandemic. Eur J Psychotraumatol 2021;12:1860356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rossi R, Socci V, Talevi D. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry 2020;11:790. 10.3389/fpsyt.2020.00790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shevlin M, Nolan E, Owczarek M, et al. COVID-19-related anxiety predicts somatic symptoms in the UK population. Br J Health Psychol 2020;25:875–82. 10.1111/bjhp.12430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang Y, Wang Y, Zeng L, et al. Prevalence and correlation of anxiety, insomnia and somatic symptoms in a Chinese population during the COVID-19 epidemic. Front Psychiatry 2020;11:568329. 10.3389/fpsyt.2020.568329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Creed FH, Davies I, Jackson J, et al. The epidemiology of multiple somatic symptoms. J Psychosom Res 2012;72:311–7. 10.1016/j.jpsychores.2012.01.009 [DOI] [PubMed] [Google Scholar]
- 11.Hinz A, Ernst J, Glaesmer H, et al. Frequency of somatic symptoms in the general population: normative values for the patient health Questionnaire-15 (PHQ-15). J Psychosom Res 2017;96:27–31. 10.1016/j.jpsychores.2016.12.017 [DOI] [PubMed] [Google Scholar]
- 12.Beutel ME, Wiltink J, Ghaemi Kerahrodi J, et al. Somatic symptom load in men and women from middle to high age in the Gutenberg Health Study - association with psychosocial and somatic factors. Sci Rep 2019;9:4610. 10.1038/s41598-019-40709-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol 2004;59:20–8. 10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- 14.Bonanno GA, Wortman CB, Lehman DR, et al. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. J Pers Soc Psychol 2002;83:1150–64. 10.1037/0022-3514.83.5.1150 [DOI] [PubMed] [Google Scholar]
- 15.Demidenko E. Sample size and optimal design for logistic regression with binary interaction. Stat Med 2008;27:36–46. 10.1002/sim.2980 [DOI] [PubMed] [Google Scholar]
- 16.Bodas M, Siman-Tov M, Kreitler S, et al. The role of victimization in shaping households' preparedness for armed conflicts in Israel. Disaster Med Public Health Prep 2018;12:67–75. 10.1017/dmp.2017.38 [DOI] [PubMed] [Google Scholar]
- 17.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 18.Shevlin M, Hyland P, Ben-Ezra M, et al. Measuring ICD-11 adjustment disorder: the development and initial validation of the International adjustment disorder questionnaire. Acta Psychiatr Scand 2020;141:265–74. 10.1111/acps.13126 [DOI] [PubMed] [Google Scholar]
- 19.Gierk B, Kohlmann S, Kroenke K, et al. The somatic symptom scale-8 (SSS-8): a brief measure of somatic symptom burden. JAMA Intern Med 2014;174:399–407. 10.1001/jamainternmed.2013.12179 [DOI] [PubMed] [Google Scholar]
- 20.Tay AK, Rees S, Steel Z, et al. Six-year trajectories of post-traumatic stress and severe psychological distress symptoms and associations with timing of trauma exposure, ongoing adversity and sense of injustice: a latent transition analysis of a community cohort in conflict-affected Timor-Leste. BMJ Open 2016;6:e010205. 10.1136/bmjopen-2015-010205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jia R, Ayling K, Chalder T, et al. Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open 2020;10:e040620. 10.1136/bmjopen-2020-040620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020;7:547–60. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Solomon Z, Bachem R, Levin Y, et al. Long-Term trajectories of posttraumatic stress disorder: categorical versus continuous assessment. Psychiatry 2018;81:376–90. 10.1080/00332747.2018.1485369 [DOI] [PubMed] [Google Scholar]
- 24.Bonanno GA, Kennedy P, Galatzer-Levy IR, et al. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabil Psychol 2012;57:236–47. 10.1037/a0029256 [DOI] [PubMed] [Google Scholar]
- 25.Li G, Jiang Z, Kang X, et al. Trajectories and predictors of anxiety and depression amongst infertile women during their first IVF/ICSI treatment cycle. J Psychosom Res 2021;142:110357. 10.1016/j.jpsychores.2021.110357 [DOI] [PubMed] [Google Scholar]
- 26.Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19: longitudinal analyses of 36,520 adults in England. Lancet Psychiatry 2021;8:141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ran L, Wang W, Ai M, et al. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: a study of the general population in China at the peak of its epidemic. Soc Sci Med 2020;262:113261. 10.1016/j.socscimed.2020.113261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haftgoli N, Favrat B, Verdon F, et al. Patients presenting with somatic complaints in general practice: depression, anxiety and somatoform disorders are frequent and associated with psychosocial stressors. BMC Fam Pract 2010;11:67. 10.1186/1471-2296-11-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hlatshwako TG, Shah SJ, Kosana P, et al. Online health survey research during COVID-19. Lancet Digit Health 2021;3:e76–7. 10.1016/S2589-7500(21)00002-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gnambs T, Kaspar K. Disclosure of sensitive behaviors across self-administered survey modes: a meta-analysis. Behav Res Methods 2015;47:1237–59. 10.3758/s13428-014-0533-4 [DOI] [PubMed] [Google Scholar]
- 31.Brick JM. The future of survey sampling. Public Opin Q 2011;75:872–88. 10.1093/poq/nfr045 [DOI] [Google Scholar]
- 32.Yang K, Banamah A. Quota sampling as an alternative to probability sampling? an experimental study. Sociol Res Online 2014;19:56–66. 10.5153/sro.3199 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.