Abstract
Purpose
The COVID-19 pandemic has put tremendous strain on healthcare systems. Surgical societies worldwide have advised minimizing non-essential surgeries in order to preserve hospital resources. Given the medical resources and COVID-19 incidence between countries across the world differ, so should colorectal practices. No formal guidelines have emerged from Asia. We wanted to find out what the current practice was in Asian colorectal centres outside China.
Introduction
The COVID-19 pandemic has significantly impacted surgical practice worldwide. At the time of the writing of this paper, there are over 4.2 million cases reported with deaths exceeding 290 000 patients.1 With an abrupt disruption to worldwide supply chains, societal lockdowns and surge of cases into many hospitals, resource allocation was diverted and prioritised for all COVID-19 related services.
Methods
A questionnaire survey of current colorectal practice was carried out involving 3 major colorectal cancer centres, one each from 3 major cities: Singapore, Taichung and Daegu. Components of the survey include infrastructure and manpower, case selection, surgical approach, operating room management and endoscopy practice.
Results
All 3 centres continued to provide standard-of-care colorectal cancer surgery despite the COVID-19 pandemic. Two centres deferred surgery for benign colorectal conditions. Minimally Invasive Surgery (MIS) was still the preferred approach when indicated but with protocolized precautions undertaken. Other services such as pelvic exenteration, TATME and pelvic lymph node dissection were still offered if oncologically indicated. Elective diagnostic endoscopy services have also continued in two centres.
Conclusion
Elective colorectal services continue to take place in the 3 surveyed Asian hospitals with heightened precautions. Provided there is adequate resource, colorectal cancer services should still continue to prevent consequences of neglecting or delaying cancer treatment. Practice should hence be tailored to the local resource of individual centres accordingly.
Keywords: COVID-19, Colorectal, Cancer, Endoscopy, Operating theatre, Personal protection equipment
Introduction
Indeed, during the onset of the global pandemic, the early guidance from numerous societies was to reschedule elective endoscopy and surgery.2 , 3 Much of the rational was on conservation of Personal Protective Equipment (PPE) as well as due to limitations of Intensive Care Unit (ICU) beds. Surgeons were also deployed in various areas to augment management of COVID-19 patients. For colorectal surgery specifically, there has been due consideration to consider stoma creations rather than anastomosis, and only to reserve Minimally invasive surgery (MIS) for selected cases.4 While there has been no data published, these approaches do suggest a compromise to the usual standard of colorectal cancer care.
In the last few months, the pandemic has shifted epicentres to Europe and US and thus most of the practice guidelines issued have been country and disease incidence specific.2, 3, 4 Asian countries outside China have generally had a relatively lower COVID-19 incidence.1 In South Korea, Taiwan and in Singapore, we too have had our challenges in adopting different strategies to manage the disease as well. To a certain extent, the three cities have had relatively controlled disease outbreaks without experiencing overwhelmed health care systems. In Singapore for example, while elective cases have been reduced to plan for any surge, we have not adopted the same guidelines entirely. For colorectal cancer surgery, MIS can proceed but with the necessary PPE precautions in place.5 , 6
The aim of this paper is to elicit and compare what the current practices were in these 3 Asian cities. In this paper, we surveyed the practice in representative cancer centres, with regards to management of colorectal cancer surgery, followed by a review of the international guidelines.
Methods
The authors surveyed a colorectal center from Singapore, Daegu in South Korea and Tai Chung in Taiwan. These 3 cities were chosen to represent 3 nations outside China with reasonable control of COVID-19 and had adequate resources to provide colorectal cancer surgery despite the pandemic.
The centers surveyed were Sengkang General Hospital (SKH), a 1000-bedded hospital in Singapore, Kyungpook National University Hospital (KNUH), a 644-bedded hospital in Daegu, South Korea, and Chinese Medical University Hospital (CMUH), a 2000-bedded hospital in Taichung, Taiwan. Though there may be other hospitals in the respective cities, these hospitals were selected as these were the practicing hospital of the authors and they were deemed representative of each respective country. This judgement was based on an adequate hospital size, reputation and had a colorectal cancer case load of more than 20 cases per surgeon per year.
An English online self-administered survey was distributed to the Heads of Department of the colorectal units. The survey was divided into five components:
-
a)
Local infrastructure and manpower
-
b)
Case selection
-
c)
Surgical Approach
-
d)
Operating Room Management
-
e)
Endoscopy
Results
The colorectal departments had a mean of 7 accredited colorectal subspecialist surgeons (range 4–12) and handled a mean of 630 (range 200–1000) colorectal cancer resections per year. The mean caseload per surgeon in all centres exceeded the recommended minimum of 20 colorectal cancer resections per year required for accreditation.7 The Singaporean unit surgeons spend a proportion of time covering COVID-19 related services while surgeons in Taiwan and Korea were not redeployed at all.
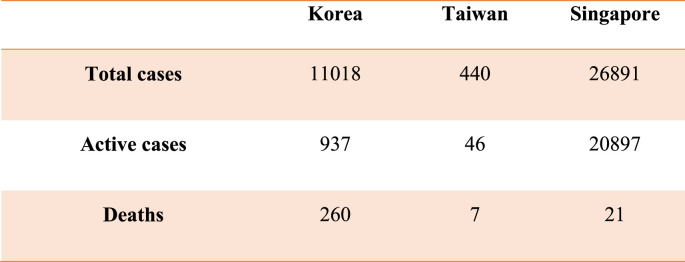
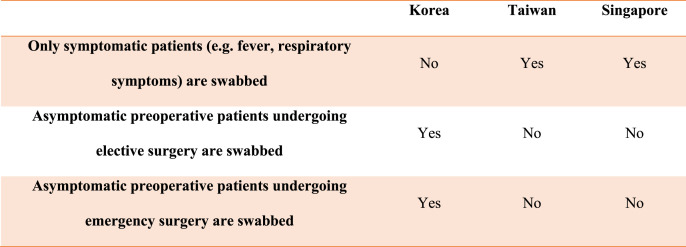
Each unit had a mean of 21 (range 14–30) intensive care unit (ICU) beds within their hospital. All hospitals, at the time of writing had managed a mean total of 118.3 (range 5–300) COVID-19 cases. At the time of manuscript preparation, the COVID-19 case load of each country is summarized in Fig. 1 with the highest incidence in Singapore followed by Korea then Taiwan.8 The screening process of surgical patients for COVID-19 in each unit is summarized in Fig. 2 . Singapore and Taiwan only screened symptomatic patients while the Korean centre also screened asymptomatic elective and emergency patients. There were no reported false negative COVID-19 tests in surgical patients, i.e. patients diagnosed as being COVID-19 negative but turned out to actually be positive later.
Fig. 1.
COVID-19 statistics for each country.8
Fig. 2.
COVID-19 screening for surgical patients.
Case selection
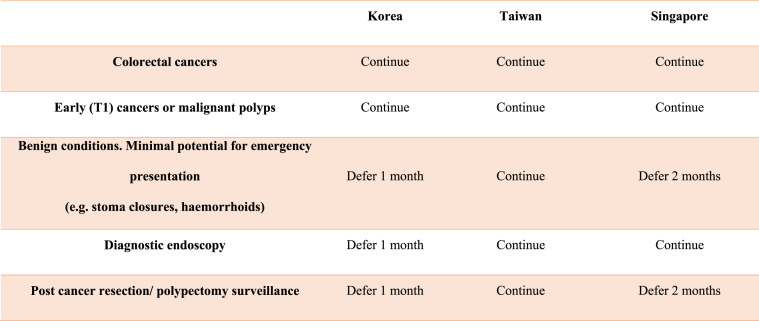
All institutions continued with colorectal cancer surgery as per usual, inclusive of early cancers and malignant polyps. Apart from Taiwan, other institutions postponed benign cases which had minimal potential for emergency presentation. Elective diagnostic endoscopy continued in the Taiwan and Singaporean centre while in Korea was deferred by a month. With the exception of Taiwan, surveillance endoscopy (post polypectomy and cancer resection) was deferred. Results are summarized in Fig. 3 .
Fig. 3.
Case selection for surgery and endoscopy.
Surgical Approach
All units continued elective colorectal cancer surgery as per standard of care. All chose to practice an MIS-preferred approach for cancer resections. This was for both non-COVID-19 and COVID-19 positive/suspected cases. All 3 units still continued to offer other colorectal operations, if usually performed and indicated, such as Transanal Total Mesorectal Excision (TaTME), robotic surgery, pelvic lymph node dissection and pelvic exenteration.
During laparoscopic surgery, all units continued to use advanced energy devices. The use of a smoke evacuation system was mandatory in the Taiwan unit but not for the other two. In two of the units (Taiwan, Singapore) there was a formal pneumoperitoneum evacuation protocol at end of procedure. In the Taiwan unit, pneumoperitoneum is extracted via smoke evacuator at the end of the procedure. In the Singapore unit, all personnel inside the theatre should have on an N95/PAPR during evacuation of pneumoperitoneum and the theatre doors are locked for 20 min after to allow adequate ambient air exchange.
PPE protocols
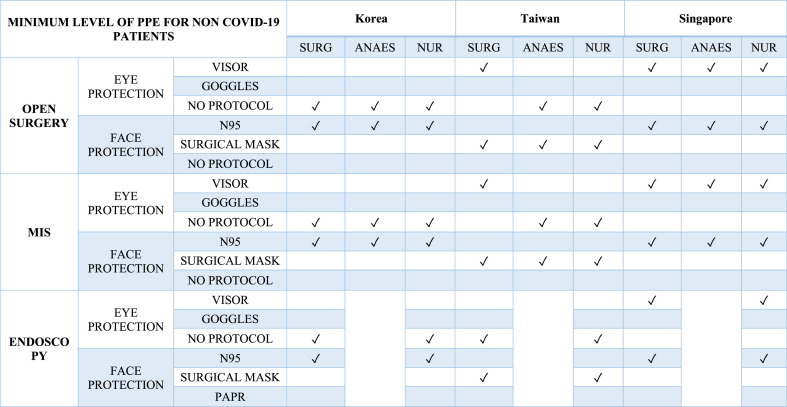
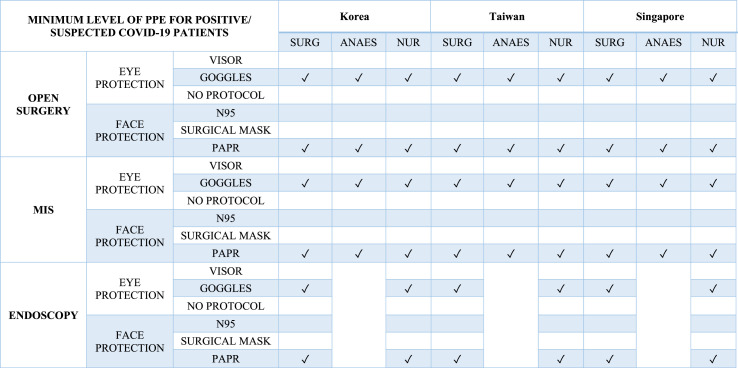
The PPE posture for each unit for operating theatre and endoscopy is summarized for non-COVID-19 patients (Fig. 4 ) and COVID-19 positive/suspected cases (Fig. 5 ).
Fig. 4.
PPE posture for Non-COVID-19 patients. (PAPR: Powered Air Purifying Respirators, SURG: Surgeon, ANAES: Anaesthetist, NUR: Nurse)).
Fig. 5.
PPE posture for COVID-19 positive/suspected patients. (PAPR: Powered Air Purifying Respirators, SURG: Surgeon, ANAES: Anaesthetist, NUR: Nurse).
Non-COVID-19 patients include those who have tested negative for COVID-19 or do not fulfil local criteria as a suspect case. For non-COVID-19 patients, Singapore adopted a higher level of protection than usual with N95 and visors for all personnel in endoscopy and operating theatre during both MIS and open surgery. Korea had a similar practice for face PPE, but eye protection had no fixed regulation. Practice in Taiwan reflected international guidance more with the use of facemasks for non-COVID-19 cases.
For COVID-19 positive/suspected cases, the posture was the same for all 3 units, with eye goggles and Powered Air Purifying Respirators (PAPR) for all personnel in theatre and endoscopy. In all 3 units, there were purposefully designed and dedicated operating theatres and endoscopy suites for COVID-19 positive/suspect patients.
Up to the time of the survey, all 3 surgical units did not have any patient to surgeon or patient to patient COVID-19 transmission. This indicates screening of surgical patients and PPE protocols were effective.
Discussion
The COVID-19 pandemic has had a significant impact on medical services worldwide. The pandemic has evolved so rapidly that various surgical societies have had to develop guidelines based on extrapolations of scarce existing data without the luxury of large studies. These guidelines from Europe,9 USA,2 , 3 UK10 and Australia,11 have had to balance the safety of health care workers (HCWs), surgical case load and limited resources. There has been limited literature from Asian countries outside China. In Singapore, while no formal guidelines have been issued, we have published some opinion papers.5 , 6 , 12 , 13 Some of the existing guidelines and rationales proposed are as follows:
-
a.
Case selection and triage
In the early days of the pandemic, evidence of overwhelmed hospital services was extrapolated from cities such as Wuhan and Lombardy in Italy. As such, much of the advice was to abandon elective surgery, defer elective endoscopy, minimize laparoscopic approach and choose stoma over anastomosis. These guidelines are summarized in Table 1 .
Table 1.
Summary of early practice recommendations.
| Recommendations regarding Surgical Response to COVID-19 | SAGES and EAES (29 Mar 2020)2 | Intercollegiate General Surgery Guidance (27 Mar 2020)14 | American College of Surgeons (24 Mar 2020)15 |
|---|---|---|---|
| Endoscopy | Postpone elective cases | Only emergency endoscopy | NA |
| Surgery | Postpone elective cases | Largely confined to emergency surgery. Stoma formation to be considered rather than anastomosis | Tiered approach for cancer cases depending on hospital resources |
In subsequent guidelines produced, there have been some modifications which take into account the hospital COVID-19 disease burden.15 , 16 These have recommended a tiered approach considering the clinical urgency of the colorectal cancer and the ICU bed availability of the individual hospital.
The approach in Taichung did not defer non-cancer operations unlike in Singapore and Daegu, this was possibility due to a lower rate of increase of COVID-19 in Taiwan compared to the other two countries. The reduction of non-time sensitive procedures in Singapore and South Korea reflects the national priority to ensure the availability of ICU/HD facilities and PPE resources to cater for the rapid surge of cases observed.
-
b.
Operating Room Management and PPE Guidelines
Numerous guidelines have emerged during the COVID-19 pandemic regarding levels of PPE required during surgical procedures. Considerations are given to whether the patients are COVID-19 positive/suspects or COVID-19 negative/non-suspects. In addition, procedures are divided into Aerosol Generating Procedures (AGP) and Non-AGPs. Guidelines are summarized in Table 2 .
-
i)
Operations on non-COVID-19 patients
Table 2.
PPE guidelines in operating theatre. (FM: Face Mask. AGP: Aerosol Generating Procedure).
| Australia11 | UK17 | USA (FACS)18 | |
|---|---|---|---|
| Non-COVID-19 Patients | Surgical FM Eye Protection For both AGP and non-AGP procedures |
Not stated | Surgical FM |
| COVID-19 Positive/Suspected Patients | AGP: N95/PAPR Non-AGP: Fluid resistant FM level 2/3 |
AGP: PAPR/N95, eye protection Non-AGP: Fluid resistant surgical mask (type IIR), eye protection |
AGP: N95/PAPR, eye protection Non-AGP: Eye protection, Surgical FM |
Most guidelines prescribe surgery in this group of patients can be performed just using standard surgical face masks.11 , 18
-
ii)
Operations on COVID-19 positive patients
For surgical procedures on COVID-19 positive or suspected cases, the general consensus worldwide is similar. It is recommended that if possible, there should be an operating theatre dedicated only for COVID-19 patients.12 Ideally the COVID-19 theatre should be stationed away from the main corridor traffic. There should be specific ingress and egress doors for personnel into the theatre. Also, a dedicated changing area for the donning and doffing of PPE. During intubation and extubation, as this is an AGP, all personnel in the room should be protected. All guidelines would recommend that all personnel in theatre wear an N95 or PAPR and eye protection.11 , 17 , 18
From our survey of these three Asian centres, surgery for colorectal cancer cases is proceeding largely as per normal but with measures in place. MIS surgeries and limited diagnostic endoscopy services have not had national restrictions imposed. As evidence grows, unlike previous influenza epidemics such as Severe Acute Respiratory Virus (SARS) and H1N1, the COVID-19 pandemic looks likely to have a protracted course. Thus, while initial international approaches to contain the disease and mitigate resource limitations was correct, a balanced approach to elective procedures has to be obtained. Evidently, prolonged deferment of diagnostic endoscopy and cancer surgery can lead to delayed diagnosis, increased disease complications, and perhaps reduced long term cancer survival.19 , 20
For colorectal cancer, advanced disease complications such as obstruction, bleeding or perforation conversely leads to higher resource utility and prolonged hospitalisation. Emergency colorectal surgery is certainly associated with higher morbidity and mortality rates of up to 33%.21 The argument of stoma creation as a temporising measure to reduce complications, or worse still as a permanent one, is also arguable. Stoma care will require frequent help from stoma therapists for skin care, admissions for fluid and electrolyte imbalances with possible long-term kidney injury sequelae. In addition, it adds on to patients’ and caregiver psychosocial burden and emotional distress on top of accepting the diagnosis of having a cancer. The utility of resources therefore in the medium and long-term perhaps is not advisable for healthcare systems that already face huge pressures.
In Taiwan, the COVID-19 burden has been the lowest among the 3 cities surveyed and elective work has not been interrupted. Like many of the guidelines, Taiwan surgeons utilised surgical FM for both MIS and open surgeries. In Daegu which was the epicentre of the outbreak in South Korea, rapid disease containment from mass screening has allowed a rapid restoration of normality in the country's healthcare system. Swabbing pre-operatively has been widely employed in Daegu and is the only city to do so and this high testing capability of South Korea, has certainly been one of their success stories in disease containment. Nonetheless, the protocol of an efficacious diagnostic swabbing remains debatable due to the presence of pre-symptomatic cases.22 , 23 Despite the presence of presumed negative swabs, South Korean surgical teams still adopt N95 postures for all open and MIS cases.
In Singapore, the trajectory of the disease remains on the ascendancy and has one of the highest volumes of COVID-19 patients in Asia. Nonetheless, the majority of affected patients are young migrant workers which are managed in the community isolation facilities. Community transmission has been low and hence hospital healthcare resources have remained comfortable to date. In view of a high disease burden, our unit has adopted N95 postures for all open and MIS surgeries to avoid unintentional exposure. With conflicting evidence of COVID-19 virus in the peritoneal fluid, a heightened PPE stance was justifiable to preserve the health of healthcare workers. (26,27) This practise however, is not universally applied across all healthcare institutions in Singapore.
Open vs Minimally Invasive Surgery (MIS)
Guidelines have advised caution when performing MIS due to the perceived danger of pneumoperitoneum.14 Studies have investigated the potential deleterious effects of surgical smoke on the health of theatre staff.24 It is known at smoke and vapour emitted during surgery can contain viruses.19
It must be noted however that most viral studies about this topic have investigated the Human Immunodeficiency Virus (HIV)20 and papilloma virus19 Although studies demonstrate presence of virus in the smoke, none have shown that this translates to an increased risk of infection in surgeons of that respective virus.25 It must also be considered that open surgery does also produce smoke which evacuates into the ambient theatre air.
In Singapore, we have performed and reported a laparoscopic appendicectomy for a positive COVID-19 patient whereby the peritoneal fluid cultures were negative.26 A report from Italy on a COVID-19 patient with small bowel obstruction however did reveal positive peritoneal fluid cultures for SARS-COV-2.27
So, while the evidence remains indeterminate, it is clear that necessary aerosolization risk mitigation measures must be adopted for safe surgery to be performed. MIS has been largely the standard of care for colorectal resections. Compared to open surgery, benefits of MIS include shorter hospital stay,28 lower rates if ICU admission and less blood transfusion requirements.29 For safe MIS surgery, the advice is to reduce air insufflation pressures, lower power settings on diathermy/energy generators and to use a smoke evacuator.2 , 18
One additional safety measure has been suggested. Most operating theatres have an average of 15–40 air exchanges per hour. 14–18 min is thus required to ensure clean operating theatre air for staff. In our institution, an intubation-extubation protocol has been in practice since the COVID-19 outbreak. In this protocol, a 5-min pause has been mandated during intubation and extubation, with only the anesthetists and assistant in OR wearing full PPE. This ensures at least two gas exchanges of the OR and enhances safety in the scenario that surgeons are operating on an undiagnosed COVID-19 case. To address the concerns of laparoscopy, an additional 15 min has been factored in, which commences on evacuation of the pneumoperitoneum.13 This has been echoed by proponents of MIS such as the society of Endoscopic and Laparoscopic Surgeons of Asia (ELSA).30
Conclusion
Deferment of cancer surgery will have a clinical impact especially if the pandemic has a protracted course. Hospitals should tailor their cancer services according to the available PPE and ICU resource on top of the trend of the COVID-19 disease burden. Given sufficient resources, it is still safe to proceed with cancer related work in a fashion each centre is comfortable with prior to the outbreak.
Funding
Not applicable.
Conflicts of interest/Competing interests
No conflicts of interest to declare.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors' contributions
Conceptualization: All authors.
Material preparation, data collection and analysis were performed by Foo Fung Joon, Leonard Ho Ming Li, Soo Yeun Park, William Tzu Liang Chen.
Manuscript prepared and edited by all authors. All authors read and approved the final manuscript.
References
- 1.COVID-19 situation reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Accessed 15 May. [Google Scholar]
- 2.SAGES. 2020. (2020) SAGES and EAES recommendations regarding surgical Response to COVID-19 crisis.https://www.sages.org/recommendations-surgical-response-covid-19/ Accessed 28 Apr. [Google Scholar]
- 3.Am. Coll. Surg. 2020. March 13 O, 2020 COVID-19: recommendations for management of elective surgical procedures.https://www.facs.org/covid-19/clinical-guidance/elective-surgery Accessed 28 Apr. [Google Scholar]
- 4.Coll R., Edin Surg, editors. Intercollegiate general surgery guidance on COVID-19 UPDATE. 2020. https://www.rcsed.ac.uk/news-public-affairs/news/2020/march/intercollegiate-general-surgery-guidance-on-covid-19-update Accessed 28 Apr. [Google Scholar]
- 5.Chew M., Koh F., Ng K. A call to arms: a perspective of safe general surgery in Singapore during the COVID-19 pandemic. Singap Med J. 2020 doi: 10.11622/smedj.2020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chew M.H., Tan W.J., Ng C.Y., Ng K.H. Deeply reconsidering elective surgery: worldwide concerns regarding colorectal surgery in a COVID-19 pandemic and a Singapore perspective. Singap Med J. 2020 doi: 10.11622/smedj.2020070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moran B., Cunningham C., Singh T., et al. Association of coloproctology of Great Britain & Ireland (ACPGBI): guidelines for the management of cancer of the colon, Rectum and Anus (2017) – surgical management. Colorectal Dis. 2017;19:18–36. doi: 10.1111/codi.13704. [DOI] [PubMed] [Google Scholar]
- 8.Coronavirus Update (Live): 4,569,106 Cases and 304,798 Deaths from COVID-19 Virus Pandemic - Worldometer. 2020. https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1?%22%20%5Cl%22countries Accessed 15 May. [Google Scholar]
- 9.Zheng M.H., Boni L., Fingerhut A. Minimally invasive surgery and the Novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Recommended PPE for Healthcare Workers by Secondary Care Inpatient Clinical Setting, NHS and Independent Sector. 1.
- 11.Health AGD of . Aust. Gov. Dep. Health. 2020. Guidance on the use of personal protective equipment (PPE) in hospitals during the COVID-19 outbreak.https://www.health.gov.au/resources/publications/guidance-on-the-use-of-personal-protective-equipment-ppe-in-hospitals-during-the-covid-19-outbreak Accessed 1 May 2020. [Google Scholar]
- 12.Ti L.K., Ang L.S., Foong T.W., Ng B.S.W. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth J Can Anesth. 2020 doi: 10.1007/s12630-020-01617-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan W.J., Foo F.J., Sivarajah S., Ho L.M.L., Koh F.H., Chew M.H. Safe colorectal surgery in the COVID-19 era - a Singapore experience. Ann Coloproctol. 2020;36:65–69. doi: 10.3393/ac.2020.04.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Surg R. Coll., editor. Updated intercollegiate general surgery guidance on COVID-19. 2020. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/ Accessed 2 May. [Google Scholar]
- 15.Surg Am Coll., editor. March 24 O, 2020 COVID-19 guidelines for triage of colorectal cancer patients. 2020. https://www.facs.org/covid-19/clinical-guidance/elective-case/colorectal-cancer Accessed 2 May. [Google Scholar]
- 16.SAGES. 2020. (2020) SAGES recommendations regarding surgical management of colorectal cancer patients during the Response to the COVID-19 crisis.https://www.sages.org/recommendations-surgical-management-colorectal-cancer-covid-19/ Accessed 2 May. [Google Scholar]
- 17.COVID-19 Personal Protective Equipment (PPE) GOV; UK: 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe Accessed 2 May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Surg Am Coll., editor. April 1 U on, 2020 | COVID-19: considerations for optimum surgeon protection before, during, and after operation. 2020. https://www.facs.org/covid-19/clinical-guidance/surgeon-protection Accessed 1 May. [Google Scholar]
- 19.Garden J.M., O'Banion M.K., Shelnitz L.S., et al. Papillomavirus in the vapor of carbon dioxide laser-treated verrucae. J Am Med Assoc. 1988;259:1199–1202. [PubMed] [Google Scholar]
- 20.Baggish M.S., Poiesz B.J., Joret D., Williamson P., Refai A. Presence of human immunodeficiency virus DNA in laser smoke. Laser Surg Med. 1991;11:197–203. doi: 10.1002/lsm.1900110302. [DOI] [PubMed] [Google Scholar]
- 21.Hogan J., Samaha G., Burke J., et al. Emergency presenting colon cancer is an independent predictor of adverse disease-free survival. Int Surg. 2015;100:77–86. doi: 10.9738/INTSURG-D-13-00281.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qian G., Yang N., Ma A.H.Y., et al. A COVID-19 Transmission within a family cluster by presymptomatic infectors in China. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020 doi: 10.1093/cid/ciaa316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei W.E. Presymptomatic transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okoshi K., Kobayashi K., Kinoshita K., Tomizawa Y., Hasegawa S., Sakai Y. Health risks associated with exposure to surgical smoke for surgeons and operation room personnel. Surg Today. 2015;45:957–965. doi: 10.1007/s00595-014-1085-z. [DOI] [PubMed] [Google Scholar]
- 25.Gloster H.M., Roenigk R.K. Risk of acquiring human papillomavirus from the plume produced by the carbon dioxide laser in the treatment of warts. J Am Acad Dermatol. 1995;32:436–441. doi: 10.1016/0190-9622(95)90065-9. [DOI] [PubMed] [Google Scholar]
- 26.Ngaserin S.H.-N., Koh F.H., Ong B.-C., Chew M.-H. COVID-19 not detected in peritoneal fluid: a case of laparoscopic appendicectomy for acute appendicitis in a COVID-19-infected patient. Langenbeck's Arch Surg. 2020 doi: 10.1007/s00423-020-01891-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coccolini F., Tartaglia D., Puglisi A., Giordano C., Pistello M., Lodato M., Chiarugi M. SARS-CoV-2 Is Present in Peritoneal Fluid in COVID-19 Patients. Ann Surg. 2020 Sep 1;272(3):e240–e242. doi: 10.1097/SLA.0000000000004030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hewett P.J., Allardyce R.A., Bagshaw P.F., et al. Short-term outcomes of the Australasian randomized clinical study comparing laparoscopic and conventional open surgical treatments for colon cancer: the ALCCaS trial. Ann Surg. 2008;248:728–738. doi: 10.1097/SLA.0b013e31818b7595. [DOI] [PubMed] [Google Scholar]
- 29.Huang Y.-M., Lee Y.-W., Huang Y.-J., Wei P.-L. Comparison of clinical outcomes between laparoscopic and open surgery for left-sided colon cancer: a nationwide population-based study. Sci Rep. 2020;10:1–7. doi: 10.1038/s41598-019-57059-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shabbir A., Menon R.K., Somani J., et al. ELSA recommendations for minimally invasive surgery during a community spread pandemic: a centered approach in Asia from widespread to recovery phases. Surg Endosc. 2020 doi: 10.1007/s00464-020-07618-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.