Abstract
Purpose
Transition back into the community following acute management of acquired brain injury (ABI) is a critical part of recovery. Post-acute rehabilitation and transitional care can significantly improve outcomes. The Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT (ABI-RESTaRT) is a novel whole-population cohort formed to better understand the needs of individuals with ABI receiving post-acute rehabilitation and disability services in Western Australia (WA), and to improve their outcomes. To do this a unique combination of (1) internal clinical/rehabilitation data, and (2) externally linked health data from the WA Data Linkage System was used, including hospitalisations, emergency department presentations, mental health service use and death records, to measure longitudinal needs and outcomes of individuals with ABI over 29 years, making this the largest, most diverse post-acute ABI cohort in Australia to date.
Participants
Whole-population cohort of individuals (n=1011) with an ABI who received post-acute community-based neurorehabilitation or disability support services through Brightwater Care Group from 1991 to 2020.
Findings to date
Comprehensive baseline demographic, clinical and rehabilitation data, outcome measures and linked health data have been collected and analysed. Non-traumatic brain injury (eg, stroke, hypoxia) was the main diagnostic group (54.9%, n=555), followed by traumatic brain injury (34.9%, n=353) and eligible neurological conditions (10.2%, n=103). Mean age at admission was 45.4 years, and 67.5% were men (n=682). The cohort demonstrated significant heterogeneity, socially and clinically, with differences between ABI groups across a number of domains.
Future plans
ABI-RESTaRT is a dynamic whole-population cohort that will be updated over time as individuals enrol in the service. Future analyses will assess longitudinal brain injury outcomes, the changing health and social needs of individuals with ABI and evaluate and inform post-acute services to best support these individuals.
Registration
This cohort is not linked to a clinical trial, and is not registered.
Keywords: rehabilitation medicine, stroke, neurological injury
Strengths and limitations of this study.
Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT (ABI-RESTaRT) is the largest Australian post-acute neurorehabilitation and disability support research cohort to date with a 29-year follow-up period.
The combined use of internal clinical and rehabilitation data and linked health data provides a detailed picture of ABI that could not be derived from a single data source; key measures include functional independence, health status and comorbidities, goal attainment, mental health and well-being, quality of life and 10-year mortality, offer a unique, holistic understanding of the needs and outcomes of individuals with ABI.
The cohort represents a diverse and complex population including individuals with non-traumatic brain injury, traumatic brain injury and eligible neurological conditions, providing a diverse range of brain injury experiences.
The study framework follows each cohort member from pre-injury to long-term follow-up after discharge from post-acute services, with a minimum 10-year look-back period (starting from 1981) and a mean follow-up time of 8.4 years following discharge.
A state-based data linkage register was used, so pre-admission or post-discharge follow-up data for cohort members based interstate or overseas will not be captured, and all clients were accessing services at a single organisation which may reduce the generalisability of findings.
Introduction
Acquired brain injury (ABI) is one of the leading causes of death and disability in Australia.1 Defined as any damage to the brain occurring after birth, ABI can be traumatic (caused by extrinsic forces to the head) or non-traumatic (eg, stroke, drug misuse, tumour, hypoxia/anoxia). Estimates suggest 2% of the population of Western Australia (WA) are living with an ABI.2 The consequences of ABI are complex and difficult to predict, but often lead to a range of impairments in cognitive, physical and psychosocial functioning.1–4 ABI can cause long-term physical disability and complex neurobehavioural effects. These can include neurological impairment (eg, motor function, sensory loss), medical complications (eg, spasticity, epilepsy), cognitive impairment (eg, memory deficits, language impairments, reduced consciousness), personality and behavioural changes (eg, impaired social skills) and lifestyle consequences (eg, loss of independence, reduced quality of life).5 Up to 75% of brain injuries in Australia occur in adults under 65 years of age,3 resulting in difficulties that can impact working ability, social engagement and community integration.6–8
Regaining independence and/or meaningful participation in life following an ABI is achievable. Transition back into the community following acute management of ABI in hospital is a critical phase of recovery, and adjustment to the cognitive, physical and behavioural impairments associated with ABI during transition predicts longer-term outcomes and overall recovery from brain injury.9 10 Post-acute care is important throughout the transition from acute services, such as hospitalisation, to home or community care, with clients and families often reporting the transition to be difficult and stressful.10 Individuals with inadequate supports risk poorer outcomes including development of a depressive disorder,9 re-hospitalisation or institutionalisation10 and reduced likelihood of returning to work.6
Post-acute care is defined as care occurring after the acute care period, with individuals who have achieved acute recovery, are medically stable, and no longer requiring hospitalisation.11 Post-acute care may occur immediately following discharge from hospital or at any time after the individual has achieved medical stability.12 The focus of post-acute care is on functional improvement and/or to support individuals to achieve meaningful participation in life, as distinct from physiological recovery.
Despite the importance of post-acute care for individuals with an ABI, little empirical evidence is available to enable service planning and policy development for this cohort. A number of community-based neurorehabilitation cohort studies examining the outcomes of individuals with ABI after rehabilitation exist in Australia.13–16 Two of these studies involved retrospective analysis of client data at discharge from community-based brain injury services in which individualised rehabilitation care was provided. The first study showed that ABI clients (n=63) who received rehabilitation services in Queensland between 2017 and 2018 had significantly improved physical outcomes compared with an historical ABI cohort who did not receive rehabilitation services between 2007 and 2009 (n=124).14 The second study, conducted with 47 ABI clients in South Australia from 2010 to 2013, demonstrated that outpatient rehabilitation significantly and immediately improved physical and psychosocial outcomes, although social well-being declined in the follow-up period.13 Client experiences of community-based rehabilitation have also been examined, with one study surveying clients (n=79) and their families (n=39) experiences following attendance to a brain injury rehabilitation unit in New South Wales from 2015 to 2017. This study indicated that person-centred care was critical to an individuals’ experience of care across a number of post-acute services.15 While this research has demonstrated the value of community-based rehabilitation, these cohort studies have small sample sizes (n<200), and short follow-up times (<3 years). Longer-term research examining the experiences of individuals accessing post-acute ABI services and the effectiveness of different types of post-acute care is required to ensure the best outcomes for individuals.
ABI-RESTaRT
The Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT (ABI-RESTaRT) is the largest research cohort of people with ABI who received post-acute rehabilitation or support services in Australia to date. The cohort is a whole-population cohort comprising of all individuals who received brain injury services through Brightwater Care Group in WA, from 1991 to 2020. Brightwater has been a main provider of post-acute community-based disability services for people with ABI in WA since 1991,17 with the goal to support people to meaningfully ‘restart’ their lives in the community after ABI.
The ABI-RESTaRT research programme uses a unique combination of internal clinical and rehabilitation data and external linked health data collections from the WA Data Linkage System.18 This enables longitudinal examination of the needs and outcomes of individuals with ABI over 29 years, making this the longest follow-up of individuals with ABI undergoing post-acute care in Australia to date.13–15 The aim of the ABI-RESTaRT research programme will focus on understanding the complex health and social needs of people with ABI during post-acute care, and identify predictors of short-term and long-term outcomes to facilitate effective service planning and delivery.
Aims
This cohort profile paper aims to: (1) describe the background and formation of ABI-RESTaRT, (2) outline data sources and key variables, (3) present baseline sociodemographic and clinical characteristics and (4) outline planned research for the cohort. Future publications will examine the specific outcomes of the cohort.
Cohort description
Cohort design and eligibility
ABI-RESTaRT is a retrospective whole-population cohort comprising all clients of Brightwater Care Group’s post-acute brain injury programmes and services (excluding respite) from inception on 15 March 1991 to 31 December 2020 (n=1011). Each individual’s entry date into the cohort represents the date of their index admission (first episode of care) to Brightwater’s community-based brain injury services.
The cohort consists of individuals with diverse brain injuries, including traumatic brain injuries (TBI), non-traumatic brain injuries (NTBI) and eligible neurological conditions, defined by the Australasian Rehabilitation Outcomes Centre (AROC) impairment codes.19 Table 1 summarises AROC diagnostic categories for the cohort. NTBI was the leading diagnostic category in the cohort (54.9%; 555 of 1011) with stroke (52.6%; 292 of 555) comprising over half of NTBI diagnoses. TBI accounted for 34.9% of the cohort (353 of 1011).
Table 1.
Brain injury diagnoses and Australasian Rehabilitation Outcomes Centre (AROC) impairment codes for the Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT (ABI-RESTaRT) cohort, 1991–2020
| AROC code, category and diagnosis | n (%) | |
| Non-traumatic (stroke) | 292 (28.9) | |
| 1.1 | Stroke—haemorrhagic | 81 (8) |
| 1.2 | Stroke—ischaemic | 178 (17.6) |
| 1.0 | Stroke—unspecified | 33 (3.3) |
| Non-traumatic (other—excluding stroke) | 263 (26) | |
| 2.11 | Subarachnoid haemorrhage | 58 (5.7) |
| 2.12 | Anoxic brain damage | 78 (7.7) |
| 2.13 | Encephalitis | 18 (1.8) |
| Meningitis | 6 (0.6) | |
| Neoplasm/tumour of brain, meninges or cranial nerves | 32 (3.2) | |
| Intracranial abscess | 2 (0.2) | |
| Hydrocephalus | 5 (0.5) | |
| Toxic encephalopathy | 35 (3.5) | |
| Metabolic encephalopathy | 7 (0.7) | |
| Other non-traumatic brain dysfunction | 22 (2.2) | |
| Traumatic | 353 (34.9) | |
| 2.21 | Traumatic, open injury | 50 (5) |
| 2.22 | Traumatic, closed injury | 280 (27.7) |
| 2.2 | Traumatic, unspecified | 23 (2.3) |
| Neurological | 103 (10.2) | |
| 3.1 | Multiple sclerosis | 16 (1.6) |
| 3.2 | Parkinsonism | 17 (1.7) |
| 3.3 | Polyneuropathy | 3 (0.3) |
| 3.4 | Guillain-Barré syndrome | 1 (0.1) |
| 3.8 | Neuromuscular disorders | 13 (1.3) |
| 3.9 | Extrapyramidal and abnormal movement disorders | 2 (0.2) |
| Spinocerebellar disease | 3 (0.3) | |
| Epilepsy | 31 (3.1) | |
| Other neurological and neurodegenerative disorders | 17 (1.7) | |
Each individual’s AROC diagnosis represents their primary brain injury diagnosis at index admission to Brightwater, but not necessarily their index brain injury. It is possible for individuals to have had prior brain injuries for which they did not access Brightwater services. Individuals with congenital neurological conditions (eg, cerebral palsy, spina bifida) or intellectual disabilities are eligible for services at Brightwater, but were excluded from the cohort. Admissions are accepted any time since injury, most often in the subacute (3–12 months post-injury) or chronic phases (>12 months post-injury).20 21
Cohorts, setting and programs
The overall cohort is comprised of four service delivery periods based on year of index admission to services: 1991–2002, 2003–2007, 2008–2013 and 2014–2020. These periods reflect significant change to service delivery programmes. Key changes are specified in table 2.
Table 2.
Key changes to programmes across four service delivery periods
| Service period | Programme (start date) | Service changes |
| 1991–2002 | TRP (1991) |
|
| SIL (1998) | 3. Commencement of long-stay brain injury accommodation. | |
| 2003–2007 | TRP |
|
| 2008–2013 | TRP |
|
| TAP (2008) | 3. Transitional Accommodation Program introduced. | |
| HACCSS (2009) | 4. Home and Community Care Social Skills Program introduced. | |
| 2014–2020 | TRP CAPB (2016) HACCSS |
|
CAPB, capacity building; HACCSS, Home and Community Care Social Skills; SIL, supported independent living; TAP, Transitional Accommodation Program; TRP, Transitional Rehabilitation Program.
Clients are able to be re-referred to Brightwater programmes, or transferred between programmes, as their goals and abilities change, and therefore can have multiple episodes of care. However, clients can only be enrolled in a single programme at any one time.
All programmes accept clients between the ages of 18–65 years, however acceptance to each programme is on a case-by-case basis. As such, some individuals outside of those age ranges have been admitted throughout the duration of the programmes. The five different community-based programmes are summarised below, ranging from full-time residential neurorehabilitation to casual home-based supports.
Transitional Rehabilitation Program
Beginning in 1991, the Transitional Rehabilitation Program was Brightwater’s first post-acute service for individuals with ABI and/or eligible neurological conditions. The programme is delivered at the Oats Street rehabilitation centre, a purpose-built community-based residential facility. The programme is funded by the WA Department of Health and can support up to 43 live-in residents, across eight group houses and eight independent living units, plus 10 additional home-based clients.
The Transitional Rehabilitation Program has a standard duration of 12–24 months, and aims to enable clients to regain the skills to live independently in the community. Clients participate in evidence-based, person-centred neurorehabilitation that is tailored to their individual goals, and are supported by an integrated multidisciplinary team of medical and allied health professionals.
The Transitional Rehabilitation Program is based on a novel model of care called Staged Community-Based Brain Injury Rehabilitation, whereby post-acute therapy and care services are provided in a stage-based approach to support a client’s continued recovery from ABI over time.22–24 On admission, clients are allocated to a house with levels of assistance appropriate for their needs, ranging from 24-hour continuous care to full independence, and graduate through stages with decreasing levels of support as their independence and functional abilities improve.24 The programme is able to support all stages of brain injury rehabilitation, from profound physical disability (including those in a minimally conscious state, in which there is reduced consciousness with evidence of environmental awareness25) to higher-level cognitive rehabilitation.
Supported Independent Living
Beginning in 1998, Supported Independent Living is a long-term supported accommodation programme for individuals with ABI who are funded by the Australian Governments’ National Disability Insurance Scheme26 (NDIS; from 2016), the Disability Service Commission (prior to 2016), or with private funding. This programme is designed for those who require additional supports to carry out activities of daily living but do not seek neurorehabilitation.27 Individuals in this programme live across eight shared houses for people with disability throughout the Perth metropolitan area.
Transitional Accommodation Program
The Transitional Accommodation Program commenced in 2008 and is funded by the WA Department of Health as a step down from hospital service.28 Referrals must come from a Perth metropolitan public hospital, and clients receive transitional care and short-term accommodation while they are supported to seek longer-term accommodation or make adjustments to existing homes. This programme operates in a socio-medical model, using short-term therapy, nursing and care supports to keep clients healthy and medically stable to promote natural recovery but does not involve comprehensive active rehabilitation. Clients in the programme can use NDIS funding to engage in activities and have sustainable discharge options. The Transitional Accommodation Program often involves setting up support structures for people with complex disabilities, including nursing and psychosocial complexity.
Home and Community Care Social Skills
Commencing in 2009, the Home and Community Care Social Skills programme provided support, privately, with Commonwealth Department of Health funding, for social engagement and activities as well as in-home care as required. This programme was for individuals with ABI who were at risk of social isolation or needed support around the home to maintain their independence. This programme began to be phased out in 2016 when the Capacity Building programme began, with no new clients accepted into the programme after June 2019.29
Capacity Building
The Capacity Building programme was launched in 2016 to replace the Home and Community Care Social Skills programme. Capacity Building offers home-based supports to individuals with ABI who have NDIS funding. The supports on offer include specialist neurorehabilitation therapy services, support coordination, equipment and assistive technology and behavioural assessment and support. Capacity Building clients are able to access services on an ad-hoc basis as determined by the client themselves, and have individually tailored rehabilitation or lifestyle goals that are achieved while living off-site.
Data sources and follow-up time
Figure 1A summarises the data sources for ABI-RESTaRT. The research programme uses a combination of internal clinical and rehabilitation data, and externally linked data collections from the WA Department of Health. Internal electronic medical records for each cohort member were probabilistically linked through the WA Data Linkage System18 to four external health data collections. We obtained data on hospitalisations (hospital morbidity data collection; 1981–2020), emergency department (ED) presentations (ED data collection; 2002–2020), deaths (mortality register, 1991–2020) and mental health (mental health information system; 1981–2020). The combination of internal and external data sources allows triangulation of information to ensure higher accuracy, continuity and completeness than could be derived from a single source.
Figure 1.
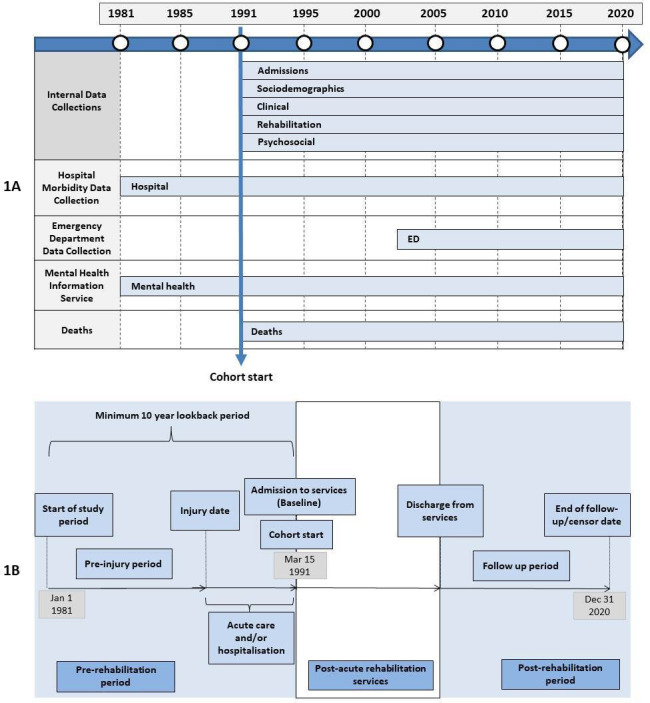
Data sources and study design for the ABI-RESTaRT (Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT) study, 1991–2020. (A) Internal and external data sources and, (B) study design.
Figure 1B summarises the ABI-RESTaRT design and follow-up time. The study framework follows each cohort member from pre-injury, acute care, post-acute care and long-term follow-up after discharge from post-acute services. For all cohort members, a minimum 10-year pre-admission look-back period is available to examine pre-injury morbidity patterns and acute care details. Linked data are obtained up to 31 December 2020 with a mean follow-up time of 8.4 years (range 0 years–29.2 years) following discharge from community-based services for each cohort member.
Key measures, variables and outcomes
Key outcome measures and variables available for ABI-RESTaRT are summarised in table 3. Study variables are primarily derived from clinical and administrative data collected as part of routine service provision. Key variables span five categories (Admissions, Demographics, Clinical, Rehabilitation and Psychosocial), offering a unique, holistic understanding of the needs and outcomes of individuals with ABI. Outcomes for each cohort member include functional independence, health status and comorbidities, goal attainment, mental health and well-being, quality of life and mortality.
Table 3.
Data sources, key measures and variables available for the ABI-RESTaRT study
| Date | Data source/type | Description | Key variables | |
| 1991–2020 | Admissions |
|
|
|
| 1991–2020 | Demographics |
|
||
| 1991–2020 | Clinical |
|
|
|
| 1991–2020 | Rehabilitation |
|
||
| 1991–2020 | Psychosocial |
|
||
| External | 1981–2020 | Hospital (HMDC) |
|
|
| 2002–2020 | Emergency department (EDDC) |
|
||
| 1981–2020 | Mental health (MHIS) |
|
||
| 1991–2020 | Deaths |
|
|
ABI-RESTaRT, Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT; ASGS, Australian statistical geography standard; ED, emergency department; EDDC, Emergency Department Data Collection; FIM+FAM, functional independence measure+functional assessment measure; GAS, Goal Attainment Scale; HMDC, Hospital Morbidity Data Collection; MHIS, Mental Health Information System; MPAI-4, mayo-portland adaptability inventory; NPDS, Northwick Park Dependency Score; NPTDA, northwick park therapy dependency assessment; NTBI, non-TBI; QOLIBRI, quality of life after brain injury; RCS, Rehabilitation Complexity Scale; SEIFA IRSD, socio-economic indexes for areas index of relative socioeconomic disadvantage; TBI, traumatic brain injuries; WA, Western Australia.
Table 4 outlines the availability of key outcome measures data for the cohort. As the cohort is a retrospective pragmatic cohort, available outcome measures data for each client differs depending on the service period, the outcome measures used at the time and the programme the client was admitted to. Comprehensive outcome measures were introduced across services in 2011, therefore, only a subset of the cohort have complete outcome measures.
Table 4.
Key ABI-RESTaRT outcome measures and data availability, 1991-2020 (n=1011)
| Key outcome measures and data | Years available | Clients with data | ||
| Total number, n | Of total cohort, % | Over years available, % | ||
| Internal data | ||||
| Functional Independence Measure and Functional Assessment Measure (FIM+FAM)51 | 2011–2020 | 383 | 37.9 | 57 |
| Mayo-Portland Adaptability Inventory-4 (MPAI-4)52 | 2011–2020 | 468 | 46.3 | 69.6 |
| Goal Attainment Scale (GAS)53 | 2011–2020 | 362 | 35.8 | 53.8 |
| Quality of Life After Brain Injury Inventory (QoLIBRI)56 | 2015–2020 | 94 | 9.3 | 19 |
| Northwick Park Dependency Score (NPDS)58 | 2011–2020 | 405 | 40.1 | 60.3 |
| Northwick Park Care Needs Assessment (NCPNA)57 | 2011–2020 | 405 | 40.1 | 60.3 |
| Rehabilitation Complexity Scale (RCS)54 | 2012–2020 | 354 | 35 | 56.9 |
| External data | ||||
| Hospital admissions | ||||
| Pre-admission | 1981–2020 | 1011 | 100 | – |
| Post-discharge (follow-up) | 1991–2020 | 829 | 81.9 | – |
| Emergency department presentations | – | |||
| Pre-admission | 2002–2020 | 692 | 68.4 | – |
| Post-discharge (follow-up) | 2002–2020 | 342 | 33.8 | – |
| Mental health information system | 1981–2020 | TBD | – | – |
| Death | 1991–2020 | TBD | – | – |
Mental health data not yet received. Updated death data not yet received.
ABI-RESTaRT, Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT; TBD, to be determined.
Data extraction, storage and security
Clinical records for active and historical ABI clients are stored within a secure internal clinical application (iCare). This data can only be accessed by users with appropriate security clearance, such as the researchers involved on the project, and relevant clinical and administrative staff. Archived historic client data is retained by the organisation and used for service evaluation and research purposes as needed. Clients provided consent on admission for their internal de-identified information to be used for service evaluation research.
Researchers extracted demographic, clinical and outcome measures data for the ABI-RESTaRT members from the iCare data warehouse using structured query language (SQL). Linked hospital and ED data were used to validate clinical diagnosis details, date of injury and cause of injury. For historic clients, researchers manually extracted admissions, demographic, clinical and outcome measures data from scanned documents (PDF) uploaded into the client’s clinical records. Researchers created a master ABI-RESTaRT database specifically for this study. This database is stored on a secure internal network drive which can only be accessed by the study investigators.
Statistical analysis
Extraction and analysis of baseline data was completed in February 2021. Basic demographic and brain injury characteristics at index admission are presented in the current cohort profile. Subsequent research will examine the health status, service use, and outcomes of the cohort in detail.
Baseline data were analysed using Stata V.16.0.30 Primary analyses were tested against an alpha level of 0.05 (uncorrected, two-tailed). Descriptive statistics were calculated and presented as mean±SD, or count (percentage). Independent samples t-tests, two-way analysis of variances and χ2 analyses were used to compare differences in continuous and categorical outcomes, respectively. Bonferroni correction was used for multiple comparisons.
Patient and public involvement
Patients or public were not involved in the development of the research question and project design or conducting the present study.
Findings to date
Sociodemographic characteristics
Table 5 summarises the baseline sociodemographic characteristics of ABI-RESTaRT. Mean age at admission was 45.4±15.5 years (range: 14.9 years–93.2 years), with 6.2% aged over 65 (n=63). Male clients (67.5%) outnumbered female clients (32.5%). The relatively young age and predominantly male cohort is consistent with other profiles of individuals seeking ABI services.13–15 The majority of the cohort was born in Australia (64.7%), with 3.4% of clients of Aboriginal and/or Torres Strait Islander background. Most of the cohort lived in a major city (84.3%) and were between average disadvantage and least disadvantaged levels of the Socio-Economic Index for Areas Index of Relative Socioeconomic Disadvantage before admission (72.3%).
Table 5.
Sociodemographic characteristics for the ABI-RESTaRT cohort at index admission to post-acute community-based brain injury support programmes, 1991–2020 (n=1011)
| Characteristics | Total, n=1011 |
1991–2002, n=231 |
2003–2007, n=145 |
2008–2013, n=220 |
2014–2020, n=415 |
| Sex, n (%) | |||||
| Male | 682 (67.5) | 150 (64.9) | 108 (74.5) | 156 (70.9) | 268 (64.6) |
| Female | 329 (32.5) | 81 (35.1) | 37 (25.5) | 64 (29.1) | 147 (35.4) |
| Age at admission, mean±SD | |||||
| Total | 45.4±15.5 | 44.1±21.5 | 39.5±12.5 | 44.2±12.8 | 48.8±12.9 |
| Male | 44.2±14.6 | 39.8±18 | 39.9±12.8 | 44.7±12.3 | 48±13.3 |
| Female | 47.9±17.1 | 51.9±25 | 38.3±11.6 | 43±13.9 | 50.2±12.1 |
| Age category at admission, n (%) | |||||
| <18 years | 15 (1.5) | 8 (3.5) | 3 (2.1) | – | 4 (1) |
| 18–29 | 190 (18.8) | 66 (28.6) | 36 (24.8) | 40 (18.2) | 48 (11.6) |
| 30–39 | 161 (15.9) | 46 (19.9) | 32 (22.1) | 34 (15.5) | 49 (11.8) |
| 40–49 | 223 (22.1) | 43 (18.6) | 43 (29.7) | 54 (24.6) | 83 (20) |
| 50–59 | 274 (27.1) | 19 (8.2) | 26 (17.9) | 78 (35.5) | 151 (36.4) |
| 60–69 | 102 (10.1) | 7 (3) | 5 (3.5) | 14 (6.4) | 76 (18.3) |
| ≥70 years | 46 (4.6) | 42 (18.2) | – | – | 4 (1) |
| Aboriginal and/or Torres Strait Islander, n (%) | |||||
| Total | 34 (3.4) | 2 (0.9) | – | 13 (5.9) | 19 (4.6) |
| Male | 24 (70.6) | 1 (0.5) | – | 11 (84.6) | 12 (63.2) |
| Female | 10 (29.4) | 1 (0.5) | – | 2 (15.4) | 7 (36.8) |
| Mean age ± SD | 38.8±13.6 | 31±0.8 | – | 40±15.2 | 38.8±13.4 |
| Marital status, n (%) | |||||
| Single | 444 (43.9) | 101 (43.7) | 76 (52.4) | 99 (45) | 168 (40.5) |
| De Facto | 38 (3.8) | 3 (1.3) | 2 (1.4) | 12 (5.5) | 21 (5.1) |
| Married | 253 (25) | 73 (31.6) | 30 (20.7) | 50 (22.7) | 100 (24.1) |
| Separated | 59 (5.8) | 13 (5.6) | 10 (6.9) | 12 (5.5) | 24 (5.8) |
| Divorced | 133 (13.2) | 14 (6.1) | 20 (13.8) | 35 (15.9) | 64 (15.4) |
| Widowed | 30 (3) | 16 (6.9) | 1 (0.7) | 3 (1.4) | 10 (2.4) |
| Unknown | 54 (5.3) | 11 (4.8) | 6 (4.1) | 9 (4.1) | 28 (6.8) |
| Country of birth, n (%) | |||||
| Australia (and external territories) | 654 (64.7) | 162 (70.1) | 98 (67.6) | 120 (54.6) | 274 (66) |
| New Zealand | 31 (3.1) | 9 (3.9) | 5 (3.5) | 5 (2.3) | 12 (2.9) |
| Maritime South-East Asia | 27 (2.7) | 3 (1.3) | 1 (0.7) | 6 (2.7) | 17 (4.1) |
| Mainland South-East Asia | 13 (1.3) | 3 (1.3) | 2 (1.4) | 2 (0.9) | 6 (1.5) |
| Southern Asia | 11 (1.1) | – | – | 3 (1.4) | 8 (1.9) |
| Chinese Asia | 9 (0.9) | 2 (0.9) | – | 2 (0.9) | 5 (1.2) |
| Southern and East Africa | 18 (1.8) | – | 2 (1.4) | 3 (1.4) | 13 (3.1) |
| UK | 84 (8.3) | 28 (12.1) | 12 (8.3) | 14 (6.4) | 30 (7.2) |
| Western Europe | 11 (1.1) | 2 (0.9) | 1 (0.7) | 4 (1.8) | 4 (1) |
| Southern Europe | 11 (1.1) | 2 (0.9) | – | 3 (1.4) | 6 (1.5) |
| Other | 44 (4.4) | 7 (3) | 4 (2.8) | 9 (4.1) | 24 (5.8) |
| Unknown | 98 (9.7) | 13 (5.6) | 20 (13.8) | 49 (22.3) | 16 (3.9) |
| Usual occupation, n (%) | |||||
| Managers | 26 (2.6) | 1 (0.4) | 4 (2.8) | 9 (4.1) | 12 (3) |
| Professionals | 49 (4.9) | 5 (2.2) | 3 (2.1) | 11 (5) | 30 (7.2) |
| Technicians and trades workers | 80 (7.9) | 3 (1.3) | 9 (6.2) | 24 (10.9) | 44 (10.6) |
| Community and personal service workers | 34 (3.4) | 2 (0.9) | 6 (4.1) | 8 (3.6) | 18 (4.3) |
| Clerical or administrative workers | 20 (2) | 1 (0.4) | 2 (1.4) | 5 (2.3) | 12 (2.9) |
| Sales workers | 10 (1) | – | 1 (0.7) | – | 9 (2.2) |
| Machinery operators and drivers | 31 (3.1) | 4 (1.7) | 2 (1.4) | 10 (4.6) | 15 (3.6) |
| Labourers | 48 (4.8) | 5 (2.2) | 6 (4.1) | 12 (5.5) | 25 (6) |
| Not in workforce | 206 (20.4) | 7 (3) | 15 (10.3) | 42 (19.1) | 142 (34.22) |
| Unknown | 507 (50.2) | 203 (87.9) | 97 (66.9) | 99 (45) | 108 (26) |
| Accommodation type, n (%) | |||||
| Private residence | 318 (31.5) | 7 (3) | 31 (21.4) | 74 (33.6) | 206 (49.6) |
| Public rental | 56 (5.5) | 4 (1.7) | 1 (0.7) | 20 (9.1) | 31 (7.5) |
| Family home | 40 (4) | 3 (1.3) | 11 (7.6) | 15 (6.8) | 11 (2.7) |
| Supported accommodation | 19 (1.9) | – | – | 1 (0.5) | 18 (4.3) |
| Residential aged care | 7 (0.7) | – | – | 1 (0.5) | 6 (1.5) |
| Temporary housing | 15 (1.5) | – | – | 1 (0.5) | 14 (3.4) |
| Crisis accommodation | 5 (0.5) | – | – | 1 (0.5) | 4 (1) |
| Hospital | 3 (0.3) | – | – | – | 3 (0.7) |
| Institutional care | 2 (0.2) | – | – | – | 2 (0.5) |
| No fixed address | 20 (2) | – | 3 (2.1) | 6 (2.7) | 11 (2.7) |
| Unknown | 526 (52) | 217 (94.9) | 99 (68.3) | 101 (45.9) | 109 (26.3) |
| ASGS—Remoteness Area, n (%) | |||||
| Major city | 814 (84.3) | 179 (77.5) | 113 (77.9) | 167 (75.9) | 355 (85.5) |
| Inner regional | 57 (5.9) | 12 (5.2) | 10 (6.9) | 19 (8.6) | 16 (3.9) |
| Outer regional | 45 (4.7) | 16 (6.9) | 13 (9) | 9 (4.1) | 7 (1.7) |
| Remote | 28 (2.9) | 6 (2.6) | 1 (0.7) | 11 (5) | 10 (2.4) |
| Very remote | 14 (1.5) | 7 (3) | 1 (0.7) | 1 (0.5) | 5 (1.2) |
| Migratory and offshore | 8 (0.8) | 6 (2.6) | 2 (1.4) | – | – |
| Missing | 45 (4.5) | 5 (2.2) | 5 (3.5) | 13 (5.9) | 22 (5.3) |
| SEIFA—Index of Relative Social Disadvantage, n (%) | |||||
| Q1—most disadvantaged | 141 (14) | 61 (26.4) | 37 (25.5) | 18 (8.2) | 25 (6) |
| Q2—more disadvantaged | 83 (8.2) | 6 (2.6) | 10 (6.9) | 25 (11.4) | 42 (10.1) |
| Q3—average | 216 (21.4) | 22 (9.5) | 19 (13.1) | 68 (30.9) | 107 (25.8) |
| Q4—less disadvantaged | 291 (28.8) | 68 (29.4) | 41 (28.3) | 53 (24.1) | 129 (31.1) |
| Q5—least disadvantaged | 224 (22.2) | 63 (27.3) | 28 (19.3) | 43 (19.6) | 90 (21.7) |
| Missing | 56 (5.5) | 11 (4.8) | 10 (6.9) | 13 (5.9) | 22 (5.3) |
ABI-RESTaRT, Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT; ASGS, Australian statistical geography standard; SEIFA, socio-economic index for areas.
Brain injury characteristics
Table 6 summarises brain injury characteristics for the cohort. There were significant differences in gender composition of the diagnostic groups (p<0.001), with more male than female clients with TBI and stroke. Gender differences were smaller in the other NTBI and neurological groups.
Table 6.
Brain injury and admission characteristics for the ABI-RESTaRT cohort at index admission to community-based brain injury services, 1991–2020 (n=1011)
| Characteristics | Total, n=1011 | Traumatic, n=353 | Non-traumatic | Neurological, n=103 |
|
| Stroke, n=292 | Other NTBI, n=263 | ||||
| Sociodemographic | |||||
| Age at injury, mean±SD (years) | 42.3±16.5, n=853 | 33.4±14.9, n=303 | 51±13.4, n=265 | 43±15, n=226 | 46.8±18.9, n=59 |
| Gender, n (%) | |||||
| Male | 682 (67.5) | 283 (80.2) | 197 (67.5) | 142 (54) | 60 (58.3) |
| Female | 329 (32.5) | 70 (19.8) | 95 (32.5) | 121 (46) | 43 (41.8) |
| Aboriginal and/or Torres Strait Islander, n (%) | |||||
| Total | 34 (3.4) | 16 (4.5) | 10 (3.4) | 5 (1.9) | 3 (2.9) |
| Male | 24 (3.5) | 13 (4.6) | 8 (4.1) | 2 (1.4) | 1 (1.7) |
| Female | 10 (3) | 3 (4.3) | 2 (2.1) | 3 (2.5) | 2 (4.7) |
| Clinical | |||||
| Injury location, n (%) | |||||
| Right | 114 (11.3) | 24 (6.8) | 76 (26) | 13 (4.9) | 1 (1) |
| Left | 145 (14.3) | 38 (10.8) | 97 (33.2) | 10 (3.8) | – |
| Unilateral—side unspecified | 101 (10) | 42 (11.9) | 40 (13.7) | 19 (7.2) | – |
| Bilateral | 595 (58.9) | 220 (62.3) | 64 (21.9) | 211 (80.2) | 100 (97.1) |
| Unknown | 56 (5.5) | 29 (8.2) | 15 (5.1) | 10 (3.8) | 2 (1.9) |
| Length of acute hospital stay, mean±SD (months) | 6±4.8, n=740 | 7±5.3, n=273 | 5.1±3.5, n=236 | 5.9±4.9, n=206 | 4.8±6.7, n=25 |
| Previous ABI, n (%) | 76 (7.5) | 15 (4.3) | 41 (14) | 19 (7.2) | 1 (1) |
| Injury phase, n (%) | |||||
| Acute (>3 months) | 56 (6) | 12 (3.5) | 21 (7.5) | 20 (8.3) | 3 (4.1) |
| Subacute (3–12 months) | 410 (43.7) | 134 (39.2) | 158 (56.2) | 109 (45) | 9 (12.3) |
| Chronic (>12 months) | 472 (50.3) | 196 (57.3) | 102 (36.3) | 113 (46.7) | 61 (83.6) |
| Admission | |||||
| Age at admission, mean±SD (years) | 45.4±15.5 | 37.8±14.5 | 52.6±13.2 | 45.4±14.5 | 50.9±15.8 |
| Time post-injury, n (%) | |||||
| <1 year | 466 (49.7) | 146 (42.7) | 179 (63.7) | 129 (53.3) | 12 (16.4) |
| 1–2 years | 161 (17.2) | 68 (19.9) | 48 (17.1) | 40 (16.5) | 5 (6.9) |
| >2 years | 311 (33.2) | 128 (37.4) | 54 (19.2) | 73 (30.2) | 56 (76.7) |
| Programme, n (%) | |||||
| TRP | 546 (54.0) | 221 (62.6) | 168 (57.5) | 140 (53.2) | 17 (16.5) |
| TAP | 121 (12.0) | 36 (10.2) | 28 (9.6) | 41 (15.6) | 16 (15.5) |
| CAPB | 107 (10.6) | 32 (9.1) | 24 (8.2) | 30 (11.4) | 21 (20.4) |
| HACCSS | 70 (6.9) | 25 (7.1) | 26 (8.9) | 14 (5.3) | 5 (4.9) |
| SIL | 167 (16.5) | 39 (11.1) | 46 (15.8) | 38 (14.5) | 44 (42.7) |
| Admitted from, n (%) | |||||
| Home | 435 (43) | 165 (46.7) | 120 (41.1) | 96 (36.5) | 54 (52.4) |
| Hospital | 437 (43.2) | 139 (39.4) | 140 (48) | 136 (51.7) | 22 (21.4) |
| Other | 22 (2.2) | 8 (2.3) | 5 (1.7) | 9 (3.4) | – |
| Unknown | 117 (11.6) | 41 (11.6) | 27 (9.3) | 22 (8.4) | 27 (26.2) |
ABI-RESTaRT, Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT; CAPB, Capacity Building; HACCSS, Home and Community Care Social Skills; NTBI, non-traumatic brain injuries; SIL, Supported Independent Living; TAP, Transitional Accommodation Program; TRP, Transitional Rehabilitation Program.
Significant differences in age at admission and ABI type (p<0.001) were also present. Clients with TBI were significantly younger than those in all other ABI groups at admission (largest corrected p<0.001), which is consistent with prior literature. Those presenting with stroke and neurological conditions were significantly older than those with other NTBI (largest corrected p<0.006), likely reflecting increasing age-related stroke risk.31 32
Clinical characteristics
Clients with neurological conditions or TBI primarily entered post-acute rehabilitation in the chronic injury phase, whereas most clients with stroke entered services during the subacute phase. This may be related to longer hospital admissions for TBI clients, but may also demonstrate the benefits of specialised stroke services in managing acute stroke,33 quickly directing people to rehabilitation. Bilateral injuries (58.9%) were the most common overall, and for TBI (62.3%), other NTBI (80.2%) and neurological condition groups (97.1%). The majority of strokes were unilateral (72.9%), with left hemispheric more common than right hemispheric stroke. Seventy-six clients had another brain injury prior to their admission injury (7.5%). Individuals with a stroke diagnosis represented 54% of those clients (41 of 76). The presence of these individuals with prior injuries is consistent with evidence that recurrent TBI is associated with increased disability,34 and prior stroke is a significant risk factor of recurrent stroke.35
The median length of acute hospital stay for the cohort was 5 months (IQR 2.8 months–8 months), with TBI clients having significantly longer acute stays (largest corrected p<0.001). Although it is not clear why this was the case, evidence suggests that accompanying injuries and complications are associated with longer hospital stays for patients with TBI.36 However, rehabilitation appears to be effective in improving independence despite longer periods between injury and rehabilitation admission.37
Cause of injury
External causes of injury—defined as environmental events, circumstances or conditions that are external to the body—are shown in table 7. Internal causes (eg, medical conditions) are not included. Half of the cohort sustained their ABI due to an external cause (50.6%, 512 of 1011). Accidents were the leading external cause of injury (60.2%; 308 of 512), with motor vehicle accidents (33.6%) the most common accident type. Clients aged below 30 were most likely to have sustained an ABI due to motor vehicle accidents (77 of 172, 44.8%), with a median age of 23.7 years (IQR 19.1 years–37.7 years), whereas clients aged from 40 to 60 were most likely to have been injured in accidental falls (35 of 61, 57.4%), corrected p<0.001. Abnormal reaction during surgical or medical procedure was the leading external cause of stroke (82.4%), while poisoning and toxic effect of substances was the leading external cause of other NTBI (48.6%).
Table 7.
Known external causes of brain injury for the ABI-RESTaRT cohort (n=1011)
| Cause of ABI, n (%) | Total, n=1011 | Traumatic, n=353 |
Non-traumatic | Neurological, n=103 | |
| Stroke, n=292 | Other NTBI, n=263 | ||||
| Individuals with known external causes of injury | 512 (50.6) | 347 (98.3) | 51 (17.5) | 111 (42.2) | 3 (2.9) |
| Accidents | |||||
| Accidental fall | 61 (11.9) | 58 (16.7) | 1 (2) | 2 (1.8) | – |
| Motor vehicle accident (including pedestrian) | 172 (33.6) | 167 (48.1) | – | 4 (3.6) | 1 (33.3) |
| Motorbike accident | 29 (5.7) | 29 (8.4) | – | – | – |
| Cycling accident | 14 (2.7) | 13 (3.8) | – | 1 (0.9) | – |
| Quad bike accident | 4 (0.8) | 4 (1.2) | – | – | – |
| Railway accident | 3 (0.6) | 3 (0.9) | – | – | – |
| Drowning and submersion | 3 (0.6) | 1 (0.3) | – | 2 (1.8) | – |
| Other accident | 12 (2.3) | 9 (2.6) | 1 (2) | 2 (1.8) | – |
| Unspecified accident | 10 (1.9) | 8 (2.3) | – | 2 (1.8) | – |
| Poisoning and toxic effect of drugs, medicaments or gases | |||||
| Accidental overdose | 12 (2.3) | – | 1 (2) | 11 (9.9) | – |
| Intentional overdose | 19 (3.7) | – | 1 (2) | 18 (16.2) | – |
| Unknown intent | 9 (1.8) | – | – | 9 (8.1) | – |
| Complication of chronic substance use | 20 (3.9) | – | 3 (3.9) | 16 (14.4) | 1 (33.3) |
| Intentional self-harm (excluding poisoning) | |||||
| Hanging or strangulation | 4 (0.8) | – | – | 4 (3.6) | – |
| Jumping from high place, or in front of moving object | 7 (1.4) | 7 (2) | – | – | – |
| Drowning | 1 (0.2) | – | – | 1 (0.9) | – |
| Unspecified suicide | 2 (0.4) | 1 (0.3) | – | 1 (0.9) | – |
| Complications of medical and surgical care | |||||
| Abnormal reaction during surgical or medical procedure | 78 (15.2) | 2 (0.6) | 42 (82.4) | 33 (29.7) | 1 (33.3) |
| Adverse effects of drugs, medicaments and biological substances during therapeutic use | 2 (0.4) | – | 1 (2) | 1 (0.9) | – |
| Assault | 50 (9.8) | 45 (13) | 1 (2) | 4 (3.6) | – |
| Individuals with known internal or unknown causes | 499 (49.4) | 6 (1.7) | 241 (82.5) | 152 (57.8) | 100 (97.0) |
Percentages for each group were calculated using the number of individuals with known external causes of injury recorded as the denominator. Individuals with known internal or unknown causes were not included in the count.
ABI-RESTaRT, Acquired Brain Injury Community REhabilitation and Support Services OuTcomes CohoRT; NTBI, non-traumatic brain injuries.
Admission characteristics
The majority of TBI (62.6%), stroke (57.5%) and other NTBI (53.2%) clients were admitted for post-acute transitional rehabilitation. The majority of neurological clients were admitted to Supported Independent Living (42.7%).
Median time from injury to admission to community-based services was 10.5 months (IQR 5.7 months–27.1 months). Clients with neurological conditions took significantly longer to access services than other ABI groups (largest corrected p<0.001). Those in the stroke group accessed services significantly faster than the TBI group (p<0.001) but did not differ from the other NTBI group (p=0.40).
Similar numbers of clients were admitted from hospital and home. There were significant differences in ABI group and admission source (p<0.001). Where admission source was known, 71.1% of individuals with neurological conditions were admitted from home, 52.9% of the TBI group, 45.3% of the stroke group and 39.8% of the other NTBI group. The over-representation of individuals with neurological injury in admissions from home is likely the result of slow onset of neurological injuries relative to acute injuries like stroke or TBI.
Future directions
The main focus of the ABI-RESTaRT research programme is to measure the short-term and long-term outcomes of cohort members following discharge from post-acute services. The heterogeneity of the cohort, and the scope and quantity of longitudinal health data available provides a unique opportunity to identify the predictors of outcomes. Findings will enable greater understanding of personal and structural factors influencing outcomes, providing valuable evidence for clinicians to generate effective, personalised post-acute programmes.
To ensure that change over time can be examined into the future, the cohort will be periodically updated with new admissions to allow a dynamic cohort of individuals to be followed through changing services over time, a possibility not seen in previous cohorts of this type.
Health comorbidities of the cohort will also be examined to understand the complex needs of people with ABI and facilitate effective person-centred care. Comorbidities—ie, chronic condition(s) co-existing with an index disease38—are common following ABI. Complex or mismanaged comorbidity can affect the course and outcome of rehabilitation and result in poorer functional outcomes, longer stay and higher use and costs of healthcare services.39–41 Better understanding of comorbidities can support a focus on the whole person, not only neurological recovery, which is critical for effective community re-integration.
Mental health disorders are common for those with ABI.41 42 Individuals with mental health comorbidities present before or after ABI have poorer outcomes than those without.41 43 Prior research using a retrospective convenience sample of 263 ABI-RESTaRT members admitted to the service from 2009 to 2018 found that mental health comorbidities were present in 55.8% of the sample (n=106), representing the most common comorbidity.44 ABI-RESTaRT provides the opportunity to examine the prevalence of mental illness, specific mental health needs and its impact on rehabilitation outcomes to inform policy and services for mental health and ABI.
Strengths and limitations
ABI-RESTaRT is the largest post-acute community-based ABI cohort in Australia. The research design provides novel opportunities to examine the longitudinal needs of people living with ABI, and to evaluate the efficacy of post-acute rehabilitation and support programmes offered. The demographic and outcomes data at Brightwater has been collected over 29 years, which will allow the effects of policy and treatment changes over time to be examined. The use of both internal clinical data and linked health data produces a detailed picture of brain injury that is more complex than could be derived from a single source, allowing complex questions around the nature of ABI and the individualised client requirements to be examined.
As ABI-RESTaRT is comprised of individuals from a single organisation, this population differs from the ABI population in WA in some ways. The cohort is relatively young, with only 6.2% of clients aged 65 years or above. This under-representation reduces the conclusions that can be drawn from this cohort around older adults. Similarly, only 3.4% of the cohort were of Aboriginal or Torres Strait Islander background despite Indigenous Australians being over-represented in TBI cases in WA2 45 and having elevated stroke risk relative to non-Aboriginal and Torres Strait Islander people.46 47 Research is needed to examine the factors impacting the engagement of Aboriginal and Torres Strait Islander peoples with post-acute services. Finally, the use of a state-based data linkage register has limitations, as pre-admission or post-discharge follow-up data for cohort members based interstate or overseas will not be captured in the WA Data Linkage System data collections, and it is not possible to distinguish these cases from individuals who remained in WA but did not access services captured by data linkage systems.
Collaboration
Researchers interested in collaborations are invited to contact the corresponding author. Initial data analyses and publications will be conducted by the primary ABI-RESTaRT investigators. Access to the linked data is only possible with express permission of the West Australian Department of Health Human Research Ethics Committees and data custodians, and may require a data sharing agreement. Analysis of linked data is currently authorised to occur at only one location in Perth, Western Australia.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge all the clients and families at Brightwater Care Group who participated in this study and all the staff who contributed to the data collection.
Footnotes
Contributors: GM performed the data collection, wrote the statistical analysis plan, analysed the data and drafted and revised the paper. LT designed and supervised the study, provided analytical input and drafted and revised the paper. JW provided clinical and service input, and revised the draft paper. AM designed and led the study, obtained linked data and revised the draft paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available. Internal data used in this protocol are highly sensitive and confidential and only accessible to approved personnel. Linked data are kept securely by the Western Australian Department of Health Data Linkage Branch and can be accessed on request. Researchers interested in collaborations or further information are invited to contact the corresponding author.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Ethics approval for this research was granted by the University of Western Australia Human Research Ethics Committee (RA/4/1/9232) and the West Australian Department of Health Human Research Ethics Committee (RGS0000002894).
References
- 1.Rushworth N. Brain injury Australia: submission to the Australian Government’s National mental health and disability employment strategy, 2008. Available: BRAININJURYAUSTRALIAsubmissionEMPLOYMENTSTRATEGYfinal
- 2.Fortune N, Wen X. The definition, incidence and prevalence of acquired brain injury in Australia. Sydney: Australian Institute of Health and Welfare, 1999. [Google Scholar]
- 3.Brain Injury Australia . About brain injury, 2016. Available: https://www.braininjuryaustralia.org.au/
- 4.Fleminger S, Ponsford J. Long term outcome after traumatic brain injury. BMJ 2005;331:1419–20. 10.1136/bmj.331.7530.1419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Victorian Neurotrauma Initiative . The economic cost of spinal cord injury and traumatic brain injury in Australia report by access economics Pty limited for the Victorian neurotrauma initiative, 2009. Available: http://www.spinalcure.org.au/pdf/Economic-cost-of-SCI-and-TBI-in-Au-2009.pdf
- 6.van Velzen JM, van Bennekom CAM, Edelaar MJA, et al. How many people return to work after acquired brain injury?: a systematic review. Brain Inj 2009;23:473–88. 10.1080/02699050902970737 [DOI] [PubMed] [Google Scholar]
- 7.McCabe P, Lippert C, Weiser M, et al. Community reintegration following acquired brain injury. Brain Inj 2007;21:231–57. 10.1080/02699050701201631 [DOI] [PubMed] [Google Scholar]
- 8.Wise EK, Mathews-Dalton C, Dikmen S, et al. Impact of traumatic brain injury on participation in leisure activities. Arch Phys Med Rehabil 2010;91:1357–62. 10.1016/j.apmr.2010.06.009 [DOI] [PubMed] [Google Scholar]
- 9.Ownsworth T, Fleming J, Haines T, et al. Development of depressive symptoms during early community reintegration after traumatic brain injury. J Int Neuropsychol Soc 2011;17:112–9. 10.1017/S1355617710001311 [DOI] [PubMed] [Google Scholar]
- 10.Turner BJ, Fleming JM, Ownsworth TL, et al. The transition from hospital to home for individuals with acquired brain injury: a literature review and research recommendations. Disabil Rehabil 2008;30:1153–76. 10.1080/09638280701532854 [DOI] [PubMed] [Google Scholar]
- 11.Malec JF, Basford JS. Postacute brain injury rehabilitation. Arch Phys Med Rehabil 1996;77:198–207. 10.1016/s0003-9993(96)90168-9 [DOI] [PubMed] [Google Scholar]
- 12.Marquez de la Plata C. Timeliness of postacute brain injury rehabilitation after TBI improves outcome. Chall 2015;9:10–12. [Google Scholar]
- 13.Curran C, Dorstyn D, Polychronis C, et al. Functional outcomes of community-based brain injury rehabilitation clients. Brain Inj 2015;29:25–32. 10.3109/02699052.2014.948067 [DOI] [PubMed] [Google Scholar]
- 14.Borg DN, Nielsen M, Kennedy A, et al. The effect of access to a designated interdisciplinary post-acute rehabilitation service on participant outcomes after brain injury. Brain Inj 2020;34:1358–66. 10.1080/02699052.2020.1802660 [DOI] [PubMed] [Google Scholar]
- 15.Christie L, Egan C, Wyborn J, et al. Evaluating client experience of rehabilitation following acquired brain injury: a cross-sectional study. Brain Inj 2021;35:215–25. 10.1080/02699052.2020.1867768 [DOI] [PubMed] [Google Scholar]
- 16.Williams E, Jackson H, Wagland J, et al. Community rehabilitation outcomes for different stroke diagnoses: an observational cohort study. Arch Rehabil Res Clin Transl 2020;2:100047. 10.1016/j.arrct.2020.100047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brightwater Care Group . Brain injury rehabilitation, 2020. Available: https://brightwatergroup.com/disability/brain-injury-rehabilitation/
- 18.Department of Health Government of Western Australia . Data linkage Western Australia, 2020. Available: https://www.datalinkage-wa.org.au/
- 19.Australian Rehabilitation Outcomes Centre . Aroc impairment coding guidelines, 2013. Available: https://documents.uow.edu.au/content/groups/public/@web/@chsd/@aroc/documents/doc/uow125260.pdf
- 20.Tsai Y-C, Liu C-J, Huang H-C, et al. A meta-analysis of dynamic prevalence of cognitive deficits in the acute, subacute, and chronic phases after traumatic brain injury. J Neurosci Nurs 2021;53:63–8. 10.1097/JNN.0000000000000570 [DOI] [PubMed] [Google Scholar]
- 21.Echlin F. Traumatic subdural Hematoma—Acute, subacute and chronic. J Neurosurg 1949;6:294–303. [DOI] [PubMed] [Google Scholar]
- 22.Cicerone KD, Mott T, Azulay J, et al. A randomized controlled trial of holistic neuropsychologic rehabilitation after traumatic brain injury. Arch Phys Med Rehabil 2008;89:2239–49. 10.1016/j.apmr.2008.06.017 [DOI] [PubMed] [Google Scholar]
- 23.Piccenna L, Knox L, Douglas L. Slow stream rehabilitation: an overview, 2016. Available: https://www.summerfoundation.org.au/wp-content/uploads/ssr-briefing-paper-7-june-2016-final.pdf
- 24.Jackson D, Seaman K, Sharp K, et al. Staged residential post-acute rehabilitation for adults following acquired brain injury: a comparison of functional gains rated on the UK functional assessment measure (UK FIM+FAM) and the Mayo-Portland adaptability inventory (MPAI-4). Brain Inj 2017;31:1405–13. 10.1080/02699052.2017.1350998 [DOI] [PubMed] [Google Scholar]
- 25.Giacino JT, Ashwal S, Childs N, et al. The minimally conscious state: definition and diagnostic criteria. Neurology 2002;58:349–53. 10.1212/wnl.58.3.349 [DOI] [PubMed] [Google Scholar]
- 26.National Disability Insurance Agency . What is the NDIS? 2020. Available: https://www.ndis.gov.au/understanding/what-ndis
- 27.Brightwater Care Group . Supported independent living, 2021. Available: https://brightwatergroup.com/disability/supported-independent-living/
- 28.Brightwater Care Group . Transitional support, 2020. Available: https://brightwatergroup.com/disability/transitional-support/
- 29.Department of Health Government of Western Australia . Access to WA community care services, 2019. Available: https://ww2.health.wa.gov.au/Articles/F_I/HACC-Home-and-Community-Care-Program/Access-to-WA-Community-Care-Services
- 30.StataCorp . Stata statistical software: release 16. College Station: StataCorp, 2019. [Google Scholar]
- 31.Simons LA, McCallum J, Friedlander Y, et al. Risk factors for ischemic stroke: Dubbo study of the elderly. Stroke 1998;29:1341–6. 10.1161/01.str.29.7.1341 [DOI] [PubMed] [Google Scholar]
- 32.Kelly-Hayes M. Influence of age and health behaviors on stroke risk: lessons from longitudinal studies. J Am Geriatr Soc 2010;58 Suppl 2:325–8. 10.1111/j.1532-5415.2010.02915.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Langhorne P, Ramachandra S, Stroke Unit Trialists' Collaboration . Organised inpatient (stroke unit) care for stroke: network meta-analysis. Cochrane Database Syst Rev 2020;4:CD000197. 10.1002/14651858.CD000197.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gavett BE, Stern RA, McKee AC. Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin Sports Med 2011;30:179–88. 10.1016/j.csm.2010.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burn J, Dennis M, Bamford J, et al. Long-Term risk of recurrent stroke after a first-ever stroke. The Oxfordshire community stroke project. Stroke 1994;25:333–7. 10.1161/01.str.25.2.333 [DOI] [PubMed] [Google Scholar]
- 36.Tardif P-A, Moore L, Boutin A, et al. Hospital length of stay following admission for traumatic brain injury in a Canadian integrated trauma system: a retrospective multicenter cohort study. Injury 2017;48:94–100. 10.1016/j.injury.2016.10.042 [DOI] [PubMed] [Google Scholar]
- 37.Williams E, Martini A, Jackson H, et al. Time between acquired brain injury and admission to community-based rehabilitation: differences in cognitive and functional gains. Brain Inj 2020;34:713–22. 10.1080/02699052.2020.1740943 [DOI] [PubMed] [Google Scholar]
- 38.Royal Australian College of General Practitioners (RACGP) . Part A: multimorbidity. In: RACGP aged care clinical guide (silver book). 5th ed. Australia: Royal Australian College of General Practitioners, 2019. [Google Scholar]
- 39.Giaquinto S. Comorbidity in post-stroke rehabilitation. Eur J Neurol 2003;10:235–8. 10.1046/j.1468-1331.2003.00563.x [DOI] [PubMed] [Google Scholar]
- 40.Stineman MG, Ross RN, Williams SV, et al. A functional diagnostic complexity index for rehabilitation medicine: measuring the influence of many diagnoses on functional independence and resource use. Arch Phys Med Rehabil 2000;81:549–57. 10.1016/S0003-9993(00)90033-9 [DOI] [PubMed] [Google Scholar]
- 41.Hart T, Brenner L, Clark AN, et al. Major and minor depression after traumatic brain injury. Arch Phys Med Rehabil 2011;92:1211–9. 10.1016/j.apmr.2011.03.005 [DOI] [PubMed] [Google Scholar]
- 42.Colantonio A, Gerber G, Bayley M, et al. Differential profiles for patients with traumatic and non-traumatic brain injury. J Rehabil Med 2011;43:311–5. 10.2340/16501977-0783 [DOI] [PubMed] [Google Scholar]
- 43.Williams LS, Ghose SS, Swindle RW. Depression and other mental health diagnoses increase mortality risk after ischemic stroke. Am J Psychiatry 2004;161:1090–5. 10.1176/appi.ajp.161.6.1090 [DOI] [PubMed] [Google Scholar]
- 44.Jackson HM, Troeung L, Martini A, Prevalence MA. Prevalence, patterns, and predictors of multimorbidity in adults with acquired brain injury at admission to staged community-based rehabilitation. Arch Rehabil Res Clin Transl 2020;2:100089. 10.1016/j.arrct.2020.100089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Katzenellenbogen JM, Atkins E, Thompson SC, et al. Missing voices: profile, extent, and 12-month outcomes of nonfatal traumatic brain injury in Aboriginal and non-Aboriginal adults in Western Australia using linked administrative records. J Head Trauma Rehabil 2018;33:412–23. 10.1097/HTR.0000000000000371 [DOI] [PubMed] [Google Scholar]
- 46.Kilkenny MF, Harris DM, Ritchie EA, et al. Hospital management and outcomes of stroke in Indigenous Australians: evidence from the 2009 acute care national stroke audit. Int J Stroke 2013;8:164–71. 10.1111/j.1747-4949.2011.00717.x [DOI] [PubMed] [Google Scholar]
- 47.Katzenellenbogen JM, Vos T, Somerford P, et al. Burden of stroke in Indigenous Western Australians: a study using data linkage. Stroke 2011;42:1515–21. 10.1161/STROKEAHA.110.601799 [DOI] [PubMed] [Google Scholar]
- 48.Australian Bureau of Statistics . Socio-Economic indexes for areas, 2018. Available: https://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa
- 49.Australian Bureau of Statistics . The Australian statistical geography standard (ASGS) remoteness structure, 2018. Available: https://www.abs.gov.au/websitedbs/D3310114.nsf/home/remoteness+structure
- 50.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. The Lancet 1974;304:81–4. 10.1016/S0140-6736(74)91639-0 [DOI] [PubMed] [Google Scholar]
- 51.Turner-Stokes L, Nyein K, Turner-Stokes T, et al. The UK FIM+FAM: development and evaluation. Clin Rehabil 1999;13:277–87. 10.1191/026921599676896799 [DOI] [PubMed] [Google Scholar]
- 52.Malec J, Lezak M. Manual for the Mayo-Portland Adaptability Inventory (MPAI-4) for adults, children and adolescents, 2003. Available: http://www.tbims.org/combi/mpai/manual.pdf
- 53.Kiresuk TJ, Sherman RE. Goal attainment scaling: a general method for evaluating comprehensive community mental health programs. Community Ment Health J 1968;4:443–53. 10.1007/BF01530764 [DOI] [PubMed] [Google Scholar]
- 54.Turner-Stokes L, Disler R, Williams H. The rehabilitation complexity scale: a simple, practical tool to identify ‘complex specialised’ services in neurological rehabilitation. Clin Med 2007;7:593–9. 10.7861/clinmedicine.7-6-593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.von Steinbuechel N, Petersen C, Bullinger M, et al. Assessment of health-related quality of life in persons after traumatic brain injury--development of the Qolibri, a specific measure. Acta Neurochir Suppl 2005;93:43–9. 10.1007/3-211-27577-0_6 [DOI] [PubMed] [Google Scholar]
- 56.von Steinbüchel N, Wilson L, Gibbons H, et al. Quality of life after brain injury (QOLIBRI): scale development and metric properties. J Neurotrauma 2010;27:1167–85. 10.1089/neu.2009.1076 [DOI] [PubMed] [Google Scholar]
- 57.Turner-Stokes L, Shaw A, Law J, et al. Development and initial validation of the Northwick Park therapy dependency assessment. Clin Rehabil 2009;23:922–37. 10.1177/0269215509337447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Turner-Stokes L, Tonge P, Nyein K, et al. The Northwick Park dependency score (NPDS): a measure of nursing dependency in rehabilitation. Clin Rehabil 1998;12:304–18. 10.1191/026921598669173600 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data are available. Internal data used in this protocol are highly sensitive and confidential and only accessible to approved personnel. Linked data are kept securely by the Western Australian Department of Health Data Linkage Branch and can be accessed on request. Researchers interested in collaborations or further information are invited to contact the corresponding author.


