Abstract
ST-segment elevation in patients sedated with propofol may be a sign of imminent malignant arrhythmias. Although propofol infusion syndrome-electrocardiographic abnormalities are usually described as Brugada-pattern, in unique cases nearly ubiquitous and extensive J-point and ST-segment elevation may be observed. These patients should undergo an ajmaline test following recovery. (Level of Difficulty: Beginner.)
Key Words: Brugada pattern, ECG, J-wave, shark fin pattern, ST-segment elevation
Abbreviations and Acronyms: ECG, electrocardiogram; PRIS, propofol infusion syndrome; STEMI, ST-segment elevation myocardial infarction
Central Illustration
Case
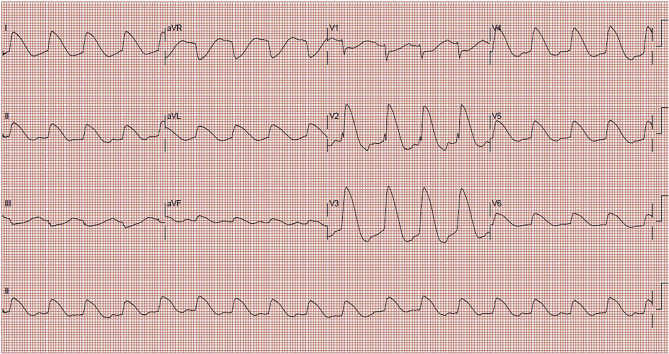
A 19-year-old female was admitted to the intensive care unit due to hemorrhagic stroke. Her medical history was unremarkable. Her family history was negative for cardiac diseases and sudden death. The electrocardiogram (ECG) on admission was normal. Propofol (4 mg/kg/h), norepinephrine, and external cooling therapies were administered to lower intracranial pressure (17 mm Hg). On day 7 of hospitalization, wide complex rhythm was noticed on the ECG monitor. The hemodynamic condition was stable, and electrolytes, pH, lactate, and kidney function were within normal range. Her ECG is shown in Figure 1.
Figure 1.
12-Lead Electrocardiogram Recorded on the 7th Day of Hospitalization
What is the diagnosis?
-
A.
ST-segment elevation myocardial infarction (STEMI)
-
B.
Takotsubo cardiomyopathy
-
C.
Intracranial-hypertension-driven ECG-abnormalities
-
D.
Hypothermia-induced ECG-abnormalities
-
E.
Propofol infusion syndrome (PRIS)
-
F.
Propofol-induced Brugada pattern in previously unrecognized Brugada syndrome
The correct answer is most likely E, but C and F and a combination of these cannot be excluded.
Explanation
The ECG shows sinus tachycardia at a rate of 104 beats/min and narrow QRS complex fused with giant T-wave (shark fin pattern) (Figure 1). Diffuse J-point and ST-segment elevation are present throughout the precordial and limb leads with the exception of V1, III, and aVR, where ST-segment depression is visible.
The shark fin pattern is usually associated with a massive anterior STEMI. Although this diagnosis cannot be entirely ruled out solely on the basis of the ECG, the absence of contralateral ST-segment depression makes it very unlikely (Supplemental Figure 1).
Osborn waves are classically described as upwardly displaced J-points, followed by diffuse concave ST-segment elevations (Supplemental Figure 1). They develop simultaneously with cooling and resolve 12 to 24 hours after the restoration of normal temperature.
Intracranial hypertension is associated with giant, deeply inverted T waves and prolonged QT intervals (Supplemental Figure 1). However, cases of brain injury with concomitant diffuse ST-segment elevation have been described. ECG abnormalities usually resolve when the intracranial pressure is lowered to <10 mm Hg (1).
PRIS is a life-threatening condition associated with rhabdomyolysis and acidosis, and is sporadically (10%) accompanied by ECG abnormalities similar to a type I Brugada pattern. Severe head injury (along with young age and catecholamine administration) is a risk factor for PRIS, as these patients usually require a high dose of propofol (2). This phenotype is not necessarily related to inherited Na-channel disease. Additionally, acidosis and hyperkalemia, although frequently present, are not necessary for the development of ECG changes. ECG abnormalities often lead to malignant arrhythmias (3). If propofol is promptly withheld, the risk of ventricular arrhythmia is lower.
Finally, propofol infusion has been described to provoke ECG abnormalities and malignant ventricular arrhythmias in patients with Brugada syndrome (3).
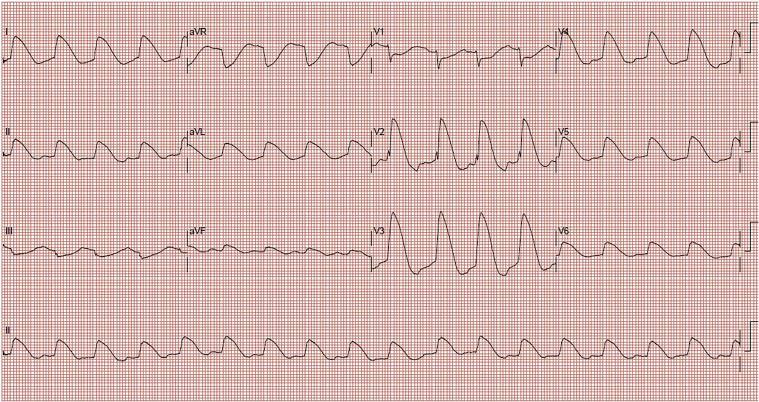
Hospital Course
In this case, hemodynamic conditions remained stable, and malignant arrhythmia was not recorded during her hospitalization. The patient’s echocardiogram and troponin concentration remained normal. Raising body temperature did not resolve the ECG abnormalities. Propofol was withdrawn a few hours after the index ECG. Electrocardiogram abnormalities slowly normalized after 40 hours (Supplemental Figure 2). Results of a genetic test for Brugada syndrome were negative. Unfortunately, the patient refused Ajmaline testing.
Conclusions
Whether the extensive ECG abnormalities were caused by Brugada syndrome, PRIS, brain injury, or a combination of these conditions is hard to tell. The fact that they resolved after propofol withdrawal makes the authors favor PRIS, possibly predisposed by an underlying Brugada syndrome.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental figures, please see the online version of this article.
Appendix
References
- 1.Hersch C. Electrocardiographic changes in head injuries. Circulation. 1961;23:853–860. doi: 10.1161/01.cir.23.6.853. [DOI] [PubMed] [Google Scholar]
- 2.Kam P.C.A., Cardone D. Propofol infusion syndrome. Anaesthesia. 2007;62:690–701. doi: 10.1111/j.1365-2044.2007.05055.x. [DOI] [PubMed] [Google Scholar]
- 3.Junttila M.J., Gonzalez M., Lizotte E. Induced Brugada-type electrocardiogram, a sign for imminent malignant arrhythmias. Circulation. 2008;117:1890–1893. doi: 10.1161/CIRCULATIONAHA.107.746495. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.