Abstract
Objective:
To determine facilitators and barriers to successful transition to adult care for adolescents living with perinatally-acquired HIV in South Africa.
Methods:
We prospectively enrolled 30 adolescents living with perinatally-acquired HIV after their pediatrician deemed them ready for transition to adult care but prior to their transition. Eighteen months after enrollment, we measured transition status, engagement in care (i.e., viral load within 12 months of transition), and viral suppression (<200 copies/ml). Additionally, we conducted in-depth interviews with adolescents before and after transition to explore facilitators and barriers to successful transition.
Results:
A total of 19/30 (63%) adolescents transitioned to adult care. Of those who transitioned, 11 (58%) were retained in care and 7 (37%) were virally suppressed one year after transition to adult care. Insufficient staff training, lack of availability of pediatric ART formulations in adult clinics, and insufficient clinical monitoring contributed to delayed transition. Rigid clinical scheduling that interfered with school and loss of clinic relationships with peers and clinical staff were major factors in contributing to poor engagement in care after transition. Maturity of the adolescent, reduced distance to clinic, and reduced length of time in the clinic were seen as facilitators to transition to adult care.
Conclusion:
Improved preparation for transition by pediatric and adult clinical staff, including restructuring of care delivery, may improve successful transition of adolescents living with perinatally acquired HIV to adult care. Transition readiness assessments are needed to determine optimal timing of transition and which adolescents are ready to transition to adult care.
Keywords: Adolescent, HIV, South Africa, transition in care
Introduction
As adolescents living with perinatally-acquired HIV age into adulthood, they require transitioning from pediatric- based care to adult-based care. Guidelines are unclear about the optimal age, timing, or preparation for adolescents, caregivers, or healthcare providers for the transition process. (American Academy of Pediatrics, American Academy of Family Physicians, & American College of Physicians-American Society of Internal Medicine, 2002; Freed & Hudson, 2006; Kung et al., 2016) South Africa, which has the highest number of children living with perinatal HIV globally,(Statistics South Africa, 2013; Andiman, 2011; South African Department of Health, 2012; Ikard et al., 2005; “Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies,” 2008; Sherman, Lilian, Bhardwaj, Candy, & Barron, 2014; “Transitioning HIV-infected youth into adult health care,” 2013; Zanoni, Archary, Buchan, Katz, & Haberer, 2016) is an ideal setting to study the issues of health care transition.
The transition to adult services has been associated with poor retention in care and poor clinical outcomes for adolescents living with chronic illnesses including HIV.(Brousseau, Owens, Mosso, Panepinto, & Steiner, 2010; Cervia, 2013; Fish, Judd, Jungmann, O’Leary, & Foster, 2014; Hunt & Sharma, 2010; Izzo et al., 2018; Judd & Davies, 2018; Ryscavage, Anderson, Sutton, Reddy, & Taiwo, 2011; Weijsenfeld et al., 2016; Xia et al., 2018) During this critical time period, numerous challenges arise including changing healthcare providers, lack of youth-friendly services, rigid scheduling interfering with school, increasing responsibilities, neurocognitive problems, and decreasing supervision of adult caregivers.(Fair, Sullivan, Dizney, & Stackpole, 2012a; Gray, Schaefer, Resmini-Rawlinson, & Wagoner, 2018; Naar-King et al., 2009) When adolescents transition to adult care, they often do not receive the coordinated services that they received under pediatric care.(Wiener, Kohrt, Battles, & Pao, 2011) These complexities are reflected in South Africa where <50% of adolescents living with HIV are virally suppressed. (Simbayi LC, 2019)
To help formulate evidence-based interventions for an improved transition process, insight may be gained through the Social-ecological Model of Adolescent and Young Adult Readiness to Transition (SMART), which incorporates modifiable targets to improve transition including: knowledge, skills/self-efficacy, beliefs, goals, relationships, social support, and peer support.(Schwartz et al., 2013; Schwartz, Tuchman, Hobbie, & Ginsberg, 2011) By emphasizing these factors, as well as the interconnected relationship between adolescents, caregivers, and healthcare providers, the SMART model identifies promising targets that can be addressed to improve transition care.(Schwartz et al., 2013; Schwartz et al., 2014; Schwartz et al., 2011) This model has been used as a framework for health care transitions and intervention development for adolescents with cancer, inflammatory bowel disease, and other chronic childhood illnesses but has not previously be used to understand HIV transition care in South Africa.(Beacham & Deatrick, 2013; de Silva & Fishman, 2014; Smits-Seemann, Kaul, Zamora, Wu, & Kirchhoff, 2017)
A retrospective review of transition outcomes among adolescents living with HIV in the United States found numerous structural barriers to successful transition such as relocation, loss to follow-up, and transfer to alternate care sites.(Maturo et al., 2015) A national survey among public healthcare facilities in Nigeria found that only 15% had written transition policies for adolescents and none had comprehensive transition care services. (Badejo et al., 2018) Additionally, a review of adolescent HIV transition in sub-Saharan Africa found that many poor transition outcomes resulted from poor infrastructure or training, lack of communication between pediatric and adult clinicians and fear of stigma. (Dahourou et al., 2017) The authors called for improved data gathering, analysis, and reporting on adolescent HIV transition outcomes. (Dahourou et al., 2017)
To evaluate modifiable factors that influence successful transition care in South Africa based on the SMART model, we prospectively enrolled adolescents living with perinatally-acquired HIV in a mixed-methods study prior to their transition to adult care.
Methods
Setting:
Mahatma Gandhi Memorial Hospital is a regional/district hospital located in the township of KwaMashu outside of Durban, South Africa. The outpatient pediatric clinic provides care for more than 650 children receiving antiretroviral therapy (ART) while the adult clinic, located on the same campus, provides care for more than 1,700 adults receiving ART.
In the pediatric clinic, adolescents are seen in monthly appointments on the same day of the week. During their visit, they are evaluated by the clinic’s single pediatrician, can attend an optional peer support group, and collect medication at an onsite pharmacy. In the adult clinic, adolescents are seen once every three months by different clinicians at each visit during clinics that run five days a week and collect medication at onsite pharmacy monthly. Adolescents are deemed eligible to transition to adult care when they are 15 years old, fully disclosed of their HIV status, and taking a fixed drug combination ART regimen. However, physician discretion ultimately determines timing for transition. There are no support groups or additional services available for adolescents in the adult clinic.
Study design:
Sampling: Through convenience sampling, we identified 30 adolescents in pediatric clinic after the clinic’s pediatrician determined that they were ready to transition to adult care, but prior to the actual transition. Criteria for participation were age 15 years or older, knowledge of their HIV status, and taking a fixed drug combination ART. In addition, we recruited 11 healthcare providers (physicians, nurses, counselors, social workers, and pharmacists) to discuss facilitators and barriers to transition care and reasons that eligible adolescents did not transition to adult care.
Recruitment: Study participants were recruited in person by a research assistant (author TS) during their routine clinic visits between September 1, 2016 and November 9, 2017. Adolescents less than 18 years old assented to study participation and written consent was obtained from the primary caregiver. Adolescents 18 years or older provided their own informed consent.
Data Collection: After explaining the purpose of the study to adolescent participants, prior to transition, we obtained baseline demographic data and conducted a baseline in-depth qualitative interview. Adolescents were then followed prospectively until at least one year after transition to adult clinic. For those who transitioned to adult care, a follow-up interview was conducted after six months in adult care. Both the pre-transition and post-transition interviews were used for analysis. Adolescents who did not transfer by July 1, 2018 were no longer followed for the second interview. The interviews used open-ended questions to obtain information on the process of transition to adult care for adolescents living with perinatally acquired HIV in South Africa. The interview guide was developed based on the SMART transition model and with expert opinion (Fair, Sullivan, Dizney, & Stackpole, 2012b; “Transitioning HIV-infected youth into adult health care,” 2013) and piloted with adolescents in a different hospital in KwaZulu-Natal, South Africa.(Zanoni, Sibaya, Cairns, & Haberer, 2019) Questions relevant to this analysis addressed: experience with clinic providers, barriers and facilitators to transition care, and experience with transition. Interviews were conducted in person in a private space located on the grounds of the clinic. All interviews were conducted by a female, bachelor’s-level, research assistant trained in qualitative methods (author TS) who was not affiliated with the clinic. Interviews were audio-recorded, lasted between 60 and 90 minutes, and were conducted in isiZulu or English based on participant preference. Interview content was transcribed verbatim and translated into English as needed by either the research assistant or a consultant at the University of KwaZulu-Natal; both are bilingual in isiZulu and English. Each transcript was reviewed by the research assistant who performed the interview for quality and accuracy.
We additionally extracted demographic data, as well as pre- and post-transition viral load and appointment data from clinic records. Clinical outcomes and data from adolescents who transitioned to adult care were monitored for one year or until July 2019, one year after the last eligible participant transitioned. Successful transition was defined as transferring to adult care and being retained in care with viral suppression one year after transition.
Data Analysis:
Quantitative data were analyzed descriptively; significance testing was not undertaken due to small sample size. We used an inductive content analysis approach to analyze qualitative data that was derived from reviewing, coding, and interpreting the data. Author BCZ reviewed the first 10 transcripts and analyzed content to develop labels, create operational definitions, and develop a codebook with selected illustrative quotes. Approximately 10% of interviews were double coded (authors BCZ and JEH) and discrepancies were discussed until consensus was obtained. The codebook was then refined using an iterative process. Following the completion of the codebook, the remainder of transcripts were coded using Dedoose software (Version 8.0.42, Los Angeles, CA). Using the coded data, themes were identified corresponding to important topics in the data. Theme examination included a combination of a priori categories (i.e., barriers to retention, facilitators to retention, social support) and additional themes that emerged from the data. The themes were further organized using the SMART model and evidence was provided using illustrative quotes from the research participants.
Ethics Statement
The Durban University of Technology Independent Research Ethics Committee, KwaZulu-Natal Department of Health, Partners Healthcare/Massachusetts General Hospital Research Ethics Board and the Emory University Independent Review Board approved this protocol.
Quantitative Results
Participant characteristics of the 30 prospectively enrolled adolescents are indicated in Table 1. Participants were a median of 16 years old (IQR 15-16); 58% were male.
Table 1.
Participant characteristics
| Transitioned to adult care (n=19) |
Remained in pediatric care (n=11) |
|
|---|---|---|
| Enrollment characteristics | ||
| Median age at enrollment (years) | 16 (IQR 15 - 16) | 16 (IQR 15 - 16) |
| Male n (%) | 11 (58%) | 7 (64%) |
| Suppressed viral load at enrollment | 18 (95%) | 11 (100%) |
| Time to transition (weeks) (IQR) | 39 (19 – 50) | n/a |
| Outcomes | ||
| Viral suppression after transition | 7 (37%)** | 8 (73%)* |
| Engaged in care after transition | 11/19 (58%) | 11 (100%)* |
12 months after participants were determined to be ready to transition yet remained in pediatric care
Successful transitions to adult care
Participant outcomes:
By June 2018 (18 months after enrollment), 19 (63%) adolescents transitioned to adult care, while 11 (37%) remained in pediatric care (Figure 1). The median time from enrollment to first visit in adult care for those that transitioned was 39.4 weeks (IQR 19.1-49.6). The median age at transition was 16.5 years (IQR 15.8-16.9). The median age of those remaining in pediatric care at the end of the study was 17.1 years (IQR 16.3-17.2). At the end of the analysis period, June 2019 (30 months after enrollment), four adolescents still remained in pediatric care and an additional eight adolescents transitioned to adult care but had <6 months of follow-up and thus could not be included in the planned analyses.
Figure 1.
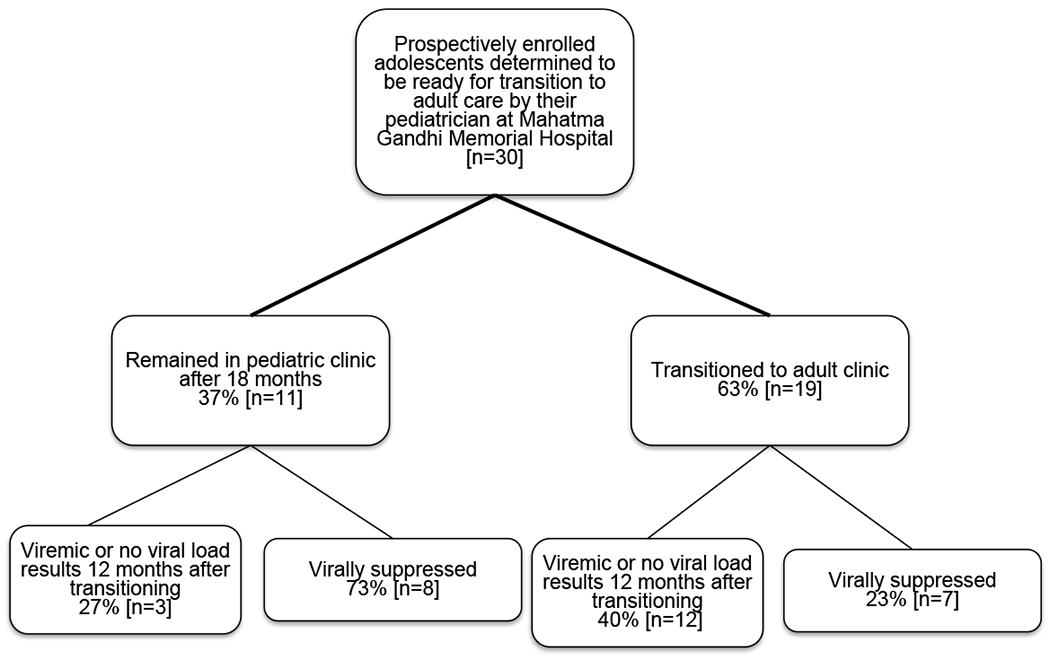
Participant follow-up during the study.
At enrollment, 29/30 (97%) adolescents were virally suppressed to <200 HIV copies/ml. One adolescent had a viral load of >1,000 HIV copies/ml prior to transitioning to adult care. Of the 19 adolescents who transitioned to adult care, 7 (37%) were documented to be virally suppressed within 12 months after transition. One adolescent became viremic to 180,000 copies/ml, while the remaining 11 (58%) did not have a viral load evaluation for more than 1 year after transition to adult care (including the adolescent with viremia at the time of transition). By study definition, 7 (23%) adolescents were deemed to have a successful transition from pediatric to adult care. Reasons for the adolescents not transitioning to adult care reported by healthcare team are listed in Table 2.
Table 2.
Reasons why adolescents did not transition to adult care as determined by clinical care team
| Adolescents receiving second-line ART |
| Closest local clinic did not have access to pediatric medication (non-fixed dose combinations) |
| Adolescents who had decreased glomerular filtration rate and could not be switched to fixed dose combination therapy |
| Adolescents with poor adherence as determined by pill counts |
| Adolescents with limited social support or lacked caregivers |
| Staff at transition site not trained in care of adolescents living with HIV |
Qualitative Results
We organized the theoretical factors affecting transition care according to the SMART model as indicated in Figure 2, presenting the most salient themes first.(Schwartz et al., 2011)
Figure 2: Modified Social-ecological Model of Adolescent and Young Adult Readiness to Transitions (SMART) theoretical model and observed factors affecting transition to adult care.
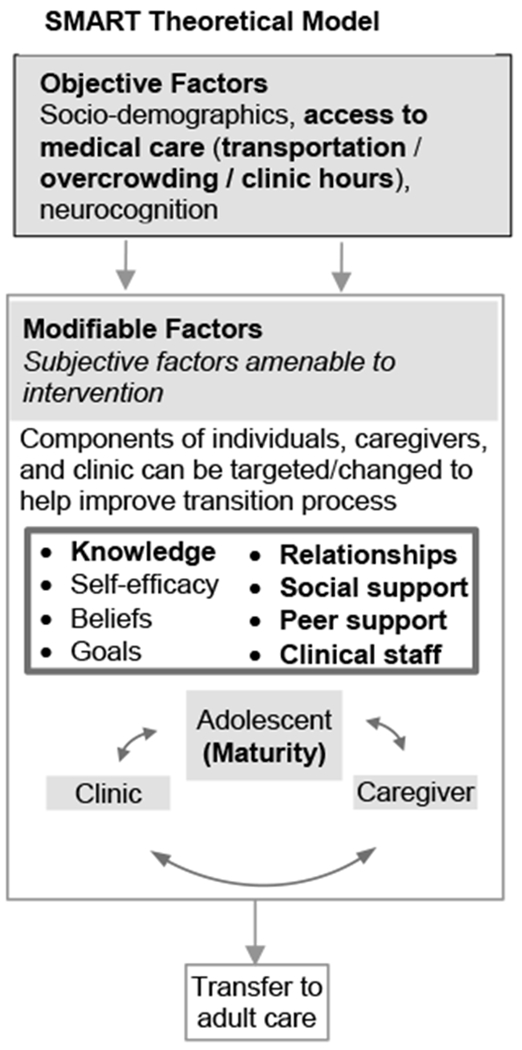
Factors in bold emerged as contributing to engagement in care during transition in this study. Additional categories were added in parentheses.
Subjective Barriers to Transition - Importance of Relationships:
Adolescents emphasized the importance of relationships with peers and with clinical staff. Stronger personal relationships facilitated engagement in care, while loss of these long-term relationships were barriers to engagement in care.
Loss of Peer Support:
When adolescents transitioned from the pediatric clinic to the adult clinic, they no longer attended clinic with their peers, and expressed displeasure with the loss of these interpersonal relationships that had been forged in the clinic over years. Adolescents also found a lack of opportunity to create similar relationships in the existing structure of adult clinical care. Without these relationships, the adult clinic became “boring” and “tedious”.
“It was not okay because you leave your friends behind while you were used to seeing them…In [adult] clinic, there is nothing as such. You only collect your things and go.” 16-year-old female, unsuccessful transition
“The challenge is meeting new people you don’t know. You can’t even ask anything since you are not familiar with them… It’s old people there, no kids of my age, you can’t even talk to anyone in the queues, all old people.” 15-year-old male, unsuccessful transition
Loss of Relationships with Clinical Staff:
Most of the adolescents preferred care under the pediatric model where interpersonal relationships were stronger, touting friendlier staff and clinicians. The strong relationships between clinical staff became part of wellbeing. Adolescents also expressed that the staff and clinicians in the adult clinics were too busy to focus on their wellbeing and did not get to know them well.
“In [Pediatric] clinic they are patient with us, and they are caring… Staff is friendly and welcoming. They know our names. We sit and talk with them. You see your friends and hug each other.” 16-year-old male, unsuccessful transition
“I did not like that fact that they don’t understand me, and they were shouting at us. There was this nurse that was busy shouting at people.”16-year-old female, unsuccessful transition describing her experience in the adult clinic.
“It was not nice; I don’t want to lie. Starting new things is not a nice process. It was like moving to a new school; starting to make new friends, getting to know new people and to understand the way they do things…I was just anxious about starting in a new clinic, starting new nurses, starting new people, not able to communicate with councilors.” 16-year-old male, unsuccessful transition
Adolescents reported that the adult clinics were often overcrowded, and the staff were overworked, leaving little time for meaningful interactions. They also found long queues and less patient-friendly organization in the adult clinic to be barriers to engagement with clinical staff.
“There is no time to explain that you are sick. If it is my clinic date, I have to collect my pills only and not to explain that I am sick. I must come the next time or the following day and report that I am sick.” 15-year-old female, successful transition
Loss of Group Support:
Adolescents reported missing the group educational classes that were held in the pediatric clinic where they were able to gain knowledge, interact with peers, and develop relationships with the clinical staff.
“They teach us during class sessions in [Pediatric] clinic, while they don’t do that in adult clinic. In Peds, they also ask if we are okay and in adult clinic they don’t. Their priority is to give your pills then you go home.”15-year-old female, successful transition
“I like sitting and attending the class and sharing things with other people and being positive about life. It’s my wish to stay [in Pediatric clinic] even now but I understand that I am [too] old.”17-year-old male, successful transition
Lack of Navigation to Account for Reduced Clinical Support:
Adolescents recommended having a navigator assist with the logistics of transition. They felt that a physical introduction to the clinical staff and procedures in the adult clinic by pediatric staff would be helpful to strengthen personal connections to new clinical staff and relieve anxiety about the unknown.
“They should have come with me to adult clinic… Send someone with me [so] I would know where to take my ARVs.” 16-year-old male, unsuccessful transition
“I think they should provide the adherence class session at adult clinic... I think the doctor should have taken me to adult clinic and show me the process until I am happy with the process.” 16-year-old female, unsuccessful transition
“There should be someone to guide you on what to do.”15-year-old female, unsuccessful transition
Among the subjective barriers to transition, adolescents mourned the loss of relationships with peers and clinical staff in addition to the loss of services such as group support and educational sessions. The adolescents also reported that there were not many gains in transitioning to the adult clinic and felt that it would be helpful to have assistance in learning new systems, clinic flows, and personnel.
Objective Structural Barriers to Transition - Student’s Paradox:
Adolescents expressed that the pediatric clinics were often accommodating about school hours, but the adult clinics had rigid scheduling and inflexible hours that interfered with school. Students were left with a difficult choice between education and health. Adolescents suggested that the transition to adult clinic should be deferred until their schooling is complete.
“Sometimes you find that I am writing a test and it is my clinic date. I end up not writing. If I come earlier than my date, they tell me that it’s not my date so I must go back home and come back on my date. Even if I tell them the reason, they don’t care.” 15-year-old female, successful transition
“I don’t think my peers will continue taking pills, because of their exams. They won’t be absent from school when they are writing an important exam. That paper that would decide if you would pass or fail the grade. They would rather leave pills and write exams because most of my peers love school.” 15-year-old female, successful transition
“Other children continue with learning while I’m in clinic.” 18-year-old male, successful transition
“I would suggest the transition to be done after I finished [school] because next year is my final year in high school.”16-year-old male did not transition
Facilitators of transition care - Maturity:
The majority of adolescents had negative feelings toward transition despite asking about positive aspects and facilitators. Some adolescents, however, expressed interest in transitioning to the adult clinic as part of natural growth and separation from their childhood. They realized that this was a natural process of growing up. These adolescents had successful transitions to adult care.
“It was boring having to wait with little kids there at the clinic and having someone to accompany me all the time to clinic. Now, it is going to be better because I am going to come alone… I think now things are going to be good. I am going to get the freedom of coming alone.” 16-year-old female with a successful transition
A few adolescents reported that they were transitioning to local clinics which were closer to their home resulting in less expensive transportation fees and faster service than the centralized pediatric clinic. However, most adolescents were apprehensive about transitioning to adult care and did not think they would gain anything from the adult care model. They voiced few facilitators or benefits from transition. When asked to name the benefits of transitioning to adult care, several adolescents responded “nothing,” while others were even more pessimistic:
“I don’t have any hope of getting same care [in the adult clinic].” 15-year-old female who did not transition
Discussion:
In this prospective study of adolescents in routine clinical care, only 23% of adolescents who were determined to be ready for transition successfully transitioned to adult care in the next 18 months. Forty percent transitioned to adult care but were less engaged in care and did not receive viral load testing for more than 12 months highlighting decreased clinical monitoring of adolescents during this vulnerable period and decreased engagement of adolescents post transition. The remaining 37% did not transition to adult care due to various clinical, psycho-social, or logistical reasons (Table 2). Structural barriers such as lack of pediatric ART formulations or second-line ART in local adult clinics prohibited eligible adolescents from transitioning to adult care. In addition, the clinical team delayed transitions due to known poor adherence or lack of adequate support or supervision at home.
The poor transition outcomes seen in this cohort are consistent with findings from other settings. Within North America and Europe, studies have seen poor viral suppression after transition to adult care ranging from 13% to 86%.(Izzo et al., 2018; Maturo et al., 2015; Ryscavage, Macharia, Patel, Palmeiro, & Tepper, 2016; Sainz & Navarro, 2017; Weijsenfeld et al., 2016) Within South Africa, loss to follow up increased over time from transitioning to adult care from 90% at one year to 84% at 3 years.(Davies et al., 2017) Death, viral failure, and decline in CD4 count have also occurred in adolescents living with HIV after transition to adult care. (Davies et al., 2017; Fish et al., 2014; Judd et al., 2017; Kakkar et al., 2016; Sainz & Navarro, 2017)
The SMART model includes several potential objective factors that influence readiness to transition (Figure 2). In our study, participants endorsed barriers to medical care including rigid scheduling, clinic overcrowding, and transportation. Rigid scheduling and overcrowding which forces adolescents to miss an entire day of school, creates a difficult choice between health and education resulting in the “student’s paradox.” As described in our previous work, adolescents must choose between attending clinic appointments or attending school, leading to either poor engagement in care or poor academics. (Zanoni et al., 2019) When asymptomatic, adolescents may prioritize attending school to avoid disclosing their status through repeated absences or as a means to improve future job opportunities. (Anabwani, Karugaba, & Gabaitiri, 2016; Cohen et al., 1997; Zanoni et al., 2019) Delaying transition to adult care until completion of education or adopting adolescent-friendly clinic hours may minimize school interruptions to improve retention in care. (Anabwani et al., 2016; Zanoni et al., 2019; Zanoni, Sibaya, Cairns, Lammert, & Haberer, 2017)
We found that the modifiable, subjective factors from the SMART model were strongly centered on personal relationships with peers and clinical staff. After losing of personal relationships with peers and with clinical staff under pediatric care, adolescents found it difficult to create new relationships in adult clinical settings. Adolescents suggested that navigation assistance and peer support could be used to decrease the anxiety associated with the transition process.(Murray et al., 2017; Zanoni et al., 2019) Peer support and connections to clinical staff have improved engagement in care among adolescents.(Berg-Kelly, 2003; Lee et al., 2016; Pettitt, Greifinger, Phelps, & Bowsky, 2013; Zanoni et al., 2019) During adolescence, strong relationships help build self-esteem and assist adolescent development.(Hoffman, Ushpiz, & Levy-Shiff, 1988) Although non directly modifiable, maturity of the adolescent was also seen as a facilitator to transition to adult care in our cohort. The healthcare system relies on mature adolescents to navigate the healthcare system independently as support from caregivers and supportive clinical services declines. Patient-centered assessments that evaluate adolescents’ maturity, transition readiness, and knowledge could assist with determining the optimal timing of transition. (Hussen et al., 2018; Klassen et al., 2015)
Several factors in the SMART model were not observed in our study. We did not find neurodevelopmental problems to be a factor in this study; however, selection bias may have been contributory. Although neurodevelopment was not formally assessed, adolescents with moderate to severe developmental delay may not have been determined to be ready for transition and would not have been referred for study enrolment. We also did not find motivation or self-efficacy to be major factors affecting transition in this cohort. This finding may reflect the structured, regimented care delivery system in South Africa without emphasis on patient-centered care and fewer options for clinical care.
The optimal age, developmental stage, or level of independence is unclear when determining timing of transition to adult care.(Jensen et al., 2017; Sawicki, Kelemen, & Weitzman, 2014; Schwartz et al., 2014; Zhang, Ho, & Kennedy, 2014) Some suggest delaying transition until adolescents are age 25 or older when they are more developmentally mature. (Maturo et al., 2015) Yet, in many settings, transition timing is dictated by policy or logistical reasons rather than a patient-centered rationale. Transition readiness scales have been created to assist with determination of transition timing for adolescents with chronic diseases, but none have been used in resource-limited settings.(Klassen et al., 2015; Sawicki et al., 2011) Future research is needed to determine the factors that contribute to transition readiness for adolescents living with perinatally acquired HIV in resource limited settings.
This study has several limitations. It is a relatively small cohort from a single site where transition occurs at approximately 15 years of age. Our results may not be generalizable to other settings were transitions occur at older or younger ages. However, the prospective nature of the study allows for complete data with a single, consistent transition policy. We were also only able to follow adolescents for 18 months after they were deemed to be ready for transition. Longer follow-up time would more accurately reflect the intermittent engagement in care among many adolescents. Additionally, because we employed convenience sampling, our findings may be incomplete and/or not representative of all adolescent transition experiences in the clinic.
Conclusion:
Current practices of transitioning adolescents living with HIV to adult care in South Africa result in inconsistent timing of transition and poor engagement in care after transition. Adolescents undergoing transition to adult care experience loss of meaningful relationships with peers and clinical staff. Guidelines and practices that include relationship strengthening through peer navigation, peer support, and improved connection to adult clinical staff as well as including adolescent-friendly clinic hours may improve the transition process for adolescents.
Acknowledgments
Funding:
This work was supported via: Harvard 4KL2 TR001100-04 PI: Zanoni; K24MH114732 PI: Haberer
Footnotes
Competing Interests: The authors have no conflicts of interest relevant to this article to disclose.
References:
- American Academy of Pediatrics, American Academy of Family Physicians, & American College of Physicians-American Society of Internal Medicine. (2002). A consensus statement on health care transitions for young adults with special health care needs. Pediatrics, 110(6 Pt 2), 1304–1306. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12456949http://pediatrics.aappublications.org/content/110/Supplement_3/1304.full.pdf [PubMed] [Google Scholar]
- Anabwani G, Karugaba G, & Gabaitiri L (2016). Health, schooling, needs, perspectives and aspirations of HIV infected and affected children in Botswana: a cross-sectional survey. BMC Pediatr, 16, 106. doi: 10.1186/s12887-016-0643-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andiman WA (2011). Transition from pediatric to adult healthcare services for young adults with chronic illnesses: the special case of human immunodeficiency virus infection. J Pediatr, 159(5), 714–719. doi: 10.1016/j.jpeds.2011.06.040 [DOI] [PubMed] [Google Scholar]
- Badejo OA, Menson WNA, Sam-Agudu NA, Pharr J, Erekaha S, Bruno T, … Ezeanolue EE. (2018). Pediatric to adult healthcare transitioning for adolescents living with HIV in Nigeria: A national survey. PloS one, 13(6), e0198802. doi: 10.1371/journal.pone.0198802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beacham BL, & Deatrick JA (2013). Health care autonomy in children with chronic conditions: implications for self-care and family management. Nurs Clin North Am, 48(2), 305–317. doi: 10.1016/j.cnur.2013.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg-Kelly K (2003). Adolescent-friendly services. Acta Paediatr, 92(11), 1241–1242. Retrieved from http://onlinelibrary.wiley.com/doi/10.1111/j.1651-2227.2003.tb00490.x/abstract [DOI] [PubMed] [Google Scholar]
- Brousseau DC, Owens PL, Mosso AL, Panepinto JA, & Steiner CA (2010). Acute care utilization and rehospitalizations for sickle cell disease. JAMA : the journal of the American Medical Association, 303(13), 1288–1294. doi: 10.1001/jama.2010.378 [DOI] [PubMed] [Google Scholar]
- Cervia JS (2013). Easing the Transition of HIV-Infected Adolescents to Adult Care. AIDS patient care and STDs, 27(12), 692–696. doi: 10.1089/apc.2013.0253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Reddington C, Jacobs D, Meade R, Picard D, Singleton K, … Hsu HW (1997). School-related issues among HIV-infected children. Pediatrics, 100(1), E8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9200382http://pediatrics.aappublications.org/content/100/1/e8.full.pdf [DOI] [PubMed] [Google Scholar]
- Dahourou DL, Gautier-Lafaye C, Teasdale CA, Renner L, Yotebieng M, Desmonde S, … Leroy V (2017). Transition from paediatric to adult care of adolescents living with HIV in sub-Saharan Africa: challenges, youth-friendly models, and outcomes. J Int AIDS Soc, 20(Suppl 3), 34–49. doi: 10.7448/IAS.20.4.21528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies MA, Tsondai P, Tiffin N, Eley B, Rabie H, Euvrard J, … Boulle A. (2017). Where do HIV-infected adolescents go after transfer? - Tracking transition/transfer of HIV-infected adolescents using linkage of cohort data to a health information system platform. J Int AIDS Soc, 20(Suppl 3), 16–24. doi: 10.7448/IAS.20.4.21668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Silva PS, & Fishman LN (2014). Transition of the patient with IBD from pediatric to adult care-an assessment of current evidence. Inflamm Bowel Dis, 20(8), 1458–1464. doi: 10.1097/MIB.0000000000000045 [DOI] [PubMed] [Google Scholar]
- Fair CD, Sullivan K, Dizney R, & Stackpole A (2012a). “It’s like losing a part of my family”: transition expectations of adolescents living with perinatally acquired HIV and their guardians. AIDS patient care and STDs, 26(7), 423–429. doi: 10.1089/apc.2012.0041 [DOI] [PubMed] [Google Scholar]
- Fair CD, Sullivan K, Dizney R, & Stackpole A (2012b). “It’s like losing a part of my family”: transition expectations of adolescents living with perinatally acquired HIV and their guardians. AIDS patient care and STDs, 26(7), 423–429. doi: 10.1089/apc.2012.0041 [DOI] [PubMed] [Google Scholar]
- Fish R, Judd A, Jungmann E, O’Leary C, & Foster C (2014). Mortality in perinatally HIV-infected young people in England following transition to adult care: an HIV Young Persons Network (HYPNet) audit. HIV Med, 15(4), 239–244. doi: 10.1111/hiv.12091 [DOI] [PubMed] [Google Scholar]
- Freed GL, & Hudson EJ (2006). Transitioning children with chronic diseases to adult care: current knowledge, practices, and directions. J Pediatr, 148(6), 824–827. doi: 10.1016/j.jpeds.2006.02.010 [DOI] [PubMed] [Google Scholar]
- Gray WN, Schaefer MR, Resmini-Rawlinson A, & Wagoner ST (2018). Barriers to Transition From Pediatric to Adult Care: A Systematic Review. Journal of pediatric psychology, 43(5), 488–502. doi: 10.1093/jpepsy/jsx142 [DOI] [PubMed] [Google Scholar]
- Hoffman MA, Ushpiz V, & Levy-Shiff R (1988). Social support and self-esteem in adolescence. J Youth Adolesc, 17(4), 307–316. doi: 10.1007/BF01537672 [DOI] [PubMed] [Google Scholar]
- Hunt SE, & Sharma N (2010). Transition from pediatric to adult care for patients with sickle cell disease. JAMA : the journal of the American Medical Association, 304(4), 408–409; author reply 409. doi: 10.1001/jama.2010.1026 [DOI] [PubMed] [Google Scholar]
- Hussen SA, Chakraborty R, Camacho-Gonzalez A, Njiemoun B, Grossniklaus E, Goodstein E, … Del Rio C. (2018). Beyond “purposeful and planned”: varied trajectories of healthcare transition from pediatric to adult-oriented care among youth living with HIV. AIDS care, 1–3. doi: 10.1080/09540121.2018.1488029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikard K, Janney J, Hsu LC, Isenberg DJ, Scalco MB, Schwarcz S, … Kahn JG. (2005). Estimation of unmet need for HIV primary medical care: a framework and three case studies. AIDS education and prevention : official publication of the International Society for AIDS Education, 17(6 Suppl B), 26–38. doi: 10.1521/aeap.2005.17.SupplementB.26 [DOI] [PubMed] [Google Scholar]
- Izzo I, Quiros-Roldan E, Saccani B, Chiari E, Casari S, Foca E, … Castelli F. (2018). Perinatally HIV-Infected Youths After Transition from Pediatric to Adult Care, a Single-Center Experience from Northern Italy. AIDS research and human retroviruses, 34(3), 241–243. doi: 10.1089/AID.2017.0120 [DOI] [PubMed] [Google Scholar]
- Jensen PT, Paul GV, LaCount S, Peng J, Spencer CH, Higgins GC, … Ardoin SP. (2017). Assessment of transition readiness in adolescents and young adults with chronic health conditions. Pediatr Rheumatol Online J, 15(1), 70. doi: 10.1186/s12969-017-0197-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd A, Collins IJ, Parrott F, Hill T, Jose S, Ford D, … Sabin C (2017). Growing up with perinatal HIV: changes in clinical outcomes before and after transfer to adult care in the UK. J Int AIDS Soc, 20(Suppl 3), 21577. doi: 10.7448/IAS.20.4.21577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd A, & Davies MA (2018). Adolescent transition among young people with perinatal HIV in high-income and low-income settings. Curr Opin HIV AIDS, 13(3), 236–248. doi: 10.1097/COH.0000000000000448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakkar F, Van der Linden D, Valois S, Maurice F, Onnorouille M, Lapointe N, … Lamarre V (2016). Health outcomes and the transition experience of HIV-infected adolescents after transfer to adult care in Quebec, Canada. BMC Pediatr, 16, 109. doi: 10.1186/s12887-016-0644-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klassen AF, Grant C, Barr R, Brill H, Kraus de Camargo O, Ronen GM, … Gorter JW. (2015). Development and validation of a generic scale for use in transition programmes to measure self-management skills in adolescents with chronic health conditions: the TRANSITION-Q. Child Care Health Dev, 41(4), 547–558. doi: 10.1111/cch.12207 [DOI] [PubMed] [Google Scholar]
- Kung TH, Wallace ML, Snyder KL, Robson VK, Mabud TS, Kalombo CD, & Bekker LG (2016). South African healthcare provider perspectives on transitioning adolescents into adult HIV care. S Afr Med J, 106(8), 804–808. doi: 10.7196/SAMJ.2016.v106i8.10496 [DOI] [PubMed] [Google Scholar]
- Lee L, Yehia BR, Gaur AH, Rutstein R, Gebo K, Keruly JC, … Network, H. I. V. R. (2016). The Impact of Youth-Friendly Structures of Care on Retention Among HIV-Infected Youth. AIDS patient care and STDs, 30(4), 170–177. doi: 10.1089/apc.2015.0263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. (2008). Lancet, 372(9635), 293–299. doi: 10.1016/S0140-6736(08)61113-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maturo D, Powell A, Major-Wilson H, Sanchez K, De Santis JP, & Friedman LB (2015). Transitioning Adolescents and Young Adults With HIV Infection to Adult Care: Pilot Testing the “Movin’ Out” Transitioning Protocol. J Pediatr Nurs, 30(5), e29–35. doi: 10.1016/j.pedn.2015.06.013 [DOI] [PubMed] [Google Scholar]
- Murray KR, Dulli LS, Ridgeway K, Dal Santo L, Darrow de Mora D, Olsen P, … McCarraher DR. (2017). Improving retention in HIV care among adolescents and adults in low- and middle-income countries: A systematic review of the literature. PloS one, 12(9), e0184879. doi: 10.1371/journal.pone.0184879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naar-King S, Montepiedra G, Nichols S, Farley J, Garvie PA, Kammerer B, … Storm D (2009). Allocation of family responsibility for illness management in pediatric HIV. Journal of pediatric psychology, 34(2), 187–194. doi: 10.1093/jpepsy/jsn065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettitt ED, Greifinger RC, Phelps BR, & Bowsky SJ (2013). Improving health services for adolescents living with HIV in sub-Saharan Africa: a multi-country assessment. Afr J Reprod Health, 17(4 Spec No), 17–31. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24689314 [PubMed] [Google Scholar]
- Ryscavage P, Anderson EJ, Sutton SH, Reddy S, & Taiwo B (2011). Clinical outcomes of adolescents and young adults in adult HIV care. Journal of acquired immune deficiency syndromes, 58(2), 193–197. doi: 10.1097/QAI.0b013e31822d7564 [DOI] [PubMed] [Google Scholar]
- Ryscavage P, Macharia T, Patel D, Palmeiro R, & Tepper V (2016). Linkage to and retention in care following healthcare transition from pediatric to adult HIV care. AIDS care, 1–5. doi: 10.1080/09540121.2015.1131967 [DOI] [PubMed] [Google Scholar]
- Sainz T, & Navarro ML (2017). HIV-Infected Youths: Transition in Spain Compared to the Netherlands. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 64(2), 230. doi: 10.1093/cid/ciw702 [DOI] [PubMed] [Google Scholar]
- Sawicki GS, Kelemen S, & Weitzman ER (2014). Ready, set, stop: mismatch between self-care beliefs, transition readiness skills, and transition planning among adolescents, young adults, and parents. Clin Pediatr (Phila), 53(11), 1062–1068. doi: 10.1177/0009922814541169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang IC, Livingood W, … Wood D. (2011). Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ--Transition Readiness Assessment Questionnaire. Journal of pediatric psychology, 36(2), 160–171. doi: 10.1093/jpepsy/jsp128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz LA, Brumley LD, Tuchman LK, Barakat LP, Hobbie WL, Ginsberg JP, … Deatrick JA. (2013). Stakeholder validation of a model of readiness for transition to adult care. JAMA Pediatr, 167(10), 939–946. doi: 10.1001/jamapediatrics.2013.2223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz LA, Daniel LC, Brumley LD, Barakat LP, Wesley KM, & Tuchman LK (2014). Measures of readiness to transition to adult health care for youth with chronic physical health conditions: a systematic review and recommendations for measurement testing and development. Journal of pediatric psychology, 39(6), 588–601. doi: 10.1093/jpepsy/jsu028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz LA, Tuchman LK, Hobbie WL, & Ginsberg JP (2011). A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev, 37(6), 883–895. doi: 10.1111/j.1365-2214.2011.01282.x [DOI] [PubMed] [Google Scholar]
- Sherman GG, Lilian RR, Bhardwaj S, Candy S, & Barron P (2014). Laboratory information system data demonstrate successful implementation of the prevention of mother-to-child transmission programme in South Africa. S Afr Med J, 104(3 Suppl 1), 235–238. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24893499 [DOI] [PubMed] [Google Scholar]
- Simbayi LC, Z K,Zungu N, Moyo S, Marinda E, Jooste S, Mabaso M, Ramlagan S, North A, van Zyl J, Mohlabane N, Dietrich C, Naidoo I and the SABSSM V Team (2019). (2019). South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017. Cape Town, South Africa: HSRC [Google Scholar]
- Smits-Seemann RR, Kaul S, Zamora ER, Wu YP, & Kirchhoff AC (2017). Barriers to follow-up care among survivors of adolescent and young adult cancer. J Cancer Surviv, 11(1), 126–132. doi: 10.1007/s11764-016-0570-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- South African National Department of Health (2012). The 2012 National Antenatal Sentinel HIV and Herpes Simplex type-2 prevalence Survey. Pretoria, South Africa: Retrieved from http://www.hst.org.za/sites/default/files/ASHIVHerp_Report2014_22May2014.pdf [Google Scholar]
- Statistics South Africa. (2013). Recorded Live Births: 2013 Pretoria, South Africa [Google Scholar]
- Transitioning HIV-infected youth into adult health care. (2013). Pediatrics, 132(1), 192–197. doi: 10.1542/peds.2013-1073 [DOI] [PubMed] [Google Scholar]
- Weijsenfeld AM, Smit C, Cohen S, Wit FW, Mutschelknauss M, van der Knaap LC, … young adults study, g. (2016). Virological and Social Outcomes of HIV-Infected Adolescents and Young Adults in The Netherlands Before and After Transition to Adult Care. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. doi: 10.1093/cid/ciw487 [DOI] [PubMed] [Google Scholar]
- Wiener LS, Kohrt BA, Battles HB, & Pao M (2011). The HIV experience: youth identified barriers for transitioning from pediatric to adult care. Journal of pediatric psychology, 36(2), 141–154. doi: 10.1093/jpepsy/jsp129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia Q, Abraham B, Shah D, Ramaswamy C, Braunstein SL, & Torian LV (2018). Transition from pediatric to adult care among persons with perinatal HIV infection in New York City, 2006–2015. AIDS. doi: 10.1097/QAD.0000000000001923 [DOI] [PubMed] [Google Scholar]
- Zanoni BC, Archary M; Buchan S; Katz I; Haberer JE (2016). Systematic Review and Meta-analysis of the Adolescent and Young Adult HIV Continuum of Care in South Africa: The Cresting Wave. BMJ Global Health(1 (3) e000004; DOI: 10.1136/bmjgh-2015-000004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanoni BC, Sibaya T, Cairns C, & Haberer JE (2019). Barriers to Retention in Care are Overcome by Adolescent-Friendly Services for Adolescents Living with HIV in South Africa: A Qualitative Analysis. AIDS and behavior, 23(4), 957–965. doi: 10.1007/s10461-018-2352-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanoni BC, Sibaya T, Cairns C, Lammert S, & Haberer JE (2017). Higher retention and viral suppression with adolescent-focused HIV clinic in South Africa. PloS one, 12(12), e0190260. doi: 10.1371/journal.pone.0190260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang LF, Ho JS, & Kennedy SE (2014). A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatr, 14, 4. doi: 10.1186/1471-2431-14-4 [DOI] [PMC free article] [PubMed] [Google Scholar]


