Abstract
Objectives:
The COVID-19 pandemic has caused considerable stress throughout the world. Little is known about how postpartum women who gave birth during the early months of the pandemic were impacted. The purpose of this study was to explore and describe the associations between potential risk, protective factors, and psychological distress among postpartum women who gave birth during the early months of the COVID-19 pandemic.
Methods:
Postpartum women over the age of 18 years who gave birth in the US hospitals between March and July of 2020 and spoke English completed a survey about their experiences. Demographic and health variables were measured via self-report. Stress was measured using the Perceived Stress Scale-10. Mastery was measured with the Pearlin Mastery Scale. Resilience was measured with the Connor–Davidson Resilience Scale-2.
Results:
This study included 885 women. Participants had higher stress and lower resilience relative to pre-pandemic norms. Participants had high levels of depression, anxiety, and stress. Women who had an infant admitted to the neonatal intensive care unit had more stress. Income, full-time employment, and partnered relationships were associated with lower stress. Resilience and mastery were related to lower stress, depression, and anxiety. Black, Indigenous, or People of Color women showed higher stress and lower resiliency. Single women were likely to report lower levels of mastery than partnered women.
Conclusion:
Stress, depression, and anxiety were high in postpartum women in this study. Income, partnered relationships, and employment security, along with protective traits such as mastery and resilience, may reduce the impact of stress on postpartum women in a pandemic. Care models should be modified to support women during a pandemic. Health disparities exist in postpartum stress. Future interventions should focus on building resiliency and mastery and ensuring appropriate resources are available to postpartum women in a pandemic.
Keywords: birth, COVID, mastery, pregnancy, resilience, stress
Introduction
The COVID-19 pandemic has been associated with increased depression, anxiety, and disrupted sleep for pregnant and postpartum women and disproportionately affects women from vulnerable populations.1–7 The perinatal time frame is a critical interval of elevated risk for stress and mental health challenges.8 Numerous factors impact stress levels during the perinatal interval, including preexisting stress, baseline mental health status, maternal or fetal health conditions, and demographic characteristics.9–11
During the early months of the COVID-19 pandemic, common perinatal stressors were compounded with pandemic-related concerns such as fear of contracting infection, disruptions to the daily routine, social isolation, job or financial changes, actual or threatened loss of loved ones, difficulty accessing medical care, increased childcare responsibilities, and the psychological demands of quarantining at home.12 Likewise, Brooks et al.13 found that during infectious disease outbreaks, pregnant women experience negative emotional states, live with uncertainty, are concerned about infection, have disrupted routines, financial and occupational concerns, and disrupted expectations of birth, prenatal, and postnatal care.
Maternal stress is associated with adverse psychological and physiological perinatal outcomes.14–18 Autonomic physiologic mechanisms in the stress response are essential to maintain homeostasis.19 A dysregulation or excessive activation of the normal physiologic stress response eventually causes “wear and tear” on body systems, known as allostatic load, leading to a myriad of health complications.19 The physiologic mechanisms associated with pregnancy include shifts in neuroendocrine, inflammatory, and autonomic activation, which can further exacerbate the stress response, increasing the risk of maternal physiological and psychological complications in the perinatal time frame.20,21
As the number and severity of stressors encountered increase, the risk of developing perinatal complications and psychological health problems such as depression and anxiety also increases.22–25 The way stress is experienced and interpreted by individuals relates to perceptions, coping mechanisms, and interaction with the environment rather than the stressor itself.26 A fundamental premise of allostatic load is not only the amount of stress but also the perception of stress, suggesting it is the individual’s interpretation and learned emotional response to the stressor that triggers a potentially maladaptive physiologic response.19
Protective factors
While the threats associated with the global pandemic would seem to be objective and universal stressors, not all women who give birth during the pandemic experience stress or poor mental health outcomes.27 When measuring a risk such as stress, it is imperative to measure strengths to provide a more balanced and accurate view of research participants.28 Strengths are protective factors that may reduce the effects of stressors and promote mental health, even under circumstances of adversity.29 Protective factors may include resources, individual traits, and additional modifiable variables on which to build future research and interventions.
Resources such as education, income, employment, and supportive relationships are protective from stress and promotive of health.30 Protective resources increase access to materials and opportunities that may reduce risk and improve the ability to manage stress as it occurs. In addition to resources, protective traits include personality characteristics and ways of thinking that affect behavior and that may reduce stress.31,32 Those with protective traits may conceptualize stress as a challenge that they can cope with and overcome, thus seeing stress as a functional cognitive process rather than viewing stress as a threat.26,33,34 This process of positive cognitive appraisal has been associated with reduced stress in pregnant women in the COVID-19 pandemic.35
The protective trait of mastery includes the individual’s belief that they have control over their life, rather than believing that they are fatalistically ruled by others.34,36 Mastery overlaps with traits of self-efficacy and internal locus of control.37 Individuals with a high sense of mastery are more likely to believe they can cope with or control life’s problems, thus being less psychologically impacted by stressors.32 Individuals with a sense of mastery may be more likely to engage in stress-reducing actions within their power, such as maintaining a routine, completing goal-oriented work, and seeking support when needed.38
Resilience is a protective trait that includes recovering from setbacks quickly and successfully adapting despite adversity.29,31 Resilience is also demonstrated by an individual’s ability to maintain optimal functioning and growth when faced with the barrage of day-to-day stressors.39 Overall, resilience is an internal trait that includes adapting to and recovering from both big and small stressors and maintaining that positive adaptation going forward.29,31,39
During the early months of the COVID-19 pandemic, postpartum women faced minor and major stressors. The purpose of this study was to explore and describe associations between potential risk (e.g. socioeconomic disadvantage, racial disparities, and perinatal variables) and protective factors (e.g. resources, mastery, and resilience) with psychological distress (perceived stress, anxiety, and depression) among postpartum women who gave birth during the early months of the COVID-19 pandemic.
Methods
This study was part of a larger project examining the prenatal, intrapartum, and postpartum experiences of women who gave birth in the US hospitals during the early months of the COVID-19 pandemic. This exploratory, descriptive cross-sectional study focused on perceived stress, mastery, resilience, and perinatal variables in this population. Ethical approval was obtained from the institutional review board (IRB) (IRB# 303-20-EP) at the University of Nebraska Medical Center. Using the number of births in the United States in the previous year, a 95% confidence interval, and a margin of error of 5%, the minimum sample size was determined to be 385 (Qualtrics, Provo, UT, USA).
Participants
To be included in the study, participants were required to be postpartum women over the age of 18 years who gave birth in a US hospital between 1 March and 22 July 2020. Participants were required to be able to read or write in English or provide an interpreter.
Procedures
Participants were recruited via social media (Facebook and Instagram) through specific ads aimed at women of childbearing age. In addition, ads for the survey were shared on social media and via word of mouth. Women were invited to complete a survey hosted on the secure REDCap research platform. Participants were provided a narrative consent which they were required to electronically agree to via a checkbox prior to completing the questionnaire. The instrument was 80 items and included demographics, health information, and validated tools on stress, resilience, and mastery as listed below.
Measures
Demographic and health information
Demographic information such as race, ethnicity, age, education level, income, and employment status was collected. To collect health information, participants were asked (yes and no), “Did you experience any of the following health conditions during your pregnancy, delivery, or postpartum in 2020?” with the following conditions: depression, anxiety, diabetes, asthma, hypertension, pre-eclampsia, shoulder dystocia, postpartum hemorrhage, or other (free text). Obstetrical information such as the number of pregnancies, deliveries, delivery method, gestational age of neonate, and neonatal intensive care unit (NICU) admission was also collected.
Perceived stress
The 10-item Perceived Stress Scale (PSS-10) was used to measure stress.40,41 The PSS-10 is a widely used instrument to measure stress that requires the participant to reflect on general stress in the previous month. A higher score on the PSS-10 reflects a higher stress level. The PSS-10 has adequate internal consistency (α = 0.78) and is both reliable and valid in multiple languages and settings.40,41 Scores range from 0 to 40, with a higher number indicating more stress. The PSS-10 is not a diagnostic instrument, so there are no official score cut-offs. However, common classification of the PSS-10 by stress level includes low (0–13), moderate (14–26), and high (27–40) stress.42 Pre-pandemic normative values were established in a US population in 2009, reporting a mean of 16.1 for women (standard deviation (SD) = 7.6) and 15.5 for men (SD = 7.4).43
Resilience
Resilience was measured using the two-item Connor–Davidson resilience index (CD-RISC2). The CD-RISC2 is a measure of the resilience attributes “bounce back” and adaptability from the original 23-item CD-RISC instrument.44,45 The original CD-RISC has high internal consistency (α = 0.81).44 The CD-RISC2 has good test–retest reliability and validity.45 A higher CD-RISC2 score correlates to higher levels of resilience. In a population survey of US adults, the normative mean CD-RISC2 score was 6.91.45 Lowered norm scores have been established for psychiatric outpatients (6.12) in those with depression (5.12) and survivors of traumatic incidents such as a tsunami natural disaster (4.67).45,46
Mastery
Mastery was measured using the 7-item Pearlin Mastery (PM) Scale, which measures the extent to which an individual regards their life circumstances as being under their control. Participants respond on a 4-point scale from “strongly agree” to “strongly disagree” on questions such as “What happens to me in the future mostly depends on me.”36 A higher PM score is associated with higher levels of mastery traits. After reverse scoring two items, an overall score is summed. Higher scores indicate a greater sense of mastery. The PM has been found to have good psychometric properties, demonstrating good reliability and convergent validity in diverse populations.47,48
Statistical analysis
We used IBM SPSS version 25 and Mplus version 8 for the statistical analyses. All available data were used, and no imputation was performed. Descriptive statistics were calculated on all study variables. Sample t-tests were conducted to compare the sample to established norms. Independent groups t-tests were used to examine differences in stress and mental health across categories on protective factors and self-reported health conditions. The Spearman correlations were calculated to assess the relationships among measures of mastery, resilience, and stress.
To test if associations found between demographic variables and stress were potentially explained by participants’ resilience or levels of mastery since these are thought to be traits on which interventions can be built, the steps outlined by Baron and Kenny were followed using a series of regression models.49 For a variable to be a mediator, the demographic variable must be associated with that variable, and the variable must then have a significant effect on the outcome. In a regression model that shows a significant effect of the demographic variable, upon adding the potential mediator as a predictor, if the effect of the demographic variable is no longer significant, then mediation is present. Indications of mediation were verified by testing significance of indirect effects via path models in Mplus version 8, using maximum likelihood estimation and bootstrapping for testing indirect effects, following the methods outlined by Preacher and Hayes.50
Results
Eight hundred eighty-five postpartum women aged 18–43 years who gave birth in the United States between 1 March and 9 July 2020 indicated they were eligible for the study, gave consent, and participated between 22 May and 22 July 2020. Sixteen hundred twenty-two individuals clicked on the study link, but it is unknown how many of these individual clicks were eligible participants. The response rate calculated simply by participation versus clicks was 54% (885/1622). There was at least one participant from each US state. The average length of time since birth was 56.8 days (SD = 31.2). The average age of the participant was 29.9 years (SD = 4.9). 84.7% were White, and 15.3% were Black, Indigenous, or People of Color (BIPOC) (2.9% Asian, 1.4% Black, 9.2% Hispanic, and 1.8% other). 82.3% were married, and 12.4% were in a committed relationship, leaving the remainder of the sample single (4.5%), widowed, or divorced (0.7%). The sample was highly educated, with 63.6% having a bachelor’s degree or higher. In addition, 56.9% had an income greater than US $70,000. Seven hundred sixty-eight women (87% of the sample) completed the PSS-10. There was a slightly higher percentage of PSS-10 completion in White participants (87.7%) than in BIPOC women (81.5%) (chi-q(1) = 3.89, p = 0.048), but no other demographic or perinatal variable differences between women who completed the PSS-10 and those who did not.
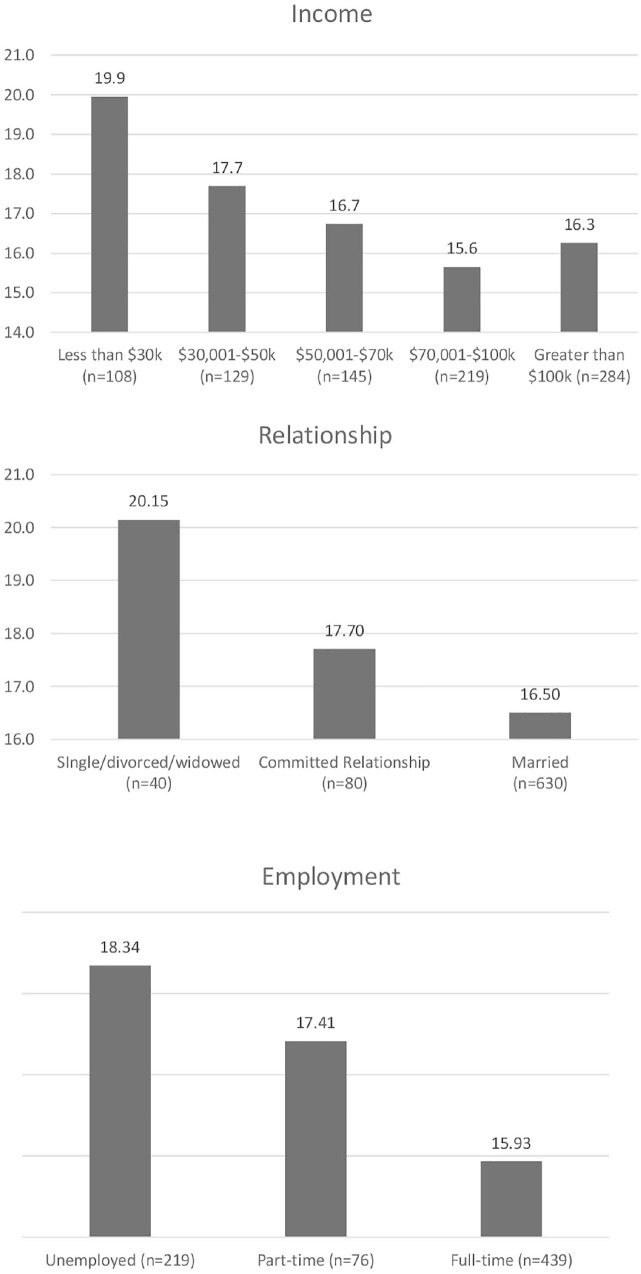
Women in our sample were significantly more stressed when compared to a normative sample (16.85 vs 16.14, p < 0.001). In our sample, 67.6% of the participants were stressed (moderate or high). Women who had an infant admitted to the NICU were more stressed than other mothers (18.1 vs 16.6, p = 0.038). Single women were significantly more stressed than partnered women (20.15 vs 16.7, p = 0.003) (Figure 1). BIPOC women were significantly more likely to report stress compared to White women (18.3 vs 16.6, p = 0.021). Education level did not associate with stress at a meaningful level (rs = −0.060, p = 0.097), but a higher income was associated with lower levels of stress (rs = −0.14, p < 0.001) and PSS-10 scores were lower when reporting employment versus no employment (16.16 vs 17.8, p = 0.002) (Figure 1).
Figure 1.
Perceived stress level by income, relationship, and employment.
When looking at the psychological variables of depression and anxiety and the remaining perinatal variables, depression was significantly higher in women who had a preterm birth (p = 0.039), and anxiety was associated with hypertension (p = 0.028) and postpartum hemorrhage (p = 0.030). There were no differences in PSS-10 based on gestational age, type of delivery, or presence of asthma, diabetes, high blood pressure, preeclampsia, postpartum hemorrhage, or shoulder dystocia.
The protective traits of resiliency and mastery were related to lower levels of PSS-10 (r = −0.436, p < 0.001, r = −0.723, p < 0.001), as well as depression and anxiety (Table 1). Relative to a normative sample, our sample had lower overall resilience levels (6.91 vs 6.00, p < 0.001). Resilience levels were lower in BIPOC women compared to White women (5.64 vs 6.06, p = 0.007). Women in relationships had higher levels of mastery than single women (36.6 vs 33.8, p = 0.024). Mastery also improved with income level (r = 0.186, p < 0.001). Table 1 shows the relationship between stress, protective traits, and depression and anxiety.
Table 1.
Perceived stress, mastery, and resilience in women who gave birth during COVID-19 by self-reported anxiety or depression status.
| Measure | Diagnosis | N | Mean | SD | t-test | Range |
|---|---|---|---|---|---|---|
| Self-reported anxiety | ||||||
| Perceived Stress Scale (PSS-10) | No anxiety | 500 | 14.91 | 6.95 | t(766) = −10.84, p < 0.001 | 0–36 |
| Anxiety | 268 | 20.47 | 6.42 | d = −0.82 | 4–37 | |
| Pearlin Mastery Scale | No anxiety | 451 | 37.95 | 6.83 | t(693) = 7.77, p < 0.001 | 14–49 |
| Anxiety | 244 | 33.68 | 7.10 | d = 0.62 | 14–49 | |
| CD-RISC2 | No anxiety | 450 | 6.24 | 1.22 | t(692) = 7.14, p < 0.001 | 2–8 |
| Anxiety | 244 | 5.56 | 1.19 | d = 0.57 | 3–8 | |
| Self-reported depression | ||||||
| Perceived Stress Scale (PSS-10) | No depression | 614 | 15.59 | 7.01 | t(266) = −11.08, p < 0.001 | 0–36 |
| Depression | 154 | 21.84 | 6.05 | d = −0.91 | 4–37 | |
| Pearlin Mastery Scale | No depression | 557 | 37.39 | 7.03 | t(693) = 7.1, p < 0.001 | 14–49 |
| Depression | 138 | 32.68 | 6.72 | d = 0.68 | 14–49 | |
| CD-RISC2 | No depression | 556 | 6.14 | 1.22 | t(692) = 6.1, p < 0.001 | 2–8 |
| Depression | 138 | 5.43 | 1.20 | d = 0.58 | 3–8 | |
SD: standard deviation; CD-RISC2: two-item Connor–Davidson resilience index.
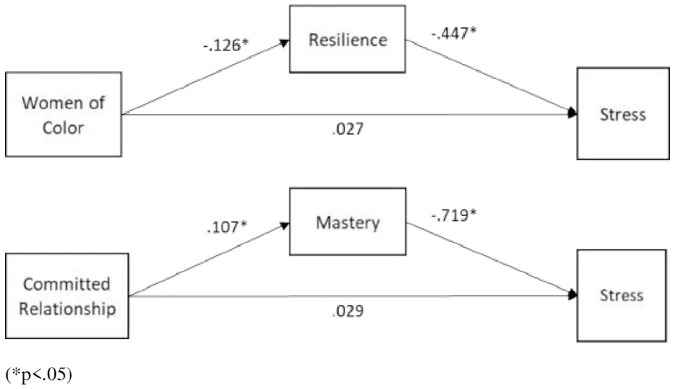
Since race, relationship status, NICU stays, and postpartum hemorrhage were found to be associated with stress, mediation models were performed to determine if associations with resilience or mastery potentially accounted for these relationships. NICU stays or postpartum hemorrhage was not found to be associated with levels of resilience or mastery. Race, however, was found to be associated with resilience and relationship status was associated with mastery. While BIPOC women were found to have significantly higher stress, they also had significantly lower levels of resilience, and lower resilience was associated with higher levels of stress. Accounting for resilience in a regression model resulted in a non-significant effect of race on stress, which is consistent with the proposed mediation model that resilience mediated the effect of race on stress. Similarly, women who were either married or in a committed relationship had significantly higher levels of mastery, which are in turn associated with lower levels of stress. Our results supported the proposed mediation model that mastery mediated the effect of relationship status on stress. Figure 2 shows the standardized path model coefficients demonstrating these significant indirect effects, which satisfied Baron and Kenny’s criteria and were verified using path models estimated in Mplus.
Figure 2.
Mediation model demonstrating indirect effects of demographic variables on stress.
Discussion
This study of 885 postpartum women who gave birth during the COVID-19 pandemic focused on the associations between potential risk, protective factors, including resilience and mastery, and psychological distress. Women in our sample had high rates of self-reported depression and anxiety and were significantly more stressed than women in previously reported normative samples.43
While the difference in PSS-10 score compared to the established normative sample was statistically significant, current normative data in childbearing women have not been established, and it is unclear whether this stress difference would be clinically significant or contextually relevant when compared to the general population’s stress levels during a pandemic. Recent studies of women in the prenatal and postpartum time frame have shown lower levels of stress as measured by the PSS-10 when compared to our sample.51 As research continues to be conducted during the COVID-19 pandemic, our results add to the emerging body of research that overall stress, depression, and anxiety levels are elevated during the pandemic and are impacting postpartum women.1,52
The stress and mental health challenges associated with perinatal variables in this study such as preterm birth, NICU stay, postpartum hemorrhage, or hypertension may have had no relationship to the pandemic since they are in and of themselves stressors. Alternatively, these stressors may have been exacerbated by the pandemic. Further research on these variables both and in and outside of a pandemic is required.
We found that multiple protective resources and traits were associated with reduced stress in our sample. The protective resources of income, employment, and a partnered (committed or married) relationship were associated with lower stress. Lower levels of stress, depression, and anxiety were related to higher levels of the protective traits of mastery and resilience.
Mastery, or the sense of control one feels over their life, may improve stress coping and stress-reducing behaviors. Partnered women had a higher level of mastery compared to single women and mastery potentially mediated the association between partnered relationship and reduced stress. When women are single mothers, they may face more situations in their life that are out of their control, such as more parental responsibility or economic uncertainty and may lack relational support. Mastery levels were not changed by race or education but were improved with income level. During the earliest months of the pandemic, there was widespread uncertainty and furloughs, layoffs, and the closure of daycares and schools were the norm. During this time, women were more likely than men to lose their jobs and face economic turmoil while being the primary caretakers of their children with potential home-educating responsibilities.53 Thus, it is unsurprising that women in this study with a lower income had lower mastery scores.
Resilience is an important trait to cope with stress when dealing with an unexpected pandemic while being a postpartum mother. Resilience scores were significantly lower for women in this study when compared to a normative sample, although these norms are not up to date or relevant to the current context of being a childbearing woman in a global pandemic. The mean score was lower than normative values that have been established for psychiatric outpatients but higher than individuals who went through a natural disaster.45 Individual’s perceptions of both stress and how they cope with stress may be different when they are being faced with a significant stressor, like a pandemic in the perinatal time frame. Similar to our mastery-related results, individuals with a higher level of income had higher resilience levels. Having a higher income is a resource that may affect the perception of and actual ability to bounce back from adversity. Interestingly, resilience was not associated with relationship status, indicating that this trait may be important to foster for women since it does not rely on a protective resource for success.
BIPOC women in our sample were likely to have higher levels of stress and lower levels of resilience compared to White women. Our findings support that BIPOC women were experiencing greater perceived and actual stress during the pandemic. During the time frame of the study, in addition to the global pandemic, the United States was also experiencing widespread protests against systemic racial injustice that may have further impacted stress levels in BIPOC postpartum women.54 While our sample under-represented most racial groups, there are known racial disparities in maternal and mental health.55,56 Cumulative discrimination throughout the lifetime affects levels of stress, resilience, and overall health.57,58 Vigilance or the continual state of being alert to the threats of racism and discrimination has deleterious effects on mental health. The chronic activated state of vigilance in individuals experiencing discrimination is associated with racial mental health disparities.59 BIPOC women faced the potential cumulative layers of stress from discrimination, racial unrest, known maternal health disparities, and a global pandemic. It is unclear why resilience was lower in BIPOC women. Resilience levels potentially mediated the association between race and stress, supporting that resilience is an especially important protective trait against stress for BIPOC postpartum women. Conclusions should not be drawn from these associations in this study due to the complexities of racial health disparities, our small sample of BIPOC women, and the use of cross-sectional data.
Recommendations
More research is needed on the experience of postpartum women during a pandemic, protective factors from stress, along with further exploration of related contextual factors. Interventions should be designed with women and should focus on diverse populations to be culturally and contextually relevant. Resilience- building interventions focused on enhancing problem-solving and planning skills, promoting spirituality, positive cognitive appraisal, and acceptance of negative situations and emotions may be of benefit to this population.60 While mastery may be more fixed than resilience, it can be improved through cognitive-behavioral and educational interventions aimed at increasing perceived control, mindfulness, and acceptance over stressful situations.61 Established evidence-based interventions for mental health during the perinatal period that may include promotion of resilience and mastery include cognitive behavior therapy, interpersonal therapy, behavioral activation, and dialectical behavior therapy.62–66
Recommendations for clinicians include incorporating trauma-informed care and assessing the patient for increased stress, depression, and anxiety.67 Principles of trauma-informed include safety, trust, support, shared decision-making, and empowerment.68 Acknowledging stress and providing women with an opportunity to safely share their concerns, even for a few minutes, are simple, effective, and beneficial interventions that may help alleviate stress. Ensuring updated and tangible resources are readily available to women is another important consideration during periods of increased societal stress. Appreciating the role of stress in the pathophysiology of physiological and psychological complications and incorporating opportunities to promote and advocate for stress-reducing strategies appropriate for each woman are critical during a pandemic.
Limitations
A limitation is that participants were not representative of the general population. While we had at least one participant from each state, the data were not distributed in a manner that would support an accurate analysis based on geography, or among participants who were in COVID “hotspots.” Normative values used for analysis were not within the past 5 years, and not reflective of a pandemic or a postpartum population. We did not include screening or diagnostic instruments or review participant’s medical records to ensure that the diagnoses they self-reported were accurate. We only collected basic information on perinatal health, and participants had varying levels of pregnancy and postpartum risk and in turn related healthcare experiences, which may have impacted stress levels. The sample was biased with low diversity, high socioeconomic status, high educational attainment, and generally good health. Based on this, we might assume that extreme mental health concerns and stress are under-represented and that the protective factors of resilience and self-mastery are over-represented.
The sample only included English speakers or those who could provide an interpreter, and no recruitment materials were provided in other languages. Another limitation is the cross-sectional study design, which restricts the determination of causality and, thus, the directionality among variables within relationships. Due to the observational nature of the data, the mediation analyses performed cannot determine causation, and do not rule out that a Type I error occurred or that the mediating variables were not confounding variables since they are statistically identical.69,70 The study only gathered information from a single time point and did not measure the longitudinal changes of stress one might expect as infection rates and social distancing measures changed throughout the course of the pandemic. The nature of the relationships between perceived stress, perinatal variables, and the protective resources and traits of resilience and mastery in childbearing women may not be consistent outside of a pandemic and should be further explored in future studies. The use of self-report to collect the data and social media for recruitment are known to be associated with a level of bias, further reducing the objectivity of the results.71
Conclusion
The COVID-19 pandemic created layers of stressors for postpartum women. Maternal stress is associated with poor health outcomes, and the development of maternal psychological problems. This study showed that women who gave birth in the pandemic had high levels of stress and self-reported depression and anxiety. Overcoming stress is a multidimensional and dynamic process that includes protective resources and individual traits. In this study, protective resources associated with reduced stress were income, full-time employment, and a partnered relationship. Protective internal traits associated with reduced stress were resilience and mastery. Racial disparities existed, with BIPOC women showing higher levels of stress and lower levels of resilience compared to White women, with resilience potentially mediating this association. In addition, single women showed higher stress and lower levels of mastery, and mastery potentially mediated this association. More research is needed on women who give birth during a pandemic, with an emphasis on strengths and protective factors, as well as health disparities.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455065211042190 for Postpartum stress and protective factors in women who gave birth in the United States during the COVID-19 pandemic by Elizabeth Mollard, Kevin Kupzyk and Tiffany Moore in Women’s Health
Footnotes
Author contributions: E.M. was responsible for study conceptualization, methodology, investigation, analysis, writing the first draft, and writing revisions. K.K. was responsible for formal analysis, writing the first draft, and writing revisions. T.M. was responsible for formal analysis, writing the first draft, and reviewing revisions.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: EM received funding for this study from the Sigma Theta Tau International Gamma Pi Chapter Sister Patricia Miller Award.
ORCID iD: Elizabeth Mollard  https://orcid.org/0000-0003-0221-3459
https://orcid.org/0000-0003-0221-3459
Supplemental material: Supplemental material for this article is available online.
References
- 1.Lebel C, MacKinnon A, Bagshawe M, et al. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord 2020; 277: 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yan H, Ding Y, Guo W.Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Front Psychol 2020; 11: 617001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Preis H, Mahaffey B, Heiselman C, et al. Vulnerability and resilience to pandemic-related stress among US women pregnant at the start of the COVID-19 pandemic. Soc Sci Med 2020; 266: 113348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corbett GA, Milne SJ, Hehir MP, et al. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol 2020; 249: 96–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Talbot J, Charron V, Konkle A.Feeling the void: lack of support for isolation and sleep difficulties in pregnant women during the COVID-19 pandemic revealed by twitter data analysis. Int J Environ Res Public Health 2021; 18(2): 393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tomfohr-Madsen LM, Racine N, Giesbrecht GF, et al. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res 2021; 300: 113912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hessami K, Romanelli C, Chiurazzi M, et al. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. Epub ahead of print 1 November 2020. DOI: 10.1080/14767058.2020.1843155. [DOI] [PubMed] [Google Scholar]
- 8.O’Hara MW, Wisner KL.Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol 2014; 28(1): 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Furtado M, Chow CH, Owais S, et al. Risk factors of new onset anxiety and anxiety exacerbation in the perinatal period: a systematic review and meta-analysis. J Affect Disord 2018; 238: 626–635. [DOI] [PubMed] [Google Scholar]
- 10.Hutchens BF, Kearney J.Risk factors for postpartum depression: an umbrella review. J Midwifery Womens Health 2020; 65(1): 96–108. [DOI] [PubMed] [Google Scholar]
- 11.Field T.Prenatal depression risk factors, developmental effects and interventions: a review. J Pregnancy Child Health 2017; 4(1): 301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pfefferbaum B, North CS.Mental health and the Covid-19 pandemic. New Eng J Med 2020; 383(6): 510–512. [DOI] [PubMed] [Google Scholar]
- 13.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020; 395(10227): 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abbott PW, Gumusoglu SB, Bittle J, et al. Prenatal stress and genetic risk: how prenatal stress interacts with genetics to alter risk for psychiatric illness. Psychoneuroendocrinology 2018; 90: 9–21. [DOI] [PubMed] [Google Scholar]
- 15.Van den Bergh BR, van den Heuvel MI, Lahti M, et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci Biobehav Rev 2020; 117: 26–64. [DOI] [PubMed] [Google Scholar]
- 16.Aizer A, Stroud L, Buka S.Maternal stress and child outcomes: evidence from siblings. J Hum Resour 2016; 51(3): 523–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bush NR, Savitz J, Coccia M, et al. Maternal stress during pregnancy predicts infant infectious and non-infectious illness. J Pediatr 2020; 228: 117–125.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pawluski JL, Lonstein JS, Fleming AS.The neurobiology of postpartum anxiety and depression. Trends Neurosci 2017; 40(2): 106–120. [DOI] [PubMed] [Google Scholar]
- 19.McEwen BS.Stress, adaptation, and disease: allostasis and allostatic load. Ann N Y Acad Sci 1998; 840(1): 33–44. [DOI] [PubMed] [Google Scholar]
- 20.Glynn LM, Davis EP, Sandman CA.New insights into the role of perinatal HPA-axis dysregulation in postpartum depression. Neuropeptides 2013; 47(6): 363–370. [DOI] [PubMed] [Google Scholar]
- 21.Torgersen CKL, Curran CA. A systematic approach to the physiologic adaptations of pregnancy. Crit Care Nurs Q 2006; 29(1): 2–19. [DOI] [PubMed] [Google Scholar]
- 22.Hammen C.Stress and depression. Annu Rev Clin Psychol 2005; 1: 293–319. [DOI] [PubMed] [Google Scholar]
- 23.Muscatell KA, Slavich GM, Monroe SM, et al. Stressful life events, chronic difficulties, and the symptoms of clinical depression. J Nerv Ment Dis 2009; 197(3): 154–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nowak AL, Anderson CM, Mackos AR, et al. Stress during pregnancy and epigenetic modifications to offspring DNA: a systematic review of associations and implications for preterm birth. J Perinat Neonatal Nurs 2020; 34(2): 134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lima SAM, El Dib RP, Rodrigues MRK, et al. Is the risk of low birth weight or preterm labor greater when maternal stress is experienced during pregnancy? A systematic review and meta-analysis of cohort studies. PLoS ONE 2018; 13(7): e0200594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lazarus RS. The Stress and Coping Paradigm. In: Eisdorfer C, Cohen D, Kleinman A, et al. (eds.), Models for Clinical Psychopathology. New York: Spectrum, 1981, pp. 177–214. [Google Scholar]
- 27.Tuason MT, Güss CD, Boyd L.Thriving during COVID-19: predictors of psychological well-being and ways of coping. PLoS ONE 2021; 16(3): e0248591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mollard E, Hatton-Bowers H, Tippens J.Finding strength in vulnerability: ethical approaches when conducting research with vulnerable populations. J Midwifery Womens Health 2020; 65: 802–807. [DOI] [PubMed] [Google Scholar]
- 29.O’Leary VE.Strength in the face of adversity: individual and social thriving. J Soc Issues 1998; 54(2): 425–446. [Google Scholar]
- 30.Allen J, Balfour R, Bell R, et al. Social determinants of mental health. Int Rev Psychiatr 2014; 26(4): 392–407. [DOI] [PubMed] [Google Scholar]
- 31.Luthar SS, Cicchetti D, Becker B.The construct of resilience: a critical evaluation and guidelines for future work. Child Dev 2000; 71(3): 543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lazarus RS, Folkman S.Stress, appraisal, and coping. New York: Springer, 1984. [Google Scholar]
- 33.Liu JJ, Vickers K, Reed M, et al. Re-conceptualizing stress: shifting views on the consequences of stress and its effects on stress reactivity. PLoS ONE 2017; 12(3): e0173188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seib C, Porter-Steele J, Ng SK, et al. Life stress and symptoms of anxiety and depression in women after cancer: the mediating effect of stress appraisal and coping. Psychooncology 2018; 27(7): 1787–1794. [DOI] [PubMed] [Google Scholar]
- 35.Khoury JE, Atkinson L, Bennett T, et al. COVID-19 and mental health during pregnancy: the importance of cognitive appraisal and social support. J Affect Disord 2021; 282: 1161–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pearlin LI, Schooler C.The structure of coping. J Health Soc Behav 1978; 1: 2–21. [PubMed] [Google Scholar]
- 37.Wallston KA. Control beliefs: health perspectives. In: International encyclopedia of the social & behavioral sciences. 2nd ed.Amsterdam: Elsevier, 2015, pp. 819–821. [Google Scholar]
- 38.Roepke SK, Grant I.Toward a more complete understanding of the effects of personal mastery on cardiometabolic health. Health Psychol 2011; 30(5): 615–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zautra AJ, Hall JS, Murray KE. Resilience: A new definition of health for people and communities. In: Reich JW, Zautra AJ, Hall JS. (eds.), Handbook of adult resilience. The Guilford Press, 2010, pp. 3–29. [Google Scholar]
- 40.Cohen S, Kamarck T, Mermelstein R.A global measure of perceived stress. J Health Soc Behav 1983; 24(4): 385–396. [PubMed] [Google Scholar]
- 41.Cohen S.Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S. (eds.), The Social Psychology of Health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage, 1988, pp. 31-67. [Google Scholar]
- 42.Perceived Stress Scale, https://das.nh.gov/wellness/docs/percieved%20stress%20scale.pdf
- 43.Cohen S, Janicki-Deverts D.Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol 2012; 42(6): 1320–1334. [Google Scholar]
- 44.Connor KM, Davidson JR.Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003; 18(2): 76–82. [DOI] [PubMed] [Google Scholar]
- 45.Vaishnavi S, Connor K, Davidson JR.An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatr Res 2007; 152(2–3): 293–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Irmansyah I, Dharmono S, Maramis A, et al. Determinants of psychological morbidity in survivors of the earthquake and tsunami in Aceh and Nias. Int J Ment Health Syst 2010; 4(1): 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marshall GN, Lang EL.Optimism, self-mastery, and symptoms of depression in women professionals. J Pers Soc Psychol 1990; 59(1): 132–139. [DOI] [PubMed] [Google Scholar]
- 48.Walford-Kraemer P, Light HK.Depression and mastery in women: differences according to personal characteristics. Psychol Rep 1984; 54: 710. [DOI] [PubMed] [Google Scholar]
- 49.Baron RM, Kenny DA.The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986; 51(6): 1173–1182. [DOI] [PubMed] [Google Scholar]
- 50.Preacher KJ, Hayes AF.Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 2008; 40(3): 879–891. [DOI] [PubMed] [Google Scholar]
- 51.Racine N, Madigan S, Plamondon A, et al. Maternal psychosocial risk profiles in pregnancy: associations with postpartum maternal health and child outcomes. Clin Psychol Sci 2018; 6(6): 783–796. [Google Scholar]
- 52.Mollard E, Wittmaack A.Experiences of women who gave birth in US hospitals during the COVID-19 pandemic. J Patient Exp. Epub ahead of print 12 January 2021. DOI: 10.1177/2374373520981492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Power K.The COVID-19 pandemic has increased the care burden of women and families. Sustain 2020; 16(1): 67–73. [Google Scholar]
- 54.Wakeel F, Njoku A.Application of the weathering framework: intersection of racism, stigma, and COVID-19 as a stressful life event among African Americans. Healthcare (Basel) 2021; 9(2): 145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Williams DR.Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Behav 2018; 59(4): 466–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wong PC, Kitsantas P.A review of maternal mortality and quality of care in the USA. J Matern Fetal Neonatal Med 2020; 33(19): 3355–3367. [DOI] [PubMed] [Google Scholar]
- 57.Heard-Garris NJ, Cale M, Camaj L, et al. Transmitting trauma: a systematic review of vicarious racism and child health. Soc Sci Med 2018; 199: 230–240. [DOI] [PubMed] [Google Scholar]
- 58.Gee GC, Walsemann KM, Brondolo E.A life course perspective on how racism may be related to health inequities. Am J Public Health 2012; 102(5): 967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.LaVeist TA, Thorpe RJ, Jr, Pierre G, et al. The relationships among vigilant coping style, race, and depression. J Soc Issues 2014; 70(2): 241–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Helmreich I, Kunzler A, Chmitorz A, et al. Psychological interventions for resilience enhancement in adults. Cochrane Database Syst Rev 2017; 2017(2): CD012527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zautra AJ, Davis MC, Reich JW, et al. Phone-based interventions with automated mindfulness and mastery messages improve the daily functioning for depressed middle-aged community residents. J Psychother Integr 2012; 22(3): 206–228. [Google Scholar]
- 62.Loughnan SA, Wallace M, Joubert AE, et al. A systematic review of psychological treatments for clinical anxiety during the perinatal period. Arch Womens Ment Health 2018; 21(5): 481–490. [DOI] [PubMed] [Google Scholar]
- 63.Dimidjian S, Goodman SH, Sherwood NE, et al. A pragmatic randomized clinical trial of behavioral activation for depressed pregnant women. J Consult Clin Psychol 2017; 85(1): 26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sockol LE.A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J Affect Disord 2015; 177: 7–21. [DOI] [PubMed] [Google Scholar]
- 65.Sockol LE.A systematic review and meta-analysis of interpersonal psychotherapy for perinatal women. J Affect Disord 2018; 232: 316–328. [DOI] [PubMed] [Google Scholar]
- 66.Kleiber BV, Felder JN, Ashby B, et al. Treating depression among adolescent perinatal women with a dialectical behavior therapy–informed skills group. Cogn Behav Pract 2017; 24(4): 416–427. [Google Scholar]
- 67.American College of Obstetricians and Gynecologists. Caring for patients who have experienced trauma: ACOG committee opinion, number 825. Obstet Gynecol 2021; 137(1): e94–e99. [DOI] [PubMed] [Google Scholar]
- 68.Choi KR, Records K, Low LK, et al. Promotion of maternal–infant mental health and trauma-informed care during the COVID-19 pandemic. J Obstet Gynecol Neonatal Nurs 2020; 49(5): 409–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.MacKinnon DP, Krull JL, Lockwood CM.Equivalence of the mediation, confounding and suppression effect. Prev Sci 2000; 1(4): 173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fiedler K, Schott M, Meiser T.What mediation analysis can (not) do. J Exp Soc Psychol 2011; 47(6): 1231–1236. [Google Scholar]
- 71.Benedict C, Hahn AL, Diefenbach MA, et al. Recruitment via social media: advantages and potential biases. Digit Health. Epub ahead of print 6 August 2019. DOI: 10.1177/2055207619867223. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455065211042190 for Postpartum stress and protective factors in women who gave birth in the United States during the COVID-19 pandemic by Elizabeth Mollard, Kevin Kupzyk and Tiffany Moore in Women’s Health