Abstract
Background
Lesbian, gay and bisexual adults are more likely than heterosexual adults to experience worse health outcomes. Despite increasing public health interest in the importance of maintaining a healthy body weight, no study has considered sexual orientation identity (SOI) and unhealthy BMI categories among adults in the UK population.
Methods
Individual participant data meta-analysis using pooled data from population health surveys reporting on 93 429 adults with data on SOI, BMI and study covariates.
Results
Adjusting for covariates and allowing for between-study variation, women identifying as lesbian (OR = 1.41, 95% CI: 1.16, 1.72) or bisexual (OR = 1.24, 95% CI: 1.03, 1.48) were at increased risk of overweight/obesity compared to heterosexual women, but men identifying as gay were at decreased risk (OR = 0.72, 95% CI: 0.61, 0.85) compared to heterosexual men. Increased risk of being underweight was seen for women identifying as ‘other’ (OR = 1.95, 95% CI: 1.07, 3.56), and men identifying as gay (OR = 3.12, 95% CI: 1.83, 5.38), bisexual (OR = 2.30, 95% CI: 1.17, 4.52), ‘other’ (OR = 3.95, 95% CI: 1.85, 8.42).
Conclusions
The emerging picture of health disparities in this population, along with well documented discrimination, indicate that sexual orientation should be considered as a social determinant of health.
Keywords: body mass index, obesity, sexual orientation, social determinants, underweight
Introduction
Overweight and obesity are strong risk factors for a number of health-damaging conditions including coronary heart disease, stroke, cancer and early mortality.1–4 Moreover there is a growing evidence base demonstrating that underweight is also linked to excess mortality.3,5 Disparities in unhealthy weight then place those with higher prevalence of unhealthy weight at higher risk of loss of healthy years lived6 and reduced life expectancy estimates.7
Several subgroups of the population have been identified as having increased risk for overweight and obesity, and policy makers and clinicians have used this evidence to design public health interventions and tailored advice.8 For example, National Institute for Health and Care Excellence (NICE) guidelines for obesity identification and management explicitly mention ethnicity and lower socioeconomic status as special groups for targeted interventions.9 For sexual minority groups in the UK, there has been a very limited evidence base on which to develop similar interventions.
Until 2008, sexual orientation identity (SOI) was not recorded in UK population health surveys, thus no data from population health surveys was available.10,11 This lack of data has serious implications for health disparities for adults who do not identify as heterosexual and has meant that until recently the inequalities affecting lesbian, gay and bisexual (LGB) populations have been hard to analyse at scale through routine datasets.12,13
International research has found that sexual minority women are more likely to have an unhealthy body weight (obese or overweight) than heterosexual women,14–16 with lesbian identity being associated with greatest levels of obesity.17 This association has been found in young,18 adult17 and older lesbian/bisexual women,19 is found within ethnic minority subgroups20,21 and is sustained over the life course.22,23
Some studies find decreased risk of overweight or obesity in sexual minority males17,19,20,24,25 and across the life span,26 some report increased risk when comparing bisexual and heterosexual males,27 and others no association,28,29 but with few population representative samples and considerable heterogeneity in methods across studies, and wide variation in recording sexual identity, there is no consensus of the scale of the risk.
Many studies that look at unhealthy weight in sexual minorities do not include underweight as a category30 or exclude underweight as a separate variable in their analysis by combining it with the healthy/normal weight category,31 often due to small numbers of respondents,32,33 viewing the results as merely showing a reduced prevalence of overweight/obesity. One study that did analyse underweight separately found gay adolescents to be more likely to be underweight than heterosexual adolescents,28 but this study did not include sexual minority adult males. In another study, Laska et al.34 found that bisexual college students were more likely to be underweight than heterosexual college students. By analysing data from only college students in a state-based study in the USA this study has limited generalizability beyond that context.
The aim of our study was to evaluate the association in UK available population level data between SOI, specifically identifying as lesbian, gay, bisexual or ‘other’ (LGBO), and unhealthy body mass index (BMI) defined as either underweight or overweight and obese. This was achieved by pooling individual participant data from 12 studies.12 Additionally, as observed in previous research,31,34,35 we evaluated whether associations differed for men and women.
Method
Design and setting
Participants were drawn from 12 datasets from five British cohort or cross-sectional health survey studies in which sexual orientation was measured consistently. These were the British Cohort Study (BCS70, 2012),36 Health Survey for England (annual waves 2011–13),37 National Survey of Sexual Attitudes and Lifestyles (Natsal-3, undertaken 2010–12),38 Scottish Health Survey (annual waves 2008–13),39 and Understanding Society (2011/12 wave).40 Studies were identified by searching the UK Data Service (search terms ‘sexual orientation’, ‘gay’, ‘lesbian’, ‘bisexual’, ‘sexuality’) and the published literature. Data were collected using either home visit interviews, self-completion questionnaires, telephone interviews, web surveys or a combination of methods. Details including sampling designs, and inclusion/exclusion criteria for each dataset are available from the UK Data Archive.41 Our study population comprised adults with available data on SOI, BMI and covariates. Data were analysed in 2017.
Participants and materials
For all included datasets, participants were recruited through random or stratified random sampling of their target population. Full details of sampling for Understanding Society are available (https://www.understandingsociety.ac.uk) and for the other surveys, they are available on the UK Data Service website (www.ukdataservice.ac.uk).
Sexual orientation identity
SOI was recorded in self-completion questionnaires in all included studies using standardized wording recommended by the Office of National Statistics (ONS).42Supplementary Table S1 shows the proportion of participants who refused to answer this question, who were excluded from our study.
Body mass index
The body mass index (BMI) is body weight in kilograms divided by the square of participants’ height in metres.43 Heights and weights were measured during nurse visits, with self-reports used for British Cohort Study and Natsal-3 participants and 49% of included Understanding Society participants. BMI values were converted into categories defined by the World Health Organization.44
Covariates
Covariates were selected on the basis that they are known to be associated with SOI and with BMI (i.e. are potential confounding factors). Covariates were harmonized across studies to ensure comparability: age, sex (male or female), ethnic group (White versus ethnic minority), educational attainment (a 5-point scale ranging from ‘none’ to university degree), smoking status (current smoker versus non-smoker), longstanding illness/disability (yes or no) and married or cohabiting (yes or no).
Statistical analysis
Bivariate associations between SOI categories, BMI categories and covariates were first evaluated using t-tests and chi-square statistics. We used an α of 0.05 for all statistical tests. For the main analysis, individual participant data (IPD) meta-analysis with logistic regression was used to evaluate the associations between SOI categories and unhealthy BMI categories (underweight, or overweight/obese), adjusting for covariates. IPD meta-analysis enables more flexible and potentially more powerful statistical analyses than are possible with aggregate data. Unlike most meta-analyses, they do not rely on aggregate data extracted from journal publications. Rather, the original data on each individual participant are sought from each eligible study. In this case each eligible study is one of several health surveys that collected data on SOI and BMI. These original data are then used to calculate summary statistics for each study before pooling these estimates, accounting for heterogeneity between studies.45–48 A key benefit of IPD meta-analysis is that it may allow the estimation of associations for smaller subgroups (such as individuals identifying as LGBO) for which the original studies were underpowered.
We used data from studies conducted over a range of years and with slightly different UK geographic foci, and so it was reasonable to assume there might be some heterogeneity in true effect sizes across studies, even once other factors were adjusted for. In conducting our meta-analyses we therefore assumed a random effects model (assumes the true effects for individual studies are normally distributed about some average effect). The study-specific odds ratios and their standard errors are pooled to produce an estimate of the average effect size for the studies. We used the Paule–Mandel method to estimate between-study variance.49
In preliminary analyses, we found evidence that effects differed significantly for men and women, leading us to separate them for the main analysis (P value for interaction < 0.01). In sensitivity analyses, we repeated results after excluding each individual study separately, to evaluate the impact of individual studies on the findings. We also checked whether results differed materially when using the alternative approach to IPD meta-analysis, where all data are analysed simultaneously with a random effect for study of origin. To evaluate the impact of survey design features, we repeated models using Understanding Society and Natsal-3 (the largest contributing studies and with complex survey design) before and after adjustment using sampling weights. All analyses were conducted using Stata version 14.0 (StataCorp. 2015, College Station, TX).
Ethical approval
For all of the original studies used, ethical approval was provided by a university or local research ethics committee (the UK Data Service website hosts details for each study).
Results
Univariate analyses
There were 93 429 adults in the analytic sample (Table 1), with 1095 (1.2%) identifying as lesbian/gay, 873 (0.9%) as bisexual and 675 (0.7%) as ‘other’. Compared to those with a healthy BMI, those with an underweight BMI were significantly younger (median age 27 versus 42 years), comprised a smaller proportion of men (31.5 versus 38.3%), more ethnic minorities (17.9 versus 9.9%), a higher proportion of smokers (37.6 versus 26.0%), and a smaller proportion who were married/cohabiting (32.6 versus 58.4%). Compared to those with a healthy BMI, those with an overweight or obese BMI were significantly older (median age 48 versus 42 years), comprised a larger proportion of men (48.6 versus 38.3%), more longstanding illness/disability (42.4 versus 28.9%) and a higher proportion who were married/cohabiting (68.7 versus 58.4%).
Table 1.
Characteristics of study variables (unweighted) comparing underweight and overweight or obese with healthy body mass index (BMI) categories
| Healthy BMI | Underweight BMI | Overweight/Obese BMI | Total (n = 93 429) | |||
|---|---|---|---|---|---|---|
| (n = 34 244) | (n = 1634) | P | (n = 57 551) | P | ||
| Age (25/50/75th percentile) | 28/42/54 | 19/27/42 | <0.001 | 39/48/63 | <0.001 | 34/44/60 |
| Male (%) | 38.3 | 31.5 | <0.001 | 48.6 | <0.001 | 44.5 |
| Lesbian/Gay identity (%) | 1.3 | 2.0 | 0.02 | 1.1 | <0.001 | 1.2 |
| Bisexual identity (%) | 1.0 | 1.6 | 0.03 | 0.9 | 0.008 | 0.9 |
| Other identity (%) | 0.6 | 1.3 | 0.001 | 0.8 | 0.001 | 0.7 |
| Ethnic minority (%) | 9.9 | 17.9 | <0.001 | 6.7 | <0.001 | 8.1 |
| Degree level education (%) | 30.0 | 20.6 | <0.001 | 23.9 | <0.001 | 26.1 |
| Smoker (%) | 26.0 | 37.6 | <0.001 | 20.4 | <0.001 | 22.7 |
| Longstanding illness/disability (%) | 28.9 | 31.3 | 0.03 | 42.4 | <0.001 | 37.3 |
| Married/cohabiting (%) | 57.6 | 32.0 | <0.001 | 68.1 | <0.001 | 63.6 |
Notes: Underweight BMI is defined as a BMI value <18.5 kg/m2. Healthy BMI is defined as a BMI value in the range 18.5–24.99 kg/m2. Overweight BMI is defined as a BMI value in the range 25–29.99 kg/m2. Obese BMI is defined as a BMI value ≥30 kg/m2. P values are for comparisons of each BMI category separately with the healthy BMI category, and are estimated from chi-square tests. The P values for difference in age were calculated using t-tests.
Compared to their heterosexual counterparts, lesbian, gay and bisexual men and women were younger, while men and women identifying as ‘other’ were significantly older (Table 2). More lesbian women and gay men were educated to degree level than heterosexual women and men, while fewer were ethnic minorities. In contrast, a greater proportion of men and women identifying as bisexual or ‘other’ were ethnic minority when compared to heterosexual men and women. In general, fewer heterosexual men and women were smokers, while more were married or cohabitating than men and women identifying as lesbian, gay, bisexual or ‘other’.
Table 2.
Characteristics of participants identified as lesbian/gay, bisexual and ‘other’ compared to heterosexuals.
| Women | Heterosexual | Lesbian | Bisexual | Other | |||
|---|---|---|---|---|---|---|---|
| (n = 50 463) | (n = 452) | P | (n = 530) | P | (n = 398) | P | |
| Underweight BMI (%) | 2.1 | 2.4 | 0.67 | 3.0 | 0.17 | 3.0 | 0.023 |
| Overweight or obese BMI (%) | 57.0 | 59.3 | 0.34 | 54.2 | 0.18 | 65.8 | <0.001 |
| Age (25/50/75 percentile) | 34/44/59 | 28/40/46 | <0.001 | 23/30/42 | <0.001 | 39/49/63 | <0.001 |
| Ethnic minority (%) | 8.0 | 4.7 | 0.01 | 11.5 | 0.003 | 19.6 | <0.001 |
| Degree level education (%) | 25.6 | 39.4 | <0.001 | 27.4 | 0.34 | 10.1 | <0.001 |
| Smoker (%) | 21.7 | 33.2 | <0.001 | 34.2 | <0.001 | 26.4 | 0.03 |
| Longstanding illness/disability (%) | 37.9 | 40.3 | 0.30 | 41.5 | 0.09 | 44.2 | 0.01 |
| Married/cohabiting (%) | 62.1 | 54.7 | 0.001 | 44.3 | <0.001 | 58.0 | 0.09 |
| Men | Heterosexual | Gay | Bisexual | Other | |||
| (n = 40 323) | (n = 643) | P | (n = 343) | P | (n = 277) | P | |
| Underweight BMI (%) | 1.2 | 3.4 | <0.001 | 2.9 | 0.003 | 3.3 | 0.002 |
| Overweight or obese BMI (%) | 67.5 | 52.4 | <0.001 | 60.4 | 0.005 | 67.9 | 0.90 |
| Age (25/50/75th percentile) | 35/45/61 | 29/42/48 | <0.001 | 29/42/58 | <0.001 | 37/55/67 | <0.001 |
| Ethnic minority (%) | 8.0 | 4.7 | 0.002 | 13.7 | <0.001 | 18.4 | <0.001 |
| Degree level education (%) | 26.6 | 39.5 | <0.001 | 27.1 | 0.82 | 17.3 | 0.001 |
| Smoker (%) | 23.5 | 31.4 | <0.001 | 30.6 | 0.002 | 26.4 | 0.26 |
| Longstanding illness/disability (%) | 36.2 | 39.5 | 0.08 | 44.0 | 0.003 | 44.8 | 0.003 |
| Married/cohabiting (%) | 68.3 | 40.6 | <0.001 | 46.9 | <0.001 | 53.4 | <0.001 |
Notes: Underweight BMI is defined as a BMI value <18.5 kg/m2. Overweight BMI is defined as a BMI value in the range 25–29.99 kg/m2. Obese BMI is defined as a BMI value ≥30 kg/m2. P values are for comparisons of each sexual orientation identity separately with Heterosexual identity, and are estimated from chi-square tests. The P values for difference in age were calculated using t-tests.
Characteristics of participants across each study separately are provided in Supplementary Table S1, which additionally shows the individual sample sizes contributing to our study.
Associations between BMI and sexual orientation identities
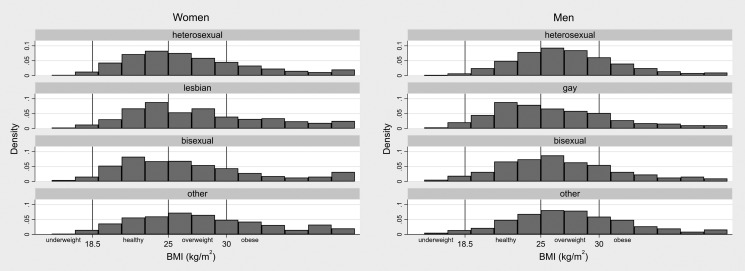
Histograms showing the distribution of BMI for women and men of each SOI category are shown in Fig. 1. The results of the main analyses looking at associations between unhealthy BMI categories and sexual orientation identities are shown in Table 3. Forest plots showing the pooling of results from individual studies are provided in the Supplementary material.
Fig. 1.
(Histogram). Unweighted distribution of BMI by gender and sexual orientation identity. Note: Bin-width equal to 2 kg/m2. Those with BMI < 15 kg/m2 are grouped in the first bin (15–17). Those with BMI > 41 kg/m2 are grouped in the final bin (39–41).
Table 3.
Odds ratios (95% confidence intervals) for underweight and overweight/obese BMI for women and men
| Underweight BMI | Overweight/Obese BMI | |||||
|---|---|---|---|---|---|---|
| % (n) | OR (95% CI) | % (n) | OR (95% CI) | |||
| Minimally adjusteda | Additionally adjustedb | Minimally adjusteda | Additionally adjustedb | |||
| Women | ||||||
| Heterosexual (n = 50 463) | 2.1 (1080) | (Reference) | (Reference) | 57.0 (28 783) | (Reference) | (Reference) |
| Lesbian (n = 452) | 2.4 (11) | 1.39 (0.75, 2.60) | 1.29 (0.69, 2.40) | 59.3 (268) | 1.36 (1.12, 1.65) | 1.41 (1.16, 1.72) |
| Bisexual (n = 530) | 3.0 (16) | 1.54 (0.75, 3.18) | 1.22 (0.63, 2.39) | 54.2 (287) | 1.26 (1.05, 1.50) | 1.24 (1.03, 1.48) |
| Other (n = 398) | 3.0 (12) | 2.45 (1.35, 4.43) | 1.95 (1.07, 3.56) | 65.8 (262) | 1.38 (1.05, 1.82) | 1.25 (0.96, 1.62) |
| Men | ||||||
| Heterosexual (n = 40 323) | 1.2 (474) | (Reference) | (Reference) | 67.5 (27 219) | (Reference) | (Reference) |
| Gay (n = 643) | 3.4 (22) | 3.27 (2.07, 5.15) | 3.12 (1.83, 5.32) | 52.4 (337) | 0.64 (0.54, 0.75) | 0.72 (0.61, 0.85) |
| Bisexual (n = 343) | 2.9 (10) | 3.07 (1.58, 5.98) | 2.30 (1.17, 4.52) | 60.3 (207) | 0.82 (0.65, 1.03) | 0.92 (0.73, 1.17) |
| Other (n = 277) | 3.2 (9) | 4.92 (2.38, 10.16) | 3.95 (1.85, 8.42) | 67.9 (188) | 0.86 (0.66, 1.12) | 0.99 (0.76, 1.30) |
Notes: Percentages shown are the percentage of participants of each sexual orientation identity with BMI values categorized as either underweight, or overweight or obese. Underweight BMI is defined as a BMI value < 18.5 kg/m2. Overweight BMI is defined as a BMI value in the range 25–29.99 kg/m2. Obese BMI is defined as a BMI value ≥30 kg/m2. aMinimally adjusted for age. bAdditionally adjusted for ethnic minority status, educational attainment, cigarette smoking, longstanding illness/disability and relationship status.
After adjustments for a range of covariates, women identifying as lesbian were at an increased risk of being overweight or obese (OR = 1.41, 95% CI: 1.16, 1.72) when compared with heterosexual women, as were women identifying as bisexual (OR = 1.24, 95% CI: 1.03, 1.48). Women identifying as ‘other’ were at an increased risk of underweight BMI (OR = 1.95, 95% CI: 1.07, 3.56), but were not at increased or decreased risk of overweight or obese BMI (OR = 1.28, 95% CI: 0.96, 1.62).
Men identifying as gay were significantly more likely than heterosexual men to be underweight (OR = 3.12, 95% CI 1.83, 5.32), as were men identifying as bisexual (OR = 2.30, 95% CI: 1.17, 4.52) and ‘other’ (OR = 3.95, 95% CI: 1.85, 8.42). Men identifying as gay were significantly less likely than heterosexual men to have an overweight or obese BMI (OR = 0.72, 95% CI: 0.61, 0.85). No associations were found between overweight or obese BMI and bisexual (OR = 0.92, 95% CI: 0.73, 1.17) or ‘other’ (OR = 0.99, 95% CI: 0.76, 1.30) identity in men.
These results are reflected in Fig. 1, which shows the distribution of gay men’s BMI skewed towards lower values, while the distributions of men identifying as bisexual or ‘other’ look similar to that of heterosexual men. Similarly, the distributions for women identifying as lesbian or ‘other’ appear to have heavier tails at the higher end of the BMI range, and both have positively shifted means compared to heterosexual and bisexual women. As no significant association was found for overweight/obese BMI in women identifying as ‘other’, these features instead reflect demographic differences between this group and others.
Sensitivity analyses
The smaller number of underweight adults in the pooled data means that effects for underweight BMI were more sensitive to removal of individual studies, and confidence intervals for underweight BMI estimates are wider. In the majority of analyses, no significant between-study heterogeneity was found (see Supplementary Table S2), however, results were similar after excluding individual studies where there was evidence of between-study variation. Running the analyses again while artificially setting the between-study heterogeneity at the upper bound of the I2 confidence intervals reported in Supplementary Table S2 resulted in associations between underweight BMI and identifying as bisexual in men and ‘other’ in both men and women no longer reaching significance. All other significant associations reported in Table 3 remained. Results were similar in the Natsal-3 and Understanding Society cohorts after adjustment for survey design using sampling weights. When the analysis was re-run after removing respondents with only self-reported BMI, the results were similar to the results reported above, with the following exceptions: the association between bisexual women and overweight BMI no longer reached significance (OR 1.15, 95% CI: 0.91–1.44) and the association between women identifying as ‘other’ and overweight BMI now reached significance (OR 1.48, 95% CI: 1.12–1.95). Due to very low numbers of underweight men identifying as bisexual or ‘other’, the analysis could not be re-run for these groups when self-reported weight data were removed.
Discussion
Main finding of this study
Our study is an important first look at the descriptive epidemiology of sexual orientation in relation to BMI categories in the UK. The results show that women who identify as lesbian or bisexual (versus heterosexual) are at increased risk of overweight or obesity, and that men who identify as gay are at decreased risk of overweight or obesity. They also indicate that women identifying as ‘other’, and men identifying as gay, bisexual or ‘other’ were at increased risk of being underweight. The associations held after adjustment for a range of covariates and were robust to several sensitivity analyses.
What is already known on this topic
Our findings are comparable with data from the USA showing that lesbians and bisexual women tend to have a higher BMI than heterosexual women14,34 and gay men are more likely to have a lower BMI than heterosexual men.20 The differential effect of gender is an important consideration when considering health outcomes such as unhealthy weight in sexual minorities.23 A possible mechanism for the association of sexual orientation and BMI may be that sexual minority groups are exposed to psychosocial stressors,50 which may influence their health behaviours such as diet or physical activity,51–53 or alcohol consumption10 indicated in weight gain54 and linked to increased risk of chronic health conditions such as diabetes24 and cardiovascular disease.16
What this study adds
The study is the first to pool population health survey data in order to consider the association between SOI and BMI in a UK population. The large LGBO sample size is a key strength of this study, allowing us to consider lesbian, gay, bisexual and ‘other’ groups separately as well as consider gender differences. Our results show that these associations can be found at the population level in the UK from representative surveys.
The large LGBO sample size also allowed us to consider the underweight category, which is frequently too small to consider in single studies and has not been included separately in previous population studies.20,55 Combining underweight and normal weight, commonly done in sexual minority studies,32,33,56 may give the impression gay and bisexual men are healthy weight. Our study, by analysing underweight separately, showed that gay men are at higher risk of being underweight.
Weight issues are inherently connected to social normative concepts of identity and desire and there are limited research that explores this in a UK context, however, international research suggests that this is a significant driver of unhealthy weight behaviours in LGB youth.57 Indeed evidence is available that suggests sexual minority male youth are not only more likely to engage in risky weight control behaviours than heterosexual peers and are more influenced by advertising focusing on physical appearance58 but also self-perceive as overweight despite being healthy or even underweight.57 Conversely, research suggests sexual minority women have higher levels of body satisfaction and reject the heteronormative standard of body-size, and self-perceive as being healthy or underweight when overweight/obese.57
The differences in weight found within the subgroups also reiterates that lesbian, gay, bisexual and those who identify as ‘other’ are not one homogenous group; gender differences are important to consider in health outcomes and in healthcare needs. The clear commitment at national and local level to address population-level weight issues provides an opportunity for policy makers and providers to use this research to better understand and address the needs of LGBO people in the UK.
Limitations of this study
One limitation of our study is the cross-sectional nature of the surveys, so we could not consider changes in BMI or whether these associations might persist over the life course, nor their onset. Due to small numbers of respondents, we were not able to consider smaller subgroups of the non-heterosexual participants allowing us to look at the impact of intersectionality on weight in this population.59 Due to the small number of underweight individuals, particularly for men identifying as bisexual and men and women identifying as ‘other’, associations between underweight BMI and SOI for these groups should be interpreted cautiously. We only considered SOI in this study. Defining sexual orientation more widely (identity, behaviour and attraction) might produce different results in our sample.
It is possible that the use of self-reported weight data may have resulted in underestimation of rates of underweight, overweight and obese BMIs.60 Finally, we considered BMI but not other indicators of fat mass and excess weight, issues which apply to any study using BMI are unlikely to differ by sexual orientation and which have been reviewed elsewhere.61 Moreover, BMI is widely used in clinical and research settings to identify adults who may be at increased risk of poor health outcomes including mortality and cancer.3,5
Little detailed information is known about the ‘other’ category, retained by the ONS sexual orientation question62 and analysed in this study; a heterogeneous group, who chose to not identify as heterosexual and differ from heterosexuals on a number of variables63 but may experience health disparities. This group is often omitted from studies or combined with subgroups, losing data on this unique subset of the population. This selection may reflect respondents’ dissatisfaction with the current categories available for SOI62,64 or the lack of questions on gender identity (beyond male/female gender category) currently omitted from all UK health surveys. As it is unclear the make-up of this group, we should be cautious in the conclusions we can draw from these results.
Conclusion
The study clearly demonstrates the link between SOI and unhealthy weight in lesbian and bisexual women and in gay and bisexual men (versus heterosexual). It is important to consider SOI health disparities in public health policy. The importance of developing tailored interventions to address these disparities and of supportive policy change to ensure development and implementation of standards of care for LGBO people are necessitated.
Supplementary Material
Acknowledgements
Our grateful thanks to Gareth Hagger-Johnson for his guidance throughout this article.
Conflict of interest
The authors declare there is no conflict of interest.
Authors’ contributions
JS conceptualized the study. TC carried out the statistical analyses. JS and TC drafted the article. All authors contributed to interpretation of the data and revision of the article and approved the final version.
Funding
The study was supported in part by the Medical Research Council [grant number MR/N013867/1]. The funders had no role in study design, analysis and interpretation of data, writing of the report, or decision to submit the article for publication.
References
- 1.Calle EE, Rodriguez C, Walker-Thurmond Ket al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 2003;348(17):1625–38. [DOI] [PubMed] [Google Scholar]
- 2.Cecchini M, Sassi F, Lauer JAet al. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet 2010;376(9754):1775–84. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Kit BK, Orpana Het al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. J Am Med Assoc 2013;309(1):71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitlock G, Lewington S, Sherliker Pet al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373(9669):1083–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ringbäck Weitoft G, Eliasson M, Rosén M. Underweight, overweight and obesity as risk factors for mortality and hospitalization. Scand J Public Health 2008;36(2):169–76. [DOI] [PubMed] [Google Scholar]
- 6.Grover SA, Kaouache M, Rempel Pet al. Years of life lost and healthy life-years lost from diabetes and cardiovascular disease in overweight and obese people: a modelling study. Lancet Diabetes Endocrinol 2015;3(2):114–22. [DOI] [PubMed] [Google Scholar]
- 7.Jensen MD, Ryan DH, Apovian CMet al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol 2014;63(25 Part B):2985–3023. [DOI] [PubMed] [Google Scholar]
- 8.Swinburn B, Dietz W, Kleinert S. A Lancet Commission on obesity. Lancet 2015;386(10005):1716–7. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Clinical Excellence . Obesity: Identification, Assessment and Management. London: NICE, 2014. [PubMed] [Google Scholar]
- 10.Hagger-Johnson G, Taibjee R, Semlyen Jet al. Sexual orientation identity in relation to smoking history and alcohol use at age 18/19: Cross-Sectional Associations from the Longitudinal Study of Young People in England (LSYPE). BMJ Open 2013;3(8):e002810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Semlyen J, King M, Varney Jet al. Sexual orientation and symptoms of common mental disorder or low wellbeing: combined meta-analysis of 12 UK population health surveys. BMC Psychiatry 2016;16(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Semlyen J. Recording sexual orientation in the UK: pooling data for statistical power. Am J Public Health 2017;107(8):1215–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mayer KH, Bradford JB, Makadon HJet al. Sexual and gender minority health: what we know and what needs to be done. Am J Public Health 2008;98(6):989–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bowen DJ, Balsam KF, Ender SR. A review of obesity issues in sexual minority women. Obesity (Silver Spring) 2008;16(2):221–8. [DOI] [PubMed] [Google Scholar]
- 15.Eliason MJ, Ingraham N, Fogel SCet al. A systematic review of the literature on weight in sexual minority women. Womens Health Issues 2015;25(2):162–75. [DOI] [PubMed] [Google Scholar]
- 16.Farmer GW, Jabson JM, Bucholz KKet al. A population-based study of cardiovascular disease risk in sexual-minority women. Am J Public Health 2013;103(10):1845–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health 2010;100(10):1953–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McElroy JA, Jordan J. Disparate perceptions of weight between sexual minority and heterosexual female college students. LGBT Health. 2014;1(2):122–30. [DOI] [PubMed] [Google Scholar]
- 19.Fredriksen-Goldsen KI, Kim H-J, Barkan SEet al. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health 2013;103(10):1802–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deputy NP, Boehmer U. Weight status and sexual orientation: differences by age and within racial and ethnic subgroups. Am J Public Health 2014;104(1):103–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz-Wise SL, Blood EA, Milliren CEet al. Sexual orientation disparities in BMI among U.S. adolescents and young adults in three race/ethnicity groups. J Obes 2014;2014:537242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hatzenbuehler ML, McLaughlin KA, Slopen N. Sexual orientation disparities in cardiovascular biomarkers among young adults. Am J Prev Med 2013;44(6):612–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jun HJ, Corliss HL, Nichols LPet al. Adult body mass index trajectories and sexual orientation: the Nurses’ Health Study II. Am J Prev Med 2012;42(4):348–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dilley JA, Simmons KW, Boysun MJet al. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific Northwest. Am J Public Health 2010;100(3):460–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deputy NP, Boehmer U. Determinants of body weight among men of different sexual orientation. Prev Med 2010;51(2):129–31. [DOI] [PubMed] [Google Scholar]
- 26.Wang J, Hausermann M, Vounatsou Pet al. Health status, behavior, and care utilization in the Geneva Gay Men’s Health Survey. Prev Med 2007;44(1):70–5. [DOI] [PubMed] [Google Scholar]
- 27.Austin SB, Nelson LA, Birkett MAet al. Eating disorder symptoms and obesity at the intersections of gender, ethnicity, and sexual orientation in US high school students. Am J Public Health 2013;103(2):e16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mereish EH, Poteat VP. Let’s get physical: sexual orientation disparities in physical activity, sports involvement, and obesity among a population-based sample of adolescents. Am J Public Health 2015;105(9):1842–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosario M, Corliss HL, Everett BGet al. Sexual orientation disparities in cancer-related risk behaviors of tobacco, alcohol, sexual behaviors, and diet and physical activity: pooled Youth Risk Behavior Surveys. Am J Public Health 2014;104(2):245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steele LS, Ross LE, Dobinson Cet al. Women’s sexual orientation and health: results from a Canadian population-based survey. Women Health 2009;49(5):353–67. [DOI] [PubMed] [Google Scholar]
- 31.Branstrom R, Hatzenbuehler ML, Pachankis JE. Sexual orientation disparities in physical health: age and gender effects in a population-based study. Soc Psychiatry Psychiatr Epidemiol 2016;51(2):289–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Strutz KL, Herring AH, Halpern CT. Health disparities among young adult sexual minorities in the U.S. Am J Prev Med 2015;48(1):76–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farmer GW, Bucholz KK, Flick LHet al. CVD risk among men participating in the National Health and Nutrition Examination Survey (NHANES) from 2001 to 2010: differences by sexual minority status. J Epidemiol Community Health 2013;67(9):772–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Laska MN, VanKim NA, Erickson DJet al. Disparities in weight and weight behaviors by sexual orientation in college students. Am J Public Health 2015;105(1):111–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blosnich JR, Farmer GW, Lee JGet al. Health inequalities among sexual minority adults: evidence from ten U.S. states, 2010. Am J Prev Med 2014;46(4):337–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elliott J, Shepherd P. Cohort profile: 1970 British Birth Cohort (BCS70). Int J Epidemiol 2006;35(4):836–43. [DOI] [PubMed] [Google Scholar]
- 37.NatCen Social Research . University College London. Department of Epidemiology and Public Health. Health Survey for England, 2011–2013. UK Data Service, 2013.
- 38.NatCen Social Research . London School of Hygiene and Tropical Medicine. Centre for Sexual and Reproductive Health Research. National Survey of Sexual Attitudes and Lifestyles, 2010–2012. 2nd edn: UK Data Service, 2017.
- 39.Scottish Centre for Social Research . University College London. Department of Epidemiology and Public Health. Scottish Health Survey, 2008–2013. UK Data Service, 2016.
- 40.NatCen Social Research . University of Essex. Institute for Social and Economic Research. Understanding Society: Waves 1–7, 2009–2016 and Harmonised BHPS: Waves 1–18, 1991–2009. 9th edn: UK Data Service, 2016.
- 41.UK Data Archive . University of Essex. http://www.data-archive.ac.uk/ (10 April 2018, date last accessed).
- 42.Haseldon LJ, Theodore. Measuring sexual identity: a guide for researchers, 2009.
- 43.Keys A, Fidanza F, Karvonen MJet al. Indices of relative weight and obesity. J Chronic Dis 1972;25(6):329–43. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organisation . Body Mass Index. http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (10 April 2018, date last accessed).
- 45.Chalmers I. The Cochrane collaboration: preparing, maintaining, and disseminating systematic reviews of the effects of health care. Ann N Y Acad Sci 1993;703(1):156–65. [DOI] [PubMed] [Google Scholar]
- 46.Stewart LA. Practical methodology of meta‐analyses (overviews) using updated individual patient data. Stat Med 1995;14(19):2057–79. [DOI] [PubMed] [Google Scholar]
- 47.Stewart LA, Tierney JF. To IPD or not to IPD? Advantages and disadvantages of systematic reviews using individual patient data. Eval Health Prof 2002;25(1):76–97. [DOI] [PubMed] [Google Scholar]
- 48.Higgins JP, Thompson SG, Deeks JJet al. Measuring inconsistency in meta-analyses. Br Med J 2003;327(7414):557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 2007;28(2):105–14. [DOI] [PubMed] [Google Scholar]
- 50.Meyer I. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003;129(5):674–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lick DJ, Durso LE, Johnson KL. Minority stress and physical health among sexual minorities. Perspect Psychol Sci 2013;8(5):521–48. [DOI] [PubMed] [Google Scholar]
- 52.Mereish EH. The weight of discrimination: the relationship between heterosexist discrimination and obesity among lesbian women. Psychol Sex Orientat Gend Divers 2014;1(4):356. [Google Scholar]
- 53.Boehmer U, Bowen DJ. Examining factors linked to overweight and obesity in women of different sexual orientations. Prev Med 2009;48(4):357–61. [DOI] [PubMed] [Google Scholar]
- 54.Arif AA, Rohrer JE. Patterns of alcohol drinking and its association with obesity: data from the Third National Health and Nutrition Examination Survey, 1988–1994. BMC Public Health 2005;5(1):126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mason TB, Lewis RJ. Minority stress, depression, relationship quality, and alcohol use: associations with overweight and obesity among partnered young adult lesbians. LGBT Health 2015;2(4):333–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.VanKim NA, Porta CM, Eisenberg MEet al. Lesbian, gay and bisexual college student perspectives on disparities in weight-related behaviours and body image: a qualitative analysis. J Clin Nurs 2016;25(23–24):3676–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hadland SE, Austin SB, Goodenow CSet al. Weight misperception and unhealthy weight control behaviors among sexual minorities in the general adolescent population. J Adolesc Health 2014;54(3):296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gigi I, Bachner-Melman R, Lev-Ari L. The association between sexual orientation, susceptibility to social messages and disordered eating in men. Appetite 2016;99:25–33. [DOI] [PubMed] [Google Scholar]
- 59.Hsieh N, Ruther M. Sexual minority health and health risk factors: intersection effects of gender, race, and sexual identity. Am J Prev Med 2016;50:746–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Elgar FJ, Stewart JM. Validity of self-report screening for overweight and obesity. Evidence from the Canadian Community Health Survey. Can J Public Health 2008;99(5):423–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nuttall F. Body mass index: obesity, BMI, and health: a critical review. Nutr Today 2015;50(3):117–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ellison G, Gunstone B. Sexual Orientation Explored: A Study of Identity, Attraction, Behaviour and Attitudes in 2009. Manchester: Equality and Human Rights Commission Manchester, 2009. [Google Scholar]
- 63.Eliason MJ, Radix A, McElroy JAet al. The ‘Something Else’ of sexual orientation: measuring sexual identities of older lesbian and bisexual women using National Health Interview Survey Questions. Womens Health Issues 2016;26(Suppl 1):S71–80. [DOI] [PubMed] [Google Scholar]
- 64.Eliason MJ, Streed CG Jr. Choosing ‘Something Else’ as a sexual identity: evaluating response options on the National Health Interview Survey. LGBT Health 2017;4(5):376–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.