Abstract
Non-alcoholic fatty liver disease (NAFLD) affects almost a quarter of the world’s population and is the most common cause of chronic liver disease in children and adolescents. The recent proposal to replace the terminology of NAFLD with metabolic-associated fatty liver disease (MAFLD) aims to reflect the pathophysiology and risk factors for this disease. Importantly, the risk factors for MAFLD may be prenatal, such as genetic factors, or postnatal, such as obesity and insulin resistance. MAFLD is increasingly recognized in children and adolescents. Early diagnosis and identification of high-risk individuals with type 2 diabetes mellitus and metabolic syndrome is important. The diagnosis and management of MAFLD in children and adolescents should follow international clinical guidelines, such as those from the American Diabetes Association (ADA) and the International Society for Pediatric and Adolescent Diabetes (ISPAD). Current guidelines recommend lifestyle and dietary modifications, exercise, screening, individualized patient assessment, and multidisciplinary patient management. This review assesses the revised terminology and discusses the epidemiology, risk factors, pathophysiology, diagnosis, and prevention of MAFLD in children and adolescents worldwide and in Mexico, and also considers the implications for public health.
Keywords: Adolescent Health, Child Nutrition Disorders, Diabetes Mellitus, Metabolic Syndrome, Non-alcoholic Fatty Liver Disease, Pediatric Obesity
Background
Non-alcoholic fatty liver disease (NAFLD) affects almost a quarter of the world’s population and is the most common cause of chronic liver disease (CLD) in children and adolescents [1]. The recent proposal to replace the terminology of NAFLD with metabolic-associated fatty liver disease (MAFLD) aims to reflect the pathophysiology and risk factors for this disease [2,3]. Importantly, the risk factors for MAFLD development in children and adolescents may be prenatal, such as genetic factors, or postnatal, such as obesity and insulin resistance (IR) [4]. Early diagnosis and identification of high-risk individuals with type 2 diabetes mellitus (T2DM) and metabolic syndrome (MetS) is highly recommended [5,6].
The NAFLD diagnostic criteria traditionally includes evidence of hepatic steatosis by imaging techniques, blood biomarkers/scores, or liver histology, as well as the absence of significant alcohol consumption or any other secondary cause of liver steatosis (eg, virus, drugs, autoimmune). Thus, MAFLD nomenclature has been developed to better describe the pathophysiology and risk factors involved in either the establishment or progression of disease. This amendment in terminology is intended for raising awareness of MAFLD and of the dysmetabolic/obesity epidemic, while positive criteria might reduce selection bias in the achievement of positive results for targeted treatment of MAFLD [2]. This review assesses the revised terminology and discusses the epidemiology, risk factors, pathophysiology, diagnosis, and prevention of MAFLD in children and adolescents worldwide and in Mexico, and the considers implications for public health.
Epidemiology of MAFLD in Adults Worldwide and in Mexico
In adults, the global prevalence of MAFLD and steatohepatitis has been continuously increasing, from 15% and 33% in 2005, to 25% and 59.1% in 2010 [1]. As a continuum, MAFLD/steatohepatitis are considered the second most common indication for liver transplantation in the United States (US) only after chronic hepatitis C. The highest rates were reported in South America (31%), the Middle East (32%), Asia (27%), USA (24%), and Europe (23%), whereas the lowest rates were reported in Africa (14%) [7,8]. In the USA, the prevalence of MAFLD and steatohepatitis were 21–24.1% and 3–4% in the general population, and the prevalence of MAFLD and the risk of NASH associated with IR were higher in Hispanic Americans [9,10]. Moreover, when the prevalence of MAFLD in individuals of Hispanic origin was 29%, individuals from Mexican origin had a higher prevalence of MAFLD (33%) than individuals of Dominican (16%) or Puerto Rican origin (18%) [11]. The prevalence of MAFLD comorbidities such as MS and T2DM were the highest in the USA, Mexico, Puerto Rico, Costa Rica, Chile, Venezuela, and Guyana in a review including 356 reports from 2000 to 2013 [12].
Epidemiology of MAFLD in Children and Adolescents Worldwide and in Mexico
MAFLD has become the most common cause of CLD in children and adolescents, and patients with childhood-onset of MAFLD had higher risk of progressive disease [13–15]. Globally, the prevalence of MAFLD in children and adolescents has increased from 19.34 million in 1990 to 29.49 million in 2017, representing an annual increase of 1.35% independent of sex, age, and region. However, the greatest increases were observed in North Africa and the Middle East [7]. Further, from 1990 to 2019, the prevalence of MAFLD among obese or overweight children and adolescents was 31.6%, exceeding the global estimations (26.9%) [15], while in the USA, 24.2% of adolescents had some degree of hepatic steatosis and 4.4% had significant fibrosis. Body mass index (BMI), sex (men), ethnicity (Hispanic), and hypertension were worse with higher steatosis severity, while higher BMI and ethnicity (non-Hispanic Black) were associated with significant fibrosis [8]. Finally, in Latin-American children and adolescents, the prevalence of obesity ranges from 9.5% to 20% [16], while 22.7–66.7% of individuals in this group had IR and 45–66.7% had MAFLD [17]. In Mexico, the prevalence of MAFLD was 12.6% in obese or overweight children from 5.5 to 12 years old in 2004 [18]. Up-to-date epidemiological information is needed and protocol design must follow the recommendations international authorities (eg, International Diabetes Federation [IDF]).
Risk Factors for MAFLD: Obesity, Type 2 Diabetes Mellitus, Metabolic Syndrome, and Genetics
Based on the best available evidence, assessing the risk of MAFLD in children and adolescents attending a medical appointment with general practitioners or pediatricians is highly recommended, but local epidemiology must guide screening programs. A recent study assessing patients after a 31-year follow-up demonstrated that the most important risk factors for adult MAFLD were BMI, plasma insulin levels, male sex, genetic background (eg, patatin-like phospholipase domain-containing 3 [PNPLA3] and transmembrane 6 Superfamily Member 2 [TM6SF2] variants), and low birth weight [19].
Environmental risk factors have been dichotomized into prenatal (those present before birth) and postnatal (those occurring after birth) factors. Prenatal risk factors include maternal obesity, MetS during pregnancy, gestational diabetes, and low birth weight. In contrast, postnatal factors include obesity, hyperinsulinemia, IR, and high dietary fructose/carbohydrate/fat consumption [4]. Importantly, maternal pre-pregnancy overweight/obesity was demonstrated to be a modifiable risk factor for pediatric MAFLD, while breastfeeding (≥6 months) was associated with a reduced risk of MAFLD, steatohepatitis, and fibrosis [14]. In Mexico, 33.25% of pregnant women were overweight, and 25% were obese (including 90% and 10% with obesity class 1–2 and class 3, respectively), and 33% had more than the recommended weight gain during pregnancy [20]. Moreover, a national representative survey in Mexico in 2018 showed that the prevalence of exclusive breastfeeding in children under 6 months was 28.3%, and only 29% continued breastfeeding after 2 years [21]. Thus, Mexican children and adolescents are considered a high-risk group due to the increased prevalence of prenatal and postnatal risk factors for MAFLD development and progression.
Obesity
Internationally, the obesity rate in children has tripled from 1960 to in 2010 (5.0% vs 16.9%) [22], and more recently, in 2015, more than 100 million of children and adolescents were obese [23]. In Latin-American children and adolescents, the prevalence of overweight and obesity was 16%, representing one of the highest rates globally [24]. In Mexico, the prevalence of obesity and overweight among children ages 5–11 years was 35.5% in 2018 (3 920 010 children), and it has increased by 8.6% from 1999 (26.9%) to 2018 (35.5%) [25]. Currently, there are no data about the prevalence of MAFLD in Latin-American children and adolescents, but we recommend assessment of risk of developing MAFLD in obese children in this region, therefore, the estimation of MAFLD prevalence might be conducted based on the country’s prevalence of obesity (including high-risk populations such as Mexican, Brazilian, and Hispanic children and adolescents) [26–30]. Importantly, metabolic parameters were similar among obese and overweight Mexican children, and authors suggested that steatohepatitis should be considered as part of the MetS criteria [18].
Importantly, weight gain between the 7th and 13th years of life was related to severity of histological features of adult MAFLD, while the risk of cirrhosis in adulthood was increased by 16% per 1 unit gain in BMI z-score in the same period. Similarly, weight gain during late adolescence can increase the risk of developing adult MAFLD [31].
Although BMI might not be a perfect marker of body composition and body fat [32], in obese children aged 9–13 years with MAFLD, baseline and increased BMI z-score independently predicted incident hepatic steatosis, while a decrease in BMI z-score independently predicted disease remission and improved transaminase level [33]. If available, bioelectrical impedance analysis or magnetic resonance imaging are accurate measures of body composition in obese youth [34]. Alternatively, waist circumference and waist-to-height ratios are suggested to be measured, as they have been demonstrated to be good parameters for adiposity and MAFLD estimation in children and adolescents [35].
Type 2 Diabetes Mellitus
MAFLD and T2DM share several pathogenic risk factors such as increasing rates of obesity and overweight, unhealthy eating habits, and an increasingly sedentary lifestyle, as well as negative impacts on quality of life, healthcare costs, and productivity. In the USA, T2DM prevalence rates for children and adolescents 10–19 years of age were 18/100 000 for non-Hispanic Whites, 46 for Hispanic Whites, 108 for African Americans, and 145 for USA Navajo Indians [36]. In Mexican children 10–14 years old, the incidence of T2DM was 2.9/100 000, while in adolescents 15–19 years old it was 7.69/100 000 adults [37].
It is recommended that T2DM be diagnosed in children and adolescents using the American Diabetes Association (ADA) criteria, while in the absence of symptoms, testing should be confirmed by repeating the test on a different day, and additional diabetes autoantibody testing should be considered (Table 1) [38]. Further, the presence of clinically relevant comorbidities should be assessed at the time of diagnosis, as early onset of microvascular and macrovascular complications can be detected earlier, especially in children [39]. The International Society for Pediatric and Adolescent Diabetes (ISPAD) recommends that pediatric patients with diabetes should be screened for MAFLD/steatohepatitis by measuring alanine aminotransferase (ALT) (22 U/L for girls and 26 U/L for boys) and aspartate aminotransferase (AST) at diagnosis, and annually thereafter. Referral to a gastroenterologist for CLD is recommended if liver enzymes remain elevated at >3 times the upper limit of normal despite weight loss and attainment of glycemic control [40].
Table 1.
Diagnostic criteria for Type 2 Diabetes Mellitus in children.
| Symptoms and/or hyperglycaemia |
| Symptoms of diabetes (polydipsia, polyuria, unexpleined weight loss) + Random plasma glucose >200 mg/dl |
| Fasting plasma glucose ≥126 mg/dl |
| Oral glucose tolerance test (75 gr glucose challenge) |
| Altered HbA1c |
Adapted from American Diabetes Association’s diagnostic criteria recommendations [38]. HbA1c – hemoglobin A1c or glycated hemoglobin.
Metabolic Syndrome
Since 2001, MAFLD has been considered the liver manifestation of MetS [5]. Although IDF recommendations state that MetS should not be diagnosed in children under age 10 years and that adult criteria can be accurate for patients older than 16 years, MetS diagnostic criteria in patients 10–16 years old include central obesity adjusted for age and sex plus at least 2 altered metabolic parameters (Table 2) [41]. In the 3rd National Health and Nutrition Examination Survey (NHANES 1988–1994) in the USA, MetS was the primary driver of MAFLD among non-Hispanic Black patients and Mexican Americans, while the Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) score was not a risk factor associated with steatohepatitis among Latino patients, but it was for non-Latino White patients with steatohepatitis [42]. In 2018, 59% of children and adolescents who had MAFLD also had IR [26]. The prevalence ratio for prediabetes in children and adolescents age 5–18 years (fasting glucose ≥100 mg/dL) for those with obesity was 1.4 and for those with MAFLD it was 26.1 relative to those with healthy weight [43]. Further, 80% of adolescents with biopsy-proven MAFLD had biochemical evidence of IR [44].
Table 2.
Diagnostic criteria for Metabolic Syndrome in children.
| Central obesity: waist circumference >90th percentile adjusted for age and gender |
| Plus at least 2 of the following |
| Systolic blood pressure >130 mmHg or >90th percentile adjusted for age and gender) |
| Diastolic blood pressure >85 mmHg (or >90th percentile adjusted for age and gender) |
| Treatment with antihypertensive medication |
| Triglyceride’s level higher than 150 mg/dl |
| HDL cholesterol lower than 40 mg/dL |
| Fasting plasma glucose >100 mg/dL |
| Known T2DM |
Adapted from International Diabetes Federation’s diagnostic criteria recommendations [41]. HDL – high density level cholesterol; T2DM – Type 2 Diabetes Mellitus.
Genetics
In obese children and adolescents, rs1260326, a single-nucleotide polymorphism (SNP) in the glucokinase regulator (GCKR), was associated with elevated triglycerides, very low-density lipoprotein, and fatty liver, and this latter association was particularly significant in Hispanics. The synergy between PNPLA3 and GCKR SNPs increased the susceptibility to fatty liver in obese children and adolescents [45]. In adolescents, SNPs rs738409 in PNPLA3 (additionally associated with severity of disease [46]), rs1044498 in ENPP1, and rs780094 in GCKR were strongly associated with MAFLD compared with adult controls. It was shown that patients with rs1260326/rs780094 minor alleles had decreased levels of GCKR protein, while rs738409 G/G carriers showed downregulation of the retinol pathway [47]. In Asian Indian adolescents with overweight/obesity, the polymorphisms rs738409 C >G of PNPLA3 and 455 T >C of APOC3 were associated with MAFLD and obesity [48].
Additionally, the I148M protein variant of PNPLA3 programs the amount of fat in liver cells, increases the risk MAFLD development by >50%, and elevates liver damage indexes in Hispanics [49,50]. This variant was significantly associated with elevated ALT levels, decreased HDL cholesterol levels, and lower BMI z-core, and the association with high ALT levels was more significant for lean MAFLD Mexican children, although overweight or obese children were more likely to have higher ALT levels [51]. Furthermore, I148M variant was inversely associated with estimated glomerular filtration rate in children when MAFLD was histologically confirmed [52].
Contrary to observations in adults, the rs641738C >T near Membrane-Bound O-Acyltransferase Domain-Containing 7 (MBOAT7) genetic variant was neither associated with hepatic steatosis after BMI stratification nor with the presence of steatohepatitis or the stage of liver fibrosis in children with biopsy-proven NAFLD [53,54].
Circulating microRNAs are promising diagnostic biomarkers of obesity-associated diseases in childhood, as it was showed that 4 miRNAs were overexpressed in obesity and 2 miRNAs (miR-122 and miR-34a) were overexpressed in children with obesity, MAFLD, and/or IR [55].
Interestingly, obese youth with MAFLD had decreased bacterial alpha-diversity and lower abundance of Bacteroidetes, Prevotella, Gemmiger, and Oscillospira but have a higher Firmicutes-to-Bacteroidetes (F/B) ratio. Further, F/B ratio, Bacteroidetes, Gemmiger, and Oscillospira were associated with increased hepatic fat content in this population. Additive effects were observed for the interactions of the PNPLA3 rs738409 with Gemmiger and Oscillospira [56].
Pathophysiology of MAFLD in Children and Adolescents
The pathogenesis of MAFLD is not yet fully understood, but lipotoxicity (a consequence of excessive dietary intake of carbohydrates and fatty acids [FA]) is projected to be one of the main triggers in a multiple-hit model for liver damage in the different stages of MAFLD spectrum of disease. The overconsumption of these nutrients causes an increase in visceral adipose tissue and in the rate of mobilization of FA toward the liver, along with increased release of proinflammatory cytokines (IL-6, TNF-α, CPR) and decreased release of adiponectin. Therefore, IR is presented at both hepatic and systemic levels [57]. Particularly in the liver, altered lipid metabolism carries increased de novo lipogenesis and transformation of FA into free FA; these later condense in the form of triglyceride droplets and are stored in the liver. High levels of FA lead to over-stimulation of FA oxidation and ROS generation pathways, and in consequence, increased effects of oxidative stress on mitochondria and endoplasmic reticulum physiology. Thus, lipotoxicity triggers the activation of proinflammatory pathways, causing steatohepatitis. In response to all these stimuli, the hepatocytes will begin to activate repair mechanisms, which results in hepatic fibrosis [58]. Once developed, MAFLD in childhood is associated with metabolic and circulatory outcomes, whereas CLD is associated with increased morbidity and mortality rates in adolescents and young adults [13]. Thus, there is an urgent need for qualitative and quantitative understanding of the lipotoxicity and crosstalk in the liver and adipose tissue on the molecular level. Further, clinical implications and degree of impact of the different hits (such as lipotoxicity) in all MAFLD phenotypes, including in children and adolescents, may help prevent and treat progressive disease [59]. Finally, it is important to uncover the pathways underlying the known histological differences among children, adolescents, and adults with MAFLD.
Diagnosis of MAFLD in Children and Adolescents
Despite new MAFLD positive diagnostic criteria in adults aimed to raise disease’s awareness among Mexican physicians and specialists [60], the impact of nomenclature for MAFLD in children and adolescents has not been explored. Recently, an international panel of experts proposed MAFLD diagnostic criteria for pediatric patients [61]. These criteria included histological, imaging (ultrasound), or blood biomarker (eg, ALT) evidence of steatosis, accompanied either by excess adiposity, presence of prediabetes or type 2 diabetes, or evidence of metabolic dysregulation. The latter is defined by 2 or more altered results on standardized biometric parameters for age and sex (including waist circumference, blood pressure, triglycerides, high-density lipoprotein cholesterol levels, fasting glucose, and triglyceride-to-HDL cholesterol ratio), but the cutoff varied according to ethnicity and genetic factors [61]. Research defining the cause and magnitude of the differences found in the biometric parameter cutoffs according to ethnicity, sex, age and genetic background is urgently needed for the enhancement of screening and diagnostic strategies in children and adolescents with MAFLD. In this review, diagnostic pearls in pediatric MAFLD are included in (Table 3).
Table 3.
MAFLD diagnostic pearls.
| Apply MAFLD criteria |
| Search for comorbidities |
| Consider metabolic syndrome |
| Do not use blood biomarkers or ICD alone |
| Perform transient elastography |
| Confirm the diagnosis with liver biopsy |
ICD – International Classification of Diseases coding; MAFLD – Metabolic Associated Fatty Liver Disease.
Although 50% of overweighted and obese children and adolescents also had MAFLD with different components of MetS as comorbid conditions [26], 35% of young patients with fibrosis had normal weight and 78% had normal levels of ALT [8]. Thus, follow-up assessment must be individualized according to the stage of disease.
The prevalence of MAFLD in children and adolescents was higher in studies using ultrasound (27.2%) or fatty liver index (30.1%) than in those using liver biochemical tests (19.1%) [15], while diagnosis based only on blood testing or ICD coding can lead to under-reporting [9]. However, among non-invasive methods (including blood-based biomarker, prediction score, and imaging technique) for staging liver fibrosis in children with MAFLD, transient elastography by FibroScan, Enhanced Liver Fibrosis test, and ultrasound elastography showed consistent accuracy compared with liver biopsy diagnosis, but due to heterogeneity in studies this evidence was not conclusive [63].
In MAFLD, the differences between children and adults on histological features are: 1) adult’s steatosis preferentially affects zone 3, or it may be panacinar, whereas children’s steatosis affects zones 1 and 3; 2) severity of steatosis trends to be higher (moderate-severe) in children, but tends to be mild or moderate in adults; 3) adult patients usually have lobular inflammation, but children usually have portal inflammation; 4) fibrosis in adult patients has been traditionally described as pericellular with strands of collagen surrounding damaged hepatocytes (sometimes called “chicken wire”), and as portal-periportal in children [64].
Although 5–10% of adults with MAFLD are at high risk for developing cirrhosis, only 1–2% of children with MAFLD have increased risk [64]. Nevertheless, adults, children, and adolescents with MAFLD have been associated with increased cardiovascular disease (CVD) risk and subclinical atherosclerosis [65] that has been detected using ultrasound vascular markers [64]. Of note, children and adolescents with MAFLD/steatohepatitis had lower whole-body or lumbar bone mass density z-scores independent of age, sex, race/ethnicity, and BMI than those without MAFLD [66].
Importantly, children under age 10 years with hepatic steatosis have a high prevalence of secondary causes (eg, glycogen storage disease, hepatitis C virus), and these must be considered in patients without traditional risk factors [67]. Further, the dentification of associated risk factors such as obstructive sleep apnea [68] and thyroid function [69] is recommended in children with high risk of or confirmed MAFLD.
Finally, children and adolescents with MAFLD commonly presented neuropsychiatric symptoms and poor quality of life, with no correlation with the degree of hepatic damage. Mentally and intellectually impaired youth appear to have a greater risk for developing MAFLD [70]. In response, a holistic approach of obese children and adolescents should include family support and guided behavior modification, as they may be effective methods of reducing BMI [71].
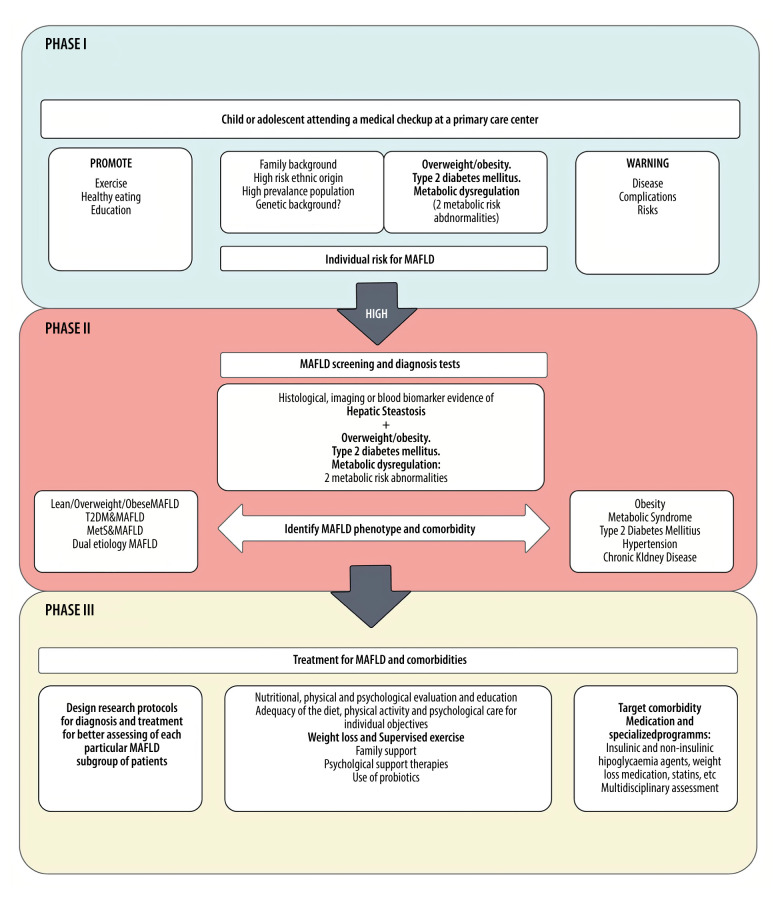
In this review we have proposed a “MAFLD in children and adolescents: risk, diagnosis, and holistic treatment assessment model” composed of 3 phases: individual risk assessment, screening and initial diagnosis, and initial treatment and referral (Figure 1).
Figure 1.
Metabolic-associated fatty liver disease in children and adolescents: risk, diagnosis, and holistic treatment assessment model. Phase I in this context: it is highly recommended that first-contact clinicians or pediatricians caring for children and adolescents in the community assess the individual risk of metabolic-associated fatty liver disease (MAFLD) and highlight activities that help to prevent it. Phase II: if the individual risk for each child/adolescent patient is high (multiple risk factors), referral to a specialist in pediatric hepatology, gastroenterology, or endocrinology, as well as MAFLD screening and diagnostic tests, should not be delayed. Further, if a MAFLD diagnosis is made, MAFLD phenotype and comorbidities must be assessed. Phase III: in this stage, after MAFLD initial assessment, non-pharmacological therapies (nutritional, physical, and psychological approaches) should be introduced based on individual objectives for weight loss and physical activity. If medications are indicated by the severity of liver disease (MAFLD) or comorbidity (eg, obesity, type II diabetes mellitus, hypertension, and chronic kidney disease), specialized programs with multidisciplinary assessment groups are encouraged.
Prevention of MAFLD in Children and Adolescents
Prevention and treatment of MAFLD based on multidisciplinary assessment and management is recommended. The interventions in patient’s behavior by establishing realistic individual objectives might interfere with the perpetuation of the observed effects in the adult population. The comprehensive approach to high risk is recommended in all practice settings (including first-contact physicians or pediatricians, metabolism-specialized clinics, and pediatric liver units), with weight loss management and calculation of appropriate energy intake for age, sex, and activity as the first step in MAFLD prevention and care (Table 4). Further guidance by a registered dietitian is recommended. Non-pharmacological lifestyle interventions were associated with significantly improved levels of BMI, ALT, and AST, and steatosis risk (the latter by 61%) in children and adolescents [72].
Table 4.
MAFLD treatment pearls.
| Education |
| Adequacy of the diet according to the basal metabolic rate |
| Supervised exercise |
| A diet low in free sugar |
| Use of probiotics |
| Weight loss |
| Family support |
| Psychological support therapies |
MAFLD – Metabolic Associated Fatty Liver Disease.
The recommended diet to reduce hepatic steatosis is low in simple carbohydrates (sweets and added sugars), with complete elimination of all fructose and sugar-sweetened beverages, and other similar components of a Western diet for 8 weeks [73]. Additionally, the implementation of ω-3 polyunsaturated FA in the diet of children and adolescents aimed to reduce AST levels in the first 6 months, and ALT levels at 12 months. These nutrients aim to increase the recovery rate of hepatic steatosis by 25% [74]. Thus, nutritional and pharmacological research must assess the importance of maintaining adequate gut-liver axis health in the holistic approach of children and adolescents with MAFLD.
Importantly, supervised exercise training performed by children and adolescents significantly reduced hepatic fat content and the risk and prevalence of MAFLD. Aerobic and resistance training are recommended at vigorous or moderate-to-vigorous intensities, with ≥60 min/session and a frequency of ≥3 sessions/week [75].
Follow-up assessment of children must be within 6 months of treatment initiation. If triglycerides are at normal levels in the follow-up laboratory test, diet and activity recommendations should be continued and reassessment should be programmed annually. In contrast, if TGs are altered (>100–130 mg/dL but <200 mg/d in children 10–19 years old), professionals should intensify diet counseling and physical activity, and perform assessment every 6 months. Further, if TG are >200 mg/dL but <500 mg/dL and lifestyle recommendations have been attempted with no weight loss, consider referral to an intensive weight loss program, or start pharmacological treatment (including statins, metformin, and insulin alone or in combination [40] if 2 additional CVD risk factors are present [76]. Benefits may be achieved from bariatric surgery in advanced steatohepatitis in noncompliant adolescents with moderate/severe obesity and comorbidities [77].
Conclusions
This review has highlighted the epidemiology, risk factors, pathophysiology, diagnosis, and prevention of MAFLD in children and adolescents worldwide and in Mexico. The prevalence of MAFLD in children and adolescents has been increasing and is now the most common form of CLD in this age group. This review has also highlighted the importance of screening children and adolescents for the known risk factors of obesity, T2DM, and MetS [36,38,40]. Evidence-based clinical diagnostic and management guidelines and disease prevention guidelines are required for children and adolescents with MAFLD. Further epidemiological studies from all countries and regions and randomized controlled clinical trials should be undertaken. International organizations, such as the ADA and ISPAD, will have an important role in coordinating and supporting future clinical studies.
Abbreviations
- ADA
American Diabetes Association
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- BMI
body mass index
- CLD
chronic liver disease
- CVD
cardiovascular disease
- FA
fatty acids
- GCKR
glucokinase regulator
- HOMA-IR
Homeostatic Model Assessment for Insulin Resistance
- MAFLD
Metabolic-Associated Fatty Liver Disease
- MBOAT7
Membrane-Bound O-Acyltransferase Domain-Containing 7
- MetS
metabolic syndrome
- NAFLD
nonalcoholic fatty liver disease
- IDF
International Diabetes Federation
- IR
insulin resistance
- ISPAD
International Society for Pediatric and Adolescent Diabetes
- PNPLA3
Patatin-Like Phospholipase Domain-Containing 3
- SNP
single-nucleotide polymorphism
- TM6SF2
Transmembrane 6 Superfamily Member 2
- USA
United States of America
Footnotes
Conflict of interest: None declared
Declaration of Figures Authenticity
All figures submitted have been created by the authors, who confirm the figures are original with no duplication and have not been previously published in whole or in part.
Financial support: This work was partially supported by the Medica Sur Clinic & Foundation
References
- 1.Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 2.Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73(1):202–9. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 3.Méndez-Sánchez N, Díaz-Orozco LE. Editorial: International consensus recommendations to replace the terminology of non-alcoholic fatty liver disease (NAFLD) with metabolic-associated fatty liver disease (MAFLD) Med Sci Monit. 2021;27:e933860. doi: 10.12659/MSM.933860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mann JP, Valenti L, Scorletti E, Byrne CD, Nobili V. Nonalcoholic fatty liver disease in children. Semin Liver Dis. 2018;38(1):1–13. doi: 10.1055/s-0038-1627456. [DOI] [PubMed] [Google Scholar]
- 5.Marchesini G, Brizi M, Bianchi G, et al. Nonalcoholic fatty liver disease: A feature of the metabolic syndrome. Diabetes. 2001;50(8):1844–50. doi: 10.2337/diabetes.50.8.1844. [DOI] [PubMed] [Google Scholar]
- 6.Hagström H, Stål P, Hultcrantz R, Hemmingsson T, Andreasson A. Overweight in late adolescence predicts development of severe liver disease later in life: A 39years follow-up study. J Hepatol. 2016;65(2):363–68. doi: 10.1016/j.jhep.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 7.Zhang X, Wu M, Liu Z, et al. Increasing prevalence of NAFLD/NASH among children, adolescents and young adults from 1990 to 2017: A population-based observational study. BMJ Open. 2021;11(5):e042843. doi: 10.1136/bmjopen-2020-042843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ciardullo S, Monti T, Perseghin G. Prevalence of liver steatosis and fibrosis detected by transient elastography in adolescents in the 2017–2018 National Health and Nutrition Examination Survey. Clin Gastroenterol Hepatol. 2021;19(2):384–390.e1. doi: 10.1016/j.cgh.2020.06.048. [DOI] [PubMed] [Google Scholar]
- 9.Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10(6):330–44. doi: 10.1038/nrgastro.2013.41. [DOI] [PubMed] [Google Scholar]
- 10.Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 11.Fleischman MW, Budoff M, Zeb I, et al. NAFLD prevalence differs among Hispanic subgroups: The multi-ethnic study of atherosclerosis. World J Gastroenterol. 2014;20(17):4987–93. doi: 10.3748/wjg.v20.i17.4987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.López-Velázquez JA, Silva-Vidal KV, Ponciano-Rodríguez G, et al. The prevalence of nonalcoholic fatty liver disease in the Americas. Ann Hepatol. 2014;13(2):166–78. [PubMed] [Google Scholar]
- 13.Castillo-Leon E, Cioffi CE, Vos MB. Perspectives on youth-onset nonalcoholic fatty liver disease. Endocrinol Diabetes Metab. 2020;3(4):e00184. doi: 10.1002/edm2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Querter I, Pauwels NS, De Bruyne R, et al. Maternal and perinatal risk factors for pediatric non-alcoholic fatty liver disease: A systematic review. Clin Gastroenterol Hepatol. 2021 doi: 10.1016/j.cgh.2021.04.014. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Cholongitas E, Pavlopoulou I, Papatheodoridi M, et al. Epidemiology of nonalcoholic fatty liver disease in Europe: A systematic review and meta-analysis. Ann Gastroenterol. 2021;34(3):404–14. doi: 10.20524/aog.2021.0604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corvalán C, Garmendia ML, Jones-Smith J, et al. Nutrition status of children in Latin America. Obes Rev. 2017;18(Suppl 2):7–18. doi: 10.1111/obr.12571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santomauro M, Paoli-Valeri M, Fernández M, et al. [Non-alcoholic fatty liver disease and its association with clinical and biochemical variables in obese children and adolescents: Effect of a one-year intervention on lifestyle]. Endocrinol Nutr. 2012;59(6):346–53. doi: 10.1016/j.endonu.2012.05.002. [in Spanish] [DOI] [PubMed] [Google Scholar]
- 18.Flores J, Gomez R, Rodriguez G, Moran S. P0223 Prevalence of nonalcoholic steatohepatitis (NASH) in mexican children of an elementary school. J Pediatr Gastroenterol Nutr. 2004;39:S143. [Google Scholar]
- 19.Suomela E, Oikonen M, Pitkänen N, et al. Childhood predictors of adult fatty liver. The Cardiovascular Risk in Young Finns Study. J Hepatol. 2016;65(4):784–90. doi: 10.1016/j.jhep.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 20.Cervantes DL, Haro ME, Ayala RI, Haro I, Fausto JA. Prevalence of obesity and weight gain in pregnant women. Aten Fam. 2019;26(2):43–47. [Google Scholar]
- 21.González-Castell LD, Unar-Munguía M, Quezada-Sánchez AD, et al. Breastfeeding and complementary feeding practices in Mexico: results from Ensanut 2018–19. Salud Publica Mex. 2020;62(6):704–13. doi: 10.21149/11567. [DOI] [PubMed] [Google Scholar]
- 22.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee EY, Yoon KH. Epidemic obesity in children and adolescents: Risk factors and prevention. Front Med. 2018;12(6):658–66. doi: 10.1007/s11684-018-0640-1. [DOI] [PubMed] [Google Scholar]
- 24.Garcia-Garcia G. Obesity and overweight populations in Latin America. Lancet Glob Health. 2021. Available from: https://www.thelancet.com/campaigns/kidney/updates/obesity-and-overweight-populations-in-latin-america.
- 25.Shamah-Levy T, Vielma-Orozco E, Heredia-Hernández O, et al. Resultados nacionales. Sociedad Mexicana de Endocrinología Pediátrica A.C. Instituto Nacional de Salud Pública; 2020. Encuesta Nacional de Salud y Nutrición 2018–19. [in Spanish] [Google Scholar]
- 26.Tricò D, Caprio S, Rosaria-Umano G, et al. Metabolic features of nonalcoholic fatty liver (NAFL) in obese adolescents: Findings from a multiethnic cohort. Hepatology. 2018;68(4):1376–90. doi: 10.1002/hep.30035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alisi A, Manco M, Panera N, Nobili V. Association between type two diabetes and non-alcoholic fatty liver disease in youth. Ann Hepatol. 2009;8(Suppl 1):S44–50. [PubMed] [Google Scholar]
- 28.Assunção SNF, Sorte NCAB, Alves CAD, et al. Inflammatory cytokines and non-alcoholic fatty liver disease (NAFLD) in obese children and adolescents. Nutr Hosp. 2018;35(1):78–83. doi: 10.20960/nh.1317. [DOI] [PubMed] [Google Scholar]
- 29.Pierlot R, Cuevas-Romero E, Rodríguez-Antolín J, et al. [Prevalence of metabolic syndrome in American children and adolescents]. TIP Rev Esp Cienc Quim Biol. 2017;20(1):40–49. [in Spanish] [Google Scholar]
- 30.Wittcopp C, Conroy R. Metabolic syndrome in children and adolescents. Pediatr Rev. 2016;37(5):193–202. doi: 10.1542/pir.2014-0095. [DOI] [PubMed] [Google Scholar]
- 31.Zimmermann E, Gamborg M, Holst C, et al. Body mass index in school-aged children and the risk of routinely diagnosed non-alcoholic fatty liver disease in adulthood: A prospective study based on the Copenhagen School Health Records Register. BMJ Open. 2015;5(4):e006998. doi: 10.1136/bmjopen-2014-006998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Javed A, Jumean M, Murad MH, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: A systematic review and meta-analysis. Pediatr Obes. 2015;10(3):234–44. doi: 10.1111/ijpo.242. [DOI] [PubMed] [Google Scholar]
- 33.Lin YC, Chang PF, Liu K, et al. Predictors for incidence and remission of nonalcoholic fatty liver disease in obese children and adolescents. J Formos Med Assoc. 2021 doi: 10.1016/j.jfma.2021.01.004. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 34.Orkin S, Yodoshi T, Romantic E, et al. Body composition measured by bioelectrical impedance analysis is a viable alternative to magnetic resonance imaging in children with nonalcoholic fatty liver disease. JPEN J Parenter Enteral Nutr. 2021 doi: 10.1002/jpen.2113. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mann JP, Goonetilleke R, McKiernan P. Paediatric non-alcoholic fatty liver disease: A practical overview for non-specialists. Arch Dis Child. 2015;100(7):673–77. doi: 10.1136/archdischild-2014-307985. [DOI] [PubMed] [Google Scholar]
- 36.Patterson C, Guariguata L, Dahlquist G, et al. Diabetes in the young – a global view and worldwide estimates of numbers of children with type 1 diabetes. Diabetes Res Clin Pract. 2014;103(2):161–75. doi: 10.1016/j.diabres.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 37.Dirección General de Epidemiología. [cited 2021 Jul 12]. Available from: https://epidemiologia.salud.gob.mx/anuario/html/anuarios.html [in Spanish]
- 38.Children and Adolescents: Standards of medical care in diabetes – 2020. Diabetes Care. 2020;43(Suppl1):S163–82. doi: 10.2337/dc20-S013. [DOI] [PubMed] [Google Scholar]
- 39.Urakami T, Owada M, Kitagawa T. Recent trend toward decrease in the incidence of childhood type 2 diabetes in Tokyo. Diabetes Care. 2006;29(9):2176–77. doi: 10.2337/dc06-1017. [DOI] [PubMed] [Google Scholar]
- 40.Zeitler P, Arslanian S, Fu J, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Type 2 diabetes mellitus in youth. Pediatr Diabetes. 2018;19(Suppl 27):28–46. doi: 10.1111/pedi.12719. [DOI] [PubMed] [Google Scholar]
- 41.Zimmet P, Alberti KG, Kaufman F, et al. The metabolic syndrome in children and adolescents – an IDF consensus report. Pediatr Diabetes. 2007;8(5):299–306. doi: 10.1111/j.1399-5448.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 42.Smits MM, Ioannou GN, Boyko EJ, Utzschneider KM. Non-alcoholic fatty liver disease as an independent manifestation of the metabolic syndrome: Results of a US national survey in three ethnic groups. J Gastroenterol Hepatol. 2013;28(4):664–70. doi: 10.1111/jgh.12106. [DOI] [PubMed] [Google Scholar]
- 43.Sharma V, Coleman S, Nixon J, et al. A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes Rev. 2019;20(10):1341–49. doi: 10.1111/obr.12904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nobili V, Marcellini M, Devito R, et al. NAFLD in children: A prospective clinical-pathological study and effect of lifestyle advice. Hepatology. 2006;44(2):458–65. doi: 10.1002/hep.21262. [DOI] [PubMed] [Google Scholar]
- 45.Santoro N, Zhang CK, Zhao H, et al. Variant in the glucokinase regulatory protein (GCKR) gene is associated with fatty liver in obese children and adolescents. Hepatology. 2012;55(3):781–89. doi: 10.1002/hep.24806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tang S, Zhang J, Mei TT, et al. Association of PNPLA3 rs738409 G/C gene polymorphism with nonalcoholic fatty liver disease in children: A meta-analysis. BMC Med Genet. 2020;21(1):163. doi: 10.1186/s12881-020-01098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hudert CA, Selinski S, Rudolph B, et al. Genetic determinants of steatosis and fibrosis progression in pediatric non-alcoholic fatty liver disease. Liver Int. 2019;39(3):540–56. doi: 10.1111/liv.14006. [DOI] [PubMed] [Google Scholar]
- 48.Jain V, Kumar A, Ahmad N, et al. Genetic polymorphisms associated with obesity and non-alcoholic fatty liver disease in Asian Indian adolescents. J Pediatr Endocrinol Metab. 2019;32(7):749–58. doi: 10.1515/jpem-2018-0543. [DOI] [PubMed] [Google Scholar]
- 49.Nobili V, Alisi A, Valenti L. NAFLD in children: New genes, new diagnostic modalities and new drugs. Nat Rev Gastroenterol Hepatol. 2019;16(9):517–30. doi: 10.1038/s41575-019-0169-z. [DOI] [PubMed] [Google Scholar]
- 50.Li J, Hua W, Ji C, et al. Effect of the patatin-like phospholipase domain containing 3 gene (PNPLA3) I148M polymorphism on the risk and severity of nonalcoholic fatty liver disease and metabolic syndromes: A meta-analysis of pediatric and adolescent individuals. Pediatr Obes. 2020;15(6):e12615. doi: 10.1111/ijpo.12615. [DOI] [PubMed] [Google Scholar]
- 51.Larrieta-Carrasco E, León-Mimila P, Villarreal-Molina T, et al. Association of the I148M/PNPLA3 variant with elevated alanine transaminase levels in normal-weight and overweight/obese Mexican children. Gene. 2013;520(2):185–88. doi: 10.1016/j.gene.2013.03.038. [DOI] [PubMed] [Google Scholar]
- 52.Marzuillo P, Di Sessa A, Guarino S, et al. Nonalcoholic fatty liver disease and eGFR levels could be linked by the PNPLA3 I148M polymorphism in children with obesity. Pediatr Obes. 2019;14(10):e12539. doi: 10.1111/ijpo.12539. [DOI] [PubMed] [Google Scholar]
- 53.Ismaiel A, Dumitrascu DL. Genetic predisposition in metabolic-dysfunction-associated fatty liver disease and cardiovascular outcomes-Systematic review. Eur J Clin Invest. 2020;50(10):e13331. doi: 10.1111/eci.13331. [DOI] [PubMed] [Google Scholar]
- 54.Zusi C, Morandi A, Maguolo A, et al. Association between MBOAT7 rs641738 polymorphism and non-alcoholic fatty liver in overweight or obese children. Nutr Metab Cardiovasc Dis. 2021;31(5):1548–55. doi: 10.1016/j.numecd.2021.01.020. [DOI] [PubMed] [Google Scholar]
- 55.Oses M, Margareto Sanchez J, Portillo MP, et al. Circulating miRNAs as biomarkers of obesity and obesity-associated comorbidities in children and adolescents: A systematic review. Nutrients. 2019;11(12):E2890. doi: 10.3390/nu11122890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Monga Kravetz A, Testerman T, Galuppo B, et al. Effect of gut microbiota and PNPLA3 rs738409 variant on nonalcoholic fatty liver disease (NAFLD) in obese youth. J Clin Endocrinol Metab. 2020;105(10):dgaa382. doi: 10.1210/clinem/dgaa382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Smith SK, Perito ER. Nonalcoholic liver disease in children and adolescents. Clin Liver Dis. 2018;22(4):723–33. doi: 10.1016/j.cld.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 58.Tiniakos DG, Vos MB, Brunt EM. Nonalcoholic fatty liver disease: Pathology and pathogenesis. Annu Rev Pathol. 2010;5:145–71. doi: 10.1146/annurev-pathol-121808-102132. [DOI] [PubMed] [Google Scholar]
- 59.Mendez-Sanchez N, Cruz-Ramon VC, Ramirez-Perez OL, et al. New aspects of lipotoxicity in nonalcoholic steatohepatitis. Int J Mol Sci. 2018;19(7):2034. doi: 10.3390/ijms19072034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Méndez-Sánchez N, Díaz-Orozco L, Córdova-Gallardo J. Redefinition of fatty liver disease from NAFLD to MAFLD raised disease awareness: Mexican experience. J Hepatol. 2021;75(1):221–22. doi: 10.1016/j.jhep.2021.04.021. [DOI] [PubMed] [Google Scholar]
- 61.Eslam M, Alkhouri N, Vajro P, et al. Defining pediatric metabolic (dysfunction)-associated fatty liver disease: An international expert consensus statement. Lancet Gastroenterol Hepatol. 2021 doi: 10.1016/S2468-1253(21)00183-7. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 62.Morales Camacho WJ, Molina Díaz JM, Plata Ortiz S, et al. Childhood obesity: Aetiology, comorbidities, and treatment. Diabetes Metab Res Rev. 2019;35:e3203. doi: 10.1002/dmrr.3203. [DOI] [PubMed] [Google Scholar]
- 63.Draijer LG, van Oosterhout JPM, Vali Y, et al. Diagnostic accuracy of fibrosis tests in children with non-alcoholic fatty liver disease: A systematic review. Liver Int. 2021;41(9):2087–100. doi: 10.1111/liv.14908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nobili V, Alisi A, Newton KP, Schwimmer JB. Comparison of the phenotype and approach to pediatric vs adult patients with nonalcoholic fatty liver disease. Gastroenterology. 2016;150(8):1798–810. doi: 10.1053/j.gastro.2016.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pacifico L, Perla FM, Roggini M, et al. A Systematic review of NAFLD-associated extrahepatic disorders in youths. J Clin Med. 2019;8(6):E868. doi: 10.3390/jcm8060868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mantovani A, Gatti D, Zoppini G, et al. Association between nonalcoholic fatty liver disease and reduced bone mineral density in children: A meta-analysis. Hepatology. 2019;70(3):812–23. doi: 10.1002/hep.30538. [DOI] [PubMed] [Google Scholar]
- 67.Mogahed EA, Sayed AA, Khalifa SE, et al. Causes of secondary non-alcoholic fatty liver disease in non-obese children below 10 years. Eur J Pediatr. 2020;179(5):719–26. doi: 10.1007/s00431-019-03551-0. [DOI] [PubMed] [Google Scholar]
- 68.Nobili V, Cutrera R, Liccardo D, et al. Obstructive sleep apnea syndrome affects liver histology and inflammatory cell activation in pediatric nonalcoholic fatty liver disease, regardless of obesity/insulin resistance. Am J Respir Crit Care Med. 2014;189(1):66–76. doi: 10.1164/rccm.201307-1339OC. [DOI] [PubMed] [Google Scholar]
- 69.Guo Z, Li M, Han B, Qi X. Association of non-alcoholic fatty liver disease with thyroid function: A systematic review and meta-analysis. Dig Liver Dis. 2018;50(11):1153–62. doi: 10.1016/j.dld.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 70.Karaivazoglou K, Kalogeropoulou M, Assimakopoulos S, Triantos C. Psychosocial issues in pediatric nonalcoholic fatty liver disease. Psychosomatics. 2019;60(1):10–17. doi: 10.1016/j.psym.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 71.Boff RM, Liboni RPA, Batista IPA, et al. Weight loss interventions for overweight and obese adolescents: A systematic review. Eat Weight Disord. 2017;22(2):211–29. doi: 10.1007/s40519-016-0309-1. [DOI] [PubMed] [Google Scholar]
- 72.Utz-Melere M, Targa-Ferreira C, Lessa-Horta B, et al. Non-alcoholic fatty liver disease in children and adolescents: Lifestyle change – a systematic review and meta-analysis. Ann Hepatol. 2018;17(3):345–54. doi: 10.5604/01.3001.0011.7380. [DOI] [PubMed] [Google Scholar]
- 73.Schwimmer JB, Ugalde-Nicalo P, Welsh JA, et al. Effect of a low free sugar diet vs usual diet on nonalcoholic fatty liver disease in adolescent boys: A randomized clinical trial. JAMA. 2019;321(3):256–65. doi: 10.1001/jama.2018.20579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen LH, Wang YF, Xu QH, Chen SS. Omega-3 fatty acids as a treatment for non-alcoholic fatty liver disease in children: A systematic review and meta-analysis of randomized controlled trials. Clin Nutr. 2018;37(2):516–21. doi: 10.1016/j.clnu.2016.12.009. [DOI] [PubMed] [Google Scholar]
- 75.Medrano M, Cadenas-Sanchez C, Álvarez-Bueno C, et al. Evidence-based exercise recommendations to reduce hepatic fat content in youth – a systematic review and meta-analysis. Prog Cardiovasc Dis. 2018;61(2):222–31. doi: 10.1016/j.pcad.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 76.Kavey REW. Combined dyslipidemia in children and adolescents. In: Feingold KR, Anawalt B, Boyce A, editors. Endotext [Internet] South Dartmouth (MA): MDText.com, Inc; 2020. Jan 4, 2000. [PubMed] [Google Scholar]
- 77.Cananzi M, Vajro P, Rela M, Dhawan A. NAFLD and Liver Transplantation in Children-Working Group Report from the ILTS Single Topic Conference on NAFLD. Transplantation. 2019;103(1):68–70. doi: 10.1097/TP.0000000000002490. [DOI] [PubMed] [Google Scholar]