INTRODUCTION
Multiple myeloma (MM) is the second most common adult hematologic malignancy and is the most common indication for autologous hematopoietic stem cell transplantation(auto-HCT) [1, 2]. In the current era of novel therapeutics, this treatment is still considered beneficial, with improvements in progression free survival (PFS) [3, 4]. The process of high dose chemotherapy and auto-HCT has thus become routine at most transplant centers and has given rise to the paradigm of out-patient auto-HCT[5].
Initial experience with myeloablative chemotherapy suggested the need for a lengthy hospital stay. However, the evolution of supportive care, including antimicrobial prophylaxis and growth factors, has changed the approach to this procedure [6]. Indeed, numerous transplant centers now routinely offer an out-patient treatment option and several studies have demonstrated comparable if not improved clinical outcomes with out-patient management [7–9].
In this manuscript, we compare the characteristics and clinical outcomes of a large cohort of patients who were treated with auto-HCT as in-patients with those who were treated as out-patients. Our findings indicate that the procedure itself is safe in either setting, but the choice for either option is strongly related to baseline risk factors, including the Hematopoietic Stem Cell Comorbidity Index, (HCTCI).
METHODS
We performed a retrospective chart review of all MM patients undergoing auto-HCT between 2008 and 2012. We divided patients into 2 groups: in-patient versus out-patient, based on their treatment plan. Primary endpoints were incidence of unscheduled admissions, treatment-related mortality (TRM), grade 2–4 adverse events (AEs) and average cost of auto-HCT in each group. Secondary endpoints were overall response (ORR) rates, PFS and overall survival (OS).
We compared clinical characteristics and outcomes between the two groups. Comorbidity was measured by the HCT-CI [10]. Time to neutrophil engraftment was defined as the first day of absolute neutrophil count >500/ul for 3 consecutive days. Time to platelet recovery was defined as the first day of platelet count >20,000/ul without need for transfusion. TRM was defined as death occurring within the first 100 days, not due to disease progression. AEs were graded per as by the National Cancer Institute’s Common Terminology Criteria, version 4.
Differences in baseline characteristics and outcomes between the 2 groups as was determined by a t-test. For patients in the out-patient group, we performed a multivariate analysis to determine which factors were significantly associated with occurrence of unplanned hospital admission. PFS and OS were calculated using the Kaplan Meier method and the long-rank test was used to determine differences in survival between the in-patient and out-patient groups and between those patients with HCT-CI>2 or ≤ 2. Using hospital billing data, we determined the average cost per transplant for both the in-patient and out-patient groups.
RESULTS
We identified 1046 patients who had undergone auto-HCT for MM between 2008–2012 at our institution. Of these, 669 (64%) were treated in the in-patient setting while 377 (36%) were treated in the out-patient setting. Baseline characteristics are listed in Table 1. Notably, the patients who were treated as out-patients were significantly younger (median age 62 for in-patients versus 58 for out-patients, p<0.001). Out-patients were also more likely to have an HCT-CI score of <2 (p=0.003) and serum creatinine <2 (p<0.001). A greater percentage of patient in the out-patient group were receiving their HCT as a first remission consolidation (73% versus 64%, p=0.02) and not in the primary refractory or relapsed setting. Finally, the preparative regimen for the out-patient group tended to be melphalan alone (95% versus 81%, p<0.002) rather than combination chemotherapy.
Table 1.
Patient characteristics
| Inpatient (%) n=669 | Outpatient (%) n=377 | P | |
|---|---|---|---|
| Male | 369 (53) | 234 (62) | |
| Median Age | 62 [31–82] | 58 [34–78] | <0.001 |
| HCT-CI score ≥ 3 | 368 (55) | 170 (45) | |
| Median Karnofsky PS | 90 [40–100] | 90 [70–100] | |
| Unknown | 184 (27) | 91 (24) | |
| Unknown | 28 (4) | 11 (3) | |
| 2nd Auto-HCT | 62 (9) | 24 (6) |
In the out-patient group, 55% of patients required admission to the hospital within the first 30 days. The main cause (42%) of these admissions was neutropenic fever. Other causes included gastrointestinal complications (nausea, vomiting or diarrhea, requiring intravenous hydration), pain (stomatitis or mucositis requiring intravenous analgesics) or treating physician’s discretion. The median time from day of transplant to admission for these patients was 8 days (range: 4–25) and median duration of admission was 6 days (range 0–77). On multivariate analysis, a serum creatinine of >1.5mg/dL and HCT-CI >2 were significantly associated with risk of unscheduled admission, (HR=1.6, 95% CI 1.2–2.2, p = 0.001).
Transplant outcomes are detailed in Table 2. 100-day TRM did not differ between the groups. However there were significantly more grade 2–4 (p=0.003) and grade 3–4 (p=0.003) AE’s in the in-patient group versus the out-patient group. For each cohort and the entire patient population, those with a HCT-CI of >2 had a greater incidence of grade 3–4 AEs (p = 0.03 for the out-patients, p=0.001 for the in patients and p<0.001 for all pts). With regard to disease outcomes, more patients in the out-patient group achieved a CR (96.5%) than those in the in-patient group (89.5%, p<0.001). Two-year PFS was significantly longer in the out-patient versus in-patient group (60% versus 50%, HR =HR 0.7, 95% CI 0.6–0.9, p =0.005, Figure 1A). Two-year OS was also longer in the out-patient versus in-patient group (83% vs. 77%, HR 0.6, 95% CI 04–0.9, p=0.01 Figure 1B). Finally, with regard to resource utilization, the average cost of the transplant procedure was $416,154 (range----) versus $292,572 (range----)
Table 2.
Transplant outcomes
| Inpatient (%) n=669 | Outpatient (%) n=377 | P | |
|---|---|---|---|
| Neutrophils, ANC 500 | 11 [7–16] | 11 [9–15] | |
| Other | 11 (1.6) | 2 (0.6) | |
| Treatment Related Deaths: Day 100 | 10 (1.5) | 1 (0.3) | 0.10 |
| Grade IV | 19 (3) | 6 (2) | 0.2 |
| NE | 7 (1) | 1 (0.3) |
Figure 1A.

Survival outcomes after in-patient or out-patient auto-HCT. Two-year PFS [A] and OS [B] was significantly longer in the out-patient versus in-patient group.
Figure 1B.
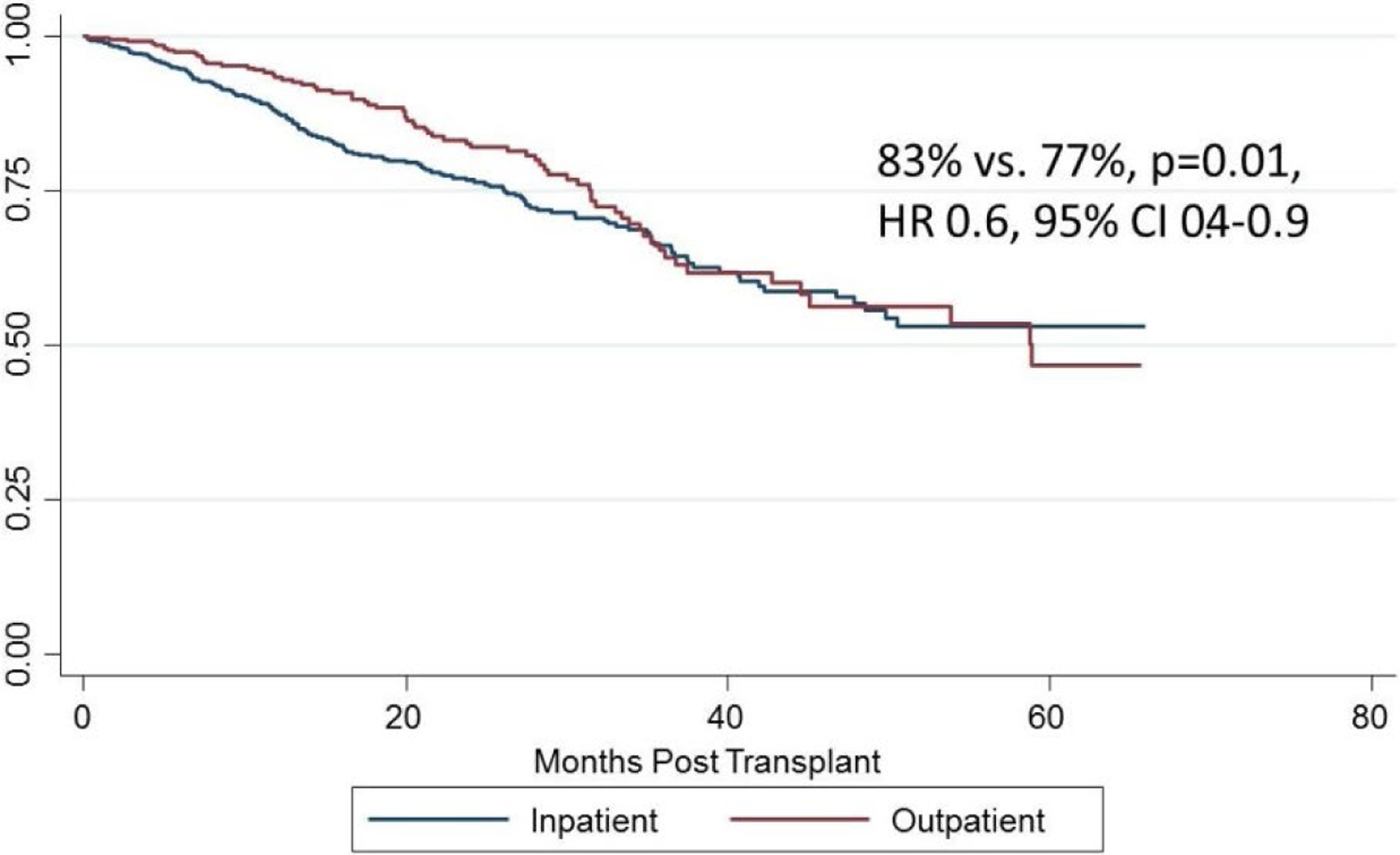
Survival outcomes after in-patient or out-patient auto-HCT. Two-year PFS [A] and OS [B] was significantly longer in the out-patient versus in-patient group.
DISCUSSION
In this analysis of a large cohort of MM patients undergoing auto-HCT, we were able to corroborate previous reports [9, 11, 12]suggesting that this procedure can be done safely in the out-patient setting. Though over half of the out-patients eventually required in-patient admission, the overall incidence of AEs was far less in this group and there was no difference in 100-day TRM.
The differences discovered between groups in clinical outcome is likely due to the differences that existed before the transplant. As would be predicted, patients treated in the in-patient setting tended to be older, with more advanced disease and with more co-morbidities (a finding also previously reported in the literature [9]). Therefore, it is not surprising that the in-patient group had greater AEs and inferior PFS and OS. Another factor in our analysis that likely impacted admission decision was the choice of chemotherapy preparative regimen; for patients treated with combination chemotherapy (for example, busulfan and melphalan) the logistics of treatment necessitated in-patient management and may have impacted AEs.
Though there are some guiding resources [5], at our institution there is no defined algorithm for determining in-patient versus out-patient treatment. However, it appears that those patients chosen for out-patient management were done so appropriately, as their toxicities were not worse than their in-patient counterparts. This suggests that the treating physician is likely able to gauge properly the patients who are best suited to be out-patients. However, it also does not answer the next question: are there patients who are being admitted for this procedure who should actually be treated as an out-patient?
There are a variety of reasons why a patient who is physiologically suitable for out-patient treatment will instead be treated as an in-patient. Housing, caregiver availability and anxiety are likely common factors [13]. However, our rough but informative cost analysis suggests that the out-patient option could save 30% of the entire transplant cost, a finding similar to previously reported analyses [14]. Our data provide the seeds of rationale for third-party payers to consider covering costs of housing or providing a monetary incentive for caregiving. This could maximize the utilization of an out-patient transplant program or even support a mixed out-patient/in-patient program, as has been suggested by others [13, 15].
There are many limitations to our study, with provider bias being the most important. A more rigorous approach, in the absence of randomization, would be to prospectively analyze transplant outcomes between those who were physically capable of out-patient management but admitted for social reasons versus those who were managed as out-patients. This study would be strengthened by accompanying patient-reported outcome data on symptoms and quality of life, which has previously been reported to be favorable in an out-patient cohort [11]. If the outcome data were similar, this would provide stronger rationale for promoting the out-patient transplant approach. Ultimately, patient co-morbidities, provider assessment and, most importantly, patient autonomy must be combined to make the final treatment decision.
REFERENCES
- 1.Moreau P, Attal M, and Harousseau JL, New developments in conditioning regimens before auto-SCT in multiple myeloma. Bone Marrow Transplant, 2011. 46(7): p. 911–5. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, and Jemal A, Cancer Statistics, 2017. CA Cancer J Clin, 2017. 67(1): p. 7–30. [DOI] [PubMed] [Google Scholar]
- 3.Palumbo A, et al. , Autologous transplantation and maintenance therapy in multiple myeloma. N Engl J Med, 2014. 371(10): p. 895–905. [DOI] [PubMed] [Google Scholar]
- 4.Gay F, et al. , Chemotherapy plus lenalidomide versus autologous transplantation, followed by lenalidomide plus prednisone versus lenalidomide maintenance, in patients with multiple myeloma: a randomised, multicentre, phase 3 trial. Lancet Oncol, 2015. 16(16): p. 1617–29. [DOI] [PubMed] [Google Scholar]
- 5.Martino M, et al. , Italian consensus conference for the outpatient autologous stem cell transplantation management in multiple myeloma. Bone Marrow Transplant, 2016. 51(8): p. 1032–40. [DOI] [PubMed] [Google Scholar]
- 6.Kim JH, et al. , Impact of a change in antibacterial prophylaxis on bacteremia and hospitalization rates following outpatient autologous peripheral blood stem cell transplantation for multiple myeloma. Transpl Infect Dis, 2014. 16(3): p. 421–9. [DOI] [PubMed] [Google Scholar]
- 7.Jagannath S, et al. , Feasibility and cost-effectiveness of outpatient autotransplants in multiple myeloma. Bone Marrow Transplant, 1997. 20(6): p. 445–50. [DOI] [PubMed] [Google Scholar]
- 8.Gertz MA, et al. , Autologous stem cell transplant in 716 patients with multiple myeloma: low treatment-related mortality, feasibility of outpatient transplant, and effect of a multidisciplinary quality initiative. Mayo Clin Proc, 2008. 83(10): p. 1131–8. [DOI] [PubMed] [Google Scholar]
- 9.Paul TM, et al. , Outpatient Autologous Stem Cell Transplantation for Patients With Myeloma. Clin Lymphoma Myeloma Leuk, 2015. 15(9): p. 536–40. [DOI] [PubMed] [Google Scholar]
- 10.Sorror ML, et al. , Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood, 2005. 106(8): p. 2912–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lisenko K, et al. , High-dose chemotherapy and autologous stem cell transplantation of patients with multiple myeloma in an outpatient setting. BMC Cancer, 2017. 17(1): p. 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones JA, et al. , In-hospital complications of autologous hematopoietic stem cell transplantation for lymphoid malignancies: clinical and economic outcomes from the Nationwide Inpatient Sample. Cancer, 2008. 112(5): p. 1096–105. [DOI] [PubMed] [Google Scholar]
- 13.Clemmons AB and Anderegg S, Mixed outpatient-inpatient autologous stem cell transplant for multiple myeloma: A cost-saving initiative in a resource constrained environment. J Oncol Pharm Pract, 2016. [DOI] [PubMed] [Google Scholar]
- 14.Holbro A, et al. , Safety and cost-effectiveness of outpatient autologous stem cell transplantation in patients with multiple myeloma. Biol Blood Marrow Transplant, 2013. 19(4): p. 547–51. [DOI] [PubMed] [Google Scholar]
- 15.Reid RM, et al. , Outpatient administration of BEAM conditioning prior to autologous stem cell transplantation for lymphoma is safe, feasible, and cost-effective. Cancer Med, 2016. 5(11): p. 3059–3067. [DOI] [PMC free article] [PubMed] [Google Scholar]


