Abstract
A better understanding of the social-structural factors that influence HIV vulnerability is crucial to achieve the goal of ending the HIV epidemic by 2030. Given the role of neighborhoods in HIV outcomes, synthesis of findings from such research is key to inform efforts toward HIV eradication. We conducted a systematic review to examine the relationship between neighborhood-level factors (e.g., poverty) and HIV vulnerability (via sexual behaviors and substance use). We searched six electronic databases for studies published from January 1, 2007 through November 30, 2017 (PROSPERO CRD42018084384). We also mapped the studies’ geographic distribution to determine whether they aligned with high HIV prevalence areas and/or the “Ending the HIV Epidemic: A Plan for the United States”. Fifty-five articles met inclusion criteria. Neighborhood disadvantage, whether measured objectively or subjectively, is one of the most robust correlates of HIV vulnerability. Tests of associations more consistently documented a relationship between neighborhood-level factors and drug use than sexual risk behaviors. There was limited geographic distribution of the studies, with a paucity of research in several counties and states where HIV incidence/prevalence is a concern. Neighborhood influences on HIV vulnerability are the consequence of centuries-old laws, policies and practices that maintain racialized inequities (e.g., racial residential segregation, inequitable urban housing policies). We will not eradicate HIV without multi-level, neighborhood-based approaches to undo these injustices. Our findings inform future research, interventions and policies.
Keywords: HIV, Neighborhoods, Prevention, Risk, Vulnerability
Introduction
HIV incidence rates in the United States (U.S.) have decreased and subsequently stabilized in the overall population [1]. However, while rates continue to decline in some groups (e.g., people who inject drugs, White men who have sex with men [MSM]), they increase or remain stable among others (e.g., Black MSM, Latinx MSM) [1]. Socially and economically disadvantaged populations experience heightened HIV vulnerability/risk of acquiring HIV; disease burden and prevention innovations are not equally distributed across populations. With sexual activity and injection drug use as the leading causes of HIV transmission, it is easy to place the onus of HIV inequities on people engaged in these behaviors. However, this negates the fact that researchers consistently demonstrate that highly affected groups are not “more risky” than other populations [2]. There are broader social-structural influences at play that shape not only individual behaviors, but also the concentration of HIV in an individual’s networks, which ultimately affects HIV vulnerability.
Brawner coined the term “geobehavioral vulnerability to HIV” to highlight that when examining HIV disease burden, one must acknowledge that it is not just what people do, but also where they do it, and with whom [3]. Where a person lives and who is in their networks is critical to understanding HIV inequities; this, however, is not always a choice. In the U.S., there are segregated geographies and constrained social and sexual networks that result from the historical legacies of slavery and institutional racial discrimination [4]. A host of social (e.g., White flight) and structural (e.g., mortgage redlining) factors govern where individuals live, as well as who is in their networks. This relegates some individuals (e.g., those from socially disadvantaged backgrounds) to neighborhoods and other geosocial spaces with limited resources. This directly affects risk for HIV through factors such as concentrated disadvantage, which is associated with limited health-related services, and increases resultant disease burden. A better understanding of the social-structural factors that increase or protect against HIV risk is crucial to the goal of ending the HIV epidemic. Neighborhoods are a concrete place to start.
The role of neighborhood-level factors in health is well documented in the literature [5]. There is increasing attention given to the mechanisms by which neighborhoods shape sexual risk and substance use [6–8]. Factors such as poverty/concentrated disadvantage, social capital and limited health-related resources are associated with HIV-related health disparities [9, 10]. Yet there is a paucity of literature to integrate findings across studies, which limits our ability to identify modifiable targets for neighborhood-level HIV prevention initiatives.
While neighborhoods themselves cannot cause HIV transmission, they do have social and psychological implications for the individuals who live and engage in those spaces [9]. Neighborhoods operate to enable or constrain individual behaviors and thus contribute to HIV vulnerabilities. Researchers have examined the impact of neighborhood on HIV risk, but as a whole, the mechanisms by which neighborhoods influence HIV vulnerability have yet to be well articulated. We conducted a systematic review to examine the relationship between neighborhood-level factors (e.g., poverty) and HIV vulnerability (via sexual behaviors and substance use) to inform future research, interventions and policies to reduce HIV disease burden in highly affected areas.
Methods
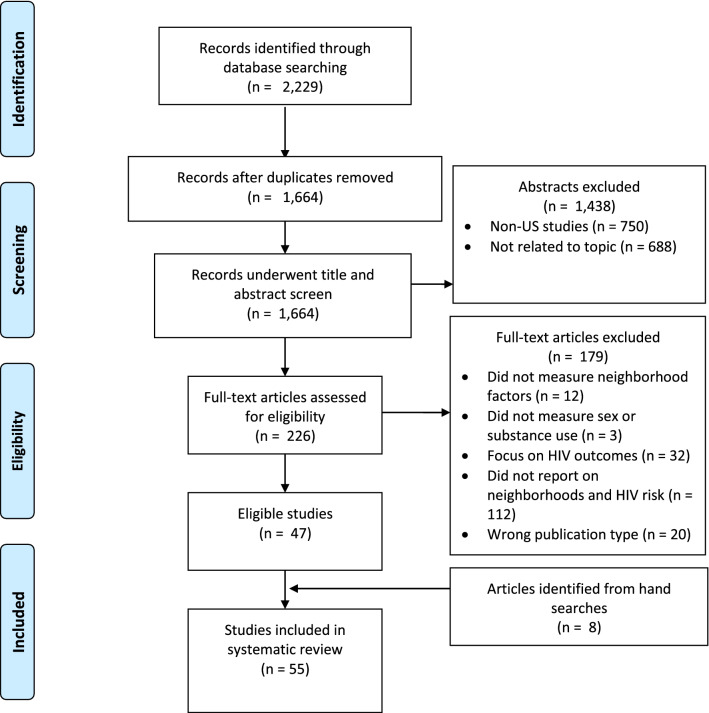
This systematic review was registered in PROSPERO (CRD42018084384), a database of prospectively registered systematic reviews. We followed current Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) guidelines [11]. We searched six electronic reference databases (PubMed, Medline, PsychINFO, Social Sciences Citation Index [SSCI], the Cumulative Index to Nursing and Allied Health Literature [CINAHL], and Sociological Abstracts). Our Boolean search strategy was developed by RJ, a biomedical sciences librarian. We used broad search terms relevant to neighborhoods (e.g., “neighborhood*”, “residence characteristics”, “communities”, “social environment”) and the outcomes (e.g., “risk factors”, "substance use”, “condom use”; see Table 1). The search was limited to data from U.S. studies published in English with abstracts and full-text available. The electronic reference database searches were conducted in January 2017 and updated in November 2017. We searched databases from January 1, 2007 through November 30, 2017 since the early 2000s experienced an uptick in work on neighborhood effects, as well as to enhance implications for current HIV prevention initiatives with more recent literature (Fig. 1).
Table 1.
Systematic review search terms
| Database | Search terms | Articles yielded |
|---|---|---|
| PubMed | ((HIV[Mesh]) AND (("Residence Characteristics"[Mesh] OR neighborhood*[tiab] OR community[tiab] OR communities[tiab] OR zipcode[tiab] OR "zip code" OR "census tract" OR "Cities"[Mesh] OR "city"[tiab] OR "Social Environment"[Mesh]))) AND ("Unsafe Sex"[Mesh] OR "Risk Factors"[Mesh] OR "Risk"[Mesh] OR "Substance-Related Disorders"[Mesh] OR "substance use" OR "drug use" OR "Behavior"[Mesh] OR “Condoms”[Mesh] OR “condom use"[tiab] OR “housing instability” OR “unstable housing” OR eviction OR evicted OR "housing insecurity" OR "insecure housing" OR (“sexual partners” AND (concurren* OR overlap*))) | 411 |
| PsycINFO | mjsub(HIV) AND (mjsub("residence characteristics") OR ti(neighborhood) OR ab(neighborhood) OR mjsub("neighborhoods") OR mjsub("communities") OR ti(zipcode*) OR ab(zipcode*) OR ti("zip code") OR ab("zip code") OR ab("census tract") OR mjsub("social environment")) AND (mjsub("unsafe sex") OR mjsub("risk factors") OR mjsub("substance-related disorders") OR (ti("substance use") OR ti("drug use")) OR mjsub(behavior) OR mjsub(condoms) OR (ti("condom use") OR ab("condom use")) OR (ti("housing instability") OR ti("unstable housing") OR ti("housing insecurity") OR ti("insecure housing")) OR (mjsub("sexual partners") AND (concurren* OR overlap*))) | 379 |
| Soc Abstracts | su(HIV) AND (su("residence characteristics") OR ti(neighborhood) OR ab(neighborhood) OR su("neighborhoods") OR su("communities") OR ti(zipcode*) OR ab(zipcode*) OR ti("zip code") OR ab("zip code") OR ab("census tract") OR su("social environment")) AND (su("unsafe sex") OR su("risk factors") OR su("substance-related disorders") OR (ti("substance use") OR ti("drug use")) OR su(behavior) OR su(condoms) OR (ti("condom use") OR ab("condom use")) OR (ti("housing instability") OR ti("unstable housing") OR ti("housing insecurity") OR ti("insecure housing")) OR (su("sexual partners") AND (concurren* OR overlap*))) | 42 |
| Social Sciences Citation Index (SCCI) | (TS = HIV) AND (TS = “residence characteristics” OR ti = neighborhood OR TS = "neighborhoods" OR TS = “communities” OR TI = zipcode* OR TI = "zip code" OR TI = “census tract” OR TS = “social environment”) AND (TS = “unsafe sex” OR TS = “risk factors” OR TS = “substance-related disorders” OR TI = “substance use” OR TI = “drug use” OR TS = behavior OR TS = condoms OR TS = “condom use” OR TI = “condom use” OR TI = “housing instability” OR TI = “unstable housing” OR TI = “housing insecurity” OR TI = “insecure housing” OR TI = “concurrent sexual partners”) | 791 |
| CINAHL | (MH “Human Immunodeficiency Virus+”) AND (MH “Social Environment+” OR City OR Cities OR MH “Urban Areas” OR “census tract” OR zipcode OR “zip code” OR community OR communities OR neighborhood* OR MH “Residence Characteristics+”) AND ((“sexual partners” AND (concurren* OR overlap*)) OR “housing insecurity” OR “insecure housing” OR eviction OR evicted OR “housing instability” OR “Unstable housing” OR “condom use” OR MH “Condoms+” OR MH “Behavior+” OR “substance use” OR “drug use” OR MH “Substance Use Disorders+” OR “risk” OR MH “Risk Factors+” OR MH “Unsafe Sex”) | 91 |
| Medline | (exp HIV/ AND (exp Social Environment/ OR exp Cities/ OR neighborhood.mp. OR neighborhoods.mp. OR community.mp. OR communities.mp. OR zipcode.mp. OR zip code.mp. OR census tract.mp. OR city.mp.) AND (exp Unsafe Sex/ OR exp Risk Factors/ OR exp Risk/ OR exp Substance-Related Disorders/ OR "substance use".mp. OR drug use".mp. OR exp Behavior/ OR exp Condoms/ OR "condom use".mp. OR housing instability.mp. OR unstable housing.mp. OR housing insecurity.mp. OR insecure housing.mp. OR eviction.mp. OR evicted.mp. OR ((sexual partners.mp. or exp Sexual Partners/) AND (concurren* or overlap*).mp)) | 515 |
| Total | 2229 |
Several of the electronic databases had specific search methods (e.g., PubMed uses Medical Subject Heading [MeSH] terms) while some other databases do not, thus the search strategy was modified according to the parameters for each database
Fig. 1.
Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) diagram for the reviewed articles
Study Selection and Data Extraction
The initial search yielded a total of 2229 articles. RJ created an EndNote X8 library for data management and independently screened titles and abstracts to identify full-text articles for final eligibility review. We considered empirical articles (including qualitative and quantitative studies) with a specific focus on the relationship between neighborhoods and HIV risk behaviors. Articles were included if they: (a) measured neighborhood-level factors (e.g., poverty), (b) measured sexual risk behavior(s) (e.g., multiple sexual partners) and/or substance use/abuse outcomes (e.g., injection drug use), and (c) examined and reported on the relationship between neighborhood-level factors and HIV risk behaviors in the analyses. Articles with a primary focus on HIV outcomes (e.g., testing, medication adherence), dissertations, non-peer reviewed publications, commentaries, literature reviews and other conceptual/theoretical work, and articles that did not expressly address neighborhood-level influences on HIV risk behaviors were excluded.
After RJ excluded duplicates (n = 565) and 1438 titles and abstracts that did not meet the inclusion criteria, BMB and JK independently reviewed the remaining 226 full-text articles for final inclusion. They each created independent lists of articles to include/exclude, with a cumulative total of 60 articles between them for consideration. They reached initial agreement on 47 of the 60 articles, and held subsequent meetings with co-authors to reach consensus on 13 articles where there were disagreements. The co-authors made a determination to exclude these 13 articles from the review as they did not strictly adhere to the inclusion criteria (e.g., the studies did not provide adequate measurement or definition of neighborhoods in the analyses). Eight articles that were not identified in the search strategy but were relevant to the topic were discovered by hand-searching the references lists in the included articles. With the 47 articles identified from the search strategy, and eight discovered in the hand-search, complete agreement was reached by all authors on the final 55 articles included in this review.
JAB and BFC conducted data extraction based on a protocol for key study characteristics including: study year(s) and location, design, individual and neighborhood sample size and description, how neighborhoods were definition/operationalized, individual-level variables, neighborhood-level variables, outcome variables, key findings/conclusion, and directions for future research. We wanted to determine whether the study locations mapped onto areas with high HIV prevalence and/or were in the “Ending the HIV Epidemic: A Plan for America” (EHE)—a U.S. Department of Health and Human Services (HHS) initiative to reduce new HIV infections in the U.S. by 90% by 2030 [12]. The EHE prioritizes efforts in 57 jurisdictions, including 48 counties, Washington, DC, San Juan, Puerto Rico, and seven states with a significant number of HIV diagnoses in rural areas (Oklahoma, Arkansas, Missouri, Mississippi, Alabama, Kentucky, and South Carolina). SB created maps in ArcGIS 10.6 (ESRI, Redlands, CA) to visualize the geographic distribution of the studies.
Results
Of the 55 articles included in this review, 44 were quantitative, 8 were qualitative and three were mixed or multi-method studies (see Table 2). While the majority of the studies focused on adult populations, 9 included youth samples. The majority included participants regardless of race or ethnicity and had samples experiencing socioeconomic challenges (e.g., homelessness). Black/African American populations were the predominant focus among the studies targeted to specific racial or ethnic groups (n = 14); only one study explicitly focused on a Latinx population. The majority did not specify sexual identity; 16 studies focused on MSM, bisexual men and/or transwomen.
Table 2.
Study design and neighborhood description
| Article citation | Study years | Location of study | Study design | Neighborhood description | Neighborhood definition |
|---|---|---|---|---|---|
| Akers, A. Y., Muhammad, M. R., & Corbie-Smith, G. (2011) | 2006 | Northeastern North Carolina | Qualitative, Grounded theory approach; focus groups of adolescents, young adults, and adults | Rural county | Kone et al., 2000 definition of a neighborhood as a group of people with existing social relationships and interaction patterns that share common interests, have similar cultural backgrounds, and live in the same geographic area |
| Bauermeister J.A., Eaton L., Andrzejewski J., Loveluck J., VanHemert W., & Pingel, E.S. (2015) | 2015 | Detroit | Cross-sectional survey | No description | Census tract |
| Bauermeister, J. A., Zimmerman, M. A., & Caldwell, C. H. (2011) | 1994–1997 | Midwest (Flint, MI) | Longitudinal study | No description | Census block group |
| Biello, K. B., Niccolai, L., Kershaw, T. S., Lin, H., & Ickovics, J. (2013) | 1997–2007 | Metropolitan areas of the United States | Longitudinal study | Population factors related to segregation concentration, clustering, exposure | Census tract |
| Bluthenthal, R. N., Do, D. P., Finch, B., Martinez, A., Edlin, B. R., & Kral, A. H. (2007) | 1998–2002 | San Francisco Bay Area | Cross-sectional study | East Bay area of San Francisco | Census tract |
| Bobashev, G. V., Zule, W. A., Osilla, K. C., Kline, T. L., & Wechsberg, W. M. (2009) | 2005–2008 | Counties of North Carolina | Cross-sectional study | Durham, Wake, Johnston, and Chatham counties | County |
| Bowleg, L., Neilands, T. B., Tabb, L. P., Burkholder, G. J., Malebranche, D. J., & Tschann, J. M. (2014) | Not reported | Philadelphia | Cross-sectional, mixed methods study | US Census blocks with a Black population of at least 50% | Census blocks |
| Boyer, C. B., Greenberg, L., Chutuape, K., Walker, B., Monte, D., Kirk, J.,... & Adolescent Med Trials, N. (2017) | 2012–2013 | Tampa, LA, DC, Philadelphia, Chicago, Bronx, NY, New Orleans, Miami, Memphis, Houston, Detroit, Baltimore, Boston, Denver | Cross-sectional study | Neighborhood examined as "community context" | N/A |
| Braine, N., Acker, C., Goldblatt, C., Yi, H., Friedman, S., & DesJarlais, D. C. (2008) | 2000–2001 | Pittsburgh | Qualitative, historical analysis | Hill District, Uptown, and other neighborhoods of Pittsburgh | Historical and socially defined neighborhoods as provided by participants; Census tracts used with historical data |
| Brawner B.M., Reason J.L., Hanlon K., Guthrie B., Schensul J.J. (2017) | 2012 | Philadelphia | Qualitative descriptive study | Community included in study included was selected to ensure the greatest diversity possible | Census tract |
| Brawner, B. M., Guthrie, B., Stevens, R., Taylor, L., Eberhart, M., & Schensul, J. J. (2017) | 2011–2013 | Philadelphia | Multi-method, comparative study | Philadelphia Census tracts selected to achieve maximal difference across the areas according to racial/ethnic composition and HIV disease burden | Census tract |
| Buot, M. L. G., Docena, J. P., Ratemo, B. K., Bittner, M. J., Burlew, J. T., Nuritdinov, A. R., & Robbins, J. R. (2014) | 1990 and 2000 | United States | Cross-sectional secondary data analysis | No description | Cities with populations greater than 100,000 in 1990 and 2000 and reported as discrete places (cities) by the CDC and the US Census Bureau |
| Buttram, M. E., & Kurtz, S. P. (2013) | 2008–2010 | Miami /Ft.-Lauderdale | Cross-sectional study | Gay neighborhoods can be defined as visible places within a city that commonly have businesses, residences, and social life dominated by gay men | Zip codes, defined as a gay neighborhood versus non-gay neighborhood |
| Cené, C. W., Akers, A. Y., Lloyd, S. W., Albritton, T., Powell Hammond, W., & Corbie-Smith, G. (2011) | 2006–2007 | Two Northeast counties in North Carolina | Community-based participatory study, semi-structured qualitative interviews | Neighborhood defined as a component of the Social Network Model | N/A |
| Cooper, H. L., Friedman, S. R., Tempalski, B., & Friedman, R. (2007) | 1990 and 1998 | United States | Lagged, cross-sectional study; secondary data analysis | Counties that include at least 1 central city home to at least 500,000 residents in 1993 | US metropolitan statistical areas (MSAs) defined by the US Census Bureau; Census tract |
| Cooper, H. L., Linton, S., Haley, D. F., Kelley, M. E., Dauria, E. F., Karnes, C. C., … & Adimora, A. (2015) | 2008–2010 | Atlanta, GA | Cross-sectional, multilevel, longitudinal study | Neighborhoods segregation between White and African-American households are a form of structural discrimination | Census tract |
| Cooper, H. L., Linton, S., Kelley, M. E., Ross, Z., Wolfe, M. E., Chen, Y. T., … & Semaan, S. (2016) | 2009 | United States | Cross-sectional, quantitative study; secondary data analysis | Neighborhoods conceptualized using the Risk Environment Model | MSAs; zip codes and counties (provided by participants) |
| Crawford, N. D., Borrell, L. N., Galea, S., Ford, C., Latkin, C., & Fuller, C. M. (2013) | 2000 | New York City (Harlem, Lower East Side, South Bronx, Jamaica-Queens and Bedford-Stuyvesant-Brooklyn) | Cross-sectional, secondary data analysis | Neighborhoods are contexts in which individuals may experience social discrimination | Census tracts |
| DePadilla, L., Elifson, K. W., & Sterk, C. E. (2012) | 2009–2011 | Atlanta, GA | Cross-sectional, quantitative study | Conceptualized neighborhoods as places where individual behaviors occur in the larger context of poverty, unequal access to health care, and uneven criminal justice involvement | Census block groups used for sampling |
| Duncan, D. T., Kapadia, F., & Halkitis, P. N. (2014) | 2009–2011 | New York City | Cross-sectional, quantitative study | Defined neighborhoods as varying spatial contexts, where individuals can move beyond where they reside (e.g. the residential neighborhood) for school, church, shopping, and socialization | Borough, neighborhood contexts (residential, social, sexual) |
| Study 1: not stated | South Florida | Cross-sectional, two-armed, randomized controlled trial | Neighborhoods conceptualized regarding MSM migration to urban neighborhoods to avoid discrimination and alienation and to find support and acceptance from other MSM, yet may increase their vulnerability to sexual risks and drug use | South Florida region | |
| Egan, J. E., Frye, V., Kurtz, S. P., Latkin, C., Chen, M., Tobin, K., … & Koblin, B. A. (2011) | Study 2: not stated | New York City | Qualitative observational study | Discussed urban "gay" neighborhoods as areas that may offer acceptance and socialization for urban MSM, yet also expose MSM to high-risk micro-environments that significantly increase risk of mental and physical health problems related to gentrification and stress associated with neighborhood tension | Distinct neighborhoods (Chelsea/Hell's Kitchen, Fort Greene, Harlem, and Washington Heights) that are part of the NYC MSA; participant-defined to map their residential neighborhood, social neighborhood, and sexual neighborhood |
| Study 3: not stated | Baltimore | Cross-sectional, randomized clinical trail | Discussed social networks that contribute to the amount, type, and source of emotional and instrumental social support | N/A (no neighborhood level variables) | |
| Frew, P. M., Parker, K., Vo, L., Haley, D., O'Leary, A., Diallo, D. D., … & Hodder, S. (2016) | 2009–2010 | New York City, Atlanta, Baltimore, Newark, Raleigh-Durham, NC; Washington, DC | Qualitative study | Neighborhood conceptualized using Bronfrenbrenner's ecological model | Zip code or census tract |
| Frye, V., Koblin, B., Chin, J., Beard, J., Blaney, S., Halkitis, P., … & Galea, S. (2010) | 1990–2000 | New York City | Multilevel analysis | Discussed neighborhoods as urban areas with a concentration of MSM that serves as an environment that may influence health behaviors | Zip code |
| Frye, V., Nandi, V., Egan, J. E., Cerda, M., Rundle, A., Quinn, J. W., … & Koblin, B. (2017) | 2010–2013 | New York City | Cross-sectional study | Neighborhoods described as gay enclaves, those with a growing gay population, as well as neighborhoods with a much less visible or documented gay presence | Neighborhood Tabulation Areas (NTAs) |
| Genberg, B. L., Gange, S. J., Go, V. F., Celentano, D. D., Kirk, G. D., Latkin, C. A., & Mehta, S. H. (2011) | 1988–2008 | Baltimore | Prospective cohort study | Urban area | Census tracts |
| Gindi, R. M., Sifakis, F., Sherman, S. G., Towe, V. L., Flynn, C., & Zenilman, J. M. (2011) | 2007 | Baltimore | Prospective cohort study | Neighborhood-level predictors are settings in which individuals choose their sex partners. Participants define what "in the neighborhood" meant | Census tracts |
| Haley, D. F., Haardorfer, R., Kramer, M. R., Adimora, A. A., Wingood, G. M., Goswami, N. D., … & Cooper, H. L. F. (2017) | 2013–2015 | Alabama, Georgia, Mississippi, Florida, and North Carolina | Cross-sectional study | Neighborhoods conceptualized as opportunity structures in which residents with greater economic disadvantage or social disorder have decreased access to resources necessary for healthy behaviors and greater risk or hazardous exposures that are detrimental to health | Census tract |
| Heimer, R., Barbour, R., Palacios, W. R., Nichols, L. G., & Grau, L. E. (2014) | 2008–2011 | Towns in Fairfield or New Haven Counties in Connecticut | Longitudinal study | Suburban communities in southwest Connecticut (with the exclusion of Bridgeport, Danbury, New Haven, Norwalk, Stamford, or Waterbury) | Census tract |
| Kelly, B. C., Carpiano, R. M., Easterbrook, A., & Parsons, J. T. (2012) | 2005 | New York City | Cross-sectional, intercept survey | NYC or New Jersey areas served by the PATH train routes; suburbs | Zip codes |
| Kerr, J. C., Valois, R. F., Siddiqi, A., Vanable, P., & Carey, M. P. (2015) | 2006–2007 | Macon, GA, Providence, RI, Syracuse, NY, and Columbia, SC | Cross-sectional study | Northeastern and Southeastern U.S. | U.S. region (Northeast, Southeast) |
| Knittel, A. K., Snow, R. C., Riolo, R. L., Griffith, D. M., & Morenoff, J. (2015) | Not reported (examined data over 5 years) | United States | Agent-based modeling | Neighborhoods simulated agents (incarcerated individuals) from urban areas in model developed in this study | N/A |
| Koblin, B. A., Egan, J. E., Rundle, A., Quinn, J., Tieu, H. V., Cerdá, M., … & Frye, V. (2013) | 2010–2012 | New York City | Cross-sectional study | NYC boroughs that are traditionally considered gay enclaves, those with a growing gay population, as well as neighborhoods with a much less visible or documented gay presence | NYC boroughs, census tracts |
| Koblin, B. A., Egan, J. E., Nandi, V., Sang, J. M., Cerda, M., Tieu, H.-V.,... Frye, V. (2017) | 2010–2013 | New York City | Cross-sectional study | Neighborhoods within NYC community districts which range in population size from 50,000 residents to more than 200,000 | Community districts and neighborhoods |
| Latkin, C. A., Curry, A. D., Hua, W., & Davey, M. A. (2007) | 2002–2004 | Baltimore | Cross-sectional study | Neighborhood conceptualized as residential location is associated with physical health and mortality | N/A |
| Lutfi, K., Trepka, M. J., Fennie, K. P., Ibanez, G., & Gladwin, H. (2015) | 2006–2010 | US metropolitan and micropolitan areas | Cross-sectional study | Neighborhood conceptualized as community factors can contribute to disparities in sexually transmitted infections related to racial segregation | Core-based statistical areas (CBSA), census tract |
| Martinez, A. N., Lorvick, J., & Kral, A. H. (2014) | 2004–2005 | San Francisco Bay Area | Cross-sectional study | Neighborhoods described as activity spaces- the local areas of neighborhoods in which individuals move throughout their course of daily activities | Census tract |
| Mustanski, B., Birkett, M., Kuhns, L. M., Latkin, C. A., & Muth, S. Q. (2015) | 2011–2012 | Chicago | Network study | Neighborhoods describes as locations in which disparities exist in socioeconomic status and HIV prevalence, and racial segregation | Community area |
| Nandi, A., Glass, T. A., Cole, S. R., Chu, H., Galea, S., Celentano, D. D.,... Mehta, S. H. (2010) | 1990–2006 | Baltimore City, MD | Prospective cohort study | Location of study had a per capita prevalence of IDU of 162 per 10,000 population, second among the largest metropolitan statistical areas in the U.S. and 14% prevalence of HIV among IDUs in 1998. Ranked 11th among the largest metropolitan statistical areas in the U.S. | Census tracts |
| Neaigus, A., Jenness, S. M., Reilly, K. H., Youm, Y., Hagan, H., Wendel, T., & Gelpi-Acosta, C. (2016) | 2010 | New York City | Cross-sectional study | Location of study described as NYC adjoining communities with high poverty zip codes areas that were designed to approximate NYC Community Planning Districts | United Hospital Fund neighborhoods |
| Pachankis, J. E., Eldahan, A. I., & Golub, S. A. (2016) | 2014 | New York City | Cross-sectional study | Neighborhood of focus in this study were described as urban neighborhoods that are destinations for gay or bisexual men | Zip codes |
| Parrado, E. A., & Flippen, C. (2010) | 2002–2003 and 2006–2007 | Durham, NC | Cohort study | Utilized a theoretical framework of social disorganization and commercial sex | Apartment complex |
| Quinn, K., Voisin, D. R., Bouris, A., & Schneider, J. (2016) | 2012–2014 | Chicago | Randomized control trial | Neighborhood conceptualized as component of “HIV risk environment”, involving a dynamic interplay between structural and network factors | N/A |
| Raymond, H. F., Al-Tayyib, A., Neaigus, A., Reilly, K. H., Braunstein, S., Brady, K. A., … & German, D. (2017) | 2011 | Baltimore, Detroit, Denver, Houston, Los Angeles, Miami, New Orleans, New York City, Philadelphia, San Francisco, Seattle, and District of Columbia | National HIV Behavioral Surveillance (NHBS) data used for the study (phylogenetic study) | Neighborhoods characterized as environments of high poverty and/or low socioeconomic status, and environments of sexual networks; these contribute to disparities in HIV incidence in the U.S. | City (NHBS data collection jurisdiction for each individual-funded entity; can include a metropolitan statistical area) |
| Raymond, H. F., Chen, Y. H., Same, S. L., Catalano, R., Hutson, M. A., & McFarland, W. (2014) | 2008 | San Francisco | Geographic analysis | Utilized a social epidemiologic framework of HIV infection which suggests that low SES neighborhoods and social and sexual networks in communities influence disparities in HIV infection | Zip code |
| Rothenberg, R. B., Dai, D., Adams, M. A., & Heath, J. W. (2017) | 2006–2011 | Atlanta | Cross-sectional study | Not reported | Zip code |
| Rudolph, A. E., Crawford, N. D., Latkin, C., Fowler, J. H., & Fuller, C. M. (2013) | 2006–2009 | New York City | Longitudinal study | Discussed neighborhoods as having structural and network factors that can contribute to increased risk for HIV | Census tract |
| Rudolph, A. E., Linton, S., Dyer, T. P., & Latkin, C. (2013) | 2005–2007 | Baltimore | Cross-sectional study | Characterized the “HIV risk environment” as a dynamic interplay between structural and network factors | City block |
| Senn, T. E., Walsh, J. L., & Carey, M. P. (2016) | Not reported | United States | Cross-sectional study | Conceptualized neighborhood as containing contextual factors that affect sexual health and STIs | Census tract |
| Sterk, C. E., Elifson, K. W., & Theall, K. P. (2007) | 2002–2004 | Atlanta | Ethnographic study | Discussed neighborhoods as having conditions, such as neighborhood disadvantage, that often result in impaired health | Inner city community |
| Stevens, R., Gilliard‐Matthews, S., Nilsen, M., Malven, E., & Dunaev, J. (2014) | Not reported | Northeastern city | Qualitative study | City of study is typified by concentrated poverty, high childhood high rate of single-parent headed households, and low graduation rate. This city also ranked second to last in the nation for safety in 2010 | City |
| Stevens, R., Icard, L., Jemmott, J. B., O'Leary, A., Rutledge, S., Hsu, J., & Stephens-Shields, A. (2017) | 2008 – 2011; 2006–2010 | Philadelphia | Cross-sectional study | Discussed neighborhoods as having characteristics, such as perceived neighborhood disorder, perceived neighborhood violence, and homelessness, that are associated with transactional sexual behaviors | Census block group |
| Tobin, K. E., Latkin, C. A., & Curriero, F. C. (2014) | 2012 | Baltimore | Cross-sectional study | Study setting is one of the most burdened cities in the country, ranking the second highest for gonorrhea, seventh for syphilis cases, and fourth highest for Chlamydia | City |
| Tobin, K. E., Hester, L., Davey-Rothwell, M. A., & Latkin, C. A. (2012) | 2008 | Baltimore | Cross-sectional, secondary data analysis | Neighborhood or residential location has been hypothesized to influence health is through facilitating social interaction sand formation and perpetuation of social norms | Census block group |
| Voisin, D. R., Hotton, A. L., & Neilands, T. B. (2014) | 2006 | Midwestern city | Cross-sectional study | Exposure to community violence is another significant public health concern that disproportionately impacts African American youth. Community violence may influence HIV risk behaviors among youth | N/A |
| Williams, C. T., & Latkin, C. A. (2007) | 1996–2002 | Baltimore City | Cross-sectional, multilevel design | Neighborhood environments represent a more distal social context that capture physical and economic features of one’s environment, and structures network composition and relations | Census block group |
Four key findings were noted: (a) there is substantial variability in how authors define and operationalize neighborhood-level factors; (b) most sexual risk behavior studies focus on condom use instead of other outcomes, and most substance use studies focus on injection drugs instead of alcohol or other drugs; (c) tests of associations more consistently document a relationship between neighborhood-level factors and drug use than sexual risk behaviors; and (d) there is limited geographic distribution of studies, with a paucity of research in several populous metropolitan areas where HIV incidence/prevalence is a concern.
Definition and Operationalization of Neighborhood-Level Factors
The majority of the studies reviewed defined neighborhoods in terms of administrative boundaries such as region of the U.S., metropolitan statistical areas, census tracts or block groups, or a combination of the above (n = 48). One study did examine apartment complexes, providing a more granular analysis of the relationship between neighborhood social milieu and sexual risk [13]. Some also chose nontraditional definitions such as groups of individuals with existing social relationships and interaction patterns [14] or locales dominated by gay men (i.e., gay neighborhood residence versus non-residence) [15]. Others allowed the study participants to define their neighborhoods relative to historical or social markers [16, 17]. Neighborhood-level variables of interest included but were not limited to sociodemographics (e.g., percentage of adults in the zip code with a college education), HIV incidence and prevalence rates, social capital (e.g., trust and connections among community members), indicators of structural disadvantage in the built environment (e.g., vacant housing), community violence and racial residential segregation. Fewer studies examined factors such as social and geographic distance [18], or spatial clustering of locations for drug and alcohol use [19].
HIV Vulnerability Outcomes of Interest
Sexual risk behaviors were the main outcome in most of the quantitative studies (n = 28; see Table 3); condom use was the most commonly reported outcome. Articles related to sexual risk also included primary outcomes of HIV/STI incidence, number of sexual partners, sexual debut, exchange/transactional sex and behavioral norms. One study measured participants’ perceptions of their partner’s risk and concurrency [20]. For those that focused on substance use (n = 10), injection drug use was the most prominent, followed by alcohol. One study also examined participants’ membership in high prevalence drug networks [21]. Eight articles included sexual and substance use behaviors as primary outcomes, examining both behaviors such as receptive/distributive syringe sharing and number of sexual partners.
Table 3.
Study sample and variables
| Article citation | Neighborhood sample size | Individual sample size | Inclusion criteria | Individual-level variables | Neighborhood-level variables | Outcome variables |
|---|---|---|---|---|---|---|
| Akers, A. Y., Muhammad, M. R., & Corbie-Smith, G. (2011) | n = 2 | n = 93 | Purposive sampling; young people aged 16–24 years (4 focus groups, n = 38), adults aged 25 years and above (5 focus groups, n = 42) and formerly incarcerated individuals (2 focus groups, n = 13) | N/A | N/A | N/A |
| Bauermeister J.A., Eaton L., Andrzejewski J., Loveluck J., VanHemert W., Pingel, E.S. (2015) | N/A | n = 328 | Age 18–29, cismale or transgender, residing in Detroit metro, and reporting having sex with men | Race/ethnicity, sexual orientation, educational attainment, relationship status, residential stability, alcohol use, marijuana use | Perceived community LGBT acceptance, perceived community LGBT stigma, Residential address, distance from LGBT bars & clubs, HIV testing sites, AIDS Service organizations, AIDSvu test locators, LGBT organizations, neighborhood disadvantage score (%households in poverty, % households in public aid, % single-headed households with children, %residents over age 25 w/o high school diploma) | HIV testing, sex with serodiscordant UAI partner |
| Bauermeister, J. A., Zimmerman, M. A., & Caldwell, C. H. (2011) | n = 123 | n = 681 | Eligible participants had a GPA of 3.0 or lower at the end of 8th grade, not diagnosed with emotional or developmental impairments, and identified as African American, White, or Bi-racial | Self-reported: condom use, frequency of sexual intercourse, number of sexual partners, pregnancy concerns, psychological distress, substance use, age, sex, parental occupation (provided by participant) | Standardized neighborhood concentrated economic disadvantage score | Condom use |
| Biello, K. B., Niccolai, L., Kershaw, T. S., Lin, H., & Ickovics, J. (2013) | n = 17 | n = 4583 | Individual-level data obtained from the National Longitudinal Survey of Youth 1997 ages 12–16 years old on December 31, 1996; data limited to non-Hispanic blacks and whites residing in Census-defined metropolitan areas | Self-reported: race, ethnicity, sex; parent-reported: gross household income, maternal and paternal education, family structure | Hyper segregation: exposure, concentration, centralization, clustering, and unevenness; population size, population density, racial composition, socioeconomic measures (percent unemployed, percent in poverty, percent with less than high school education) | Sexual risk behavior |
| Bluthenthal, R. N., Do, D. P., Finch, B., Martinez, A., Edlin, B. R., & Kral, A. H. (2007) | n = 294 tracts (Syring sharing sample); n = 282 (sexual behavior sample) | n = 4956 | Data obtained from the Urban Health Study (UHS); participants were 18 years or older and had physical evidence of drug injection (track marks or stigmata) | Self-reported: gender (male, female), age (continuous), education (less than high school, high school, some college, college, or college graduate), race (white, African American, Hispanic, or other), sexual orientation (heterosexual or gay/lesbian/bisexual), homelessness (yes or no), main income source (paid work, government assistance, or other), consistent sex partner (yes or no), syringe exchange program in the past 6 months (yes or no), and participation in same gender sex in the past 6 months (yes or no), street and cross-street of residence; researcher determined: HIV positive status (yes or no) | Percent African American, percent male unemployment, percent of households that receive public assistance, median household income; economic deprivation (average of four indicators: proportion of 16–19 year-old high school drop outs, male unemployment rate, households receiving public assistance, and female head of households) | Receptive syringe sharing, distributive syringe sharing, unprotected sex, and multiple sex partners |
| Bobashev, G. V., Zule, W. A., Osilla, K. C., Kline, T. L., & Wechsberg, W. M. (2009) | n = 4 | n = 1730 | Males, at least 18 years old; female sex partners also included in study; report history of substance abuse (heroin, cocaine, methamphetamine, or injection drug) in the past 6 months; report anal sex with a male in the past 6 months, participants who were recruited with their partner must have reported to have sex with that partner in the past 6 months | Sex (male or female), bisexual behavior, psychological distress (depression, anxiety, somatization subscales of the BSI-18), drug use, binge drinking of alcohol, sexual risk behaviors, partner change within the past 6 months, HIV, any STIs, unprotected sex | Provided by participants: perceived neighborhood violence and neighborhood disorder | Transactional sex (purchasing or selling sex) |
| Bowleg, L., Neilands, T. B., Tabb, L. P., Burkholder, G. J., Malebranche, D. J., & Tschann, J. M. (2014) | n = 60 | n = 526 | Black/African American men, identifying as heterosexual, 18–44 years old, and reported vaginal sex during the last 2 months | Substance use, depression, demographics (age, education, employment status, relationship status) | Participant-reported City Stress Inventory (CSI) 18-item measure | Sexual risk behavior |
| Boyer, C. B., Greenberg, L., Chutuape, K., Walker, B., Monte, D., Kirk, J.... & Adolescent Med Trials, N. (2017) | N/A | N = 1818 |
Study eligibility included being aged 12–24 years and having a self-reported history of engaging in consensual sex (oral, anal, or vaginal) in the 12-month period prior to survey administration |
Age, birth and identified sex, race and ethnicity, sexual orientation, educational attainment, history of homelessness, current living situation, and relationship status | Participant-reported economic insecurity, job training, housing instability, crime victimization, and perceived community norms | Transactional sex (selling sex) |
| Braine, N., Acker, C., Goldblatt, C., Yi, H., Friedman, S., & DesJarlais, D. C. (2008) | n = 30 | n = 151 | Respondents must report regularly receiving syringes during the last year, either directly from volunteers or indirectly through secondary exchange/distribution | Demographics, neighborhood of residence, drug use, sexual behavior, HIV risk behavior, health status, and syringe distribution networks | Historical policy of migration, neighborhood formation, entertainment venues, and drug policy | N/A |
| Brawner B.M., Reason J.L., Hanlon K., Guthrie B., Schensul J.J. (2017) | n = 1 | n = 10 | Age 18 and older, lived, worked and/or had a vested interest in the Philadelphia Census tract with the highest HIV and AIDS rates in the city. Included administrators, direct HIV/AIDS service provider, or community member | Demographic variables (age, income) | N/A | N/A |
| Brawner, B. M., Guthrie, B., Stevens, R., Taylor, L., Eberhart, M., & Schensul, J. J. (2017) | n = 4 | n = 339 | HIV surveillance case data included if cases: resided in one of the four targeted Census tracts, were diagnosed on or before December 31, 2010, were living as of January 1, 2006, and were at least 18 years of age | Current age, Census tract of current residence (most recently recorded address), gender, race/ethnicity, insurance status, and most recently recorded CD4 count | Census tracts categorized as (a) predominantly white high HIV prevalence, (b) predominantly black high HIV prevalence, (c) predominantly white low HIV prevalence, and (d) predominantly black low HIV prevalence | Mode of HIV transmission (Male-to-male sexual contact, heterosexual, or IDU) |
| Buot, M. L. G., Docena, J. P., Ratemo, B. K., Bittner, M. J., Burlew, J. T., Nuritdinov, A. R., & Robbins, J. R. (2014) | n = 80 | N/A | N/A | N/A | 1990–2000 US Census data: housing, segregation, living wage estimates, health insurance estimates, crime, anti-MSM stigma (SSM legislation); CDC Wonder database: race/ethnicity, HIV risk behavior categorization | Average HIV incidence |
| Buttram, M. E., & Kurtz, S. P. (2013) | n = 2 | n = 482 | Substance-using MSM who reported recent UAI | Demographic, physical health, mental health, legal involvement, vocational attainment | N/A | Substance use, sexual risk behaviors, prosocial participation |
| Cené, C. W., Akers, A. Y., Lloyd, S. W., Albritton, T., Powell Hammond, W., & Corbie-Smith, G. (2011) | N/A | n = 93 | Focus groups: Age 16 and older; Interviews: Individuals identified by community partners as having valuable opinions on HIV risk, disparities, and potential solutions | Descriptive statistics | Population size, percent African American, State ranking in three-year average rage of new HIV cases, percent of HIV/AIDS cases per county among African Americans, median household income, percent with less than a high school education, percent with a high school diploma, percent with a bachelor's degree or higher | N/A |
| Cooper, H. L., Friedman, S. R., Tempalski, B., & Friedman, R. (2007) | n = 93 | N/A | N/A | N/A | Segregation (concentration and isolation), prevalence of injection drug users per MSA, MSA population size, racial/ethnic composition, geographic region | Injection drug use prevalence among Black adults |
| Cooper, H. L., Linton, S., Haley, D. F., Kelley, M. E., Dauria, E. F., Karnes, C. C., … & Adimora, A. (2015) | n = 77 | n = 172 | Participants must have resided in one of the seven complexes targeted for demolition; being at least 18 years old; self-identifying as Non-Hispanic Black/African American; reported sexual activity in the past year; and not have lived with a previously enrolled participant | Gender, age, marriage status, high school education, annual household income, same-sex behavior, self-reported HIV positive, binge drinking, drug use, alcohol or drug dependence, moved to a new Census tract, perceived community violence | Median household income, poverty rate, percent adults (greater or equal to 25 years old) whose highest degree is a high school diploma or GED, violent crime rate, density of alcohol outlets per square mile, economic disadvantage component, social disorder component, male: female sex ratio | Perceived partner risk, perceived indirect concurrency, perceived neighborhood conditions |
| Cooper, H. L., Linton, S., Kelley, M. E., Ross, Z., Wolfe, M. E., Chen, Y. T. … & Semaan, S. (2016) | n = 19 | n = 9170 | Eligible participants reported injecting drugs in the past 12 months and provided proof of injection (e.g., track marks); lived in the target MSA; and were 18 years old | Race/ethnicity (Latino, white, black), participant-reported zip codes and counties, sociodemographic characteristics, drug-related behaviors | Availability of sex partners, race/ethnic composition, exposure to violence, racial/ethnic segregation, exposure to economic disadvantage, income inequality, spatial access to drug- and HIV related programs, access to general medical care, HIV epidemic among PWID, exposure to law enforcement, policies governing syringe access, health and law enforcement expenditures, access to alcohol, exposure to abandoned buildings | N/A |
| Crawford, N. D., Borrell, L. N., Galea, S., Ford, C., Latkin, C., & Fuller, C. M. (2013) | n = 143 | n = 638 | Participants were ages of 18 and 40. Injection drug users had to report injecting heroin, crack or cocaine for 4 years or less and at least once in the past 6 months. Non-injection drug users had to report non-injection use of heroin, crack or cocaine for 1 year or more at least 2–3 times a week in the past 3 months | Age, female sex partners, male sex partners, age at sexual debut, race/ethnicity, sex, education, marital status, primary drug used, injection status, female condom use (past 2 months), male condom use (past 2 months), HIV testing frequency (lifetime), lifetime depression, HIV status. discrimination, | Neighborhood minority composition (percent black, percent Latino), poverty (percent living below 100% of the poverty threshold), education (percent less than a high school education) | Drug using ties, heroin injecting ties |
| DePadilla, L., Elifson, K. W., & Sterk, C. E. (2012) | n = 77 | n = 1050 | African American, at least 18 years old, and have resided in the sample neighborhood in the past year | demographics (male/female, age), alcohol use in the past 30 days, crack/cocaine use in the past 30 days, marijuana use in the past 30 days, relationship status/sexual partnership, SES (income, employment, health insurance coverage), perception of social cohesion, perceived neighborhood disorder, knowledge of crime, observed violence | N/A | Lack of condom use during vaginal sex with steady partners |
| Duncan, D. T., Kapadia, F., & Halkitis, P. N. (2014) | n = 122 | n = 598 | Participants eligible for study if 18–19 years old at the time of the baseline assessment, biologically male, lived in the New York City metropolitan area, reported having had sex (any physical contact that could lead to orgasm) with another male in the 6 months preceding the baseline assessment, and self-reported a HIV-negative or unknown serostatus | Race/ethnicity, current school enrollment, perceived familial socioeconomic status, foreign-born status, household composition, sexual identity, in a relationship with another man, housing status, ethnic identity, experiences with gay-related stigma, disclosure of sexual orientation, internalized homophobia, gay community affinity, social support network, self-reported residential, social, and sexual neighborhoods | N/A | Condomless anal, condomless oral intercourse |
| n = 1 | n = 325 | Men, age 18–25, report recent UAI with non-monogamous partner(s), report using drugs (excluding marijuana) on at least three days in the past 90 days or getting drunk three or more times in the past month | Demographics (age, education, income, race/ethnicity, sexual identity), regency of migration to South Florida, health/social risk, victimization history, substance use | N/A | Sexual behaviors (past 90 days) | |
| Egan, J. E., Frye, V., Kurtz, S. P., Latkin, C., Chen, M., Tobin, K., … & Koblin, B. A. (2011) | n = 4 | n = 20 | Male sex at birth, reported insertive or receptive sex with a male partner in the past 6 months, at least 18 years old, reported living in Chelsea/Hell's Kitchen, Harlem, Washington Heights, or Ft. Green for a least 12 months, speak English, and able to provide informed consent | Demographics (age, race/ethnicity, sexual orientation), HIV status | N/A (described by participants) | N/A (described by participants) |
| N/A | n = 188 | 18 or older, identify as male, self-report black, or African-American race/ethnicity, report having at least two sex partners in the past three months (one of which must be male), report UAI with a male partner in the past three months, willingness to take an HIV test if negative or unknown status or provide documentation of HIV positive status, and willingness to identify social network members and recruit them into the study | Social network characteristics (number of network members, number of network members to talk to/offer help/loan money or valuables/entrust with money/provide health advice/give support to), sexual partner characteristics (number of male/female sex partners, number of partners met through friends/on internet/bar/social support group/at a party/chat online, number of male/female partners who loan money, to hang out with, see at least weekly; number of HIV positive partners, dependence on partners), social network density, demographic characteristics (age, education, employment status), HIV status, lifetime incarceration | Provided by participants: residential distance from sexual partners (all partners outside the same neighborhood, partners in the same neighborhood but not the same household, partners in the same household) | N/A | |
| Frew, P. M., Parker, K., Vo, L., Haley, D., O'Leary, A., Diallo, D. D. … & Hodder, S. (2016) | n = 10 | n = 288 | Women, ages 18–44 years, residing in Census tracts or zip codes (New York City) in the top 30th percentile of HIV prevalence and > 25% of inhabitants living in poverty, reporting at least one episode of unprotected sex with a man in the six months before enrollment, and also reporting at least one additional HIV risk behavior (either personal or partner). Using venue-based sampling, eligible women were enrolled between May 2009 and July 2010 from 10 communities in six geographic areas of the US (Atlanta, GA; Baltimore, MD; New York City, NY; Newark, NJ; Raleigh-Durham, NC; Washington, DC) | N/A | N/A | N/A |
| Frye, V., Koblin, B., Chin, J., Beard, J., Blaney, S., Halkitis, P. … & Galea, S. (2010) | n = 113 | n = 385 | Ages 23–29 years, reside in one of the five boroughs of New York City or specified contiguous counties in Long Island, and New Jersey; data from the Young Men’s Study 2 (YMS2), or the aged 23–29 cohort of the YMS-NYC data for both the outcome and individual-level covariate data | Demographic characteristics (age, race/ethnicity, education, employment, income, living situation, zip code, psychosocial factors), "outness" (whether the respondent was known to be gay), venue attendance (ever attended circuit parties and frequency of bar/club attendance), lifetime sexual behavior, sexual behavior over the previous 6 months, history of sexually transmitted diseases, history and most recent results of HIV-1 antibody testing, drug and alcohol use in the past 6 months | Age distribution, racial composition, ethnic heterogeneity, foreign-born presence, concentrated poverty, median household income, percent of high school graduates, percent unemployed, residential instability, vacant housing, and neighborhood gay presence (% of households headed by same-sex partners) | HIV-1 antibodies, hepatitis B, syphilis, and frequency of risk behaviors among MSM |
| Frye, V., Nandi, V., Egan, J. E., Cerda, M., Rundle, A., Quinn, J. W. … & Koblin, B. (2017) | n = 87 | n = 766 | Biological male at birth; at least 18 years of age; reside in NYC; report anal sex with a man in the past 3 months; communicate in English or Spanish; and willing and able to give informed consent for the study | Age, education, employment, income, partnership/marital status, income security, lifetime incarceration, self-reported HIV status, ethnic identity, sexual orientation, outness, partnership status, exposure to neighborhood, kin/friend networks in neighborhood, neighborhood involvement, neighborhood attachment, neighborhood engagement, experience of intimate partner violence | Gay presence, homophobia, vacant housing, broken/boarded-up windows, dirty streets/sidewalks, homicide rate, residential stability, ethnic heterogeneity, homicide rate, poverty | Serodiscordant condomless anal intercourse, five or more sex partners |
| Genberg, B. L., Gange, S. J., Go, V. F., Celentano, D. D., Kirk, G. D., Latkin, C. A., & Mehta, S. H. (2011) | Not reported | n = 1697 | Older than 18 years of age, acquired immune deficiency syndrome (AIDS)-free and had a history of injecting at baseline | Sociodemographics, injection history, lifetime medical history, HIV risk behaviors (sexual and drug-related) and drug treatment history, healthcare utilization, life events (incarceration, homelessness) | Neighborhood deprivation (Percentage of individuals employed in professional/managerial occupations, percentage of households with crowding, percentage of households living in poverty, percentage of female-headed households with dependent children (< 18 years), percentage of households on public assistance, percentage of households earning low income, percentage of individuals with less than high school education and percentage of unemployed males and females (> 16 years)) | 3 Consecutive years without self-reported injection drug use |
| Gindi, R. M., Sifakis, F., Sherman, S. G., Towe, V. L., Flynn, C., & Zenilman, J. M. (2011) | n = 48 | n = 307 | Eligible participants were between 18 and 50 years of age; residents anywhere of Baltimore MSA; male or female (not transgender); reported vaginal or anal sex with a person of the opposite sex in the past 12 months; and had the ability to complete the interview in English | Five most recent sexual partners in the past 12 months; sexual partnerships (residential, demographic, and behavioral); partner concurrency behavior; condom use; race; partner race; age range of partner | Census quartiles of poverty; heterosexually transmitted HIV/AIDS case rates for Baltimore City in 2006 | Census tract of participants and their five most recent partners; asked participants to report whether they met partners "in the neighborhood where they live" |
| Haley, D. F., Haardorfer, R., Kramer, M. R., Adimora, A. A., Wingood, G. M., Goswami, N. D., … & Cooper, H. L. F. (2017) | Not reported | N = 737 | WIHS eligibility criteria included ages 25–60 years old. HIV-infected women were ART naïve or HAART after December 31, 2004; never used didanosine, zalcitabine, or stavudine (unless during pregnancy or for pre- or post-exposure HIV prophylaxis); never been on non-HAART ART, and had documented pre-HAART CD4 counts and HIV viral load | Demographics: age, married or cohabitating, race, annual household income ≤ $18,000, self-rated quality of life (QOL), alcohol or illicit substance use exchange of sex for drugs, money or housing, homeless | Social disorder (i.e., vacant housing units, violent crime rate, STI prevalence, poverty, unemployment) and 2) social disadvantage (i.e., renter-occupied housing and alcohol outlet density) | Condomless vaginal intercourse (CVI), anal intercourse (AI), and condomless anal intercourse (CAI) in the past 6 months |
| Heimer, R., Barbour, R., Palacios, W. R., Nichols, L. G., & Grau, L. E. (2014) | Not reported | n = 454 | Self-reported injection drug use within the past 30 days or evidence of injection stigmata, ≥ 18 years of age, proof of residence for at least 6 months in a Fairfield or New Haven County town, willingness to participate, and competence to provide informed consent | Sociodemographics, drug use history, current injection behaviors, medical history, interactions between with substance abuse treatment/ harm reduction services, social support, spirituality, interactions with criminal justice system; depression (CES-D), anxiety (Beck Anxiety Inventory), alcohol use (AUDIT-C), pain (Brief Pain Inventory); HBV antibodies | Community disadvantage index (CDI), income of Census tract | Unsafe injection risk score |
| Kelly, B. C., Carpiano, R. M., Easterbrook, A., & Parsons, J. T. (2012) | n = 125–132 (across five analytic samples) | n = 710 | Gay identity, geographic locale, and HIV status. Men who reported HIV negative or unknown HIV status | Social network variables (socializes with gay men and gay-centric network); attachment to the gay community; age; education; income; race/ethnicity; relationship status; data collection site | Zip code level: gay neighborhoods (local knowledge and Census data); gay enclave; index of concentration at the extremes (ICE); residential stability | Receptive and insertive unprotected anal intercourse (UAI); barebacking identity; recent internet use for finding sexual partners; Party and Play (PnP) |
| Kerr, J. C., Valois, R. F., Siddiqi, A., Vanable, P., & Carey, M. P. (2015) | N/A | n = 1602 | Eligible participants identified as African American between the ages of 14–17 years old and were participants in a HIV risk reduction intervention | Age, sex, racial background, and eligibility for free or reduced price school lunch, STI acquisition, sexual risk behavior; participant reported neighborhood quality (Neighborhood Stress Index) | Region-based neighborhood quality measures (reported by participants and aggregated by location), region-neighborhood quality dyads | STIs and sexual risk behavior |
| Knittel, A. K., Snow, R. C., Riolo, R. L., Griffith, D. M., & Morenoff, J. (2015) | N/A | n = 250 | Stimulated with incarcerated population | N/A; experimental variables in model: sex ratio, male agent quantity distribution | Rates of incarceration | Male agents—probability of incarceration at each time step; mean and standard deviation of a distribution of sentence lengths (in weeks); probability of relationship break-up at the time of incarceration, probability of starting a new relationship while incarcerated, quality measure decreases as a penalty for incarceration |
| Koblin, B. A., Egan, J. E., Rundle, A., Quinn, J., Tieu, H. V., Cerdá, M., … & Frye, V. (2013) | n = 347 | n = 706 | Participants were eligible if they identified as biological male at birth, were 18 years of age or older, resided in NYC, reported engaging in anal sex with a man in the past 3 months, spoke English or Spanish, and were willing and able to give informed consent for the study | Demographics, general and HIV-related health questions (e.g. HIV testing history, occurrence of STIs), history of incarceration and sexual identity, sexual behaviors in the 3 months prior to the study (number of partners, number of insertive and receptive anal sex acts and use of condoms and partner HIV status), self-reported neighborhood characteristics and definition (boundaries) | Borough of residence, neighborhood (pre-defined, historic name), and boundaries; socioeconomic status, housing quality, ethnicity, residential stability, crime rates, and cleanliness of streets and sidewalks, neighborhood safety (geocoded assaults), access to public transportation, land use mix, location and quality of parks, green space, location of recreation facilities, unexpected deaths (geocoded from NYC Medical Examiner) | Sexual risk behaviors, substance use, and depression among MSM in NYC |
| Koblin, B. A., Egan, J. E., Nandi, V., Sang, J. M., Cerda, M., Tieu, H.-V.,... Frye, V. (2017) | n = 347 | n = 1493 | Eligible participants identified as biological male at birth, at least 18 years of age, resided in NYC, reported engaging in anal sex with a man in the past 3 months, communicated in English or Spanish | Age; race/ethnicity; sexual identity; socioeconomic status (education, employment, annual personal income, and financial security); outness (how many of the people you know or see day-to-day know you have sex with men?); gay community attachment; place of birth; place where participant spent most of their life; whether the participant would live in their current home neighborhood if they could live anywhere in NYC; Neighborhood Locator Questionnaire, neighborhood congruence; social ties, neighborhood connectedness, neighborhood lifetime and recent experiences | N/A | Serodiscordant/unknown status condomless anal intercourse (serodiscordant CAI); CAI with partners found using the Internet or mobile application |
| Latkin, C. A., Curry, A. D., Hua, W., & Davey, M. A. (2007) | N/A | n = 838 | 18 years of age or older, daily or weekly contact with drug users, willingness to conduct AIDS outreach education, willingness to bring network members to be interviewed, not currently enrolled in other HIV prevention studies | Demographic characteristics (age, race/ethnicity), HIV status, employment, incarceration, housing, education, use of public assistance; Perkins and Taylor's Block Environmental Inventory, psychological distress (CES-D), sexual risk behaviors (number of partners, sex with someone who used injection drugs, sex with someone who used crack cocaine), injection drug or crack cocaine use | N/A | Psychological distress and sexual risk behavior |
| Lutfi, K., Trepka, M. J., Fennie, K. P., Ibanez, G., & Gladwin, H. (2015) | n = 110 | n = 3643 | Completed the National Survey of Family Growth 2006–2010 survey, identified as non-Hispanic black race | Age, gender, marital status, educational attainment, and income; risky sexual behavior (number of partners in the past 12 months, condom used at last sex, and composite measure of these two) | Census-level: racial residential segregation ( index of dissimilarity, isolation index, relative concentration index, absolute centralization index, spatial proximity index), hypersegregation; CBSA-level: racial residential segregation and poverty | Sexual behaviors |
| Martinez, A. N., Lorvick, J., & Kral, A. H. (2014) | Not reported | n = 1084 | Being aged 18 years or older and drug injection within the past 30 days (self-reported) | HIV serostatus; syringe sharing; non-fatal overdose in the past 12 months; gender (male and female); age (under 30 vs. older age); race/ethnicity; sources of income (government assistance or illegal means) in the past 30 days, years of injection drug use, and homeless status. Arrest history; injection and non-injection drug use (heroin, methamphetamine, and crack smoking); trading sex for cash or drugs, and frequency of syringe exchange program use | Activity spaces: routes, activity space distances, syringe program locations; Census tract: poverty level, dichotomized poverty (high vs low), concentrated poverty | HIV serostatus, syringe sharing, non-fatal overdose |
| Mustanski, B., Birkett, M., Kuhns, L. M., Latkin, C. A., & Muth, S. Q. (2015) | n = 77 | n = 167 (egocentric network) n = 837 (alters) | 16–20 years old, born male, spoke English, had a sexual encounter with a male or identify as gay/bisexual, and available for follow-up for 2 years | Name generator, demographic characteristics (age, race [mutually exclusive], gender, perceived sexual identity, cross streets or neighborhood residence), characteristics of the relationship, and behaviors with that person, sexual behavior from prior 6 months, HIV and STI (gonorrhea and Chlamydia) test results, relationship type, concurrency | HIV prevalence, network density, multiplexity, assortativity by race | Individual and sexual network characteristics |
| Nandi, A., Glass, T. A., Cole, S. R., Chu, H., Galea, S., Celentano, D. D.,... Mehta, S. H. (2010) | n = 174 | n = 1875 | Participants initially recruited into the AIDS Link to Intravenous Experiene (ALIVE) cohort study: individuals were eligible if they reported injection drug use within the past 11 years, were at least 8 years of age, and, were AIDS free upon study enrollment (for HIV-positive participants); added requirement for identifiable address for enrollment in this study | Sociodemographic characteristics (gender, age, race/ethnicity, educational attainment, employment in the formal economy, formal income), drug use characteristics (age at first injection, needle sharing, crack use, shooting gallery attendance), sexual behaviors, medical history (HIV status, presence of any sexually transmitted diseases), health care utilization (methadone treatment usage), and life events (homelessness, jail/incarceration) | Neighborhood poverty levels (% of residents living in poverty) | Drug use cessation |
| Neaigus, A., Jenness, S. M., Reilly, K. H., Youm, Y., Hagan, H., Wendel, T., & Gelpi-Acosta, C. (2016) | n = 42 | n = 494 | Participants must identify as heterosexuals at high risk of HIV (having had vaginal or anal sex with opposite gender partners in the past 12 months), self-identified as male or female, aged 18–60 years, residing in NYC, being able to complete the interview in English or Spanish, and not previously participating in the National HIV Behavioral Surveillance (NHBS) system in the hererosexual cycle (HET2) | Sociodemographic characteristics, drug and alcohol use, sexual risk behaviors and partnerships, and other HIV-related information; blood specimens for HIV antibodies | Zip code of closest street internstion of the place where they last had sex with up to 6 of their most recent partners in the past 12 months; HIV prevalence by NYC communities | N/A |
| Pachankis, J. E., Eldahan, A. I., & Golub, S. A. (2016) | N/A | n = 273 | 18–29 years, having moved to NYC in the past 12 months, and identifying as gay or bisexual man | Sexual identity, education, employment status, class background, relationship status, and HIV status, hometown characteristics—hometown size, outside USA, hometown structural stigma, and hometown interpersonal discrimination | Same-sex couple households (US Census) | HIV transmission risk (condomless vaginal or anal sex with serodiscordant and unknown-status partners), heavy substance use (used marijuana more than once per week on average or any other drug more than once per month), alcohol use (Alcohol Use Disorders Identification test (AUDIT)), depression and anxiety (Brief Symptom Inventory (BSI)) |
| Parrado, E. A., & Flippen, C. (2010) | n = 32 | n = 1446 | Hispanic male immigrants living in one of 32 apartment complexes, who answered the door and were eligible, | Age, years of education, wages, marital status—single men, accompanied married men (who reside with a spouse), and unaccompanied married main (whose wives continue to reside in their communities of origin), | Median wages, the share of migrants who were recently arrives (with less than 3 years in the Durham area), race and ethnicity (to determine the share of the apartment complex population that is not Hispanic) | Self-reported commercial sex worker (CSW) |
| Quinn, K., Voisin, D. R., Bouris, A., & Schneider, J. (2016) | N/A | n = 92 | Being born biologically male, self-identifying as Black or African American, between the ages of 18 and 29, inclusive, having an HIV diagnosis for greater than three months, and having disclosed their status to at least one person in their close social network | Demographic characteristics (age, race/ethnicity), education, employment; participant reported exposure to community violence (Exposure to Violence Probe) | N/A | Substance use (frequency of substance use in the past 3 months), medication adherence (currently taking ARVs, medications prescribed for HIV, number of days with missed medication in the past 30 days, percent of days medication was taken in the past 30 days), psychological distress (Brief Symptom Inventory (BSI)—18), sexual risk behaviors (use of substances for sex, condomless anal intercourse) |
| Raymond, H. F., Al-Tayyib, A., Neaigus, A., Reilly, K. H., Braunstein, S., Brady, K. A., … & German, D. (2017) | n = 13 | n = 6137 | Participants identified as 18 years or older, lived in one of the study cities, and reported ever having had sex with a man | Transmission risk group variables: sexual partners (only having male partners; male and female partners; female partners only but identified as gay/bisexual), sexual orentation; IDU as only risk; male and female partners and IDU; IDU and male partners; female partners and IDU; none of the above behaviors in the past 12 months | HIV case reporting data; city poverty level; race/ethnicty | Transmission risk behaviors; HIV case reporting data |
| Raymond, H. F., Chen, Y. H., Same, S. L., Catalano, R., Hutson, M. A., & McFarland, W. (2014) | N/A | n = 523 | 18 or older, identify as Black, has valid study referral coupon, identify as gay or bisexual or has had at least 1 male partner in the pas 12 month, male, resident of San Francisco | Race, age, income, education, neighborhood of residence, often risk taking, per contact risk of acquiring HIV, sexual behavior, stimulant, SES | Neighborhood HIV prevalence | HIV acquisition risk from sex and drug use |
| Rothenberg, R. B., Dai, D., Adams, M. A., & Heath, J. W. (2017) | Not reported | n = 927 |
18 years or older, being involved in HIV risk- taking, either through use of drugs or sexual activity, and who communicated a willingness to name and discuss their partners |
Age, race, marital status, education, religious affiliation, employment, homelessness, sources of income, criminal justice system involvement, threatened with weapon, general health status, sexual orientation, STD history, drug use, sexual behavior | Compound risk indicator (e.g. number of sex partners, injection drug use, anal sex, sex with IDU, sex work); geographic areas delineated by higher and lower risk | Social and geographic distance (network) |
| Rudolph, A. E., Crawford, N. D., Latkin, C., Fowler, J. H., & Fuller, C. M. (2013) | Not reported | n = 378 | 18–40 years old and were active injection or non-injection drug users | Demographics, network characteristics and relationships, drug use and sex behaviors, and health service use | Minority composition, educational attainment, unemployment, income/poverty, inequality, and crowding | Membership in high HIV prevalence drug networks |
| Rudolph, A. E., Linton, S., Dyer, T. P., & Latkin, C. (2013) | Not reported | n = 417 | Females (18–55 years of age) who had not injected drugs in the past 6 months, self-reported heterosexual sex in the past 6 months, and had > = 1 of the following sexual risk factors: (A) > 2 partners in the past 6 months, (b) STD diagnosis in the past 6 months, or (c) a high-risk sex partner in the past 90 days/ | Age, race (African American vs. other), incarceration in the past 6 months, weekly alcohol use, employment status in the past 6 months, HIV status, marital status, current main sex partner, cocaine metabolites, opiate metabolites, education, heroin use in the past 6 months, crack/cocaine use in the past 6 months, and homelessness in the past 6 months, social network, sexual network; perception of neighborhood | N/A | Exchange sex |
| Senn, T. E., Walsh, J. L., & Carey, M. P. (2016) | Not reported | n = 1010 | Age 16 or older, engaged in sexual risk behavior in the past 3 months | Sex, age, race, income, education, employment, health behaviors, exposure to violence | Per capita income in the Census tract, percentage of individuals with a college education in the Census tract, | Community violence with sexual risk behavior |
| Sterk, C. E., Elifson, K. W., & Theall, K. P. (2007) | N/A | n = 65 | Eligible participants were 18 years or older; identified as heterosexually active African American women who reported drug use; resided in one of the study communities; reported that they were out of drug treatment or any other institutional setting, spoke English, and reported HIV-negative status. Participants also were eligible if they had vaginal sex with a man at least once during the month prior to the interview and reported active drug use | N/A | N/A | N/A |
| Stevens, R., Gilliard‐Matthews, S., Nilsen, M., Malven, E., & Dunaev, J. (2014) | N/A | n = 30 | 13 to 24 year old females, English speaking, living in the study city, and self-identified as African American and/or Latina | N/A | N/A | N/A |
| Stevens, R., Icard, L., Jemmott, J. B., O'Leary, A., Rutledge, S., Hsu, J., & Stephens-Shields, A. (2017) | n = 321 | n = 564 | Men were eligible to participate if they were at least 18 years of age, self-identified as black or African American, were born a male, and reported having anal intercourse with a man in the previous 90 days | High school non-completion, income, and problem drug use | High school non-completion, neighborhood socioeconomic characteristics | Transactional sex |
| Tobin, K. E., Latkin, C. A., & Curriero, F. C. (2014) | n = 1 | n = 51 | Participants were eligible if they were ages 18 years old or older; self-reported African American race/ethnicity; self-reported male sex; self-reported sex with a male in the prior 90 days; reported living address within Baltimore City | Age, highest educational attainment, current employment status, sexual identity; HIV status, sexual orientation, employment status, whether the network knows that the Index has sex with men; where they spend their time; relationship/attribute items for place-based socio-spatial inventory (see neighborhood measures) | Street intersections and latitude/longitude of: places of residence, socializing, meeting with sex partners and work; drug and alcohol use places within Baltimore City (spatial clustering) | Social network characteristics of drug and alcohol use |
| Tobin, K. E., Hester, L., Davey-Rothwell, M. A., & Latkin, C. A. (2012) | Not reported | n = 720 | Eligible participants were 18 years and older, self-reported injection drug use in the prior 6 months, reported current drug use, or sex partner of study referent | Age, sexual identity, employment, homeless, incarceration, injection drug use, crack use, sex exchange, peer norms regarding sex exchange | Median household income, percent minority, percent rental, percent in labor force, violent crime | Sex exchange (having sex in exchange for drugs, money, food or shelter in the prior 90 days) |
| Voisin, D. R., Hotton, A. L., & Neilands, T. B. (2014) | N/A | n = 563 | Students were eligible for participation in the study if they self-identified as African American, were between the ages of 13–19 years, and were attending regular high school classes (i.e., non-special education classes) | Gender, exposure community violence, student–teacher connectedness (Student Assessment of Teachers Scale), school engagement (GPA), Risky peer norms, History of gang involvement, internalizing or externalizing behaviors and withdrawal (Youth Self-Report (YSR) Survey), PTSD (University of California at Lost Angeles' PTSD Reaction Index (UCLARI)), negative perceptions of peer attitudes about safer sex, gang membership, sexual behaviors | N/A | Sexual behaviors |
| Williams, C. T., & Latkin, C. A. (2007) | n = 249 | n = 1305 | Participants were eligible for this study if they were at least 18 years old; having regular contact with drug users; willingness to conduct peer outreach; and willingness to bring in 1 to 2 network members | Age, gender, education, employment, and income (control variables); participant's partner score on a depression screening instrument, and self-reported HIV status; depressive symptoms (CES-D); drug use; and network inventory (characteristics of total network) (not reported but sample was primarily African American) | Percent in poverty, percent receiving public assistance, percent unemployment, percent with low educational level, percent female-headed households, median household income, neighborhood disadvantage (as a composite measure), percent of persons not in the labor force, percent vacant housing, percent of blue collar and professional occupations, percent renters, and percent disabled | Any use (versus no use) of heroin, cocaine, or crack within the past year |
Relationships Between Neighborhood-Level Factors and HIV Vulnerability
Multiple neighborhood-level factors were associated with heightened HIV vulnerability, but this relationship varied by key factors including how neighborhood condition was defined (objective vs subjective) and whether HIV vulnerabilities stemmed from drug use or sexual risk behavior (see Table 4).
Table 4.
Study results and future directions
| Article citation | Sample description | Key findings/conclusions | Future directions |
|---|---|---|---|
| Akers, A. Y., Muhammad, M. R., & Corbie-Smith, G. (2011) | 42 participants in general adult group, 13 formerly incarcerated, and 38 adolescents and young adults; larger proportion of women in general adult and adolescent/young adult groups; general adult population had higher educational attainment than formerly incarcerated adults; formerly incarcerated adults on average under than general adults most participants made less than $40,000 for an annual income | Absence of recreational options & limited safe environments for socializing for community, adolescent focused themes: lack of diverse leisure-time activities, few recreational options for dating, access to inappropriate leisure activities promoting risk behaviors, cost-barriers to recreational activities, inadequate parental supervision of time alone and with opposite-sex friends, and poor community monitoring of social activities; developed conceptual model linking neighborhood social and structural organization that may contribute to adolescent sexual behaviors | Focus group findings contributed to the development of a conceptual framework and findings of this study can inform future interventions that are specific to the neighborhood and community context |
| Bauermeister J.A., Eaton L., Andrzejewski J., Loveluck J., VanHemert W., Pingel, E.S. (2015) | Sample predominately Black, gay-identified, Above federal poverty level, and not in a relationship | HIV testing associated with greater socioeconomic neighborhood disadvantage, being black, being in a relationship, and community acceptance. Participants less likely to test reporting individual poverty and longer distance to ASO. UAI with serodiscordant partner associated alcohol use, poverty, distance and from ASO. Protective factors for UAI: neighborhood socioeconomic disadvantage and being in a relationship | Examine whether HIV-related correlates vary based on whether YMSMS live in closer proximity to areas with greater concentrations of ASOs and venues servicing LGBT clientele |
| Bauermeister, J. A., Zimmerman, M. A., & Caldwell, C. H. (2011) | Average age about 15 years old; less than half (42.6%) live with mother or mother and siblings; 14.51% reported households that were receiving public assistance and 21.42% of households were earning less than $15,000; 8.98% of participants lived in a household without a high school degree | No direct association between initial condom use scores and proportions of households with less than a high school degree or with varying unemployment rates; no indirect relationship between neighborhood disadvantage and condom use over time; neighborhood disadvantage associated with more consistent condom use | Future studies will be conducted to explore how positive and negative neighborhood characteristics influence youths' sexual behaviors in order to develop community-level HIV/STI prevention programs |
| Biello, K. B., Niccolai, L., Kershaw, T. S., Lin, H., & Ickovics, J. (2013) | Participants ages ranged from 14–27, with the greatest proportion of participants aged 17–21 years old. A total of 1388 participants lived in hypersegregated areas, with 647 of these individuals identifying as Black non-Hispanic and 741 identifying as White, non-Hispanic. 3195 participants resided in non-hypersegregrated areas, and 1183 of these individuals identified as Black, non-Hispanic while 2012 identified as White, non-Hispanic | Sexual risk behavior scores increased as participants aged into adolescense, scores leveled off and decreased by mid 20s; African Americans initially at higher risk than Caucasians; Caucasian risk increased over time to surpass African American sexual risk scores; hypersegregation was not associated with increased sexual risk scores nor did it modify the trajectory of sexual risk scores over time | Future research should explore whether segregation is associated with sexual networks and if networks mediate the relationship between segregation and STIs; future studies will examine whether concurrency and sex with casual and high-risk partners is associated with segregation |
| Bluthenthal, R. N., Do, D. P., Finch, B., Martinez, A., Edlin, B. R., & Kral, A. H. (2007) | Sample predominantly male (> 70%), minorities (> 60%), with low paying employment (15%), high experiences of homelessness (50%), and moderate HIV prevalence (11%) | Unadjusted models indicate that there is a statistically significant relationship between community economic and racial factors and receptive and distributive syringe sharing outcomes, but do not account for differences across tracts; adjusted models demonstrated that percent African American had an effect on syringe sharing (less syringe sharing) and unprotected sex (lower odds of unprotected sex) | Research investigating proximal measures of HIV risk behaviors, such as the presence of prostitutes, shooting galleries, crack houses, drug markets, and incidence of drug users, can provide meaningful information to understanding community context; further research is needed to determine risk and protective factors for HIV at the community level |
| Bobashev, G. V., Zule, W. A., Osilla, K. C., Kline, T. L., & Wechsberg, W. M. (2009) | Majority of sample identified as male in both syringe sharing (71.1%) and sexual behavior (69.5) sample groups; mean age was around 43 years old; majority of sample either identified as African American or White for both groups; about half of participants in either group reported homelessness and about 15% of syringe sharing and 16% of sexual behavior samples reported that paid work was their main source of income | Homelessness, history of injection, bisexual behavior, forced first sexual encounter, and perceived neighborhood violence associated with increased odds of males selling sex; homelessness, history of incarceration, history of injection, elevated substance use, bisexual behavior, forced first sexual encounter, elevated psychological distress, and elevated perceived neighborhood disorder and perceived neighborhood violence associated with males purchasing sex | Respondent driven recruitment can be an effective strategy for recruiting drug users and MSM in rural and urban settings; further research is needed to understand the relationship between bisexual behavior and transactional sex to see if transactional sex promotes the spread of HIV and STIs to other groups in the general population |
| Bowleg, L., Neilands, T. B., Tabb, L. P., Burkholder, G. J., Malebranche, D. J., & Tschann, J. M. (2014) | Age: M = 28.8, SD = 7.75; 63% of participants reported as having high school education, a GED or less; almost half (48%) made < $10,000 and majority (64%) unemployed | Results suggest that variability in sexual risk is explained by direct influences of neighborhood context, depression, and substance use, with neighborhood context influencing sexual risk behaviors through substance abuse indirectly | Future interventions to reduce sexual risk require consideration of social-structural level variables that influence sexual risk behaviors |
| Boyer, C. B., Greenberg, L., Chutuape, K., Walker, B., Monte, D., Kirk, J.,... & Adolescent Med Trials, N. (2017) | The median age of participants was 21.0 years; 42.2% were males, and 4.6% were transgender (most reported a birth sex of male). Almost one-third (32.1%) identified as gay or lesbian and 18.1% identified as bisexual. The majority (66.2%) of participants identified as Black, non-Hispanic and 21.0% identified as Hispanic. A small number (1.3%) of participants were ‘living on the street’. One-third (29.5%) had experienced homelessness. Roughly 16.% of participants reported exchanged sex, 13% had sex with someone they knew to be HIV-infected, 8% had sex with someone who injected drugs, and 1.3% also injected drugs. One-third of participants (32.1%) reported a history of having an STI, and 83% tested for HIV previously | Multivariate comparisons identified a variety of characteristics-being male or transgender, homelessness, sex with a partner who has HIV, STI history, unemployment, reduced job training access, housing instability, crime victimization, perceived community norms of exchanged sex- as significantly associated with increased exchange of sex (p < 0.05) | More research targeting adolescents and young adults to address initiation of transactional sex, conditions in which it occurs, and frequency and length of warranted exchange sex. Longitudinal studies on predictors of transactional sex |
| Braine, N., Acker, C., Goldblatt, C., Yi, H., Friedman, S., & DesJarlais, D. C. (2008) | Black participants (n = 101) statistically significantly (p < 0.001) older (average age = 40.6), less likely to have completed high school (53%), have ever been incarcerated (87%) as compared to their white counterparts (n = 50) in this study (average age = 32.0, high school graduates = 94%, ever incarcerated = 44%) | Hill District contains significant and visible drug market activity for both white and black participants; neighborhood of residence reflects historical patterns of racial segregation of Pittsburgh; strong pattern within social networks of syringes flowing from blacks to whites (93% of black-white dyads and 70% of white-black dyads involve whites receiving syringes from blacks) | This study illustrated that IDUs maintain long-term social networks across neighborhoods within urban settings and can use them to reduce the risk of HIV transmission |
| Brawner B.M., Reason J.L., Hanlon K., Guthrie B., Schensul J.J. (2017) | Participants included three administrators, three direct HIV/AIDS service providers and four community members. All participants were African American; nine women and one man. Mean age: 31.3 years. All participants had a high school diploma or general educational development (GED) certificate; 3 completed postgraduate work. 90% of participants employed. Four participants had annual household income less than $40,000. 3 received public assistance | Geographic and social constraints can increase HIV risk by constraining selection pool of potential partners to locales with elevated HIV burden. Black neighborhoods have abundance of bars, liquor stores and welfare offices, but lack relevant resources such as health centers. There are a lack of resources to combat HIV in the areas that need them the most. Racial segregation concentrates Black people into areas with elevated HIV burden | Community-level HIV prevention approaches have potential to reduce multilevel influences of the HIV epidemic and these approaches should involve stakeholders in the process |
| Brawner, B. M., Guthrie, B., Stevens, R., Taylor, L., Eberhart, M., & Schensul, J. J. (2017) | Compared to predominately white tracts, predominantly black tracts had lower percentages of residents with GEDs, higher unemployment, and higher percentages of persons living below federal poverty level. Among HIV/AIDS cases (N = 319), male-to-male sexual transmission was predominant mode of transmission (59.9%). 14.7% of cases attributable to IDU. Cases predominately male (80.3%), black (47.3%), and mean age of 48.1. Most recently mean CD4 count was 117 (SD = 133) | Lower odds hetero transmission (vs. IDU) for Census tracts with high HIV prevalence among Blacks compared to tracts with high HIV prevalence of Whites (OR: 0.25) Females more likely for hetero vs IDU (OR: 5.3). Compared to privately insured/HMO, Medicaid and uninsured less likely for MTM vs IDU (OR 0.04 and OR 0.07), respectively). Blacks more likely (OR 7.43) for hetero vs MTM. Medicaid more likely for hetero vs MTM transmission (OR 9.69) than privately insured/HMO. Odds of IDU vs MTM transmission higher among Medicaid (OR 22.85) and uninsured (OR 14.40), respectively | Findings can be used to guide larger studies for the development of future neighborhood-level structural interventions. Develop risk-reduction programming considering the ways in which neighborhood characteristics may be influenced by dominant risk behaviors (e.g., opening a needle exchange program in an area with high IDU prevalence) |
| Buot, M. L. G., Docena, J. P., Ratemo, B. K., Bittner, M. J., Burlew, J. T., Nuritdinov, A. R., & Robbins, J. R. (2014) | N/A | Income inequality, poverty, and racial segregation were significant predictors of HIV incidence in 2000; High income inequality, low incomes, high unemployment, high poverty, low home ownership, and high cost of living correlated positively with HIV incidence, risk increased by 2–threefold; low rates of marriage within cities demonstrated roughly fourfold higher HIV rates; Rates by heterosexual contact were significantly associated with income inequality, poverty, education, and segregation; MSM risk is associated with income inequality, poverty and segregation (at lower values) | Future intervention efforts should view the continuation of the HIV epidemic as a set of recurring structural circumstances that select for viral transmission |
| Buttram, M. E., & Kurtz, S. P. (2013) | Residents in the gay neighborhood (Wilton Manors) tended to be older, white, and slightly more educated than other areas of Miami/Ft- Lauderdale | Methamphetamine use, increased reported receptive UAI, and decreased reported prosocial participation were found to be associated with gay neighborhood residence; gay neighborhood residence appeared to be protective against cocaine use and substance dependence | Future research should examine how men decide to move to a gay neighborhood versus other locations, and how they experience living in different types of neighborhoods, which can inform how risk and protective factors associated with varying neighborhood contexts |
| Cené, C. W., Akers, A. Y., Lloyd, S. W., Albritton, T., Powell Hammond, W., & Corbie-Smith, G. (2011) | 4 samples: focus groups—individuals age 16–24, individuals age 25 and older, the formerly incarcerated. Interviews: participants deemed by community partners as knowledgeable about HIV risk and prevention | Four themes emerged impacting HIV vulnerability: Interpersonal processes (social cohesion, social tension, and HIV-related stigma), community structural factors (availability of resources, accessibility of resources, segregation, political forces, & institutional racism) social disorder, and civic engagement. Stigma, lack of community resources (for example funding to address HIV), and lack of care access led to risk behaviors (as escapism), resources to adequately address HIV at the structural level and inhibited HIV prevention (like testing) | Clinicians should consider assessing social histories of patients to tailor treatment recommendations |
| Cooper, H. L., Friedman, S. R., Tempalski, B., & Friedman, R. (2007) | Of MSAs, 79% had residents that identified as White, Non-Hispanic; MSAs fairly evenly distributed across geographic regions (Northeast, South, Midwest, and West) of the US. The median adult population was 720,975 per MSA | Median injection drug use prevalence was 1983 per 100,000 Black adults (interquartile range: 1422 to 2759 per 100,000). Median isolation index was 0.48 (range: 0.05 to 0.84). Average Black resident in this study resided a Census tract where 48% or greater were also Black. An increase of 0.50 in racial isolation was associated with a 23% increase in injection drug use prevalence among Black adults. Racial concentration was unrelated to injection drug use prevalence among Black adults | Future studies should examine the pathways through which increased racial isolation is associated with injection drug use prevalence; examination of other racial/ethnic groups should be conducted as well; future research should also explore the extent to which racial isolation influences the distribution if injection drug use and related health problems among urban Black populations |
| Cooper, H. L., Linton, S., Haley, D. F., Kelley, M. E., Dauria, E. F., Karnes, C. C., … & Adimora, A. (2015) | Participants were mostly women with a mean age of 43 years old; high poverty (mean annual income $9849) at baseline | Mean poverty rate in tracts in which public housing complexes occurred (46%) was higher than the mean poverty rate in tracts that participants moved to (30.2%). Perceived partner declined after individuals relocated from housing complexes; decreased perceived partner risk was associated with reduced violent crime rates and reduced perceived community violence | Future research must contribute to efforts to diminish place-based inequalities to eliminate disparities |
| Cooper, H. L., Linton, S., Kelley, M. E., Ross, Z., Wolfe, M. E., Chen, Y. T., … & Semaan, S. (2016) | The sample lived in 15 states, 19 MSAs, 51 counties, and 969 zip codes. About half (51.79%) of the participants were black 30.24% were white, and 17.97% were Latino. About a quarter (28.40%) of this sample was female and the average age was 45.76 (SD = 10.55). Most participants were impoverished and 39.80% were currently homeless. Participants had injected drugs for an average of 23.27 years (SD = 12.98); primarily injected heroin; and most injected more than once a day. HIV serostatus varied by race/ethnicity, with 10.70% of black PWID, 7.60% of Latino PWID, and 6.24% of white PWID testing positive. Participants were mostly women with a mean age of 43 years old; high poverty (mean annual income $9849) at baseline | Black PWID were more likely than white PWID to live in environments associated with vulnerability to adverse HIV-related outcomes; black PWID lived in ZIP codes with higher poverty rates and worse spatial access to substance abuse treatment and in counties with higher violent crime rates; Black PWID were less likely to live in states with laws facilitating sterile syringe access (e.g., laws permitting over-the-counter syringe sales);. Latino/ white differences in risk environments emerged at the MSA level (e.g., Latino PWID lived in MSAs with higher drug-related arrest rates) | Future research should assess the extent to which varying environmental exposures are associated with disparities in HIV-related outcomes among IDUs |
| Crawford, N. D., Borrell, L. N., Galea, S., Ford, C., Latkin, C., & Fuller, C. M. (2013) | Most participants were more likely to be black and Hispanic, male, lower socio-economic status and un-married. The majority of the sample did not inject drugs and used crack cocaine. The median number of female and male sex partners was 1 (IQR: 0–2) and 0 (IQR: 0–1), and most participants used condoms infrequently regardless of the partner’s gender. The median age at sexual debut was 14 (IQR: 12 – 16) and most participants received four or more HIV tests in their lifetime. Most experienced depression in their lifetime | Experiencing discrimination due to drug use associated with drug ties in neighborhoods with fewer blacks. Communities with lower educational attainment associated with greater drug using and heroin/injecting ties | Future research should examine how neighborhood context impacts relationships regarding discrimination and development of high risk-relationships and tailor interventions to address social discrimination |
| DePadilla, L., Elifson, K. W., & Sterk, C. E. (2012) | Sample was split equally based on gender (49% men and 51% women) and 51% were older than 35 years old | Age 35 or older, alcohol use, steady partnership, having never been homeless, and perceived neighborhood disorder were associated with increased odds of lack of condom use when engaging in vaginal sex in the past 30 days. Crack/cocaine use, marijuana use, increased social cohesion, consistent health insurance, and having more than one steady partner were negatively associated with a lack of condom use in the past 30 days | Social science research should recognize the importance of epidemiological information in the larger socio-political and ecological context in future studies |
| Duncan, D. T., Kapadia, F., & Halkitis, P. N. (2014) | Of the five New York City boroughs, 32% and 15% of participants reported residence in Manhattan or Brooklyn, while approximately 10% reported either The Bronx or Queens as their borough of residence | About two-thirds of participants reported concordance between residential/socializing, residential/sex, and sex/socializing boroughs, while 25% reported concordance between all three residential, socializing, and sex boroughs. Borough concordance varied by some individual-level characteristics. YMSM who reported experiencing gay-related stigma in public forums were more likely to report discordant socializing/sex and residential/socializing/sex boroughs (p < 0.001). YMSM who reported residential/socializing/sex borough concordance were more likely to report recent (last 30 days) alcohol use, recent marijuana use, and recently engaging in condomless oral sex (all p < 0.05) | Future research among YMSM populations should consider multiple neighborhood contexts in order to provide a more nuanced understanding of how and which neighborhood contexts influence the health and well-being of YMSM |
| Participants had high education, low income, and high levels of substance dependence, mental health problems, HIV infection and ongoing sex risk | Men who lived in South Florida for greater than one year had a statistically significant greater number of friends who use drugs (t = -2.82, p = .005) and greater proportion who were HIV positive (t = -2.43, p = .02); me who resided in South Florida for 1–5 years reported a statistically significantly greater number of unprotected anal intercourse in the past 90 days than those who resided in that area for less than one year (t = -2.69, p = .009) | Future interventions should focus on the immediate post-migration period and incorporate skills and needs for social relationships with the broader community | |
| Egan, J. E., Frye, V., Kurtz, S. P., Latkin, C., Chen, M., Tobin, K., … & Koblin, B. A. (2011) | Mean age was 34 years old; participants identified as Latino (30%), African American (30%), multiracial (20%), white (15%), or Asian American (5%); seven men were HIV positive | Both men who were born in NYC or migrated to it sought neighborhoods with reduced discrimination and more social opportunities; those who grew up outside of Manhattan but in NYC described anti-gay and homophobic attitudes in their original neighborhoods; the importance of community engagement within their residential neighborhood varied greatly among participants, with participants describing the positive (acceptance, reduced oppression) and negative (increased availability of sex and drugs, social pressures to conform to norms of appearance/conduct, lack of affordability of housing) aspects. Men who traveled between gay neighborhoods often modified their behavior based on their location (gay neighborhood vs other neighborhoods) and who they were with (gay friends vs others); some men felt excluded from the gay neighborhood (Chelsea) related to race/ethnicity stereotypes of who lives there (white, middle-class, stylish, fit men) | Research regarding the relations among behaviors and neighborhoods can contribute to geographically specific and norms-based health outreach and programs |
| Participants reported sociodemographic disadvantage with 79.68% having ever been incarcerated in life and only 27.7% working full or part time and only 46.3% have an income of more than $10,000 | more than half of participants reported sexual partners outside of their neighborhood and about 20% had a partner living in the same neighborhood but not the same household; the average number of sexual partners was about 3, with no statistically significant difference in the number of partners based on whether or not partners lived in the same household (p = 0.99); participants living with their sexual partners report statistically significant greater financial dependence on partners (p = 0.004) | Studies should explore the relationship between residential location of partners and co-habitation, with mental and physical health outcomes, such as HIV care and support for medication adherence | |
| Frew, P. M., Parker, K., Vo, L., Haley, D., O'Leary, A., Diallo, D. D., … & Hodder, S. (2016) | The median age of the women in our sample was 27 years. Most women in the sample were Black/African American (86%, n = 247) and reported having a “non-partnered” single status (67%, n = 194) | Perceived discrimination inhibits efforts to target African American communities for initiatives to address HIV risk reduction. An imbalance of available male sexual partners in communities also increases HIV vulnerability. Individuals from disadvantaged communities engage in survival sex to achieve basic needs | Programs emphasizing financial education and resources and those potentially addressing microfinance opportunities in the community may facilitate greater access to prevention education. Multilevel interventions focused on finance and empowerment education focusing on sexual concurrency, IPV, and HIV risk behavior have potential for addressing HIV vulnerability among this population |
| Frye, V., Koblin, B., Chin, J., Beard, J., Blaney, S., Halkitis, P., … & Galea, S. (2010) | About 40% of this sample was between 23–24 years old; 31% identified as Hispanic, 30% identified as Black, 21% identified as White and 18% identified as Other; a majority of participants were post-high school graduates (27%) or have completed college or more education (44%); only 16% of participants earned $40 k or more | Roughly half of the sample’s respondents were consistent condom users during both receptive and insertive anal intercourse; living with a partner and sex while high or buzzed on drugs were negatively associated with consistent condom use | Investigators must explore factors "upstream" and around at the social and physical context that constitutes the risk environment for MSM. Multi-level studies of the neighborhood environment are crucial to these efforts, as are qualitative inquiries into the lived experience of the neighborhood and how this relates to sexual behavior |
| Frye, V., Nandi, V., Egan, J. E., Cerda, M., Rundle, A., Quinn, J. W., … & Koblin, B. (2017) | Mean age Black: 32 years. Mean age White: 34 years. 25% & 4% of Black & white participants (respectively) had high school degree/GED or less; 44% & 17% of Black & white participants were unemployed. 37% & 12% of Black & white participants had annual income below $10,000. Almost 9% & 2% of Black & white participants (respectively) had incarceration history. 4.5% & 5% of Black & white participants were married or partnered (with a man) | This study found little evidence to support the association between social disorganization and sexual risk behaviors among MSM. Less physical disorder and ethnic heterogeneity in neighborhoods protective against condomless anal sex with serodiscordant partner among Black MSM. Cleaner neighborhoods indicate higher risk for White MSM | Future studies should examine how non-geographically bounded communities (e.g. social networks) and neighborhood characteristics closer to actual sex acts |
| Genberg, B. L., Gange, S. J., Go, V. F., Celentano, D. D., Kirk, G. D., Latkin, C. A., & Mehta, S. H. (2011) | 75% male, 95% African American, 57% did not have a high school diploma. 66% never married. Median age was 35 years. Median years injected was 14. Approximately 50% reported injection daily or more frequently. 65% injected heroin & cocaine (speedball). 58% resided in most deprived (4th quartile) neighborhoods | Drug cessation significantly less likely to occur to happen in most deprived neighborhoods. Moving from deprived neighborhoods increased odds of cessation | Examine appropriateness of 3 years as a measure of long-term changes in behaviors. Determine mechanisms through which relocation and neighborhood deprivation impact long-term changes in drug use |
| Gindi, R. M., Sifakis, F., Sherman, S. G., Towe, V. L., Flynn, C., & Zenilman, J. M. (2011) | Majority of the 307 participants were black, they were evenly divided by gender and had a mean age of 33 years. One-third (34%) lived in the Census tracts in the top quartile of HIV/AIDS case rates in Baltimore City. Almost half (43%) reported 3 or more partners in the past 12 months. Casual partnerships were most common (44%), with 39% of partnerships classified as main and 16% as exchange. Participants reported concurrency in 67% of partnerships and suspected partner concurrency in 56% of partnerships | Almost half the population reported choosing spatially assortative partners. Participants living in HIV core areas more likely to choose spatially assortative partners than residents of non-core areas after adjusting for partnership type, gender, & number of partners. Women engaging in exchange sex most likely to report spatial assortativity. Contextual factors that may impact geography of partner selection include access to public transportation, residential segregation, natural boundaries (rivers & roads) & access to social institutions that create meeting opportunities | There is a need for more research on geographical and contextual factors in HIV/STD prevention. Capitalize on the spatial proximity of partners in high-prevalence areas by supplementing individual focus messages with social marketing campaigns. Shared geographical space may be the underlying mechanism by which social norms are developed in a network. So there is a need to assess the impact of social norms and attitudes on sexual behavior based on geographical context |
| Haley, D. F., Haardorfer, R., Kramer, M. R., Adimora, A. A., Wingood, G. M., Goswami, N. D., … & Cooper, H. L. F. (2017) | Average age: 44 years old. 83% African American, 67% had annual household incomes of ≤ $18,000. 72% HIV-infected. 42% reported condomless vaginal intercourse, 7% reported anal intercourse, and 4% reported condomless anal intercourse in the last 6 months. On average, participants lived in Census tracts where 16% of residents were unemployed, 29% lived in poverty, and roughly half of housing units were renter-occupied | Social disorder and social disadvantage not associated with condomless vaginal intercourse. Greater social disorder was associated with less anal intercourse and condomless anal intercourse | Longitudinal and qualitative studies needed to establish the causality of relationships and to better understand pathways through which neighborhood characteristics shape sexual risk, and inform development of future multilevel interventions to improve and reduce HIV/STI transmission |
| Heimer, R., Barbour, R., Palacios, W. R., Nichols, L. G., & Grau, L. E. (2014) | Sample was 62.1% male, 81.9% White, 9.7& Hispanic, 6.3% African American | Injection drug users in more economically disadvantaged areas are engaging in more HIV risk behaviors than those in the neighboring suburban communities. In more disadvantaged areas, there is less access to harm reduction services and less awareness and education about injection-associated diseases | Comprehensive, integrated programs are needed to improve public health responses for injection drug users, and should include a dual-diagnosis approach to providing harm reduction service |
| Kelly, B. C., Carpiano, R. M., Easterbrook, A., & Parsons, J. T. (2012) | Five analytic samples (one for each outcome within the last 3 months), which ranged in size from 584 (82.3%) and 661 (931.1%). Any insertive (585); any receptive (584); barebacker identity (661); Party and play (641); and meet a man via internet for sex (621) | Gay enclave (a substantially gay population, gay institutions, and conspicuous gay subcultures. Levine (1979)) residents were not directly associated with sexual risk behaviors but with PnP. Having a gay-centric network was associated with higher odds of engaging in IAI, engaging in PnP, and using the internet to find sexual partners. Social networks has the highest impact of determining participation in risky sexual behaviors | A better contextualization of health risk that moves beyond a focus on individual-level factors and considers the role of the social contexts in which the gay community's health behaviors take place |
| Kerr, J. C., Valois, R. F., Siddiqi, A., Vanable, P., & Carey, M. P. (2015) | African American adolescents between the ages of 14 and 17, the majority of the sample were and females (59%); mean age of the sample was 15.1. The majority of the sample was low income as 76% of the sample qualified for free or reduced price school lunch | Participants from the Southeastern communities had higher risk for HIV/STI. Of the neighborhood dyads, participant-reported low quality neighborhoods faced greater risk of STI/HIV | Further examine the relationship between region and neighborhood with probability samples and qualitative research |
| Knittel, A. K., Snow, R. C., Riolo, R. L., Griffith, D. M., & Morenoff, J. (2015) | N/A; data for model development was obtained from African American residents of 270 metropolitan areas defined in the 1980 US Census; men in the labor force and non-institutionalized women | When community incarceration rates are high, there is an increase in the number of sexual partnerships at the community level over five years. This may explain differences in the numbers of sexual partners, increased rates of STDs and HIV observed in these communities. There is more of an effect for men than women | Policy's that reform the criminal justice system that enable the maintenance of inmate's relationships with partners and family to reduce the instability of partnerships for men who have been incarcerated. Ways to decrease the cost of relationship maintenance |
| Koblin, B. A., Egan, J. E., Rundle, A., Quinn, J., Tieu, H. V., Cerdá, M., … & Frye, V. (2013) | The average age was 32.4, 34% of the sample was white; 31% Hispanic, 23% Black/African American; and 11% another ethnicity. 31% were born in NYC, over 50% of men reported possessing at least a college degree, 5% reported a lifetime history of incarceration | MSM influenced by the environments in which they socialize and have sex as well as the duration and intensity of exposure to neighborhood environments. Men perceived their home, social and sexual neighborhoods in different ways. They identified their social neighborhoods as being the largest while the size of their sexual neighborhoods was the smallest | The research provides groundwork for the development of structural and neighborhood-based interventions, as well as for identifying approaches that augment individual-level interventions through community development initiatives and health messages for MSM specific to their neighborhood context |
| Koblin, B. A., Egan, J. E., Nandi, V., Sang, J. M., Cerda, M., Tieu, H.-V.,... Frye, V. (2017) | Average age 32.1 (SD = 103); 31.9% White (non-Hispanic); 30.4% Latino; 25.2% Black/African American; 12.5% reported another race/ethnicity; men (87.3%) self-identified as gay, homosexual, queer, or same-gender loving; 49.3% have at least a college degree; 63.3% were employed; 26.3% average personal income of less than $10,000 per year, 47.9% they did not have enough money for necessities in the prior 3 months | Most men in study report incongruence among neighborhoods—1 in 6 reported complete congruence among home, social, and sex neighborhoods. Risk behaviors highest among MSM reporting being Black and/or Latino, with lower educational levels, lower personal income, and greater financial insecurity. They were more likely to have been born in NYC with close connections to kin network and less mobile financial and lowest mean score of outness. White men, with higher education, higher personal income, and born outside of NYC report neighborhood congruence of all neighborhoods. This means they have higher control over their living situation. Neighborhood incongruence associated with sexual risk | Longitudinal studies are needed to better understand how these relations change over time. More research is needed to understand how neighborhood/geography impacts the lives of men living in smaller cities in rural areas. Studies should include incorporating the complexities of how different spaces and places impact the health and behavior of MSM to reach different populations |
| Latkin, C. A., Curry, A. D., Hua, W., & Davey, M. A. (2007) | Participants identified as 97% African American. 59% male and 22% HIV positive; 81% reported unemployment, 63% on public assistance, and 19% had been incarcerated, and 14% homeless. Participants had a median age was 43 years and 47% had completed less than 11 years of school. Virtually all (97%) of participants reported a history of heroin or cocaine use; 27% reported recent injection drug use and 36% reported recent crack cocaine smoking | Statistically significant direct associations were observed between neighborhood disorder and psychological distress; neighborhood disorder and sexual risk behaviors; and neighborhood disorder and drug use. There were also significant indirect associations of neighborhood disorder on sexual risk behaviors. These findings reinforce the significance of neighborhood disorder in relation to sexual risk behaviors and drug use | Future focuses should be centered on community programs that mitigate the norms of violence and drug abuse, improve relationships between communities and law enforcement, and economic development |
| Lutfi, K., Trepka, M. J., Fennie, K. P., Ibanez, G., & Gladwin, H. (2015) | Non-Hispanic African Americans between eh ages of 15–44. Majority were male, had a HS diploma, and were under the age of 35 | Racial residential segregation was associated with risky sexual behavior. This association was stronger with the centralization and concentration dimensions of racial residential segregation. These findings suggest that risky sexual behavior was more strongly associated with neighborhoods with high concentrations of non-Hispanic blacks located in an urban core | Examination of prevention strategies (STI education and methods to prevent partner instability) in racially segregated residential areas and the role that they may play in lowering risky sexual behaviors |
| Martinez, A. N., Lorvick, J., & Kral, A. H. (2014) | 61% reported usually sleeping in Census tracts with 20% or more households living in poverty; 12% tested positive for HIV infection at the time of interview; 35% reported syringe sharing in the past 6 months, 9% reported at least one non-fatal overdose in the past 12 months | The mean activity space distance in this sample was 1.5 miles. Only 9.6% of participants had a syringe exchange program located along their activity space. This study observed an association between increases in activity space distance with a decrease in odds of being HIV positive. An increase in residential transience, or the number of different locations slept in by participants in a 6 month time period, was associated with higher odds of syringe sharing. Activity space distance was not independently associated with overdose or syringe sharing in this study | Future approaches should examine the types, frequency, and timing of habitually visited locations of injection drug users for targeted interventions. Document all geographic locations that an individual has direct contact with as a result of his or her day to day activities through diaries or smartphones |
| Mustanski, B., Birkett, M., Kuhns, L. M., Latkin, C. A., & Muth, S. Q. (2015) | Egos (n = 167): median age is 20.1, 100% male, 54.5% Black, 22.2% Latino, 83.9% identified as gay, majority (95.2%) reported stable housing. 41.3% of egos reported high school graduate or less education, and majority were not employed. Alters (n = 837): median age 22.4, 91.6% identified as male, with 7.5% identifying as female and 0.8% identifying as transgender. 49.0% identified as Black, 21.0% identified as Latino, and 22.6% identified as White. 75% of egos identified as gay/lesbian, 15.3% identified as bisexual, and 7.8% identified as heterosexual | BYMSM more likely to have sex partners identified as main partner and report strong relationships with partners. Black YMSM had greater proportion of sexual partners from high HIV prevalence neighborhoods than Latino, White, and other YMSM. Black and Latino YMSM had denser sexual networks than White YMSM. Sex partners more likely than non-sex partners to be either drug partners or to be support network members | To eliminate racial inequities in HIV we may need to consider how network and geographic factors can be addressed through structural interventions in concert with prevention at the individual level |
| Nandi, A., Glass, T. A., Cole, S. R., Chu, H., Galea, S., Celentano, D. D.,... Mehta, S. H. (2010) | 36% of participants had an age greater than or equal to 35 years at baseline. The majority of participants identified as male (75%) and Black (95%), and a majority reported less than high school education (56%), unemployed in the past 6 months (77%, and had a formal income less than $2500 in the past 6 months (79%). 36% of participants reported that they were HIV positive, 48% reported that their age at first injection was less than 20 years old, and 30% reported needle sharing | IDUs living in more impoverished neighborhoods were less likely to stop injecting drugs, independent of individual level covariates. Neighborhood environment may be an important determinant of drug injection | Consider the use of IPW (inverse probability weights) as a method to address confounding by determinants of neighborhood selection, specifically for handling time-varying confounders affected by prior exposure |
| Neaigus, A., Jenness, S. M., Reilly, K. H., Youm, Y., Hagan, H., Wendel, T., & Gelpi-Acosta, C. (2016) | The sample identified as 60.1% male, 79.6% non-Hispanic Black, and 19.6% Hispanic race/ethnicity; the median age was 40 years; 23.9% reported non-heterosexual activity; 37.7% had ever been homeless (past 12 months); 16.6% had ever injected drugs; in the past 12 months 76.7% used non-injection drugs; 90.1% engaged in condomless vaginal or anal sex; 9.6 tested HIV positive; Reside in Brooklyn (53.2%), Manhattan (31.4%), Bronx (13.6); and Queens (1.8%) | Community sexual bridging in NYC is common meaning the risk of heterosexually transmitted HIV from condomless sex with current or former drug injectors is considerable. Higher bridging communities had a greater percentage of Black or Hispanic residents. Hidden bridging communities were more likely to include Black residents, which may facilitate the spread of heterosexually transmitted HIV among Black women in lower HIV-prevalence communities. It is also associated with homelessness and subsequent geographic mobility | Describing and understanding patterns of community sexual bridging can enhance geographically targeted HIV interventions in urban areas. Bridging communities are important to understand in HIV prevention/intervention |
| Pachankis, J. E., Eldahan, A. I., & Golub, S. A. (2016) | Majority of participants were gay-identified, single, HIV-negative, had completed college or were currently enrolled in college, were either employed full time or enrolled as a student. Over one third reported growing up working class or poor. One third were from a hometown with a population of less than 50,000; 13.2% were from non-US hometowns and were moving from outside the USA. Most currently lived in a neighborhood with a higher-than-average density of same-sex households, earned less than $30,000 per year, knew at least one person in NYC upon arrival and had arrived in the past 6 months | Participants reported encountering moderate degrees of hometown stigma and discrimination and moved to NYC to escape stress & pursue opportunity. Men who escaping stress were more likely to live outside a gay-dense neighborhood upon NYC arrival. Hometown interpersonal discrimination strongly related to all assessed health risks, including HIV risk, substance use, alcohol problems, & mental health problems, although hometown structural stigma climate was associated with lower odds of heavy drug use | Need for more programs that facilitate social support outside of sex risk and substance use sciences, encourage healthy goal pursuit, and promote healthy identity development away from the threat of hometown discrimination might possess particular promise. Research utilizing longitudinal designs and matches samples of non-migrants can extend the results of this research to establish causal threats to the health of this sizable and vulnerable segment of the urban population |
| Parrado, E. A., & Flippen, C. (2010) | The average Hispanic immigrant in the area is nearly 30 years-old, has 7.6 years of education, and earns $14 hourly. Less than 40% of migrant men are married and residing with their spouse; the vast majority are unaccompanied. The average duration of residence in Durham area is less than 4.4 years, only 64% of migrant men reported speaking any English, and 8% reported speaking English well or very well | Likelihood of CSW varies in conjunction with accumulated time in Durham, though not in linear fashion. CSW increases during the first years after migration as migrants gain financial resources, peaks, and then declines over time in conjunction with developing social bonds and attachments. Share of community who are recent migrants positively associated with CSW use. Neighborhood concentration of Hispanic migrants tends to overlap with the concentration of single men. Social disorganization positively correlate with CSW | Move beyond individualistic approaches and address the social milieu in which migrants operate, improving neighborhood conditions and affecting the structural impediments to positive sexual adaptation in the U.S |
| Quinn, K., Voisin, D. R., Bouris, A., & Schneider, J. (2016) | Average age of 23.8 years, over 90% had at least a high school degree, and two-thirds were working full- or part time. One-third reported any lifetime use of hard drugs and 15.2% reported hard drug use over the previous 3 months (cocaine, amphetamines, inhalants, sedatives or sleeping pills, hallucinogens, or opioids), 40% reported daily tobacco use, over half reported daily marijuana use. 20% reported having condomless anal intercourse with an unknown or different status partner. 84.8% currently taking HIV medications, the entire sample reported high rates of exposure to community violence | Findings establish that exposure to community violence was a significant correlate of low medication adherence and unprotected anal sex among YBMSM. Significant differences among HIV positive YBMSM with regards to poor mental health, higher substance use, condomless anal intercourse and lower medication adherence based on levels of exposures to community violence. Secondary HIV prevention initiatives for persons living with HIV should address exposure to community violence | Using larger samples and longitudinal designs, might better estimate whether lifetime or past 12 month exposure to community violence is associated with health-related outcomes across varying time intervals for this populations. Future longitudinal approaches are also needed to establish the temporal ordering between exposures to community violence and the health-related factors observed among this study |
| Raymond, H. F., Al-Tayyib, A., Neaigus, A., Reilly, K. H., Braunstein, S., Brady, K. A., … & German, D. (2017) | The mean number of men per city was 511. The majority (80%) of men reported only MSM behavior in the last 12 months. Baltimore reported lowest MSM behavior (66.8%) in the past 12 months. Percent of men who reported a female partner varied across sites, with a range of 0% to 5%. All sites had low percentages of MSM and IDU behavior in the past 12 months | Findings demonstrated high correlation (0.93) between the percentage of reported living HIV cases attributed to heterosexual sexual contact, and a moderate nonsignificant correlation (0.49) between the percentage of men who had sex with men and women (MSMW). Cities with high levels of poverty and African American/Black residents had higher levels of MSMW and higher levels of heterosexual female cases | More research to understand facts such as financial instability, incarceration, internalized homonegativity, society gay stigma, gender role conflict, and childhood sexual abuse among African American/Black communities and African American/Black MSM contribute to the potential bridging of HIV from MSM to female heterosexuals |
| Raymond, H. F., Chen, Y. H., Same, S. L., Catalano, R., Hutson, M. A., & McFarland, W. (2014) | 165 HIV-negative BMSM, 170 HIV-negative transfemales, and 188 HIV-negative WMSM, (demographic data reported for each group separately), | BMSM & transfemales more similar in SES than they are to WMSM. WMSM more likely to have college education or greater, higher incomes and health insurance. WMSM had highest SES scores while BMSM and transfemales had similar, lower levels of SES. BMSM and transfemales have higher IV drug use than WMSM. All populations similar in regards to number of partners in drug use, numbers of partners in the past 6 months, and sexual risk taking. BMSM had more acts of potentially discordant unprotected anal intercourse and more partners | Interventions must take into account the very specific must take into account the very specific contexts and patterns of behavior related to HIV risk taking on a subpopulation basis. Future research will by necessity address a wide range of neighborhood effects (lack of services, domestic violence, neighborhood based partnering) that may have a relationship with HIV risk taking |
| Rothenberg, R. B., Dai, D., Adams, M. A., & Heath, J. W. (2017) | HIV prevalence in lower-risk area 12% compared to 17% in higher-risk area. Sample more than 90% African American. 1:1 male-to-female ratio. Approximately 70% single, 40% had high school diploma/GED. Homelessness less in lower-risk areas and among women (male: lower, higher: 10%, 27%; female: lower, higher: 6%, 21%). Over 90% of men in both areas had been incarcerated; proportion varied from 63% (lower risk) to 77% (higher risk) in women. Majority of participants identified as heterosexual. Crack use about 2 × higher in higher- risk areas. Heroin and drug injection highest among men in the higher-risk area (22%) and anal sex in the past 6 months was highest among women in the higher-risk areas (12%) | Higher risk areas demonstrated greater social and geographic compactness. Indicates greater concentration of HIV risk in higher risk areas. Endemic HIV transmission in at-risk communities is maintained though the interaction of intense compound risk taking, geographic compactness, and a conducive network structure | Further exploration of the interaction of the multiple factors that affect transmission is likely to provide greater insight into the dynamics |
| Rudolph, A. E., Crawford, N. D., Latkin, C., Fowler, J. H., & Fuller, C. M. (2013) | 10.5% HIV positive, 7.14 HIV status unknown, 15.13 total income > 10,000, 68.5% homeless in past 6 months, mostly African American 55.8%, 34.4% Hispanic, 74.8% male | Membership in high HIV prevalence networks was not random; individuals who recruited (or were recruited by) HIV positive individual more likely to be HIV positive and strength/significance of association did not diminish with increasing degrees of separation. Association between exchanging sex, crack use, and increased HIV prevalence in drug using networks. High HIV prevalence network members were more likely to be recruited in neighborhoods characterized by increased inequality, higher-valued owner-occupied housing, and a greater proportion of Latinos | Network-driven approaches which also take features of the social/structural environment into account may be appropriate to reduce HIV transmission and/or support care seeking and HIV drug adherence for HIV positive individuals, but further research is needed to better characterize neighborhood factors associated with HIV-clustering among drug-using populations in NYC |
| Rudolph, A. E., Linton, S., Dyer, T. P., & Latkin, C. (2013) | Predominately African American (96.9%), the median age was 42 years, 10.8% reported being HIV positive, and 30.7% reported > = 1 exchange sex partner in the last 90 days. Median network size was 8 and median number of sex network members in the past 90 days was 1. Women reported living in their current neighborhood for a median 12 months and 65.1% reported spending most/all of their time in that neighborhood. Problems on their block more than half reported: (1) selling drugs, (2) groups of teenagers hanging out on the street, (3) litter/trash on the streets, (4) people fighting arguing, and (5) people saying insulting things or bothering other people when they walk down the street 6. vacant housing | Crack/coke use, HIV infection, & homelessness associated with exchange sex in unadjusted models. Association between homelessness and exchange sex may be explained by perceived neighborhood disorder & social network variables. High-risk network members and multiplex networks participate in higher risk sexual behaviors, having a greater proportion of network members using drugs and who perceived both social support and drug support were associated with an increased likelihood of exchange sex in the unadjusted model | Structural interventions that provide targeted assistance or referrals to subsidized assistance to women who exchange sex may be warranted. Structural interventions that target neighborhoods are need that address social disorder. Especially ones focusing on employment, quality of housing stock, and educational opportunities. More research is needed to better characterize exchange sex partners and to describe how they differ from other types of partners so that more effective network-based interventions can be developed |
| Senn, T. E., Walsh, J. L., & Carey, M. P. (2016) | Predominantly socioeconomically disadvantaged, with at least half of participants reporting an income < $15,000/year (53%), a high school or less education (63%), and current unemployment (50%). Participants also lived in socioeconomically disadvantaged Census tracts, with a median per capita income of $14,267 per year. Median percentage of college graduates in these Census tracts was 13% | Community violence associated with sexual risk behavior in a sample of adults attending an urban STI clinic. Association btw community violence and sexual risk behavior remained after controlling for individual and Census tract-level SES. Associations differed for men and women; for men, higher rates of community violence associated with more partners in the past three months. Women: community violence associated with more episodes of unprotected sex with a non-steady partner | Consider potential sex differences and investigate multiple sexual behavior outcomes. Longitudinal research is needed to clarify the direction of effects |
| Sterk, C. E., Elifson, K. W., & Theall, K. P. (2007) | The parent study sample included 336 HIV negative African American female drug users. Ages ranged from 18 to 59 (mean age of 38 years). Over one half had less than a complete high school education (53%), and approximately 38% were married (including common law) at the time of baseline assessment. 72% reporting any lifetime physical abuse, 60% sexual abuse, 87% emotional abuse. 13% never being in jail or prison, and 48% worked legally in the year prior to baseline interview. 79% were primarily crack cocaine smokers, 8% were injection drug users (IDUs) who did not smoke crack, and 13% were IDUs who also smoked crack | Women in the study's individual HIV risk-reduction is associated with individual characteristics, community norms, opportunity structures, and environmental conditions. The findings contribute to the ongoing debates on community context and health and the link between individual actions and environmental cues | Inclusion of data collection from a larger cross-section of residents to determine how individual actions and community context need to be studied congruently, allowing a focus on individual agency as well as collective efficacy |
| Stevens, R., Gilliard‐Matthews, S., Nilsen, M., Malven, E., & Dunaev, J. (2014) | 30 females who identified as African American (43%), Latina (40% of Dominican or Puerto Rican descent), and both (17%). Ages ranged from 13 to 20, with a mean age of 17. All participants were in high school or in community college at the time of the interview. One half reported having engaged in sexual intercourse in the past. The sexually active participants were significantly older and more likely to report alcohol and marijuana use than nonactive girls. No other significant difference in living situation or sexual attraction. Although their sexual experience levels varied, common themes emerged from their stories, particularly their rationales related to sexual decision making | Neighborhood/social environment impact girls/young women sexual decision making in 3 ways: 1. severe & persistent structural challenges (chronic disinvestment, high poverty & unemployment) reflected in neighborhood fabric. Lack of investment created neighborhood disorder evidenced by high crime and violence. 2. Result of the economic depression in area and the effect on parental supervision & monitoring. 3. High level of visible drug trafficking, drug use, and abuse destroy neighborhood cohesion and increase violence and crime | Consider neighborhood, social, and new media environments as not only the contexts in which individual decision making occurs, but also as systems ripe for targeted intervention |
| Stevens, R., Icard, L., Jemmott, J. B., O'Leary, A., Rutledge, S., Hsu, J., & Stephens-Shields, A. (2017) | African American MSM whose age ranged from 18 to 69 years (mean = 41.7; SD = 10.7); About 20.0% of participants engaged in transactional sex. About 29.7%said they were HIV-positive. About 52.7%did not complete high school or obtain a GED, and 62.6% earned less than $851 per month. About 36.4% lived in their own house or apartment | Participants were more likely to engage in transactional sex if they did not complete high school, demonstrated elevated drug use, and if neighborhood had elevated non-completion rate for high school | Examine motivational factors for substance use and sexual engagement. Examine factors related to housing stability and transactional sex for MSM |
| Tobin, K. E., Latkin, C. A., & Curriero, F. C. (2014) | Majority had at least 12 years of education (82%), nearly half were working full or part time, about half identified as gay and nearly one-third self-report HIV positive status (31%). Substance use with social networks included alcohol only (27%), alcohol and marijuana (27%), marijuana only (16%), and combinations of alcohol, crack, and heroin (20%) | Spatial concentration of drug/alcohol use places may have both health promoting and deleterious effects on the health of African American MSM. Gay neighborhoods or enclaves also may have risk factors associated with them. Spatially focused alcohol/drug areas may be one mechanism for mixing individuals from diverse social networks, thus contributing to disease transmission dynamics | Determine underlying geographic characteristics or migratory patterns that could explain clustering by identified characteristics—desire for privacy, distance from residence, and the racial composition of the area |
| Tobin, K. E., Hester, L., Davey-Rothwell, M. A., & Latkin, C. A. (2012) | The mean age of this sample was 43.9 (SD = 7.53) years old, 66% male, and 95% of this sample reported their sexual identity as straight. In a 6 month period proir to the study, 90% reported unemployment, 28% reported homelessness, and 28% reported incarceration. Greater proportion of sex exchangers were younger, female, bisexual, homeless, smoked crack and injected drugs in the past 6 months | Findings from this study demonstrated spatial clustering of sex exchangers. Perceived norms aligned with spatial clustering of sex exchangers. A specific housing complex of East Baltimore contained the highest concentration of sex exchangers. Participants reporting sex exchange behaviors spatially cluster more. Regions with increased density of sex exchange spatially aligned with regions that with high density of participants reporting that a few to all friends engaging in sex exchange and no friends who would disapprove of sex exchange | Future studies should examine spatial aspects of social networks of sex exchangers within and external to the neighborhood of residence |
| Voisin, D. R., Hotton, A. L., & Neilands, T. B. (2014) | The overall sample was composed of 563 African American youth (219 boys and 344 girls). Mean age was 16.1 (SD = 1.2) and the majority of boys and girls (61 and 59%, respectively) reported receiving ''free school lunch.'' | Community violence associated with risky sex and sexual debut, through pathways of aggression and negative peer norms towards safer sex for boys and girls in this study | These findings indicate a need for more structural interventions focusing on violence in the interests of reducing HIV risk, as well as a need longitudinal studies with larger samples |
| Williams, C. T., & Latkin, C. A. (2007) | 70% of participants reported using heroin, crack and/or cocaine in the past year. 49% were drug injectors, mean age 38, 39% females, 53% received a high school education, 80% not working, 70% having monthly incomes less than $500, 60% reported having a main (sexual partner), depressive symptom scores were at or above the threshold for clinical depression, associated with current drug use, 18% self-reported being HIV positive | Negative effects of neighborhood disadvantage were observed on drug use. Neighborhood poverty and drug influences in the network were positively associated with current drug use, network social support and ties to employed person were protective of drug use. Neighborhood poverty is robust in the sense that its effects are not attenuated when network attributes are taken into account. Included street-recruited drug users who are often marginalized, and neighborhood environment impacts them differently | Future research is needed to understand the aspects of social and physical environments that matter for drug outcomes before effective policy and research interventions can be developed |
Objective Measurements
Living in a more disadvantaged neighborhood was associated with HIV vulnerability when assessed using objective measures of disadvantage such as existing data on percentage of residents living below the federal poverty level, violent crime rates and number of vacant housing units. Six studies indicated a relationship between HIV vulnerability and neighborhood-level factors based on examinations of economic indicators (i.e., income level, poverty) and HIV incidence as well as sexual network factors (e.g., sexual network density among Black and Latino young MSM). Buot et al. [22] found that income inequality and poverty were associated with elevated HIV incidence in cities. Income inequality and lower socioeconomic status was also consistently associated with increased risk of HIV transmission among heterosexuals and MSM. Four studies indicated that communities experiencing heightened HIV prevalence and risk behaviors contained individuals more likely to have dense sexual networks or networks that were spatially constrained [18, 19, 23, 24].
Neighborhood Composition
Fourteen studies examined neighborhood composition and HIV risk behavior, mainly focusing on the concentration of racial/ethnic and sexual minorities. Findings regarding racial and ethnic neighborhood composition and HIV risk behavior are mixed although ethnic heterogeneity was protective against HIV in two studies [22, 25]. For the other studies, one found that a larger African American neighborhood composition was protective against drug risk and sexual risk behaviors [26], another found greater presence of African Americans was associated with increased sexual risk behavior [27], and another did not identify a relationship between ethnic heterogeneity and HIV risk [28]. Of note, Knittel et al. [29] found that the incarceration rates of African American males increases HIV vulnerability via increased sexual partnerships at the community level. Neaigus et al. [30] looked at community bridging—sexual ties among individuals that bring sexually transmitted HIV from one locale to another—and discovered a greater percentage of Black or Latinx residents in high HIV-spread communities (high bridging and high HIV prevalence), and a greater percentage of Black residents in hidden bridging communities (high bridging and low HIV prevalence). Pachankis et al. [31] examined HIV transmission risk (e.g., number of condomless anal or vaginal sex acts with serodiscordant and unknown-status partners) among gay and bisexual migrants to New York City and found a higher odds of engaging in sexual risk behaviors among individuals who came from a smaller town, had recently arrived, and moved to pursue opportunity.
Three studies indicated that a higher composition of MSM in neighborhoods was associated with sexual risk (e.g., unprotected anal intercourse) [15, 32, 33]. One study did not find this association [34]. Tobin et al. [35] reported on spatial clustering of sex exchange behavior as well as norms, and identified a housing complex with the highest density of exchange sex. Duncan et al. [36] examined the concept of spatial polygamy, the ways individual move across and experience multiple neighborhood contexts, and noted that young MSM who reported concordance among their residential, socializing and sex neighborhoods were more likely to report recent engagement in condomless oral sex. Raymond et al. [37] found that Black MSM and transwomen were more likely to live in high HIV prevalence, low income areas, and that increasing neighborhood HIV prevalence was associated with an increase in the number of potentially serodiscordant unprotected sex acts.
Subjective Measurements
Lower perceived neighborhood condition among residents was consistently associated with more drug use and sexual risk behavior in seventeen studies. Twelve studies identified a relationship between poorer perceived neighborhood quality and increased sexual risks [7, 13, 20, 38–46]. Perceived neighborhood social disorder (e.g., perpetuation of violence) was consistently associated transactional sex [13, 38, 46], STIs [7], having higher risk partners [20, 41], unprotected intercourse [40, 42], number of partners [43], and other indicators of sexual risk (i.e., sex while using drugs) [45].
Drug Risk and HIV Vulnerability
Six studies identified a relationship between living in a more disadvantaged neighborhood and increased HIV vulnerability due to drug risks [47–52]. Four studies indicated that individuals in more disadvantaged neighborhoods had less access to harm reduction services [50] and drug treatment [47, 49, 51]. Two studies found that lower socioeconomic status of neighborhoods was associated with increased drug use, particularly injection drugs [48, 52]. Contrasting these studies, one study of street recruited injection drug users found that residing in a census tract with concentrated poverty was associated with less syringe sharing; this was true for those who most often slept in concentrated poverty tracts, while those with more transient residence experienced increased odds in syringe sharing [53]. Another study also noted increases in injection drug use as residential segregation increased [54]. With findings from qualitative interviews with female drug users, Sterk et al. [55] interpreted the data to indicate that a neighborhood’s physical and social infrastructure could lead to alienation, in turn negatively affecting behavior change efforts, while social capital and social support could mediate these negative effects.
Sexual Risk Behaviors and HIV Vulnerability
Seven studies examined the relationship between objective measures of neighborhood-level factors and sexual risks behavior. Living in a more disadvantaged neighborhood was associated with inconsistent condom use [25, 56, 57]. However, findings regarding anal intercourse were mixed as one study identified an inverse relationship between neighborhood condition and anal sex [34] while another detected a direct relationship [57]. Young MSM in neighborhoods with greater disadvantage (e.g., percentage of households in poverty) were less likely to report serodiscordant partners [58]. Further, areas with fewer people completing high school contained individuals more likely to engage in transactional sex [6]. In cities with high levels of both poverty and Black residents, there were higher reports of men who have sex with men and women, and more heterosexual female HIV cases [59].
Six studies highlighted social determinants (e.g., lack of sexual health support services, lack of activities for young people, mass incarceration, poverty, neighborhood segregation) that restrict the types of individuals in one’s social/sexual networks, impair access to HIV prevention tools (e.g., condoms, PrEP), impact community norms about drug use and sexual behaviors, and foster HIV risk behaviors [44, 60–64]. Several multi-level pathways were identified between neighborhood quality and HIV vulnerability. Neighborhood condition affects sexual risks indirectly through psychological distress and substance use [39, 41]. Geographic restrictions constrain selection pools [62] and racial residential segregation concentrates African Americans in areas of higher HIV prevalence [8]. Among women, an imbalance of male partners increases HIV vulnerability and neighborhood disadvantage may also exacerbate the necessity of transactional sex [64].
Geographic Distribution of the Reviewed Studies
The majority of the studies were conducted in the Northeast and South regions of the U.S.; few took place in the Midwest or West (see Fig. 2). The Northeast and South have historically been hit hardest by the HIV epidemic, thus it is logical for more studies to be conducted in those areas. However, given HIV incidence and prevalence in the West, there were fewer studies conducted than anticipated. In all regions, studies tended to take place in large urban centers, with many studies concentrated in the New York-Washington, D.C. corridor. However, several populous metropolitan areas, including Dallas, San Antonio, Phoenix, and San Diego, were unstudied in the reviewed literature despite historical HIV incidence and prevalence rates that would warrant further investigation. Further, Nevada, Arizona, Oklahoma, Missouri, Kentucky and Ohio are states/have counties prioritized in the EHE, but were absent from the review. Alabama, Arkansas and South Carolina were only represented by one study each, and several counties were underrepresented in Texas.
Fig. 2.
Maps of the “Ending the HIV Epidemic” (EHE) jurisdictions (top) (source https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview) and locations of the included studies (bottom). In the bottom map, major cities are denoted with a square; each dot represents a single study
Discussion
In the context of HIV vulnerability, the neighborhoods where people live and/or frequent, and the sexual or substance use behaviors in which they engage while there, matter. Underscoring the importance of healthography [65], the notion that geography and where people live shapes health and well-being, this systematic review affirms the importance of neighborhood-level vulnerabilities for HIV risk. We advance knowledge about the relationship between neighborhoods and risk with five noteworthy contributions.
First, we highlight that neighborhood disadvantage, regardless of whether it is assessed objectively or subjectively, is one of the most robust correlates of HIV risk. Our review indicates that HIV is not randomly distributed in neighborhoods, but instead concentrated in neighborhoods characterized by factors such as high rates of poverty, crime, and abandoned buildings. These forms of neighborhood disadvantage are not naturally occurring. Rather, they are the consequence of laws, policies and practices to maintain racialized inequities such as residential segregation and inequitable urban housing policies (e.g., those that limit access to public housing for people with criminal or incarceration records). Historically, policies such as these have relegated people at the most marginalized intersections of social-structural inequality—people who are racial/ethnic minority, poor, immigrants and undocumented, those addicted to substances—to predominantly poor urban and rural neighborhoods characterized by risk factors (e.g., substance use, sexual networks with dense HIV concentration). This increases HIV vulnerability. This finding has important implications for structural interventions, namely local, state and federal initiatives to increase affordable housing and housing stability for low-income people. Building on evidence that stable housing programs are effective in improving HIV outcomes (e.g., Housing Opportunities for Persons with AIDS [HOPWA]) [66], it stands to reason that similar housing and neighborhood improvement programs at the population level could also be leveraged as an HIV prevention strategy.
Second, we illustrate key gaps in neighborhood and HIV prevention research. Although the Food and Drug Administration approved PrEP as an effective biomedical HIV intervention tool in 2012, and PrEP is included as a key pillar in the HIV Prevention Continuum, we found no studies in the 2007 to 2017 review period focused on neighborhood-level effects on PrEP uptake. There remains a critical need for research in this area; newer findings document PrEP access disparities among people from high poverty neighborhoods [67]. There is also a paucity of research with youth and transgender persons, and racial/ethnic diversity is lacking (i.e., only one study focused on Latinx populations). This highlights opportunities for research and interventions to expand HIV prevention services for diverse groups of people who live in or frequent disadvantaged neighborhoods. Specifically, it suggests that HIV/AIDS services organizations should adopt or expand mobile outreach units to deliver HIV prevention services such as HIV testing, condom distribution, and PrEP access to people in neighborhoods at increased HIV risk. Such a neighborhood-based approach to HIV prevention could provide an effective remedy to some of the barriers to HIV prevention services (e.g., lack of public transportation, limited childcare options).
Third, our findings underscore methodological and data-related barriers to advancing the science of neighborhood-level effects on HIV-related outcomes. There is no standardized way to define neighborhoods, and best practices to generate and analyze data on the relationship between neighborhoods and HIV vulnerability are lacking. This hinders our ability to fully understand the role of neighborhoods in HIV vulnerability, as well as to implement interventions to mitigate the negative effects. Novel partnerships are needed among health departments, community-based organizations, academic institutions and others to collect and organize data across multiple levels for more nuanced analyses. Given prior critiques, it will be important to account for residential and nonresidential exposures in such work to avoid confounding effects from the places people visit over time [68]. Additionally, while diverse theoretical approaches were applied in the reviewed studies (e.g., ecology-oriented theories), most of the research used the same frameworks. There remains a need to apply, and even develop, theories that account for the mediating role of factors such as the intersectional identities of neighborhood residents, unintended consequences of spatialized policies (e.g., drug reform and targeting of racial and other minoritized communities) and resource availability in the relationship between HIV vulnerability and neighborhood context. This will contribute to the generation of theory driven hypotheses to clearly articulate how neighborhoods are linked to this key outcome [69].
Our assessment of geographical distribution is the fourth noteworthy contribution. Our analyses indicate that the majority of the counties/states identified in the EHE were represented in the studies included in this review (89%, n = 51). However, there were considerable gaps with underrepresentation of research in highly affected rural areas and Southern states. This key knowledge can be used to set future research priorities and allocate resources to underserved communities. Such priority setting is increasingly important given intersections among healthography, structural injustice (e.g., inequitable drug policies, over-policing) and HIV-related outcomes. For example, communities with higher rates of mass incarceration demonstrate elevated HIV rates [70]. Thus, actions within the criminal justice system may increase HIV vulnerability in neighborhoods. Specifically, the War on Drugs and “get tough on crime” policies from the late twentieth century may impact neighborhood viability and subsequently facilitate elevated HIV vulnerability, particularly in Black communities. These policies foster over-policing in Black communities [71]. Coupled with harsher charges (often for similar crimes as White people) and sentencing disparities, this approach to criminal justice has helped facilitate the large scale removal of many Black people, particularly Black men, from their homes and communities [71]. This increases HIV vulnerability through several pathways including alteration of sexual networks (e.g., monogamy interruption, imbalanced sex ratio) and the downstream deleterious impacts on intimate relationship dynamics (e.g., condom negotiation, negotiation against sexual concurrency) [72]. Moreover, the increased risk for economic disenfranchisement and undermined access to HIV prevention resources following incarceration further increases HIV vulnerability [72].
Lastly, our work aligns with mounting advocacy to jettison the socially constructed concept of “race” as an explanatory variable for health inequities such as HIV—and now COVID-19—that disproportionately affect Black, Latinx, Indigenous and other racial/ethnic minority communities. Instead, we must emphasize the role of structural injustice based on race in constraining the ability of people in disadvantaged and impoverished neighborhoods to protect themselves from HIV compared with people who inhabit resource and income-rich neighborhoods. Applied to our focus on neighborhoods and HIV vulnerability, the historical legacy of structural racism affects virtually every aspect of where Black people live in the U.S., and in turn their HIV ulnerability, access to HIV prevention services, and even HIV viral suppression [73, 74]. Indeed, there is now ample empirical evidence that people in diverse Black communities (e.g., young heterosexual adults; gay, bisexual and other MSM) are at disproportionate risk for HIV despite engaging in fewer sexual and substance use risk behaviors than their White counterparts [75–77]. Assessing risk at the neighborhood level underscores that many racial differences in HIV incidence and prevalence reflect shared experiences of oppression structured by race (e.g., residential segregation), not genetic or biological predispositions to HIV. This knowledge is promising, because it lays a foundation for the field to prioritize factors that are modifiable. This supports the development and implementation of multilevel interventions, such as simultaneously providing comprehensive individual education and enacting policies to desegregate communities and reduce neighborhood poverty concentration [4]. Ultimately, such an approach will address the neighborhood-level structural inequities that increase HIV risk—rather than continue to reify the intractability of inequality by highlighting factors (i.e., “race”) that are in essence, immutable [78].
Limitations
This review examined articles from 2007 through 2017 in a proscribed set of databases. While a substantive number of studies were included in the review, we missed related papers published outside of this window. With the focus narrowed to HIV risk behaviors, we are unable to provide implications for other highly relevant HIV outcomes (e.g., medication adherence). However, this more focused approach allowed us to provide richer insights on behavior, and the methods can be replicated to examine additional relevant outcomes.
Conclusion
We spotlight neighborhoods as a critical context for understanding HIV vulnerability above and beyond the exclusively individual-level that has conventionally characterized most social and behavioral HIV prevention research. Our findings underscore a need to challenge solely individualistic explanations for HIV risk behaviors, in favor of a more expansive structural approach, focused on neighborhood-level influences. Conversely, more research is also needed to advance knowledge and interventions about the neighborhood-level factors that are protective, particularly in poor and under-resourced neighborhoods (e.g., initiatives designed to foster social cohesion). As for HIV prevention and other health equity researchers, our findings underscore a need for structural competency. Albeit developed primarily for clinical trainees, the structural competency paradigm has applied utility for those who conduct HIV prevention research and design interventions and policy. The structural competency approach proposes five steps to increase knowledge about how “… the organization of institutions and policies, as well as of neighborhoods and cities…” (p. 127) determine health [79]. Greater attention to understanding and developing interventions to address which particular aspects of neighborhoods increase and reduce HIV risk, how, and for whom (i.e., key intersections of race, gender, class, sexual and gender minority status, and/or immigration status), will likely hold greater promise for meeting the goals of the EHE than continuing to ignore the role of neighborhoods in increasing HIV vulnerability.
Author Contributions
All authors contributed to the study and manuscript writing. BMB and JK conceptualized and lead the study. RJ created the reference library for data management and independently screened titles and abstracts to identify full-text articles for final eligibility review. BFC and JAB conducted data extraction based on a protocol for key study characteristics. SB created maps to visualize the geographic distribution of the studies. RS and LB reviewed and edited manuscript drafts.
Funding
This work was supported by the National Institutes of Health (NIH)/National Institute of Mental Health (NIMH; grant R25MH087217, Brawner pilot project PI; grant R01 MH100022-02, Bowleg PI). J. A. B. received support from the Robert Wood Johnson Foundation Future of Nursing Scholars Program. S. B. received support from the Rita & Alex Hillman Foundation Hillman Scholars Program in Nursing Innovation. The content is solely the responsibility of the authors and does not represent the official views of the funding sources.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention. HIV in the United States and Dependent Areas 2019 [cited 2020 February 6]. https://www.cdc.gov/hiv/pdf/statistics/overview/cdc-hiv-us-ataglance.pdf.
- 2.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 3.Brawner BM. A multilevel understanding of HIV/AIDS disease burden among African American women. J Obstet Gynecol Neonatal Nurs. 2014;43(5):633–643. doi: 10.1111/1552-6909.12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smedley BD. Multilevel interventions to undo the health consequences of racism: the need for comprehensive approaches. Cultur Divers Ethnic Minor Psychol. 2019;25(1):123–125. doi: 10.1037/cdp0000263. [DOI] [PubMed] [Google Scholar]
- 5.Meijer M, Röhl J, Bloomfield K, Grittner U. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74(8):1204–1212. doi: 10.1016/j.socscimed.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 6.Stevens R, Icard L, Jemmott JB, O'Leary A, Rutledge S, Hsu J, et al. Risky trade: individual and neighborhood-level socio-demographics associated with transactional sex among urban African American MSM. J Urban Health. 2017;94(5):676–682. doi: 10.1007/s11524-017-0187-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kerr JC, Valois RF, Siddiqi A, Vanable P, Carey MP. Neighborhood condition and geographic locale in assessing HIV/STI risk among African American adolescents. AIDS Behav. 2015;19(6):1005–1013. doi: 10.1007/s10461-014-0868-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brawner BM, Guthrie B, Stevens R, Taylor L, Eberhart M, Schensul JJ. Place still matters: racial/ethnic and geographic disparities in HIV transmission and disease burden. J Urban Health. 2017;94(5):716–729. doi: 10.1007/s11524-017-0198-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Latkin CA, German D, Vlahov D, Galea S. Neighborhoods and HIV: a social ecological approach to prevention and care. Am Psychol. 2013;68(4):210–224. doi: 10.1037/a0032704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson PA, Nanin J, Amesty S, Wallace S, Cherenack EM, Fullilove R. Using syndemic theory to understand vulnerability to HIV infection among Black and Latino men in New York City. J Urban Health. 2014;91(5):983–998. doi: 10.1007/s11524-014-9895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. J Am Med Assoc. 2019;321(9):844–845. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- 13.Parrado EA, Flippen C. Community attachment, neighborhood context, and sex worker use among Hispanic migrants in Durham, North Carolina, USA. Soc Sci Med. 2010;70(7):1059–1069. doi: 10.1016/j.socscimed.2009.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akers AY, Muhammad MR, Corbie-Smith G. "When you got nothing to do, you do somebody": a community's perceptions of neighborhood effects on adolescent sexual behaviors. Soc Sci Med (1982) 2011;72(1):91–99. doi: 10.1016/j.socscimed.2010.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buttram ME, Kurtz SP. Risk and protective factors associated with gay neighborhood residence. Am J Mens Health. 2013;7(2):110–118. doi: 10.1177/1557988312458793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braine N, Acker C, Goldblatt C, Yi H, Friedman S, Desjarlais DC. Neighborhood history as a factor shaping syringe distribution networks among drug users at a U.S. Syringe Exchange. Soc Netw. 2008;30(3):235–246. doi: 10.1016/j.socnet.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egan JE, Frye V, Kurtz SP, Latkin C, Chen M, Tobin K, et al. Migration, neighborhoods, and networks: approaches to understanding how urban environmental conditions affect syndemic adverse health outcomes among gay, bisexual and other men who have sex with men. AIDS Behav. 2011;15(Suppl 1):S35–50. doi: 10.1007/s10461-011-9902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gindi RM, Sifakis F, Sherman SG, Towe VL, Flynn C, Zenilman JM. The geography of heterosexual partnerships in Baltimore city adults. Sex Transm Dis. 2011;38(4):260–266. doi: 10.1097/OLQ.0b013e3181f7d7f4. [DOI] [PubMed] [Google Scholar]
- 19.Tobin KE, Latkin CA, Curriero FC. An examination of places where African American men who have sex with men (MSM) use drugs/drink alcohol: a focus on social and spatial characteristics. Int J Drug Policy. 2014;25(3):591–597. doi: 10.1016/j.drugpo.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cooper HLF, Linton S, Haley DF, Kelley ME, Dauria EF, Karnes CC, et al. Changes in exposure to neighborhood characteristics are associated with sexual network characteristics in a cohort of adults relocating from public housing. AIDS Behav. 2015;19(6):1016–1030. doi: 10.1007/s10461-014-0883-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rudolph AE, Crawford ND, Latkin C, Fowler JH, Fuller CM. Individual and neighborhood correlates of membership in drug using networks with a higher prevalence of HIV in New York City (2006–2009) Ann Epidemiol. 2013;23(5):267–274. doi: 10.1016/j.annepidem.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buot M-LG, Docena JP, Ratemo BK, Bittner MJ, Burlew JT, Nuritdinov AR, et al. Beyond race and place: distal sociological determinants of HIV disparities. PLoS ONE. 2014;9(4):e91711. doi: 10.1371/journal.pone.0091711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mustanski B, Birkett M, Kuhns LM, Latkin CA, Muth SQ. The role of geographic and network factors in racial disparities in HIV among young men who have sex with men: an egocentric network study. AIDS Behav. 2015;19(6):1037–1047. doi: 10.1007/s10461-014-0955-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rothenberg RB, Dai D, Adams MA, Heath JW. The Human immunodeficiency virus endemic: maintaining disease transmission in at-risk urban areas. Sex Transm Dis. 2017;44(2):71–78. doi: 10.1097/OLQ.0000000000000561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frye V, Nandi V, Egan JE, Cerda M, Rundle A, Quinn JW, et al. Associations among neighborhood characteristics and sexual risk behavior among Black and White MSM living in a major urban area. AIDS Behav. 2017;21(3):870–890. doi: 10.1007/s10461-016-1596-2. [DOI] [PubMed] [Google Scholar]
- 26.Bluthenthal RN, Do DP, Finch B, Martinez A, Edlin BR, Kral AH. Community characteristics associated with HIV risk among injection drug users in the San Francisco Bay Area: a multilevel analysis. J Urban Health. 2007;84(5):653–666. doi: 10.1007/s11524-007-9213-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lutfi K, Trepka MJ, Fennie KP, Ibanez G, Gladwin H. Racial residential segregation and risky sexual behavior among non-Hispanic blacks, 2006–2010. Soc Sci Med. 2015;140:95. doi: 10.1016/j.socscimed.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biello KB, Niccolai L, Kershaw TS, Lin H, Ickovics J. Residential racial segregation and racial differences in sexual behaviours: an 11-year longitudinal study of sexual risk of adolescents transitioning to adulthood. J Epidemiol Community Health. 2013;67(1):28–34. doi: 10.1136/jech-2011-200520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knittel AK, Snow RC, Riolo RL, Griffith DM, Morenoff J. Modeling the community-level effects of male incarceration on the sexual partnerships of men and women. Soc Sci Med. 2015;147:270–279. doi: 10.1016/j.socscimed.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neaigus A, Jenness SM, Reilly KH, Youm Y, Hagan H, Wendel T, et al. Community sexual bridging among heterosexuals at high-risk of HIV in New York City. AIDS Behav. 2016;20(4):722–736. doi: 10.1007/s10461-015-1244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pachankis JE, Eldahan AI, Golub SA. New to New York: ecological and psychological predictors of health among recently arrived young adult gay and bisexual urban migrants. Ann Behav Med. 2016;50(5):692–703. doi: 10.1007/s12160-016-9794-8. [DOI] [PubMed] [Google Scholar]
- 32.Egan JE, Frye V, Kurtz SP, Latkin C, Chen M, Tobin K, et al. Migration, neighborhoods, and networks: approaches to understanding how urban environmental conditions affect syndemic adverse health outcomes among gay, bisexual and other men who have sex with men. AIDS Behav. 2011;15:S50. doi: 10.1007/s10461-011-9902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kelly BC, Carpiano RM, Easterbrook A, Parsons JT. Sex and the community: the implications of neighbourhoods and social networks for sexual risk behaviours among urban gay men. Sociol Health Illn. 2012;34(7):1085–1102. doi: 10.1111/j.1467-9566.2011.01446.x. [DOI] [PubMed] [Google Scholar]
- 34.Frye V, Koblin B, Chin J, Beard J, Blaney S, Halkitis P, et al. Neighborhood-level correlates of consistent condom use among men who have sex with men: a multi-level analysis. AIDS Behav. 2010;14(4):974–985. doi: 10.1007/s10461-008-9438-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tobin KE, Hester L, Davey-Rothwell MA, Latkin CA. An examination of spatial concentrations of sex exchange and sex exchange norms among drug users in Baltimore, Maryland. Ann Assoc Am Geogr. 2012;102(5):1058–1066. doi: 10.1080/00045608.2012.674902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duncan DT, Kapadia F, Halkitis PN. Examination of spatial polygamy among young gay, bisexual, and other men who have sex with men in New York City: the P18 Cohort Study. Int J Environ Res Public Health. 2014;11(9):8962–8983. doi: 10.3390/ijerph110908962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raymond HF, Chen YH, Syme SL, Catalano R, Hutson MA, McFarland W. The role of individual and neighborhood factors: HIV acquisition risk among high-risk populations in San Francisco. AIDS Behav. 2014;18(2):346–356. doi: 10.1007/s10461-013-0508-y. [DOI] [PubMed] [Google Scholar]
- 38.Bobashev GV, Zule WA, Osilla KC, Kline TL, Wechsberg WM. Transactional sex among men and women in the south at high risk for HIV and other STIs. J Urban Health. 2009;86(1):32–47. doi: 10.1007/s11524-009-9368-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bowleg L, Neilands TB, Tabb LP, Burkholder GJ, Malebranche DJ, Tschann JM. Neighborhood context and Black heterosexual men’s sexual HIV risk behaviors. AIDS Behav. 2014;18(11):2207–2218. doi: 10.1007/s10461-014-0803-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.DePadilla L, Elifson KW, Sterk CE. Beyond sexual partnerships: the lack of condom use during vaginal sex with steady partners. Int Public Health J. 2012;4(4):435–446. [PMC free article] [PubMed] [Google Scholar]
- 41.Latkin CA, Curry AD, Hua W, Davey MA. Direct and indirect associations of neighborhood disorder with drug use and high-risk—sexual partners. Am J Prev Med. 2007;32(6):S241. doi: 10.1016/j.amepre.2007.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quinn K, Voisin DR, Bouris A, Schneider J. Psychological distress, drug use, sexual risks and medication adherence among young HIV-positive Black men who have sex with men: exposure to community violence matters. AIDS Care. 2016;28(7):866–872. doi: 10.1080/09540121.2016.1153596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Senn TE, Walsh JL, Carey MP. Mediators of the relation between community violence and sexual risk behavior among adults attending a public sexually transmitted infection clinic. Arch Sex Behav. 2016;45(5):1069–1082. doi: 10.1007/s10508-016-0714-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stevens R, Gilliard-Matthews S, Nilsen M, Malven E, Dunaev J. Socioecological factors in sexual decision making among urban girls and young women. Jognn. 2014;43(5):644–654. doi: 10.1111/1552-6909.12493. [DOI] [PubMed] [Google Scholar]
- 45.Voisin DR, Hotton AL, Neilands TB. Testing pathways linking exposure to community violence and sexual behaviors among African American youth. J Youth Adolesc. 2014;43(9):1513–1526. doi: 10.1007/s10964-013-0068-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rudolph AE, Linton S, Dyer TP, Latkin C. Individual, network, and neighborhood correlates of exchange sex among female non-injection drug users in Baltimore, MD (2005–2007) AIDS Behav. 2013;17(2):598–611. doi: 10.1007/s10461-012-0305-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cooper HL, Linton S, Kelley ME, Ross Z, Wolfe ME, Chen Y-T, et al. Racialized risk environments in a large sample of people who inject drugs in the United States. International Journal of Drug Policy. 2016;27:43–55. doi: 10.1016/j.drugpo.2015.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crawford ND, Borrell LN, Galea S, Ford C, Latkin C, Fuller CM. The Influence of neighborhood characteristics on the relationship between discrimination and increased drug-using social ties among illicit drug users. J Community Health. 2013;38(2):328–337. doi: 10.1007/s10900-012-9618-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Genberg BL, Gange SJ, Go VF, Celentano DD, Kirk GD, Latkin CA, et al. The effect of neighborhood deprivation and residential relocation on long-term injection cessation among injection drug users (IDUs) in Baltimore, Maryland. Addiction. 2011;106(11):1966–1974. doi: 10.1111/j.1360-0443.2011.03501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Heimer R, Barbour R, Palacios WR, Nichols LG, Grau LE. Associations between injection risk and community disadvantage among suburban injection drug users in Southwestern Connecticut, USA. AIDS Behav. 2014;18(3):452–463. doi: 10.1007/s10461-013-0572-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nandi A, Glass TA, Cole SR, Chu H, Galea S, Celentano DD, et al. Neighborhood poverty and injection cessation in a sample of injection drug users. Am J Epidemiol. 2010;171(4):391–398. doi: 10.1093/aje/kwp416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Williams CT, Latkin CA. Neighborhood socioeconomic status, personal network attributes, and use of heroin and cocaine. Am J Prev Med. 2007;32(6):S203–S210. doi: 10.1016/j.amepre.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martinez AN, Lorvick J, Kral AH. Activity spaces among injection drug users in San Francisco. Int J Drug Policy. 2014;25(3):516–524. doi: 10.1016/j.drugpo.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 54.Cooper HLF, Friedman SR, Tempalski B, Friedman R. Residential segregation and injection drug use prevalences among Black adults in US metropolitan areas. Am J Public Health. 2007;97(2):344–352. doi: 10.2105/AJPH.2005.074542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sterk CE, Elifson KW, Theall KP. Individual action and community context: the health intervention project. Am J Prev Med. 2007;32(6):S181. doi: 10.1016/j.amepre.2007.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bauermeister JA, Zimmerman MA, Caldwell CH. Neighborhood disadvantage and changes in condom use among African American adolescents. J Urban Health. 2011;88(1):66–83. doi: 10.1007/s11524-010-9506-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Haley DF, Haardorfer R, Kramer MR, Adimora AA, Wingood GM, Goswami ND, et al. Associations between neighborhood characteristics and sexual risk behaviors among HIV-infected and HIV-uninfected women in the southern United States. Ann Epidemiol. 2017;27(4):252–259. doi: 10.1016/j.annepidem.2017.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bauermeister JA, Eaton L, Andrzejewski J, Loveluck J, VanHemert W, Pingel ES. Where you live matters: structural correlates of HIV risk behavior among young men who have sex with men in metro Detroit. AIDS Behav. 2015;19(12):2358–2369. doi: 10.1007/s10461-015-1180-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Raymond HF, Al-Tayyib A, Neaigus A, Reilly KH, Braunstein S, Brady KA, et al. HIV among MSM and heterosexual women in the United States: an ecologic analysis. JAIDS. 2017;75:S280. doi: 10.1097/QAI.0000000000001422. [DOI] [PubMed] [Google Scholar]
- 60.Akers AY, Muhammad MR, Corbie-Smith G. “When you got nothing to do, you do somebody”: a community’s perceptions of neighborhood effects on adolescent sexual behaviors. Soc Sci Med. 2011;72(1):91–99. doi: 10.1016/j.socscimed.2010.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Boyer CB, Greenberg L, Chutuape K, Walker B, Monte D, Kirk J, et al. Exchange of sex for drugs or money in adolescents and young adults: an examination of sociodemographic factors, hiv-related risk, and community context. J Community Health. 2017;42(1):90–100. doi: 10.1007/s10900-016-0234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Brawner BM, Reason JL, Hanlon K, Guthrie B, Schensul JJ. Stakeholder conceptualisation of multi-level HIV and AIDS determinants in a Black epicentre. Cult Health Sex. 2017;19(9):948–963. doi: 10.1080/13691058.2016.1274428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cené CW, Akers AY, Lloyd SW, Albritton T, Powell Hammond W, Corbie-Smith G. Understanding social capital and HIV risk in rural African American communities. J Gen Intern Med. 2011;26(7):737–744. doi: 10.1007/s11606-011-1646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Frew PM, Parker K, Vo L, Haley D, O'Leary A, Diallo DD, et al. Socioecological factors influencing women's HIV risk in the United States: qualitative findings from the women's HIV SeroIncidence study (HPTN 064) BMC Public Health. 2016;16(1):803. doi: 10.1186/s12889-016-3364-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Greenberg MR. Healthography. Am J Public Health. 2014;104(11):2022. doi: 10.2105/AJPH.2014.302232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wolitski RJ, Kidder DP, Pals SL, Royal S, Aidala A, Stall R, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493–503. doi: 10.1007/s10461-009-9643-x. [DOI] [PubMed] [Google Scholar]
- 67.Salcuni P, Smolen J, Jain S, Myers J, Edelstein Z. Trends and associations with PrEP prescription among 602 New York City (NYC) ambulatory care practices, 2014–2016. Open Forum Infect Dis. 2017;4(suppl_1):S21-S.
- 68.Chaix B, Duncan D, Vallée J, Vernez-Moudon A, Benmarhnia T, Kestens Y. The, “residential” effect fallacy in neighborhood and health studies. Epidemiology. 2017;28(6):789–797. doi: 10.1097/EDE.0000000000000726. [DOI] [PubMed] [Google Scholar]
- 69.Bishop AS, Walker SC, Herting JR, Hill KG. Neighborhoods and health during the transition to adulthood: a scoping review. Health Place. 2020;63:102336. doi: 10.1016/j.healthplace.2020.102336. [DOI] [PubMed] [Google Scholar]
- 70.Ojikutu BO, Srinivasan S, Bogart LM, Subramanian S, Mayer KH. Mass incarceration and the impact of prison release on HIV diagnoses in the US South. PLoS ONE. 2018;13(6):e0198258. doi: 10.1371/journal.pone.0198258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Alexander M. The New Jim Crow. New York, NY: The New Press; 2011. [Google Scholar]
- 72.Kerr J, Jackson T. Stigma, sexual risks, and the war on drugs: examining drug policy and HIV/AIDS inequities among African Americans using the Drug War HIV/AIDS Inequities Model. Int J Drug Policy. 2016;37:31–41. doi: 10.1016/j.drugpo.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 73.Khazanchi R, Sayles H, Bares SH, Swindells S, Marcelin JR. Neighborhood deprivation and racial/ethnic disparities in HIV viral suppression: a single-center cross-sectional study in the U.S. midwest. Clinical Infect Dis. 2020 [DOI] [PubMed]
- 74.Olatosi B, Weissman S, Zhang J, Chen S, Haider MR, Li X. Neighborhood matters: impact on time living with detectable viral load for new adult HIV diagnoses in South Carolina. AIDS Behav. 2020;24(4):1266–1274. doi: 10.1007/s10461-019-02734-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, 4th, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. The Lancet. 2012;380(9839):341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 76.Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and drug behavior patterns and HIV/STD racial disparities: the need for new directions. Am J Public Health. 2007;97:1–8. doi: 10.2105/AJPH.2005.075747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kanny D, Jeffries WL, Chapin-Bardales J, Denning P, Cha S, Finlayson T, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men–23 Urban Areas, 2017. Morb Mortal Mon Rep (MMWR) 2019;68(37):801–806. doi: 10.15585/mmwr.mm6837a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 79.Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103:126–133. doi: 10.1016/j.socscimed.2013.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]