Supplemental Digital Content is available in the text.
Keywords: angiotensin II, angiotensin-converting enzyme, COVID-19, Japan, uric acid
Abstract
Severe acute respiratory syndrome coronavirus 2 in coronavirus disease 2019 invades the host through ACE (angiotensin-converting enzyme) 2 as the host cellular receptor for a viral spike protein. ACE2 converts angiotensin II to angiotensin-(1–7) and cleaved ACE2 is detectable in urine and plasma. However, regulation of U-ACE2 (urinary ACE2) and P-ACE2 (plasma ACE2) and their alterations by renin-angiotensin-aldosterone system inhibitors remain unclear. We simultaneously investigated U-ACE2 and P-ACE2 in 605 Japanese participants (male/female: 280/325, mean age: 65±15 years) in the Tanno-Sobetsu cohort study in 2017. Males had significantly lower U-ACE2 and higher P-ACE2 than did females. There was no significant correlation between U-ACE2 and P-ACE2. P-ACE2 was significantly lower in subjects treated with renin-angiotensin-aldosterone system inhibitors than in those not treated with renin-angiotensin-aldosterone system inhibitors, but there was no significant difference in U-ACE2 between the groups. Multivariable regression analyses showed that female sex, high levels of systolic blood pressure, hemoglobin A1c, and urinary albumin-to-creatinine ratio, and low uric acid level were independent predictors of high U-ACE2 level and that high levels of γ-glutamyl transpeptidase, estimated glomerular filtration rate, and uric acid were independent predictors of high P-ACE2 level. In conclusion, U-ACE2 and P-ACE2 are distinctly regulated and the use of renin-angiotensin-aldosterone system inhibitors is not an independent predictor of their levels in a Japanese general population. U-ACE2 is associated with high blood pressure, high glucose level, and microalbuminuria, and low urate level, whereas P-ACE2 is associated with liver dysfunction, high glomerular filtration rate, and high urate level.
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) started in Wuhan, Hubei, China in December 20191 and has become a worldwide pandemic, leading to global threats to health and economic stability. It has been shown that SARS-CoV-2 invades the host through ACE (angiotensin-converting enzyme) 2, a type I transmembrane glycoprotein, as the host cellular receptor for a viral spike protein.2 SARS-CoV-2 has been reported to be infected by endocytosis of ACE2-binding SARS-CoV-23–5 and TMPRSS2 (transmembrane protease serine 2)-mediated cleavage of SARS-CoV-2 accompanied by ACE2.2,4,5
ACE2 is broadly expressed in the heart, kidneys, intestine, liver, and alveolar epithelial cells of the lungs6,7 (Figure S1A in the Data Supplement: data shown by the Genotype-Tissue Expression project). ACE2, a membrane-bound enzyme, is distinctly shed from the membrane by ADAM17 (a disintegrin and metalloproteinase 17), and a soluble form of ACE2 exists in body fluids.8 ACE2 is an important modulator of the renin-angiotensin-aldosterone system (RAAS) by reducing angiotensin II levels and increasing the generation of angiotensin-(1–7),9,10 leading to reduction of vasoconstriction, sodium retention, inflammation, and fibrosis through the MAS (MAS1 proto-oncogene) receptor.11 It has recently been reported that several RAAS inhibitors, including ACE inhibitors, angiotensin II receptor blockers, and mineralocorticoid receptor antagonists, increase the expression and activity of ACE2 in rodent models.12,13 We previously showed in a case-control analysis that olmesartan, an angiotensin II receptor blocker, may increase U-ACE2 (urinary ACE2) in hypertensive patients.14
ACE2 is detectable in urine,15 which most likely reflects its release from proximal tubules,16 but not its filtration through the glomerulus, since the full-length sequence for human ACE2 encodes an 805-amino-acid protein with a calculated mass of 92.4 kDa and the glycosylated form of ACE2 is 120 kDa.9 It has recently been suggested that U-ACE2 could be a potential biomarker of kidney disease.17 U-ACE2 level was elevated in patients with renal diseases including diabetic nephropathy and in patients who had undergone renal transplantation,18–20 indicating a possible role of U-ACE2 as a noninvasive disease biomarker. It has also been reported that U-ACE2 is independently associated with microalbuminuria14,21 and estimated salt intake in humans.14
However, determinants of P-ACE2 (plasma ACE2) measured by using an immunoassay based on proximity extension assay technology, in which data are expressed as relative quantification, have been reported to include sex, ancestry, body mass index, and diabetes in a subset of participants in the PURE (Prospective Urban Rural Epidemiology) prospective study.22 P-ACE2 level was higher in men than in women, and the level in East Asia was the highest.22,23 Furthermore, use of an ACE inhibitor or an angiotensin II receptor blocker was not associated with higher P-ACE2 concentration.22,23 P-ACE2 has also been reported to be associated with increased risk of major cardiovascular events,22 heart failure,24 and stroke.25 Notably, it has recently been reported that P-ACE2 level was unchanged in patients with COVID-19.26
However, regulation of P-ACE2 and U-ACE2 measured simultaneously and alterations in their levels caused by RAAS inhibitors have not been fully addressed, especially in a general population. In the present study, we investigated levels of U-ACE2 and P-ACE2 and regulatory effects of RAAS inhibitors on levels of U-ACE2 and P-ACE2 in a Japanese general population.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Subjects
In the Tanno-Sobetsu Study, a study with a population-based cohort, a total of 605 Japanese subjects (male/female: 280/325, mean age: 65±15 years) were recruited from residents of Sobetsu Town who received annual health examinations in 2017. This study was performed with the approval of the Ethical Committee of Sapporo Medical University and conformed to the principles outlined in the Declaration of Helsinki. Written informed consent was received from all of the study subjects.
Measurements
Medical checkups were performed early in the morning after an overnight fast as previously described.27 Blood pressure was measured using an automated sphygmomanometer (HEM-907, Omron Co, Kyoto, Japan), and average blood pressure was used for analysis. Body mass index was calculated as body weight (kg) divided by the square of body height (meters). Urine and peripheral venous blood samples were immediately analyzed or stored at −80 °C until biochemical analyses. Measurements of biochemical parameters were performed as previously reported.27
Concentrations of U-ACE2 and P-ACE2 were measured using a commercially available ELISA kit (R&D Systems, Minneapolis, MN). The intra-assay and interassay coefficient variances in the kit were <10%. U-ACE2 level was normalized by urinary creatinine level (µg/gCr). Fractional excretion of ACE2 (FEACE2, %), which quantifies the percent of filtered ACE2 that is excreted into urine, was calculated from the standard formula: ([U-ACE2]×[plasma creatinine])/([P-ACE2]×[urinary creatinine])×100. Creatinine and lipid profiles, including total cholesterol, HDL (high-density lipoprotein) cholesterol, and triglycerides, were determined by enzymatic methods. LDL (low-density lipoprotein) cholesterol level was calculated by the Friedewald equation.28 Homeostasis model assessment of insulin resistance was calculated by the following formula29: homeostasis model assessment of insulin resistance=insulin (μU/mL)×glucose (mg/dL)/405. Hemoglobin A1c (HbA1c) was determined by a latex coagulation method and expressed in National Glycohemoglobin Standardization Program scale. BNP (brain natriuretic peptide) was measured using a commercially available immunoassay kit (Shionogi & Co, Osaka, Japan). Estimated glomerular filtration rate (eGFR; mL/min per 73 m2) was calculated by an equation for Japanese30: 194×Cr (−1.094)×age (−0.287)×0.739 (if female). Urinary albumin-to-creatinine ratio (U-ACR; mg/gCr) was used as an index of microalbuminuria.
A self-administered questionnaire survey was performed to obtain information on current smoking habit, alcohol drinking habit, and use of drugs for diabetes, hypertension, and dyslipidemia. Hypertension was diagnosed as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥ 90 mm Hg, or self-reported use of antihypertensive drugs. Diabetes was diagnosed in accordance with the guidelines of the American Diabetes Association31: fasting plasma glucose ≥126 mg/dL, HbA1c ≥6.5%, or self-reported use of antidiabetic drugs. Dyslipidemia was diagnosed as LDL cholesterol ≥140 mg/dL, HDL cholesterol <40 mg/dL, triglycerides ≥150 mg/dL, or self-reported use of antidyslipidemic drugs.
Statistical Analysis
Numeric variables are expressed as means±SD for normal distributions or medians (interquartile ranges) for skewed variables. The distribution of each parameter was tested for its normality using the Shapiro-Wilk W test, and non-normally distributed parameters were logarithmically transformed for regression analyses. Intergroup differences in percentages of demographic parameters were examined by the χ2 test. Comparisons between two groups for parametric and nonparametric parameters were performed by using Student t test and the Mann-Whitney U test, respectively. The correlation between two variables was evaluated using Pearson correlation coefficient. Multivariable regression analysis was performed to identify independent determinants of the level of U-ACE2, P-ACE2 or FEACE2 using age, sex, use of RAAS inhibitors including ACE inhibitors, angiotensin II receptor blockers and mineralocorticoid receptor antagonists, and the variables with a significant correlation as independent predictors after consideration of multicollinearity, showing the t ratio calculated as the ratio of regression coefficient and SE of regression coefficient and the percentage of variance in the level of U-ACE2, P-ACE2 or FEACE2 that they explained (R2). Among the candidate models, the best-fit model using Akaike information criterion (AIC) for each dependent variable was selected. A P value of <0.05 was considered statistically significant. All data were analyzed by using JMP 15.2.1 for Macintosh (SAS Institute, Cary, NC).
Results
Basal Characteristics of the Study Subjects
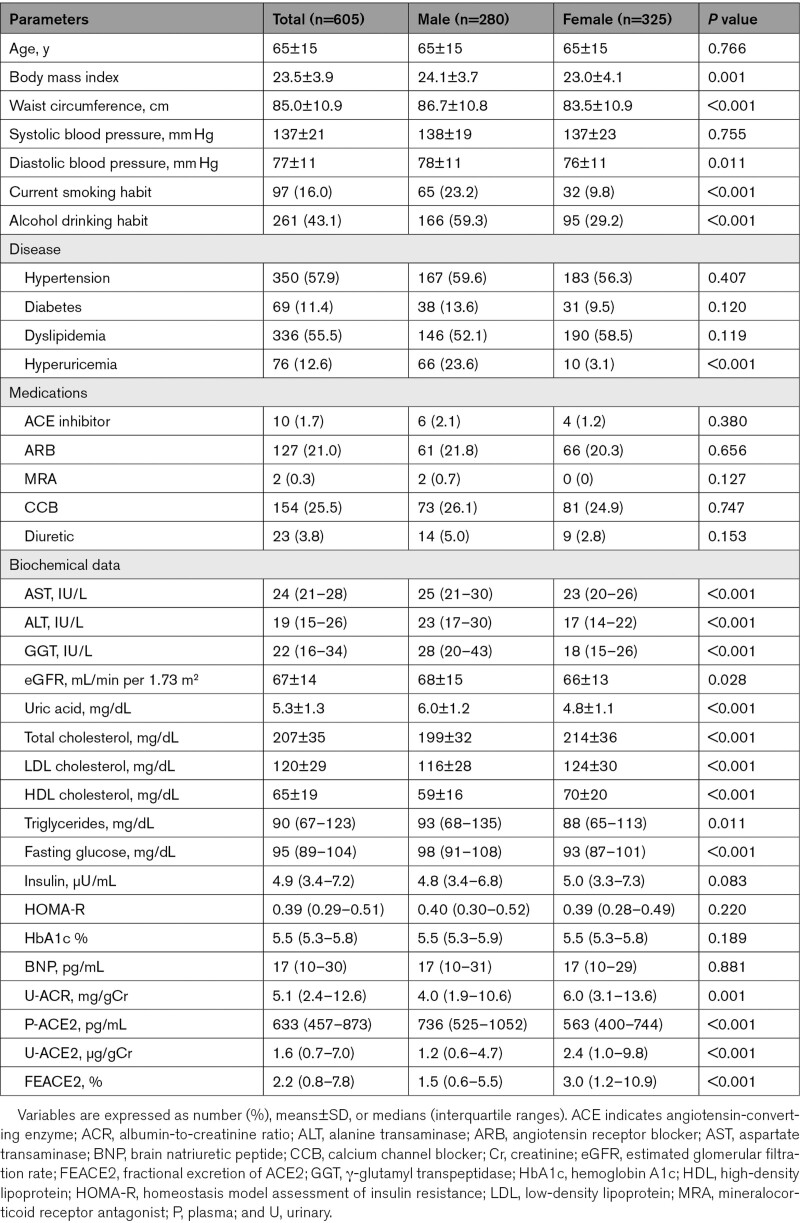
Basal characteristics of the recruited subjects are shown in Table 1. Male subjects had significantly larger body mass index and waist circumference, higher frequencies of habits of smoking and alcohol drinking, higher levels of systolic and diastolic blood pressures, AST (aspartate transaminase), ALT (alanine transaminase), GGT (γ-glutamyl transpeptidase), eGFR, uric acid, triglycerides and fasting glucose and significantly lower levels of total cholesterol, LDL cholesterol, and HDL cholesterol than did female subjects. There was no significant sex difference in frequencies of hypertension, diabetes, and dyslipidemia. The frequency of hyperuricemia was significantly higher in male subjects than in female subjects. The use of RAAS inhibitors (n=137) consisted of ACE inhibitors (n=10), angiotensin II receptor blockers (n=127), and mineralocorticoid receptor antagonists cotreated with an angiotensin II receptor blocker (n=2). There was no sex difference in use of RAAS inhibitors including ACE inhibitors, angiotensin II receptor blockers, and mineralocorticoid receptor antagonists.
Table 1.
Characteristics of the Recruited Subjects
Comparisons and Correlations of U-ACE2
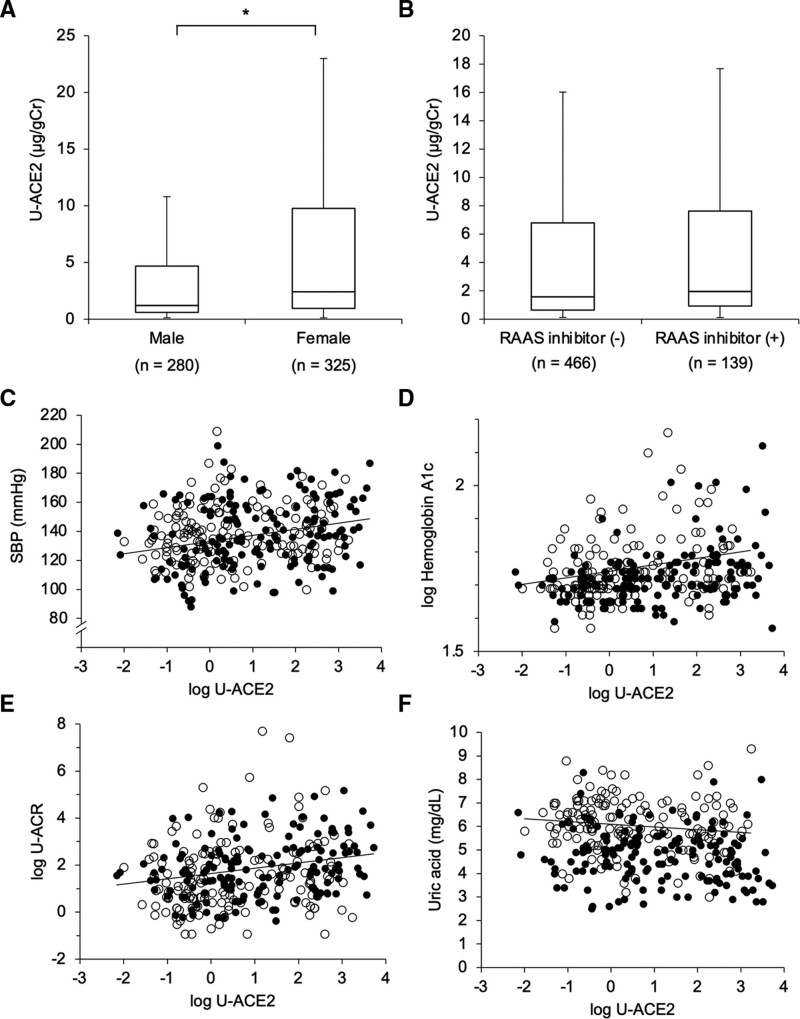
U-ACE2 was significantly higher in female subjects than in male subjects (Figure 1A). U-ACE2 levels were significantly lower in subjects with a smoking habit, alcohol drinking habit, and hyperuricemia than in those with each control, respectively (Table S1). U-ACE2 levels were significantly higher in subjects with hypertension and diabetes than in those with each control, respectively (Table S1). There was no significant difference in U-ACE2 level between subjects treated with RAAS inhibitors and those not treated with RAAS inhibitors (Figure 1B, Table S1).
Figure 1.
Comparisons and correlations of U-ACE2 (urinary angiotensin-converting enzyme 2) A and B, Comparisons of U-ACE2 levels are shown by box plots in male subjects (n=280) and female subjects (n=325; A) and in subjects treated with RAAS (renin-angiotensin-aldosterone system) inhibitors including angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and mineralocorticoid receptor antagonists (n=139, male/female: 69/70) and those not treated with RAAS inhibitors (n=466, male/female: 211/255; B). C–F, Systolic blood pressure (SBP) (C), logarithmically transformed (log) hemoglobin A1c (D), log urinary albumin-to-creatinine ratio (U-ACR; E), and uric acid (F) were plotted against log U-ACE2 in each subject. Open circle: males (n=280), closed circle: females (n=325). *P<0.05.
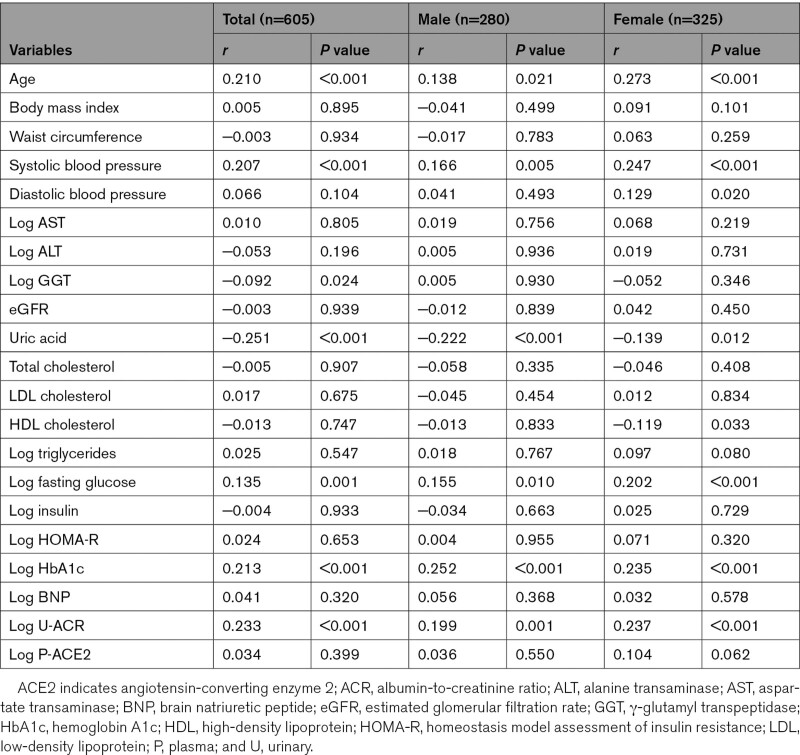
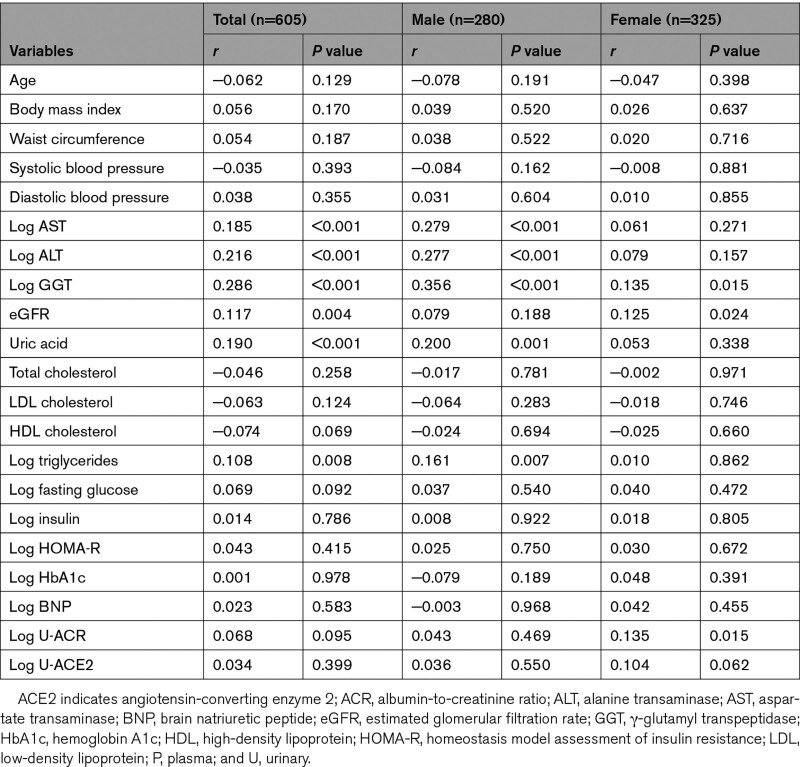
As shown in Table 2, U-ACE2 level was positively correlated with age, systolic blood pressure (Figure 1C), and levels of fasting glucose, HbA1c (Figure 1D), and U-ACR (Figure 1E) and was negatively correlated with levels of GGT and uric acid (Figure 1F). There was no significant correlation of U-ACE2 with BNP or P-ACE2 (Table 2). When the subjects were divided by sex, similar correlations were observed (Table 2).
Table 2.
Correlation Analyses for Log U-ACE2
Comparisons and Correlations of Plasma ACE2
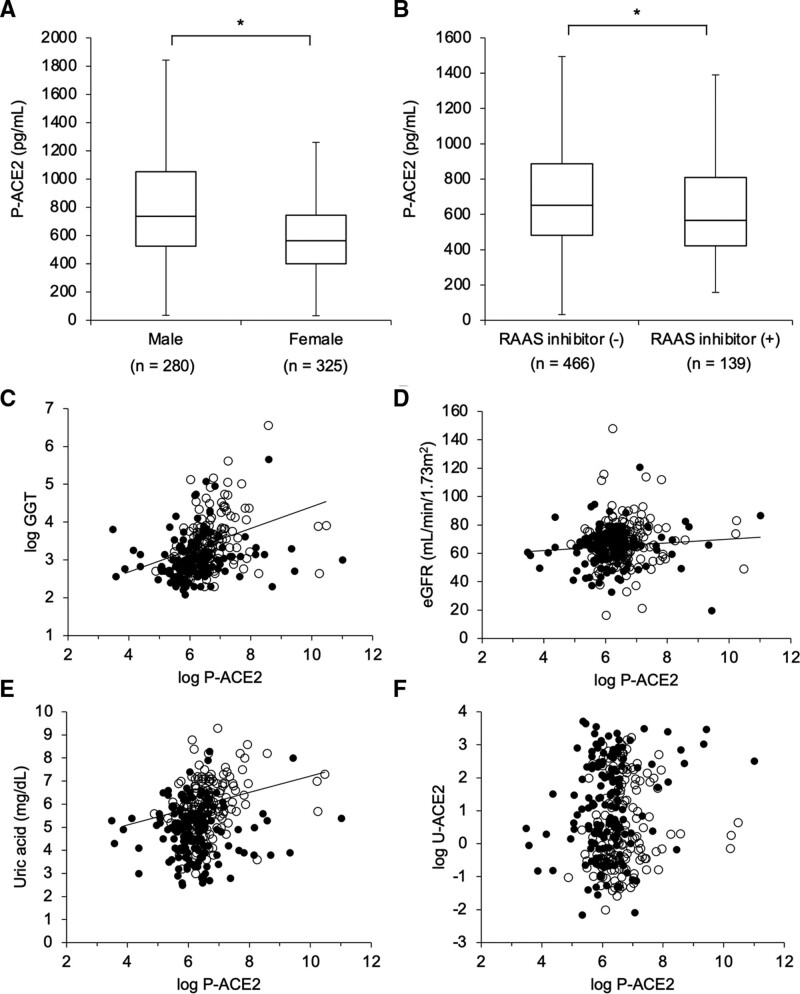
P-ACE2 level was significantly higher in male subjects than in female subjects (Figure 2A). P-ACE2 levels were significantly higher in subjects with an alcohol drinking habit and hyperuricemia than in those with each control, respectively (Table S2). P-ACE2 level was significantly lower in subjects treated with RAAS inhibitors than in those not treated with RAAS inhibitors (Figure 2B, Table S2).
Figure 2.
Comparisons and correlations of P-ACE2 (plasma angiotensin-converting enzyme 2) A and B, Comparisons of P-ACE2 levels are shown by box plots in male subjects (n=280) and female subjects (n=325, A) and in subjects treated with RAAS (renin-angiotensin-aldosterone system) inhibitors including angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and mineralocorticoid receptor antagonists (n=139, male/female: 69/70) and those not treated with RAAS inhibitors (n=466, male/female: 211/255; B). *P<0.05. C– F. Logarithmically transformed (log) GGT (γ-glutamyl transpeptidase; C), estimated glomerular filtration rate (eGFR; D), uric acid (E), and log U-ACE2 (urinary ACE2) (F) were plotted against log P-ACE2 in each subject. Open circle: males (n=280), closed circle: females (n=325).
As shown in Table 3, P-ACE2 level was positively correlated with levels of AST, ALT, GGT (Figure 2C), eGFR (Figure 2D), uric acid (Figure 2E), and triglycerides. There were no significant correlations of P-ACE2 level with parameters of glucose metabolism, BNP, U-ACR, and U-ACE2 (Figure 2F). When the subjects were divided by sex, similar correlations were observed (Table 3).
Table 3.
Correlation Analyses for Log P-ACE2
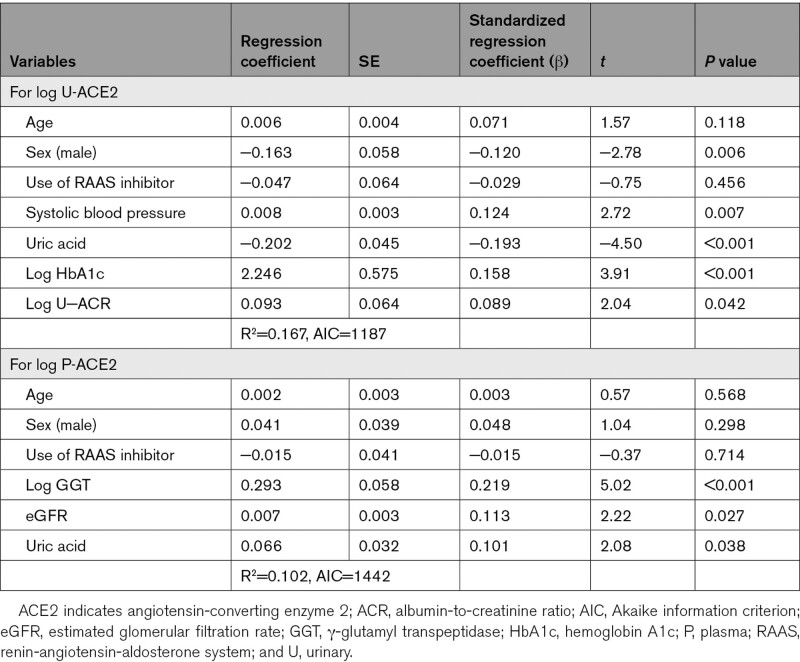
Independent Associations of U-ACE2 and P-ACE2 With Parameters
After adjustment of age, sex, and use of RAAS inhibitors, U-ACE2 level was significantly associated with systolic blood pressure and levels of uric acid, fasting glucose, HbA1c, and U-ACR (Table S3). As a consideration of multicollinearity, HbA1c (AIC: 1195), but not fasting glucose (AIC: 1199), was incorporated in further analyses for U-ACE2. Multivariable regression analysis as the best-fit model showed that female sex, high levels of systolic blood pressure, HbA1c, and U-ACR, and low uric acid level were independent predictors of high U-ACE2 level (AIC: 1187; Table 4).
Table 4.
Multivariable Regression Analyses for Log U-ACE2 and Log P-ACE2
On the other hand, after adjustment of age, sex, and use of RAAS inhibitors, P-ACE2 level was significantly associated with levels of AST, ALT, GGT, eGFR, uric acid, and triglycerides (Table S3). As a consideration of multicollinearity, GGT (AIC: 1446), but not AST (AIC: 1463) or ALT (AIC: 1464), was incorporated in further analyses for P-ACE2. Multivariable regression analysis as the best-fit model showed that high levels of GGT, eGFR, and uric acid were independent predictors of high P-ACE2 level (AIC: 1442; Table 4).
Comparisons, Correlations, and Independent Associations of FEACE2
The median level of FEACE2, a marker of the percentage of filtered ACE2 that is excreted into urine, was 2.2% (interquartile range, 0.8–7.8), and it was significantly higher in females (3.0% [1.2–10.9]) than in males (1.5% [0.6–5.5]; Table 1). Levels of FEACE2 were significantly higher in subjects with a smoking habit, hypertension, and diabetes than in those with each control, respectively (Table S4). Levels of FEACE2 were significantly lower in subjects with an alcohol drinking habit and hyperuricemia than in those with each control, respectively. FEACE2 was significantly higher in subjects treated with RAAS inhibitors than in those not treated with RAAS inhibitors.
FEACE2 was positively corelated with age, systolic blood pressure, and levels of fasting glucose, HbA1c, U-ACR, and U-ACE2 and was negatively correlated with levels of AST, ALT, GGT, uric acid, and P-ACE2 (Table S5). Multivariable regression analyses after adjustment of age, sex, eGFR, and use of RAAS inhibitors showed that high levels of systolic blood pressure and HbA1c and low levels of GGT and uric acid were independent predictors of FEACE2 (Table S6).
Discussion
The present study for the first time showed regulation of both U-ACE2 and P-ACE2 measured simultaneously in a relatively large number of subjects (n=605). Male subjects had significantly lower U-ACE2 level and higher P-ACE2 level than did female subjects, and there was no significant correlation between levels of U-ACE2 and P-ACE2. Multivariable regression analyses showed that female sex, high levels of systolic blood pressure, HbA1c, and U-ACR, and low uric acid level were independent predictors of high U-ACE2 level. On the other hand, high levels of GGT, eGFR, and uric acid were independent predictors of high P-ACE2 level. Therefore, there was an obviously distinct regulation of U-ACE2 and P-ACE2 in a Japanese general population. It has been shown that ACE2 plays a crucial role in protection against organ damage including renal and cardiovascular diseases.32,33 ACE2 is mainly a membrane-anchored tissue enzyme, and levels of soluble ACE2 cleaved by ADAM17 have been reported to be relatively low in local fluids and circulation.34 It has been shown that levels of soluble ACE2 in several fluids are reflected by physiological and pathological conditions,35 implying that amounts of U-ACE2 and P-ACE2 are compensatory responses of renal and several local tissues to insults.
It has been reported that P-ACE2 is higher in male subjects than in female subjects,22,24 although sex difference in U-ACE2 levels was not examined in previous studies.14,18–21 It was shown that the highest-ranked determinants of P-ACE2 concentrations were sex and geographic ancestry in the PURE study from 14 countries across 5 continents including Africa, Asia, Europe, North America, and South America, and it was shown that East Asians had the highest P-ACE levels.22 The ACE2 gene maps on chromosome X (Xp22.2).9 One of the 2 X chromosomes is randomly inactivated in females during development, a phenomenon called X chromosome inactivation. Although most genes are silenced, about 15% of X-linked human genes escape from the inactivation.36 The escape from X chromosome inactivation is not uniform across different tissues, and ≈10% of gene escape occurs selectively in specific tissues.36,37 A recent systematic survey of the landscape of human X-linked gene inactivation using RNA sequencing-based approaches showed that ACE2 presents remarkable differences in male-female expression levels.38 Tissue differences in the escape of X chromosome inactivation can directly translate into tissue-specific sex biases in gene expression of ACE2. It has also been reported that expression and activity of ACE2 change throughout life in a sex-specific manner and that estrogen regulates the expression and activity of ACE2 in a tissue-dependent manner.39 The escape of X chromosome inactivation and tissue-dependent regulation by estrogen of ACE2 may lead to the sex difference in U-ACE2 and P-ACE2.
ACE2 is highly expressed in the kidney, particularly within cells of the proximal tubule.16,40,41 It has been suggested that the elevated U-ACE2 is derived from the kidney rather than glomerular filtration from P-ACE2 because of the molecular weight of ACE2 (92.4–120 kDa)9 and the lack of increased ACE2 activity in urine by infusion of recombinant ACE2.17 In the present study, the median level of FEACE2, a marker of the percentage of filtered ACE2 that is excreted into urine, was 2.2% (Table 1), indicating that a part of ACE2 is filtered at the glomeruli and excreted into urine. Furthermore, high levels of systolic blood pressure and HbA1c were independent predictors of FEACE2 (Table S6). Glomerular hypertension, which has been reported to be induced by high blood pressure and high blood glucose level,42 may increase FEACE2, though the main source of U-ACE2 is derived from the kidney.
Deletion or inhibition of ACE2 was shown to be associated with albuminuria in diabetic mice43,44 and the development of angiotensin II–dependent renal damage.45 Administration of human recombinant ACE2 reduced blood pressure and attenuated glomerular injury in rodent models.46,47 ACE2 delivery by a recombinant protein or virus ameliorated the progression of diabetes-related complications such as nephropathy and retinopathy.48–50 Taken together, the earlier findings indicate that ACE2 is an endogenous protector against the progression of hypertension, diabetes, and chronic kidney disease.18,40 It has been reported that U-ACE2 is positively associated with systolic blood pressure, parameters of glucose metabolism, and U-ACR.14,21,51 We confirmed independent and positive associations of U-ACE2 with systolic blood pressure, HbA1c, and U-ACR in the present study.
On the other hand, there was no significant correlation between U-ACE2 and eGFR in the present study. Interestingly, there was a positive association of eGFR with P-ACE2 but not with U-ACE2, suggesting that a high rate of glomerular filtration, but not renal dysfunction, is an independent modulator of P-ACE2. Glomerular hyperfiltration as increased filtration per nephron unit has been reported to be a risk factor for the progression of chronic kidney disease and cardiovascular disease.52 P-ACE2 level might be a burden marker of single nephron filtration, though the mean level of eGFR (67±14 mL/min per 1.73 m2) was not high in the present study. The significance of an independent and positive association between P-ACE and eGFR remains unclear.
It has been reported that determinants of P-ACE2 include body mass index, diabetes, and increased risk of major cardiovascular events including heart failure.22,24 However, there were no significant associations of P-ACE2 level with body mass index, fasting glucose, HbA1c, and BNP in the present study. Different backgrounds of the recruited subjects may have caused the discrepancy in results since approximately half of the recruited subjects (n=290, 47.9%) in the present study were untreated and possibly healthy subjects. On the other hand, P-ACE2 was positively correlated with levels of AST, ALT and GGT, and GGT was an independent predictor of P-ACE2 in multivariable regression analysis. To the best of our knowledge, the present study is the first study showing an association of P-ACE2 with liver dysfunction. Under normal conditions, ACE2 expression in the liver is lower than that in other organs including the heart, kidneys, and intestine6,7 (Figure S1A). However, it has been reported that expression of ACE2 is increased in chronic liver diseases including hepatic fibrosis.53,54 The degree of expression and the biologic relevance of ACE2 may vary depending on the tissue and clinical state.37 As another possible mechanism, activation of ADAM17 in liver injury may cause increased P-ACE2, although the public database of the Genotype-Tissue Expression project showed that the expression level of ADAM17 (Figure S1B), but not that of TMPRSS2 (Figure S1C) as another ACE2-related protease in connection with SARS-CoV-2 infection, is relatively low in the liver.
Notably, there were opposite correlations of uric acid level with U-ACE2 and P-ACE2. There were independently negative and positive associations of uric acid with U-ACE2 and P-ACE2, respectively. The mechanism underlying the opposite associations for uric acid is unclear. The main cause of hyperuricemia is reduced urate excretion from the kidneys,55 although quantification of urate excretion was not performed in the present study. A high serum level of uric acid itself may cause insults in several tissues of the body, leading to an increase in P-ACE2. However, a high serum level of uric acid mainly due to reduced urate excretion in urine may reduce the production of ACE2 in kidneys by low urinary urate. In addition, because uric acid level has been shown to be significantly higher in male subjects than in female subjects,55–57 the sex difference in levels of P-ACE2 and U-ACE2 might be, at least in part, due to the difference in plasma and urine levels of uric acid. Notably, it has recently been reported that uric acid level was an independent predictor of deterioration of COVID-19.58 A potential role of interaction between uric acid and ACE2 might be associated with deterioration of COVID-19. Further investigations about the relationship between ACE2 and uric acid need to be performed in the future.
Earlier studies did not show significant effects of RAAS inhibitors on P-ACE222,23 and U-ACE219,21 except for a study on the effects of olmesartan on U-ACE2.14 In the present study, P-ACE2, but not U-ACE2, was significantly lower in subjects treated with RAAS inhibitors than in those not treated with RAAS inhibitors, although the mechanism remains unknown. However, the use of RAAS inhibitors was not an independent predictor of U-ACE2 or P-ACE2 in multivariable regression analyses. The effects were analyzed for multiple RAAS inhibitors including several ACE inhibitors, angiotensin II receptor blockers, and mineralocorticoid receptor antagonists and not specific to each drug in the present and previous studies. Interventional investigations for each drug among RAAS inhibitors need to be performed.
It has been suggested that a soluble recombinant ACE2 protein intercepts the virus from binding to membrane-anchored ACE2 in the cell plasma membrane.59 Restoration of ACE2 through administration of recombinant ACE2 was reported to reverse lung injury in mouse models of other viral infections.60 Clinical trials to test whether administration of recombinant ACE2 protein may be beneficial in restoring balance to the RAAS network and potentially preventing organ injury have also been arranged in patients with COVID-19 (https://www.clinicaltrials.gov; Unique identifiers: NCT04287686 and NCT04335136).5 However, viral entry through angiotensin II type 1 receptor and arginine vasopressin receptor 1B with ADAM17-mediated cleavage of ACE2 has recently been reported as a novel mechanism of SARS-CoV-2 infection.61 It has recently been reported that P-ACE2 level was unchanged in patients with COVID-19.26 However, the time course of P-ACE2 levels was not investigated. Further investigations of the association between ACE2 levels and COVID-19 are needed in the future.
Whether possible induction of ACE2 by RAAS inhibitors is beneficial or harmful for SARS-CoV-2 infection and for deterioration of lung injury in COVID-19 patients remains unclear.5 Recently, BRACE CORONA (Blockers of Angiotensin Receptor and Angiotensin-Converting Enzyme inhibitors suspension in hospitalized patients with coronavirus infection) and REPLACE COVID (Randomized Elimination or ProLongation of Angiotensin Converting Enzyme inhibitors and angiotensin receptor blockers in Coronavirus Disease 2019) randomized controlled trials showed that continuous administration of ACE inhibitors and angiotensin II receptor blockers can be safe in patients admitted to hospital with COVID-19.62,63 However, de novo effects of ACE inhibitors and angiotensin II receptor blockers on COVID-19 in subjects not receiving RAAS inhibitors are still unclear. Furthermore, effects of MR antagonists on COVID-19 have not been fully investigated.
The present study has some limitations. First, this study was a cross-sectional design, and the results of the present study relied on correlation analyses. It remains unclear whether there are direct relationships of U-ACE2 and P-ACE2 with the independent parameters. Second, the relationships between changes in U-ACE2 and P-ACE2 and time course of each parameter were not investigated in the present study. Prospective longitudinal studies are necessary for determining the significance of U-ACE2 and P-ACE2 in a general population. Third, we could not measure other components of RAAS, including angiotensinogen, renin, ACE, angiotensin II, and aldosterone, because there were not sufficient amounts of remaining blood and urine samples in the present study. Fourth, gene polymorphisms of ACE2 were not investigated in the present study, and they need to be examined in the future to provide fundamental evidence of the associations of U-ACE2 and P-ACE2 with ACE2 polymorphisms. Lastly, because only Japanese people and mainly elderly subjects were enrolled, the results of the present study might not be applicable to other races and young people.
In conclusion, U-ACE2 and P-ACE2 are distinctly regulated, and the use of RAAS inhibitors is not an independent modulator of their levels in a Japanese general population. Male individuals have significantly lower U-ACE2 level and higher P-ACE2 level than do female individuals, and there is no significant correlation between U-ACE2 and P-ACE2. U-ACE2 is associated with high blood pressure, high glucose level and microalbuminuria, and low urate level, whereas P-ACE2 is associated with liver dysfunction, high glomerular filtration rate, and high urate level.
Perspectives
ACE2 plays a crucial role in protection against organ damage including renal and cardiovascular diseases. ACE2 is mainly a membrane-anchored tissue enzyme, and levels of soluble ACE2 cleaved by ADAM17 are reflected by physiological and pathological conditions, implying that amounts of U-ACE2 and P-ACE2 are compensatory responses of renal and several local tissues to insults. Earlier studies showed that U-ACE2 is associated with hypertension, diabetes and chronic kidney disease and that P-ACE2 is associated with body mass index, diabetes, and increased risk of major cardiovascular events including heart failure. In the present study using a Japanese general population, U-ACE2 was similarly associated with high blood pressure, high glucose level, and microalbuminuria. However, P-ACE2 was differentially associated with liver dysfunction but was not associated with body mass index and parameters of glucose metabolism and heart failure. Notably, there were opposite correlations of uric acid level with U-ACE2 and P-ACE2. A further understanding of the distinct regulation of U-ACE2 and P-ACE2 may enable the development of new therapeutic strategies for metabolic and cardiovascular diseases as well as COVID-19.
Sources of Funding
M. Furuhashi has been supported by grants from Japan Society for the Promotion of Science.
Disclosures
None.
Supplementary Material
Nonstandard Abbreviations and Acronyms
- ACE
- angiotensin-converting enzyme
- ADAM17
- a disintegrin and metalloproteinase 17
- AIC
- Akaike information criterion
- ALT
- alanine transaminase
- AST
- aspartate transaminase
- BNP
- brain natriuretic peptide
- COVID-19
- coronavirus disease 2019
- eGFR
- estimated glomerular filtration rate
- FEACE2
- fractional excretion of ACE2
- GGT
- γ-glutamyl transpeptidase
- HbA1c
- hemoglobin A1c
- HDL
- high-density lipoprotein
- LDL
- low-density lipoprotein
- P-ACE2
- plasma ACE2
- PURE
- Prospective Urban Rural Epidemiology
- RAAS
- renin-angiotensin-aldosterone system
- SARS-CoV-2
- severe acute respiratory syndrome coronavirus 2
- TMPRSS2
- transmembrane protease serine 2
- U-ACE2
- urinary ACE2
- U-ACR
- urinary albumin-to-creatinine ratio
For Sources of Funding and Disclosures, see page 1148.
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/HYPERTENSIONAHA.121.17674.
Contributor Information
Akiko Sakai, Email: akiko1119jp@yahoo.co.jp.
Marenao Tanaka, Email: tanakamarenao@yahoo.co.jp.
Yukimura Higashiura, Email: corosukecorocororin8@icloud.com.
Kazuma Mori, Email: kirakunifujinoki@yahoo.co.jp.
Masayuki Koyama, Email: masa3yuki3@hotmail.com.
Hirofumi Ohnishi, Email: hohnishi@sapmed.ac.jp.
Shigeyuki Saitoh, Email: ssaitoh@sapmed.ac.jp.
Kazuaki Shimamoto, Email: k_shimamoto@nihoniryo-c.ac.jp.
Novelty and Significance
What Is New?
This is the first study showing regulation of P-ACE2 (plasma angiotensin-converting enzyme 2) and U-ACE2 (urinary ACE2) measured simultaneously and alterations in their levels caused by renin-angiotensin-aldosterone system inhibitors in a general population.
What Is Relevant?
ACE2 plays a crucial role in protection against organ damage, including renal and cardiovascular diseases, and levels of soluble ACE2 cleaved in fluids are reflected by physiological and pathological conditions. There is a distinct regulation of U-ACE2 and P-ACE2.
Summary
U-ACE2 and P-ACE2 are distinctly regulated, and the use of renin-angiotensin-aldosterone system inhibitors is not an independent modulator of their levels in a Japanese general population. Male individuals have significantly lower U-ACE2 level and higher P-ACE2 level than do female individuals, and there is no significant correlation between U-ACE2 and P-ACE2. U-ACE2 is associated with high blood pressure, high glucose level and microalbuminuria, and low urate level. However, P-ACE2 is associated with liver dysfunction, high glomerular filtration rate, and high urate level.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, Guo L, Guo R, Chen T, Hu J, et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun. 2020;11:1620. doi: 10.1038/s41467-020-15562-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zumla A, Chan JF, Azhar EI, Hui DS, Yuen KY. Coronaviruses - drug discovery and therapeutic options. Nat Rev Drug Discov. 2016;15:327–347. doi: 10.1038/nrd.2015.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Furuhashi M, Moniwa N, Takizawa H, Ura N, Shimamoto K. Potential differential effects of renin-angiotensin system inhibitors on SARS-CoV-2 infection and lung injury in COVID-19. Hypertens Res. 2020;43:837–840. doi: 10.1038/s41440-020-0478-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single-cell rna-seq data analysis on the receptor ace2 expression reveals the potential risk of different human organs vulnerable to 2019-ncov infection. Front Med. 2020;14:185–192. doi: 10.1007/s11684-020-0754-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hikmet F, Méar L, Edvinsson Å, Micke P, Uhlén M, Lindskog C. The protein expression profile of ACE2 in human tissues. Mol Syst Biol. 2020;16:e9610. doi: 10.15252/msb.20209610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kato T, Hagiyama M, Ito A. Renal ADAM10 and 17: their physiological and medical meanings. Front Cell Dev Biol. 2018;6:153. doi: 10.3389/fcell.2018.00153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem. 2000;275:33238–33243. doi: 10.1074/jbc.M002615200 [DOI] [PubMed] [Google Scholar]
- 10.Ingelfinger JR. Angiotensin-converting enzyme 2: implications for blood pressure and kidney disease. Curr Opin Nephrol Hypertens. 2009;18:79–84. doi: 10.1097/MNH.0b013e32831b70ad [DOI] [PubMed] [Google Scholar]
- 11.Forrester SJ, Booz GW, Sigmund CD, Coffman TM, Kawai T, Rizzo V, Scalia R, Eguchi S. Angiotensin II signal transduction: an update on mechanisms of physiology and pathophysiology. Physiol Rev. 2018;98:1627–1738. doi: 10.1152/physrev.00038.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agata J, Ura N, Yoshida H, Shinshi Y, Sasaki H, Hyakkoku M, Taniguchi S, Shimamoto K. Olmesartan is an angiotensin II receptor blocker with an inhibitory effect on angiotensin-converting enzyme. Hypertens Res. 2006;29:865–874. doi: 10.1291/hypres.29.865 [DOI] [PubMed] [Google Scholar]
- 13.Kreutz R, Algharably EAE, Azizi M, Dobrowolski P, Guzik T, Januszewicz A, Persu A, Prejbisz A, Riemer TG, Wang JG, et al. Hypertension, the renin-angiotensin system, and the risk of lower respiratory tract infections and lung injury: implications for COVID-19. Cardiovasc Res. 2020;116:1688–1699. doi: 10.1093/cvr/cvaa097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Furuhashi M, Moniwa N, Mita T, Fuseya T, Ishimura S, Ohno K, Shibata S, Tanaka M, Watanabe Y, Akasaka H, et al. Urinary angiotensin-converting enzyme 2 in hypertensive patients may be increased by olmesartan, an angiotensin II receptor blocker. Am J Hypertens. 2015;28:15–21. doi: 10.1093/ajh/hpu086 [DOI] [PubMed] [Google Scholar]
- 15.Warner FJ, Lew RA, Smith AI, Lambert DW, Hooper NM, Turner AJ. Angiotensin-converting enzyme 2 (ACE2), but not ACE, is preferentially localized to the apical surface of polarized kidney cells. J Biol Chem. 2005;280:39353–39362. doi: 10.1074/jbc.M508914200 [DOI] [PubMed] [Google Scholar]
- 16.Shaltout HA, Westwood BM, Averill DB, Ferrario CM, Figueroa JP, Diz DI, Rose JC, Chappell MC. Angiotensin metabolism in renal proximal tubules, urine, and serum of sheep: evidence for ACE2-dependent processing of angiotensin II. Am J Physiol Renal Physiol. 2007;292:F82–F91. doi: 10.1152/ajprenal.00139.2006 [DOI] [PubMed] [Google Scholar]
- 17.Wysocki J, Garcia-Halpin L, Ye M, Maier C, Sowers K, Burns KD, Batlle D. Regulation of urinary ACE2 in diabetic mice. Am J Physiol Renal Physiol. 2013;305:F600–F611. doi: 10.1152/ajprenal.00600.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang G, Lai FM, Lai KB, Chow KM, Kwan CH, Li KT, Szeto CC. Urinary mRNA expression of ACE and ACE2 in human type 2 diabetic nephropathy. Diabetologia. 2008;51:1062–1067. doi: 10.1007/s00125-008-0988-x [DOI] [PubMed] [Google Scholar]
- 19.Mizuiri S, Aoki T, Hemmi H, Arita M, Sakai K, Aikawa A. Urinary angiotensin-converting enzyme 2 in patients with CKD. Nephrology (Carlton). 2011;16:567–572. doi: 10.1111/j.1440-1797.2011.01467.x [DOI] [PubMed] [Google Scholar]
- 20.Xiao F, Hiremath S, Knoll G, Zimpelmann J, Srivaratharajah K, Jadhav D, Fergusson D, Kennedy CR, Burns KD. Increased urinary angiotensin-converting enzyme 2 in renal transplant patients with diabetes. PLoS One. 2012;7:e37649. doi: 10.1371/journal.pone.0037649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park SE, Kim WJ, Park SW, Park JW, Lee N, Park CY, Youn BS. High urinary ACE2 concentrations are associated with severity of glucose intolerance and microalbuminuria. Eur J Endocrinol. 2013;168:203–210. doi: 10.1530/EJE-12-0782 [DOI] [PubMed] [Google Scholar]
- 22.Narula S, Yusuf S, Chong M, Ramasundarahettige C, Rangarajan S, Bangdiwala SI, van Eikels M, Leineweber K, Wu A, Pigeyre M, et al. Plasma ACE2 and risk of death or cardiometabolic diseases: a case-cohort analysis. Lancet. 2020;396:968–976. doi: 10.1016/S0140-6736(20)31964-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sama IE, Ravera A, Santema BT, van Goor H, Ter Maaten JM, Cleland JGF, Rienstra M, Friedrich AW, Samani NJ, Ng LL, et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J. 2020;41:1810–1817. doi: 10.1093/eurheartj/ehaa373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hisatake S, Kiuchi S, Kabuki T, Oka T, Dobashi S, Ikeda T. Serum angiotensin-converting enzyme 2 concentration and angiotensin-(1-7) concentration in patients with acute heart failure patients requiring emergency hospitalization. Heart Vessels. 2017;32:303–308. doi: 10.1007/s00380-016-0877-z [DOI] [PubMed] [Google Scholar]
- 25.Mogi M, Kawajiri M, Tsukuda K, Matsumoto S, Yamada T, Horiuchi M. Serum levels of renin-angiotensin system components in acute stroke patients. Geriatr Gerontol Int. 2014;14:793–798. doi: 10.1111/ggi.12167 [DOI] [PubMed] [Google Scholar]
- 26.Rieder M, Wirth L, Pollmeier L, Jeserich M, Goller I, Baldus N, Schmid B, Busch HJ, Hofmann M, Kern W, et al. Serum ACE2, Angiotensin II, and Aldosterone levels are unchanged in patients with COVID-19. Am J Hypertens. 2021;34:278–281. doi: 10.1093/ajh/hpaa169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ishimura S, Furuhashi M, Watanabe Y, Hoshina K, Fuseya T, Mita T, Okazaki Y, Koyama M, Tanaka M, Akasaka H, et al. Circulating levels of fatty acid-binding protein family and metabolic phenotype in the general population. PLoS One. 2013;8:e81318. doi: 10.1371/journal.pone.0081318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 29.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883 [DOI] [PubMed] [Google Scholar]
- 30.Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A; Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–992. doi: 10.1053/j.ajkd.2008.12.034 [DOI] [PubMed] [Google Scholar]
- 31.American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017;40:S11–S24. doi: 10.2337/dc17-S005 [DOI] [PubMed] [Google Scholar]
- 32.Wysocki J, Ye M, Soler MJ, Gurley SB, Xiao HD, Bernstein KE, Coffman TM, Chen S, Batlle D. ACE and ACE2 activity in diabetic mice. Diabetes. 2006;55:2132–2139. doi: 10.2337/db06-0033 [DOI] [PubMed] [Google Scholar]
- 33.Alghamri MS, Weir NM, Anstadt MP, Elased KM, Gurley SB, Morris M. Enhanced angiotensin II-induced cardiac and aortic remodeling in ACE2 knockout mice. J Cardiovasc Pharmacol Ther. 2013;18:138–151. doi: 10.1177/1074248412460124 [DOI] [PubMed] [Google Scholar]
- 34.Wysocki J, Batlle D. Reduced plasma ACE2 activity in dialysis patients: another piece in the conundrum of factors involved in hypertension and cardiovascular morbidity? Nephrol Dial Transplant. 2013;28:2200–2202. doi: 10.1093/ndt/gft240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bitker L, Burrell LM. Classic and nonclassic renin-angiotensin systems in the critically Ill. Crit Care Clin. 2019;35:213–227. doi: 10.1016/j.ccc.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prothero KE, Stahl JM, Carrel L. Dosage compensation and gene expression on the mammalian X chromosome: one plus one does not always equal two. Chromosome Res. 2009;17:637–648. doi: 10.1007/s10577-009-9063-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pirola CJ, Sookoian S. COVID-19 and ACE2 in the liver and gastrointestinal tract: putative biological explanations of sexual dimorphism. Gastroenterology. 2020;159:1620–1621. doi: 10.1053/j.gastro.2020.04.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tukiainen T, Villani AC, Yen A, Rivas MA, Marshall JL, Satija R, Aguirre M, Gauthier L, Fleharty M, Kirby A, et al. ; GTEx Consortium; Laboratory, Data Analysis &Coordinating Center (LDACC)—Analysis Working Group; Statistical Methods groups—Analysis Working Group; Enhancing GTEx (eGTEx) groups; NIH Common Fund; NIH/NCI; NIH/NHGRI; NIH/NIMH; NIH/NIDA; Biospecimen Collection Source Site—NDRI; Biospecimen Collection Source Site—RPCI; Biospecimen Core Resource—VARI; Brain Bank Repository—University of Miami Brain Endowment Bank; Leidos Biomedical—Project Management; ELSI Study; Genome Browser Data Integration &Visualization—EBI; Genome Browser Data Integration &Visualization—UCSC Genomics Institute, University of California Santa Cruz. Landscape of X chromosome inactivation across human tissues. Nature. 2017;550:244–248. doi: 10.1038/nature2426529022598 [Google Scholar]
- 39.Viveiros A, Rasmuson J, Vu J, Mulvagh SL, Yip CYY, Norris CM, Oudit GY. Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones. Am J Physiol Heart Circ Physiol. 2021;320:H296–H304. doi: 10.1152/ajpheart.00755.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ye M, Wysocki J, Naaz P, Salabat MR, LaPointe MS, Batlle D. Increased ACE 2 and decreased ACE protein in renal tubules from diabetic mice: a renoprotective combination? Hypertension. 2004;43:1120–1125. doi: 10.1161/01.HYP.0000126192.27644.76 [DOI] [PubMed] [Google Scholar]
- 41.Li N, Zimpelmann J, Cheng K, Wilkins JA, Burns KD. The role of angiotensin converting enzyme 2 in the generation of angiotensin 1-7 by rat proximal tubules. Am J Physiol Renal Physiol. 2005;288:F353–F362. doi: 10.1152/ajprenal.00144.2004 [DOI] [PubMed] [Google Scholar]
- 42.Helal I, Fick-Brosnahan GM, Reed-Gitomer B, Schrier RW. Glomerular hyperfiltration: definitions, mechanisms and clinical implications. Nat Rev Nephrol. 2012;8:293–300. doi: 10.1038/nrneph.2012.19 [DOI] [PubMed] [Google Scholar]
- 43.Wong DW, Oudit GY, Reich H, Kassiri Z, Zhou J, Liu QC, Backx PH, Penninger JM, Herzenberg AM, Scholey JW. Loss of angiotensin-converting enzyme-2 (Ace2) accelerates diabetic kidney injury. Am J Pathol. 2007;171:438–451. doi: 10.2353/ajpath.2007.060977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Soler MJ, Wysocki J, Ye M, Lloveras J, Kanwar Y, Batlle D. ACE2 inhibition worsens glomerular injury in association with increased ACE expression in streptozotocin-induced diabetic mice. Kidney Int. 2007;72:614–623. doi: 10.1038/sj.ki.5002373 [DOI] [PubMed] [Google Scholar]
- 45.Oudit GY, Herzenberg AM, Kassiri Z, Wong D, Reich H, Khokha R, Crackower MA, Backx PH, Penninger JM, Scholey JW. Loss of angiotensin-converting enzyme-2 leads to the late development of angiotensin II-dependent glomerulosclerosis. Am J Pathol. 2006;168:1808–1820. doi: 10.2353/ajpath.2006.051091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wysocki J, Ye M, Rodriguez E, González-Pacheco FR, Barrios C, Evora K, Schuster M, Loibner H, Brosnihan KB, Ferrario CM, et al. Targeting the degradation of angiotensin II with recombinant angiotensin-converting enzyme 2: prevention of angiotensin II-dependent hypertension. Hypertension. 2010;55:90–98. doi: 10.1161/HYPERTENSIONAHA.109.138420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oudit GY, Liu GC, Zhong J, Basu R, Chow FL, Zhou J, Loibner H, Janzek E, Schuster M, Penninger JM, et al. Human recombinant ACE2 reduces the progression of diabetic nephropathy. Diabetes. 2010;59:529–538. doi: 10.2337/db09-1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Verma A, Shan Z, Lei B, Yuan L, Liu X, Nakagawa T, Grant MB, Lewin AS, Hauswirth WW, Raizada MK, et al. ACE2 and Ang-(1-7) confer protection against development of diabetic retinopathy. Mol Ther. 2012;20:28–36. doi: 10.1038/mt.2011.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu CX, Hu Q, Wang Y, Zhang W, Ma ZY, Feng JB, Wang R, Wang XP, Dong B, Gao F, et al. Angiotensin-converting enzyme (ACE) 2 overexpression ameliorates glomerular injury in a rat model of diabetic nephropathy: a comparison with ACE inhibition. Mol Med. 2011;17:59–69. doi: 10.2119/molmed.2010.00111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nadarajah R, Milagres R, Dilauro M, Gutsol A, Xiao F, Zimpelmann J, Kennedy C, Wysocki J, Batlle D, Burns KD. Podocyte-specific overexpression of human angiotensin-converting enzyme 2 attenuates diabetic nephropathy in mice. Kidney Int. 2012;82:292–303. doi: 10.1038/ki.2012.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ni X, Sun C, Tian Y, Huang Y, Gong T, Song L, Yang X, Li K, Zheng N, Wang J, et al. Could urinary ACE2 protein level help identify individuals susceptible to SARS-CoV-2 infection and complication? Sci China Life Sci. 2020;63:1766–1767. doi: 10.1007/s11427-020-1759-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kanbay M, Ertuglu LA, Afsar B, Ozdogan E, Kucuksumer ZS, Ortiz A, Covic A, Kuwabara M, Cherney DZI, van Raalte DH, et al. Renal hyperfiltration defined by high estimated glomerular filtration rate: a risk factor for cardiovascular disease and mortality. Diabetes Obes Metab. 2019;21:2368–2383. doi: 10.1111/dom.13831 [DOI] [PubMed] [Google Scholar]
- 53.Warner FJ, Rajapaksha H, Shackel N, Herath CB. ACE2: from protection of liver disease to propagation of COVID-19. Clin Sci (Lond). 2020;134:3137–3158. doi: 10.1042/CS20201268 [DOI] [PubMed] [Google Scholar]
- 54.Rajapaksha IG, Gunarathne LS, Angus PW, Herath CB. Update on new aspects of the Renin-Angiotensin system in hepatic fibrosis and portal hypertension: implications for novel therapeutic options. J Clin Med. 2021;10:702. doi: 10.3390/jcm10040702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dalbeth N, Choi HK, Joosten LAB, Khanna PP, Matsuo H, Perez-Ruiz F, Stamp LK. Gout. Nat Rev Dis Primers. 2019;5:69. doi: 10.1038/s41572-019-0115-y [DOI] [PubMed] [Google Scholar]
- 56.Furuhashi M, Mori K, Tanaka M, Maeda T, Matsumoto M, Murase T, Nakamura T, Koyama M, Moniwa N, Ohnishi H, et al. Unexpected high plasma xanthine oxidoreductase activity in female subjects with low levels of uric acid. Endocr J. 2018;65:1083–1092. doi: 10.1507/endocrj.EJ18-0127 [DOI] [PubMed] [Google Scholar]
- 57.Mori K, Furuhashi M, Tanaka M, Numata K, Hisasue T, Hanawa N, Koyama M, Osanami A, Higashiura Y, Inyaku M, et al. U-shaped relationship between serum uric acid level and decline in renal function during a 10-year period in female subjects: BOREAS-CKD2. Hypertens Res. 2021;44:107–116. doi: 10.1038/s41440-020-0532-z [DOI] [PubMed] [Google Scholar]
- 58.Ishii M, Terai H, Kabata H, Masaki K, Chubachi S, Tateno H, Nakamura M, Nishio K, Koh H, Watanabe R, et al. ; Keio COVID-19 Research Consortium (K-CORC) and the Keio Donner Project Team. Clinical characteristics of 345 patients with coronavirus disease 2019 in Japan: a multicenter retrospective study. J Infect. 2020;81:e3–e5. doi: 10.1016/j.jinf.2020.08.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Batlle D, Wysocki J, Satchell K. Soluble angiotensin-converting enzyme 2: a potential approach for coronavirus infection therapy? Clin Sci (Lond). 2020;134:543–545. doi: 10.1042/CS20200163 [DOI] [PubMed] [Google Scholar]
- 60.Zou Z, Yan Y, Shu Y, Gao R, Sun Y, Li X, Ju X, Liang Z, Liu Q, Zhao Y, et al. Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections. Nat Commun. 2014;5:3594. doi: 10.1038/ncomms4594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yeung ML, Teng JLL, Jia L, Zhang C, Huang C, Cai JP, Zhou R, Chan KH, Zhao H, Zhu L, et al. Soluble ACE2-mediated cell entry of SARS-CoV-2 via interaction with proteins related to the renin-angiotensin system. Cell. 2021;184:2212–2228.e12. doi: 10.1016/j.cell.2021.02.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lopes RD, Macedo AVS, de Barros E Silva PGM, Moll-Bernardes RJ, Dos Santos TM, Mazza L, Feldman A, D’Andréa Saba Arruda G, de Albuquerque DC, Camiletti AS, et al. ; BRACE CORONA Investigators. Effect of discontinuing vs continuing Angiotensin-converting enzyme inhibitors and Angiotensin II receptor blockers on days alive and out of the hospital in patients admitted with COVID-19: a randomized clinical trial. JAMA. 2021;325:254–264. doi: 10.1001/jama.2020.25864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cohen JB, Hanff TC, William P, Sweitzer N, Rosado-Santander NR, Medina C, Rodriguez-Mori JE, Renna N, Chang TI, Corrales-Medina V, et al. Continuation versus discontinuation of renin-angiotensin system inhibitors in patients admitted to hospital with COVID-19: a prospective, randomised, open-label trial. Lancet Respir Med. 2021;9:275–284. doi: 10.1016/S2213-2600(20)30558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.