Abstract
Renovascular hypertension is one of the most common forms of secondary hypertension. Over 95% of cases of renovascular hypertension are due either to atherosclerosis of the main renal artery trunks or to fibromuscular dysplasia. These two causes of renal artery stenosis have been extensively discussed in recent reviews and consensus. The aim of the current article is to provide comprehensive and up-to-date information on the remaining causes. While these causes are rare or extremely rare, etiologic and differential diagnosis matters both for prognosis and management. Therefore, the clinician cannot ignore them. For didactic reasons, we have grouped these different entities into stenotic lesions (neurofibromatosis type 1 and other rare syndromes, dissection, arteritis, and segmental arterial mediolysis) often associated with aortic coarctation and other arterial abnormalities, and nonstenotic lesions, where hypertension is secondary to compression of adjacent arteries and changes in arterial pulsatility (aneurysm) or to the formation of a shunt, leading to kidney ischemia (arteriovenous fistula). Finally, thrombotic disorders of the renal artery may also be responsible for renovascular hypertension. Although thrombotic/embolic lesions do not represent primary vessel wall disease, they are characterized by frequent macrovascular involvement. In this review, we illustrate the most characteristic aspects of these different entities responsible for renovascular hypertension and discuss their prevalence, pathophysiology, clinical presentation, management, and prognosis.
Keywords: aneurysm; arteriovenous fistula; dissection; hypertension, renovascular; neurofibromatosis 1
Renovascular hypertension (RVHT), usually caused by renal artery stenosis (RAS), is one of the most common causes of secondary hypertension. RAS may result in the development of resistant hypertension, a progressive decline in renal function and cardiac destabilization syndromes, which may include flash pulmonary edema or congestive heart failure.1,2 The most common cause of RVHT is atherosclerosis of the main renal artery, and most of the remaining cases are attributed to fibromuscular dysplasia (FMD). Atherosclerotic RAS accounts for ≈90% of cases of RAS and is more common in populations with other atherosclerotic lesions or risk factors, including increasing age, diabetes, smoking history, hypertension, or coronary artery disease.3,4 In contrast, FMD is typically diagnosed in young- or middle-aged women and is seldom accompanied by a significant loss in renal function.3,5 It may be occasionally observed in men and older patients, sometimes coexisting with atherosclerotic lesions.
Less commonly encountered types of renal artery disease associated with RVHT include neurofibromatosis type 1 (NF1), midaortic syndrome, renal artery aneurysm (RAA), and arteriovenous fistula.1 Even rarer causes have been described in the literature (Table). Of note, the existing literature dealing with these rare entities mostly consists of case reports, small clinical series, or reviews. In addition, the prevalence and incidence of these lesions and malformations in the general population is not clearly established and may be overestimated, as most cases have been diagnosed in tertiary referral centers. In recent decades, such rare causes of RVHT are, nevertheless, increasingly identified due to extensive use of noninvasive imaging techniques.
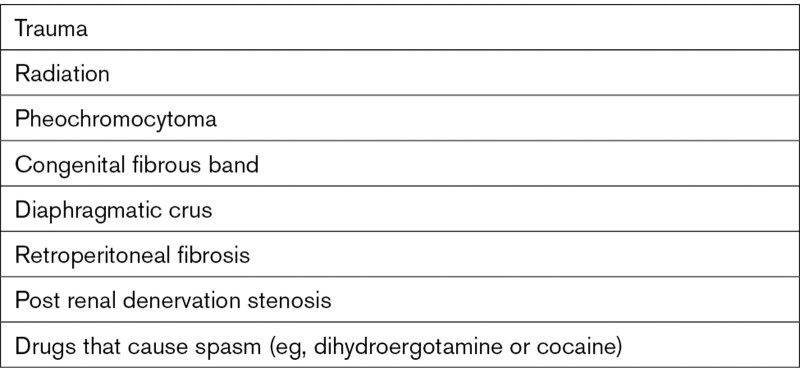
Table.
Rare Additional Stenotic Causes6
However, clinical management of patients with rare renal artery diseases deserves to be individualized because of marked differences in the processes underlying these different lesions. Altered geometry and flow in the renal artery can lead to renin-dependent hypertension. Other changes in renal artery geometry, for example, RAA, may alter flow sufficiently to affect the pressure difference between the ostium of the renal artery and kidney baroreceptors.
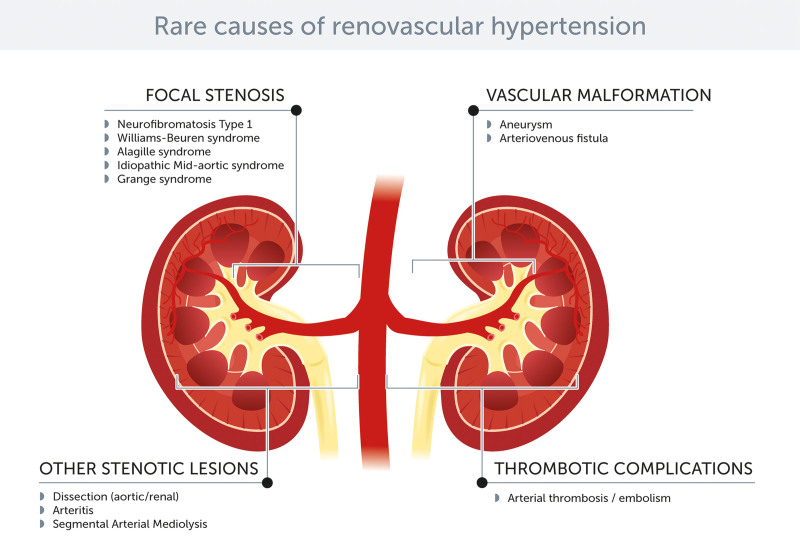
All rare causes of RVHT may be subdivided into stenotic and nonstenotic lesions (Figure 1). Patients with stenotic lesions (NF1, midaortic syndrome, dissection, arteritis, or segmental arterial mediolysis [SAM]; Figure 2) exhibit an unusually high frequency of arterial abnormalities, including abdominal aortic coarctation or diffuse narrowing of renal arteries of variable lengths. Patients with nonstenotic lesions, namely aneurysms and arteriovenous fistulae, may develop hypertension due to compression of the adjacent arteries and changes in the pulsatile character of blood flow (aneurysm) or formation of a shunt, resulting in local kidney ischemia (arteriovenous fistula). Finally, thrombotic disorders of the renal artery may also produce RVHT (Figure 3). Although thrombotic/embolic lesions do not represent primary vessel wall disease, they do contribute to RVHT.
Figure 1.
Rare causes of renovascular hypertension in a nutshell.
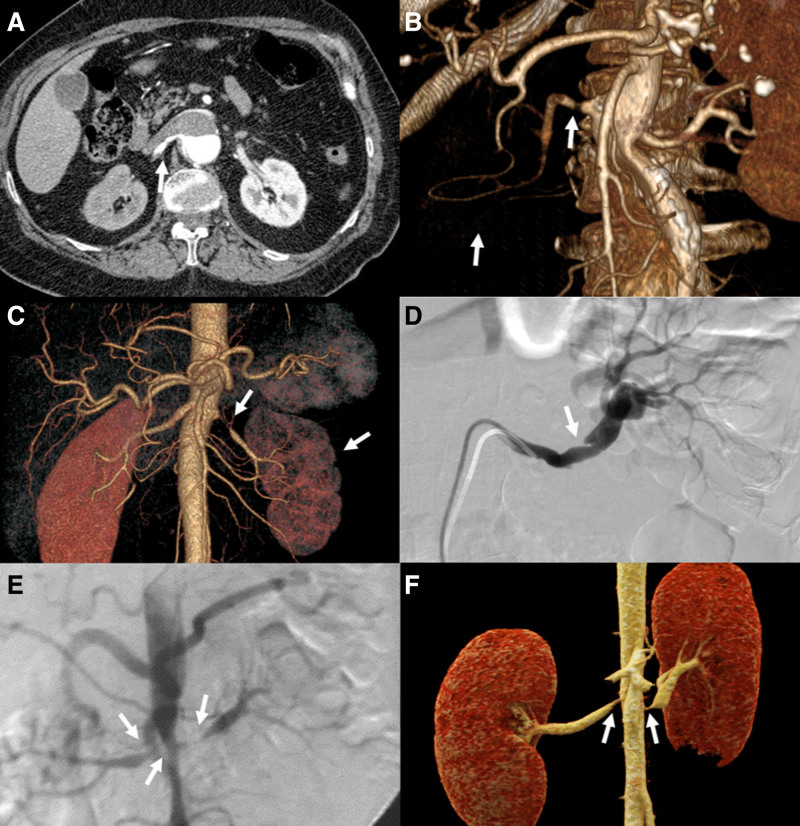
Figure 2.
Rare causes of renovascular hypertension—stenotic lesions. A, A 64-y-old woman with type B aortic dissection. Axial plane shows false lumen protruding into the right renal artery causing severe static type stenosis (arrow). B, Three-dimensional reconstruction of the abdominal aorta in the same patient shows a stenosis of the right renal artery (arrow) and reduced opacification of right renal parenchyma (arrow). C, A 46-y-old woman, treated for arteritis. Computed tomographic angiography (CTA) performed during workup for difficult-to-control hypertension shows high-grade renal artery stenosis (arrow) with left kidney decreased size (arrow). D, A 62-y-old woman with moderate hypertension. Angiography, performed following noninvasive CTA diagnostic examination to plan endovascular treatment (stent), shows dissection of left renal artery (arrow). E, Angiography of an 11-y-old boy with neurofibromatosis type 1 (NF1) showing stenosis of aorta and both renal arteries (arrows). F, Three-dimensional image of the abdominal arteries depicting bilateral renal arteries stenoses (arrows) in a 12-y-old boy with NF1.
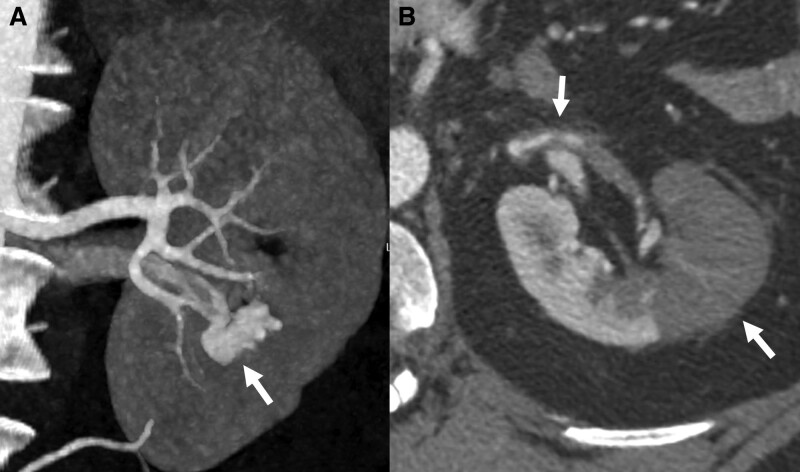
Figure 3.
Rare causes of renovascular hypertension—nonstenotic lesions. A, Female patient, 37-y-old, with moderate hypertension, screened for secondary causes of hypertension. Computed tomographic angiography (CTA) shows an arteriovenous fistula in the lower part of left kidney (arrow). B, Male patient, 35-y-old, with left flank pain at admission and worsening hypertension control. CTA performed after ultrasound screening discloses a thrombus in the abdominal branch of left renal artery (arrow), with parenchymal ischemia visible in axial scan (arrow).
In the absence of a recent and comprehensive review on the topic, we set out to describe the rare causes of RVHT, their incidence, pathophysiology, clinical presentation, radiological features, treatment, and prognosis. Our sole focus on only the rare causes of RVHT makes this review unique.
Neurofibromatosis Type 1
NF1 or Von Recklinghausen disease is a rare autosomal dominant disorder. NF1 is characterized by café-au-lait macules, neurofibromas, Lisch nodules of the iris, axillary freckling, optic nerve gliomas, and distinctive bone lesions. Phaeochromocytomas can occur in up to 5% of patients. NF1 and NF1 vasculopathy are primarily diagnosed in childhood.
Hypertension occurs in 16% to 19% of children with NF1, and its prevalence increases with age.7–10 Patients can present with symptomatic severe hypertension. However, hypertension is often an incidental finding detected during admission for another reason. Conversely, NF1 may only be diagnosed during the workup of hypertension, especially in children and young adults.11,12 End-organ damage, especially left ventricle hypertrophy, can already be present as well.11–13 Twenty-four–hour ambulatory blood pressure (BP) monitoring is advised, as some children with vascular lesions and normal office BP may have masked hypertension, particularly during the night.9 Sometimes, an abdominal bruit is observed during physical examination.
The most frequent cause of hypertension in children with NF1 is RAS, with a highly variable reported frequency from 7% to 58% and with a mean age at diagnosis of hypertension being 11.2 years.14,15
The pathogenesis of the vasculopathy in NF1 is not completely elucidated. Besides genetic predisposition, the vasculopathy also appears to be an acquired progressive condition. The loss of neurofibromin, which also acts as a tumor suppressor gene, produces increased mitogenic signaling and leads to increased cellular proliferation/differentiation. Arterial stenoses or aneurysms might develop through a complex process of cellular proliferation, degeneration, healing, smooth muscle loss, and fibrosis caused by deficiency in neurofibromin within the endothelium and smooth muscle cells of the arterial wall.16
To our knowledge, data on the rate of progression of vascular disease are scarce and anecdotal. Vasculopathy of NF1 tends to be progressive and rapid progression of RAS, from 70% to 90% in 1 month, has been reported.11,12,16,17
In a review of 237 patients with NF1, 320 vascular abnormalities were found. Renal artery lesions were the most frequent (41%), were unilateral in 68%, were more often stenotic than aneurysmal, and were found at all segments of the renal artery to the intraparenchymal branches.14,18 Bilateral and concomitant stenoses of other arteries are frequent and may include midaortic syndrome and stenoses of the celiac axis and the superior or inferior mesenteric arteries.12 Coronary and extra- and intracranial cerebrovascular disease, particularly aneurysms, are also observed in many patients.14,19 The renal artery lesions may be long and tapered, extending into the primary branches of the artery and sparing its aortic origin, as well as single and short (<10 mm) with ostial involvement.16,20
The current consensus is that noninvasive diagnostic imaging of the RA should be considered first, when RA stenosis is clinically suspected.15,21 However, none is a substitute for conventional angiography as the accuracy of these tests to detect RAS in NF1 may be lower due to the morphological complexity of the arterial lesions.11
Treatment depends on patient’s age and the type and location of the lesion. Isolated renal artery disease has been treated with medical therapy, percutaneous transluminal angioplasty (PTA) with or without stenting, open bypass surgery, ex vivo surgical repair with renal autotransplantation, or even nephrectomy.4,13,16 Despite pharmacological treatment not being satisfactory in many cases, medical treatment is often advised as the initial approach to control hypertension to allow maximal body growth in children before any intervention.9,22
Endovascular treatment is generally accepted as a first-line invasive therapy for RAS due to NF1, because of the absence of major complications and no adverse effect on subsequent vascular reconstruction. Open surgical repair is usually reserved for complex vascular lesions or PTA failure/complications. Arterial stenting is generally avoided in the pediatric population unless angioplasty results in a flow-limiting dissection, complete recoil of stenosis, or focal arterial rupture.15,17
Survival is 10 to 20 years shorter in patients with NFI compared with the general population. After malignancy, vascular disease is the second leading cause of death, especially among individuals aged <40 years. Severe hypertension is the most frequently described life-threatening or fatal complication in young patients with NF1.7,16,23
Resolution of arterial abnormalities and cure/improvement of hypertension depends on the extent and location of the lesions. Diffuse intrarenal vessel involvement, renal end-organ damage secondary to persistent hypertension, or the presence of aortic involvement may preclude the success of revascularization in improving BP control.9,13 PTA and open surgical repair have a good technical success rate (67%–72% and 78%–90%, respectively) with resolution of hypertension in up to 71% and 97% of patients, respectively.8,17,22,24,25 Restenosis after PTA has been reported in up to 44% of cases.17 As the vasculopathy in NF1 is a progressive disease and the vascular malformations may recur after revascularization, long-term monitoring of these patients is strongly advised.
Other Rare Syndromic Causes of Focal RAS
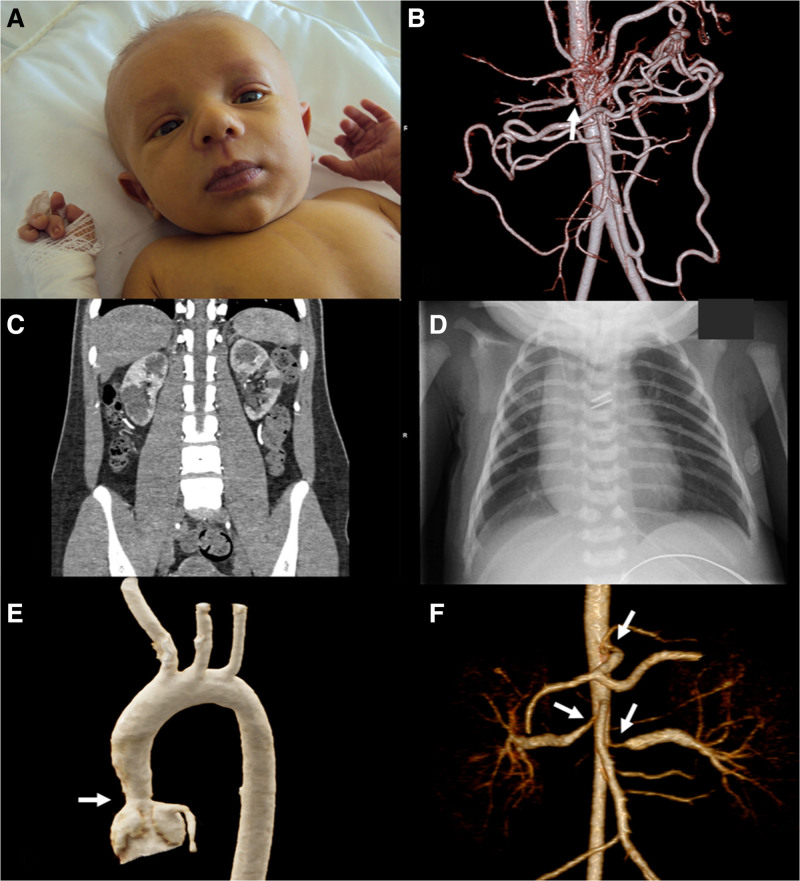
Several pediatric syndromes are associated with focal stenosis of renal arteries, leading to RVHT. The most frequent are NF1, the Williams-Beuren syndrome (WBS), and the Alagille syndrome (AS; Figure 4). The angiographic aspect of RAS in these different syndromes is indistinguishable from that observed in children/adolescents with focal FMD and, as the latter, often associated with aortic abdominal coarctation (midaortic syndrome).3,15
Figure 4.
Abnormalities in patients with Alagille and Williams syndrome. A, Infant with Alagille syndrome showing typical facial features: a broad, prominent forehead, deep-set eyes, and a small, pointed chin (courtesy of Dr Dorota Wicher, Department of Clinical Genetics, The Children’s Memorial Health Institute, Warsaw, Poland) B, Three-dimensional image of the abdominal arteries depicting extensive collateral circulation through the Riolan arcade and marginal artery of Drummond due to celiac trunk and superior mesenteric stenoses, as well as critical right renal artery stenosis (arrow) in a 16-y-old girl with Alagille syndrome (courtesy of Dr Jędrzej Sarnecki, Department of Diagnostic Imaging, The Children’s Memorial Health Institute, Warsaw, Poland). C, Coronal multiplanar reconstruction image showing bilateral multiple renal cystic lesions in the same patient (courtesy of Dr Jędrzej Sarnecki, Department of Diagnostic Imaging, The Children’s Memorial Health Institute, Warsaw, Poland). D, Th11 butterfly vertebra in a male neonate with Alagille syndrome (courtesy of Dr Jędrzej Sarnecki, Department of Diagnostic Imaging, The Children’s Memorial Health Institute, Warsaw, Poland). E, Three-dimensional image of the thoracic aorta depicting the supravalvular aortic stenosis (arrow) in a 3-y-old boy with Williams syndrome (courtesy of Dr Jędrzej Sarnecki, Department of Diagnostic Imaging, The Children’s Memorial Health Institute, Warsaw, Poland). F, Three-dimensional image of the abdominal arteries depicting bilateral renal arteries stenoses (arrows) and celiac trunk stenosis (arrow) in a 2-y-old boy with Williams syndrome (courtesy of Dr Jędrzej Sarnecki, Department of Diagnostic Imaging, The Children’s Memorial Health Institute, Warsaw, Poland).
Accordingly, the diagnostic strategy and therapeutic management are similar to those proposed in patients with pediatric focal FMD. These syndromes are defined by a wide constellation of cardiovascular, endocrine, and neurological manifestations, and lists of criteria cannot entirely replace clinical expertise. Patients with midaortic syndrome demonstrate a BP gradient between upper and lower extremities and weak femoral pulses.
Imaging may include renal duplex ultrasound, computed tomographic angiography (CTA), and magnetic resonance angiography, but formal exclusion of RAS can be made only by catheter-based angiography.15 While surgery is restricted to complex cases, the preferred revascularization option is renal artery PTA, which may be associated with aortic angioplasty/stenting in case of associated abdominal coarctation.15 In contrast with adult patients with FMD,3 children with focal stenosis, whether syndromic or not, are sometimes treated with renal artery stenting15 or even a cutting balloon,24 though such approaches are controversial and should be restricted to expert centers.
Williams-Beuren Syndrome
WBS is a genetic condition due to deletion of the WBS region of chromosome 7, which encompasses 26 to 28 genes, including ELN—the gene coding for elastin. Deletion of ELN is responsible for the cardiovascular manifestations of the disease and instrumental to make the diagnosis, typically by Fluorescence In Situ Hybridization.26 WBS is considered as an autosomal dominant disorder because one copy of the altered chromosome is sufficient to cause the disorder but most cases occur de novo.27 The prevalence of WBS is estimated to be 1 in 10 000 people.26
WBS should be suspected in children with so-called elfin face (broad forehead, upturned nose, and pointed chin), intellectual impairment, and sociable behavior. Hypercalcemia is highly suggestive but only found in a minority of patients.26 Hypercalcemia in WBS is thought to be due to an increase in both digestive and renal calcium absorption.28
While the most common cardiovascular abnormality is supravalvular aortic stenosis, narrowing of other arteries due to smooth muscle overgrowth leading to thickening of the media may be observed, either in isolation or in multiple vessels. RAS has been reported in 7% to 58% of patients, usually in combination with midaortic syndrome.29
Alagille Syndrome
AS is an autosomal dominant syndrome due to mutations in the genes JAG1(>90% of cases) or NOTCH2, both part of the Notch pathway. De novo mutations may occur in 50% to 70% of cases.30
The main clinical features of AS are chronic cholestasis due to paucity of intrahepatic bile ducts, congenital heart disease (pulmonary stenosis or less often tetralogy of Fallot), butterfly vertebrae, characteristic face (broad forehead, deep-set eyes, and pointed chin), posterior embryotoxon or anterior segment abnormalities of the eyes, and pigmentary retinopathy. Additional features may include intracranial bleeding and dysplastic/cystic kidneys.31
The incidence of AS in the general population has been recently reevaluated to about 1 in 30 000 live births.32 In a large retrospective chart review including 268 children with AS,33 9% had noncardiac vascular anomalies. While the most commonly reported were aortic, cerebral, or basilar artery aneurysms, a single patient had documented RAS. In a subsequent report from the same authors,34 only 2 of 187 AS patients evaluable for renal abnormalities (2.7%) had RAS. As for WBS and other pediatric forms of focal stenosis, AS-related RAS is often associated with aortic coarctation. It may be progressive, with increases in BP, decreases in glomerular filtration rate, and kidney atrophy.30 Renal artery occlusion and RAAs have also been reported.30 Patients who survive to adulthood have mostly mild liver abnormalities and may develop multiple artery stenoses over time.
The diagnosis of AS deserves to be considered in adult patients with RAS and at least one of the classical features, even without liver disease,35 and in the absence of genetic confirmation, the differential diagnosis with FMD/midaortic syndrome may be challenging.36
Grange Syndrome
Grange syndrome is a rare autosomal recessive syndrome first described in 1998 and characterized by progressive arterial narrowing broadly similar to focal FMD in angiographic appearance and distribution, congenital cardiac defects (patent ductus arteriosus, bicuspid aortic valve, and ventricular septal defect), brachydactyly, syndactyly, bone fragility with multiple fractures, and learning disabilities.22
The vascular spectrum of the disease includes RAS with hypertension. While only a limited number of cases have been identified since the initial report,22 this unique entity has recently come to the forefront, since the group of Dianna Milewicz37 has identified mutations in YY1AP1 at the origin of the disease. The latter gene codes for the YY1 (yin yang 1)-associated protein 1—an activator of the YY1 transcription factor and a component of the INO80 chromatin remodeling complex, which is responsible for transcriptional regulation, DNA repair, and replication.37
Other Rare Entities Seldom Associated With RAS
Finally, RAS or aneurysms have also been occasionally reported in patients with Marfan syndrome,38 tuberous sclerosis,39 Turner syndrome,40 Pseudoxanthoma elasticum,41 and VACTERL syndrome.42
Renal Artery Complications Following Aortic Dissection
Population-based studies estimate the annual incidence of aortic dissection (AD) at between 2.9 and 3.5 per 100 000. Twenty-five percent to 30% of patients with acute AD demonstrate peripheral vascular ischemia. The renal circulation is the second most commonly malperfused arterial bed in AD, following iliofemoral arteries (11%).43
Angiographic findings of the largest reported cohort with renal malperfusion accompanying AD demonstrated that right and left renal arteries arose exclusively from the true, false, and both lumens in 70% versus 42%, 7% versus 20%, and 23 versus 38%, respectively.43–45
The pressure difference between the false lumen and true lumen may allow the mobile intima-media flap to bulge into the ostia of renal arteries, leading to either transient (dynamic) or persistent (static) obliteration of renal artery ostia.44,45 Dynamic obstruction, which is intermittent in nature, more commonly causes renal malperfusion syndrome and is responsible for ≈80% of cases.
There are 2 distinct mechanisms of dynamic renal malperfusion.43–45
In the first one, the false lumen pressure increases rapidly as a result of poor outflow, which in turn results in a true lumen compression. Insufficient flow through the true lumen may lead to kidney hypoperfusion when renal artery perfusion is maintained by the true lumen.43–46 This process occurs most commonly in the setting of a deep proximal tear with the absence of a large distal fenestration. Hypertension may result from diminished kidney perfusion with subsequent local renal ischemia and secondary activation of the renin-angiotensin system.
The second mechanism of dynamic obstruction reflects the mobility of the intimal flap—when the false lumen prolapses into the renal artery ostium, flow is dynamically compromised. Static obstruction, characterized by narrowing or occlusion of branch vessels, is the consequence of false lumen protrusion into the branch vessel with subsequent thrombosis.43–46 In some patients with AD and kidney malperfusion, the renal artery may be occluded by means of a dissecting hematoma propagating along the renal artery trunk and associated with a renal infarction.43–46
Of note, this mechanism is reversible and the initial ischemic episode caused by the hematoma and subsequent dissection of the vessel is followed by circumferential reentry of the dissection into renal artery trunk. This phenomenon leads to the relief of obstruction, reperfusion, and finally recovery of renal flow and improvement of renal function. Under such circumstances, renal artery inflow is supported both by true and false lumen.43,47
The most frequent presentation of acute AD is sudden-onset severe chest or back pain that migrates from chest to lower back. Not infrequently, initial neurological signs coexist with pain, ranging from transient or permanent central nervous symptoms, including syncope, to various spinal signs such as paraparesis or paraplegia.43,47
Clinical suspicion of renal artery malperfusion in patients with AD is based on worsening hypertension or evolving renal insufficiency manifested by oliguria, anuria, or a rise in serum urea and creatinine.43,44 CTA is currently the most widely used noninvasive diagnostic modality for AD and is also able to demonstrate renal hypoperfusion or infarction, where present, in most cases of AD with or without renal artery dissection.43–45 Evidence of kidney malperfusion may include radiographic evidence of compression of the true lumen, presence of renal parenchymal infarction, visualization of an occlusive intimal flap, or asymmetrical kidney enhancement.
Despite significant progress in diagnosis of renal malperfusion, the positive predictive value of CTA for malperfusion remains imperfect and approaches only 70%. A study of the diagnostic accuracy of CTA and MRI showed that pooled sensitivities (98%–100%) and specificities (95%–98%) were comparable to confirm or rule out AD.43,44 Renal duplex ultrasonography has also an added value. Increased proximal renal artery peak systolic and diastolic velocity in combination with a reduced intrarenal resistance index have been shown to suggest renal malperfusion. Additionally, a normal distal renal artery waveform has been shown to carry a negative predictive value of 100% for malperfusion.44,46,47
The management of patients with renal artery dissection secondary to AD should be individualized. Techniques to alleviate renal malperfusion, especially if a proximal thoracic endovascular aortic repair does not resolve renal ischemia, include central aortic fenestration, branch artery stenting, or combination of both.48–50
Persistent hypertension, older age, smoking, aortic size, and the presence of a patent false lumen are all predictors of late complications. The 10-year survival of patients with acute dissection ranges from 30% to 60%. Of note, AD predisposes the entire aorta and its branches to dissection, aneurysm formation, and rupture.47
Isolated Renal Artery Dissection
Isolated renal artery dissection (IRAD) that does not occur as a consequence of AD is uncommon. The exact prevalence of IRAD is unknown and probably underestimated. Importantly, in specific contexts such as renal infarction, it may reach 40%.51
Hypertension due to IRAD may result from functional RAS, distal parenchymal embolization of a mural thrombus, or from hemodynamic changes/turbulence in the dissected vessel, all leading to decreased renal perfusion and activation of the renin-angiotensin system. Conversely, hypertension may be a causative factor.
IRAD is most commonly associated with atherosclerosis and FMD.52 IRAD may also be iatrogenic, resulting from interventional procedures such as percutaneous balloon angioplasty and stenting53 or radiofrequency renal nerve ablation.54
Less common disease associations include vascular Ehlers-Danlos syndrome, Marfan syndrome, malignant hypertension, blunt trauma, and strenuous physical activity.
A recent study including 61 patients with unexplained renal artery dissection has shown the added value of brain-to-pelvis arterial scanning to define etiology and prognosis. Indeed, by contrast with patients with renal artery dissection in the context of FMD or harboring aneurysm(s) or dissection(s) of other arterial beds, patients with confirmed IRAD (39% of the whole series) appear to be at low risk of recurrent dissection, either in renal or other arterial beds.55 Based on these findings, in the absence of known underlying vascular disease, whole body arterial scanning deserves to be considered in all patients with apparent IRAD.56
IRAD typically presents with acute flank or abdominal pain but may be silent and discovered incidentally. IRAD can also present as a rapid onset of severe hypertension. Finally, renal dysfunction progressing to renal failure may be a manifestation of IRAD when renal perfusion of the affected kidney is compromised.
Duplex ultrasound is a noninvasive method allowing measurement of flow in the renal arteries, measurement of reduced intrarenal resistance index, and increased acceleration time and renal perfusion. However, it may not be sensitive enough when the dissection affects distal renal arteries.52
Unless contraindicated due to low glomerular filtration, CTA should be performed. Images often show a linear filling defect in the lumen or a uniform narrowing. CTA also allows detection of renal infarction.
No prospective randomized controlled trials have compared medical therapy to intervention. Medical therapy is an appropriate strategy when estimated glomerular filtration rate is stable and when symptoms and hypertension can be controlled medically.57,58 Options are either antiplatelet or anticoagulation treatment.59
In the largest case-series reported in patients with IRAD and uncontrolled hypertension, Pellerin et al have shown that renal artery PTA and stenting was safe and effective in 16 consecutive patients. After a mean follow-up of 8.6±3.4 years, mean BP was within normal limits on ≤2 hypertensive agents, plasma creatinine levels were also normal, and all stents were patent on imaging.60
The results of surgical treatment have been reported in a case-series of 22 patients with IRAD and uncontrolled hypertension. Surgical treatment consisted of arterial repair (17) or nephrectomy (8). Hypertension was cured in 9 patients (41%), BP was improved in 11 (50%), and unchanged in 2 (9%).61 An observational study of 23 patients with symptomatic IRAD aimed to manage all patients conservatively. Over a mean of 20 months, 8 patients required endovascular interventions, and there were 4 dissection-related deaths.62 This study indicates that patients with IRAD are a high-risk group, whether treated medically or with intervention, and that close follow-up is warranted.
Renal Arteritis–Takayasu Arteritis
RAS can also be secondary to an arteritis, defined as inflammation of the renal artery. The most common arteritis involving the renal arteries is Takayasu arteritis, which is a chronic, progressive, granulomatous, large-vessel panarteritis with preferential involvement of the aorta and its major branches. Takayasu arteritis affects women in 80% to 90% of cases, with a mean age at diagnosis between 25 and 30 years, and is more frequent in Asia and South Africa.63
Diagnosis is based on criteria established by the American College of Rheumatology in 1990. At least 3 of the following 6 criteria have to be present for differentiating Takayasu arteritis from other systemic vasculitis, including age at diagnosis (onset, ≤40 years), claudication of the extremities, decreased brachial artery pulse, BP difference >10 mm Hg between limbs, a bruit over the subclavian arteries, or angiographic abnormalities on imaging.64 Hypertension is found in more than half of cases. Imaging abnormalities include arteriographic narrowing or occlusion of the entire aorta, its primary branches or large arteries in the proximal upper or lower extremities, not due to arteriosclerosis, FMD, or similar causes. Changes are usually focal or segmental.65
Laboratory abnormalities usually reflect the inflammatory process. However, after the initial phase, systemic inflammation does not always show a positive correlation with inflammatory activity in the vessel wall.
The pathogenesis of Takayasu arteritis remains unknown, although some hypotheses have been suggested, including genetic involvement (HLA-B*52 gene association), infectious (association with tuberculosis), and autoimmune causes. The underlying pathophysiology of renovascular hypertension in patients with Takayasu arteritis is RAS. Dysfunction of baroreceptors of the aortic sinus and the carotid arteries may also play a role.65
Imaging of the arterial tree should be performed by CTA, magnetic resonance angiography, or color Doppler ultrasound. Imaging shows vessel wall thickening and luminal narrowing. 18-fluorodeoxyglucose positron emission tomography with computed tomography is highly sensitive in determining the extent and severity of inflammation in the arterial wall and can, therefore, differentiate Takayasu arteritis from FMD.63
First-line management includes pharmacological treatment with antihypertensive drugs, glucocorticoids, conventional immunosuppressive agents, and biologic agents including tumor necrosis factor inhibitors.66 Revascularization, either by endovascular or open surgical strategies, should be delayed until inflammation has resolved, as complications are more likely to occur when inflammation is active.67 Endovascular treatment of RAS is the intervention of first choice. Surgical revascularization of the renal arteries is reserved for patients with other aortic pathologies or those in whom the endovascular approach failed.65
Other vasculitides such as Cogan syndrome, Behçet disease, polyarteritis nodosa, Kawasaki disease, and giant cell arteritis may involve the renal arteries as well.15,68,69 Therefore, clinical evaluation should be thorough and include the search for interstitial keratitis and vestibule-auditory dysfunction, recurrent oral aphthae and erythematous nodules, and 18-fluorodeoxyglucose positron emission tomography for the detection of inflammatory aortitis.
Segmental Arterial Mediolysis
SAM is an uncommon nonatherosclerotic, noninflammatory arteriopathy. Its incidence in the United States is estimated to be as high as 1/100 000 cases per year.70
The three largest series (>300 patients) report a male preponderance.71–73 Patients usually present for the first time in their 50’s, most commonly with abdominal pain. Those vessels most commonly affected include mesenteric, renal, and iliac arteries, with multiple vessel involvement in the majority of cases.71–73 Carotid, cerebral, and coronary artery involvement has also been described.74 Renovascular hypertension is a rare presentation of SAM. One large series of 117 patients reports acute hypertension as a presenting feature in 13.7% (16 patients) and renal artery involvement in 49.6%.73 Other relevant publications are single case reports.75–77
SAM itself has 2 distinct pathological phases—the injurious and the reparative phases. Features of the injurious phase include mediolysis, resulting in dilation and aneurysms, and a tear that separates the media from the adventitia, bleeding into which results in dissections. Features of the reparative phase include repair by fibrosis, resulting in stenoses similar to those found in FMD, and thrombosis, which leads to arterial occlusions.78 In the largest series of hypertensive cases published, the specific underlying arterial lesion was not documented. The commonest radiological findings in this cohort were dissection, focal stenosis, beading, and occlusion,73 all of which can cause hypertension if renal arteries are involved. Additional case reports of SAM document hypertension due to renal arterial dissection.75–77 The underlying cause of SAM is unknown, and no predisposing factors have been identified.
The principal imaging hallmark of SAM is the dissecting aneurysm. A peripheral isolated arterial dissection is also suggestive.74 Otherwise, the diagnosis of SAM should be considered in those patients who present with aneurysms, a string-of-beads appearance, arterial stenosis, or occlusion, without an alternative diagnosis of a connective tissue disorder, vasculitis, or FMD and with negative inflammatory markers.79 It is impossible radiographically to distinguish the string of beads of SAM from that of FMD. The diagnosis of FMD requires the presence of a stenosis; in those patients who present with nonstenotic arterial lesions, particularly dissecting aneurysms, SAM should be considered. Even histologically, if in the reparative phase, SAM and FMD can be indistinguishable.78
Management ranges from conservative to endovascular (coil embolization, angioplasty, or stenting) or open surgery (organ resection±arterial repair).70 Of the 16 patients in the large series who presented with acute hypertension, four were treated with intervention, but the type of intervention and the outcomes were not described.73 In the three individual case reports, 2 patients were treated with renal artery angioplasty and 1 was managed conservatively.75–77 Both patients who received intervention were complicated; one had hypertensive encephalopathy, and the second failed medical treatment.77 The patient managed medically alone had a good response to medical therapy and did not require further intervention.76
Patients with SAM are generally followed up with angiography; up to 30% progress on imaging, after an average follow-up of 3 years.73 Both patients described in the case reports who had renal artery intervention had completion angiograms that showed no significant residual stenosis. Their BP improved, but they were kept on antihypertensive medication (β-blockers and calcium channel blockers) as prophylaxis against future aneurysm rupture.75,77 The patient who received medical management only was weaned off antihypertensives at 6 months and CTA confirmed almost complete regression of the dissections.76
Idiopathic Aneurysm
Each main renal artery has an internal diameter of 6.2 to 6.6 mm.80 A RAA is defined as a focal dilated segment of all 3 layers of the renal arterial wall that exceeds 1.5× the diameter of the disease-free proximal adjacent arterial segment.81 RAAs are uncommon, occurring in ≈0.09% of the general population.82
Approximately 70% of patients with RAA have hypertension.83 Hypotheses for the mechanism include
Distal parenchymal embolization from dislodged mural thrombus,86
Compression or kinking of associated renal artery branches,
Hemodynamic changes from turbulent blood flow within the aneurysm resulting in decreased distal renal artery perfusion,83 which can induce renin-dependent hypertension.87
Idiopathic RAAs are more likely to present in the sixth decade of life.88–91 Women, including multiparous women, are more commonly afflicted with RAA92 and have multivessel involvement. The majority of these patients lack traditional cardiovascular risk factors other than hypertension.
FMD is primarily a stenotic disease. It is, however, increasingly recognized that aneurysms form part of the disease spectrum and occur with higher frequency than thought previously3 but on their own are insufficient for a diagnosis of FMD. It is possible that many cases of idiopathic RAA may in fact be due to FMD. Other causes of RAA include atherosclerotic degeneration, vasculitides (eg, Behçet disease, Takayasu, giant cell arteritis), phakomatoses (eg, tuberous sclerosis, neurofibromatosis), hereditary arteriopathies (eg, Loeys-Dietz syndrome),90 intrinsic collagen deficiency (eg, vascular Ehlers-Danlos91 or Marfan syndromes), and SAM.
Many RAAs are detected incidentally in asymptomatic individuals88 and can be associated with other visceral artery aneurysms (of the splenic or hepatic arteries). Symptoms beyond hypertension are rare (4%–23%) and include abdominal or flank pain, as well as hematuria.93 Chronic kidney disease has been identified in 4% to 14% of patients with aneurysms.84,94 Two-thirds of RAA affect the right renal artery88 possibly due to the longer vessel length, with the average reported RAA size being 1.3 to 3.8 cm, and operative series reporting larger diameters.88,89 Two-thirds originate in the main renal artery bifurcation; the majority (85%) are saccular, and 18% to 68% calcified.88 Ten percent to 20% of RAAs are bilateral.82 Eight percent to 11% demonstrate thromboembolism.
Medical management hinges on tight BP control and smoking cessation. Certain types of small (<2 cm) aneurysms may not be treated but undergo surveillance for growth or development of other complications. Currently accepted indications for intervention include size >2 cm, any size above 1 cm in pregnancy (rupture during pregnancy has been described in aneurysms as small as 0.5 cm),92,95 pain, hematuria, refractory hypertension, thromboembolism, dissection, and rupture.82,83,88 Syndromes such as the Loeys-Dietz syndrome96 are associated with an increased risk of aneurysm rupture. The presence of calcification is not associated with a lower risk of rupture. Treatment may be endovascular (eg, coiling, covered stents) or surgical (resection or bypass), depending on aneurysm location.
A large, contemporary, multi-institutional study of 865 RAAs of all causes in 760 patients demonstrated that asymptomatic RAAs rarely rupture (even when >2 cm).88 Aneurysm repair can cure hypertension in 32% and improve hypertension in 26% of patients with difficult-to-control hypertension.88,89
The natural history of RAA is likely more benign than historic reports have suggested, with a low risk of rupture, slow to null rate of growth, and improved survival following rupture. While short-term follow-up at 1 year remains prudent for a newly diagnosed RAA, subsequently longer intervals between surveillance imaging may be appropriate. The exception is pregnancy given the increased risk of rupture, and should it happen, the poor prognosis for both mother and fetus. The potential for gestational rupture, therefore, remains a valid indication for repair in women of child-bearing age.92
Renal Arteriovenous Fistula
Renal arteriovenous fistula (rAVF) is defined as a single direct communication between a renal artery and an adjacent vein. Since most of rAVFs are asymptomatic and remain undetected, their real incidence is unknown but should be low.97,98
Hypertension is found in about 40% of patients with rAVF and may be caused by local renal ischemia resulting from a short circuit of blood with secondary activation of the renin-angiotensin system.97,99 It has been reported that rAVF may be a cause of severe hypertension in pregnancy, and successful embolization has been followed by subsequent decrease in BP.100 It should also be taken into consideration that a subset of patients with rAVF may have in fact coexisting essential hypertension.
rAVFs comprise about 70% to 80% of renal arteriovenous abnormalities and can be divided into congenital and acquired types.97 Congenital rAVFs are high-flow shunts, and the compromised vessels are enlarged, sometimes with associated venous aneurysms. Acquired rAVFs are more common than congenital rAVFs and usually result from percutaneous renal biopsy, penetrating trauma, surgery, malignancy, or inflammation. It has been reported that arteriovenous fistulas may be associated with renal FMD.42,97,101,102
The largest study based on routine Doppler ultrasound evaluation has shown that rAVF is a frequent vascular complication after percutaneous renal biopsy, with an estimated incidence of 14.4%. Most rAVFs (95%) were asymptomatic, and 47% closed spontaneously in <30 days.103
The clinical manifestations of rAVFs vary widely, from an asymptomatic presentation, flank pain, or hematuria to hypertension.97,104 In patients with rAVF, increased cardiac output and hypertension may lead to the development of cardiac failure in about 40% of subjects, with severity of symptoms and hemodynamic changes depending on blood flow through the fistula.97 On physical examination, the most frequent clinical signs of rAVF are widened pulse pressure, brisk arterial pulsation, mild tachycardia, and a bruit over the region where the fistula is localized.99 Duplex Doppler sonography is the preferred initial diagnostic method, and available studies indicate its effectiveness in diagnosing and following patients with rAVFs. This method is also suitable for detection of rAVF following kidney allograft biopsy.97 Ultrasonography of arteriovenous fistulas shows increased flow velocity, decreased arterial resistance, and arterial waveforms in the outflow vein. The resistive index of the feeding artery may be dramatically decreased—to between 0.30 and 0.40.105 Spiral CTA and magnetic resonance angiography may be useful in detecting rAVF, although the definite diagnosis of arteriovenous malformations must be confirmed by arteriography, which remains the gold standard.97 With CTA or magnetic resonance angiography, rAVFs are characterized by a single dilated feeding artery and early enhancement of a dilated draining vein. The renal parenchyma overlying the fistula may become atrophic secondary to ischemia.105
In symptomatic patients with volume overload and heart failure, closure of rAVF is indicated with good chance of a definitive cure. Endovascular therapy with embolization is considered the effective and safe procedure of choice in the treatment of rAVF. It allows permanent closure of the nidus and feeding vessels with preservation of unaffected renal parenchyma.97 Surgery is reserved for those patients who are not candidates for embolization of shunt vessels, primarily because of anatomic reasons, including magnitude and multiplicity of the shunt vessels. The goals of surgical treatment are excision of the fistula, ligation of the feeding vessels, or partial or total nephrectomy.106 The interventional or surgical treatment of rAVF should preserve function of the renal parenchyma, resolve symptoms, and restore normal intrarenal hemodynamics with subsequent normalization or improvement of BP control. Long-term follow-up is recommended for all patients.
Renal Artery Thrombosis
Isolated renal artery thrombosis is extremely rare, and only a few cases have been reported to date.107 The mechanism of hypertension in patients with renal artery thrombosis is multifactorial. Pain secondary to ischemia from infarction or an associated arterial dissection can increase BP acutely. Ischemia itself induces a reflex activation of both the renin-angiotensin and the sympathetic nervous systems.108 Renal artery thrombosis secondary to other causes is much more common than isolated renal artery thrombosis and may have a prevalence of ≈2/100 000.109 Underlying arterial causes include atherosclerosis, dissecting hematoma, FMD, dissection, aneurysm,51 and trauma (including instrumentation and renal transplantation).110 Thrombophilic causes include cancer, vasculitis, sickle cell anemia, nephrotic syndrome,111 antiphospholipid antibody syndrome,112 sepsis, and coronavirus disease 2019 (COVID-19).113 Embolic causes include atrial fibrillation and valvular or aortic wall disease.51
The clinical presentation of patients with renal artery thrombosis is nonspecific and may be insidious, which may lead to a delayed diagnosis. Flank or abdominal pain is usually present and can be associated with nausea, vomiting, fever, and hypertension. Microscopic hematuria is often reported, macroscopic hematuria is rare, and proteinuria may be present in patients with chronic complete renal artery occlusion.114 Laboratory abnormalities are also nonspecific and include an increase in leukocyte count, lactate dehydrogenase, C-reactive protein, serum creatinine, and a fall in estimated glomerular filtration rate.
Color Doppler ultrasonography has a lower sensitivity than other modalities but is noninvasive and can be valuable in the follow-up after treatment of renal artery thrombosis.115,116 A decreased peak systolic velocity, with tardus parvus arterial wave forms may be observed.116 When the renal artery is completely occluded, the absence of intrarenal blood flow can be documented.117 Renal isotope scans and CTAs have a good diagnostic sensitivity.115 The gold standard radiological exam is renal artery angiography.
Treatment should be decided on a case-by-case basis.118 Options include anticoagulation or catheter-directed thrombolysis. Once thrombolysis is complete, if an underlying arterial lesion is uncovered, it may be managed by angioplasty or stenting.119 Trauma may necessitate open surgical thrombectomy and artery repair.120
Successful outcomes have been described after both anticoagulation and intervention.118 A series of 10 patients who presented with acute renal artery thromboembolism underwent catheter-directed thrombolysis. Five also had angioplasty of underlying renal artery lesions. Immediate angiographic success was achieved in 7 patients. After 3 days, one of these patients had a recurrence of thrombosis but underwent a second successful catheter-directed thrombolysis.121
Conclusions
The different rare stenotic and nonstenotic causes of RVHT discussed in this article represent an important though heterogeneous group of entities to be considered. The clinical manifestations of these renal artery lesions vary widely, from an asymptomatic presentation to the development of refractory hypertension. Because of the controversies surrounding their nature and classification, they may present a diagnostic dilemma. However, understanding of the natural history, vascular anatomy, and hemodynamics of these lesions helps to determine the best therapeutic option, avoiding potentially catastrophic vascular complications. Nowadays, surgical treatment of these lesions has been largely replaced by endovascular procedures, which allows management of these potentially curable forms of RVHT with preservation of uninvolved renal parenchyma.
Sources of Funding
None.
Disclosures
None.
Nonstandard Abbreviations and Acronyms
- AD
- aortic dissection
- AS
- Alagille syndrome
- BP
- blood pressure
- CTA
- computed tomographic angiography
- FMD
- fibromuscular dysplasia
- IRAD
- isolated renal artery dissection
- NF1
- neurofibromatosis type 1
- PTA
- percutaneous transluminal angioplasty
- RAA
- renal artery aneurysm
- RAS
- renal artery stenosis
- rAVF
- renal arteriovenous fistula
- RVHT
- renovascular hypertension
- SAM
- segmental arterial mediolysis
- WBS
- Williams-Beuren syndrome
- YY1
- yin yang 1
For Sources of Funding and Disclosures, see page 908.
A. Persu, C. Canning, M. Januszewicz, and A. Januszewicz contributed equally.
Contributor Information
Alexandre Persu, Email: alexandre.persu@uclouvain.be.
Caitriona Canning, Email: cnichainin@gmail.com.
Aleksander Prejbisz, Email: aprejbisz@ikard.pl.
Laurence Amar, Email: laurence.amar@aphp.fr.
Constantina Chrysochou, Email: tina.chrysochou@srft.nhs.uk.
Jacek Kądziela, Email: jkadziela@onet.pl.
Mieczysław Litwin, Email: m.litwin@ipczd.pl.
Daan van Twist, Email: d.vantwist@zuyderland.nl.
Patricia Van der Niepen, Email: patricia.vanderniepen@uzbrussel.be.
Gregoire Wuerzner, Email: gregoire.wuerzner@chuv.ch.
Peter de Leeuw, Email: p.deleeuw@maastrichtuniversity.nl.
Michel Azizi, Email: michel.azizi@aphp.fr.
Magda Januszewicz, Email: ajanuszewicz@ikard.pl.
Andrzej Januszewicz, Email: ajanuszewicz@ikard.pl.
References
- 1.Herrmann SM, Textor SC. Current concepts in the treatment of renovascular hypertension. Am J Hypertens. 2018;31:139–149. doi: 10.1093/ajh/hpx154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prince M, Tafur JD, White CJ. When and how should we revascularize patients with atherosclerotic renal artery stenosis? JACC Cardiovasc Interv. 2019;12:505–517. doi: 10.1016/j.jcin.2018.10.023 [DOI] [PubMed] [Google Scholar]
- 3.Gornik HL, Persu A, Adlam D, Aparicio LS, Azizi M, Boulanger M, Bruno RM, de Leeuw P, Fendrikova-Mahlay N, Froehlich J, et al. First International Consensus on the diagnosis and management of fibromuscular dysplasia. Vasc Med. 2019;24:164–189. doi: 10.1177/1358863X18821816 [DOI] [PubMed] [Google Scholar]
- 4.Pappaccogli M, Di Monaco S, Warchoł-Celińska E, Lorthioir A, Amar L, Aparicio LS, Beauloye C, Bruno RM, Chenu P, de Leeuw P, et al. ; European/International FMD Registry and Initiative (FEIRI), and the Working Group ‘Hypertension and the Kidney’ of the European Society of Hypertension (ESH). The European/International Fibromuscular Dysplasia Registry and Initiative (FEIRI)-clinical phenotypes and their predictors based on a cohort of 1000 patients. Cardiovasc Res. 2021;117:950–959. doi: 10.1093/cvr/cvaa102 [DOI] [PubMed] [Google Scholar]
- 5.Plouin PF, Perdu J, La Batide-Alanore A, Boutouyrie P, Gimenez-Roqueplo AP, Jeunemaitre X. Fibromuscular dysplasia. Orphanet J Rare Dis. 2007;2:28. doi: 10.1186/1750-1172-2-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaplan NM, Victor RG. Kaplan’s Clinical Hypertension. 2015. Wolters Kluwer [Google Scholar]
- 7.Bergqvist C, Servy A, Valeyrie-Allanore L, Ferkal S, Combemale P, Wolkenstein P; NF France Network. Neurofibromatosis 1 French national guidelines based on an extensive literature review since 1966. Orphanet J Rare Dis. 2020;15:37. doi: 10.1186/s13023-020-1310-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubov T, Toledano-Alhadef H, Chernin G, Constantini S, Cleper R, Ben-Shachar S. High prevalence of elevated blood pressure among children with neurofibromatosis type 1. Pediatr Nephrol. 2016;31:131–136. doi: 10.1007/s00467-015-3191-6 [DOI] [PubMed] [Google Scholar]
- 9.Fossali E, Signorini E, Intermite RC, Casalini E, Lovaria A, Maninetti MM, Rossi LN. Renovascular disease and hypertension in children with neurofibromatosis. Pediatr Nephrol. 2000;14:806–810. doi: 10.1007/s004679900260 [DOI] [PubMed] [Google Scholar]
- 10.Zinnamosca L, Petramala L, Cotesta D, Marinelli C, Schina M, Cianci R, Giustini S, Sciomer S, Anastasi E, Calvieri S, et al. Neurofibromatosis type 1 (NF1) and pheochromocytoma: prevalence, clinical and cardiovascular aspects. Arch Dermatol Res. 2011;303:317–325. doi: 10.1007/s00403-010-1090-z [DOI] [PubMed] [Google Scholar]
- 11.Beladan CC, Geavlete OD, Botezatu S, Postu M, Popescu BA, Ginghina C, Coman IM. Revascularization in a 17-Year-old girl with neurofibromatosis and severe hypertension caused by renal artery stenosis. Tex Heart Inst J. 2017;44:50–54. doi: 10.14503/THIJ-15-5466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kurien A, John PR, Milford DV. Hypertension secondary to progressive vascular neurofibromatosis. Arch Dis Child. 1997;76:454–455. doi: 10.1136/adc.76.5.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han M, Criado E. Renal artery stenosis and aneurysms associated with neurofibromatosis. J Vasc Surg. 2005;41:539–543. doi: 10.1016/j.jvs.2004.12.021 [DOI] [PubMed] [Google Scholar]
- 14.Friedman JM, Arbiser J, Epstein JA, Gutmann DH, Huot SJ, Lin AE, McManus B, Korf BR. Cardiovascular disease in neurofibromatosis 1: report of the NF1 Cardiovascular Task Force. Genet Med. 2002;4:105–111. doi: 10.1097/00125817-200205000-00002 [DOI] [PubMed] [Google Scholar]
- 15.Tullus K, Brennan E, Hamilton G, Lord R, McLaren CA, Marks SD, Roebuck DJ. Renovascular hypertension in children. Lancet. 2008;371:1453–1463. doi: 10.1016/S0140-6736(08)60626-1 [DOI] [PubMed] [Google Scholar]
- 16.Oderich GS, Sullivan TM, Bower TC, Gloviczki P, Miller DV, Babovic-Vuksanovic D, Macedo TA, Stanson A. Vascular abnormalities in patients with neurofibromatosis syndrome type I: clinical spectrum, management, and results. J Vasc Surg. 2007;46:475–484. doi: 10.1016/j.jvs.2007.03.055 [DOI] [PubMed] [Google Scholar]
- 17.Raborn J, McCafferty BJ, Gunn AJ, Moawad S, Mahmoud K, Aal AKA, Saddekni S. Endovascular management of neurofibromatosis type I-associated vasculopathy: a case series and brief review of the literature. Vasc Endovascular Surg. 2020;54:182–190. doi: 10.1177/1538574419885257 [DOI] [PubMed] [Google Scholar]
- 18.Baser ME, Friedman JM, Aeschliman D, Joe H, Wallace AJ, Ramsden RT, Evans DG. Predictors of the risk of mortality in neurofibromatosis 2. Am J Hum Genet. 2002;71:715–723. doi: 10.1086/342716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruggieri M, D’Arrigo G, Abbate M, Distefano A, Upadhyaya M. Multiple coronary artery aneurysms in a child with neurofibromatosis type 1. Eur J Pediatr. 2000;159:477–480. doi: 10.1007/s004310051313 [DOI] [PubMed] [Google Scholar]
- 20.Srinivasan A, Krishnamurthy G, Fontalvo-Herazo L, Nijs E, Meyers K, Kaplan B, Cahill AM. Spectrum of renal findings in pediatric fibromuscular dysplasia and neurofibromatosis type 1. Pediatr Radiol. 2011;41:308–316. doi: 10.1007/s00247-010-1854-9 [DOI] [PubMed] [Google Scholar]
- 21.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, et al. ; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904. doi: 10.1542/peds.2017-1904 [DOI] [PubMed] [Google Scholar]
- 22.Grange DK, Balfour IC, Chen SC, Wood EG. Familial syndrome of progressive arterial occlusive disease consistent with fibromuscular dysplasia, hypertension, congenital cardiac defects, bone fragility, brachysyndactyly, and learning disabilities. Am J Med Genet. 1998;75:469–480. doi: 10.1002/(sici)1096-8628(19980217)75:5<469::aid-ajmg4>3.0.co;2-i [DOI] [PubMed] [Google Scholar]
- 23.Rasmussen SA, Yang Q, Friedman JM. Mortality in neurofibromatosis 1: an analysis using U.S. death certificates. Am J Hum Genet. 2001;68:1110–1118. doi: 10.1086/320121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Srinivasan A, Krishnamurthy G, Fontalvo-Herazo L, Nijs E, Keller MS, Meyers K, Kaplan B, Cahill AM. Angioplasty for renal artery stenosis in pediatric patients: an 11-year retrospective experience. J Vasc Interv Radiol. 2010;21:1672–1680. doi: 10.1016/j.jvir.2010.07.012 [DOI] [PubMed] [Google Scholar]
- 25.Booth C, Preston R, Clark G, Reidy J. Management of renal vascular disease in neurofibromatosis type 1 and the role of percutaneous transluminal angioplasty. Nephrol Dial Transplant. 2002;17:1235–1240. doi: 10.1093/ndt/17.7.1235 [DOI] [PubMed] [Google Scholar]
- 26.Pober BR. Williams-Beuren syndrome. N Engl J Med. 2010;362:239–252. doi: 10.1056/NEJMra0903074 [DOI] [PubMed] [Google Scholar]
- 27.Sadler LS, Robinson LK, Verdaasdonk KR, Gingell R. The Williams syndrome: evidence for possible autosomal dominant inheritance. Am J Med Genet. 1993;47:468–470. doi: 10.1002/ajmg.1320470406 [DOI] [PubMed] [Google Scholar]
- 28.Letavernier E, Rodenas A, Guerrot D, Haymann JP. Williams-Beuren syndrome hypercalcemia: is TRPC3 a novel mediator in calcium homeostasis? Pediatrics. 2012;129:e1626–e1630. doi: 10.1542/peds.2011-2507 [DOI] [PubMed] [Google Scholar]
- 29.Collins RT., 2nd.Cardiovascular disease in Williams syndrome. Circulation. 2013;127:2125–2134. doi: 10.1161/CIRCULATIONAHA.112.000064 [DOI] [PubMed] [Google Scholar]
- 30.Salem JE, Bruguiere E, Iserin L, Guiochon-Mantel A, Plouin PF. Hypertension and aortorenal disease in Alagille syndrome. J Hypertens. 2012;30:1300–1306. doi: 10.1097/HJH.0b013e3283531e1f [DOI] [PubMed] [Google Scholar]
- 31.Turnpenny PD, Ellard S. Alagille syndrome: pathogenesis, diagnosis and management. Eur J Hum Genet. 2012;20:251–257. doi: 10.1038/ejhg.2011.181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kamath BM, Spinner NB, Rosenblum ND. Renal involvement and the role of Notch signalling in Alagille syndrome. Nat Rev Nephrol. 2013;9:409–418. doi: 10.1038/nrneph.2013.102 [DOI] [PubMed] [Google Scholar]
- 33.Kamath BM, Spinner NB, Emerick KM, Chudley AE, Booth C, Piccoli DA, Krantz ID. Vascular anomalies in Alagille syndrome: a significant cause of morbidity and mortality. Circulation. 2004;109:1354–1358. doi: 10.1161/01.CIR.0000121361.01862.A4 [DOI] [PubMed] [Google Scholar]
- 34.Kamath BM, Podkameni G, Hutchinson AL, Leonard LD, Gerfen J, Krantz ID, Piccoli DA, Spinner NB, Loomes KM, Meyers K. Renal anomalies in Alagille syndrome: a disease-defining feature. Am J Med Genet A. 2012;158A:85–89. doi: 10.1002/ajmg.a.34369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacquet A, Guiochon-Mantel A, Noël LH, Sqalli T, Bedossa P, Hadchouel M, Grünfeld JP, Fakhouri F. Alagille syndrome in adult patients: it is never too late. Am J Kidney Dis. 2007;49:705–709. doi: 10.1053/j.ajkd.2007.02.262 [DOI] [PubMed] [Google Scholar]
- 36.Dejardin A, Goffette P, Moulin P, Verhelst R, Cornu G, De Plaen JF, Persu A. Severe hypoplasia of the abdominal aorta and its branches in a patient and his daughter. J Intern Med. 2004;255:130–136. doi: 10.1046/j.0954-6820.2003.01240.x [DOI] [PubMed] [Google Scholar]
- 37.Guo DC, Duan XY, Regalado ES, Mellor-Crummey L, Kwartler CS, Kim D, Lieberman K, de Vries BBA, Pfundt R, Schinzel A, et al. ; University of Washington Center for Mendelian Genomics. Loss-of-function mutations in YY1AP1 lead to grange syndrome and a fibromuscular dysplasia-like vascular disease. Am J Hum Genet. 2017;100:21–30. doi: 10.1016/j.ajhg.2016.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baum MA, Harris HW, Jr, Burrows PE, Schofield DE, Somers MJ. Renovascular hypertension in Marfan syndrome. Pediatr Nephrol. 1997;11:499–501. doi: 10.1007/s004670050327 [DOI] [PubMed] [Google Scholar]
- 39.Patzer L, Basche S, Misselwitz J. Renal artery stenosis and aneurysmatic dilatation of arteria carotis interna in tuberous sclerosis complex. Pediatr Nephrol. 2002;17:193–196. doi: 10.1007/s00467-001-0799-5 [DOI] [PubMed] [Google Scholar]
- 40.De Groote K, Demulier L, De Backer J, De Wolf D, De Schepper J, T’sjoen G, De Backer T. Arterial hypertension in Turner syndrome: a review of the literature and a practical approach for diagnosis and treatment. J Hypertens. 2015;33:1342–1351. doi: 10.1097/HJH.0000000000000599 [DOI] [PubMed] [Google Scholar]
- 41.Zimmo L, Rudarakanchana N, Thompson M, Hamady MS, Cheshire NJ, Bicknell CD. Renal artery aneurysm formation secondary to pseudoxanthoma elasticum. J Vasc Surg. 2013;57:842–844. doi: 10.1016/j.jvs.2012.09.016 [DOI] [PubMed] [Google Scholar]
- 42.Alomari AK, Alomari AI. A rare association of fibromuscular dysplasia, renal agenesis, renal arteriovenous fistulae, and vertebral anomalies: expanding the V in VACTERL association. Am J Med Genet A. 2012;158A:2863–2865. doi: 10.1002/ajmg.a.33523 [DOI] [PubMed] [Google Scholar]
- 43.Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet. 2015;385:800–811. doi: 10.1016/S0140-6736(14)61005-9 [DOI] [PubMed] [Google Scholar]
- 44.Williams DM, Lee DY, Hamilton BH, Marx MV, Narasimham DL, Kazanjian SN, Prince MR, Andrews JC, Cho KJ, Deeb GM. The dissected aorta: part III. Anatomy and radiologic diagnosis of branch-vessel compromise. Radiology. 1997;203:37–44. doi: 10.1148/radiology.203.1.9122414 [DOI] [PubMed] [Google Scholar]
- 45.García-Familiar A, Ortiz-Gutiérrez F, De Blas-Bravo M, Sánchez-Abuín J, Rodríguez Sáenz de Buruaga V, Egaña-Barrenechea JM. Isolated spontaneous renal artery dissection: endovascular management. Ann Vasc Surg. 2014;28:1034.e5–1034.e8. doi: 10.1016/j.avsg.2013.06.043 [DOI] [PubMed] [Google Scholar]
- 46.Crawford TC, Beaulieu RJ, Ehlert BA, Ratchford EV, Black JH., 3rd.Malperfusion syndromes in aortic dissections. Vasc Med. 2016;21:264–273. doi: 10.1177/1358863X15625371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Howard DP, Banerjee A, Fairhead JF, Perkins J, Silver LE, Rothwell PM; Oxford Vascular Study. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford vascular study. Circulation. 2013;127:2031–2037. doi: 10.1161/CIRCULATIONAHA.112.000483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Greenberg R, Khwaja J, Haulon S, Fulton G. Aortic dissections: new perspectives and treatment paradigms. Eur J Vasc Endovasc Surg. 2003;26:579–586. doi: 10.1016/s1078-5884(03)00415-5 [DOI] [PubMed] [Google Scholar]
- 49.Barnes DM, Williams DM, Dasika NL, Patel HJ, Weder AB, Stanley JC, Deeb GM, Upchurch GR., Jr.A single-center experience treating renal malperfusion after aortic dissection with central aortic fenestration and renal artery stenting. J Vasc Surg. 2008;47:903–910. discussion 910. doi: 10.1016/j.jvs.2007.12.057 [DOI] [PubMed] [Google Scholar]
- 50.Lauterbach SR, Cambria RP, Brewster DC, Gertler JP, Lamuraglia GM, Isselbacher EM, Hilgenberg AD, Moncure AC. Contemporary management of aortic branch compromise resulting from acute aortic dissection. J Vasc Surg. 2001;33:1185–1192. doi: 10.1067/mva.2001.115377 [DOI] [PubMed] [Google Scholar]
- 51.Faucon AL, Bobrie G, Jannot AS, Azarine A, Plouin PF, Azizi M, Amar L. Cause of renal infarction: a retrospective analysis of 186 consecutive cases. J Hypertens. 2018;36:634–640. doi: 10.1097/HJH.0000000000001588 [DOI] [PubMed] [Google Scholar]
- 52.Renaud S, Leray-Moraguès H, Chenine L, Canaud L, Vernhet-Kovacsik H, Canaud B. Spontaneous renal artery dissection with renal infarction. Clin Kidney J. 2012;5:261–264. doi: 10.1093/ckj/sfs047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Funaki B. Iatrogenic renal dissection during renal artery stenting. Semin Intervent Radiol. 2005;22:141–143. doi: 10.1055/s-2005-871870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, Kapelak B, Walton A, Sievert H, Thambar S, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009;373:1275–1281. doi: 10.1016/S0140-6736(09)60566-3 [DOI] [PubMed] [Google Scholar]
- 55.Faucon AL, Bobrie G, Azarine A, Mousseaux E, Mirault T, Lorthioir A, Azizi M, Amar L. Renal outcome and new-onset renal and extrarenal dissections in patients with nontrauma renal artery dissection associated with renal infarction. Hypertension. 2021;78:51–61. doi: 10.1161/HYPERTENSIONAHA.120.16540 [DOI] [PubMed] [Google Scholar]
- 56.Persu A, Ciurică S, Pappaccogli M. Baseline brain-to-pelvis imaging predicts subsequent arterial complications in patients with renal artery dissection. Hypertension. 2021;78:62–64. doi: 10.1161/HYPERTENSIONAHA.121.17294 [DOI] [PubMed] [Google Scholar]
- 57.Afshinnia F, Sundaram B, Rao P, Stanley J, Bitzer M. Evaluation of characteristics, associations and clinical course of isolated spontaneous renal artery dissection. Nephrol Dial Transplant. 2013;28:2089–2098. doi: 10.1093/ndt/gft073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Reilly LM, Cunningham CG, Maggisano R, Ehrenfeld WK, Stoney RJ. The role of arterial reconstruction in spontaneous renal artery dissection. J Vasc Surg. 1991;14:468–77. doi: 10.1016/0741-5214(91)90240-U [PubMed] [Google Scholar]
- 59.Markus HS, Hayter E, Levi C, Feldman A, Venables G, Norris J; Investigators Ct. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (cadiss): a randomised trial. Lancet Neurol. 2015;14:361–367. doi: 10.1016/S1474-4422(15)70018-9 [DOI] [PubMed] [Google Scholar]
- 60.Pellerin O, Garçon P, Beyssen B, Raynaud A, Rossignol P, Jacquot C, Plouin PF, Sapoval M. Spontaneous renal artery dissection: long-term outcomes after endovascular stent placement. J Vasc Interv Radiol. 2009;20:1024–1030. doi: 10.1016/j.jvir.2009.04.069 [DOI] [PubMed] [Google Scholar]
- 61.Lacombe M. Isolated spontaneous dissection of the renal artery. J Vasc Surg. 2001;33:385–391. doi: 10.1067/mva.2001.111736 [DOI] [PubMed] [Google Scholar]
- 62.Jeong MJ, Kwon H, Kim A, Ko GY, Han Y, Kwon TW, Cho YP. Clinical outcomes of conservative treatment in patients with symptomatic isolated spontaneous renal artery dissection and comparison with superior mesenteric artery dissection. Eur J Vasc Endovasc Surg. 2018;56:291–297. doi: 10.1016/j.ejvs.2018.05.002 [DOI] [PubMed] [Google Scholar]
- 63.Kim ESH, Beckman J. Takayasu arteritis: challenges in diagnosis and management. Heart. 2018;104:558–565. doi: 10.1136/heartjnl-2016-310848 [DOI] [PubMed] [Google Scholar]
- 64.Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY, Lie JT, Lightfoot RW., Jr.The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990;33:1129–1134. doi: 10.1002/art.1780330811 [DOI] [PubMed] [Google Scholar]
- 65.Kinjo H, Kafa A. The results of treatment in renal artery stenosis due to Takayasu disease: comparison between surgery, angioplasty, and stenting. A monocentrique retrospective study. G Chir. 2015;36:161–167. doi: 10.11138/gchir/2015.36.4.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zaldivar Villon MLF, de la Rocha JAL, Espinoza LR. Takayasu arteritis: recent developments. Curr Rheumatol Rep. 2019;21:45. doi: 10.1007/s11926-019-0848-3 [DOI] [PubMed] [Google Scholar]
- 67.Saadoun D, Lambert M, Mirault T, Resche-Rigon M, Koskas F, Cluzel P, Mignot C, Schoindre Y, Chiche L, Hatron PY, et al. Retrospective analysis of surgery versus endovascular intervention in Takayasu arteritis: a multicenter experience. Circulation. 2012;125:813–819. doi: 10.1161/CIRCULATIONAHA.111.058032 [DOI] [PubMed] [Google Scholar]
- 68.Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, et al. 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheum. 2013;65:1–11. doi: 10.1002/art.37715 [DOI] [PubMed] [Google Scholar]
- 69.Weyand CM, Goronzy JJ. Medium- and large-vessel vasculitis. N Engl J Med. 2003;349:160–169. doi: 10.1056/NEJMra022694 [DOI] [PubMed] [Google Scholar]
- 70.Skeik N, Olson SL, Hari G, Pavia ML. Segmental arterial mediolysis (SAM): systematic review and analysis of 143 cases. Vasc Med. 2019;24:549–563. doi: 10.1177/1358863X19873410 [DOI] [PubMed] [Google Scholar]
- 71.Shenouda M, Riga C, Naji Y, Renton S. Segmental arterial mediolysis: a systematic review of 85 cases. Ann Vasc Surg. 2014;28:269–277. doi: 10.1016/j.avsg.2013.03.003 [DOI] [PubMed] [Google Scholar]
- 72.Naidu SG, Menias CO, Oklu R, Hines RS, Alhalabi K, Makar G, Shamoun FE, Henkin S, McBane RD. Segmental arterial mediolysis: abdominal imaging of and disease course in 111 patients. AJR Am J Roentgenol. 2018;210:899–905. doi: 10.2214/AJR.17.18309 [DOI] [PubMed] [Google Scholar]
- 73.Peng KX, Davila VJ, Stone WM, Shamoun FE, Naidu SG, McBane RD, Money SR. Natural history and management outcomes of segmental arterial mediolysis. J Vasc Surg. 2019;70:1877–1886. doi: 10.1016/j.jvs.2019.02.068 [DOI] [PubMed] [Google Scholar]
- 74.Alhalabi K, Menias C, Hines R, Mamoun I, Naidu S. Imaging and clinical findings in segmental arterial mediolysis (SAM). Abdom Radiol (NY). 2017;42:602–611. doi: 10.1007/s00261-016-0887-4 [DOI] [PubMed] [Google Scholar]
- 75.Unal N, Paytoncu S, Saylam GS, Kumtepe S, Kösecik M, Kir M, Akçoral A, Kozan O. Takayasu’s arteritis with bilateral renal artery stenosis: unilateral kissing balloon angioplasty. Int J Cardiol. 2004;93:299–300. doi: 10.1016/S0167-5273(03)00165-7 [DOI] [PubMed] [Google Scholar]
- 76.Gaud S, Cridlig J, Claudon M, Diarrassouba A, Kessler M, Frimat L. [Segmental arterial mediolysis and renovascular hypertension]. Nephrol Ther. 2010;6:597–601. doi: 10.1016/j.nephro.2010.06.002 [DOI] [PubMed] [Google Scholar]
- 77.Cohen DL, Soulen MC. A patient with acute kidney pain and high blood pressure. Clin J Am Soc Nephrol. 2015;10:696–702. doi: 10.2215/CJN.10171014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Slavin RE. Segmental arterial mediolysis: course, sequelae, prognosis, and pathologic-radiologic correlation. Cardiovasc Pathol. 2009;18:352–360. doi: 10.1016/j.carpath.2008.09.001 [DOI] [PubMed] [Google Scholar]
- 79.Kalva SP, Somarouthu B, Jaff MR, Wicky S. Segmental arterial mediolysis: clinical and imaging features at presentation and during follow-up. J Vasc Interv Radiol. 2011;22:1380–1387. doi: 10.1016/j.jvir.2011.07.001 [DOI] [PubMed] [Google Scholar]
- 80.Talenfeld AD, Schwope RB, Alper HJ, Cohen EI, Lookstein RA. MDCT angiography of the renal arteries in patients with atherosclerotic renal artery stenosis: implications for renal artery stenting with distal protection. AJR Am J Roentgenol. 2007;188:1652–1658. doi: 10.2214/AJR.06.1255 [DOI] [PubMed] [Google Scholar]
- 81.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, et al. ; American Association for Vascular Surgery/Society for Vascular Surgery; Society for Cardiovascular Angiography and Interventions; Society for Vascular Medicine and Biology; Society of Interventional Radiology; ACC/AHA Task Force on Practice Guidelines. ACC/AHA Guidelines for the Management of Patients with Peripheral Arterial Disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Associations for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (writing committee to develop guidelines for the management of patients with peripheral arterial disease)–summary of recommendations. J Vasc Interv Radiol. 2006;17:1383–1397. quiz 1398. doi: 10.1097/01.RVI.0000240426.53079.46 [DOI] [PubMed] [Google Scholar]
- 82.Stanley JC, Rhodes EL, Gewertz BL, Chang CY, Walter JF, Fry WJ. Renal artery aneurysms. Significance of macroaneurysms exclusive of dissections and fibrodysplastic mural dilations. Arch Surg. 1975;110:1327–1333. doi: 10.1001/archsurg.1975.01360170067009 [DOI] [PubMed] [Google Scholar]
- 83.Henke PK, Cardneau JD, Welling TH, 3rd, Upchurch GR, Jr, Wakefield TW, Jacobs LA, Proctor SB, Greenfield LJ, Stanley JC. Renal artery aneurysms: a 35-year clinical experience with 252 aneurysms in 168 patients. Ann Surg. 2001;234:454–462. discussion 462. doi: 10.1097/00000658-200110000-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Martin RS, 3rd, Meacham PW, Ditesheim JA, Mulherin JL, Jr, Edwards WH. Renal artery aneurysm: selective treatment for hypertension and prevention of rupture. J Vasc Surg. 1989;9:26–34. [PubMed] [Google Scholar]
- 85.Klausner JQ, Harlander-Locke MP, Plotnik AN, Lehrman E, DeRubertis BG, Lawrence PF. Current treatment of renal artery aneurysms may be too aggressive. J Vasc Surg. 2014;59:1356–1361. doi: 10.1016/j.jvs.2013.11.062 [DOI] [PubMed] [Google Scholar]
- 86.Pfeiffer T, Reiher L, Grabitz K, Grünhage B, Häfele S, Voiculescu A, Fürst G, Sandmann W. Reconstruction for renal artery aneurysm: operative techniques and long-term results. J Vasc Surg. 2003;37:293–300. doi: 10.1067/mva.2003.117 [DOI] [PubMed] [Google Scholar]
- 87.Down LA, Papavassiliou DV, O’Rear EA. Arterial deformation with renal artery aneurysm as a basis for secondary hypertension. Biorheology. 2013;50:17–31. doi: 10.3233/BIR-130623 [DOI] [PubMed] [Google Scholar]
- 88.Klausner JQ, Lawrence PF, Harlander-Locke MP, Coleman DM, Stanley JC, Fujimura N; Vascular Low-Frequency Disease Consortium. The contemporary management of renal artery aneurysms. J Vasc Surg. 2015;61:978–984. doi: 10.1016/j.jvs.2014.10.107 [DOI] [PubMed] [Google Scholar]
- 89.Coleman DM, Stanley JC. Renal artery aneurysms. J Vasc Surg. 2015;62:779–785. doi: 10.1016/j.jvs.2015.05.034 [DOI] [PubMed] [Google Scholar]
- 90.Loeys BL, Schwarze U, Holm T, Callewaert BL, Thomas GH, Pannu H, De Backer JF, Oswald GL, Symoens S, Manouvrier S, et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med. 2006;355:788–798. doi: 10.1056/NEJMoa055695 [DOI] [PubMed] [Google Scholar]
- 91.Pepin M, Schwarze U, Superti-Furga A, Byers PH. Clinical and genetic features of Ehlers-Danlos syndrome type IV, the vascular type. N Engl J Med. 2000;342:673–680. doi: 10.1056/NEJM200003093421001 [DOI] [PubMed] [Google Scholar]
- 92.Cohen JR, Shamash FS. Ruptured renal artery aneurysms during pregnancy. J Vasc Surg. 1987;6:51–59. doi: 10.1067/mva.1987.avs0060051 [DOI] [PubMed] [Google Scholar]
- 93.Klein GE, Szolar DH, Breinl E, Raith J, Schreyer HH. Endovascular treatment of renal artery aneurysms with conventional non-detachable microcoils and Guglielmi detachable coils. Br J Urol. 1997;79:852–860. doi: 10.1046/j.1464-410x.1997.00157.x [DOI] [PubMed] [Google Scholar]
- 94.Tsilimparis N, Reeves JG, Dayama A, Perez SD, Debus ES, Ricotta JJ., 2nd.Endovascular vs open repair of renal artery aneurysms: outcomes of repair and long-term renal function. J Am Coll Surg. 2013;217:263–269. doi: 10.1016/j.jamcollsurg.2013.03.021 [DOI] [PubMed] [Google Scholar]
- 95.Ha JF, Phillips M, Faulkner K. Splenic artery aneurysm rupture in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2009;146:133–137. doi: 10.1016/j.ejogrb.2009.05.034 [DOI] [PubMed] [Google Scholar]
- 96.Kozaki S, Miyamoto S, Shuto T, Tanaka H, Wada T, Anai H. Rupture of the remaining renal artery aneurysm while waiting for stage 2 surgery for a patient with bilateral renal artery aneurysms and multiple aneurysms. Ann Vasc Surg. 2019;57:275.e5–275.e8. doi: 10.1016/j.avsg.2018.10.032 [DOI] [PubMed] [Google Scholar]
- 97.Cura M, Elmerhi F, Suri R, Bugnone A, Dalsaso T. Vascular malformations and arteriovenous fistulas of the kidney. Acta Radiol. 2010;51:144–149. doi: 10.3109/02841850903463646 [DOI] [PubMed] [Google Scholar]
- 98.Jacobi J, Hilgers KF, Lang W, Eckardt KU, Uder M. Images in vascular medicine: renal arteriovenous fistula. Vasc Med. 2010;15:433–434. doi: 10.1177/1358863X10376000 [DOI] [PubMed] [Google Scholar]
- 99.Paschalis-Purtak K, Januszewicz M, Rokicki A, Puciłowska B, Imiela J, Cybulska I, Cieśla W, Prejbisz A, Szostek M, Januszewicz A. Arteriovenous fistula of the kidney: a case report of 47-year-old female patient treated by embolisation. J Hum Hypertens. 2003;17:293–296. doi: 10.1038/sj.jhh.1001544 [DOI] [PubMed] [Google Scholar]
- 100.Perrin M, Lousquy R, Rossignol M, Bonnin P. Renal arteriovenous fistula revealed by severe hypertension during pregnancy. BMJ Case Rep. 2013;2013:bcr2013200559. doi: 10.1136/bcr-2013-200559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.de Jong PE, van Bockel JH, de Zeeuw D. Unilateral renal parenchymal disease with contralateral renal artery stenosis of the fibrodysplasia type. Ann Intern Med. 1989;110:437–445. doi: 10.7326/0003-4819-110-6-437 [DOI] [PubMed] [Google Scholar]
- 102.Imray TJ, Cohen AJ, Hahn L. Renal arteriovenous fistula associated with fibromuscular dysplasia. Urology. 1984;23:378–380. doi: 10.1016/0090-4295(84)90146-8 [DOI] [PubMed] [Google Scholar]
- 103.Sosa-Barrios RH, Burguera V, Rodriguez-Mendiola N, Galeano C, Elias S, Ruiz-Roso G, Jimenez-Alvaro S, Liaño F, Rivera-Gorrin M. Arteriovenous fistulae after renal biopsy: diagnosis and outcomes using Doppler ultrasound assessment. BMC Nephrol. 2017;18:365. doi: 10.1186/s12882-017-0786-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tarif N, Dunne PM, Parachuru PR, Bakir AA. Life-threatening hematuria from an arteriovenous fistula complicating an open renal biopsy. Nephron. 1998;80:66–70. doi: 10.1159/000045129 [DOI] [PubMed] [Google Scholar]
- 105.Al-Katib S, Shetty M, Jafri SM, Jafri SZ. Radiologic assessment of native renal vasculature: a multimodality review. Radiographics. 2017;37:136–156. doi: 10.1148/rg.2017160060 [DOI] [PubMed] [Google Scholar]
- 106.Alscher DM, Hupp T, Mettang T, Kuhlmann U. A patient with hypertension was cured after resection of a renal AV fistula. Nephrol Dial Transplant. 2000;15:249–250. doi: 10.1093/ndt/15.2.249 [DOI] [PubMed] [Google Scholar]
- 107.Pineo GF, Thorndyke WC, Steed BL. Spontaneous renal artery thrombosis: successful lysis with streptokinase. J Urol. 1987;138:1223–1225. doi: 10.1016/s0022-5347(17)43557-9 [DOI] [PubMed] [Google Scholar]
- 108.Cao W, Li A, Li J, Wu C, Cui S, Zhou Z, Liu Y, Wilcox CS, Hou FF. Reno-cerebral reflex activates the renin-angiotensin system, promoting oxidative stress and renal damage after ischemia-reperfusion injury. Antioxid Redox Signal. 2017;27:415–432. doi: 10.1089/ars.2016.6827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Korzets Z, Plotkin E, Bernheim J, Zissin R. The clinical spectrum of acute renal infarction. Isr Med Assoc J. 2002;4:781–784. [PubMed] [Google Scholar]
- 110.Raghavendran M, Sarkar M, Kumar KG. “Isolated spontaneous renal artery thrombosis - a rare cause of acute flank pain”. Urol Case Rep. 2016;9:4–5. doi: 10.1016/j.eucr.2016.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nakamura M, Ohnishi T, Okamoto S, Yamakado T, Isaka N, Nakano T. Abdominal aortic thrombosis in a patient with nephrotic syndrome. Am J Nephrol. 1998;18:64–66. doi: 10.1159/000013307 [DOI] [PubMed] [Google Scholar]
- 112.Bienaimé F, Legendre C, Terzi F, Canaud G. Antiphospholipid syndrome and kidney disease. Kidney Int. 2017;91:34–44. doi: 10.1016/j.kint.2016.06.026 [DOI] [PubMed] [Google Scholar]
- 113.Philipponnet C, Aniort J, Chabrot P, Souweine B, Heng AE. Renal artery thrombosis induced by COVID-19. Clin Kidney J. 2020;13:713. doi: 10.1093/ckj/sfaa141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hazanov N, Somin M, Attali M, Beilinson N, Thaler M, Mouallem M, Maor Y, Zaks N, Malnick S. Acute renal embolism. Forty-four cases of renal infarction in patients with atrial fibrillation. Medicine (Baltimore). 2004;83:292–299. doi: 10.1097/01.md.0000141097.08000.99 [DOI] [PubMed] [Google Scholar]
- 114.Rossignol P, Chatellier G, Azizi M, Plouin PF. Proteinuria in renal artery occlusion is related to active renin concentration and contralateral kidney size. J Hypertens. 2002;20:139–144. doi: 10.1097/00004872-200201000-00020 [DOI] [PubMed] [Google Scholar]
- 116.Cai S, Ouyang YS, Li JC, Dai Q, Tan L, Xia Y, Xu ZH, Li HJ, Jiang YX. Evaluation of acute renal artery thrombosis or embolism with color Doppler sonography. Clin Imaging. 2008;32:367–371. doi: 10.1016/j.clinimag.2008.02.023 [DOI] [PubMed] [Google Scholar]
- 117.Taylor KJ, Morse SS, Rigsby CM, Bia M, Schiff M. Vascular complications in renal allografts: detection with duplex Doppler US. Radiology. 1987;1621 Pt 131–38. doi: 10.1148/radiology.162.1.3538150 [DOI] [PubMed] [Google Scholar]
- 118.Januszko-Giergielewicz B, Kubiak M, Gromadziński L, Paszkowska E. [Renal artery thrombosis and renal infarction, diagnostic and therapeutic difficulties–reports of two cases]. Przegl Lek. 2014;71:410–412. [PubMed] [Google Scholar]
- 119.Monterrosas OG, Pereda López LA, Velasco Barcena JA, Scalone G. Acute thrombosis of left renal artery treated with thrombolysis and percutaneous transluminal angioplasty. Eur Heart J. 2016;37:2734. doi: 10.1093/eurheartj/ehw243 [DOI] [PubMed] [Google Scholar]
- 120.Lopez VM, Glauser J. A case of renal artery thrombosis with renal infarction. J Emerg Trauma Shock. 2010;3:302. doi: 10.4103/0974-2700.66569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Salam TA, Lumsden AB, Martin LG. Local infusion of fibrinolytic agents for acute renal artery thromboembolism: report of ten cases. Ann Vasc Surg. 1993;7:21–26. doi: 10.1007/BF02042655 [DOI] [PubMed] [Google Scholar]