Abstract
Context:
Multiple chronic illnesses associated with ageing population demands the role of polypharmacy. Drug utilization study in terms of description of drug use pattern in the geriatric patients aids in monitoring polypharmacy as well as to determine the factors contributing to it.
Objectives:
To analyse the drug utilization pattern in geriatric patients at a rural health training centre.
Subjects and Methods:
A cross-sectional study was conducted in a rural health centre to assess the drug utilization pattern using the WHO core drug prescribing indicators. Polypharmacy was defined as usage of 5-8 drugs and excessive polypharmacy as intake of 10 or more drugs. The drugs were coded using Anatomical Therapeutical Chemical classification. Univariate and bivariate analysis were done using SPSS to present the data.
Results:
Among 207 patients, 29.5% were on polypharmacy and 1.5% patients on excessive polypharmacy. About 75% of patients had one or more comorbid medical condition. A total number of 829 drugs were prescribed and the average number of drugs per prescription was 4.02.
Conclusion:
The drug utilization pattern analysis in the geriatric patients reveals deviation of the average number of drugs per prescription from the WHO standard recommendation. The most common comorbid condition among the geriatric patients was diabetes mellitus. This drug utilization study imparts knowledge about the use of polypharmacy, comorbidities and the pattern of commonly used drugs among the geriatric patients in rural area. Periodic assessment of the pattern of drug utilization in the elderly aids to improve the prescribing pattern and minimize patient harm.
Keywords: Drug utilization, geriatrics, polypharmacy
Introduction
Ageing is at a growing pace globally and is considered to be one of the most significant phenomena of the century. In India by the year 2050 about 12.5% of the population will be 60 years and older as outlined by the United Nations Population Fund (UNFPA) report in 2017. In relation to the health sector, ageing tends to increase the risk of development of concomitant chronic diseases significantly.[1] This in turn poses a great challenge as the need of quality healthcare rises.
Multiple chronic illnesses in older population demands the role of polypharmacy. According to WHO, the administration of many drugs at the same time or administration of excessive number of drugs is defined as polypharmacy.[2] Excessive polypharmacy is defined as concomitant use of ten or more drugs in regular or need basis.[3] Use of polypharmacy may increase the risk of adverse drug reactions, drug interactions, patient noncompliance with treatment and medication errors especially in the elderly.[4]
Drug utilization study in terms of description of drug use pattern in the geriatric patients aids in monitoring polypharmacy as well as to determine the factors contributing to it. About two thirds of the elderly population in India live in rural areas and studies on drug utilization pattern in the elderly in a rural health setup are limited.[5] Such studies aid the primary care physicians at rural health centres to improve towards rational prescribing of drugs to the elderly. Also, periodic assessment of the pattern of drug utilization and optimization is essential for a better healthcare to the geriatric population. Hence the objective of this study is to analyse the drug utilization pattern in geriatric patients at a rural health training centre.
Subjects and Methods
Study design and setting
A prospective cross-sectional study was conducted for a period of two months in a Geriatric Health Clinic which is held once a week at a rural health training centre after obtaining prior Institutional Human Ethics Committee clearance and as per GCP guidelines.
Participants
All the geriatric patients irrespective of gender aged above 60 years attending the Geriatric Health Clinic willing to participate in the study and who gave written informed consent were included in the study. Written informed consent written in patient's vernacular language was obtained. Out of 296 elderly patients who attended the clinic at the rural health centre during the period of 8 weeks, 207 patients consented to participate in the study. Confidentiality of the study participants was maintained.
Data collection
Data collection proforma consisting of details such as patient's age, gender, marital status, occupation, socioeconomic and educational status, details of any comorbid conditions, diagnosis and treatment given was recorded from the prescriptions given by the consulting physician. Information regarding health status, usage of medicines, any alternative system of medicine followed was collected through a self-administered questionnaire. Initially a pre-test to elicit the reliability and any problem in clarity or interpretation of questions was conducted and rectified.
Drug utilization evaluation
The various tools used to analyse the drug utilization pattern were the WHO core drug prescribing indicators wherein the number of drugs prescribed and the dosage regimen of each of the prescription was assessed.[6] The brand name of the drugs recorded by the investigator was subsequently coded using Anatomical Therapeutical Chemical (ATC) classification as defined by World Health Organization.[7] Polypharmacy was defined as usage of 5 to 8 drugs whereas excessive polypharmacy was defined as intake of 9 or more drugs.
Statistical analysis
Data collected was entered into Microsoft excel. Data analysis was performed using SPSS software version 17. Univariate analysis such as frequencies and percentages were used to present the data. Relation between dependent and independent variables will be given by bivariant analysis. The P value of <0.005 will be considered statistically significant.
Results
A total of 296 elderly patients who attended the geriatric clinic at rural health centre were approached who were willing to give written consent to participate in this study and at the end of 2 months, a total of 207 prescriptions from consented patients were analyzed (response rate: 70%).
On analysis about 29.5% (61) were on polypharmacy and only 1.5% (3) patients were on excessive polypharmacy.
Characteristics of the elderly patients attending the rural health centre
Out of the 207 patients, 51.2% (106) were males and 48.8% (101) were females. Most of the patients, 42% (87) were in the age group of 65-69 years. One or more comorbid conditions were present in all of the patients (100%) on excessive polypharmacy and in about 84.4% of the patients on polypharmacy [Table 1].
Table 1.
Sociodemographic characteristics of the geriatric out-patients at a rural health training centre
| Variable | Non-Polypharmacy n=143 (%) | Polypharmacy n=61 (%) | Excessive Polypharmacy n=3 (%) | Total n=207 (%) |
|---|---|---|---|---|
| Age in years | ||||
| 60-64 | 45 (31.5) | 15 (24.6) | 1 (33.3) | 61 (29.5) |
| 65-69 | 57 (39.9) | 29 (47.5) | 1 (33.3) | 87 (42) |
| 70-74 | 24 (16.8) | 11 (18) | 1 (33.3) | 36 (17.4) |
| 75-79 | 10 (7) | 5 (8.2) | - | 15 (7.2) |
| >80 | 7 (4.9) | 1 (1.6) | - | 8 (3.9) |
| Gender | ||||
| Male | 74 (51.7) | 29 (47.5) | 3 (100) | 106 (51.2) |
| Female | 69 (48.3) | 32 (52.5) | - | 101 (48.8) |
| Marital status | ||||
| Widowed/Married | 58 (40.6) | 21 (34.4) | 2 (66.7) | 81 (39.1) |
| Unmarried | 85 (59.4) | 40 (65.6) | 1 (33.3) | 126 (60.9) |
| 0 | 0 | 0 | 0 | |
| Occupation | ||||
| Unemployed/Housewife | 65 (45.5) | 35 (57.4) | 3 (100) | 101 (48.8) |
| Employed | 78 (54.5) | 26 (42.6) | 0 | 106 (51.2) |
| Socioeconomic Status | ||||
| Lower Middle Class | 36 (25.2) | 19 (31.1) | 1 (66.7) | 56 (27.1) |
| Middle Class | 100 (69.9) | 40 (65.6) | 2 (33.3) | 142 (68.6) |
| Upper Middle Class | 6 (4.2) | 2 (3.3) | 0 | 8 (3.9) |
| High Class | 1 (0.7) | 0 | 0 | 1 (0.5) |
| Educational Status | ||||
| Illiterate | 64 (44.6) | 29 (47.5) | 3 (100) | 95 (45.9) |
| Primary Education | 54 (37.5) | 27 (44.3) | 82 (39.6) | |
| Higher Education | 25 (17.5) | 5 (8.2) | 30 (14.5) | |
| Comorbid conditions | ||||
| Present | 101 (70.5) | 51 (84.4) | 3 (100) | 155 (75) |
| Absent | 42 (29.5) | 10 (16.6) | 0 | 52 (25) |
In this study about 18.7% of the elderly patients with polypharmacy and excessive polypharmacy reported about irregular intake of medicines. An overall of 44% patients had visited health care facility in the past one month. None of the patients on excessive polypharmacy revealed to be on any complementary system of medicines [Table 2].
Table 2.
Characteristics of the elderly patients
| Variable | Non-Polypharmacy n=143 (%) | Polypharmacy n=61 (%) | Excessive Polypharmacy n=3 (%) | Total n=207 (%) |
|---|---|---|---|---|
| Self-Reported Health | ||||
| Good | 22 (15.4) | 5 (8.2) | 0 | 27 (13) |
| Moderate | 106 (74.1) | 48 (78.7) | 3 (100) | 157 (75.8) |
| Poor | 15 (10.5) | 8 (13.1) | 0 | 23 (11.1) |
| Usage of Medicines | ||||
| Regular | 69 (48.3) | 45 (73.8) | 2 (66.7) | 116 (56) |
| Irregular | 74 (51.7) | 16 (26.2) | 1 (33.3) | 91 (44) |
| Health Status | ||||
| Any longstanding illness or chronic conditions | 13 (9.1) | 11 (18) | 1 (33.3) | 25 (12.1) |
| Handicap | 0 | 0 | 0 | 0 |
| Depression in past one year | 8 (5.6) | 3 (4.9) | 0 | 11 (5.3) |
| Contact with health services in past one month | 58 (40.6) | 31 (50.8) | 2 (66.7) | 91 (44) |
| Hospitalization in past one year | 14 (9.8) | 4 (6.6) | 0 | 18 (8.7) |
| Undergone any surgery in past one year | 4 (2.8) | 1 (1.6) | 0 | 5 (2.4) |
| Nil | 46 (32.2) | 11 (18) | 0 | 57 (27.5) |
| Alternative system of Medicine Followed | ||||
| Ayurvedic | 5 (3.5) | 6 (9.8) | 0 | 11 (5.3) |
| Homeopathic | 5 (3.5) | 1 (1.6) | 0 | 6 (2.9) |
| Siddha | 4 (2.8) | 1 (1.6) | 0 | 5 (2.4) |
| Unani | 0 | 0 | 0 | 0 |
| Nil | 129 (90.2) | 53 (87) | 3 (100) | 185 (89.4) |
Statistically significant differences were not obtained between the three subgroups of patients namely non- polypharmacy, polypharmacy and excessive polypharmacy, based on their sociodemographic and health related characteristics.
Comorbid medical conditions prevalent in the geriatric patients
The average number of comorbidities was 1.6 with the most common comorbid medical condition being diabetes mellitus in about 35.6% (55), followed by hypertension and osteoarthritis in 30.4% (47) of patients respectively [Table 3].
Table 3.
Comorbid medical conditions prevalent in the geriatric patients
| Comorbid medical conditions | Number of patients (percentage of patients who suffered from particular disease) |
|---|---|
| Diabetes mellitus | 55 (35.6) |
| Hypertension | 47 (30.4) |
| Heart disease | 21 (13.5) |
| Musculoskeletal disorders | 42 (27.1) |
| Osteoarthritis | 47 (30.4) |
| Respiratory diseases | 17 (11.1) |
| CNS disorders | 13 (8.5) |
Prescription pattern of the study population
The average number of drugs per encounter was 4 and about 85.5% (709) of drugs were prescribed by the generic name. Percentage of encounters with an antibiotic injection prescribed were 9.2% and 22.7% respectively. A total of 87.6% (726) drugs were prescribed from National List of Essential Medicine [Table 4].
Table 4.
Prescription pattern in the study population using World Health Organization core drug prescribing indicators
| Core prescribing indicators | Values |
|---|---|
| Average number of drugs prescribed per encounter | 4 |
| Percentage of drugs prescribed by generic name | 709 (85.5) |
| Percentage of encounters with an injection prescribed | 47 (22.7) |
| Percentage of encounters with an antibiotic prescribed | 19 (9.2) |
| Percentage of drugs prescribed from National list of essential medicine | 726 (87.6) |
| Percentage of drugs prescribed as fixed dose combinations | 20 (9.7) |
Drug utilization pattern of the study population
A total number of 829 drugs were prescribed of which most of the drugs 91.6% (759) were prescribed as oral formulations, while 5.7% (47) and 2.7% (22) were prescribed as injectable and topical preparations respectively. Class A drugs acting on the gastrointestinal system 24% (200) were the most frequently prescribed drugs [Figure 1]. Among the active substances prescribed, majority of the patients received Ranitidine (A02BA02) 19% (158). Further, Metformin (A10BA02) 6% (50) and Enalapril (C09AA02) 8% (66) were the most commonly prescribed drugs for the comorbid conditions such as diabetes mellitus and hypertension respectively [Table 5].
Figure 1.
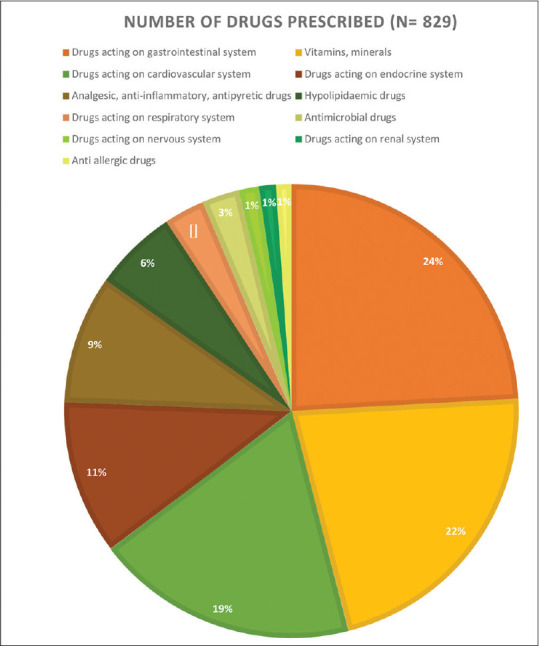
Category-Wise Distribution of the Drugs Prescribed in the Geriatric Population
Table 5.
Drugs utilization pattern according to WHO-ATC classification in the geriatric population
| Category of Drugs | Drug Name | Number of Drugs (%) (n=829) | Dosage Form | ATC Code |
|---|---|---|---|---|
| Drugs acting on | Ranitidine | 158 (19) | Oral | A02BA02 |
| gastrointestinal system | Metoclopramide | 15 (1.8) | Oral | A03FA01 |
| Ondansetron | 12 (1.4) | Oral, parenteral | A04AA01 | |
| Loperamide | 5 (0.6) | Oral | A07DA03 | |
| Oral rehydration salts | 5 (0.6) | Oral | A07CA | |
| Antacid | 5 (0.6) | Oral | A02AD01 | |
| Vitamins, minerals | Multivitamins | 73 (8.8) | Oral | A11AA03 |
| Calcium | 67 (8.1) | Oral | A02AC01 | |
| Ferrous sulphate | 23 (2.8) | Oral | B03AA07 | |
| Vitamin B 12 | 18 (2.2) | Parenteral | B03BA01 | |
| Drugs acting on | Enalapril | 66 (8) | Oral | C09AA02 |
| cardiovascular system | Aspirin | 29 (3.5) | Oral | B01AC06 |
| Clopidogrel | 26 (3.1) | Oral | B01AC04 | |
| Amlodipine | 18 (2.2) | Oral | C08CA01 | |
| Isosorbide dinitrate | 10 (1.2) | Oral | C01DA08 | |
| Spironolactone | 6 (0.7) | Oral | C03DA01 | |
| Drugs acting on | Metformin | 50 (6) | Oral | A10BA02 |
| endocrine system | Glibenclamide | 30 (3.6) | Oral | A10BB01 |
| Insulin | 7 (0.8) | Parenteral | A10AB02 | |
| Betamethasone | 4 (0.5) | Topical | D07XC01 | |
| Analgesic, anti- inflammatory, antipyretic drugs | Diclofenac | 50 (6) | Oral, topical, parenteral | M01AB05 |
| Paracetamol | 16 (1.9) | Oral | N02BE01 | |
| Ibuprofen | 10 (1.2) | Oral | M01AE01 | |
| Hypolipidaemic drugs | Atorvastatin | 49 (5.9) | Oral | C10AA05 |
| Drugs acting on | Salbutamol | 11 (1.3) | Oral | R03CC02 |
| respiratory system | Theophylline | 3 (0.4) | Oral | R03DA04 |
| Cough suppressant | 10 (1.2) | Oral | R05FB01 | |
| Antimicrobial drugs | Amoxycillin | 7 (0.8) | Oral | J01CA04 |
| Metronidazole | 5 (0.6) | Oral | A01AB17 | |
| Ciprofloxacin | 4 (0.5) | Oral | J01MA02 | |
| Gentamicin | 3 (0.4) | Topical | J01GB03 | |
| Norfloxacin | 3 (0.4) | Oral | J01MA06 | |
| Drugs acting on nervous system | Phenytoin | 7 (0.8) | Oral | N03AB02 |
| Valproate | 5 (0.6) | Oral | N03AG01 |
Discussion
On analysis, a total of 829 drugs were prescribed to the study population. The average number of drugs per encounter was 4 which is much lower when compared to a study done in geriatric patients at a secondary care hospital.[8] Although the average number of drugs prescribed is twice that of WHO recommendations, only about 29.5% and 1.5% were on polypharmacy and excessive polypharmacy. It is also notable that half 48.8% of the study population, with one or more comorbidities were not on polypharmacy.
Majority of the drugs 85.5% were prescribed by their generic names. By prescribing generic drugs, the risk of medication errors can be reduced by enabling clear and better communication among the health care professionals. The other advantages of generic drug prescribing is that they are cheap and readily available at various health sectors.
In this study, the most commonly prescribed antimicrobial drug was Amoxicillin (0.8%) and the percentage of encounters with an antibiotic prescribed was 9.7%, which is less than the value reported by Jyothsna et al.[9] This highlights the rational practice of a judicious use of antibiotics in geriatric patients, which was being followed at the rural health centre. Further, appropriate prescribing of antibiotics tends to play a pivotal role in preventing the emergence of antimicrobial resistance.
A total of 87.6% drugs were prescribed from National List of Essential Medicine as against the WHO standard at 100%.[10] One of the WHO initiatives for improving rational prescribing of drugs was the use of drugs from WHO or essential medicines list. By following essential medicines list, the health care professionals tend to prioritize and cater to major medical needs of the population.
One out of three patients in the study population on excessive polypharmacy was on irregular use of medicines and had no contact with the health services in the past one month. Research on the untoward effect such as nonadherence in geriatric patients on polypharmacy is well established.[11] This could be attributed to the cognitive and functional impairment associated with ageing.[12]
The most common ATC class of drugs prescribed was class A drugs for alimentary tract and metabolism, majority of which were in relation to gastrointestinal disorders. Further, Ranitidine was the most commonly prescribed drug. Prevalence of gastrointestinal disorders increase with ageing due to physiological process and also in relation to comorbidities. In this study, Ranitidine was prescribed in most of the encounters as a gastroprotective agent to counteract the epigastric pain associated with the use of non-steroidal anti-inflammatory drugs and Metformin.
This study has provided information about the pattern of drug use among geriatric patients in a rural healthcare center. Its strength is it being a prospective study, using the standard core WHO prescribing indicators and ATC classification of drug codes for analyzing the drug utilization pattern. The limitations of the study were its shorter duration and it being a single centered study.
Conclusion
The drug utilization pattern analysis in the geriatric patients reveals deviation of the average number of drugs per prescription from the WHO standard recommendation. The most common comorbid condition among the geriatric patients was diabetes mellitus. Among the drugs prescribed, alimentary tract and metabolism class of drugs were the most frequently prescribed drugs with Ranitidine being the highest prescribed drug among the elderly in the rural health centre. Periodic assessment of the pattern of drug utilization in the geriatric patients aids to improve the prescribing pattern and minimise patient harm.
Key messages
This study provides an insight about the drug utilization pattern in the geriatric population of rural areas in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Maresova P, Javanmardi E, Barakovic S, Barakovic Husic J, Tomsone S, Krejcar O, et al. Consequences of chronic diseases and other limitations associated with old age - A scoping review. BMC Public Health. 2019;19:1431. doi: 10.1186/s12889-019-7762-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.A glossary of terms for community health care and services for older persons. 2004. [Accessed November 05, 2004]. Available from: https://apps.who.int/iris/handle/10665/68896 .
- 3.Zhang N, Sundquist J, Sundquist K, Ji J. An increasing trend in the prevalence of polypharmacy in Sweden: A nationwide register-based study. Front Pharmacol. 2020;11:326. doi: 10.3389/fphar.2020.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Badawy NA, Labeeb SA, Alsamdan MF, Alazemi BF. Prevalence and risk of polypharmacy among community-dwelling, elderly Kuwaiti patients. Med Princ Pract. 2020;29:166–73. doi: 10.1159/000503298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ingle GK, Nath A. Geriatric health in India: Concerns and solutions. Indian J Community Med. 2008;33:214–8. doi: 10.4103/0970-0218.43225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. How to Investigate Drug Use in Health Facilities: Selected Drug use Indicators. Geneva: WHO/DAP/93.1; 1993. [Google Scholar]
- 7.World Health Organization. The Anatomical Therapeutic Chemical Classification System with Defined Daily Doses (ATC/DDD) Oslo: WHO; 2006. [Google Scholar]
- 8.Sumithira G, Anilkumar A, Rahman CVH, Bharanidharan SE, Ganesan V. Drug utilization pattern in geriatric patients of general medicine in a Secondary Care Hospital. Int J Pharm Sci Res. 2019;10:3364–72. [Google Scholar]
- 9.Jyothsna CS, Nagarajaiah BH, Shiva Kumar KM. Drug utilization pattern in geriatric inpatients of medicine wards at a government tertiary care hospital. Natl J Physiol Pharm Pharmacol. 2019;9:320–7. [Google Scholar]
- 10.WHO. Promoting Rational Use of Medicines: Core Components-WHO Policy Perspectives on Medicines. Geneva: World Health Organization; 2002. [Google Scholar]
- 11.Lai X, Zhu H, Huo X, Li Z. Polypharmacy in the oldest old (≥80 years of age) patients in China: A cross-sectional study. BMC Geriatr. 2018;18:64. doi: 10.1186/s12877-018-0754-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Assari S, Wisseh C, Saqib M, Bazargan M. Polypharmacy is associated with lower memory function in African American older adults. Brain Sci. 2020;10:49. doi: 10.3390/brainsci10010049. [DOI] [PMC free article] [PubMed] [Google Scholar]


