BACKGROUND:
The traditional paradigm of hospital surgical ward care consists of episodic bedside visits by providers with periodic perusals of the patient’s electronic health record (EHR). Vital signs and laboratory results are directly pushed to the EHR but not to providers themselves. Results that require intervention may not be recognized for hours. Remote surveillance programs continuously monitor electronic data and provide automatic alerts that can be routed to multidisciplinary providers. Such programs have not been explored in surgical general care wards.
METHODS:
We performed a quality improvement observational study of otolaryngology and ophthalmology patients on a general care ward from October 2017 to March 2019 during nighttime hours (17:00–07:00). The study was initiated due to the loss of on-site anesthesiology resources that historically helped respond to acute physiologic deterioration events. We implemented a remote surveillance software program to continuously monitor patients for severe vital signs and laboratory abnormalities and automatically alert the ward team and a remote critical care anesthesiology team. The primary end point was the true positive rate, defined as the proportion of alerts that were associated with a downstream action that changed the care of the patient. This was determined using systematic chart review. The secondary end point, as a measure of alarm fatigue, was the average number of alerts per clinician shift.
RESULTS:
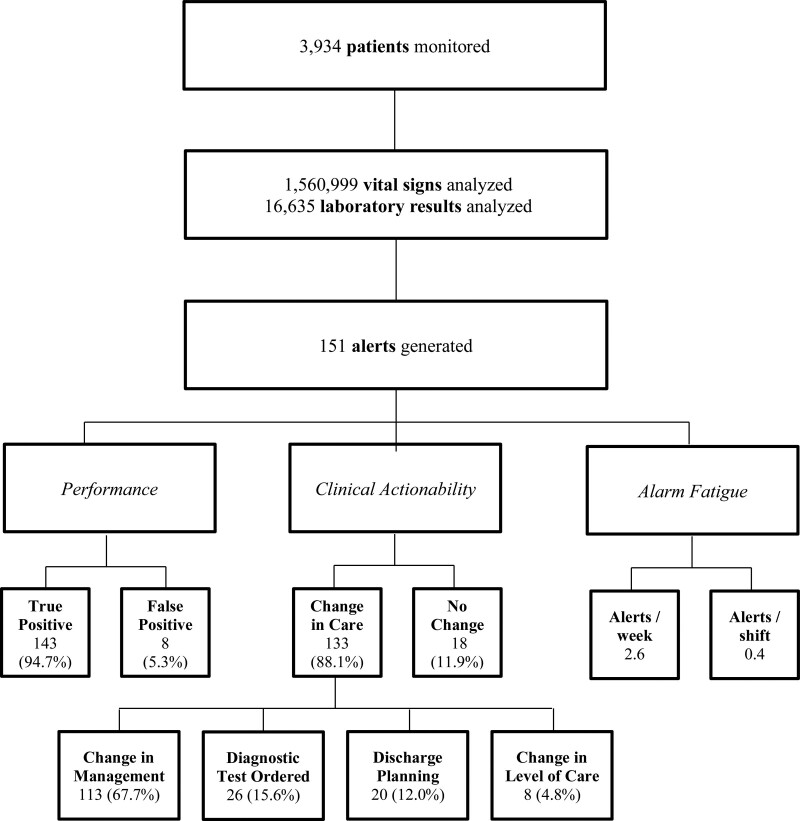
The software monitored 3926 hospital visits and analyzed 1,560,999 vitals signs and 16,635 laboratories. It generated 151 alerts, averaging 2.6 alerts per week. Of these, 143 (94.7%) were numerically accurate and 8 (5.3%) were inaccurate. Hypoxemia with oxygen saturation <88% was the most common etiology (92, 63%) followed by tachycardia >130 beats per minute (19, 13.3%). Among the accurate alerts, 133 (88.1%) were true positives with an associated clinical action. Actions included a change in management 113 (67.7%), new diagnostic test 26 (15.6%), change in discharge planning 20 (12.0%), and change in level of care to the intensive care unit (ICU) 8 (4.8%). As a measure of alarm fatigue, there were 0.4 alerts per clinician shift.
CONCLUSIONS:
In a surgical general care ward, a remote surveillance software program that continually and automatically monitors physiologic data streams from the EHR and alerts multidisciplinary providers for severe derangements provided highly actionable alarms at a rate that is unlikely to cause alarm fatigue. Such programs are feasible and could be used to change the paradigm of monitoring.
KEY POINTS.
Question: Can a remote surveillance software program that monitors surgical ward patients for physiologic derangement provide actionable alerts without alarm fatigue to a multidisciplinary team?
Findings: The program generated 151 alerts, 94.1% of which were numerically accurate. Among alerts, 88.1% were clinically actionable alerts leading to a change in patient management, diagnostic work-up, discharge planning, or triage to an intensive care unit (ICU). There were 0.4 alerts per clinician shift.
Meaning: A remote surveillance software program that continually monitors surgical ward patients for physiologic derangement can provide real-time alerts to a multidisciplinary team that is clinically useful without alarm fatigue.
Care in hospital wards relies on the physical presence of clinicians to evaluate patients at the bedside while maintaining a team of anesthesiologists and/or intensivists on-site for patients who experience acute physiologic deterioration. Hospitalized surgical patients are increasingly elderly and medically comorbid, as healthier patients are receiving surgery in ambulatory settings.1–3 Nighttime coverage is often sparse with surgical teams spread across the hospital and responsible for a large volume of patients. Critical care teams are usually not involved until a patient decompensates.
Bedside monitors have been challenged by highly sensitive but nonspecific alerts, leading to low actionability and alarm fatigue among providers.4–6 Their alarms are also only detectable to staff who are within earshot. A new opportunity exists as a result of electronic health records (EHRs), which enable the continuous delivery of electronic vital signs and laboratory data to the patient’s record. Despite this opportunity, most clinicians must search for data as it does not arrive to them automatically and synchronously to when it is recorded.
In this challenging environment, failure to rescue events has increased.7–10 These trends suggest the need for reevaluation of the traditional monitoring and alerting approach.11 One such approach being tested are software programs that automatically rove the EHR and provide alerts directly to providers for out-of-threshold values of clinical parameters. Examples of this innovation have been tested in the operating room setting and, most recently, on obstetrical wards.12–15 There have been no studies to examine such a system in the postoperative inpatient ward setting.
We designed and implemented a remote surveillance software program (RSSP) with the ability to continuously survey data from the EHR to detect physiologic derangements and automatically alert a multidisciplinary team. The RSSP was implemented in a surgical inpatient general care ward where there were limited staffing resources during nighttime hours. The motivation for the study on this ward was a loss of on-site anesthesia support for emergency physiologic deteriorations at nighttime, which occurred just before the initiation of the study. The RSSP was designed to alert members of the team on the ward and a critical care team of anesthesiologists located remotely. We evaluated the feasibility of such a program to provide clinically useful data without alarm fatigue. The primary end point of the study was the true positive rate, defined as proportion of alerts that led to a change in management of the patient, and the secondary end point of the study was the overall frequency of alerts per clinician shift.
METHODS
This project was a quality improvement (QI) initiative and was therefore exempt from institutional review board approval as determined by minimal risk standards established by our institution. Patient consent was waived. The patient inclusion, exclusion, primary outcome, secondary outcomes, and statistical analysis plan were prespecified and available on reviewers’ request. The study is reported in consultation with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) recommendations.
Intervention
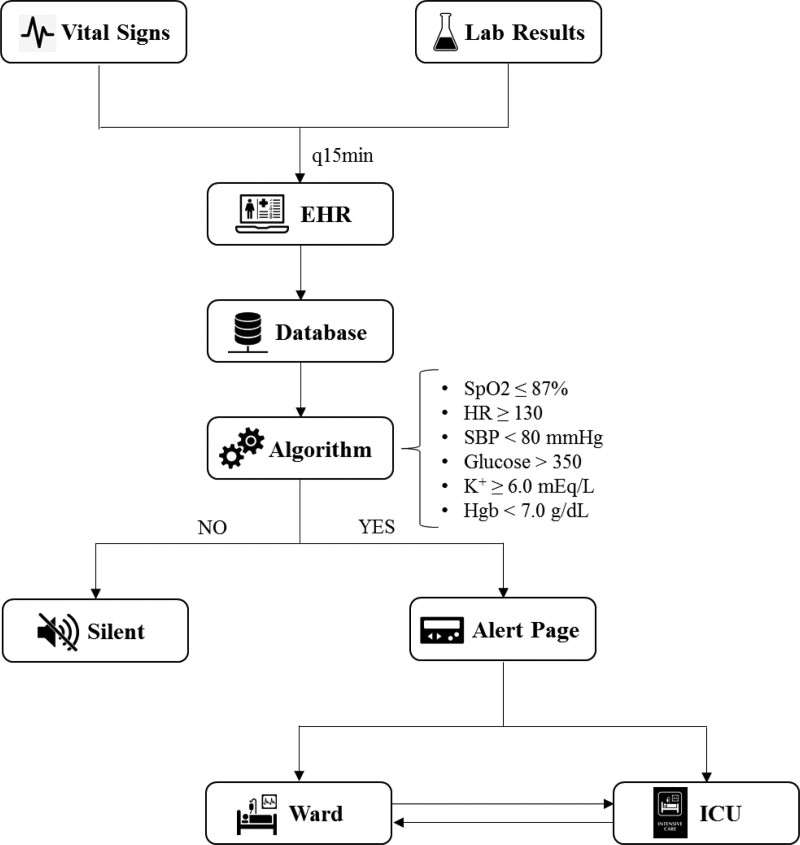
The RSSP was a software program designed by members of the study team in conjunction with members of the team from AlertWatch LLC (Ann Arbor, MI). The study team was responsible for identifying data parameters, defining alert thresholds, and determining which team members would be alerted. AlertWatch was responsible for receiving physiologic data, generating alerts, and routing them to recipients. A schema demonstrating the RSSP’s data acquisition process, alert parameters, thresholds, and alert routing is shown in Figure 1. The RSSP supplemented existing standard of care and did not replace or eliminate any existing monitoring systems, alerts, or communication protocols.
Figure 1.
Design of the remote software surveillance program. EHR indicates electronic health record; Hgb, hemoglobin; HR, heart rate; ICU, intensive care unit; SBP, systolic blood pressure; Spo2, oxygen saturation.
Study Population and Design
This was a single-center study conducted at a large academic medical center. We included patients who were admitted to the otolaryngology and ophthalmology 24-bed inpatient ward in an inpatient infirmary adjacent to our main hospital. Patients on the inpatient ward were cared for by a bedside nurse and an otolaryngology or ophthalmology resident, who was also responsible for consultations in the emergency department (ED) and throughout the hospital at nighttime. There is a physical connection between the main hospital and the infirmary but the inpatient ward being studied is approximately ¼ of a mile away from the critical care physicians who were alerted by the RSSP.
Patients admitted to the inpatient ward consisted of pre, -post-, and nonoperative patients and many patients were postoperative for head and neck tumor removal. Patients were excluded if they were <18 years old.
The intervention cohort was defined as all patients who were admitted to the inpatient ward from October 1, 2017 to March 31, 2019 during the hours from 17:00 to 07:00 7 days per week. The RSSP was intended to send an alert page to the recipients specified above for all abnormalities detected in the intervention cohort.
Outcomes
The accuracy of the alerts was defined as the proportion of alerts paged by the RSSP that were confirmed to be numerically correct. These were confirmed by chart review of vital signs and laboratory documentation and nursing notes (Supplemental Digital Content, Appendix Figure 1, http://links.lww.com/AA/D440).
The primary outcome of the study was the clinical actionability of alerts. This was defined as the true positive rate of alerts, which was the proportion of alerts that were clinically actionable. An alert was categorized as clinically actionable if it was associated with an action by the clinical team that changed the care of a patient, including a new diagnostic test or treatment, triage to a higher level of care, or change in the patient’s discharge planning. Clinical actions were identified by a member of the study team via chart review guided by the algorithm in Supplemental Digital Content, Appendix Figure 1, http://links.lww.com/AA/D440.
The secondary outcome of the study was the frequency of alerts per clinician shift. This outcome was intended to measure the possibility of alarm fatigue.
Statistical Analysis
This study is primarily focused on descriptive summaries. Analysis was conducted for demographics, covariates, and all adverse event outcomes. Numeric variables were summarized using means and standard deviations (SDs). Categorical variables were summarized using frequencies and percentages. All analyses were performed using R statistical software V 3.2.6 and Rstudio V1.0 (Rstudio Inc, Boston, MA).
RESULTS
The RSSP monitored a total of 3934 unique patients during the study period from 17:00 to 07:00. Demographic characteristics of patients during the study period are summarized in Table 1.
Table 1.
Patient Demographics and Baseline Clinical Characteristics
| Postintervention | |
|---|---|
| Variables\no. of patients | n = 3934 |
| Age | 58.8 (17.3) |
| Sex: male (%) | 1716 (43.7%) |
| BMI | 27.7 (7.5) |
| ASA physical status (%) | |
| I | 141 (12.8) |
| II | 716 (64.8) |
| III | 246 (22.3) |
| IV | 2 (0.2) |
Numeric variables including age and BMI are summarized using mean and standard deviations; categorical variables including sex and insurance. Status is summarized using frequencies and percentages.
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index.
The RSSP analyzed in total 1,560,999 vital signs and 16,635 laboratory results during the study period (1711.6 per day and 18.2 per day on average, respectively). Overall, 151 alerts were generated and paged to recipients, including 120 abnormal vital sign events and 31 abnormal laboratory events. Among the 151 alerts that were paged (2.6 alerts per week), 143 (94.7%) were numerically accurate and 8 (5.3%) were inaccurate.
Table 2 demonstrates the etiology of accurate alerts. The most common etiology was hypoxemia, which represented over half of all alerts (92; 63%). Hyperkalemia was the least common etiology (2; 1%).
Table 2.
Number and Proportion of Alerts by Parameter
| Alert parameter | n (%) |
|---|---|
| Oxygen saturation (<88%) | 92 (63) |
| Heart rate (>130 bpm) | 19 (13.3) |
| Systolic blood pressure (<80 mm Hg) | 3 (4) |
| Glucose (>350 mg/dL) | 17 (12) |
| Hemoglobin (<7 g/dL) | 10 (7) |
| Potassium (>6 mEq/L) | 2 (1) |
Abbreviation: bpm, beats per minute.
Figure 2 demonstrates the primary and secondary study outcomes related to feasibility, including the clinical actionability of alerts (true positive rate) and alarm fatigue (average number of alerts per clinician shift). Overall, the majority of alerts were true positives (133; 88.1%). The most common clinical action related to the alert was a change in management/intervention (113; 67.7%). In terms of alarm fatigue, there was an average of 0.4 alerts per clinician shift.
Figure 2.
Alert volume, frequency, accuracy, and actionability.
DISCUSSION
We evaluated a remote surveillance program that monitored patients on a surgical ward at nighttime and sent alerts for significant physiologic and laboratory derangements to a multidisciplinary team. We found that the RSSP provided alerts that were accurate at a rate of 94.7%. The majority of time the alerts were true positives (88.1% led to a change in the patient’s care). Further, there was low concern for alarm fatigue with an average of 0.4 alerts per clinician shift. Finally, the RSSP was implemented on the surgical ward for this study because at the start of the study period there was a reduction in nighttime on-site anesthesiologists to manage patients experiencing acute decompensation.
Our findings add to the literature on RSSPs documenting an increase in awareness of patient’s physiologic events. Prior studies have demonstrated that such systems can provide useful alerts in the operating room and on the labor and delivery unit for postpartum patients.12,14 Our study included patients on the surgical general ward and establishes the feasibility of such a system to provide actionable alerts that lead to changes in patient care without causing alarm fatigue.
In addition, the impact of an RSSP on the general care ward may be even greater than in the operating room setting or intensive care unit (ICU) given the smaller ratios of patients to clinicians and the lower frequency of obtainment of physiologic data. These factors increase the risk of failure to rescue events. The advantage of an RSSP is that it automatically and synchronously detects valuable clinical data values and provides immediate alerts that can be routed to any provider in any location. Such a system can overcome inefficiencies of traditional monitoring systems that require physical presence near devices connected to the patient or asynchronous pursual of the EHR by the provider.
Such systems also enable a multidisciplinary care team to receive the same information and convene around the patient when such events occur, which may lead to more efficient consultation involvement of teams with expertise in managing acute deranged physiology. In our study, a team of anesthesia intensivists was alerted in parallel with the primary team. The RSSP can lead to earlier awareness and proactive collaboration between the teams before significant deterioration. RSSPs should be explored as a method to improve the consultation mechanisms of anesthesiologists and intensivists in hospitals.
We selected the general care ward in this study to implement the RSSP due to the loss of anesthesia personnel during nighttime hours that occurred just before the study period. Hospital clinical leadership believed that the RSSP could help support the clinical staff that remained in the hospital to recognize the acute physiologic deterioration of patients at nighttime despite the loss of personnel. Their hypothesis was that the RSSP could maintain or improve safety by increasing real-time awareness and collaboration of the primary surgical team with a remote anesthesia critical care team. Our study was not powered to test this hypothesis, though it represents an important future direction. Future studies should be designed to determine whether remote surveillance technologies can maintain or even reduce adverse events, such as cardiopulmonary arrests, rapid responses, or triage to the ICU.
One important challenge in designing an RSSP that we encountered in this study was the limitation in the frequency of vital sign attainment and the timing with which they were entered at the bedside. The nurse or technician had to manually obtain and then validate them through the push of a button or by entering them in the patient’s record.14,15 Every 4 hours or even less, frequent manual obtainment and validation of vital signs are typical for general care wards at most hospitals. The benefit of the RSSP consuming these vital signs was that the data were validated before being entered in the EHR and thus detected by the RSSP. This likely led to the high accuracy of alerts that we observed, which has been a struggle for other systems that deal with more frequent and unvalidated data.
Thus, there were significant intervals where a patient may not be monitored. To address this challenge, wearable sensors that noninvasively measure vital signs and other physiologic data continuously should be considered. Others using continuous remote monitoring with novel mobile sensors have shown that they can detect pneumonia, atrial fibrillation, and other clinical conditions in general care ward patients.16,17 Such an arrangement could significantly augment the ability of RSSPs to reduce failure to rescue events, though careful attention would be needed to ensure that alarms are of manageable frequency and highly actionable.
This study has limitations. This is a single-center experience in a specialty surgical population, and as such, the results may not be generalizable to other institutions or populations. In addition, we were not able to comment on the false-negative rate of the system. For example, the RSSP obtained vital signs every 15 minutes and used the latest recorded vital sign to determine whether an alert would be sent. Thus, a vital sign out of range that occurred earlier than the last vital sign obtained by the RSSP over the 15-minute interval could have been beyond threshold. This could be considered a false negative.
In conclusion, remote surveillance software appears to improve the traditional paradigm on general care ward patient monitoring by taking advantage of electronic data streams in the EHR. Such a program can also enable proactive consultations from the anesthesia critical care team. We found that such a system is feasible to implement and can be designed in a manner that provides a manageable number of alerts that are highly actionable with substantive changes to the patient’s care pathway. These systems may play an increasingly vital role in the quality and safety fabric of surgical care in hospitals given the increasingly complex and elderly inpatient population.
ACKNOWLEDGMENTS
We thank Dr Jeffrey and Mrs Judy Buzen for their donation of funds for this research. We also thank the ICU fellows, surgeons, and general care ward nurses who participated in this quality improvement effort.
DISCLOSURES
Name: Kyan C. Safavi, MD, MBA.
Contribution: This author helped design the study, analyze, interpret, and write the manuscript.
Name: Hao Deng, PhD.
Contribution: This author helped analyze the statistics and write the manuscript.
Name: William Driscoll, MA.
Contribution: This author helped with study design and data acquisition.
Name: Milcho Nikolov, MA.
Contribution: This author helped with study design and data acquisition.
Name: Kalpan Tolia, MA.
Contribution: This author helped with study design and data acquisition.
Name: Jeanine P. Wiener-Kronish, MD.
Contribution: This author helped design the study, interpret and write the manuscript.
This manuscript was handled by: Thomas M. Hemmerling, MSc, MD, DEAA.
Supplementary Material
GLOSSARY
- ASA
- American Society of Anesthesiologists
- BMI
- body mass index
- bpm
- beats per minute
- ED
- emergency department
- EHR
- electronic health record
- Hgb
- hemoglobin
- HR
- heart rate
- ICU
- intensive care unit
- QI
- quality improvement
- RSSP
- remote surveillance software program
- SBP
- systolic blood pressure
- SD
- standard deviation
- Spo2
- oxygen saturation
- STROBE
- Strengthening the Reporting of Observational Studies in Epidemiology
Published ahead of print April 08 2021.
Reprints will not be available from the authors.
Funding: None.
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website.
REFERENCES
- 1.Hollenbeck BK, Dunn RL, Suskind AM, Strope SA, Zhang Y, Hollingsworth JM. Ambulatory surgery centers and their intended effects on outpatient surgery. Health Serv Res. 2015;50:1491–1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCrum ML, Lipsitz SR, Berry WR, Jha AK, Gawande AA. Beyond volume: does hospital complexity matter?: an analysis of inpatient surgical mortality in the United States. Med Care. 2014;52:235–242. [DOI] [PubMed] [Google Scholar]
- 3.Hollenbeck BK, Dunn RL, Suskind AM, Zhang Y, Hollingsworth JM, Birkmeyer JD. Ambulatory surgery centers and outpatient procedure use among Medicare beneficiaries. Med Care. 2014;52:926–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitka M. Joint commission warns of alarm fatigue: multitude of alarms from monitoring devices problematic. JAMA. 2013;309:2315–2316. [DOI] [PubMed] [Google Scholar]
- 5.Ruskin KJ, Hueske-Kraus D. Alarm fatigue: impacts on patient safety. Curr Opin Anaesthesiol. 2015;28:685–690. [DOI] [PubMed] [Google Scholar]
- 6.Jones K. Alarm fatigue a top patient safety hazard. CMAJ. 2014;186:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lafonte M, Cai J, Lissauer ME. Failure to rescue in the surgical patient: a review. Curr Opin Crit Care. 2019;25:706–711. [DOI] [PubMed] [Google Scholar]
- 8.Khan M, Jehan F, Zeeshan M, et al. Failure to rescue after emergency general surgery in geriatric patients: does frailty matter? J Surg Res. 2019;233:397–402. [DOI] [PubMed] [Google Scholar]
- 9.Sheetz KH, Dimick JB, Ghaferi AA. Impact of hospital characteristics on failure to rescue following major surgery. Ann Surg. 2016;263:692–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burke JR, Downey C, Almoudaris AM. Failure to rescue deteriorating patients: a systematic review of root causes and improvement strategies. J Patient Saf. Published online May 21, 2020. DOI: 10.1097/PTS.0000000000000720. [DOI] [PubMed] [Google Scholar]
- 11.Safavi KC, Driscoll W, Wiener-Kronish JP. Remote surveillance technologies: realizing the aim of right patient, right data, right time. Anesth Analg. 2019;129:726–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tremper KK, Mace JJ, Gombert JM, Tremper TT, Adams JF, Bagian JP. Design of a multifunction decision support display for anesthesia care; Alert Watch OR. BMC Anesthesiol. 2018;1:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kherterpal S, Shanks A, Tremper KK. Impact of a novel multiparameter decision support system on intraoperative processes of care and postoperative outcomes. Anesthesiology. 2018;128:272–282. [DOI] [PubMed] [Google Scholar]
- 14.Klumpner TT, Kountanis JA, Langen ES, Smith RD, Tremper KK. Use of a novel electronic maternal surveillance system to generate automated alerts on the labor and delivery unit. BMC Anesthesiol. 2018;18:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klumpner TT, Kountanis JA, Meyer SR, et al. Use of a novel electronic maternal surveillance system and the maternal early warning criteria to detect severe postpartum hemorrhage. Anesth Analg. 2020;131:857–865. [DOI] [PubMed] [Google Scholar]
- 16.Breteler MJM, KleinJan E, Numan L, et al. Are current wireless monitoring systems capable of detecting adverse events in high-risk surgical patients? A descriptive study. Injury. 2020;51(suppl 2):S97–S105. [DOI] [PubMed] [Google Scholar]
- 17.Breteler MJM, KleinJan EJ, Dohmen DAJ, et al. Vital signs monitoring with wearable sensors in high-risk surgical patients: a clinical validation study. Anesthesiology. 2020;132:424–439. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.