Abstract
Purpose
To identify disparities in the use of telemedicine during the coronavirus disease 2019 (COVID-19) pandemic.
Design
A cross-sectional study of completed clinical encounters in an academic ophthalmology center from March 2020 through August 2020.
Participants
A total of 5023 patients comprising 8116 ophthalmic clinical encounters.
Methods
Medical charts were abstracted for demographic information. We identified zip code-level socioeconomic characteristics, which were drawn from the 2019 American Community Survey 5-year estimates.
Main Outcome Measures
The completion of a synchronous video encounter, the completion of a telephone (audio-only) encounter in the absence of any video encounters, or the completion of in-person encounters only.
Results
During the study period, 8116 total clinical encounters were completed for 5023 unique patients. Of these patients, 446 (8.9%) participated in a video encounter, 642 (12.8%) completed a telephone encounter, and 3935 (78.3%) attended clinical appointments in person only. In adjusted analysis, patients who were Black (odds ratio [OR], 0.65; 95% confidence interval [CI], 0.52–0.80; P < 0.001) or Hispanic/Latino (OR, 0.65; 95% CI, 0.49–0.85; P = 0.002) were significantly less likely to complete a video or telephone appointment. Older patients (OR, 0.99; 95% CI, 0.98–0.99; P < 0.001), patients whose primary language was not English (OR, 0.49; 95% CI, 0.28–0.82; P = 0.01), Black patients (OR, 0.45; 95% CI, 0.32–0.62; P < 0.001), and Hispanic/Latino patients (OR, 0.56; 95% CI, 0.37–0.83; P = 0.005) were significantly less likely to complete a video encounter. Finally, among patients completing any type of telemedicine encounter, older age, (OR, 1.02; 95% CI, 1.01–1.03; P < 0.001), Medicare insurance (OR, 1.55; 95% CI, 1.11–2.17; P = 0.01), and Black race (OR, 1.97; 95% CI, 1.33–2.94; P < 0.001) were associated with using only phone visits.
Conclusions
Ethnic/racial minorities, older patients, and non–English-speaking individuals were significantly less likely to complete a video telehealth encounter. With the expansion of telemedicine and the need to reduce the disparate impact of COVID-19 on minorities, it will be increasingly important to identify barriers to telehealth use and opportunities to improve access.
Keywords: COVID-19, Disparities, Telehealth, Teleophthalmology, Video visits
The coronavirus disease 2019 (COVID-19) pandemic significantly disrupted the provision of ophthalmic care in the United States. Reports during the height of the pandemic found that ophthalmology practices suffered the greatest decline in patient visits among all medical specialties.1 Although ophthalmic care long has been considered to be unconducive to virtual encounters because of the importance of the physical examination and imaging, statewide stay-at-home orders and the expansion of reimbursement for telemedicine-based services catalyzed the incorporation of telemedicine into many ophthalmology practices.2 , 3 In a study of a large commercial insurance plan in Michigan, telehealth visits comprised 17% of total ophthalmic visits among patients during 1 week in April 2020, and by September 2020, 37% of ophthalmologists in the study had used telehealth at least once.4
As in ophthalmology, telemedicine is growing rapidly as a valid care delivery method across all medical fields. However, research during the COVID-19 pandemic has identified lower rates of telehealth use among vulnerable patient populations in other medical specialties.5, 6, 7, 8, 9 These differences in use mirror disparities in access to technology required for virtual visits, including laptop ownership and broadband internet subscription.10, 11, 12 One recent study of a single institution identified demographic differences in the rates of in-person visits for eye care during the pandemic13; however, there remains a paucity of literature about disparities in the uptake of telemedicine in ophthalmology, a field in which demographic differences in care use have been identified even before the COVID-19 pandemic.14
As telehealth use in routine medical care continues to grow and COVID-19 continues to impact minority patients disproportionately, it is imperative to identify potential disparities in access to and use of virtual mediums in ophthalmic care. Therefore, the purpose our study was to examine the association between sociodemographic factors and the use of telemedicine in a large, single-institution ophthalmology center during the peak of the COVID-19 pandemic.
Methods
This was a single-institution retrospective cohort study of patients who received outpatient ophthalmic care at the Yale New Haven Hospital health system, a large urban tertiary care center. The Yale University Institutional Review Board approved this study prospectively and waived informed patient consent requirements. This study was conducted in accordance with the tenets of the Declaration of Helsinki.
Population
We queried the Yale New Haven Hospital health system’s electronic health records to identify all encounters with an ophthalmology provider from March 1, 2020, through August 31, 2020. This 6-month duration represented the beginning of the first COVID-19 pandemic disease surge in the United States, during which ophthalmologists most frequently transitioned to telemedicine-based care.2, 3, 4 We included patients who had completed an appointment and excluded those who had cancelled or were unable to make their appointments as well as those younger than 18 years. We also excluded patient encounters in which the primary provider was an optometrist to focus on the use of telehealth for ophthalmic care.
Measures
To identify differential rates of telemedicine use in this study’s cohort, we abstracted the following sociodemographic factors from chart review: patient age, ethnicity or race, sex, primary language spoken, and primary payer status. Ethnicity or race was patient reported and categorized into mutually exclusive groups as Hispanic or Latino, non-Hispanic Black, non-Hispanic White, Asian, and other. Primary language also was patient reported and divided into English and non-English. We categorized primary payer status into 4 main groups: privately insured, insured by Medicare, insured by Medicaid, and uninsured. The private insurance category included commercial health plans and workers' compensation.
Previous research has demonstrated an association between the uptake of telemedicine and socioeconomic factors.5 , 6 These factors are not gathered in the duration of a typical medical appointment and were not included in Yale New Haven Hospital’s electronic health records. Therefore, we assigned zip code tabulation areas (ZCTA) to each patient based on their home address and used these ZCTAs to obtain information about median household income and educational attainment from the 2019 American Community Survey.15 Each of these factors reflects information about all households in the ZCTA and therefore are only surrogate markers of a patient’s true socioeconomic status (SES). We divided these 2 factors into quartiles to facilitate analysis.
Recent research has shown differential rates of telemedicine use among ophthalmic subspecialties.4 To control for confounding because of differences in patient demographics between subspecialties, we categorized each patient encounter into mutually exclusive ophthalmic subspecialties via chart abstraction of each encounter’s provider subspecialty. These provider categories were comprehensive ophthalmology, cornea, glaucoma, neuro-ophthalmology, oculofacial plastics and orbital conditions, pediatric ophthalmology, retinal and vitreous conditions, and uveitis and ocular inflammation. For patients completing multiple clinical visits with different subspecialty providers, we classified the patient-level provider specialty, during regression analysis, based on the most commonly seen provider.
Outcome Measure
Our primary outcome measure was the encounter type of each patient visit. We categorized encounter types into 3 main groups: (1) video, (2) telephone, and (3) in person. We defined video as the synchronous use of video and audio input and output in a virtual setting, whereas telephone encounters were audio only. Similar to previous studies on telehealth use, we used patient-level data.5 Therefore, for patients with multiple encounters during the study period, we categorized them as having used video if they completed any video-based visit during the study period. If patients had completed no video visits, but had a telephone-based encounter, they were categorized as having used a telephone encounter. Finally, patients who had not engaged in either telemedicine or telephone-based visits were considered to have used in-person visits only. We included only those encounters with an associated signed note from an attending ophthalmologist.
Institutional Telehealth Policies
Our academic center did not use on-site telemedicine for patient encounters. Therefore, all patients who completed a video or telephone encounter did so outside of the clinical setting and used their own laptop or mobile devices. Video encounters were conducted using smartphones, laptops, or tablets through web-based videoconferencing software. If patients were unable to access the technological requirements for a video encounter or expressed a strong preference not to use video, a phone visit was conducted. For phone visits, no specialized equipment was used for phone encounters, and ophthalmologists or clinical technicians dialed patient’s preferred phone numbers on their chart to initiate a phone visit.
Institutionally, ophthalmologists, clinical receptionists, and clinical schedulers were informed to encourage the use of synchronous video as the preferred virtual method during appointments, scheduling, and the check-in and check-out process. Appointments were scheduled either in person by a clinical receptionist after in-person clinical encounters or via phone with staff members who regularly assist callers with ambulatory appointment scheduling, referral management, and care coordination. The decision to use either in-person or telehealth for a visit was determined by providers based on clinical need for an in-person encounter as well as a patient’s ability to access and use telehealth.
Statistical Analysis
We reported mean and standard deviation for continuous variables and proportion for categorical variables unless otherwise specified. To characterize fully the association between patient sociodemographic factors and use of telehealth, we conducted 3 separate analyses. First, we compared patients who completed video or telephone visits with those who completed in-person visits only to identify disparities in the use of any kind of telehealth. Second, we compared patients using video telehealth versus those who used telephone or in-person visits only to identify patient populations that were unable to participate in care because of the greater technological requirements of synchronous video calls. Finally, to determine if specific patient characteristics were associated with telephone use among those completing any type of telehealth encounter, we created a subcohort of patients who had completed a virtual appointment at least once during the study period and compared patients who completed phone versus video visits. We used univariate and multivariate logistic regression models for all analyses. Additionally, all analyses included the subspecialty of encounters as a controlling covariate to account for differential rates of telehealth use among different ophthalmic subspecialties. Because the purpose of this study was to identify potential risk factors associated with low telehealth use, rather than to develop predictive algorithms of uptake, we separately highlighted the results of our univariate analysis and did not perform a Bonferroni correction on univariate regressions. In multivariate regressions, we included all covariates and performed Bonferroni correction with a significance level set at P < 0.0125 (0.05/3), accounting for 3 separate multivariate comparisons. To examine if the association between patient characteristics and telemedicine use varied by the type of ophthalmology subspecialist seen, we assessed an interaction term between the patient-level ophthalmology subspecialty and each other demographic or SES covariate in multivariate regression for all 3 analyses. All statistical analyses were conducted in R software version 3.6.0 (R Foundation for Statistical Computing). We used GraphPad Prism 8 software (GraphPad Software) for graphical depictions.
Results
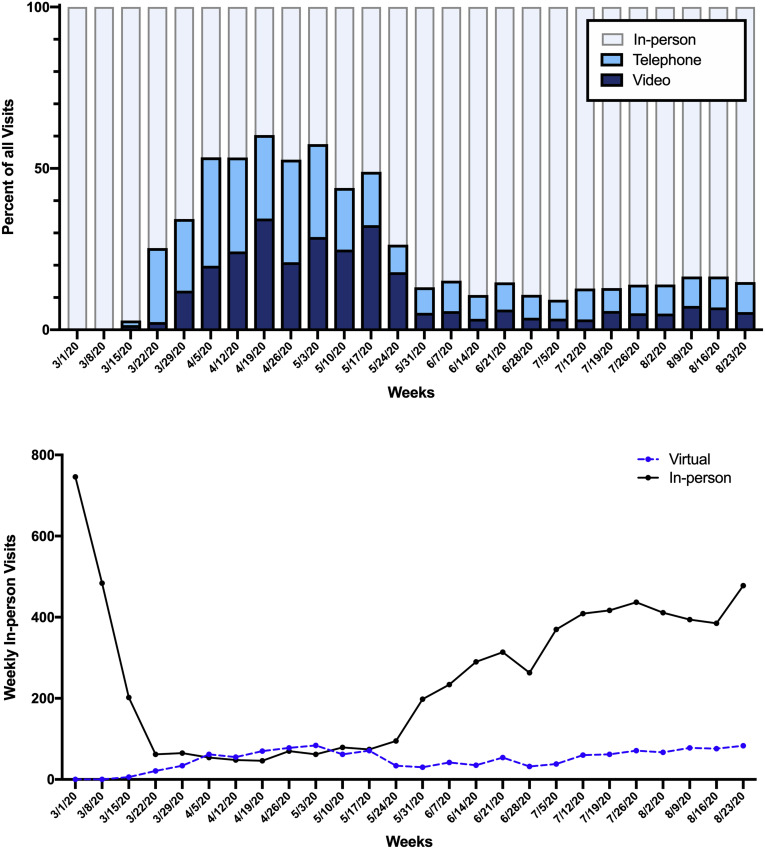
From March 1 through August 31, 2020, 8116 completed patient encounters occurred, of which 572 (7.0%), 757 (9.3%), and 6787 (83.6%) were telemedicine, telephone, and in-person visits, respectively. Table 1 summarizes characteristics of this study’s cohort on the patient level. A total of 5023 unique patients comprised all encounters in this period, of which 1497 patients (29.8%) underwent more than 1 encounter. Of this cohort, the median age among all patients was 64 years (range, 19–103 years) and 2821 patients (56.2%) were women. By race and ethnicity, 2828 patients (56.3%) were non-Hispanic White, 753 patients (15.0%) were Hispanic or Latino, 1025 patients (20.4%) were non-Hispanic Black, and 417 patients (8.4%) were categorized as other. Most patients self-reported English (90.2%) as their primary language. By encounter type, 446 patients (8.9%) completed at least 1 telemedicine appointment, 642 patients (12.8%) completed at least 1 telephone appointment, and the remaining 3935 patients (78.3%) completed in-person visits only. Patients seeing oculoplastic (46.7%) and comprehensive (36.3%) ophthalmologists showed the greatest percentage of telehealth use (at least 1 telephone or video visit), whereas patients seen by glaucoma (9.4%) and pediatric (7.5%) specialists had the least (Table 1). The number of video or telephone visits as a proportion of all clinical encounters rapidly increased in March 2020, with a peak in use from April 19, 2020 through April 25, 2020, during which telemedicine-based visits constituted more than 60% of all encounters (Fig 1 ). After the initial surge in use, telemedicine encounters accounted for an average of 13.8% of visits from June 1, 2020, through August 31, 2020.
Table 1.
Baseline Study Group Characteristics by Visit Type Classification
| Characteristic | All Patients | Visit Type∗ |
||
|---|---|---|---|---|
| Video | Telephone | In Person | ||
| Total no. (% of entire study cohort) | 5023 | 446 (8.9) | 642 (12.8) | 3935 (78.3) |
| Age (yrs) | 64 (19–103) | 63 (19–93) | 67 (19–96) | 63 (19–103) |
| Gender | ||||
| Female | 2821 (56.2) | 256 (57.4) | 365 (56.9) | 2200 (56.2) |
| Male | 2202 (43.8) | 190 (42.6) | 277 (43.1) | 1735 (43.8) |
| Ethnicity or race† | ||||
| Non-Hispanic White | 2828 (56.3) | 316 (70.9) | 403 (62.8) | 2109 (53.6) |
| Black | 1025 (20.4) | 54 (12.1) | 126 (19.6) | 845 (21.5) |
| Hispanic or Latino | 753 (15.0) | 37 (8.3) | 78 (12.1) | 638 (16.2) |
| Other | 417 (8.4) | 39 (8.7) | 35 (5.5) | 343 (8.7) |
| Insurance status | ||||
| Private | 1459 (29.0) | 168 (37.7) | 138 (21.5) | 1153 (29.3) |
| Medicare | 2540 (50.6) | 201 (45.1) | 389 (60.6) | 1950 (49.6) |
| Medicaid | 929 (18.5) | 69 (15.5) | 109 (17.0) | 751 (19.1) |
| Uninsured | 95 (1.9) | 8 (1.8) | 6 (0.9) | 81 (2.1) |
| Primary language | ||||
| English | 4533 (90.2) | 429 (96.2) | 593 (92.4) | 3511 (89.2) |
| Other | 490 (9.8) | 17 (3.8) | 49 (7.6) | 424 (10.8) |
| Household median income quartile‡ | ||||
| Lowest | 826 (16.4) | 57 (12.8) | 109 (17.0) | 660 (16.8) |
| Second | 697 (13.9) | 54 (12.1) | 97 (15.1) | 546 (13.9) |
| Third | 831 (16.5) | 73 (16.4) | 97 (15.1) | 661 (16.8) |
| Highest | 2666 (53.1) | 262 (58.7) | 339 (52.8) | 2065 (52.5) |
| Educational attainment quartile‡ | ||||
| Lowest | 801 (15.9) | 53 (11.9) | 99 (15.4) | 649 (16.5) |
| Second | 1167 (23.2) | 80 (17.9) | 152 (23.7) | 935 (23.8) |
| Third | 1514 (30.1) | 135 (30.3) | 189 (29.4) | 1190 (30.2) |
| Highest | 1540 (30.7) | 178 (39.9) | 202 (31.5) | 1160 (29.5) |
| Subspecialty§ | ||||
| Comprehensive | 799 (15.9) | 115 (14.4) | 175 (21.9) | 509 (63.7) |
| Cornea | 658 (13.1) | 53 (8.1) | 92 (14.0) | 513 (78.0) |
| Glaucoma | 1015 (20.2) | 27 (2.7) | 68 (6.7) | 920 (90.6) |
| Neuro-ophthalmology | 561 (11.2) | 23 (4.1) | 78 (13.9) | 460 (82.0) |
| Oculofacial plastics and orbital | 413 (8.2) | 119 (28.8) | 74 (17.9) | 220 (53.3) |
| Pediatric ophthalmology | 40 (0.8) | 0 (0.0) | 3 (7.5) | 37 (92.5) |
| Retinal and vitreous | 953 (19.0) | 62 (6.5) | 103 (10.8) | 788 (82.7) |
| Uveitis and ocular inflammation | 584 (11.6) | 47 (8.0) | 49 (8.4) | 488 (83.6) |
Data are presented as median (range) or no. (%).
Patients completing at least 1 video encounter were categorized as “video,” patients completing no video encounters but at least 1 telephone encounter were categorized as “telephone,” and patients completing only in-person encounters were categorized as “in person.”
“Other” includes patients of Asian, American Indian, Alaskan Native, or Pacific Islander descent as well as those who did not provide their ethnicity or race.
Socioeconomic characteristics were derived from patients’ zip code tabulation areas (ZCTAs) matched with the 2019 American Community Survey. Educational attainment was defined as the proportion of adults in the ZCTA who had completed high school.
For patients completing multiple clinical visits with different provider subspecialties during the study period, we classified the patient-level provider specialty based on the most commonly seen provider.
Figure 1.
A, Bar graph showing encounter types as a proportion of total visits from March 1, 2020, through August 31, 2020. B, Line graph showing total virtual (telephone or audio telehealth) as well as in-person encounters from March 1, 2020, through August 31, 2020.
Factors Associated with Video or Telephone Use for an Ophthalmic Clinical Visit
Univariate Analysis
In univariate analysis (Table 2 ), several demographic factors were associated significantly with telemedicine use, defined as encounters with video- or audio-only input. Black patients (odds ratio [OR], 0.66; 95% confidence interval [CI], 0.55–0.80; P < 0.001) or Hispanic or Latino patients (OR, 0.55; 95% CI, 0.44–0.69; P < 0.001) were significantly less likely to use telemedicine compared with non-Hispanic White patients (Table 2). Patients with a primary language other than English were less likely to complete a video or telephone encounter (OR, 0.56; 95% CI, 0.42–0.74; P < 0.001), and patients covered by Medicare were significantly more likely to use telehealth compared with patients with private insurance (OR, 1.23; 95% CI, 1.05–1.45; P = 0.01). Older age was also associated with any telehealth use (OR, 1.01; 95% CI, 1.00–1.01; P = 0.005). Household income was not associated with telehealth use, but patients residing in a neighborhood with the highest quartile of educational attainment were more likely to use telehealth compared with patients in the lowest (OR, 1.40; 95% CI, 1.13–1.75; P = 0.003). By ophthalmic subspecialty, patients seen by oculoplastic ophthalmologists were significantly more likely to have used any form of telemedicine compared with patients seeking comprehensive ophthalmology care (OR, 1.54; 95% CI, 1.21–1.96; P < 0.001). Patients seeing all other subspecialist types were significantly less likely to use telehealth.
Table 2.
Factors Associated with the Use of Telemedicine, Defined as at Least 1 Video or Telephone Ophthalmic Clinical Encounter
| Factor | Univariate Analysis |
Multivariate Analysis |
||
|---|---|---|---|---|
| Odds Ratio (95% Confidence Interval)∗ | P Value | Odds Ratio (95% Confidence Interval)∗ | P Value† | |
| Age | 1.01 (1.00–1.01) | 0.005 | 1.00 (0.99–1.01) | 0.88 |
| Gender | ||||
| Female | 1.00 | 1.00 | ||
| Male | 0.97 (0.84–1.11) | 0.63 | 0.96 (0.83–1.11) | 0.61 |
| Ethnicity or race∗ | ||||
| Non-Hispanic White | 1.00 | 1.00 | ||
| Black | 0.66 (0.55–0.80) | <0.001 | 0.65 (0.52–0.80) | <0.001 |
| Hispanic or Latino | 0.55 (0.44–0.69) | <0.001 | 0.65 (0.49–0.85) | 0.002 |
| Other | 0.70 (0.53–0.92) | 0.013 | 0.75 (0.56–0.99) | 0.05 |
| Insurance status | ||||
| Private | 1.00 | 1.00 | ||
| Medicare | 1.23 (1.05–1.45) | 0.01 | 1.27 (1.04–1.54) | 0.017 |
| Medicaid | 0.90 (0.73–1.11) | 0.34 | 1.10 (0.87–1.37) | 0.43 |
| Uninsured | 0.63 (0.33–1.11) | 0.13 | 0.83 (0.43–1.51) | 0.56 |
| Primary language | ||||
| English | 1.00 | 1.00 | ||
| Other | 0.56 (0.42–0.74) | <0.001 | 0.71 (0.50–0.98) | 0.04 |
| Household median income quartile | ||||
| Lowest | 1.00 | 1.00 | ||
| Second | 1.12 (0.87–1.45) | 0.39 | 1.06 (0.80–1.40) | 0.68 |
| Third | 0.98 (0.77–1.26) | 0.90 | 0.82 (0.62–1.08) | 0.16 |
| Highest | 1.15 (0.95–1.41) | 0.16 | 0.69 (0.50–0.95) | 0.02 |
| Educational attainment quartile | ||||
| Lowest | 1.00 | 1.00 | ||
| Second | 1.05 (0.83–1.33) | 0.69 | 1.02 (0.78–1.33) | 0.90 |
| Third | 1.15 (0.92–1.44) | 0.21 | 1.21 (0.88–1.65) | 0.24 |
| Highest | 1.40 (1.13–1.75) | 0.003 | 1.46 (1.03–2.09) | 0.03 |
| Subspecialty‡ | ||||
| Comprehensive | 1.00 | 1.00 | ||
| Cornea | 0.50 (0.39–0.63) | <0.001 | 0.49 (0.38–0.61) | <0.001 |
| Glaucoma | 0.18 (0.14–0.23) | <0.001 | 0.18 (0.14–0.24) | <0.001 |
| Neuro-ophthalmology | 0.39 (0.30–0.50) | <0.001 | 0.40 (0.31–0.53) | <0.001 |
| Oculofacial plastics and orbital | 1.54 (1.21–1.96) | <0.001 | 1.63 (1.27–2.08) | <0.001 |
| Pediatric ophthalmology | 0.14 (0.03–0.40) | 0.001 | 0.15 (0.04–0.43) | 0.002 |
| Retinal and vitreous | 0.37 (0.29–0.46) | <0.001 | 0.38 (0.30–0.48) | <0.001 |
| Uveitis and ocular inflammation | 0.35 (0.26–0.45) | <0.001 | 0.37 (0.29–0.49) | <0.001 |
All univariate and multivariate analyses included ophthalmic subspecialty as a controlling covariate.
The threshold of significance in this study was Bonferroni corrected to P < 0.013 (0.05/4) to account for multiple analyses.
For patients completing multiple clinical visits with different provider subspecialties during the study period, we classified the patient-level provider specialty based on the most commonly seen provider.
Multivariate Analysis
In multivariate analysis, Black patients (OR, 0.65; 95% CI, 0.52–0.80; P < 0.001) or Hispanic or Latino patients (OR, 0.65; 95% CI, 0.49–0.85; P = 0.002) were significantly less likely to use telemedicine compared with non-Hispanic White patients. Additionally, patients seen by oculoplastic specialists were significantly more likely to use telehealth compared with those seen by comprehensive ophthalmologists (OR, 1.63; 95% CI, 1.27–2.08; P < 0.001), whereas all other subspecialties remained less likely to have completed a telephone or video encounter. However, older age, having English as a primary language, and higher educational attainment were factors that did not remain associated significantly with teleophthalmology use. We also examined if the association between patient factors and telemedicine use varied by the type of ophthalmic subspecialist. However, the coefficients of all interaction terms were not significant.
Factors Associated with the Use of Video for an Ophthalmic Clinical Visit
Univariate Analysis
Black patients (OR, 0.44; 95% CI, 0.32–0.58; P < 0.001), Hispanic or Latino patients (OR, 0.44; 95% CI, 0.31–0.61; P < 0.001), and those whose primary language was not English (OR, 0.34; 95% CI, 0.21–0.54; P < 0.001) showed significantly lower use of telemedicine (Table 3 ). Older patients (OR, 0.99; 95% CI, 0.99–1.00; P = 0.004) as well as those with Medicare coverage (OR, 0.70; 95% CI, 0.56–0.87; P = 0.001) or Medicaid coverage (OR, 0.63; 95% CI, 0.47–0.83; P = 0.001) showed lower rates of video-based telehealth uptake. Among SES factors, residence in neighborhoods in the highest household income (OR, 1.66; 95% CI, 1.24–2.26; P < 0.001) or educational attainment quartile (OR, 2.00; 95% CI, 1.47–2.77; P < 0.001) were associated significantly with video use. Patients completing visits with oculoplastic subspecialists showed significantly higher odds of completing a video encounter compared with those completing visits with comprehensive ophthalmologists (OR, 2.77; 95% CI, 2.09–3.69; P < 0.001).
Table 3.
Factors Associated with the Use of Video Telemedicine for an Ophthalmic Clinical Encounter
| Factor | Univariate Analysis |
Multivariate Analysis |
||
|---|---|---|---|---|
| Odds Ratio (95% Confidence Interval)∗ | P Value | Odds Ratio (95% Confidence Interval)∗ | P Value† | |
| Age | 0.99 (0.99–1.00) | 0.004 | 0.99 (0.98–0.99) | <0.001 |
| Gender | ||||
| Female | 1.00 | 1.00 | ||
| Male | 1.01 (0.83–1.22) | 0.93 | 0.98 (0.80–1.19) | 0.81 |
| Ethnicity/race∗ | ||||
| Non-Hispanic White | 1.00 | 1.00 | ||
| Black | 0.44 (0.32–0.58) | <0.001 | 0.45 (0.32–0.62) | <0.001 |
| Hispanic or Latino | 0.44 (0.31–0.61) | <0.001 | 0.56 (0.37–0.83) | 0.005 |
| Other | 0.91 (0.63–1.27) | 0.58 | 0.89 (0.61–1.27) | 0.53 |
| Insurance status | ||||
| Private | 1.00 | 1.00 | ||
| Medicare | 0.70 (0.56–0.87) | 0.001 | 0.95 (0.73–1.24) | 0.71 |
| Medicaid | 0.63 (0.47–0.83) | 0.001 | 0.86 (0.63–1.17) | 0.34 |
| Uninsured | 0.58 (0.25–1.18) | 0.16 | 0.86 (0.36–1.81) | 0.70 |
| Primary language | ||||
| English | 1.00 | 1.00 | ||
| Other | 0.34 (0.21–0.54) | <0.001 | 0.49 (0.28–0.82) | 0.01 |
| Household median income quartile | ||||
| Lowest | 1.00 | 1.00 | ||
| Second | 1.18 (0.80–1.73) | 0.41 | 1.01 (0.67–1.53) | 0.97 |
| Third | 1.27 (0.89–1.84) | 0.19 | 0.90 (0.60–1.36) | 0.63 |
| Highest | 1.66 (1.24–2.26) | <0.001 | 0.72 (0.45–1.15) | 0.17 |
| Educational attainment quartile | ||||
| Lowest | 1.00 | 1.00 | ||
| Second | 1.04 (0.73–1.49) | 0.83 | 0.88 (0.59–1.32) | 0.54 |
| Third | 1.46 (1.06–2.03) | 0.02 | 1.29 (0.82–2.03) | 0.27 |
| Highest | 2.00 (1.47–2.77) | <0.001 | 1.69 (1.03–2.80) | 0.04 |
| Subspecialty‡ | ||||
| Comprehensive | 1.00 | 1.00 | ||
| Cornea | 0.59 (0.43–0.82) | 0.002 | 0.56 (0.40–0.77) | <0.001 |
| Glaucoma | 0.19 (0.13–0.28) | <0.001 | 0.20 (0.13–0.30) | <0.001 |
| Neuro-ophthalmology | 0.26 (0.16–0.39) | <0.001 | 0.20 (0.12–0.31) | <0.001 |
| Oculofacial plastics and orbital | 2.77 (2.09–3.69) | <0.001 | 2.57 (1.92–3.45) | <0.001 |
| Pediatric ophthalmology | 0.30 (0.05–1.00) | 0.10 | 0.24 (0.04–0.80) | 0.05 |
| Retinal and vitreous | 0.44 (0.32–0.60) | <0.001 | 0.43 (0.31–0.58) | <0.001 |
| Uveitis and ocular inflammation | 0.61 (0.43–0.85) | 0.004 | 0.62 (0.43–0.87) | 0.006 |
All univariate and multivariate analyses included ophthalmic subspecialty as a controlling covariate.
The threshold of significance in this study was Bonferroni corrected to P < 0.013 (0.05/4) to account for multiple analyses.
For patients completing multiple clinical visits with different provider subspecialties during the study period, we classified the patient-level provider specialty based on the most commonly seen provider.
Multivariate Analysis
Black patients (OR, 0.45; 95% CI, 0.32–0.62; P < 0.001) or Hispanic or Latino patients (OR, 0.56; 95% CI, 0.37–0.83; P = 0.005) remained associated significantly with lower video use. Older patients (OR, 0.99; 95% CI, 0.98–0.99; P < 0.001) and patients whose primary language was not English (OR, 0.49; 95% CI, 0.28–0.82; P = 0.01) also showed lower rates of video-based telehealth uptake in multivariate analysis. Insurance status, household income, and educational attainment were no longer associated significantly with video use after controlling for all patient characteristics. Compared with patients seen by comprehensive ophthalmologists, patients seen by oculoplastic subspecialists (OR, 2.57; 95% CI, 1.92–3.45; P < 0.001) were significantly more likely to have used a video encounter, whereas those seen by cornea (OR, 0.56; 95% CI, 0.40–0.77; P < 0.001), glaucoma (OR, 0.20; 95% CI, 0.13–0.30; P < 0.001), neuro-ophthalmology (OR, 0.20; 95% CI, 0.12–0.31; P < 0.001), retina (OR, 0.43; 95% CI, 0.31–0.58; P < 0.001), and uveitis (OR, 0.62; 95% CI, 0.43–0.87; P = 0.006) specialists were significantly less likely. No significant interaction terms were found between patient characteristics and ophthalmic subspecialty in assessing use of synchronous video encounters.
Factors Associated with the Use of Telephone among Patients Completing Any Telehealth Visit
Univariate Analysis
When examining factors associated specifically with use of a phone visit among patients completing any type of telehealth visit, older patients (OR, 1.02; 95% CI, 1.01–1.03; P < 0.001), those with Medicare (OR, 2.28; 95% CI, 1.72–3.02; P < 0.001) and Medicaid (OR, 1.97; 95% CI, 1.36–2.86; P < 0.001) insurance, patients with a primary language other than English (OR, 2.30; 95% CI, 1.34–4.10; P = 0.003), and those seeing neuro-ophthalmologists (OR, 2.42; 95% CI, 1.48–4.09; P < 0.001) were significantly more likely to have a phone encounter (Table 4 ). Black patients (OR, 0.50; 95% CI, 0.35–0.71; P < 0.001) or Hispanic or Latino patients (OR, 0.65; 95% CI, 0.43–0.98; P = 0.04) patients were significantly less likely to have completed only telephone encounters in the study period. Patients residing in the neighborhoods in the highest quartile of household median income (OR, 0.66; 95% CI, 0.46–0.94; P = 0.02) and educational attainment (OR, 0.62; 95% CI, 0.42–0.91; P = 0.02) were significantly less likely to complete only phone encounters. By ophthalmic subspecialty type, patients visiting oculoplastic specialists also showed significantly lower odds of using phone encounters (OR, 0.35; 95% CI, 0.24–0.50; P < 0.001).
Table 4.
Factors Associated with the Use of Phone Encounter among Patients Completing Any Virtual Visit Type (Phone or Video)
| Factor | Univariate Analysis |
Multivariate Analysis |
||
|---|---|---|---|---|
| Odds Ratio (95% Confidence Interval)∗ | P Value | Odds Ratio (95% Confidence Interval)∗ | P Value† | |
| Age | 1.02 (1.01–1.03) | <0.001 | 1.02 (1.01–1.03) | <0.001 |
| Gender | ||||
| Female | 1.00 | 1.00 | ||
| Male | 0.93 (0.73–1.18) | 0.55 | 0.97 (0.76–1.25) | 0.86 |
| Ethnicity/race∗ | ||||
| Non-Hispanic White | 1.00 | 1.00 | ||
| Black | 0.50 (0.35–0.71) | <0.001 | 1.97 (1.33–2.94) | <0.001 |
| Hispanic or Latino | 0.65 (0.43–0.98) | 0.04 | 1.32 (0.78–2.25) | 0.34 |
| Other | 1.53 (0.95–2.47) | 0.08 | 0.76 (0.46–1.25) | 0.25 |
| Insurance status | ||||
| Private | 1.00 | 1.00 | ||
| Medicare | 2.28 (1.72–3.02) | <0.001 | 1.55 (1.11–2.17) | 0.01 |
| Medicaid | 1.97 (1.36–2.86) | <0.001 | 1.64 (1.11–2.44) | 0.02 |
| Uninsured | 1.09 (0.34–3.37) | 0.88 | 0.51 (0.14–1.66) | 0.43 |
| Primary language | ||||
| English | 1.00 | 1.00 | ||
| Other | 2.30 (1.34–4.10) | 0.003 | 2.36 (1.19–4.87) | 0.02 |
| Household median income quartile | ||||
| Lowest | 1.00 | 1.00 | ||
| Second | 0.89 (0.56–1.41) | 0.61 | 0.94 (0.56–1.58) | 0.87 |
| Third | 0.74 (0.47–1.15) | 0.18 | 0.91 (0.55–1.51) | 0.68 |
| Highest | 0.66 (0.46–0.94) | 0.02 | 1.07 (0.60–1.90) | 0.85 |
| Educational attainment quartile | ||||
| Lowest | 1.00 | 1.00 | ||
| Second | 1.03 (0.67–1.58) | 0.90 | 1.16 (0.70–1.91) | 0.47 |
| Third | 0.79 (0.53–1.17) | 0.24 | 1.04 (0.59–1.83) | 0.87 |
| Highest | 0.62 (0.42–0.91) | 0.02 | 0.82 (0.43–1.53) | 0.59 |
| Subspecialty‡ | ||||
| Comprehensive | 1.00 | 1.00 | ||
| Cornea | 1.06 (0.71–1.57) | 0.79 | 1.17 (0.78–1.77) | 0.45 |
| Glaucoma | 1.46 (0.92–2.37) | 0.11 | 1.45 (0.89–2.39) | 0.14 |
| Neuro-ophthalmology | 2.42 (1.48–4.09) | <0.001 | 3.47 (2.04–6.07) | <0.001 |
| Oculofacial plastics and orbital | 0.35 (0.24–0.50) | <0.001 | 0.39 (0.26–0.57) | <0.001 |
| Pediatric ophthalmology | 0.99 (0.16–7.61) | 0.99 | 1.23 (0.19–10.00) | 0.83 |
| Retinal and vitreous | 1.09 (0.75–1.60) | 0.66 | 1.18 (0.79–1.77) | 0.41 |
| Uveitis and ocular inflammation | 0.68 (0.44–1.06) | 0.09 | 0.76 (0.48–1.20) | 0.24 |
All univariate and multivariate analyses included ophthalmic subspecialty as a controlling covariate.
The threshold of significance in this study was Bonferroni corrected to P < 0.013 (0.05/4) to account for multiple analyses.
For patients completing multiple clinical visits with different provider subspecialties during the study period, we classified the patient-level provider specialty based on the most commonly seen provider.
Multivariate Analysis
In multivariate analysis controlling for all patient factors, older age (OR, 1.02; 95% CI, 1.01–1.03; P < 0.001), Black race (OR, 1.97; 95% CI, 1.33–2.94; P < 0.001), and having Medicare insurance (OR, 1.55; 95% CI, 1.11–2.17; P = 0.01) were associated significantly with using only phone encounters. Of note, the association between Black race is the inverse of the relationship observed in univariate analysis (in univariate analysis, Black race was associated with a higher likelihood of video use). Additionally, non-English language and SES factors were no longer associated with completing only phone clinical encounters. Neuro-ophthalmology encounters remained significantly associated with phone use (OR, 3.47; 95% CI, 2.04–6.07; P < 0.001), whereas oculoplastic encounters were associated with a lower likelihood of phone use (OR, 0.39; 95% CI, 0.26–0.57; P < 0.001). Interaction terms between ophthalmology subspecialty and demographic factors were not significant in multivariate analysis.
Discussion
Our study found that in an urban tertiary care center, ethnic and racial minorities as well as older patients were significantly less likely to use synchronous video visits for ophthalmic care during the first 6 months of the COVID-19 pandemic. Additionally, among patients using any telehealth methods, older patients and Black patients were significantly more likely to complete only phone encounters.
Historically, synchronous methods of telehealth, such as video-based encounters, have been used sparingly in ophthalmology.16 However, the COVID-19 pandemic has spurred significant growth in ophthalmologists’ capacity to provide virtual care.2 , 4 In our study, telehealth encounters constituted more than half of all visits in an entire month after the American Academy of Ophthalmology’s recommendation to reduce in-person visit frequency on March 18, 2020, and a statewide stay-at-home order issued on March 20, 2020.17 Although increased knowledge of COVID-19 transmission prevention facilitated a return to primarily in-person clinical encounters, telemedicine continued to represent a significant proportion of ophthalmic visits, particularly for patients seeing oculoplastic subspecialists and comprehensive ophthalmologists. However, the long-term role of telemedicine in ophthalmology is uncertain. Numerous studies during the pandemic have demonstrated patients’ interest in this approach and ophthalmologists’ ability to incorporate telehealth in clinical encounters for which examination and imaging are not necessary. Even before the pandemic, research indicated patient’s willingness to use telehealth for eye care: a study of glaucoma patients at a single institution found that nearly half of those surveyed expressed favorable attitudes toward using telemedicine.18 With Medicare payment for services delivered via video telehealth extended until at least the end of 2021, the establishment of telemedicine infrastructure among clinical practices, and trends in patient preference for remote care, telemedicine is likely to become a permanent method of care delivery for many patients seeking ophthalmic care.19
However, continued expansion of telehealth for routine care requires careful scrutiny regarding accessibility. The COVID-19 pandemic already has been demonstrated to impact the health and financial status of vulnerable communities disproportionately, and several recent studies have identified socioeconomic disparities in telehealth use in other medical specialties.5, 6, 7 , 9 , 20 Our findings mirror many of these reports and show that older age was associated significantly with a lower likelihood of completing a video-based appointment but not a phone-based visit. This is unsurprising, given that telephone visits are more easily accessible for patients inexperienced with technology and that increasing age is associated with lower internet access via broadband or cellular network, as well as lower ownership of digital devices necessary for video interfacing, including laptops and smart phones.21 , 22 In contrast, greater parity exists in the ownership rates of any type of telephone among age groups in the United States.23 Technological literacy is another limiting factor for elderly patients. In a recent study of adults older than 65 years in the United States, technological inexperience was reported more frequently as the reason for unreadiness to use telemedicine, rather than infrastructural limitations.24 In a recent survey of patients with glaucoma, those older than 70 years had significantly lesser knowledge about all types of telemedicine compared with younger patients.18 Generational differences in attitudes about healthcare technology, including trust of diagnoses provided in a virtual setting or concerns about privacy, also may impact uptake among older patients.25, 26, 27 Finally, elderly patients are more likely to have motor or sensory limitations impacting telemedicine accessibility. Visual impairment is of particular concern in patients seeking eye care, and telephone calls are likely far easier to use for these patients than video encounters.
Our study also found that Black and Hispanic or Latino patients showed significantly lower uptake of both video as well as audio-only telehealth, a disparity that has been described in reports before and during the pandemic.8 , 9 , 13 Similar to elderly individuals, ethnic minorities have slightly lower rates of smartphone ownership (82% among Whites, 80% among Blacks, and 79% among Hispanics), but significantly lower rates of broadband access (79% among Whites, 66% among Blacks, and 61% among Hispanics) in the United States.11 , 12 , 21 These differences reflect wealth disparities among racial groups in the United States, and the additional financial strain imposed by the COVID-19 pandemic may exacerbate further disparate technology access. Because of the importance of in-person examinations in ophthalmic care, it is likely that telehealth is used more frequently for follow-up visits. However, both Hispanic and Black patients are less likely to use outpatient ophthalmology services than non-Hispanic White patients.14 Therefore, ethnic and racial minorities may have been more likely to require new, rather than follow-up, appointments during the pandemic, which are less able to be conducted in telemedicine settings. Telehealth underuse among minorities also may be related to awareness and the advertising of such services. A study of qualitative interviews in an underserved Hispanic population before the COVID-19 pandemic revealed that more than 90% of participants had not heard of telehealth.28
We also identified that patients for whom English was not their primary language showed lower use of synchronous video encounters even after controlling for other demographic and socioeconomic markers. Difficulties in accessing health care and underuse of clinical services in the United States among non–English-speaking patients is well documented, and it is unsurprising that language barriers persist in virtual settings.29 , 30 Difficulties for these patients can include the lack of multilingual web applications and inconsistent availability of translation services from setup to appointment completion. We did not find that the association between telemedicine use and ethnicity or race or primary language differed by the type of ophthalmology subspecialist seen. These results suggest that minority patient populations are significantly less likely to use telehealth regardless of the type of ophthalmic care they are seeking and that barriers to use are not subspecialty specific.
Differences in rates of telehealth access among patient populations were not as prevalent when including the completion of either a video or telephone visit. Indeed, on univariate analysis, older age was associated with use of any type of telehealth, which likely is reflective of the more limited technological requirements of audio-only encounters. However, expanded reimbursement for audio-only calls are likely to be discontinued at the end of the COVID-19 public health emergency.31 This has important implications for patients who may prefer or only have access to telephone-based clinical encounters. Our study specifically found that older patients, Black patients, those with Medicare, and patients seeing neuro-ophthalmologists were significantly more likely to have completed only phone visits after controlling for demographic and SES factors. Furthermore, in univariate analysis, lower household income and educational status were associated with phone, rather than video, use. Although research has demonstrated that video conferencing facilitates a higher quality of care,32 discontinued reimbursement for phone-based visits may limit the accessibility of virtual care for these patients. Continued expansion of telemedicine services will require simultaneous research efforts to determine if these patient populations prefer phone visits or have limited literacy and technology to use video methods. In the meantime, policies affect phone-based reimbursements, and policy makers should remain cognizant of potential gaps in patient access.
Differences in the use of telehealth identified in this study suggest that certain patient populations also may have been unable to access any ophthalmic care during the COVID-19 pandemic, particularly during the early phase of the pandemic when in-person encounters were severely limited. Future research specifically should examine appointment cancellations and should identify whether vulnerable populations demonstrated lower rates appointment rescheduling, as in-person appointments were resumed. These studies will help to identify patients who may have been lost to care and subsequently are at higher risk of vision loss.
Efforts to address existing barriers to telehealth uptake among vulnerable populations require an approach cognizant of systemic racism and discrimination in medicine and should include strategies to improve patient trust, telemedicine literacy, and technology accessibility. Among elderly and certain ethnic and racial minority patients, targeted promotion and education about telehealth services via local networks (e.g., churches, grocery stores, barber shops), bilingual mediums, and nonelectronic mediums such as newspapers could increase awareness and knowledge of telemedicine.33 Establishment of regulatory bodies or federal policies to enhance patient privacy in virtual mediums, particularly for consumer-facing apps and devices, is important to increase trust among populations that historically have mistrusted the health care system.34 Beyond establishing patient acceptance of telehealth, efforts should be made to increase device access among socioeconomically disadvantaged populations. Reduction of this digital divide will require subsidies for internet access, which currently is being explored by the federal government in their recent proposal to increase broadband affordability for rural and ethnic minority populations.35 Telehealth accessibility also might be improved by health plan coverage of telecommunication devices with video capacity because of medical necessity. Facilitating the introduction of telehealth to these patients through these changes may result in significant long-term uptake. Indeed, studies have found that patient satisfaction among elderly patients and ethnic and racial minorities after completing telehealth visits is extremely high and that after a telemedicine encounter, the majority of patients are willing to use telehealth again in the future.36 , 37
Study Limitations
This study has several limitations. First, the inclusion of only patients within a single academic center may limit the generalizability of our findings. However, institutional data allowed us to assess more detailed patient demographic and socioeconomic characteristics and to include heterogeneity in payment provider types. Additionally, our academic center treats an ethnically and racially diverse population representative of other large urban areas.38 Second, our center is a large academic institution with a well-developed telemedicine infrastructure. Therefore, our findings may not apply to eye care settings in group and single practices. However, we believe that inability to access or use teleconferencing technology is more dependent on patient-level factors. Third, patients’ ZCTAs served as a surrogate for exact socioeconomic characteristics. Zip code tabulation areas can span a significant area and are less accurate compared with patient-specific data. Fourth, the study might not have captured patients who might have been unable to access telemedicine and also might have been hesitant to receive in-person care. Finally, it is possible that lower use of telehealth did not necessarily equate to disruptions in care provision or a lower quality of care. To understand this topic better, future studies should compare rates of ophthalmic health care use before and during the COVID-19 pandemic among different patient populations.
In conclusion, as the COVID-19 pandemic continues to impact minority populations disproportionately, our findings indicate that a technology intended to reduce inequitable health care access unintentionally may exacerbate pre-existing disparities in health care use. Ethnic and racial minorities, older patients, and non–English-speaking patients showed significantly lower rates of video telehealth use during the COVID-19 pandemic, which parallel well-documented demographic differences in technology literacy, access, and trust. Further research is necessary to identify the potential impact on health outcomes of differences in telehealth use and which populations may benefit most from additional educational and infrastructural support.
Manuscript no. D-21-00870.
Footnotes
Disclosure(s):
All authors have completed and submitted the ICMJE disclosures form.
The author(s) have no proprietary or commercial interest in any materials discussed in this article. The study is supported by a Career Development Award from the National Eye Institute (grant no. 1 K23 EY030530-01), Yale Diabetes Center (grant no. P30 DK045735), and the Doris Duke Fund to Retain Clinical Scientists. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. This work has been supported in part by an unrestricted/challenge award to Yale Eye Center from the Research to Prevent Blindness, Inc.
HUMAN SUBJECTS: Human subjects were included in this study. The human ethics committees at Yale University approved the study. All research adhered to the tenets of the Declaration of Helsinki. The ethics committees waived informed patient consent requirements.
No animal subjects were included in this study.
Author Contributions:
Conception and design: Chen, Andoh, Nwanyanwu
Analysis and interpretation: Chen, Andoh, Nwanyanwu
Data collection: Chen, Andoh, Nwanyanwu
Obtained funding: N/A; Study was performed as part of the authors' regular employment duties. No additional funding was provided.
Overall responsibility: Chen, Andoh, Nwanyanwu
References
- 1.Mehrotra A.C.M., Linetsky D., Hatch H., Cutler D. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges. 2020. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits Available at:
- 2.Safadi K., Kruger J.M., Chowers I., et al. Ophthalmology practice during the COVID-19 pandemic. BMJ Open Ophthalmol. 2020;5(1) doi: 10.1136/bmjophth-2020-000487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams A.M., Kalra G., Commiskey P.W., et al. Ophthalmology practice during the coronavirus disease 2019 pandemic: the University of Pittsburgh experience in promoting clinic safety and embracing video visits. Ophthalmol Ther. 2020;9(3):1–9. doi: 10.1007/s40123-020-00255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Portney D.S., Zhu Z., Chen E.M., et al. COVID-19 and use of teleophthalmology (CUT Group): trends and diagnoses. Ophthalmology. 2021;128:1483–1485. doi: 10.1016/j.ophtha.2021.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Darrat I., Tam S., Boulis M., Williams A.M. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg. 2021;147(3):287–295. doi: 10.1001/jamaoto.2020.5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eberly L.A., Kallan M.J., Julien H.M., et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaffe D.H., Lee L., Huynh S., Haskell T.P. Health inequalities in the use of telehealth in the United States in the lens of COVID-19. Popul Health Manag. 2020;23(5):368–377. doi: 10.1089/pop.2020.0186. [DOI] [PubMed] [Google Scholar]
- 8.Pierce R.P., Stevermer J.J. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2020 doi: 10.1177/1357633X20963893. 1357633x20963893. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wegermann K., Wilder J.M., Parish A., et al. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19. Dig Dis Sci. 2021 Jan 28:1–7. doi: 10.1007/s10620-021-06842-5. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jain V., Al Rifai M., Lee M.T., et al. Racial and geographic disparities in internet use in the U.S. among patients with hypertension or diabetes: implications for telehealth in the era of COVID-19. Diabetes Care. 2021;44(1):e15–e17. doi: 10.2337/dc20-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perrin AT E. Smartphones help blacks, Hispanics bridge some—but not all—digital gaps with whites. 2019. https://www.pewresearch.org/fact-tank/2019/08/20/smartphones-help-blacks-hispanics-bridge-some-but-not-all-digital-gaps-with-whites/
- 12.Ryan C. American Community Survey Reports, ACS-39. United States Census Bureau; Washington, DC: 2017. Computer and internet use in the United States: 2016. [Google Scholar]
- 13.Newman Casey P.A., De Lott L., Cho J., et al. Telehealth-based eye care during the COVID-19 pandemic: utilization, safety and the patient experience. Am J Ophthalmol. 2021;230:234–242. doi: 10.1016/j.ajo.2021.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rasendran C., Tye G., Knusel K., Singh R.P. Demographic and socioeconomic differences in outpatient ophthalmology utilization in the United States. Am J Ophthalmol. 2020;218:156–163. doi: 10.1016/j.ajo.2020.05.022. [DOI] [PubMed] [Google Scholar]
- 15.Iwata A.J., Williams A.M., Taylor A.R., Chang S.S. Socioeconomic disparities and comorbidities, not race, affect salivary gland malignancy survival outcomes. Laryngoscope. 2017;127(11):2545–2550. doi: 10.1002/lary.26633. [DOI] [PubMed] [Google Scholar]
- 16.Rathi S., Tsui E., Mehta N., et al. The current state of teleophthalmology in the United States. Ophthalmology. 2017;124(12):1729–1734. doi: 10.1016/j.ophtha.2017.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Government of Connecticut Emergency orders issued by the governor and state agencies. 2021. https://portal.ct.gov/Coronavirus/Pages/Emergency-Orders-issued-by-the-Governor-and-State-Agencies
- 18.Rhodes L.A., Huisingh C.E., McGwin G., et al. Glaucoma patient knowledge, perceptions, and predispositions for telemedicine. J Glaucoma. 2019;28(6):481–486. doi: 10.1097/IJG.0000000000001238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donelan K., Barreto E.A., Sossong S., et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Managed Care. 2019;25(1):40–44. [PubMed] [Google Scholar]
- 20.Tai D.B.G., Shah A., Doubeni C.A., et al. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2021;72(4):703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenberg-Worisek A.J., Kurani S., Finney Rutten L.J., et al. Tracking healthy people 2020 internet, broadband, and mobile device access goals: an update using data from the Health Information National Trends Survey. J Med Internet Res. 2019;21(6) doi: 10.2196/13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson M. Pew Research Center; Washington, DC: 2015. 2015. The demographics of device ownership.https://www.pewresearch.org/internet/2015/10/29/technology-device-ownership-2015/ [Google Scholar]
- 23.Pew Reserach Center Demographics of mobile device ownership and adoption in the United States. 2019. https://www.pewresearch.org/internet/fact-sheet/mobile/
- 24.Lam K., Lu A.D., Shi Y., Covinsky K.E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med. 2020;180(10):1389–1391. doi: 10.1001/jamainternmed.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anthony D.L., Campos-Castillo C., Lim P.S. Who isn’t using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff (Project Hope) 2018;37(12):1948–1954. doi: 10.1377/hlthaff.2018.05117. [DOI] [PubMed] [Google Scholar]
- 26.Fischer S.H., David D., Crotty B.H., et al. Acceptance and use of health information technology by community-dwelling elders. Int J Med Inform. 2014;83(9):624–635. doi: 10.1016/j.ijmedinf.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graham C. Do People Trust Telemedicine? Technology Advice. https://technologyadvice.com/blog/healthcare/2015-telemedicine-healthcare-study/; 2015. Accessed March 8, 2021.
- 28.Ghaddar S., Vatcheva K.P., Alvarado S.G., Mykyta L. Understanding the intention to use telehealth services in underserved Hispanic border communities: cross-sectional study. J Med Internet Res. 2020;22(9) doi: 10.2196/21012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Derose K.P., Baker D.W. Limited English proficiency and Latinos’ use of physician services. Med Care Res Rev. MCRR. 2000;57(1):76–91. doi: 10.1177/107755870005700105. [DOI] [PubMed] [Google Scholar]
- 30.Kim G., Worley C.B., Allen R.S., et al. Vulnerability of older Latino and Asian immigrants with limited English proficiency. J Am Geriatr Soc. 2011;59(7):1246–1252. doi: 10.1111/j.1532-5415.2011.03483.x. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Medicare and Medicaid Services Final policy, payment, and quality provisions changes to the Medicare Physician Fee Schedule for calendar year 2021. 2020. https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year-1
- 32.Donaghy E., Atherton H., Hammersley V., et al. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract. 2019;69(686):e586–e594. doi: 10.3399/bjgp19X704141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martinez M., Perle J.G. Reaching the Latino population: a brief conceptual discussion on the use of telehealth to address healthcare disparities for the large and growing population. J Technol Behav Sci. 2019;4(3):267–273. [Google Scholar]
- 34.Hall J.L., McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff (Project Hope) 2014;33(2):216–221. doi: 10.1377/hlthaff.2013.0997. [DOI] [PubMed] [Google Scholar]
- 35.The White House . The White House Briefing Room; 2021. Fact Sheet: the American Jobs Plan [press release]https://www.whitehouse.gov/briefing-room/statements-releases/2021/03/31/fact-sheet-the-american-jobs-plan/ [Google Scholar]
- 36.Gustke S.S.B., Balch D.C., West V.L., Rogers L.O. Patient satisfaction with telemedicine. Telemedicine Journal. 2004;6(1):5–13. [Google Scholar]
- 37.Ramaswamy A., Yu M., Drangsholt S., et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22(9) doi: 10.2196/20786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kolko J. ‘Normal America’ is not a small town of White people. 2016. https://fivethirtyeight.com/features/normal-america-is-not-a-small-town-of-white-people/