Abstract
Introduction
Injuries cause significant burdens in sub-Saharan Africa. In Rwanda, national regulations to reduce COVID-19 altered population mobility and resource allocations. This study evaluated epidemiological trends and care among injured patients preceding and during the COVID-19 pandemic at the Centre Hospitalier Universitaire de Kigali (CHUK) in Kigali, Rwanda.
Methods
This prospective interrupted cross-sectional study enrolled injured adult patients (≥15 years) presenting to the CHUK emergency department (ED) from January 27th-March 21st (pre-COVID-19 period) and June 1st-28th (intra-COVID-19 period). Trained study personnel continuously collected standardized data on enrolled participants through the first six-hours of ED care. The Kampala Trauma Score (KTS) was calculated as a metric of injury severity. Case characteristics prior to and during the pandemic were compared, statistical differences were assessed using χ2 or Fisher's exact tests.
Results
Data were collected from 409 pre-COVID-19 and 194 intra-COVID-19 cases. Median age was 32, with a male predominance (74.3%). Road traffic injuries (RTI) were the most common injury mechanism pre-COVID-19 (47.8%) and intra-COVID-19 (53.6%) (p = 0.27). There was a significant increase in the number of transfer cases during the intra-COVID-19 period (52.1%) versus pre-COVID-19 (41.3%) (p = 0.01). KTS was significantly lower among intra-COVID-19 patients (p = 0.04), indicating higher severity of presentation. In the intra-COVID-19 period, there was a significant increase in the number of surgery consultations (40.7%) versus pre-COVID-19 (26.7%) (p < 0.001). The number of hospital admissions increased from 35.5% pre-COVID-19 to 46.4% intra-COVID-19 (p = 0.01). There was no significant mortality difference pre-COVID-19 as compared to the intra-COVID-19 period among injured patients (p = 0.76).
Conclusion
Emergency injury care showed increased injury burden, inpatient admission and resource requirements during the pandemic period. This suggests the spectrum of disease may be more severe and that greater resources for injury management may continue to be needed during the ongoing COVID-19 pandemic in Rwanda and other similar settings.
Keywords: Rwanda, Injury care, COVID-19, Coronavirus, Global health, Lockdown
African relevance
-
•
Injuries cause significant morbidity and mortality in sub-Saharan African countries such as Rwanda.
-
•
The COVID-19 pandemic caused shifts in resource allocations in Africa and specific data on the impact of these changes are needed to inform ongoing care delivery.
-
•
During the COVID-19 pandemic an increase in injury burden and resource requirements was observed, suggesting a more severe disease spectrum and continued need for injury care resources
Introduction
Injuries cause major morbidity and mortality worldwide, accounting for over 10% of the global burden of disease and approximately five million deaths annually [1]. Disproportionately, more than 90% of morbidity and mortality from injuries occurs in low- and middle-income countries (LMICs) [1]. In Africa where injuries burdens are high, road traffic incidents (RTIs) are the most common mechanism of injury 1., 2., [3].
Injury care requires rapid access to potentially life-saving treatments due to the diverse and time sensitive nature of illness [3]. Yet, injury care resources remain limited in LMICs, making delivering appropriate emergency care challenging. Trauma, a significant burden in Rwanda, accounts for 22% of the deaths in the capital city of Kigali 4., [5]. Furthermore, an estimated 9% of deaths and 10% of disability adjusted life years (DALYs) in Rwanda are attributable to injuries [6].
In early 2020, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus which causes coronavirus disease (COVID-19), became a global pandemic threat [7]. The first case of COVID-19 in Rwanda was identified on March 14, 2020. In response, Rwanda implemented prevention and containment measures, including: a national lockdown consisting of closure of all borders, limitations on air travel, suspension of public transport, restrictions on unnecessary movements, closure of public spaces, as well as isolation and care for COVID-19 infected patients and suspected cases. Following this lockdown, the Rwandan government implemented curfews and limited social gatherings 8., 9.. These actions reduced population mobility in Rwanda, particularly motorized transport 8., 9..
The COVID-19 pandemic has changed health care delivery, particularly the allocation of resources for pandemic response but also all other forms of health care [10], [11]. In LMIC settings which already have reduced access to healthcare resources and personnel, the impacts of the pandemic response on other common disease processes such as injuries may be substantial 12., 13., 14.. This study evaluated injury epidemiology and emergency injury care in Kigali, Rwanda prior to and during the COVID-19 pandemic.
Methods
This prospective cross-sectional study was designed to evaluate adult injury burdens and acute care treatments at the emergency department (ED) at CHUK, the main public referral health facility and teaching hospital in Rwanda. CHUK is the largest of 4 injury referral hospitals which serve Rwanda's population of more than 6 million and one of the two located in Kigali [15]. The proportion of patients seeking injury care is estimated to be as high as 45% [16]. For the study protocol, the first 6 h of care were defined as the acute emergency care period of interest. The epidemiology of injuries and the provision of acute emergency care during these first hours of treatment were defined as the outcomes of interest. Subsequent to the pandemic restrictions, the outcomes were expanded to include final ED disposition. All patients older than 15 years of age presenting to the ED with an injury were eligible for inclusion. Patients with concurrent medical needs unrelated to the index injury, pregnant patients, those unable or unwilling to provide informed consent, and legal prisoners of the state were excluded. The research activities were approved by the CHUK ethics committee (CHUK.EC. 155.2019, CHUK.EC. 024.2019), University of Rwanda College of Medicine and Health Sciences and the institutional review board of Rhode Island Hospital (Lifespan IRB00000396).
Data collection was initially planned for a continuous period of 16 weeks. However, due to disruptions related to the COVID-19 pandemic data were collected from January 27th-March 21st and June 1st- June 28th 2020, with a cessation of all research activities during the first nation-wide lockdown which took place from March 22nd to May 3rd. Data collection resumed on June 1st, 2020 after regulations were relaxed, but a curfew from 9 pm to 5 am was still enforced. Due to these external regulations, the data available represents four time periods: pre-COVID-19 (study period, January 27th-March 21st, 2020), intra-COVID-19 (during lockdown, non-study period, March 22nd-May 3rd, 2020), intra-COVID-19 (non-lockdown, non-study period, May 3rd-May 31st, 2020) and intra-COVID-19 (non-lockdown, study period, June 1st- June 28th, 2020) 9., 17..
Adult patients presenting for care to the CHUK ED were continuously screened during the pre-COVID-19 (study period, January 27th-March 21st, 2020) and intra-COVID-19 (non-lockdown, study period, June 1st- June 28th, 2020) recruitment periods. Patients were screened after initial triage and stabilization had been conducted by clinicians as to not impede care. Screened patients meeting inclusion criteria and providing informed consent were enrolled. If a patient was unable to consent due to incapacity, a legally authorized patient representative provided informed consent.
Dedicated research personnel trained in standardized protocols collected data continuously using structured case reporting forms. Data were collected via hourly assessments, for the first 6 h of care after presentation. This was achieved by directly assessing enrolled participants or their authorized representative and from the medical records. Following enrolment, prospective data was gathered on sociodemographic and anthropomorphic characteristics, vital signs, mechanism of injury, markers of injury severity and medical interventions, and ED disposition. Time since injury to presentation was calculated in minutes. A Kampala Trauma Score (KTS), a validated prognostic indicator of injury severity in LMICs was calculated [18], [19]. A lower KTS (≤12) indicates more severe injury whereas a higher KTS (≥13) indicates a less severe injury state [18]. Shock index at triage was calculated using heart rate divided by systolic blood pressure and dichotomized at a cut point of >0.9 consistent with prior studies [20].
Data were inputted daily into a secure electronic database by trained study personnel. For cases in which the final ED disposition was not known within 6 h of presentation patient charts were retrospectively reviewed to ascertain the ED outcomes status if the final outcome status was available from the medical documentation. Additionally, to evaluate case presentations during the intra-COVID-19 lockdown, non-study period and intra-COVID-19 non-lockdown, non-study period which included the dates March 22nd to May 31st, 2020 registry logs were reviewed with standardized data retrospectively abstracted and entered into an electronic database.
STATA Version 15.0 (Stata Corp; College Station, USA) was used for analyses. The epidemiologic profile of the population was characterized using descriptive statistics based on the comparative study periods of interest. Summary statistics were calculated using frequencies and percentages for categorical variables, and continuous variables were described using median values with associated interquartile ranges (IQR). Cases were stratified by time periods Pre-COVID-19 and Intra-COVID-19. Differences in characteristics were assessed using χ2 or Fisher's exact tests for categorical variables and independent t-tests for continuous variables.
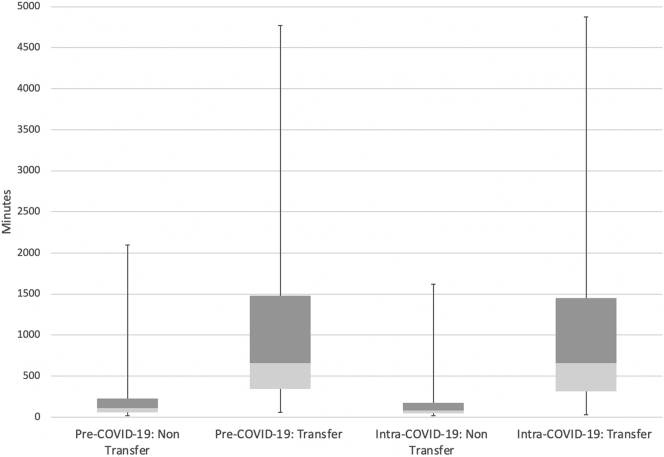
Trends in ED cases were summarized and analysed by collapsing daily counts into weekly injured patient frequencies. Period specific averages with associated standard deviations (SD) were calculated. Linear regression models were constructed to assess weekly changes in ED patient volume, including fitting trendlines for study periods and performing hypothesis testing to query significance of regression coefficients, including trendline slopes. A box and whisker plot was created to describe elapsed time from injury to ED presentation stratified by transfer status across the pre-COVID-19 and intra-COVID-19 study periods. Outliers were identified and excluded from the plot if data points were greater than 1.5 times the bounds of the associated IQR for the specific series plotted.
Results
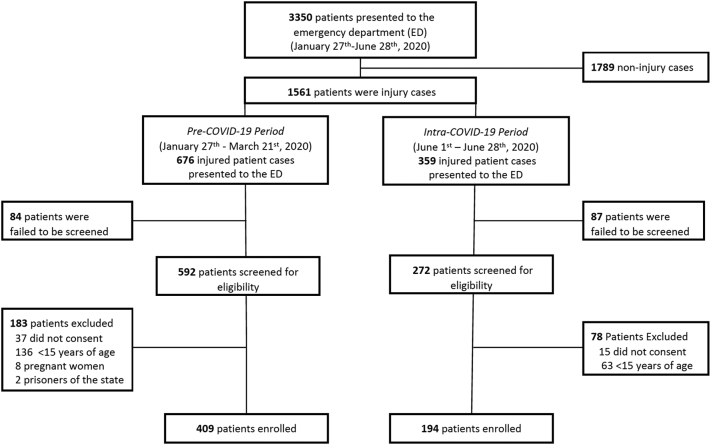
A total of 864 adult patients seeking care for injuries were screened for study inclusion. Of these, 603 (70.0%) consented and were enrolled. Of those enrolled, 409 (67.8%) patients presented for injury care pre-COVID-19 (January 27th-March 21st) and 194 (32.2%) patients intra-COVID-19 (June 1st-June 28th) (Fig. 1).
Fig. 1.
Study flow diagram.
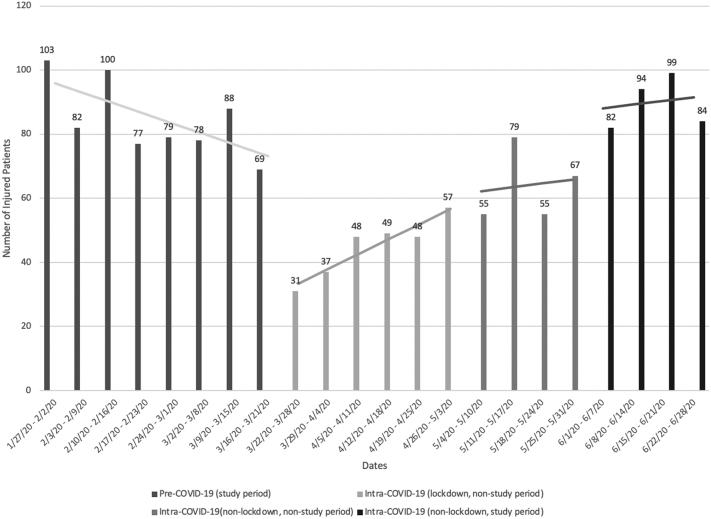
The average weekly volumes of injury cases varied significantly throughout the four-time periods (Fig. 2). During the pre-COVID-19 study period, there was an average of 84.5 (±SD = 11.8) injured patients per week in the ED with an insignificant negative trend in the slope over the time period (-3.24 weekly, p = 0.07). During the intra-COVID-19 lockdown non-study period there was an observed reduction in weekly cases, with an average of 45 (±SD = 9.36) injury cases per week. However, despite this decrease in observed weekly cases during this time period there was still a significant positive trend in slope with increasing weekly average case presentations (+4.69 weekly, p = 0.006). There was an average of 64 (±SD = 11.5) ED injury patients per week during the intra-COVID-19 non-lockdown non-study period, with an insignificant up trending slope per week (+1.20 weekly, P = 0.87). During the intra-COVID-19 non-lockdown study period when the study's enrolment resumed, ED injury volume averaged 89.8 (±SD = 8.10) cases per week with an insignificant positive slope trend line (+1.10 weekly, p = 0.83) (Fig. 2). When all three intra-COVID periods are combined as one continuous intra-COVID period (lockdown, non-lockdown, and enrolment) the slope of the trendline is significantly positive (+4.68 weekly, p < 0.001).
Fig. 2.
Frequency of injury cases presenting for emergency care over time.a
aTrendlines represent the slope for each time period of interest.
In comparison of cases from the pre-COVID-19 and intra-COVID-19 time periods, there was no statistical difference in gender (p = 0.19) or age (p = 0.99) (Table 1). The primary injury mechanism was RTIs in both time periods (47.8% vs. 53.6%), with no statistical differences in mechanisms of injury between groups. During both time periods, the most common anatomical regions of injuries were extremities and craniofacial, with no statistical difference between regions of injury. There was a significant increase in the number of patients transferred intra-COVID-19 (52.1%) when compared to pre-COVID-19 (41.3%%) (p = 0.01). The distribution of calculated KTS were less severe in the pre-COVID-19 population than the intra-COVID-19 one (p = 0.04). There was a slight increase in median time from injury to care presentation during the pandemic; however, this was found to not be statistically different (238.5 vs. 289 min, p = 0.55) (Table 1).
Table 1.
Case comparisons between the pre-COVID-19 and intra-COVID-19 periods.a
| Pre-COVID-19 (n = 409) |
Intra-COVID-19 (n = 194) |
P value | |
|---|---|---|---|
| n (%) or median (IQR) | n (%) or median (IQR) | ||
| Gender | |||
| Male | 297 (72.79%) | 151 (77.84%) | 0.19 |
| Female | 111 (27.21%) | 43 (22.16%) | |
| Age (years) | 32 (25, 43) | 32 (25, 42) | 0.99 |
| Mechanism of injury | |||
| Road traffic injuries | 194 (47.8%) | 104 (53.6%) | |
| Fall | 115 (28.3%) | 53 (27.3%) | |
| Burn/electrocution | 15 (3.69%) | 3 (1.55%) | 0.27 |
| Stab/cut | 35 (8.62%) | 8 (4.12%) | |
| Other penetrating | 24 (5.91%) | 15 (7.73%) | |
| Other blunt | 6 (1.48%) | 2 (1.03%) | |
| Assaults unspecified | 17 (4.19%) | 9 (4.64%) | |
| Anatomical regions of injuriesb | |||
| Craniofacial | 136 (33.25%) | 71 (36.6%) | 0.42 |
| Neck | 15 (3.67%) | 9 (4.64%) | 0.57 |
| Thorax | 49 (11.98%) | 18 (9.28%) | 0.32 |
| Abdomen-pelvis | 34 (8.31%) | 11 (5.67%) | 0.25 |
| Cervical spine | 15 (3.67%) | 5 (2.58%) | 0.49 |
| Thoracic spine | 9 (2.20%) | 2 (1.03%) | 0.32 |
| Lumbar spine | 11 (2.69%) | 2 (1.03%) | 0.19 |
| Upper extremity | 135 (33.0%) | 55 (28.35%) | 0.25 |
| Lower extremity | 166 (40.6%) | 78 (40.21%) | 0.93 |
| Genitalia | 5 (1.22%) | 2 (1.03%) | 0.84 |
| Types of injuries | |||
| Fracture closed | 127 (31.1%) | 65 (33.5%) | 0.55 |
| Fracture open | 49 (12.0%) | 39 (20.1%) | 0.008 |
| Bruise | 143 (35.0%) | 67 (34.5%) | 0.92 |
| Open wound | 112 (27.4%) | 52 (26.8%) | 0.88 |
| Burn | 14 (3.42%) | 3 (1.55%) | 0.19 |
| Vascular injury | 14 (3.42%) | 2 (1.03%) | 0.09 |
| Nerve injury | 5 (1.22%) | 0 (0.0%) | 0.12 |
| Dislocation | 7 (1.71%) | 9 (4.64%) | 0.04 |
| Time since injury (minutes) | 238.5 (83, 820) | 289 (80, 970) | 0.55 |
| Time of injury | |||
| 5 am to 9 pm (non-curfew) | 340 (83.7%) | 170 (87.6%) | 0.21 |
| 9 pm to 5 am (curfew) | 66 (16.3%) | 24 (12.4%) | |
| Transferred from other health facility | |||
| Yes | 169 (41.3%) | 101 (52.1%) | 0.01 |
| No | 240 (58.7%) | 93 (47.9%) | |
| Shock index | |||
| <0.9 | 374 (91.4%) | 175 (90.2%) | 0.62 |
| ≥0.9 | 35 (8.56%) | 19 (9.79%) | |
| Kampala trauma score | |||
| 10 | 1 (0.24%) | 1 (0.52%) | |
| 11 | 3 (0.73%) | 5 (2.58%) | |
| 12 | 13 (3.18%) | 8 (4.12%) | 0.04 |
| 13 | 25 (6.11%) | 11 (5.67%) | |
| 14 | 97 (23.72%) | 51 (26.29%) | |
| 15 | 242 (59.17%) | 112 (57.73%) | |
| 16 | 28 (6.85%) | 6 (3.09%) | |
| Glasgow Coma Scale | |||
| 3-8 | 5 (1.24%) | 6 (3.21%) | |
| 9-12 | 15 (3.73%) | 12 (6.42%) | 0.09 |
| 13-15 | 382 (95.0%) | 169 (90.4%) |
Pre-Covid-19 data was collected from January 27th-March 21st and intra-COVID-19 from June 1st-June 28th, 2020.
Variable categories are not mutually exclusive therefore cumulative percentages may be greater than 100%.
There were observed increases in the proportion of ED procedures performed during the intra-COVID-19 period compared to the pre-COVID-19 period. Splinting (35.1% vs. 24.26%, p = 0.006), tourniquet use (3.61% vs. 0.74%, p = 0.01), point of care ultrasound (eFAST) (36.6% vs 23.7%, p < 0.001), and IV fluids (51.6% vs. 38.6%, p = 0.003) were found to all have occurred more frequently in the intra-COVID period (Table 2). There was a significant increase in patients receiving surgical consultations during the intra-COVID-19 period (64.4%) versus pre-COVID-19 (50.1%, p < 0.001). Evaluation by a subspecialty between the time periods of interest showed significantly more consultations during the intra-COVID-19 period for orthopaedics (40.7% vs. 26.7%, p < 0.001) and neurosurgery (16.0% vs. 9.05%, p = 0.01). Overall, hospital admission increased from 35.5% pre-COVID-19 to 46.4% intra-COVID-19 (p = 0.01). However, there was no significant difference between the two time periods in outcomes based on ED mortality with 1.71% pre-COVID-19 vs. 2.06% intra-COVID-19 (p = 0.76).
Table 2.
Comparison of emergency care provision Pre-COVID-19 and intra-COVID-19.a
| Pre-COVID-19 (n = 409) |
Intra-COVID-19 (n = 194) |
P value | |
|---|---|---|---|
| n (%) or median (IQR) | n (%) or median (IQR) | ||
| In ED proceduresb | |||
| Intubation | 10 (2.44%) | 9 (4.64%) | 0.15 |
| Spinal immobilization | 23 (5.64%) | 11 (5.67%) | 0.99 |
| Splinting | 99 (24.26%) | 68 (35.1%) | 0.006 |
| Wound care | 173 (42.40%) | 90 (46.4%) | 0.36 |
| Vasopressors | 3 (0.74%) | 0 (0.0%) | 0.56 |
| Tourniquet | 3 (0.74%) | 7 (3.61%) | 0.01 |
| Chest tube | 49 (12.0%) | 18 (9.28%) | 0.06 |
| Point-of-care ultrasound | 97 (23.7%) | 71 (36.6%) | <0.001 |
| IV fluids | 158 (38.6%) | 100 (51.6%) | 0.003 |
| Red blood cell transfusion | 14 (3.42%) | 6 (3.09%) | 0.83 |
| Platelet transfusion | 1 (0.24%) | 3 (1.55%) | 0.07 |
| Plasma transfusion | 1 (0.24%) | 1 (0.52%) | 0.59 |
| Surgery consultationsb | |||
| Total | 205 (50.1%) | 125 (64.4%) | <0.001 |
| General surgery | 46 (11.3%) | 12 (6.19%) | 0.05 |
| Orthopaedics | 109 (26.7%) | 79 (40.7%) | <0.001 |
| Neurosurgery | 37 (9.05%) | 31 (16.0%) | 0.01 |
| Otolaryngology | 3 (0.73%) | 4 (2.06%) | 0.22 |
| Stomatology | 5 (1.22%) | 9 (4.64%) | 0.009 |
| Urology | 1 (0.49%) | 1 (0.8%) | 0.54 |
| Ophthalmology | 1 (0.49%) | 0 (0.00%) | 1.00 |
| Burn unit | 1 (0.49%) | 0 (0.00%) | 1.00 |
| Emergency care disposition | |||
| Admitted | 145 (35.5%) | 90 (46.4%) | 0.01 |
| Deceased | 7 (1.71%) | 4 (2.06%) | 0.76 |
| Discharged | 227 (55.5%) | 87 (44.9%) | 0.01 |
| Transferred | 5 (1.22%) | 2 (1.03%) | 1.00 |
| Missing | 25 (6.07%) | 11 (5.67%) | 0.97 |
Pre-Covid-19 data was collected from January 27th-March 21st and intra-COVID-19 from June 1st-June 28th, 2020.
Variable categories are not mutually exclusive therefore cumulative percentages may be greater than 100%.
Between the study periods of interest there was a significant increase in the proportion of injury cases that were transferred from other health facilities to CHUK. During the pre-COVID-19 period transfers accounted for 41.3% of cases while in the intra-COVID-19 period they accounted for 52.1% of cases (p = 0.013) (Table 2).
As represented in the box and whisker plot the median time from injury to ED arrival was greater for transferred cases versus those not transferred when evaluating the pre- and intra-COVID-19 time periods. However, there was no substantial difference observed in median times, and the associated variance, for those transferred or not transferred (Fig. 3).
Fig. 3.
Box and whisker plot of time since injury to presentation based on transfer status for pre-COVID-19 and intra-COVID-19 periods.a
aPre-Covid-19 data was collected from January 27th-March 21st and intra-COVID-19 from June 1st-June 28th, 2020.
A comparison of emergency care provision among transfer cases pre-COVID-19 and intra-COVID-19 is located in supplement 1.
Discussion
A total of 864 adult patients seeking care for injuries were screened for study inclusion. Of these, 603 (70.0%) consented.
In this prospective emergency care population studied, where injury cases were accrued pre- and intra- COVID-19 pandemic, there were notable observed differences in presentation and required acute treatments. Specifically, injury care at the study site had high disease burdens, increased inpatient admission with greater resource requirements during the intra-COVID-19 pandemic period. This suggests that as COVID-19 continues injuries remain an important driver of health needs and may require greater resources for management in Rwanda and other similar settings in Africa.
Observations in gender, age, mechanism, and anatomical locations of injuries remained similar pre-COVID-19 and intra-COVID-19, as observed in other countries during the pandemic 21., [22]. RTIs were the most common cause of trauma and there was no significant difference in their prevalence between the pre- and intra-COVID-19 periods. These findings are similar to reports which found the prevalence of RTIs persisted during the pandemic, possibly due to greater risk-taking behaviour on roads with lower densities of motorists 23., 24.. In contrast, some studies found decreased RTIs after the implementation of measures to reduce social mobility which could stem from population differences in terms of access to motor vehicles or public transport 25., 26., 27., [28], [29]. Given the ongoing need for pandemic control through physical distancing and social prevention measures, further understanding of the factors involved in seeking injury care would be beneficial to inform public health approaches in relation to COVID-19.
During the COVID-19 pandemic the number of patients presenting to the ED for injury care varied. Notably reduced numbers of ED injury patients seeking care were observed as the public health response enacted strict guidelines on mobility during the lockdown periods. Similar to reports from other settings, the Rwandan population has likely been less mobile, spending more time indoors, reducing exposures that may cause injury 25., 26.. Combined with the finding that the cases presenting utilized more acute interventions, surgical consults and hospital admissions, the decrease in weekly number of injury patients at the ED may indicate that patients were not readily seeking care for mild or moderate injuries [25]. This could be related to delays in healthcare-seeking behaviours due to mobility restrictions or fear of entering health facilities during the pandemic. As the pandemic continues, observations found in the current results point towards the need for the provision of more comprehensive injury care services such that the immensely common healthcare needs due to trauma in LMICs can be sufficiently met.
When comparing pre-COVID-19 and intra-COVID-19 periods, there was a significant increase in number of injured patients transferred to CHUK from other health centres during the pandemic time periods. As the study site is the largest and one of the most well-resourced public referral centres for injury care in Rwanda, this may indicate that more patients presenting to outside health centres had increased healthcare needs necessitating transfer. As indicators of injury severity were greater in the intra-COVID-19 period this hypothesis would be supported and has been observed in other countries [30], [31]. Alternatively, care of pandemic patients may have diverted human and material resources away from other medical care, an effect that may be pronounced in smaller health centres and result in more patient transfers to higher-level centres. Future work should aim to disentangle the driving factors for transfers so setting appropriate adjustments can be enacted to ensure resources match needs at both lower-resourced referring and high-resourced receiving facilities.
Finally, as Rwanda has had one of the most successful pandemic responses in Africa, and globally, comparisons with other countries of the COVID-19 impact on trauma may yield insights into whether and how public health measures in Rwanda mitigated or prevented harmful changes to emergency healthcare delivery [32]. It is important to note at the time of this writing, Rwanda gradually eased lockdown measures and was settling into a new, long-term normal, until January 19th, 2021. At that time, a new city-wide lockdown in Kigali was implemented after increased COVID-19 cases [33]. Restrictions on social mobility and public transportation were implemented with a plan for gradual re-opening.
There are limitations to this study. Firstly, the initial intent of the prospective assessment was designed specifically to evaluate temporal trends associated with acute injury care at the study site. However, the COVID-19 pandemic occurred during data collection and the study was adapted to meet the constraints existing in the research setting. This allowed for reorientation of the work and the data evolved in a manner that logically supported the present analysis. However, the lack of a pre-planned approach for the pandemic topical matter must be acknowledged. Relatedly, prospective individual case level data collection was ceased during the period of national lockdown, due to considerations for public health and adherence to guidelines, which prevents full understanding of injury trends during portions of the COVID-19 pandemic.
It is important to address that this study took place 3 months prior to the pandemic and then 1 month during the pandemic. This is a limited observation time to draw conclusions on the pandemic's full impact on injury care. The possible influence of seasonal trends and other cyclical effects could not be quantified. However, the observations here are similar to reports from other country's trauma registries which observed decreases in injury presentations 34., [35], [36], [37]. Also, despite the employment of a prospective methodology, there were cases not captured in the screening process. Although the number of missed cases was not large it is possible selection bias was introduced, and it is unknown if the missed cases were significantly different from those that were studied. There was also missing data for final ED disposition. This was secondary to an inability to discern final outcome status from the available medical documentation. Although possible that the missingness in the dispositions data could have impacted the findings, this was a small number of cases comprising only 5.9% and as such is unlikely to alter any of the findings in a clinically substantial manner.
Additionally, the presented data does not allow to differentiate between intentional and unintentional injuries as this may be important. Finally, the current data are derived from a single centre with relatively robust access to injury care services and the extrapolation to country level implications and other health facilities is not clear. Despite these limitations, the results allow for observations in injury trends and resource needs in the setting of the COVID-19 pandemic in Rwanda and could be used to inform future research and may serve as a recourse for healthcare development and policy in the study setting and other similar LMICs.
Adult injury patterns and related acute emergency care in Rwanda preceding the COVID-19 pandemic were different as compared to during the pandemic. Patient volumes decreased during lockdown periods while injury care needs increased during the pandemic period, suggesting regulations may have affected exposures and health-seeking behaviour with a skewing of injury events to a more severe spectrum of trauma. As one of the few prospective studies on injury care in a LMIC during the COVID-19 pandemic, this study provides insights on the impacts of the pandemic and public health response on injury patterns in Rwanda and may serve to inform care delivery as the pandemic continues.
The following is the supplementary data related to this article.
Comparison of emergency care provision among transfer cases pre-COVID-19 and intra-COVID-19a.
Dissemination of results
Preliminary results from this work were presented at the Society for Academic Emergency Medicine. The results of this study were also shared with the ED at the study site through an informal presentation.
Authors' contribution
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: CU, CGM and AB contributed 45%; ARA 10%; and ZM, FRT, LJ, VN, DU, MN, OT, SN, SJ 5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors have no conflicts of interest.
Acknowledgements
The authors would like to thank the Emergency Department staff at the Centre Hospitalier Universitaire de Kigali for all their help and support of the study. Funding for this research was provided through Brown Physicians Incorporated and Brown Emergency Medicine research grants. ARA was supported by funding from the National Institutes of Health, National Institute of Allergy and Infectious Diseases (1K23AI145411). The funders had no role in the study design, data collection or reporting processes.
References
- 1.Haagsma J.A., Graetz N., Bolliger I., Naghavi M., Higashi H., Mullany E.C. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the global burden of disease study 2013. Inj Prev J Int Soc Child Adolesc Inj Prev. 2016 Feb;22(1):3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adeloye D., Thompson J.Y., Akanbi M.A., Azuh D., Samuel V., Omoregbe N. The burden of road traffic crashes, injuries and deaths in Africa: a systematic review and meta-analysis. Bull World Health Organ. 2016 Jul;94(7):510–521A. doi: 10.2471/BLT.15.163121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mbanjumucyo G., George N., Kearney A., Karim N., Aluisio A.R., Mutabazi Z. Epidemiology of injuries and outcomes among trauma patients receiving prehospital care at a tertiary teaching hospital in Kigali, Rwanda. Afr J Emerg Med Rev Afr Med d’urgence. 2016 Dec;6(4):191–197. doi: 10.1016/j.afjem.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim W.C., Byiringiro J.C., Ntakiyiruta G., Kyamanywa P., Irakiza J.J., Mvukiyehe J.P. Vital statistics: estimating injury mortality in Kigali, Rwanda. World J Surg. 2016 Jan;40(1):6–13. doi: 10.1007/s00268-015-3258-3. [DOI] [PubMed] [Google Scholar]
- 5.Petroze R.T., Joharifard S., Groen R.S., Niyonkuru F., Ntaganda E., Kushner A.L. Injury, disability and access to care in Rwanda: results of a nationwide cross-sectional population study. World J Surg. 2015 Jan;39(1):62–69. doi: 10.1007/s00268-014-2544-9. [DOI] [PubMed] [Google Scholar]
- 6.Odland M.L., Whitaker J., Nepogodiev D., Aling’ C.A., Bagahirwa I., Dushime T. Identifying, prioritizing and visually mapping barriers to injury care in Rwanda: a multi-disciplinary stakeholder exercise. World J Surg. 2020;44(9):2903–2918. doi: 10.1007/s00268-020-05571-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pacifique N., Menelas N., Nadia H., David T., Ernest N., Fidele B. Knowledge, attitudes and preventive practices towards COVID-19 among frontline healthcare workers in Rwanda. Rw Public Health Bull. 2020;2(1):16–21. [Google Scholar]
- 9.Republic of Rwanda, Office of the Prime Minister . 21 March 2020. Announcement on enhanced COVID-19 prevention measures. Kigali, Rwanda. [Google Scholar]
- 10.Adiamah A., Moody N., Blackburn L., Dickson E., Thompson A., Reilly J.J. ICON trauma (impact of COVID-19 on major trauma workload) study. Vol. 107. 2020. pp. e412–e413. (Br J Surg). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sutherland M., McKenney M., Elkbuli A. Vehicle related injury patterns during the COVID-19 pandemic: what has changed? Am J Emerg Med. 2020 Sep;38(9):1710–1714. doi: 10.1016/j.ajem.2020.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Nuwagira E., Muzoora C. Is Sub-Saharan Africa prepared for COVID-19? Trop Med Health. 2020;48(1) doi: 10.1186/s41182-020-00206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Sadr W.M., Justman J. Africa in the path of Covid-19. N Engl J Med. 2020;383(3) doi: 10.1056/NEJMp2008193. [DOI] [PubMed] [Google Scholar]
- 14.Anjorin A.A., Abioye A.I., Asowata O.E., Soipe A., Kazeem M.I., Adesanya I.O. Comorbidities and the COVID-19 pandemic dynamics in Africa. Trop Med Int Health. 2021;26(1):2–13. doi: 10.1111/tmi.13504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ntakiyiruta G., Wong E.G., Rousseau M.C., Ruhungande L., Kushner A.L., Liberman A.S. Trauma care and referral patterns in Rwanda: implications for trauma system development. Can J Surg. 2016 Feb;59(1):35–41. doi: 10.1503/cjs.008115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aluisio A.R., Barry M.A., Martin K.D., Mbanjumucyo G., Mutabazi Z.A., Karim N. Impact of emergency medicine training implementation on mortality outcomes in Kigali, Rwanda: an interrupted time-series study. african. J Emerg Med. 2019;9(1):14–20. doi: 10.1016/j.afjem.2018.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Republic of Rwanda, Office of the Prime Minister . 30 April 2020. Statement of cabinet resolutions of 30th April 2020. Kigali, Rwanda. [Google Scholar]
- 18.Akay S., Ozturk A.M., Akay H. Comparison of modified Kampala trauma score with trauma mortality prediction model and trauma-injury severity score: a National Trauma Data Bank Study. Am J Emerg Med. 2017;35(8):1056–1059. doi: 10.1016/j.ajem.2017.02.035. [DOI] [PubMed] [Google Scholar]
- 19.Gardner A., Forson P.K., Oduro G., Stewart B., Dike N., Glover P. Diagnostic accuracy of the Kampala trauma score using estimated abbreviated injury scale scores and physician opinion. Injury. 2017;48(1):177–183. doi: 10.1016/j.injury.2016.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.King R.W., Plewa M.C., Buderer N.M., Knotts F.B. Shock index as a marker for significant injury in trauma patients. Acad Emerg Med Off J Soc Acad Emerg Med. 1996 Nov;3(11):1041–1045. doi: 10.1111/j.1553-2712.1996.tb03351.x. [DOI] [PubMed] [Google Scholar]
- 21.Li Y., Zeng L., Li Z., Mao Q., Liu D., Zhang L. Emergency trauma care during the outbreak of corona virus disease 2019 (COVID-19) in China. World J Emerg Surg. 2020 May;15(1):33. doi: 10.1186/s13017-020-00312-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haut E.R., Leeds I., Livingston D.H. The effect on trauma care secondary to the COVID-19 pandemic: collateral damage from diversion of resources. Ann Surg. 2020 May;272(3):e204–e207. doi: 10.1097/SLA.0000000000004105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vingilis E., Beirness D., Boase P., Byrne P., Johnson J., Jonah B. Coronavirus disease 2019: what could be the effects on road safety? Accid Anal Prev. 2020 Sep;144:105687. doi: 10.1016/j.aap.2020.105687. 2020/07/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Inada H., Ashraf L., Campbell S. COVID-19 lockdown and fatal motor vehicle collisions due to speed-related traffic violations in Japan: a time-series study. Inj Prev. 2021 Feb 1;27(1) doi: 10.1136/injuryprev-2020-043947. 98 LP – 100. [DOI] [PubMed] [Google Scholar]
- 25.Morris D., Rogers M., Kissmer N., Du Preez A., Dufourq N. Impact of lockdown measures implemented during the Covid-19 pandemic on the burden of trauma presentations to a regional emergency department in Kwa-Zulu Natal, South Africa. Afr J Emerg Med. 2020 Dec;10(4):193. doi: 10.1016/j.afjem.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rhodes H.X., Petersen K., Biswas S. Trauma trends during the initial peak of the COVID-19 pandemic in the midst of lockdown: experiences from a rural trauma center. Cureus<label/>. 2020 Aug;12(8) doi: 10.7759/cureus.9811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nourazari S., Davis S.R., Granovsky R., Austin R., Straff D.J., Joseph J.W. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med. 2020 Nov;42:203–210. doi: 10.1016/j.ajem.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kamine T.H., Rembisz A., Barron R.J., Baldwin C., Kromer M. Decrease in trauma admissions with COVID-19 pandemic. West J Emerg Med. 2020 May;21(4):819–822. doi: 10.5811/westjem.2020.5.47780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sutherland M., McKenney M., Elkbuli A. Vehicle related injury patterns during the COVID-19 pandemic: what has changed? Am J Emerg Med. 2020 Sep;38(9):1710–1714. doi: 10.1016/j.ajem.2020.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Czeisler M.É., Marynak K., Clarke K.E.N., Salah Z., Shakya I., Thierry J.M. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jeffery M.M., D’Onofrio G., Paek H., Platts-Mills T.F., Soares W.E., Hoppe J.A. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karuhanga J. The New Times; 2021 Jan 28. Rwanda named among top 10 countries that responded best to Covid-19 outbreak.https://www.newtimes.co.rw/news/rwanda-named-among-top-10-countries-responded-best-covid-19-outbreak Available from: [Google Scholar]
- 33.Republic of Rwanda, Office of the Prime Minister . 18 January 2021. Cabinet Communiqué. Kigali, Rwanda. [Google Scholar]
- 34.Maleitzke T., Pumberger M., Gerlach U.A., Herrmann C., Slagman A., Henriksen L.S. Impact of the COVID-19 shutdown on orthopedic trauma numbers and patterns in an academic Level I Trauma Center in Berlin, Germany. PLoS One. 2021;16(2 February):1–17. doi: 10.1371/journal.pone.0246956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacob S., Mwagiru D., Thakur I., Moghadam A., Oh T., Hsu J. Impact of societal restrictions and lockdown on trauma admissions during the COVID-19 pandemic: a single-centre cross-sectional observational study. ANZ J Surg. 2020 Nov;90(11):2227–2231. doi: 10.1111/ans.16307. [DOI] [PubMed] [Google Scholar]
- 36.Christey G., Amey J., Campbell A., Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma Centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020 Apr;133(1513):81–88. [PubMed] [Google Scholar]
- 37.Waseem S., Nayar S.K., Hull P., Carrothers A., Rawal J., Chou D. The global burden of trauma during the COVID-19 pandemic: a scoping review. J Clin Orthop Trauma. 2021;12(1):200–207. doi: 10.1016/j.jcot.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of emergency care provision among transfer cases pre-COVID-19 and intra-COVID-19a.