Abstract
Purpose
The COVID-19 pandemic has led to the development and worsening of eating disorder (ED) symptoms in adolescents and young adults. In order to examine COVID-19-related trends in ED care-seeking at our institution.
Methods
We used interrupted time series regression to examine pre- and postpandemic monthly summary data of the following: (1) ED-related inpatient admissions for medical stabilization; (2) ED-related hospital bed-days; (3) completed outpatient ED assessments; and (4) ED outpatient care-related inquiries at a children’s hospital in Boston, MA.
Results
Inpatient admissions, hospital bed-days, and outpatient care-related inquiries increased on average over time postpandemic compared to stable volume over time prepandemic (p < .01). Outpatient assessments decreased precipitously initially following COVID-19-related limitations, and rose quickly back to baseline.
Conclusion
These results indicate increased need for ED-related care during the pandemic. Bolstering resources to meet the needs of these vulnerable patients is critical as the effects of the pandemic continue to be felt.
Keywords: COVID-19, Eating disorders, Adolescents, Young adults
Implications and Contribution.
This study demonstrates the increasing volume of inpatient and outpatient needs in adolescents and young adults with eating disorders over time since the COVID-19 pandemic began. This is crucial information showing the necessity to expand available resources for this vulnerable population.
See Related Editorial on p.535
The COVID-19 pandemic has led to declining mental health for individuals across the globe [1,2]. Of particular concern is the pandemic’s effect on the development or worsening of eating disorders (EDs), which are associated with profound medical complications [3], high rates of comorbid psychiatric disorders [3], and elevated mortality rates [4]. For adolescents and young adults (AYAs), disruptions to routines, social isolation, and interruptions to treatment may contribute to ED-related symptomatology [5,6]. As such, new or increasing ED thoughts and behaviors such as hyper-exercising, restrictive eating, and purging have been reported in the context of the pandemic [7,8]. Worsening symptomatology increases the risk for medical complications such as hemodynamic instability, electrolyte imbalances, and rapid weight loss, which can require medical hospitalization [9].
Early identification and treatment of EDs is associated with better outcomes [10]. Development or exacerbation of ED symptomatology [6] coupled with limited treatment access during the pandemic [11] has raised concerns for the patient volume outstripping available treatment resources. This imbalance may delay care and could be detrimental to the prognosis of individuals struggling with EDs. The aim of this study is to examine pre- and postpandemic summary data of the following: (1) ED-related inpatient admissions for medical stabilization; (2) hospital bed-days for ED-related admissions; (3) completed outpatient new ED assessments; and (4) ED outpatient care-related inquiries for AYAs at a hospital in Boston, MA.
Methods
Sample and measures
Our ED program is within a tertiary care children’s hospital in Boston, MA, caring for patients approximately 8–26 years old with any ED diagnosis. Monthly summary data of ED inpatient admissions to our AYA service for medical stabilization, hospital bed-days (which reflects length of stay and census), and completed outpatient ED assessments were obtained from January 2018 to February 2021 using ICD-10 billing codes. Patient/parent inquiries (seeking advice or new appointments) were available from our outpatient quality improvement database from May 2019 to February 2021. This study was granted exemption from Boston Children’s Hospital Institutional Review Board as no patient-level data were obtained.
Analysis
The first cases of COVID-19 were identified in Boston in early March 2020. On March 18, 2020, our institution limited patient encounters to only urgent/emergent visits. Starting in July 2020, our institution gradually increased capacity for new, in-person visits. For this study, January 2018 to March 2020 is considered “prepandemic” and April 2020 to February 2021 “postpandemic.”
We examined the impact of COVID-19 restrictions on ED-related volume using interrupted time series regression. Models examined the trend in monthly volume prepandemic compared to postpandemic allowing for different slopes in the pre- and postperiods (interaction) and testing for an immediate shift following restrictions (intercept). All analyses were performed in SAS (v9.4; Cary, NC).
Results
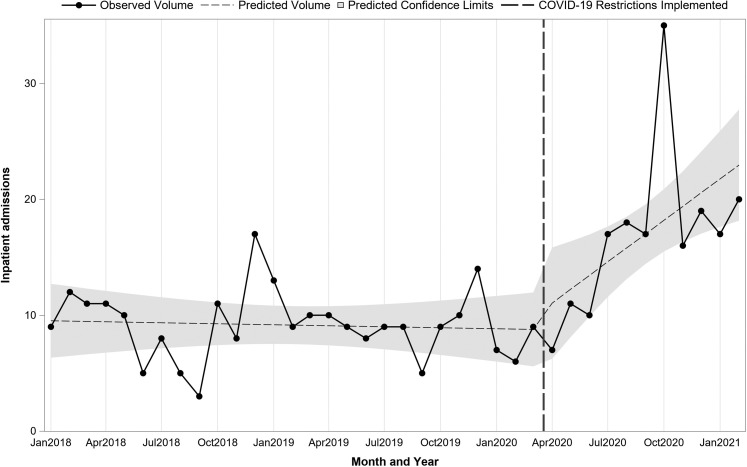
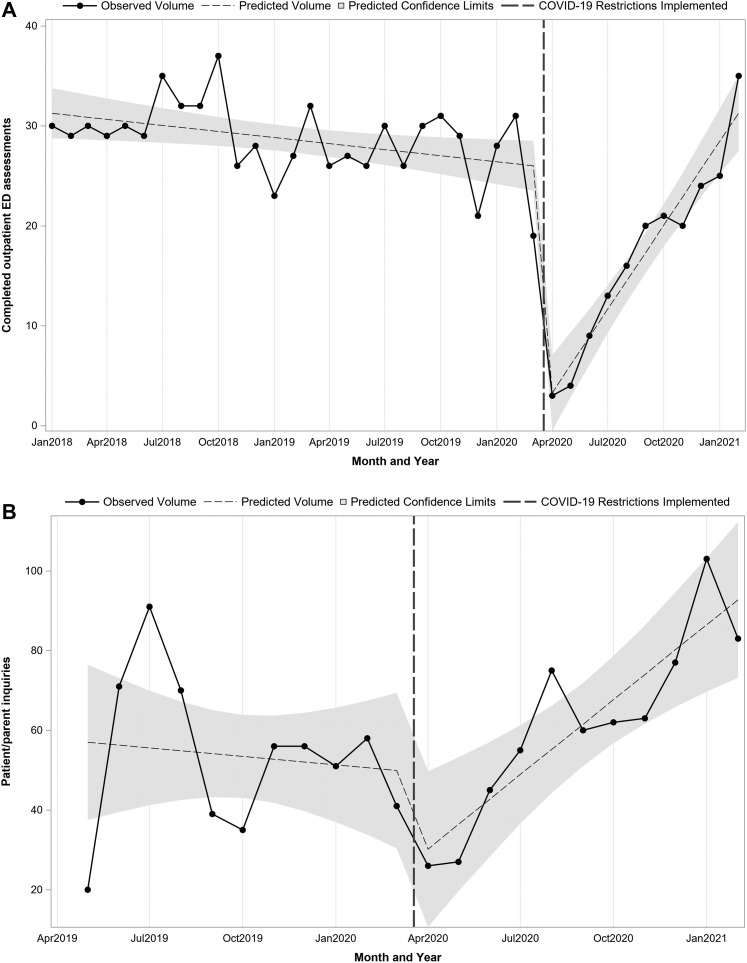
At the onset of the pandemic, there was no immediate shift in the number of inpatient ED medical admissions (intercept = 1.08, p = .73). However, postpandemic, the number of admissions per month began increasing over time (slope = 1.22, p = .006) in contrast to prepandemic when the number of admissions remained stable (slope = −.03, p = .78; Figure 1 ). Findings were similar for inpatient bed-days (postpandemic slope = 21.4, p < .001 vs. prepandemic slope = −.42, p = .74). Completed new outpatient ED assessments were decreasing slightly over time prepandemic (slope = −.20, p = .02), dropped immediately as COVID-related restrictions were implemented (intercept = −25.5, p < .001), and began to increase significantly over time as the pandemic continued (slope = 3.00, p < .001; Figure 2 A), reaching prepandemic levels at the end of 2020 and continuing to increase over time. Prepandemic, patient/parent inquiries were stable over time (slope = −.71, p = .66), while postpandemic inquiries increased significantly (slope = 6.96, p = .006) with no immediate shift (intercept = −26.0, p = .08).
Figure 1.
Monthly inpatient admissions pre- and postpandemic.
Figure 2.
Monthly completed outpatient assessments (A) and ED care-related inquiries (B), pre- and postpandemic.
Discussion
We found a significant increase in the number ED-related medical hospitalizations, hospital bed-days, and patient/parent inquiries after the onset of COVID-19, rising above our baseline totals. This finding is similar to rising hospital admissions for patients <16 years old with anorexia nervosa during the pandemic in Australia [12]. Anecdotally, the multiple hospitals that provide inpatient ED care in our area also reported increased admissions. A sensitivity analysis showed that our AYA service’s non-ED hospitalizations and bed-days were stable pre- and post-pandemic, highlighting this distinct rise in ED-related needs (data not shown). In our clinical experience, many patients report that their ED symptoms began or worsened soon after the pandemic started, consistent with growing literature describing worsening ED symptomatology during this time [[6], [7], [8]]. Our findings may represent increased incidence, prevalence, and/or acuity of EDs during the COVID-19 pandemic.
As a result of pandemic-related restrictions within our institution, our ability to complete outpatient assessments initially fell dramatically before returning to baseline. Concurrently, the rate of patient/parent inquiries increased postpandemic, reflecting rising needs. Our inability to rapidly increase outpatient assessment capacity, even with the use of telehealth, may have contributed to the increase in inquiries and hospital admissions as individuals may have decompensated to the point of needing medical stabilization due to the wait for consultative care. Additionally, pandemic-related restrictions at local ED facilities may have limited patient access to intermediate levels of therapeutic care. Therefore, availability of more multidisciplinary treatment is critical to meet the greater need. The use of technology-based interventions can be effective for early ED detection and relapse prevention [13,14]. Studies are needed to better understand the interplay of increased need, flexibility of current treatment models, efficacy of telehealth for ED treatment, and the difficulty in rapidly increasing care capacity influencing long-term ED-related outcomes.
Our findings may not be generalizable as our region experienced earlier COVID-19 spread and implementation of restrictions than most of the country. As a result, our institution may have had stricter restrictions. Additionally, patients may have experienced higher COVID-19-related anxiety related to in-person visits, reducing their willingness to seek care. We also suspect that increased hospitalizations and hospital bed-days may reflect severity of illness and/or limited availability and capacity at ED treatment facilities (e.g., residential, inpatient psychiatry). However, we were limited to summary data, and patient-level data are needed to confirm that relationship. Future directions include partnering with other programs nationally to understand the impact of COVID-19 across the U.S.
In summary, individuals with EDs require increased support during this stressful time, both in ambulatory and inpatient settings. Initially, and during the COVID-19 pandemic, services within the hospital and community programs were greatly restricted, and patients may have been reluctant to access care until their symptoms were severe. Strengthening and expanding the resources to meet the needs of these vulnerable patients is critical as the effects of the pandemic persist.
Footnotes
Sara F. Forman and Tracy K. Richmond are co-senior authors.
Conflicts of interest: There were no conflicts of interest for any of the named authors. The funding sources did not have any role in the study design, collection, analysis or interpretation or data, writing of the report, or decision to submit the manuscript for publication.
Funding Sources
This article was supported in part by the Health Resources and Services Administration of the U.S. Department of Health and Human Services as part of an MCHB T71MC00009 LEAH training grant. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.
References
- 1.Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 2.Hossain M.M., Tasnim S., Sultana A. Epidemiology of mental health problems in COVID-19: A review. F1000Research. 2020;9:636. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herpertz-Dahlmann B. Adolescent eating disorders: Update on definitions, symptomatology, epidemiology, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2015;24:177–196. doi: 10.1016/j.chc.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Arcelus J., Mitchell A.J., Wales J., Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. Arch Gen Psychiatry. 2011;68:724. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- 5.Rodgers R.F., Lombardo C., Cerolini S. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. 2020;53:1166–1170. doi: 10.1002/eat.23318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Touyz S., Lacey H., Hay P. Eating disorders in the time of COVID-19. J Eat Disord. 2020;8:19. doi: 10.1186/s40337-020-00295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Phillipou A., Meyer D., Neill E. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int J Eat Disord. 2020;53:1158–1165. doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scharmer C., Martinez K., Gorrell S. Eating disorder pathology and compulsive exercise during the COVID-19 public health emergency: Examining risk associated with COVID-19 anxiety and intolerance of uncertainty. Int J Eat Disord. 2020;53:2049–2054. doi: 10.1002/eat.23395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golden N.H., Katzman D.K., Sawyer S.M. Position paper of the Society for Adolescent Health and Medicine: Medical management of restrictive eating disorders in adolescents and young adults references. J Adolesc Heal. 2015;56:121–125. doi: 10.1016/j.jadohealth.2014.10.259. [DOI] [PubMed] [Google Scholar]
- 10.Forman S.F., Grodin L.F., Graham D.A. An eleven site national quality improvement evaluation of adolescent medicine-based eating disorder programs: Predictors of weight outcomes at one year and risk adjustment analyses. J Adolesc Heal. 2011;49:594–600. doi: 10.1016/j.jadohealth.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 11.Termorshuizen J.D., Watson H.J., Thornton L.M. Early impact of COVID-19 on individuals with self-reported eating disorders: A survey of ∼1,000 individuals in the United States and The Netherlands. Int J Eat Disord. 2020;53:1780–1790. doi: 10.1002/eat.23353. [DOI] [PubMed] [Google Scholar]
- 12.Haripersad Y.V., Kannegiesser-Bailey M., Morton K. Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Arch Dis Child. 2021;106:e15. doi: 10.1136/archdischild-2020-319868. [DOI] [PubMed] [Google Scholar]
- 13.Bauer S., Moessner M. Harnessing the power of technology for the treatment and prevention of eating disorders. Int J Eat Disord. 2013;46:508–515. doi: 10.1002/eat.22109. [DOI] [PubMed] [Google Scholar]
- 14.Barakat S., Maguire S., Smith K.E. Evaluating the role of digital intervention design in treatment outcomes and adherence to eTherapy programs for eating disorders: A systematic review and meta-analysis. Int J Eat Disord. 2019;52:1077–1094. doi: 10.1002/eat.23131. [DOI] [PubMed] [Google Scholar]