Abstract
Background
The tuberculosis targets for the UN Sustainable Development Goals (SDGs) call for a 90% reduction in tuberculosis deaths by 2030, compared with 2015, but meeting this target now seems highly improbable. To assess the economic impact of not meeting the target until 2045, we estimated full-income losses in 120 countries, including those due to excess deaths resulting from COVID-19-related disruptions to tuberculosis services, for the period 2020–50.
Methods
Annual mortality risk changes at each age in each year from 2020 to 2050 were estimated for 120 countries. This risk change was then converted to full-income risk by calculating a population-level mortality risk change and multiplying it by the value of a statistical life-year in each country and year. As a comparator, we assumed that current rates of tuberculosis continue to decline through the period of analysis. We calculated the full-income losses, and mean life expectancy losses per person, at birth and at age 35 years, under scenarios in which the SDG targets are met in 2030 and in 2045. We defined the cost of inaction as the difference in full-income losses and tuberculosis mortality between these two scenarios.
Findings
From 2020 to 2050, based on the current annual decrease in tuberculosis deaths of 2%, 31·8 million tuberculosis deaths (95% uncertainty interval 25·2 million–39·5 million) are estimated to occur, corresponding to an economic loss of US$17·5 trillion (14·9 trillion–20·4 trillion). If the SDG tuberculosis mortality target is met in 2030, 23·8 million tuberculosis deaths (18·9 million–29·5 million) and $13·1 trillion (11·2 trillion–15·3 trillion) in economic losses can be avoided. If the target is met in 2045, 18·1 million tuberculosis deaths (14·3 million–22·4 million) and $10·2 trillion (8·7 trillion–11·8 trillion) can be avoided. The cost of inaction of not meeting the SDG tuberculosis mortality target until 2045 (vs 2030) is, therefore, 5·7 million tuberculosis deaths (5·1 million–8·1 million) and $3·0 trillion (2·5 trillion–3·5 trillion) in economic losses. COVID-19-related disruptions add $290·3 billion (260·2 billion–570·1 billion) to this cost.
Interpretation
Failure to achieve the SDG tuberculosis mortality target by 2030 will lead to profound economic and health losses. The effects of delay will be greatest in sub-Saharan Africa. Affected countries, donor nations, and the private sector should redouble efforts to finance tuberculosis programmes and research because the economic dividend of such strategies is likely to be substantial.
Funding
None.
Introduction
Ending tuberculosis, a major global health threat, is widely agreed to be an attractive and important investment.1 Nonetheless, realising the UN Sustainable Development Goal (SDG) of ending the tuberculosis epidemic by 2030 now seems increasingly improbable.2 Even before the COVID-19 pandemic, there was broad scepticism that without an effective mechanism to interrupt transmission, achieving the targets would be difficult.3 Unfortunately, COVID-19 has had a profound impact on global tuberculosis programmes, interrupting routine services,4 restricting care-seeking,5 and limiting the availability of care providers and essential diagnostic products.6 Early modelling suggested that in India, Kenya, and Ukraine, a 3-month shutdown followed by a 10-month recovery period was projected to give rise to substantial additional tuberculosis burden in the next 5 years,7 adding US$1·95 billion to tuberculosis-related health spending in India, $29·43 million in Kenya, and $96·38 million in Ukraine.8 The Global Tuberculosis Report 2020 found that the 14% cumulative reduction in tuberculosis deaths from 2015 to 2019 fell far short of the 35% needed to reach the 2030 mortality target.9 Understanding the full costs and consequences of not meeting the targets is, therefore, of great importance. Moreover, a full assessment of costs strengthens the case for advanced trials and licensure of a tuberculosis vaccine, the funding for which could now be increasingly diverted towards COVID-19-related priorities. It also allows governments to carefully allocate resources that are now highly constrained.10
Research in context.
Evidence before this study
We searched PubMed for articles published between Jan 1, 2000, and Dec 31, 2020, using search terms that were broadly representative of health and economic impacts of tuberculosis, inclusive of mortality and morbidity impacts, and consequent economic and welfare losses. We excluded studies that were published in languages other than English. We found that previous macroeconomic assessments of tuberculosis treatment and control have examined the impact of specific interventions such as the directly observed treatment short-course strategy, proposed in the Global Plan to Stop TB 2006–2015. Existing studies have also sought to evaluate the effect of changing tuberculosis incidence on per-capita and per-worker gross domestic product growth. The years of life lost due to tuberculosis, as well as the effects of tuberculosis treatment on all-cause mortality, have also been previously estimated, most notably as a part of benefit–cost calculations in the Lancet Commission on investing in health. The likelihood of meeting the tuberculosis mortality targets set in the Sustainable Development Goals (SDGs) was evaluated by the Global TB Report 2020, which concluded that the cumulative reduction in tuberculosis deaths between 2015 and 2019 was 14%, less than halfway towards the 35% reduction needed. To our knowledge, no previous estimates have been made of the effects on life expectancy or full-income due to the decline in tuberculosis deaths in 120 countries from 2020 until 2050. More importantly, there are no previous estimates of the economic consequences of meeting the SDG tuberculosis mortality target, particularly on full-income, which gives a more accurate and complete picture of the value of investments in tuberculosis control efforts compared with previous studies of economic impact.
Added value of this study
To our knowledge, this is the first study to estimate full-income losses due to tuberculosis mortality in 120 countries, in 2018, and from 2020 to 2050. Moreover, it is the first to extend these estimates to assess the economic consequences of not meeting the SDG tuberculosis mortality target by 2030. The study also establishes the contribution of tuberculosis among people living with HIV and multidrug-resistant tuberculosis to economic losses. Because our economic burden estimates are supplemented by estimates of the impact on life expectancy, they provide a complementary view of the impact of tuberculosis mortality. Lastly, the study includes estimates of the excess full-income losses due to excess tuberculosis deaths resulting from COVID-19-related disruptions in 120 countries, which, to the best of our knowledge, has not been previously estimated.
Implications of all the available evidence
This study provides an assessment of the potential impact of not meeting the SDG tuberculosis mortality target by 2030, highlighting the substantial economic losses that will result from failing to achieve a 90% reduction in tuberculosis mortality (compared with 2015) until 2045 compared with achieving it in 2030. The analysis also provides some insight into how COVID-19-related-disruptions could exacerbate these losses.
The economic impact of tuberculosis has been widely studied over the past 20 years.11, 12 Tuberculosis adversely affects the labour force,13 exhausts government health budgets,14 depresses household savings,15, 16, 17 and disrupts local economies.18 However, the overall evidence on the economics of ending tuberculosis has remained heterogeneous, without a comprehensive assessment of the cost of the tuberculosis epidemic on economic welfare.1 The COVID-19 pandemic has reasserted the need to understand these broader welfare consequences of disease.
Building on the economic analysis outlined in the Lancet Commission on Tuberculosis,1 we provide a comprehensive assessment of the global economic impact of tuberculosis mortality. We use a full-income approach, which measures the impact on living standards in terms of consumption, and the added value of averting mortality, in terms of the individual valuation of the trade-off between consumption and health.19, 20 We supplement the economic assessment with an assessment of the impact on population life expectancy. Correspondingly, we calculate the economic and life expectancy dividend of achieving the SDG target of reducing tuberculosis deaths by 90% of 2015 rates by 2030,21 and the respective penalties should achievement be delayed until 2045 (the best-case plausible scenario, in line with the Lancet Commission on tuberculosis,1 even with COVID-19). We refer to this economic and life expectancy penalty as the cost of inaction, and calculate its magnitude as well as its share attributable to HIV and multidrug-resistant (MDR) tuberculosis, across 120 countries from 2020 to 2050. We present, to the best of our knowledge, the first estimate of the global economic cost of tuberculosis mortality.
Methods
Study design
We calculated gains in life expectancy22 from 2020 to 2050 in 120 countries (which accounted for 99·41% of global tuberculosis deaths in 201923), should tuberculosis deaths decline under three scenarios: at a steady 2% annually,23 referred to as the business-as-usual scenario; at a constant annual rate that allows the SDG tuberculosis mortality target to be met in 2030, and continuing on the same trajectory until 2050; or at a constant annual rate that allows the SDG tuberculosis mortality target to be met in 2045, and continuing on the same trajectory until 2050 (appendix pp 14–15). We calculated excess deaths due to COVID-19-related disruptions in tuberculosis services on the basis of a modelling analysis by Cilloni and colleagues7 (appendix p 15). We used the life tables and population projections for each country available from the World Population Prospects database of the UN Population Division.24
Procedures
We included deaths due to tuberculosis or its sequalae (International Classification of Diseases, 10th revision codes: A15–19 and B90) and deaths in people living with HIV if tuberculosis is the contributory cause,25 all of which are estimated in the Global Tuberculosis Report 2020.23 We calculated tuberculosis deaths in each World Population Prospects life table age interval, using the age distribution of tuberculosis deaths in 2018,26 which we assumed applied through 2050 for deaths due to all causes and deaths due to all causes excluding HIV. For tuberculosis deaths in people living with HIV, we used the age incidence of HIV in 2018,27 which we assumed remained constant through 2050. To model the decline in tuberculosis deaths to meet the SDG tuberculosis mortality target in 2030 and 2045, we assumed an exponential decline at a fixed average annual rate that led to deaths in these respective years being reduced to 10% of the tuberculosis deaths in 2015.
We denoted the full-income losses due to tuberculosis as V(e 0, e TB, y), where e 0 is the hazard of mortality without tuberculosis, e TB is the hazard of mortality with active tuberculosis and y is the income per capita. We transformed the excess hazard of mortality to standardised mortality units (∆SMU; a 1 in 10 000 change in mortality risk), then calculated the population value of this risk change for each country and year by multiplying the ∆SMU value by the population in each age interval (n(a)) and rescaling for the life expectancy at the age interval (e(a)) using life expectancy at age 35 years (e(35)) as the reference life expectancy. To estimate the monetary value of the risk change, we calculated the population value of the risk change at each age and then multiplied by the value of a statistical life-year (for the country and year), calculated as a proportion (γ) of the income per capita, which we modelled over the 30 years (appendix p 12).20 For a given country and year, we thus estimated V(e 0, e TB, y) as:
We calculated the value of a statistical life based on benefits transfer, by adjusting the value of a statistical life in the USA ($9 702 616) at an income of $63 280 (in purchasing power parity-adjusted international $ rates),28 assuming an income elasticity of 1·0 (1·5 considered in the sensitivity analysis).29 We calculated the present value of full-income from the perspective of 2020, assuming a discount rate of 3% (and 5% in the sensitivity analysis).30 We defined the cost of inaction as the full-income value of incremental tuberculosis deaths if the SDG tuberculosis mortality target was met in 2045 instead of 2030.
We did a probabilistic uncertainty and sensitivity analysis to evaluate the sensitivity to parameter uncertainty and choice. We sampled 5000 draws for parameter values, from uniform distributions (parameter boundaries are described in the appendix pp 15–17), using a Latin hypercube sampling algorithm.31 We additionally considered sensitivity scenarios recommended for full-income-based benefit–cost analysis.32 We estimated uncertainty in all model outputs by calculating the 2·5th, 50th, and 97·5th percentiles, denoting the interval between the 2·5th and 97·5th percentile as the 95% uncertainty interval (UI).
All calculations, including the life table calculations and sensitivity analysis, were done using Stata (IC version 14.2) and Microsoft Excel for Mac (version 16.45). We report all costs in 2018 US$ rates using exchange rates and deflator values available from the World Bank.33
Role of the funding source
There was no funding source for this study.
Results
In 2018, the 1·4 million deaths (95% UI 1·2 million–1·7 million) due to all forms of tuberculosis in 120 countries resulted in $580·1 billion (95% UI 481·9 billion–695·2 billion) in full-income losses (an average of $407 821 per tuberculosis death). The highest losses were concentrated in sub-Saharan Africa ($200·8 billion; 141·5 billion–270·4 billion). If the deaths had not occurred or had been averted within the 2018 calendar year, then an individual living in one of the 120 countries would have gained an average of 0·47 years (SD 0·74) in life expectancy at birth, and an average of 0·27 years (0·43) in life expectancy at age 35 years. In the 33 sub-Saharan African countries, the gains would have been 1·31 years (0·95) at birth and 0·77 years (0·54) at age 35 years (appendix pp 20–24).
In the 30 countries with the highest burden of MDR tuberculosis (appendix pp 6–9), 1·2 million tuberculosis deaths (95% UI 0·9 million–1·4 million) occurred in 2018, resulting in $476·5 billion (399·7 billion–566·8 billion) in economic losses (a loss of $526 735 per tuberculosis death, on average; appendix pp 20–24). 79·5% of the economic losses came from five countries: India, South Africa, Nigeria, Indonesia, and China, with India contributing 39·9%. The per-person gains in life expectancy at birth due to averting tuberculosis deaths were concentrated in ten countries (Mozambique, South Africa, Angola, Kenya, Democratic Republic of Congo, Nigeria, Papua New Guinea, Myanmar, India, and Indonesia), which accounted for almost 74% of gains in the 30 countries. In the 30 countries with the highest rates of tuberculosis–HIV co-infections (appendix pp 6–9), 224 245 tuberculosis deaths occurred, resulting in an economic loss of $96·9 billion ($407 077 per tuberculosis death, on average). Of the 30 high MDR tuberculosis burden countries, ten had economic losses exceeding 5% of the 2018 gross domestic product (GDP) and of the 30 countries with the highest tuberculosis–HIV co-infection rates, 24 countries had losses exceeding 5% of the GDP (appendix pp 20–24).
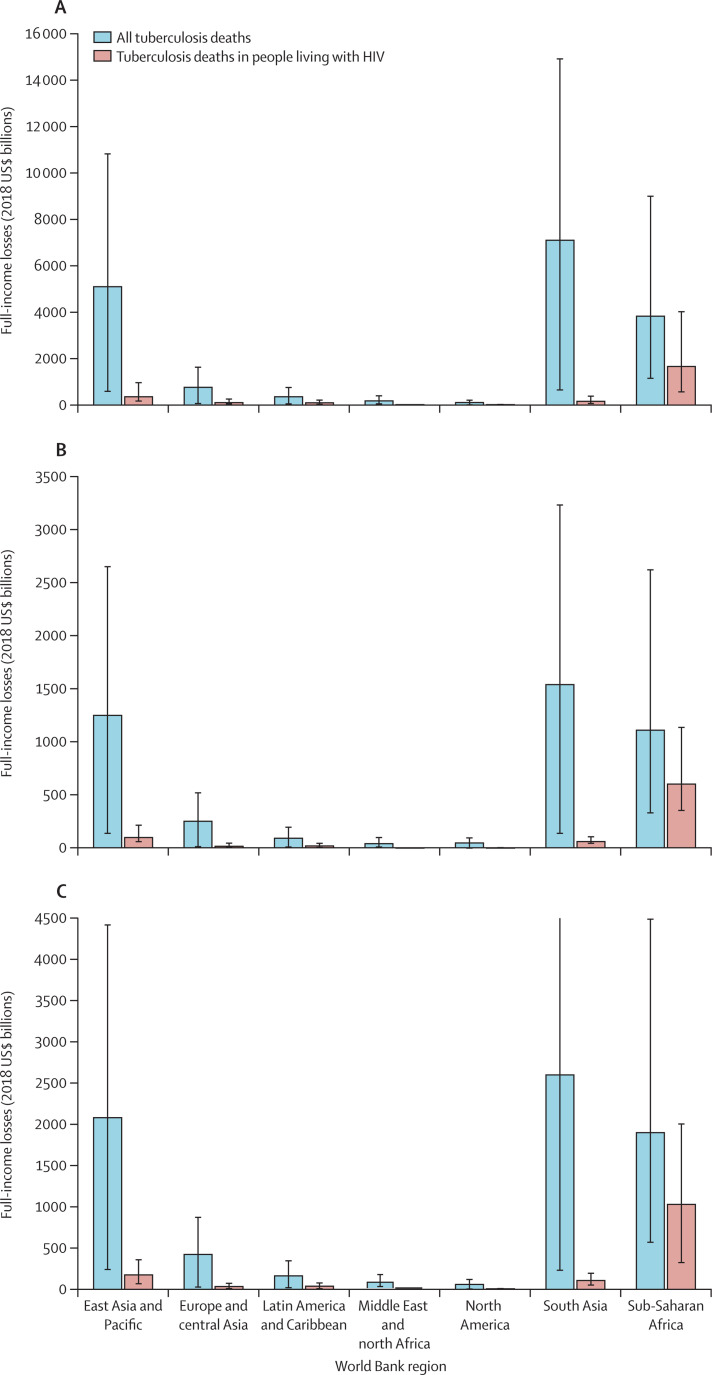
In the business-as-usual scenario, if tuberculosis deaths continue to decline at 2% annually until 2050, 31·8 million deaths (95% UI 25·2 million–39·5 million) could occur over the period 2020–50. The economic loss due to these deaths is $17·5 trillion (14·9 trillion–20·4 trillion) in 2020 (assuming a 3% discount rate and an income elasticity of 1·0). In 2030, the life expectancy benefit at birth of a 2% decline in global tuberculosis mortality would be 0·31 years (SD 0·49) on average and at age 35 years, it would be 0·17 years (0·26). The highest economic losses would be in south Asia ($7·1 trillion; 6·5 trillion–7·9 trillion). The greatest effect on life expectancy would be in sub-Saharan Africa, where on average a person would gain 0·84 years (0·64) in life expectancy in 2030 (figure 1A ; Table 1, Table 2 ).
Figure 1.
Economic losses by World Bank region in 2020–50 under three scenarios for reductions in tuberculosis mortality
(A) Business-as-usual scenario. (B) Tuberculosis mortality target met in 2030. (C) Tuberculosis mortality target met in 2045. Error bars represent 95% uncertainty intervals.
Table 1.
Mean life expectancy loss per person in 2030, at birth and at age 35 years
| East Asia and Pacific | Europe and central Asia | Latin America and Caribbean | Middle East and north Africa | North America | South Asia | Sub-Saharan Africa | Global average | |
|---|---|---|---|---|---|---|---|---|
| Life expectancy at birth | ||||||||
| Business-as-usual scenario | 0·27 (0·77) | 0·04 (0·14) | 0·08 (0·19) | 0·05 (0·15) | 0·01 (0·03) | 0·39 (0·86) | 0·84 (1·23) | 0·31 (0·49) |
| Target met in 2030 | 0·04 (0·46) | 0·01 (0·09) | 0·01 (0·15) | 0·01 (0·08) | 0·00 (0·04) | 0·06 (0·63) | 0·13 (1·38) | 0·05 (0·08) |
| Savings from meeting target in 2030 | 0·22 | 0·04 | 0·07 | 0·04 | 0·00 | 0·33 | 0·72 | 0·26 |
| Target met in 2045 | 0·13 (1·37) | 0·02 (0·24) | 0·04 (0·39) | 0·02 (0·24) | 0·00 (0·05) | 0·18 (1·99) | 0·40 (4·40) | 0·15 (0·24) |
| Savings from meeting target in 2045 | 0·14 | 0·02 | 0·04 | 0·02 | 0·00 | 0·21 | 0·44 | 0·16 |
| Cost of inaction | 0·08 | 0·01 | 0·02 | 0·01 | 0·00 | 0·12 | 0·28 | 0·10 |
| Life expectancy at age 35 years | ||||||||
| Business-as-usual scenario | 0·12 (1·36) | 0·02 (0·22) | 0·05 (0·51) | 0·02 (0·24) | 0·00 (0·03) | 0·18 (1·97) | 0·46 (5·05) | 0·17 (0·26) |
| Target met in 2030 | 0·02 (0·20) | 0·00 (0·04) | 0·01 (0·07) | 0·00 (0·03) | 0·00 (0·00) | 0·03 (0·29) | 0·07 (0·75) | 0·02 (004) |
| Savings from meeting target in 2030 | 0·11 | 0·02 | 0·04 | 0·02 | 0·00 | 0·15 | 0·39 | 0·14 |
| Target met in 2045 | 0·06 (0·62) | 0·01 (0·11) | 0·02 (0·22) | 0·01 (0·11) | 0·00 (0·01) | 0·08 (0·93) | 0·22 (2·39) | 0·08 (0·13) |
| Savings from meeting target in 2045 | 0·07 | 0·01 | 0·03 | 0·01 | 0·00 | 0·09 | 0·24 | 0·09 |
| Cost of inaction | 0·04 | 0·01 | 0·01 | 0·01 | 0·00 | 0·06 | 0·15 | 0·05 |
Data are presented as mean life expectancy loss (SD), in years, by World Bank region. Life expectancy at birth represents the average number of years that a newborn could expect to live, if he or she were subject to the age-specific mortality rates of a given period. Life expectancy at age 35 years represents the average number of years that an individual at exact age 35 years is expected to live, if he or she were subject to the age-specific mortality rates of a given period. All estimates include people living with HIV.
Table 2.
The cost of inaction in terms of tuberculosis deaths and economic losses, by World Bank region, from 2020 to 2050
|
Economic losses, 2018 $US billions |
Total economic losses, 2018 $US billions | Total tuberculosis deaths, millions | |||||||
|---|---|---|---|---|---|---|---|---|---|
| East Asia and Pacific | Europe and central Asia | Latin America and Caribbean | Middle East and north Africa | North America | South Asia | Sub-Saharan Africa | |||
| Business-as-usual scenario | 5110 (4530–5750) | 763 (706–871) | 351 (303–402) | 172 (126–223) | 100 (96–103) | 7120 (6470–7850) | 3840 (2690–5190) | 17 456 (14 921–20 389) | 31·8 (25·2–39·5) |
| Target met in 2030 | 1250 (1110–1400) | 253 (239–268) | 93 (82–104) | 43 (32–57) | 48 (47–49) | 1540 (1400–1690) | 1110 (779–1510) | 4337 (3689–5077) | 8·0 (6·3–10·1) |
| Savings from meeting target in 2030 | 3860 (3420–4350) | 510 (467–603) | 258 (220–298) | 129 (94–166) | 52 (49–54) | 5580 (5070–6160) | 2730 (1911–3680) | 13 119 (11 232–15 311) | 23·8 (18·9–29·5) |
| Target met in 2045 | 2080 (1840–2340) | 422 (396–450) | 162 (143–183) | 76 (57–101) | 58 (57–59) | 2600 (2370–2860) | 1900 (1330–2590) | 7299 (6192–8583) | 13·7 (10·8–17·2) |
| Savings from meeting target in 2045 | 3030 (2690–3410) | 341 (310–421) | 189 (160–219) | 96 (69–122) | 42 (40–44) | 4520 (4100–4990) | 1940 (1360–2600) | 10 157 (8729–11 805) | 18·1 (14·3–22·4) |
| Cost of inaction | 830 (730–940) | 169 (157–182) | 69 (61–79) | 34 (25–44) | 10 (10–11) | 1060 (970–1170) | 790 (551–1080) | 2962 (2503–3506) | 5·7 (5·1–8·1) |
The cost of inaction was computed as the difference in tuberculosis deaths and economic losses between the scenario of meeting the tuberculosis mortality target in 2030 versus meeting it in 2045. Data are presented with 95% uncertainty intervals.
By contrast, if the SDG tuberculosis mortality target were met in 2030, 8·0 million deaths (95% UI 6·3 million–10·1 million) would occur, with estimated economic losses of $4·3 trillion (3·7 trillion–5·1 trillion; figure 1B; table 2). Meeting the SDG tuberculosis mortality target in 2030 would thus avert 23·8 million deaths and $13·1 trillion in economic losses, compared with the business-as-usual scenario. Averting tuberculosis deaths in people living with HIV by meeting the 2030 SDG tuberculosis mortality target (1·8 million [22·94%] of the 8·0 million deaths) would contribute $1·6 trillion to the savings of $13·1 trillion (figure 1B; appendix pp 24–29). Moreover, by achieving the SDG tuberculosis mortality target by 2030 instead of after 2050, in 2030, a person would gain 0·26 years (SD 0·04) in life expectancy at birth on average and 0·14 years (0·02) at age 35 years (figure 1B, Table 1, Table 2). In a country such as Lesotho, a person would gain as many as 2·00 years of life expectancy at birth in 2030; in the Central African Republic, they would gain 1·85 years (table 1; appendix pp 24–29).
If the SDG tuberculosis mortality target were to be met in 2045, 13·7 million tuberculosis deaths (95% UI 10·8 million–17·2 million) would still occur between 2020 and 2050 (a reduction of 18·1 million tuberculosis deaths from the business-as-usual scenario; figure 1C; table 2). The economic losses would be $7·3 trillion (6·2 trillion–8·6 trillion; a $10·2 trillion reduction from the business-as-usual scenario). The economic losses resulting from unaverted deaths among people living with HIV between 2020 and 2045 would be $983·4 billion (809·1 billion–1150·4 billion; appendix pp 40–41). Moreover, meeting the SDG tuberculosis mortality target in 2045 would reduce potential gains in life expectancy by 0·16 years (SD 0·05) at birth in 2030 and by 0·09 years (0·03) at age 35 years, compared with the business-as-usual scenario (figure 1C, Table 1, Table 2). In Lesotho, life expectancy gains would be reduced by as much as 1·03 years; in Mozambique, they would be reduced by 0·73 years (appendix pp 33–37).
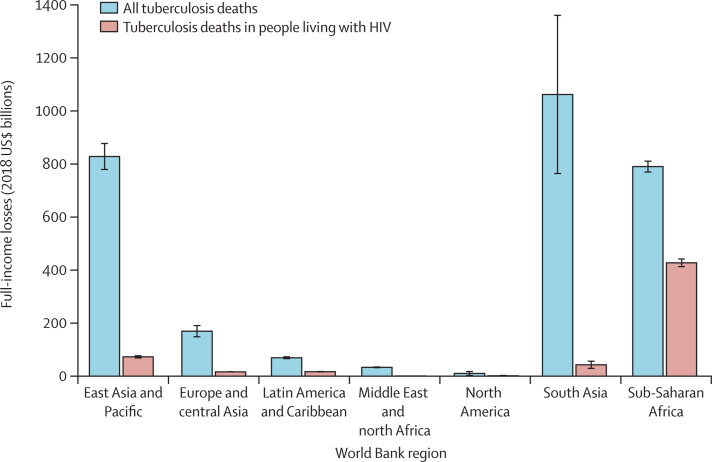
The overall cost of inaction (ie, savings from meeting the SDG tuberculosis mortality target in 2030 that would be foregone by only meeting this target in 2045) is $3·0 trillion (95% UI 2·5 trillion–3·5 trillion; 5·7 million tuberculosis deaths [5·1 million–8·1 million]; figure 2 ; table 2). The cost of inaction is highest in south Asia, including or excluding people living with HIV ($1·1 trillion including people living with HIV, $1·0 trillion excluding people living with HIV). The cost of inaction for people living with HIV is highest in sub-Saharan Africa, at $427·0 billion (54·1% of the total cost of inaction), which is nearly six times that of the next highest region (east Asia and Pacific, $74·2 billion; appendix pp 40–41). The cost of inaction in terms of life expectancy at birth across the 120 countries in 2030 is 0·10 (SD 0·01) years on average; at age 35, it is 0·05 years (0·00; figure 2, Table 1, Table 2).
Figure 2.
The cost of inaction by World Bank region
Costs represent the full-income savings from meeting the tuberculosis mortality targets in 2030 rather than in 2045. Error bars represent 95% CIs.
Disruptions to tuberculosis services due to COVID-19 will increase tuberculosis deaths until 2025,7 increasing full-income losses up to 2050 by $1·0 trillion (from $17·5 trillion [95% UI 14·9 trillion–20·4 trillion] to $18·5 trillion [3·8 trillion–33·2 trillion]). If the SDG target is not met until 2045, the cost of inaction is $3·2 trillion (1·2 trillion–5·3 trillion), which represents an increase of $290·3 billion (260·2 billion–570·1 billion) compared with the cost of inaction if no disruption to tuberculosis services had been caused by COVID-19 (appendix pp 41–42).
The uncertainty in tuberculosis deaths (14·4 million deaths in the business-as-usual scenario; 3·8 million deaths if the target is met in 2030; and 6·4 million deaths if the target is met in 2045) leads to a cost of inaction in the range of $2·5 trillion to $3·5 trillion. Probabilistic analysis suggests that in a high-burden country such as South Africa, when additionally considering the uncertainty due to the economic parameters (value of a statistical life and the choice of discount rate), the sensitivity to those parameters far outweighs the sensitivity to the uncertainty in tuberculosis deaths. In particular, if the income elasticity is allowed to vary between 0·5 and 1·5, full-income varies between $61·6 billion and $125·4 billion (range of $63·8 billion). The highest variation in full-income due to the uncertainty in tuberculosis deaths is $5·4 billion, due to the uncertainty in tuberculosis deaths at age 25–29 years (appendix pp 46–47).
At the global level, when income elasticity is allowed to vary between 0·5 and 1·5, full-income varies between $12·3 trillion and $25·6 trillion (range of $13·3 trillion). When the US value of a statistical life in 2020 is allowed to vary between its reported lower and upper bounds ($1·8 million and $17·6 million),28 full-income varies between $15 trillion and $20·9 trillion (range of $5·9 trillion). When the discount rate is allowed to vary between 3% and 5%,30 full-income varies between $16·6 trillion and $19·4 trillion (range of $2·8 trillion; appendix pp 44–45).
Discussion
Failure to meet the SDG tuberculosis mortality target by 2030 will have adverse health and economic consequences. Our estimates suggest that $3·0 trillion will be lost if the target is not met until 2045, and in 2030, an average of 0·31 years at birth and 0·17 years at age 35 years will be lost per person due to tuberculosis deaths.
Our analysis also sheds light on the geographical distribution of these global losses. First, although aggregate economic losses are highest in the south Asia and east Asia and Pacific regions, mean life expectancy losses per person, both at birth and at age 35 years are highest in sub-Saharan Africa (6–7 times the losses in the next highest region). Welfare losses due to tuberculosis disproportionately burden sub-Saharan Africa, although the effects are less apparent due to lower per-capita incomes. Second, population age structure can protract economic welfare losses over generations. In this regard, sub-Saharan Africa is also burdened because life expectancy losses in peak productive ages can deter a much anticipated demographic dividend34, 35 and depress income growth. Third, despite massive recent scale-up in HIV investment, loss of life expectancy in people living with HIV comprises as much as 50% to the cost of inaction. Estimates for 2018, which are least prone to uncertainty, suggest that countries that are more burdened by tuberculosis co-infections in patients with HIV accrue more life expectancy losses than countries more burdened by MDR tuberculosis. Lastly, excess tuberculosis deaths due to COVID-19-related disruptions are contained between 2020 and 2025, given the best available evidence to date.7 Although the associated excess welfare losses are also contained within this period, excess life expectancy losses can have a longer lasting effect.
These insights provide new evidence to guide investment in tuberculosis control. First, although full-income is a reasonable measure of broader economic welfare, it is depressed in countries with lower per-capita incomes. The share of consumption that an individual is willing to pay each year to gain an additional life-year is indeed higher when per-capita incomes are higher. Full-income also fails to capture losses due to post-tuberculosis morbidity, and the cost of mortality in individuals who received treatment and recovered.36 Life expectancy losses are a useful refinement to full-income, though not fully accounting for these deficits. Second, as much as considerations of broader welfare are important in investment decision-making, micro-level impacts on individuals and households cannot be overlooked. As two of the eight countries with the highest economic losses, 43·8% of the total tuberculosis spending in India and 51·6% in Nigeria is borne by individuals and households.14 In Indonesia, 36% of households experience catastrophic spending due to tuberculosis;37 in south India, 31% of households experience such losses.38 Third, consolidated investment in the near term will have a substantially higher impact than piecemeal investment over the longer term. Fourth, with almost 50% of economic losses in sub-Saharan Africa occurring due to the deaths of people living with HIV, investment in tuberculosis control must necessarily be separate from investment in HIV control. Lastly, although the displacement of tuberculosis funding due to COVID-19-related priorities can undoubtedly be catastrophic, with effective collaboration, smart investments, and efficient synergies, COVID-19 efforts could strengthen the global tuberculosis response and not undermine it.8
Among the limitations of our analysis, the most important is the uncertainty arising from projecting populations, deaths, and per-capita incomes over 30 years. Implicit in our assumption of a 2% annual decline in tuberculosis deaths in the business-as-usual scenario is the premise that the net effect of the drivers of tuberculosis mortality, and thereby tuberculosis incidence, is potentially declining. This is indeed the case with HIV in sub-Saharan Africa, where incidence has been declining at a steady 4% annually since 2017.27 However, in other high tuberculosis burden countries such as India, where the effect of HIV is marginal, declines in tuberculosis burden might be attributable to steady improvements in tuberculosis services,39 as well as gradual declines in determinants of tuberculosis, such as malnutrition.40 Our business-as-usual scenario essentially assumes that all of these existing trends would continue indefinitely. The uncertainty in projections is also elevated by the presence of COVID-19, which can alter the trajectory of tuberculosis mortality and disrupt secular and cyclical trends in economic growth. We accounted for the effects on tuberculosis mortality by predicting potential fluctuations due to COVID-19, but because COVID-19 is yet to diminish as a public health threat, the evidence is still evolving. Unfortunately, effects on economic trends are less amenable to statistical prediction given the scope of the study. The full-income estimates are also inherently sensitive to income elasticities,41 which inflate losses in higher-income settings.42 Our estimates are nonetheless consistent with empirical estimates of country values of a statistical life-year. In South Africa, we estimated a loss of US$1 249 279 per tuberculosis death. On average, each death incurs a loss of 33·76 years of life expectancy (the life expectancy at the median age in South Africa), suggesting a value of a (statistical) life-year of $37 005 per life-year. This estimate is approximately 4·4 times per-capita GDP in 2020 ($8429), which is in agreement with empirically measured values for sub-Saharan Africa (4·5 times the per-capita GDP).43 However, empirically established values of a statistical life are also now less reliable because the mean social valuation of mortality risk reduction is likely to be influenced by the emergence of the COVID-19 global pandemic. Our estimates also do not reflect losses due to deaths in individuals who received treatment for tuberculosis and then recovered.36 We also assumed that the age distribution of tuberculosis deaths for 2018 (age distribution of HIV for people living with HIV) remain unchanged until 2050, which adds further uncertainty.
Our analysis provides compelling evidence that the failure to act to reduce tuberculosis deaths will have major economic and demographic consequences. Although the COVID-19 pandemic has understandably diverted attention and investment in other disease control programmes, neglect of tuberculosis in particular, especially in high-burden countries, could have long-lasting economic and social effects. The current trajectory of the COVID-19 pandemic, and its effects on tuberculosis incidence, mortality, and economic losses suggest that action is needed now.
This online publication has been corrected. The corrected version first appeared at thelancet.com/lancetgh on September 21, 2021
Data sharing
All primary data used in this study are publicly available. Our analyses are summarised in the appendix (pp 20–47).
Declaration of interests
We declare no competing interests.
Contributors
MR and SS conceived the study. SS developed the economic and demographic analysis. NA provided input into the technical analysis and contributed to finalising the manuscript. RA provided input into the overall analysis and contributed to finalising the manuscript. EG contributed to finalising the manuscript. MR and SS wrote the intial draft and were responsible for all subsequent revisions. All authors approved the final submitted version. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors accessed and verified the data.
Supplementary Material
References
- 1.Reid MJA, Arinaminpathy N, Bloom A. Building a tuberculosis-free world: the Lancet Commission on tuberculosis. Lancet. 2019;393:1331–1384. doi: 10.1016/S0140-6736(19)30024-8. [DOI] [PubMed] [Google Scholar]
- 2.Floyd K, Glaziou P, Houben RMGJ, Sumner T, White RG, Raviglione M. Global tuberculosis targets and milestones set for 2016–2035: definition and rationale. Int J Tuberc Lung Dis. 2018;22:723–730. doi: 10.5588/ijtld.17.0835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Menzies NA, Gomez GB, Bozzani F. Cost-effectiveness and resource implications of aggressive action on tuberculosis in China, India, and South Africa: a combined analysis of nine models. Lancet Glob Health. 2016;4:e816–e826. doi: 10.1016/S2214-109X(16)30265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hogan AB, Jewell BL, Sherrard-Smith E. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8:e1132–e1141. doi: 10.1016/S2214-109X(20)30288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buonsenso D, Iodice F, Sorba Biala J, Goletti D. COVID-19 effects on tuberculosis care in Sierra Leone. Pulmonology. 2021;27:67–69. doi: 10.1016/j.pulmoe.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Venkatesan P. COVID-19 diagnostics—not at the expense of other diseases. Lancet Microbe. 2020;1:e64. doi: 10.1016/S2666-5247(20)30041-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cilloni L, Fu H, Vesga JF. The potential impact of the COVID-19 pandemic on the tuberculosis epidemic a modelling analysis. EClinicalMedicine. 2020;28 doi: 10.1016/j.eclinm.2020.100603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reid MJA, Silva S, Arinaminpathy N, Goosby E. Building a tuberculosis-free world while responding to the COVID-19 pandemic. Lancet. 2020;396:1312–1313. doi: 10.1016/S0140-6736(20)32138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO Global tuberculosis report 2020. 2020. http://www.who.int/tb/publications/global_report/en
- 10.Center for Global Development COVID-19 and budgetary space for health in developing economies. July 16, 2020. https://www.cgdev.org/publication/covid-19-and-budgetary-space-health-developing-economies
- 11.Laxminarayan R, Klein E, Dye C, Floyd K, Darley S, Adeyi O. Economic benefit of tuberculosis control. 2007. https://documents1.worldbank.org/curated/en/554871468175465282/pdf/wps4295.pdf
- 12.Vassall A. In: Prioritizing development: a cost benefit analysis of the United Nations' Sustainable Development Goals. Lomborg B, editor. Cambridge University Press; Cambridge: 2018. Benefits and costs of TB control for the post-2015 development agenda; pp. 255–265. [Google Scholar]
- 13.Rajeswari R, Balasubramanian R, Muniyandi M, Geetharamani S, Thresa X, Venkatesan P. Socio-economic impact of tuberculosis on patients and family in India. Int J Tuberc Lung Dis. 1999;3:869–877. [PubMed] [Google Scholar]
- 14.Su Y, Garcia Baena I, Harle AC. Tracking total spending on tuberculosis by source and function in 135 low-income and middle-income countries, 2000–17: a financial modelling study. Lancet Infect Dis. 2020;20:929–942. doi: 10.1016/S1473-3099(20)30124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan H-Q, Bele S, Feng Y. Analysis of the economic burden of diagnosis and treatment of tuberculosis patients in rural China. Int J Tuberc Lung Dis. 2013;17:1575–1580. doi: 10.5588/ijtld.13.0144. [DOI] [PubMed] [Google Scholar]
- 16.Lönnroth K, Glaziou P, Weil D, Floyd K, Uplekar M, Raviglione M. Beyond UHC: monitoring health and social protection coverage in the context of tuberculosis care and prevention. PLoS Med. 2014;11 doi: 10.1371/journal.pmed.1001693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bloom BR, Atun R, Cohen T. In: Major infectious diseases. Holmes KK, Bertozzi S, Bloom BR, Jha P, editors. The World Bank; Washington, DC: 2017. Tuberculosis; pp. 233–314. [Google Scholar]
- 18.Delfino D, Simmons PJ. Dynamics of tuberculosis and economic growth. Environ Dev Econ. 2005;10:719–743. [Google Scholar]
- 19.Nordhaus WD. The health of nations: the contribution of improved health to living standards. SSRN. 2002 https://papers.ssrn.com/abstract=302579 published online March 14. (preprint). [Google Scholar]
- 20.Jamison DT, Summers LH, Alleyne G. Global health 2035: a world converging within a generation. Lancet. 2013;382:1898–1955. doi: 10.1016/S0140-6736(13)62105-4. [DOI] [PubMed] [Google Scholar]
- 21.Uplekar M, Weil D, Lonnroth K. WHO's new end TB strategy. Lancet. 2015;385:1799–1801. doi: 10.1016/S0140-6736(15)60570-0. [DOI] [PubMed] [Google Scholar]
- 22.Preston S, Heuveline P, Guillot M. Wiley-Blackwell; Hoboken, NJ: 2000. Demography: measuring and modeling population processes. [Google Scholar]
- 23.WHO Global tuberculosis report 2019. 2019. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-report-2019
- 24.UN Department of Economic and Social Affairs World population prospects. 2019. https://esa.un.org/unpd/wpp
- 25.Glaziou P, Sismanidis C, Carel P, Floyd K. Methods used by WHO to estimate the global burden of TB disease. 2016. https://www.who.int/tb/publications/global_report/gtbr2016_online_technical_appendix_global_disease_burden_estimation.pdf
- 26.WHO Global tuberculosis report 2018. 2018. https://apps.who.int/iris/handle/10665/274453
- 27.UNAIDS AIDSinfo: new HIV infections—adults (15+) https://aidsinfo.unaids.org?did=5f0104c9629b296603d55a9b&r=world&t=2020&tb=m&bt=mnli&ts=0,0&aid=5f0106a7629b296603d55aa0&mav=Population: All adults (15+)&ml=2&mt=1.html
- 28.US Environmental Protection Agency Guidelines for preparing economic analyses. 2014. https://www.epa.gov/environmental-economics/guidelines-preparing-economic-analyses
- 29.Robinson LA, Hammitt JK, Jamison DT, Walker DG. Conducting benefit-cost analysis in low- and middle-income countries: introduction to the special issue. J Benefit Cost Anal. 2019;10(suppl 1):1–14. doi: 10.1017/bca.2019.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tan-Torres Edejer T, Baltussen R, Adam T. Making choices in health: WHO guide to cost-effectiveness analysis. 2003. http://www.who.int/choice/publications/p_2003_generalised_cea.pdf
- 31.Orwa TO, Mbogo RW, Luboobi LS. Uncertainty and sensitivity analysis applied to an in-host malaria model with multiple vaccine antigens. Int J Appl Comput Math. 2019;5:73. [Google Scholar]
- 32.Robinson LA, Hammitt JK, Cecchini M. Reference case guidelines for benefit-cost analysis in global health and development. 2019. https://cdn1.sph.harvard.edu/wp-content/uploads/sites/2447/2019/05/BCA-Guidelines-May-2019.pdf
- 33.World Bank World Bank open data: official exchange rate (LCU per US$, period average) https://data.worldbank.org/indicator/PA.NUS.FCRF
- 34.Bloom D, Canning D, Sevilla J. RAND Corporation; Santa Monica, CA: 2003. The demographic dividend: a new perspective on the economic consequences of population change. [Google Scholar]
- 35.Bloom DE, Kuhn M, Prettner K. Africa's prospects for enjoying a demographic dividend. J Demogr Economics. 2017;83:63–76. [Google Scholar]
- 36.Romanowski K, Baumann B, Basham CA, Ahmad Khan F, Fox GJ, Johnston JC. Long-term all-cause mortality in people treated for tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2019;19:1129–1137. doi: 10.1016/S1473-3099(19)30309-3. [DOI] [PubMed] [Google Scholar]
- 37.Fuady A, Houweling TA, Mansyur M, Richardus JH. Adaptation of the tool to estimate patient costs questionnaire into Indonesian context for tuberculosis-affected households. Acta Med Indones. 2018;50:3–10. [PubMed] [Google Scholar]
- 38.Muniyandi M, Thomas BE, Karikalan N. Association of tuberculosis with household catastrophic expenditure in south India. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2019.20973. [DOI] [PubMed] [Google Scholar]
- 39.Mandal S, Chadha VK, Laxminarayan R, Arinaminpathy N. Counting the lives saved by DOTS in India: a model-based approach. BMC Med. 2017;15:47. doi: 10.1186/s12916-017-0809-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Swaminathan S, Hemalatha R, Pandey A. The burden of child and maternal malnutrition and trends in its indicators in the states of India: the Global Burden of Disease Study 1990–2017. Lancet Child Adolesc Health. 2019;3:855–870. doi: 10.1016/S2352-4642(19)30273-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hammitt JK, Robinson LA. The income elasticity of the value per statistical life: transferring estimates between high and low income populations. J Benefit Cost Anal. 2011;2:1–29. [Google Scholar]
- 42.Fleurbaey M, Luchini S, Muller C, Schokkaert E. Equivalent income and fair evaluation of health care. Health Econ. 2013;22:711–729. doi: 10.1002/hec.2859. [DOI] [PubMed] [Google Scholar]
- 43.Patenaude BN, Semali I, Killewo J, Bärnighausen T. The value of a statistical life-year in sub-Saharan Africa: evidence from a large population-based survey in Tanzania. Value Health Reg Issues. 2019;19:151–156. doi: 10.1016/j.vhri.2019.07.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All primary data used in this study are publicly available. Our analyses are summarised in the appendix (pp 20–47).