Abstract
Background
The most challenging aspect of rehabilitation is the high costs of in-patient rehabilitation programs and poor continuity of care while patients are transferred to home. In this regard, numerous home-based rehabilitation programs have been developed. The purpose of this study was to investigate the effects of home-based rehabilitative programs on postural balance, walking, and quality of life in individuals with chronic hemiparetic stroke.
Design
A CONSORT-compliant randomized controlled trial.
Methods
Seventeen community-dwelling people diagnosed with a first stroke participated in this study. They randomly divided the home-based rehabilitative program (HBP) group (n = 9) and control group (n = 8). The HBP group received coordination exercises at home and the control group received clinic-based exercises. This study measured postural balance, walking, and quality of life using four outcome measures: 10-meter walk test, figure of 8 walk test, four-square step test, and 36 item short-form survey.
Results
After analysis, it was found that the HBP improved postural balance, comfortable speed, and fast speed walking, and straight and curved walking for chronic stroke. Second, clinic-based rehabilitation services improved postural balance, comfortable speed, and fast speed walking abilities in patients with chronic stroke.
Conclusion
The results of this study suggest that the HBP group received positive benefits with regard to the postural balance and walking abilities of chronic hemiparetic stroke patients compared to the clinical setting exercise program.
Keywords: home care, rehabilitation, stroke
1. Introduction
Stroke is a leading cause of permanent physical disabilities and, ultimately, death in adults, and permanent disabilities in stroke survivors face the need to improve their functional activities and quality of life for a long time, and also perhaps their life expectancy. They would experience daily struggles with physical, psychological, and financial problems in order to return to their previous social roles in life expectancy.[1,2] Another cause of the increase following the stroke was the limited resources in rehabilitation facilities. Medical costs are a burden to both patients and the healthcare policy services. Most stroke patients do not require long-term rehabilitation services because of their medical health insurance and the limited resources of the facilities.[2] Therefore, most stroke survivors leave the hospital and return to their home or community without requiring sufficient rehabilitative time for both patients and their families or caregivers to learn about their new life situations.[3]
Most studies try to facilitate strategies to decrease the high medical costs following stroke and to prepare stroke survivors for their successful return to ordinary life.[4–8] Home-based rehabilitative program (HBP) following stroke has recently been regarded as offering potential benefits compared to hospital rehabilitation.[4] There is growing rehabilitative service demand for home-based rehabilitative programs to improve disability and to integrate the community and social roles for stroke survivors.[6,7] The HBP changed from a focus on avoiding hospitalization to a focus on early discharge from care but with support from ongoing recovery by providing rehabilitation and other services in a community setting.
HBP for stroke patients has several advantages compared to care in rehabilitation centers. HBP would lower heavy medical costs and develop the efficacy of these services by using the patient's own life circumstances. HBP has been found to induce active participation of families and caregivers and compensate for the lack of interactions between patients and therapists.[5,8] The HBP would positively affect the patient's quality of life. Satisfaction with rehabilitation services is higher than that of hospital-based rehabilitation because HBP allows stroke patients to functionally practice their activities in a real environment, but within a standardized hospital environment.[9,10]
The HBP for stroke patients has three different aims: early supported discharge, replacing rehabilitation centers with home, and healthy promotion.[4] Olney et al[11] compared the outcomes achieved by two groups of people with chronic stroke, one with 10 weeks of supervised training, and one group given 1 week of supervised training to learn the program, followed by 9 weeks of unsupervised training carried out at home. Both groups made equally modest gains with regard to the indicators of motor impairment and cardiovascular risk and on physical and mental health.[11] Mayo et al subsequently designed a trial of HBP: a task-oriented exercise and walking program and a cycling regimen for a 1-year period. All patients were visited at home 13 times in 12 months and underwent regular telephone monitoring. Both groups had elements of repetitive training, but the cycling regimen was simpler, with more opportunities for continuous repetitive training. The cycle group would experience greater increases in walking ability, secondarily to developing better exercise habits and, consequently, greater gains in participation and health-related quality of life.[12] However, there is insufficient data to compare the effectiveness of HBP and clinical-based rehabilitation for chronic hemiparetic stroke patients.
This study investigated the effects of home exercise to prevent deterioration and promote physical activities as well as quality of life in patients with chronic hemiparetic stroke. The purpose of this study was to compare the effects of HBP and clinic-based rehabilitation on postural balance, walking, and quality of life in individuals with hemiparetic stroke. This study involved a coordination exercise program based on the rhythmic movements of the lower extremities as an HBP. The hypothesis of this study was that there would be a cost difference between HBP and clinical-based rehabilitation for chronic hemiparetic stroke patients.
2. Methods
This study was a pre–post control group study design with a single-blind, randomized controlled trial. This study aimed to clarify the effects of coordination exercises at home and conventional therapy in rehabilitation centers. The study protocol was approved by the Institutional Review Board and Ethics Committee of the Chosun University of Bioscience (Approval No. 2-1041055-AB-N-01-2018-14).
2.1. Participants
Seventeen people who had a diagnosis of first stroke participated in this study. The inclusion criteria were as follows: an adult with
-
1.
community-dwelling after discharge from rehabilitation centers;
-
2.
duration post-stroke of 24 months or above;
-
3.
no cognitive impairment (i.e., a Mini-Mental State Examination score of 24 or higher);
-
4.
50-meter walking ability, with or without assistive devices; and
-
5.
a functional independence measure score of 88 or higher at the time of discharge.
This study excluded those who
-
1.
were diagnosed with other diseases or pathologies, except the first stroke affecting postural balance and gait,
-
2.
consciousness level was >0; aphasia, ≥2; and unilateral neglect of ≥2 in the NIH stroke scale questionnaire.
This study also excluded those who participated in similar studies within the last 6 months. Table 1 shows the common clinical characteristics of the participants (Table 1).
Table 1.
Rehabilitation Frame of the home-based limb coordination exercise.
| Sessions | Descriptions |
| Session #1 | Visit to the physical therapist |
| Test and measure of physical function and activities limitations | |
| Video recording of physical performance abilities | |
| Set the expected goals of the patient | |
| Session #2 | Visit to the physical therapist to educate patient regarding the coordination exercise |
| Exercise positions: supine, sidelying, half standing, and standing against wall | |
| Exercise modes: ①flexion, adduction, and lateral rotation on the left shoulder joint with extension, abduction, and medial rotation on the right hip joint, ②extension, abduction, and medial rotation on the right hip joint with flexion, adduction, and lateral rotation on the left hip joint | |
| Exercise intensity: hold for 7 s/1 time/3 sets and rest for 10 s. Rest 1 minute after transfer position. | |
| Education for patients and family or care-giver as to the exercise. | |
| Video call and supervision when requested by family or care-giver | |
| Session #3 to #5 | Repeat the exercise of session #2 with the patient's family or care-giver |
| Sessions #6 | Tele-counseling and supervision, and repetition of the exercise of session #2 with the patient's family or care-giver |
| Session #7 to #10 | Repeat the exercise of session#2 with the patient's family or care-giver |
| Session #11 | Visit to the physical therapist to supervise the patients and their family or care-giver |
| Correct the wrong exercise methods | |
| Checking the patient's complaints | |
| Checking activity limitations in the house and suggest solutions | |
| Session #12 to #15 | Repeat the exercises of session 2 with the patient's family or care-giver |
| Session #16 | Tele-counseling and supervision, and repetition of the exercise of session 2 with the patient's family or care-giver |
| Session #17 to #20 | Repeat the exercise of session 2 with the patient's family or care-giver |
| Session #21 | Tele-counseling and supervision, and repetition of the exercise of session#2 with the patient's family or care-giver |
| Session #22 to #25 | Repeat the exercise of session #2 with the patient's family or care-giver |
| Session #26 | Tele-counseling and supervision, and repetition of the exercise of session#2 with the patient's family or care-giver |
| Session #27 to #30 | Repeat the exercise of session #2 with the patient's family or care-giver |
2.2. Procedure
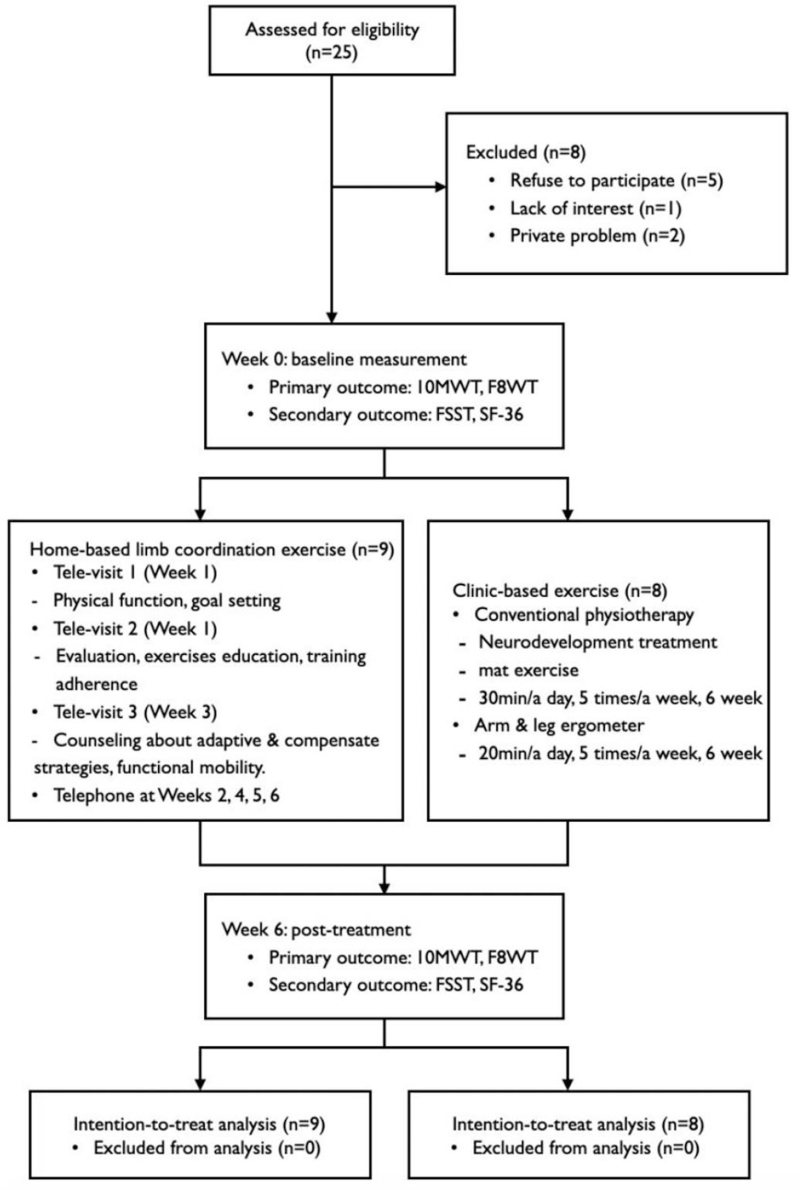
The study was conducted from March 27, 2018 to March 26, 2019. After approval from the Institutional Review Board and Ethics Committee of the C University of Bioscience, notice calling for participants was posted on the bulletin boards of the rehabilitation centers and local community centers. There were 25 people who read the notice and wanted to participate in the study. Eight people of them withdrew from the study (five people refused to participate, one person lacked interest, and two had private problems) after hearing the researcher's explanation of the detailed purpose and procedure of the study. Finally, seventeen individuals participated in this study; they were randomly divided into two groups (HBP group, n = 9 and control group, n = 8) using Excel with randomize tool, after signing the study consent spontaneously (Fig. 1).
Figure 1.
Flow diagram of the study. The figure illustrates the study processing through the phases of a parallel randomized trial of two groups.
G∗Power 3.1 program was used to perform a priori power analysis for this study taking Wilcoxon–Mann–Whitney test (two groups) for the validation of the measurement model. The required power was set at 1 − β = 0.80, and level of significance was kept at α = 0.05. The total sample size of n = 16 was needed for this study. Therefore, this study tried to recruit 20 participants, but only 17 participants who met the inclusion and exclusion criteria of the study could be collected.
The HBP group conducted coordination exercises for the lower extremities at home for 6 weeks with visiting rehabilitative service-providers (they were visited by a physical therapist on the first and the third week) and tele-rehabilitative services (on the second, fourth, fifth, and sixth weeks), while the control group received conventional therapy for the same period of time. This study measured postural balance, walking, and quality of life using the 10 meter walk test (10MWT), figure of 8 walk test (F8WT), four-square step test (FSST), and 36 item short-form survey (SF-36), answered by the participants before and after the intervention period. Figure 1 shows the flow diagram of this study through the phases of a parallel randomized controlled trial of two different groups from enrolment to data analysis (Fig. 1). All testing and intervention procedures were conducted by three physical therapists (HR, LL, and EK), except for the researchers in this study.
2.3. Intervention
In this study, HBP, which involved two different strategies, including visiting rehabilitation service and tele-rehabilitation service five times per week for 6 weeks, was conducted. The HBP consisted of coordination exercises for the lower extremities and augmented feedback. Before starting therapeutic intervention in the first week, a physical therapist visited the patient's home and interviewed the patient to determine their body function and activity limitations. After discussing the patient's desired level of rehabilitation expectations, the therapist set therapeutic goals through goal attainment scaling. The therapist measured the postural balance, walking, and quality of life of the participants and recorded the participant's home environment and physical performance through a video recording.
On the second home visit for the intervention at home, the therapist instructed the participant to perform coordination exercises in the home environment. The participant conducted coordination exercises for the upper and lower extremities in four positions: supine, side-lying, half-standing, and standing on the wall. The coordination exercises involved shoulder and hip joint exercises: flexion, adduction, and lateral rotation of the left shoulder joint with extension, abduction, and medial rotation of the right hip joint; and extension, abduction, and medial rotation of the right hip joint with flexion, adduction, and lateral rotation of the left hip joint. Table 1 shows detailed explanations of the exercise protocols. Exercise progression was performed at an intensity of 11 to 15 among Borg 6 to 20 grades. The therapist also recorded a video of the patient's exercise performance during the second visit. On the third visit, the therapist educated the participant based on his/her problems that conformed throughout the video recordings of the first and second visits. The caregiver recorded the patient's exercise status.
Clinic-based exercises at rehabilitation outpatient centers were conducted for the control group five times per week for 6 weeks. The program, consisting of neurodevelopment therapy and mat training, was conducted in a 1:1 ratio with a physical therapist for 30 minutes each session. The mat program consisted of mobility tasks, including posture maintenance and transfer. The upper and lower ergometers were devices equipped tools to determine speed, distance, and heart rate. The target threshold for training was set to 50% to 70% of the maximum age-predicted heart rate based on the stress test.[13]
2.4. Outcome measures
Measurements were made in this study using four different outcome tools: 10MWT, F8WT, FSST, and SF-36. The 10MWT is a functional evaluation tool that can be easily used in clinical practice. The 14-meter straight line distance between two points was marked and presented, and the participants walked this distance at a comfortable and fast speed. Considering the initial acceleration and the last deceleration, the first 2 m and the last 2 m were excluded from the measurement. The walking time for a 10-meter distance was repeatedly measured three times, and the mean value was selected for analysis. The verbal instruction for walking at a comfortable pace was, “If I say start, walk at a comfortable pace until I say to stop.” The instruction for high-speed walking was, “If I say start, walk at the fastest speed as possible until I tell you to stop.” In the 10-meter walking speed test, the reliability was r = 0.89–1.00 between the measurers and within the measurer.[14] The test-retest reliability was 0.93.[15]
The F8WT is designed to measure straight and curved walking abilities.[16] Before performing the figure-8 walk, the therapist verbally explained to the participant how to know the test method. In the F8WT, the participant is asked to walk around two cones, following a figure eight shape. The overall length of the F8WT is 1.5 m and the width is 1.2 m. The distance between the two obstacles is 1.52 m. Scores in three areas—speed, amplitude, and accuracy—are recorded. This study measured walking speed for scoring. The test–retest reliability of F8WT speed in stroke patients was reported as ICC = 0.94–0.99.[17]
The FSST is a tool for measuring dynamic stability and the ability of the participant to step over low objects forward, sideways, and backward.[18] Four canes, 2.5 cm high and 80 cm long, were placed on the floor in a cross shape, to make a square. The participant was required to sequentially step over four canes in a cross configuration on the ground. At the start of the test, the participant stood in square 1, facing square 2. The goal of the test is to step as fast as possible into each square with both feet in a clockwise to counterclockwise sequence. The time starts when the first foot contacts the floor in square 2 and finishes when the last foot comes back to touch the floor in square 1. The therapist instructed the participants to “try to complete the sequence as quickly and safely as possible without touching the sticks. Both feet must make contact with the floor in each square. If possible, face forward during the entire sequence.” Two trials were performed, and the better time was recorded as the participant's score. If the participant's time recorded was more than 15 seconds, the risk of falls was judged to be high. The test was reported to have good intrarater and interrater reliability in persons with chronic stroke, to assess dynamic standing balance.[19,20]
The SF-36 is an oft-used, well-researched, self-reported measure of health, and comprises 36 questions that cover eight domains of health: limitations in physical, social, and usual role activities, bodily pain, general mental health, vitality, and general health perceptions. The tool was used to measure the participant's quality of life. Participants were asked to fill out the questionnaire by themselves. It should be done in comparison to the overall score, and the total score indicates a range of low to high quality of life. The validity of the SF-36 was found have a Cronbach’ s alpha value of 0.92 to 0.93, and the test–retest reliability was 0.71 to 0.89.[21–23]
2.5. Data analysis
To examine the normal distribution in all correcting data, this study used the Shapiro–Wilks test. The data did not meet the normal distribution because of small sample sizes; thus, this study selected nonparametric tests. Differences in demographic information, HBP, and clinic-based exercise were evaluated using the Mann–Whitney U test. The Wilcoxon signed-rank test was performed to determine the differences between the pre-test scores and post-test scores of the two groups. The Mann–Whitney U test was performed between the experimental and control groups to determine the differences between the two groups. The analyses were performed using IBM SPSS for Windows (version 22.0; IBM Co., Armonk, NY). The level of significance was set at P = .05.
3. Results
The general characteristics of the two groups are presented in Table 2. The HBP group had a mean age of 70.11 years, was composed of five males and four females, and had a mean post-disease duration of 62.77 months, six had left hemiparesis while three had right hemiparesis, four had infarctions, and five had hemorrhages. The control group had a mean age of 68.52, was composed of five males and three females, had mean post-disease duration of 45.12 months, four had left hemiparesis while the other four had right hemiparesis, four had infarctions, and four had hemorrhages. There was no significant difference between the groups in any of the general characteristics.
Table 2.
Demographic and clinical characteristics of the subjects (N = 17).
| Characteristics | HBP group (n = 9) | Control group (n = 8) | Z | P |
| Age (years) | 70.11 ± 6.51∗ | 68.62 ± 9.10 | −0.048 | .962 |
| Height (cm) | 163.55 ± 6.32 | 164.25 ± 7.79 | −0.243 | .808 |
| Weight kg) | 62.77 ± 8.48 | 62.96 ± 13.07 | −0.193 | .847 |
| Onset (months) | 62.77 ± 7.99 | 45.12 ± 12.06 | −0.725 | .469 |
| Sex (male/female) | 5/4 | 5/3 | −0.282 | .778 |
| Hemi-side (Left/Right) | 6/3 | 4/4 | −0.676 | .499 |
| Injury (Infarction/Hemorrhage) | 4/5 | 4/4 | −0.222 | .824 |
HBP = home-based rehabilitation program.
Mean ± standard deviation.
3.1. Comparison of postural balance, walking abilities, and quality of life between pre-test and post-test
Significant differences in postural balance, walking abilities, and quality of life between the pre-test and post-test are shown in Table 3. In the HBP group, 10MWT scores on comfortable speed (median value 39.00 to 33.00), 10MWT on fast speed (median value, 36.00 to 29.00), F8WT speed (median value 30.00 to 22.00), F8WT step (median value 30.00 to 24.00), and FSST median value (36.00 to 33.00) were significantly different between the pre-test and post-test (P < .05). In the control group, 10MWT on comfortable speed (median value 27.88 to 22.25), 10MWT at fast speed (median value, 24.34 to 19.32), F8WT speed (median value 34.39 to 30.00), and F8WT step (median value 31.00 to 24.50) were significantly different between the pre-test and post-test (P < .05). However, the scores of SF-36 were not significantly different between the pre-test and post-test in both groups, and there was no significance difference between the control group's pre-test and post-test with regard to the FSST scores (P > .05).
Table 3.
Differences in postural balance, walking abilities, and quality of life between pre-intervention and post-intervention (N = 17).
| HBP group (n = 9) | Control group (n = 8) | |||||||
| Variable | Pre-intervention | Post-intervention | Z | P | Pre-intervention | Post-intervention | Z | P |
| 10-MWT (C)(m/s) | 39.00 (10.57–43.07)∗ | 33.00 (9.93–40.67) | −2.666 | .008 | 27.88 (11.35–40.95) | 22.25 (12.14–36.87) | −1.960 | .050 |
| 10-MWT (F)(m/s) | 36.00 (9.15–40.89) | 29.00 (9.21–34.00) | −2.073 | .038 | 24.34 (9.69–39.46) | 19.32 (9.83–35.63) | −2.380 | .017 |
| F8WT speed (second) | 30.00 (17.41–34.66) | 22.00 (10.49–26.50) | −2.668 | .008 | 34.39 (22.64–37.58) | 30.00 (18.48–36.02) | −2.240 | .025 |
| F8WT step (number) | 30.00 (25.50–33.50) | 24.00 (17.00–25.00) | −2.673 | .008 | 31.00 (28.75–34.25) | 24.50 (24.00–30.75) | −2.176 | .030 |
| FSST (second) | 36.00 (18.97–41.00) | 33.00 (17.04–39.00) | −2.524 | .012 | 36.19 (23.85–49.33) | 34.65 (22.80–46.61) | −1.400 | .161 |
| SF-36 | ||||||||
| Physical component scale | (43.13−57.50) | (33.13−62.81) | −0.237 | .813 | 47.81 (37.19−65.31) | 42.19 (43.82−71.58) | −0.700 | .484 |
| Mental component scale | (36.30–55.99) | (41.30–56.40) | −0.533 | .594 | 49.42 (49.40–67.89) | 59.32 (35.15–63.59) | −0.280 | .779 |
Median (25% interquartile range, 75% interquartile range). 10-MWT (C), 10-Meter Walk Test with comfortable; 10-MWT (F), 10-Meter Walk Test with fast; F8WT, Figure of 8 Walk Test; FSST, Four Square Step Test; SF-36, Short-Form 36 Health Survey. https://3months.tistory.com/127.
3.2. Comparison of postural balance, walking abilities, and quality of life between experimental and control groups
Table 4 shows the changeable values between the pre-test and post-test in both groups. The F8WT speed score was significantly different between the HBP group (median changeable value −6.74) and control group (median changeable value −2.00). However, the scores of 10MWT-comfortable speed, 10MWT-fast speed, F8WT step, FSST, and SF-36 were not significantly different between the two groups.
Table 4.
Comparison of changeable value between pre-test and post-test in postural balance, walking abilities and quality of life in the participants (N = 17).
| Variable | HBP group (n = 9) | Control group (n = 8) | Mann–Whitney U value | Z | Exact Sig. (two-tailed) |
| 10MWT (C)(m/s) | −5.20 (−8.00 to −0.57)∗ | −4.27 (−6.17 to 0.01) | 29.00 | −0.674 | 0.541 |
| 10-MWT (F)(m/s) | −1.11 (−9.50 to −0.85) | −3.29 (−6.30 to −0.44) | 28.00 | −0.770 | 0.481 |
| F8WT speed (second) | −6.74 (−8.67 to −5.74) | −2.00 (−8.19 to −0.21) | 14.00 | −2.118 | 0.036 |
| F8WT step (number) | −8.00 (−11.00 to −5.50) | −4.50 (−6.75 to −1.25) | 19.50 | −1.597 | 0.114 |
| FSST (second) | −2.60 (−4.28 to −1.00) | −1.54 (−1.59 to −1.04) | 24.00 | −1.158 | 0.277 |
| SF-36 | |||||
| Physical component scale | −0.63 (−4.37 to 9.06) | −3.44 (−17.18 to 9.37) | 29.50 | −0.626 | 0.541 |
| Mental component scale | −4.06 (−23.34 to −14.68) | −2.71 (−13.69 to 12.71) | 33.00 | −0.288 | 0.815 |
Median (25% interquartile range, 75% interquartile range).
10-MWT (C), 10-Meter Walk Test with comfortable; 10-MWT (F), 10-Meter Walk Test with fast; F8WT, Figure of 8 Walk Test; FSST, Four Square Step Test; SF-36, Short-Form 36 Health Survey.
4. Discussion
This study examined the effects of HBP on postural balance, walking ability, and quality of life compared with clinic-based rehabilitation services for chronic hemiparetic stroke. The main findings were as follows: first, HBP improved postural balance, comfortable speed, and fast speed walking, and straight and curved walking in patients diagnosed with chronic stroke. Second, clinic-based rehabilitation services improved postural balance, comfortable speed, and fast speed walking abilities in patients diagnosed with chronic stroke. Finally, there was no significant difference in postural balance and walking abilities, except for straight and curved walking speeds, between the HBP and clinic-based rehabilitation services for chronic stroke.
Nor Azlin et al studied the effectiveness of home-based carer-assisted therapy in comparison to hospital-based therapist-delivered therapy for community-dwelling stroke survivors.[24] They reported that home-based carer-assisted therapy is as effective as hospital-based therapist-delivered training in improving post-stroke functions and quality of life. Hsieh et al investigated the treatment effects of a home-based rehabilitation program compared to clinic-based rehabilitation in patients with stroke.[25] They reported that the home- and clinical-based rehabilitation groups had comparable benefits with regard to the outcomes of impairment level but showed differential effects on the outcomes of activity and participation levels. The results of this study showed that providing HBP through coordination exercises is both less costly and more effective than hospital-based rehabilitative approaches. This study did not investigate the medical expenses paid by study participants during the study period. However, the HBP group did not visit the hospital, so it would have had less hospital charges than the control group. An advantage of the HBP in this study is that all exercises are performed in the patient's home and are familiar to the patient. The factors responsible for these results in tele-supervision may include the possibility of creating an individualized program that offers support and close follow-up in a home environment.
The central pattern generator in the spinal cord is a neural circuit composed of inhibitory and excitable interneurons that can perform rhythmic movements. A rhythmic limb exercise similar to a normal gait pattern is helpful in improving gait abilities.[26] The principle of specificity states that the effect of motion is maximized when there is similarity of the external structure of motion, that is, the angle of the joint, the speed of motion of the joint, and similarity of force applied. The motion included in the limb coordination exercise promotes the rhythmic movement of the neural network through alternating limb movements while keeping the head straight. It is thought that rhythmic movement stimulates neural circuits to enhance the mechanical coupling between trunk and leg movements, resulting in improved trunk movement.[27] The limb coordination exercise and ergometer, which were practiced similarly to the movements that occur during gait pattern, are considered to have contributed to the improvement of walking abilities. This study conducted coordination exercises for the lower limbs as part of the HBP to improve postural balance and walking abilities. The results of this study showed that HBP improved postural balance and walking abilities.
This study examined the effects of HBP on postural balance, walking ability, and quality of life in stroke patients. The HBP has positive benefits for postural balance, walking ability, and quality of life in the same way a clinic-based rehabilitation approach does. This study is limited in that it only examines the outcomes of small sample sizes. This study did not establish the optimal treatment intensity of HBP. It is important to assess the cost-effectiveness of home-based rehabilitation in future applications. Further studies are needed to compare treatment effects in patients with subacute stroke. The HBP of this study involved coordination exercises for the upper and lower extremities. In future studies, it will be necessary to apply an exercise that combines coordination, resistance, and aerobic exercise to reduce activity limitations and participation restrictions. This study also did not measure medical expenditure or community-dwelling activities. This will also be the content to be pursued in future research. The HBP would be another benefit to integrate the community-dwelling and is one of the safe exercise programs that can be carried out through self-directed learning. The spontaneity of a patient is very important in the rehabilitation field. Therefore, various HBPs should be planned and carried out in the future.
Author contributions
Conceptualization: Hye-Sun Lee, Chiang-soon Song.
Data curation: Jae-Heon Lim, Chiang-soon Song.
Formal analysis: Jae-Heon Lim, Hye-Sun Lee, Chiang-soon Song.
Investigation: Jae-Heon Lim, Hye-Sun Lee, Chiang-soon Song.
Methodology: Jae-Heon Lim, Chiang-soon Song.
Project administration: Chiang-soon Song.
Resources: Jae-Heon Lim, Chiang-soon Song.
Software: Jae-Heon Lim, Chiang-soon Song.
Supervision: Hye-Sun Lee, Chiang-soon Song.
Validation: Hye-Sun Lee, Chiang-soon Song.
Visualization: Jae-Heon Lim, Chiang-soon Song.
Writing – original draft: Chiang-soon Song.
Writing – review & editing: Jae-Heon Lim, Hye-Sun Lee, Chiang-soon Song.
Footnotes
Abbreviations: 10MWT = 10 meter walk test, F8WT = figure of 8 walk test, FSST = four-square step test, HBP = Home-based rehabilitative programs, SF-36 = 36 item short-form survey.
How to cite this article: Lim JH, Lee HS, Song CS. Home-based rehabilitation programs on postural balance, walking, and quality of life in patients with stroke: a single-blind, randomized controlled trial. Medicine. 2021;100:35(e27154).
This study was supported by research fund from Chosun University, 2019.
The authors have no conflict of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Feigin, Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009;8:355–69. [DOI] [PubMed] [Google Scholar]
- [2].Nor Azlin MN, Aziz NA, Saperi BS, Aljunid SM. Functional limitation and health-related quality of life, and associated factors among long term stroke survivors in a Malaysian community. Med J Malaysia 2016;71:313–21. [PubMed] [Google Scholar]
- [3].Aziz AFA, Aziz NAA, Nordin NAM, Ali MF, Sulong S, Aljunid SM. What is next after transfer of care from hospital to home for stroke patients? Evaluation of a community stroke care service based in a primary care clinic. J Neurosci Rural Pract 2013;4:413–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Mayo NE. Stroke rehabilitation at home. Stroke 2016;47:1685–91. [DOI] [PubMed] [Google Scholar]
- [5].Peirone E, Goria PF, Anselmino A. A dual-task home-based rehabilitation programme for improving balance control in patients with acquired brain injury: a single-blind, randomized controlled pilot study. Clin Rehabil 2014;28:329–38. [DOI] [PubMed] [Google Scholar]
- [6].Rezaei M, Sharifi A, Vaccaro AR, Rehimi-Movaghar V. Home-based rehabilitation programs: promising field to maximize function of patients with traumatic spinal cord injury. Asian J Neurosurg 2019;14:634–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Tousignant M, Corriveau H, Kairy D, et al. Tai-Chi-based exercise program provided via telerehabilitation compared to home visits in a post-stroke population who have returned home without intensive rehabilitation: study protocol for a randomized, non-inferiority clinical trial. Trials 2014;15:42.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Van der Veen DJ, Dopp CME, Siemonsma PC, et al. Factors influencing the implementation of home-based stroke rehabilitation: professionals’ perspective. PLoS One 2019;14:e0220226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Doig E, Fleming J, Kuipers P, Cornwell PL. Comparison of rehabilitation outcomes in day hospital and home settings for people with acquired brain injury—a systematic review. Disabil Rehabil 2010;32:2061–77. [DOI] [PubMed] [Google Scholar]
- [10].Turton AJ, Cunningham P, van Wijck F, et al. Home-based reach-to-grasp training for people after stroke is feasible: a pilot randomized controlled trial. Clin Rehabil 2017;31:891–903. [DOI] [PubMed] [Google Scholar]
- [11].Olney SJ, Nymark J, Brouwer B, et al. A randomized controlled trial of supervised versus unsupervised exercise programs for ambulatory stroke survivors. Stroke 2006;37:476–81. [DOI] [PubMed] [Google Scholar]
- [12].Mayo NE, MacKay-Lyons MJ, Scott SC, Moriello C, Brophy J. A randomized trial of two home-based exercise programmes to improve functional walking post-stroke. Clin Rehabil 2013;27:659–71. [DOI] [PubMed] [Google Scholar]
- [13].Gordon NF, Gulanick M, Costa F, et al. Physical activity and exercise recommendations for stroke survivors: an American Heart Association scientific statement from the council on clinical cardiology, subcommittee on exercise, cardiac rehabilitation, and prevention; the council on cardiovascular nursing; the council on nutrition, physical activity, and metabolism; and the stroke council. Circulation 2004;109:2031–41. [DOI] [PubMed] [Google Scholar]
- [14].Fulk GD, Echternach JL. Test-retest reliability and minimal detectable change of gait speed in individuals undergoing rehabilitation after stroke. J Neurol Phys Ther 2008;32:08–13. [DOI] [PubMed] [Google Scholar]
- [15].Salbach NM, Mayo NE, Higgins J, et al. Responsiveness and predictability of gait speed and other disability measures in acute stroke. Arch Phys Med Rehabil 2001;82:1204–12. [DOI] [PubMed] [Google Scholar]
- [16].Hess RJ, Brach JS, Piva SR, et al. Walking skill can be assessed in older adults: validity of the figure-of-8 walk test. Phys Ther 2010;90:89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wong SST, Yam M-S, Ng SSM. The figure-of-eight walk test: Reliability and associations with stroke-specific impairments. Disabil Rehabil 2013;35:1896–902. [DOI] [PubMed] [Google Scholar]
- [18].Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 2002;83:1566–71. [DOI] [PubMed] [Google Scholar]
- [19].Blennerhassett JM, Jayalath VM. The four square step test is a feasible and valid clinical test of dynamic standing balance for use in ambulant people poststroke. Arch Phys Med Rehabil 2008;89:2156–61. [DOI] [PubMed] [Google Scholar]
- [20].Goh EY, Chua SY, Hong SJ, Ng SS. Reliability and concurrent validity of four square step test scores in subjects with chronic stroke: a pilot study. Arch Phys Med Rehab 2013;94:1306–11. [DOI] [PubMed] [Google Scholar]
- [21].Anderson, Anderson C, Rubenach S, et al. Home or hospital for stroke rehabilitation? Results of a randomized controlled trial: I: health outcomes at 6 months. Stroke 2000;31:1024–31. [DOI] [PubMed] [Google Scholar]
- [22].Han CW, Lee EJ, Iwaya T, et al. Development of the Korean version of short-form 36-item health survey: Health related qol of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med 2004;203:189–94. [DOI] [PubMed] [Google Scholar]
- [23].Lins L, Carvalho F. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016. Published online 2016;4:2050312116671725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Nor Azlin MN, Aziz NA, Sulung S, Aljunid SM. Effectiveness of home-based carer-assisted in comparison to hospital-based therapist-delivered therapy for people with stroke: a randomized controlled trial. Neurorehabil 2019;45:87–97. [DOI] [PubMed] [Google Scholar]
- [25].Hsieh YW, Chang KC, Hung JW, Wu CY, FU MH, Chen CC. Effects of Home-based versus clinic-based rehabilitation combining mirror therapy and task-specific training for patients with stroke: a randomized crossover trial. Arch Phys Med Rehabil 2018;99:2399–407. [DOI] [PubMed] [Google Scholar]
- [26].Minassian K, Hofstoetter US, Dzeladini F, Guertin PA, Ijspeert A. The human central pattern generator for locomotion: does it exist and contribute to walking? Neuroscientist 2017;23:649–63. [DOI] [PubMed] [Google Scholar]
- [27].Haghpanah SA, Farahmand F, Zohoor H. Modular neuromuscular control of human locomotion by central pattern generator. J Biomech 2017;53:154–62. [DOI] [PubMed] [Google Scholar]