Summary
Background: Coronavirus Disease (COVID-19) is currently spreading exponentially around the globe. Various digital health technologies are currently being used as weapons in the fight against the pandemic in different ways by countries. The main objective of this review is to explore the role of digital health technologies in the fight against the COVID-19 pandemic and address the gaps in the use of these technologies for tackling the pandemic.
Methods: We conducted a scoping review guided by the Joanna Briggs Institute guidelines. The articles were searched using electronic databases including MEDLINE (PubMed), Cochrane Library, and Hinari. In addition, Google and Google scholar were searched. Studies that focused on the application of digital health technologies on COVID-19 prevention and control were included in the review. We characterized the distribution of technological applications based on geographical locations, approaches to apply digital health technologies and main findings. The study findings from the existing literature were presented using thematic content analysis.
Results: A total of 2,601 potentially relevant studies were generated from the initial search and 22 studies were included in the final review. The review found that telemedicine was used most frequently, followed by electronic health records and other digital technologies such as artificial intelligence, big data, and the internet of things (IoT). Digital health technologies were used in multiple ways in response to the COVID-19 pandemic, including screening and management of patients, methods to minimize exposure, modelling of disease spread, and supporting overworked providers.
Conclusion: Digital health technologies like telehealth, mHealth, electronic medical records, artificial intelligence, the internet of things, and big data/internet were used in different ways for the prevention and control of the COVID-19 pandemic in different settings using multiple approaches. For more effective deployment of digital health tools in times of pandemics, development of a guiding policy and standard on the development, deployment, and use of digital health tools in response to a pandemic is recommended.
Keywords: COVID-19, digital health, pandemics, technology, review
1 Background
In recent decades, the world has seen a dramatic rise in global pandemics, from the Severe Acute Respiratory Syndrome (SARS) pandemic in 2003 to Avian Influenza in 2006, H1N1 influenza in 2009, Middle East Respiratory Syndrome (MERS) in 2012, Ebola in 2014, the appearance of the Zika virus in Latin America in 2015. These pandemics are inextricably bound up in modern socio-technical developments and processes of globalization [1-3]. In early 2020, the World Health Organization declared a new pandemic, caused by Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2), a previously unknown SARS virus variant [ 1 , 4 ]. SARS-CoV-2 causes the infectious disease known as COVID-19. Characteristic of a pandemic in general, COVID-19 is spreading around the globe exponentially, causing considerable disruption not only on the health system but also on the world economy. Compared with SARS and MERS, COVID-19 spreads more rapidly owing to increased globalization, a longer incubation period, and asymptomatic transmission.
The management and control of pandemics represent a unique challenge to health systems because novel infectious diseases can be transmitted rapidly to others and thus require a focus on early detection and treatment, surveillance, and outbreak control. Applications of digital health technologies like artificial intelligence, telehealth, mobile health, big data, 5G, and the Internet of Things (IoT) may be useful to support the control of a pandemic [ 5 , 6 ].
Digital health technologies (DHTs) have played an important role in pandemics, aiding understanding of the disease, improving diagnostic tools, and controlling the spread of the infection [ 4 ]. DHTs bring health services directly to people's homes and underserved communities that make health care more responsive and productive [ 6 ]. It has been reported that DHTs such as telehealth, when used for health surveys and data collection, surveillance, health awareness-raising, and decision support systems from different sources can be used to prevent and control pandemics or outbreaks without disrupting the regular social order [ 7 , 8 ]. The use of digital tools such as contact tracing apps to monitor outbreaks and their extent, and online consultations to help keep health professionals and patients safe while providing continued care are some of the ways that the potential of digital health has been harnessed during the COVID-19 pandemic [ 9 ].
The COVID-19 pandemic has challenged health systems in many ways and it is critically important to fight COVID-19 effectively. In line with this, digital health solutions provide an opportunity to optimize time and human resources in the fight against the pandemic. These solutions facilitate communication between community members, hospitals, and health care providers [ 10 ]. Yet, there are few reviews for how DHTs contribute to pandemics, especially COVID-19. A rigorous scoping review that examines the role of DHT in preventing and controlling the COVID-19 pandemic is needed to examine how DHTs were rapidly deployed to support COVID-19 response.
We used a Population, Concept, and Context (PCC) framework developed by the Joanna Briggs Institute (JBI) to frame our primary research questions as follows:
What is the available evidence on the role of digital health technologies in the prevention and control of COVID-19?
What were the barriers that influence the practice of digital health technologies in the prevention and control of the COVID -19 pandemic?
To answer these questions, we aimed to map the evidence of digital health technologies on COVID-19 pandemic control and barriers during the application of these technologies.
2 Methods
Our scoping review aimed to map the available evidence on the role of DHTs, such as electronic health records, mHealth, telehealth, and artificial intelligence for preventing and controlling COVID-19. This review was conducted within the Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist and it was guided by the Joanna Briggs Institute scoping review guidance [ 11 ].
2.1 Eligibility Criteria
See Table 1 .
Table 1. Lists of the inclusion and exclusion criteria of studies for the scoping review.
| Inclusion criteria | Exclusion criteria |
|---|---|
| ▪ Both quantitative and qualitative studies ▪ Studies related to the role of digital health technologies to manage the COVID-19 pandemic ▪ Studies published in the English language ▪ Studies published in peer-reviewed journals |
▪ Case reports ▪ Individual views or “perspective” pieces ▪ Literature reviews ▪ Studies published in a language other than English ▪ Studies published in preprint literature |
2.2 Data Sources and Search Strategy
A comprehensive search was performed on the following databases: MEDLINE (PubMed), Cochrane library, Hinari 1 , Google, and Google Scholar advanced databases. Medical Subject Headings (MeSH) terms were used for searching and Boolean operators (AND, OR) were used to specify combinations of search terms. The following keywords and medical subject headings were used:
For coronavirus: COVID-19 OR “coronavirus pandemic” OR pandemic OR “public health epidemics” OR “global pandemics” OR “disease outbreaks” OR coronavirus OR “coronavirus 2019” OR “novel coronavirus disease 2019” OR SARS-CoV-2
AND
For digital health technologies: “health informatics” OR “clinical informatics” OR “(computer science, medical)” OR “health information technology” OR informatics OR “medical computer science” OR “medical records systems” OR “electronic health records” OR “biomedical informatics community” OR telemedicine OR telemed OR “telehealth eHealth” OR mHealth OR “electronic health records” OR “electronic medical record” OR “patient-facing technology”
AND
Prevention OR control OR Management.
The search was performed from October 09, 2020 to October 12, 2020. Additional relevant articles were identified by searching the reference lists of full-text articles studies published up to the last searched date of October 12, 2020, were included ( Supplement File 1 ).
Initial searches were performed by an author (DA), who has experience in systematic reviews. Screening of titles, abstracts, and full texts was conducted independently by two authors (DA and KD). In this process, a second reviewer was blinded to the primary reviewer's decision for selecting the articles; this helped to mitigate the risk of bias during the assessment stages of the reviews. Any differences of opinion were discussed, and a consensus was reached; otherwise, a third reviewer (BT) was involved to arbitrate any issues that remained unresolved.
2.3 Data Extraction
Two authors (DA and BF) extracted the data independently and compared the results. We extracted the following data from each study: author name, year of publication, country, types of digital health technology used, purpose(s) of applying digital health technology, service users, study design, approaches to applications of digital health technologies to address COVID-19, the study main findings, and barriers to implementation or adoption ( Table 1 ).
2.4 Analysis
Based on the methodological framework for scoping reviews [ 12 ], we were able to present our narrative account of findings in two ways. First, attention was given to the basic numerical analysis, and the distribution of the studies included in the review. We determined the distribution of electronic technologies used in COVID-19 prevention and control by geographical location. Second, the study findings from the existing literature were evaluated using thematic content analysis. Our narrative was then structured around the categories derived from the included study results or outcomes. These categories were: 1) types of commonly used digital health technologies, approaches or methods of application of digital health technologies for pandemic prevention and control; 2) the main role of the digital health technologies; and 3) barriers for the proper use of digital health technologies to prevent and control the pandemic.
3 Results
The initial search generated 2,601 articles. After duplicates were excluded, 2,431 articles remained. Titles and abstracts of the remaining articles were screened for potential eligibility. We excluded most of these potentially relevant papers (89.6%) based on a review of the title (n=1,188) or abstract (n=991). As a result, a total of 252 articles were eligible for full-text screening. After screening, 230 articles were excluded due to: lack of relevant information (n=74, 32.2%), for example, no information about DHTs rather provide information only about COVID-19 and other infectious diseases; electronic technologies applied for other types of disease such as HIV/AIDS, tuberculosis, or diabetes mellitus (n=99, 43%); focus only on health information technology in general, such as for communication and academic education (n=36, 15.7%). Another 21 (9.1%) documents, representing perspective articles or literature reviews were excluded ( Figure 1 ).
Fig. 1.
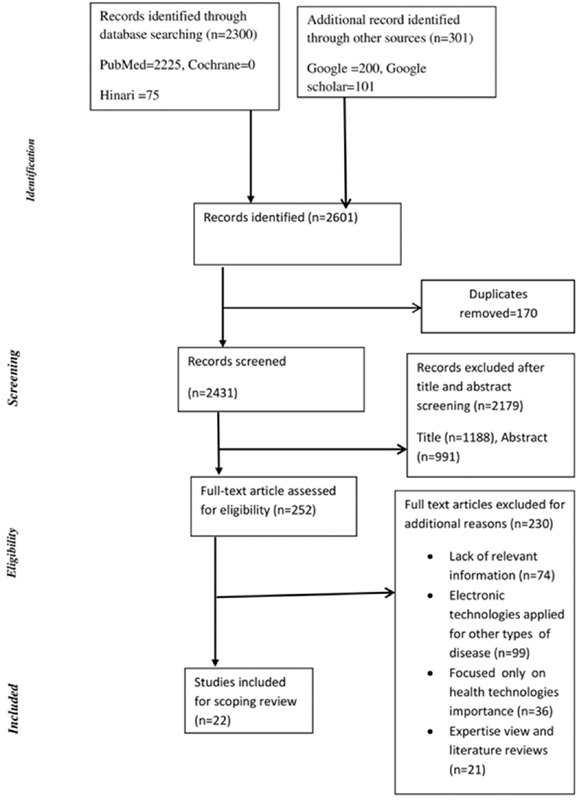
Flow Diagram for the scoping review process adapted from the PRISMA statement by Moher and colleagues (2009)
3.1 Characteristics of Included Studies
Of the 22 included studies 13 (59%) of them were from the USA [6, 13-24], three were from China [25-27], two were from Iran [ 28 , 29 ] , Australia [ 16 ], Spain [ 30 ], Canada [ 31 ], and Taiwan [ 32 ] each contributed one ( Table 2 ). The use of digital health technologies to combat COVID-19 was predominantly reported by North American studies (64%), followed by Asia (27%).
3.2 What Is the Available Evidence for the Role of Digital Health Technologies for Preventing and Controlling Coronavirus Pandemic?
3.2.1 Purpose of Digital Health Technologies Applied for COVID-19 Pandemic
Different digital health technologies were applied by health care providers for different purposes to prevent and control the COVID-19 pandemic at the community and health care facility levels. These technologies were categorized as telemedicine, Electronic Health Record, Artificial Intelligence, and Internet of Things. In this scoping review, the most frequently used technologies were telemedicine, including telehealth and mHealth [6, 15-24, 27-31], and electronic health records [ 13 , 14 , 26 , 32 ]. Less frequently used technologies include artificial intelligence [ 6 , 13 ], 5G+ [ 6 , 25 ], and the Internet of Things [ 6 ] ( Table 2 ).
Table 2. Characteristics of individual studies included in this scoping review.
| Author | Country | Types health informatics | Methods of application/approach | Aim/purpose | Main findings | Barriers |
|---|---|---|---|---|---|---|
| Ye Q | China | mobile internet big data cloud computing 5G+ telemedicine clinical information system | Provide a variety of web-based services for the public during the outbreak, including screening and consultation services. Release official statistics about the COVID-19. Apply predictive modeling and turning point projection, monitor crowd activity. Assist the development of epidemic prevention and control strategies. Intelligently manage information Facilitate clinical management related to COVID-19 |
To understand the actions taken by the health informatics community in China during the COVID-19 outbreak and to develop a health information technology framework for epidemic response based on health information technology–related measures and methods | Health information technologies play a very important role in responding to the COVID-19 epidemic. Information technology was used at all stages of the epidemic, such as prediction of epidemic trends, tracking of close contacts, and remote diagnosis They recommend that Health informatics communities in all countries should react quickly and make full use of health information technology to respond to the epidemic. |
Not mentioned in the study |
| Dean F | USA | electronic health record | To explore the need of national health information technology on prevention and control of COVID-19 | Health information technology would involve a collection of interconnected health care nodes, with each node representing a health care organization using an electronic health record (HER) health information exchanges (HIEs) can facilitate the collection, exchange, and analysis of clinical and administrative data between health care organizations and clinicians | Not mentioned in the study | |
| Reeves JJ | USA | electronic health record (Screening protocols, System Level EHR-Templates) COVID-19 Operational Dashboard Communication Channels Artificial Intelligence Patient Facing Technology | Telephone calls direct email, and EHR messaging, all before in person encounters. A protocolized triage system was developed and embedded into multiple EHR templates which could be rapidly updated as screening guidance evolved. In order to limit exposure and relieve the burden on physical healthcare locations, automated email notifications were sent to patients prior to their clinic appointments indicating that persons with fever and/or new cough should call the health system for proper triage before presenting to the healthcare facility. |
Describing the implementation of technological support important for optimizing clinical management of the COVID-19 pandemic supporting the health systems efforts to prepare for the current pandemic the challenges associated with the risk | The electronic health record and associated technologies are vital and requisite tools in supporting outbreak management that should be leveraged to their full potential. | The need to frequently adjust build to meet rapidly evolving requirements communication, and adoption, and to coordinate the needs of multiple stakeholders |
| Lin C | Taiwan | Cloud-based health records | Integrate recent history of travel to China from the database of Customs and Immigration Submit claims to the single-payer platform within 24 hours. | Integrating recent history of travel to China from the database of Customs and Immigration to supplement the NHI's centralized cloud-based health records. | Medical providers would be aware of patients' travel history when they made an appointment or came in Information that let clinicians and Taiwan CDC track or trace back all doctor visits. |
Not mentioned in the study |
| Gong M | China | Cloud-based hardware | Designed Honghu Hybrid System (HHS) for the collection, integration, standardization, and analysis of COVID-19-related data from multiple sources, which includes a case reporting system, diagnostic labs, electronic medical records, and social media on mobile devices. | To illustrate how new medical informatics technologies may enable effective control of the pandemic through the development and successful 72-hour deployment of the Honghu Hybrid System (HHS) for COVID-19 in the city of Honghu in Hubei, China. | The HHS has been observed to be effective and feasible for COVID-19 surveillance and control. It helped strengthen the checkpoints on the full chain of COVID-19 control, including “early test, early report, early isolation, and early treatment” during the outbreak |
Not mentioned in the study |
| Ye J | USA | Artificial intelligence, Telemedicine or telehealth, Mobile health, Big data, 5G, and the Internet of Things | Forming a multisource platform that integrates data monitoring, exchange, convergence, and feedback mechanisms for the pandemics | Assessing the role of health technology and informatics in a global public health emergency: Practices and Implications From the COVID-19 Pandemic | Through combining health technology and health care systems, diagnosis efficiency and patients' medical experiences can be improved Remote sharing of high-quality medical resources and real-time information interaction can also be achieved The establishment of an integrated intelligent health care system for COVID-19 pandemic prevention and control will also provide a positive reference for the design and development of subsequent intelligent health care platforms for other public health crises The use of remote consultation reduces the occurrence of on-site diagnoses, which also saves PPE, and reduces the risk of infection spread caused by the transfer of diagnosed patients to the superior hospitals. |
Not mentioned in the study |
| Katzow MW |
USA | Telemedicine | Not clearly mentioned | To give health care service of the children at their home to strengthen stay home and keeping social distancing | The application of telemedicine was the one health technology that protects patients to come the hospital and decrease contact of clinicians with the patient. This reduced the psychological stress of the patients in the COVID -19 pandemics |
Limited English proficiency Internet interruption Inaccessibility of smart phone Limited telemedicine service |
| Smith A | Australia | Telemedicine (telehealth) | Not described in the study | To illustrate the use of telehealth for caring, consulting and screening patients during COVID-19 where clinical service is not well organized | For this infectious pandemic telehealth provide rapidly deploy large numbers of providers Facilitate triage so that front-line providers are not overwhelmed with new presentations Supply clinical services when local clinics or hospitals are damaged or unable to meet demand Decrease the risk of communicable diseases which are transmitted by person-to-person contact. Telehealth also provide care for non-infected people during an infectious pandemic. |
Clinician's unwillingness to adopt telehealth due to limited telehealth training in medical, nursing and allied health preregistration curricula |
| Hoffman | USA | Telehealth | Not described in the study | To describe the use of telehealth and identifying public policy barriers to the implementation of telehealth (reimbursement, privacy/cybersecurity, liability, licensure, technology access, and artificial intelligence (AI)) | Telehealth encourage health researchers to use the increased data provided by telehealth services to train AI software that can further improve not only the telehealth services, research, but also increase other clinical care and healthcare operations access during COVID-19 | |
| Bryne MD | USA | Not described in the study | Describing the importance of telehealth to prevent and control the COVID-19 pandemic | Telehealth was a crucial tool during the early phases of the pandemic and allowed, in most cases, for the closing of some service delivery gaps and as a financial life boat for health care practices. For patients, particularly those at high risk because of chronic conditions, telehealth may have been their only means of follow-up and support. |
Before the pandemic, the lack of a reimbursement incentive had limited interest in investing in telehealth applications or the training needed to use them | |
| Moazzami | Iran | Telemedicine | Not described in the study | Enabling patients to connect with their healthcare provider at a distance using telemedicine to reduce health care provider burnout during COVID-19 | The application of telemedicine by health care providers reduces the major causes of psychological distress among healthcare workers are including long work hours, sleep disturbances, debilitating fatigue, and the risk of getting infection and put their family at risk of a life-threatening condition at large during this COVID-19 Pandemic. | Not described in the study |
| Villegas | Spain | Telemedicine | A new teleconsultation protocol was implemented to tend the patients with respiratory difficulties and/or compatible with the disease provoked by COVID-19, at the hospital emergency service (HES) | To evaluate the effectiveness of a teleconsultation protocol with patients who had respiratory symptoms in the reduction of the consumption of personal protective equipment (PPE) in a hospital emergency service (HES) during the COVID-19 pandemic | The possibility of patient-doctor spread has been reduced The use of the PPEs has been optimized, and The making of decisions has been streamlined in the first stage of care of suspected COVID-19 patients. |
Not described in the study |
| Esfehani RJ |
Iran | Telemedicine (web-based software) | proposed web-based software that provides a virtual workspace for two kinds of users, including specialists | To highlight the importance of effective disease control and case tracing, to reducing the pressure on the medical staff and health care workers to improve their medical judgment and performance abilities, and educating the physicians who have not previously encountered COVID-19 cases and are not familiar with their clinical and radiological presentations | The application of web-based software reduces close contact of health care providers with the patient Minimize burnout of care providers Minimize mis diagnosis of COVID suspected cases By using such telemedicine platforms, the experience of the specialists will be provided for every suspicious patient in every unequipped center manifestation using telemedicine |
|
| Chavis A | USA | Prevention of exposure to COVID-19 in a medically complex patient with a mild presentation by applying telemedicine | A telehealth examination of a patient presenting with a less common and thus unexpected coronavirus disease-2019 symptom prevented the exposure of the healthcare team in an academic general paediatrics clinic | Not described in the study | ||
| Annis T | USA | Telehealth (mhealth) | A COVID-19–specific remote patient monitoring solution (GetWell Loop) was offered to patients with COVID-19 symptoms mHealth Fairview was integrated as academic healthcare system with 12 hospitals (2,071 beds), 56 primary care clinics, 100 specialties, and 34,000 employees located in the urban Twin Cities area | To evaluate early lessons from a remote patient monitoring engagement and education technology solution for patients with coronavirus disease 2019 (COVID-19) symptoms. | Patients have been extremely grateful and positive about their experience using the tool and feel it has helped them stay safe at home. This demonstrates what can be accomplished through a shared imperative and effective partnerships between industry, and healthcare delivery |
Not mentioned in the study |
| Russ SC | USA | Telehealth (TeleEM) | Using both synchronous video and telephonic tools for complex or critically ill patients. TeleEM physician via video to consult and give care the patients at their home |
To outline current Mayo Clinic strategies harnessing telehealth solutions for COVID-19 emergency preparedness and acute emergency care. Minimize front-line provider exposure and conserve personal protective equipment |
In the hands of all acute care providers for consultation, telehealth tools are helping to limit disease spread, reduce HCW exposure, and conserve valuable PPE at emergency department service | Not described in the study |
| Wosik J | USA | Telehealth (smart phone and tablets | e-consult, patient intiated messaging, telephon visit and vidio visit Home peripheral devices were used with certain patients to facilitate remote visits (blood pressure machines and cuffs) |
Adopting of telehealth, or the entire spectrum of activities used to deliver care at a distance for the three phases (1) stay-at home outpatient care, (2) initial COVID-19 hospital surge, and (3) post-pandemic recovery | Virtual patient waiting rooms, privacy and security, and easy scheduling were important when evaluating a platform Reducing virus transmission, stretching human and technical resources, and protecting patients and healthcare workers in the inpatient care setting |
Not described in the study |
| Lam P | Canada | Telemedicine Network virtual care platform and telephone for reminder | The COVID-19 Expansion to Outpatients (COVIDEO) program was developed at the health care Centre, Toronto, Ontario, to provide ongoing care for outpatients diagnosed with COVID-19. | To develop and test the feasibility of a virtual care program for self-isolating outpatients diagnosed with COVID-19 | The use of virtual care in medicine has become an attractive strategy to minimize unnecessary patient travel to health care institutions for medical care and has a unique application in patients who require self-isolation In addition to the care provided to the patient, potential benefits of a virtual care program include the ability for health care providers to plan for a safe and controlled hospital transfer for those showing signs of clinical deterioration, and the ability to reduce further community spread by informing public health of any household contacts with symptoms. |
Unable to comment on the long-term sustainability of such a program As the number of patients diagnosed with COVID-19 continues to increase, the COVIDEO program will inevitably become more timeand labour intensive, patient and physician related factors (old people may not comfortable for technology…, the inability of family members or caregivers to assist owing to self-isolation requirements, increase number of patients over time |
| Joshi AU | USA | Telehealth | Telehealth care clinicians primarily trained in emergency medicine, internal medicine and family medicine followed a patient decision pathway to risk stratify patients into three groups: home quarantine no testing, home quarantine with outpatient COVID-19 testing and referral for in-person evaluation in the ED, for symptomatic and potentially unstable patients. | To design a time-sensitive, practical, effective and innovative scaleup of telehealth services as a response to the demand for COVID-19 evaluation and testing | There has been a decreased rate of referral to a higher level of care. due to :(1) an increased number of telehealth patient visits for stable and non-critical care, and (2) clinicians, while following a pathway, are motivated to keep stable patients socially distanced and quarantined at home | Not described in the study |
| Reiss AB | USA | Telehealth | The physical exam conducted virtually is patient/caregiver facilitated via video observation The patient or another member of household may take as many vital signs as possible, including temperature, body weight, blood pressure, heart rate. |
To describe telemedicine approach for COVID-19 as practiced in the offices of physicians affiliated with a major urban medical center To assess live interactive telemedicine during the COVID-19 pandemic to provide medical screening and assessment remotely |
The telehealth platform allows for delivery of care while maintaining the physical distancing necessary to prevent the spread of COVID-19 infectious disease | |
| Barney A | USA | Telemedicine (wearables smart phone accessories) | To describe the rapid implementation of telemedicine within an adolescent and young adult (AYA) medicine clinic in response to the COVID-19 pandemic | Providers noted that telemedicine seemed acceptable to Adolescent and young adult who generally had competence with electronic communications platforms and welcomed the convenience of meeting with providers remotely | Not described in the study | |
| Song X | China | Telemedicine | At community: psychological consulting, on-line clinic consulting, updating information on COVID-19. At patient: screening latent severe patients, consulting. Medical staff: training, panel discussion, psychological consulting, quality improvement |
To describe the role of telemedicine during the COVID-19 epidemic in China | Telemedicine activities avoid close contact and decrease the latent COVID-19 infection chance | Not described in the study |
3.2.2 Telemedicine and mHealth
Physicians, infectious disease epidemiologists, medical students, and others used telemedicine-based technologies to manage care and to prevent and control the COVID-19 pandemic in the following ways:
To give health care to the children in their home and to support stay-home orders and to maintain social distancing [ 15 ];
To care for, consult with, and to screen patients during the COVID-19 pandemic where clinical service is not well organized [ 16 ];
To identify barriers to the implementation of telehealth during the control of the COVID-19 pandemic [ 17 ];
To enable patients to connect with their healthcare provider at a distance using telemedicine to reduce health care provider burnout during COVID-19 [ 29 ];
To evaluate the effectiveness of a teleconsultation protocol with patients who had respiratory symptoms in the face of reduction of the availability of personal protective equipment in a hospital emergency service during the COVID-19 pandemic [ 30 ];
To highlight the importance of effective disease control and contact tracing, to reducing the pressure on the medical staff and health care workers, to improve their medical judgment and performance abilities, and to educate physicians and other health professionals who have not previously encountered COVID-19 cases and who are not familiar with the clinical and radiological presentations of the disease [ 28 ];
To outline current health care strategies for harnessing telehealth solutions for COVID-19 emergency preparedness and acute emergency care and minimize front-line provider exposure and to conserve personal protective equipment [ 21 ];
To adopt telehealth for the entire spectrum of activities used to deliver care at a distance for the three phases of stay-at-home: (1) outpatient care, (2) initial COVID-19 hospital surge, and (3) post-COVID recovery [ 22 ];
To develop and test the feasibility of a virtual care program and automated e-mail notifications for self-isolating outpatients diagnosed with COVID-19 [ 31 ];
To assess live, interactive telemedicine during the COVID-19 pandemic to provide remote medical screening and assessment [ 24 ].
3.2.3 Electronic Health Records (EHRs)
Countries used EHRs for different purposes. These included:
Using cloud-based or locally maintained EHRs to document and integrate the recent history of travel from customs and immigration databases to supplement, in turn, centralized cloud-based health records maintained by national health institutes [ 13 , 32 ];
Using EHRs to explore the need for national digital health technology on prevention and control of COVID-19 and to illustrate how new digital information technologies can enable effective control of the pandemic, such as realized in the development and successful 72-hour deployment of the Honghu Hybrid System for COVID-19 in the city of Honghu in Hubei [ 14 , 26 ];
Creating a protocolized triage system was developed and embedded into multiple EHR templates which could be rapidly updated as screening guidance evolved [ 13 ]. Another example was the Honghu Hybrid System for the collection, integration, standardization, and analysis of COVID-19-related data from multiple sources, which includes a case reporting system, diagnostic labs, electronic medical records, and social media on mobile devices [ 26 ].
3.2.4 Artificial Intelligence (AI) and Internet of Things (IoT)
To manage, prevent, and control the COVID-19 pandemic; health care providers used AI and IoT for the following purposes:
To understand the actions taken by the health informatics community in China during the COVID-19 outbreak and developing a digital health technology framework for epidemic response based on digital health technology-related measures and methods by using IoT [ 25 ];
To support health system efforts to prepare for the current pandemic challenges associated with the risk by using AI [ 13 ];
To assess the role of digital health technology in a global Public Health Emergency by using both AI and IoT [ 6 ];
Managing information and facilitating clinical management related to COVID-19 including screening and consultation services, predicting modelling and turning point projection (6)
3.3 What Was the Additional Importance of Using Digital Health Technologies for the Prevention and Control of COVID-19?
3.3.1 Exchanging Health Information and Minimizing Pandemic Exposure
The applications of DHTs had contributed to exchanging information and preventing exposure of health care providers and patients to COVID-19. Telemedicine activities avoid close contact and decrease the latent COVID-19 infection chance, limit disease spread, reduce health care workers exposure, minimize patient-doctor spread, and help to streamline decisions made in the first stage of care of suspected COVID-19 patients [ 21 , 27 ]. Patient-facing telemedicine platforms included a COVID-19 information page, which updated the latest information in real-time, including providing community patients with symptom information through online clinic consultation services, instructions for quarantine processes at home, personal protection applications, and when to seek medical attention [ 19 , 21 , 27 , 30 ].
3.3.2 Early Test, Isolation, and Treatment During the Outbreak
Through combining health technology and health care systems, remote sharing of high-quality medical resources and real-time information interaction can be achieved [ 6 ]. In addition, diagnostic efficiency and disease course can be improved. Using electronic health record components such as screening protocols, system-level EHR-templates, COVID-19 operational dashboards, and communication channels, rapid screening processes, and laboratory testing, clinical decision support, and patient-facing technology related to COVID-19 were achieved [ 6 , 13 ]. Digital health technologies such as telemedicine network virtual care platforms and cloud-based hardware helped strengthen the checkpoints on the full chain of COVID-19 control, including “early test, early report, early isolation, and early treatment” during the outbreak [ 25 , 28 , 31 ].
3.3.3 Remote Consultation and Reducing Psychological Stress
The application of telemedicine by health care providers reduces the major causes of psychological distress among healthcare workers by reducing long work hours, sleep disturbances, debilitating fatigue, and fear of getting an infection that could also put their family at risk of infection. Furthermore, it protects patients who otherwise might come to the hospital and thus decreases contact with health care providers [ 15 , 29 ].
3.3.4 Reduce Crowding of Health Service and Care Provider Burnout
Telehealth was a crucial tool during the COVID-19 pandemic and allowed in most cases, for the closing of some service delivery gaps and as a financial lifeboat for health care practices [ 17 ]. It also increased other clinical care and healthcare operations access during COVID-19 [ 17 , 18 ]. Developing telemedicine platforms by using web-based software reduced close contact of health care providers with the patient, minimized exhaustion and burnout of care providers, and minimized misdiagnosis of COVID suspected cases [ 23 , 28 ].
3.3.5 Digital Health Technologies to Assist Epidemiologists and Infectious Disease Professionals
In addition to the specific types of digital health information technology modalities described above, our review found that the application of digital health technologies (DHTs) was important to controlling and preventing the COVID-19 pandemic. A study in China revealed that DHTs were effective for the prediction of epidemic trends, tracking of close contacts, and remote diagnosis of COVID-19 pandemics. This will help public health decision-makers to develop COVID-19 pandemic prevention and control strategies [ 33 , 34 ]. Additionally, these technologies will facilitate effective COVID-19 vaccine delivery by tracking vaccine individuals, managing the data, and maintaining the cold chain [ 34 ].
3.4 What Were the Barriers That Influence the Practice of Digital Health Technologies During COVID-19 Prevention and Control of the Pandemic?
The COVID-19 pandemic has had an impact on public health infrastructure necessitating the development and use of digital health technologies. The need to frequently adjust this technology to meet rapidly evolving requirements, communication and adoption to coordinate the needs of multiple stakeholders for controlling and management of the pandemic pushed the need to use digital technologies even further. During the period covered by these reviews, some barriers reduced the effectiveness of the prevention of COVID-19. These barriers are mainly centered in three categories: patients, health care providers, and financial issues [ 16 , 18 , 25 ].
Some of the commonest barriers were: clinician's unwillingness to adopt telehealth due to limited telehealth training in medical, nursing and allied health pre-registration curricula [ 16 ], the economic incentive for doctors (doctors and their staffs time), and for system integrators and device manufacturers to develop the technology [ 17 ]. The old people were not also comfortable with technologies, the inability of family members or caregivers to assist owing to self-isolation requirements, increase the number of COVID-19 case over time, the lack of a reimbursement incentive, and economic incentives for health care providers. Additionally, limited English proficiency, internet service interruption, and inaccessibility of smartphones were the barriers of digital technologies service to be effective for controlling and preventing the pandemics [ 15 , 18 , 31 ].
Various papers revealed that there are different barriers to apply DHTs properly; such as lack of technical supporter, interference with a patient-provider relationship, increased patient anxiety, cost of digital health equipment, and lack of integration of technology with clinical workflow [ 35 , 36 ].
The current review showed that limited English proficiency of the patients, internet interruption, inaccessibility of smartphone, limited telehealth training for health care providers were some barriers reduced the effectiveness of the digital health technologies. This is also supported by a WHO review in which disparities in digital literacy and access to equipment, broadband, and the internet are important for increasing the effectiveness of telemedicine on COVID- 19 pandemic prevention [ 37 ]. This indicates that there is a need for immediate action by responsible stakeholders to facilitate the application of electronic technologies to reduce the burden of the pandemics and to recover the normal life of the world people especially countries which do not have good health care system [38-40].
4 Discussion
Our aim in this review was three-fold: 1) to map the role of digital health technologies on prevention and control of the COVID-19 pandemic; 2) to understand how the digital technologies have been applied to prevent the pandemic; and 3) to investigate the main barriers to the use of these technologies for tracking the pandemic.
About two-thirds of published studies on digital technologies for preventing and controlling the COVID-19 pandemic were from North America followed by Asia. Furthermore, we found that there were no published studies from Africa and limited studies from Europe and Australia. Our review found that the most commonly used DHTs to track COVID-19 pandemics were: telehealth, mHealth, EHRs, AI, and IoT. This finding is supported by prior analyses in which these digital health technologies were used to control and manage the Ebola and Zika [ 41 , 42 ] pandemics using similar approaches.
We found that the internet provides a variety of web-based services for the public during the outbreak, including video consultation, screening, and diagnosis. These services support the health care provider to identify a suspected case of COVID-19 and to provide medical and psychological advice to patients with the disease. Our review found that health care providers applied DHTs using different approaches for preventing and controlling coronavirus 2019. For instance, online clinic consultation, updating information on COVID-19 for the community, video and telephone consultation, and a multi-source platform that integrated data monitoring, exchange, and feedback mechanisms for pandemics-related issues.
This review suggests that digital health technologies like telehealth, EHRs, AI, IoT, and telemedicine platforms contributed to reducing COVID-19 exposure and transmission from person to person by exchanging health information, early testing and diagnosis, early isolation, early treatment during the outbreak, and remote consultation. This potentially helps to reduce burnout of health care providers, psychological stress, and overcrowding of health facilities. Also, it facilitates real-time information interaction and provides support for data-driven decision-making in the time of this pandemic and increasing susceptibility to COVID-19 especially for the elderly and those with comorbid conditions [ 9 , 43 ].
As we have seen, elderly people who might not be comfortable with technologies, the inability of family members or caregivers to assist owing to self-isolation requirements, increase the number of COVID-19 case over time, the lack of a reimbursement incentive, and economic incentives for health care providers are the most common barriers that decreased the effectiveness of DHTs application for prevention and control of COVID-19.
To expand the DHTs for the next pandemic, it is recommended that providing a variety of web-based services for the public during the outbreak, including screening and consultation service; forming a multisource platform that integrates data monitoring, exchange, convergence, and feedback mechanisms for the pandemics-related parties, and offering COVID-19 specific remote patient monitoring solutions.
Though this review uses a comprehensive search strategy from various databases, scoping reviews are broad and provide an overview of existing literature regardless of quality, providing a broad and contextual overview in comparison to systematic reviews. A formal assessment of methodological quality is not undertaken when conducting a scoping review and synthesis of the incorporating studies, nor is a demonstration of cause-and-effect relationships. Excluding grey literature and languages other than English are additional limitations of the review.
5 Conclusion
The current scoping review showed that using DHTs are effective in the prevention and control of the COVID-19 pandemic. These digital health technologies are principally used for the early test, report, isolation, treatment, exchanging information, remote consulting, reducing the overcrowding of health care facilities, minimizing burnout of health care providers, and model prediction COVID-19. The lessons learned during the COVID-19 pandemic should be applied to future digital health technologies that seek to support health system response to a pandemic.
Acknowledgments
The authors would like to acknowledge Dr. Brian Dixon and Dr. John Holmes for their support throughout the production of this review article.
Footnotes
Hinari Programme set up by World Health Organization together with major publishers, enables low- and middle- income countries to gain access to one of the world's largest collections of biomedical and health literature. ( https://www.who.int/hinari/en/ )
Supplementary Material
References
- 1.Fagherazzi G, Goetzinger C, Rashid M A, Aguayo G A, Huiart L. Digital health strategies to fight COVID-19 worldwide: challenges, recommendations, and a call for papers. J Med Internet Res. 2020;22(06):e19284. doi: 10.2196/19284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson C, Jumbert M G. The new informatics of pandemic response: humanitarian technology, efficiency, and the subtle retreat of national agency. Journal of International Humanitarian Action. 2018;3(01):1–13. doi: 10.1186/s41018-018-0036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mantas J, Hasman A, Househ M.The Importance of Health Informatics in Public Health during a PandemicIOS Press2020 [DOI] [PubMed]
- 4.Ahmadi S, Bempong N-E, De Santis O, Sheath D, Flahault A.The role of digital technologies in tackling the Zika outbreak: a scoping reviewJ Public Health Emerg 2018;2(06):
- 5.Wood C S, Thomas M R, Budd J, Mashamba-Thompson T P, Herbst K, Pillay D.Taking connected mobile-health diagnostics of infectious diseases to the field Nature 2019566(07745):467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ye J. The role of health technology and informatics in a global public health emergency: practices and implications from the COVID-19 pandemic. JMIR Med Inform. 2020;8(07):e19866. doi: 10.2196/19866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang S, Ding S, Xiong L. A New System for Surveillance and Digital Contact Tracing for COVID-19: Spatiotemporal Reporting Over Network and GPS. JMIR MHealth UHealth. 2020;8(06):e19457. doi: 10.2196/19457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kahn J P. Digital contact tracing for pandemic response: Ethics and governance guidance. Johns Hopkins University Press. 2020.
- 9.Cassione E B, Zanframundo G, Biglia A, Codullo V, Montecucco C, Cavagna L. Response to: ‘COVID-19 pandemic: an opportunity to assess the utility of telemedicine in patients with rheumatic diseases’ by Lopez-Medina et al. Ann Rheum Dis. 2020. [DOI] [PubMed]
- 10.Peden C J, Mohan S, Pagán V. Telemedicine and COVID-19: an Observational Study of Rapid Scale Up in a US Academic Medical System. J Gen Intern Med 2020 Sep. 35(09):2823–5. doi: 10.1007/s11606-020-05917-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peters M, Godfrey C, Khalil H, McInerney P, Soares C, Parker D. Guidance for the Conduct of JBI Scoping Reviews. 2017.
- 12.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(01):19–32. [Google Scholar]
- 13.Reeves J J, Hollandsworth H M, Torriani F J, Taplitz R, Abeles S, Tai-Seale M. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020;27(06):853–9. doi: 10.1093/jamia/ocaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sittig D F, Singh H. COVID-19 and the Need for a National Health Information Technology Infrastructure. JAMA 2020 Jun 16. 323(023):2373–4. doi: 10.1001/jama.2020.7239. [DOI] [PubMed] [Google Scholar]
- 15.Katzow M W, Steinway C, Jan S. Telemedicine and Health Disparities During COVID-19. Pediatrics 2020; Aug. 146(02):e20201586. doi: 10.1542/peds.2020-1586. [DOI] [PubMed] [Google Scholar]
- 16.Smith A C, Thomas E, Snoswell C L, Haydon H, Mehrotra A, Clemensen J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare 2020 Jun. 26(05):309–3. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffman D A. Increasing access to care: telehealth during COVID-19. J Law Biosci. 2020;7(01):lsaa043. doi: 10.1093/jlb/lsaa043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Byrne M D. Telehealth and the COVID-19 Pandemic. J Perianesth Nurs. 2020;35(05):548–51. doi: 10.1016/j.jopan.2020.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chavis A, Bakken H, Ellenby M, Hasan R. COVID-19 and Telehealth: Prevention of Exposure in a Medically Complex Patient With a Mild Presentation. J Adolesc Health. 2020;67(03):456–8. doi: 10.1016/j.jadohealth.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Annis T, Pleasants S, Hultman G, Lindemann E, Thompson J A, Billecke S. Rapid Implementation of a COVID-19 Remote Patient Monitoring Program. J Am Med Inform Assoc 2020 Aug 1. 27(08):1326–30. doi: 10.1093/jamia/ocaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russi C S, Heaton H A, Demaerschalk B M. Elsevier; 2020. Emergency Medicine Telehealth for COVID-19: Minimize Front-Line Provider Exposure and Conserve Personal Protective Equipment. Mayo Clinic Proceedings. [DOI] [PMC free article] [PubMed]
- 22.Wosik J, Fudim M, Cameron B, Gellad Z F, Cho A, Phinney D. Telehealth Transformation: COVID-19 and the rise of Virtual Care. J Am Med Inform Assoc. 2020;27(06):957–62. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Joshi A U, Lewiss R E. Telehealth in the time of COVID-19. Emerg Med J. 2020;37(010):637–8. doi: 10.1136/emermed-2020-209846. [DOI] [PubMed] [Google Scholar]
- 24.Reiss A B, De Leon J, Dapkins I P, Shahin G, Peltier M R, Goldberg E R. A Telemedicine Approach to Covid-19 Assessment and Triage. Medicina (Kaunas) 2020;56(09):461. doi: 10.3390/medicina56090461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ye Q, Zhou J, Wu H. Using Information Technology to Manage the COVID-19 Pandemic: Development of a Technical Framework Based on Practical Experience in China. JMIR Med Inform. 2020;8(06):e19515. doi: 10.2196/19515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gong M, Liu L, Sun X, Yang Y, Wang S, Zhu H. Cloud-Based System for Effective Surveillance and Control of COVID-19: Useful Experiences From Hubei, China. J Med Internet Res. 2020;22(04):e18948. doi: 10.2196/18948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song X, Liu X, Wang C. The role of telemedicine during the COVID-19 epidemic in China’experience from Shandong province. Crit Care 2020 Apr 28. 24(01):178. doi: 10.1186/s13054-020-02884-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jafarzadeh-Esfehani R, Fard M M, Hatam-Ghale F H, Kalat A R, Fathi A, Shariati M. Telemedicine and Computer-Based Technologies during Coronavirus Disease 2019 Infection; A Chance to Educate and Diagnose. Arch Iran Med. 2020;23(08):561–3. doi: 10.34172/aim.2020.60. [DOI] [PubMed] [Google Scholar]
- 29.Moazzami B, Razavi-Khorasani N, Moghadam A D, Farokhi E, Rezaei N. COVID-19 and telemedicine: Immediate action required for maintaining healthcare providers well-being. J Clin Virol. 2020. p. 104345. [DOI] [PMC free article] [PubMed]
- 30.Lopez-Villegas A, Maroto-Martin S, Baena-Lopez M A, Garzon-Miralles A, Bautista-Mesa R J, Peiro S. Telemedicine in Times of the Pandemic Produced by COVID-19: Implementation of a Teleconsultation Protocol in a Hospital Emergency Department. Healthcare (Basel) 2020 Sep 23. 8(04):357. doi: 10.3390/healthcare8040357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lam P W, Sehgal P, Andany N, Mubareka S, Simor A E, Ozaldin O. A virtual care program for outpatients diagnosed with COVID-19: a feasibility study. CMAJ Open. 2020;8(02):E407–E13. doi: 10.9778/cmajo.20200069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin C, Braund W E, Auerbach J, Chou J-H, Teng J-H, Tu P. Policy Decisions and Use of Information Technology to Fight COVID-19, Taiwan. Emerg Infect Dis. 2020;26(07):1506–12. doi: 10.3201/eid2607.200574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuniya T. Prediction of the epidemic peak of coronavirus disease in Japan, 2020. J Clin Med. 2020;9(03):789. doi: 10.3390/jcm9030789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chretien J-P, Swedlow D, Eckstrand I, George D, Johansson M, Huffman R.Advancing epidemic prediction and forecasting: a new US government initiativeOnline J Public Health Inform 2015;7(01).
- 35.Inkster B, O’Brien R, Selby E, Joshi S, Subramanian V, Kadaba M.Digital Health Management During and Beyond the COVID-19 Pandemic: Opportunities, Barriers, and Recommendations JMIR Ment Health 2020. Jul 6707e19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palacholla R S, Fischer N, Coleman A, Agboola S, Kirley K, Felsted J. Provider-and patient-related barriers to and facilitators of digital health technology adoption for hypertension management: scoping review. JMIR Cardio. 2019;3(01):e11951. doi: 10.2196/11951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Greenhalgh T, Wherton J, Shaw S, Morrison C.Video consultations for covid-19. BMJ 2020 Mar 12;368:m998. [DOI] [PubMed]
- 38.Alwashmi M F. The use of digital health in the detection and management of COVID-19. Int J Environ Res Public Health. 2020;17(08):2906. doi: 10.3390/ijerph17082906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hageman J R. The emergence of pediatric telehealth as a result of the COVID-19 pandemic. Pediatric Ann. 2020;49(07):e283–e284. doi: 10.3928/19382359-20200626-01. [DOI] [PubMed] [Google Scholar]
- 40.Castelnuovo G, Pietrabissa G, Manzoni G M, Sicurello F, Zoppis I, Molinari E. Fighting the COVID-19 pandemic using the technology-based second-line in Italy and Lombardy: The urgent need of home-based remote monitoring systems to avoid the collapse of the hospital-centred first line. J Global Health 2020 Dec. 10(02):10371. doi: 10.7189/jogh.10.020371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khubchandani J, Jordan T R, Yang Y T. Ebola, Zika, Corona… What Is Next for Our World? Int J Environ Res Public Health 2020 May 2. 17(09):3171. doi: 10.3390/ijerph17093171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sacks J A, Zehe E, Redick C, Bah A, Cowger K, Camara M. Introduction of mobile health tools to support Ebola surveillance and contact tracing in Guinea. Glob Health Sci Pract. 2015;3(04):646–59. doi: 10.9745/GHSP-D-15-00207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carlson J L, Goldstein R. Using the Electronic Health Record to Conduct Adolescent Telehealth Visits in the Time of COVID-19. J Adolesc Health 2020 Aug. 67(02):157–8. doi: 10.1016/j.jadohealth.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


