Abstract
Background and aims
The survey aimed to assess COVID-19 vaccine acceptance and hesitancy rate among patients with diabetes and address barriers and beliefs that affect acceptance to take COVID-19 vaccine.
Methods
A quantitative research approach with cross-sectional design was used to collect data from March–May’2021. Saudi residents with diabetes, aged ≥18 years were included.
Results
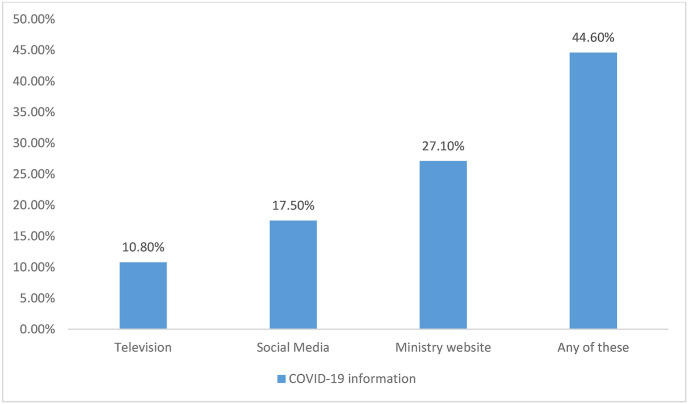
Of the total 709 participants, 42.2% had family member with COVID-19, 14.7% had COVID-19, 34.0% had been with someone who had COVID-19. 34.7% of participants taken COVID-19 vaccination, 36.2% were willing to take, while 79.0% supported COVID-19 vaccine. Main reasons behind uncertainties towards vaccinations were relatively fast production, not many trials done and about genetic component. 44.6% got information about COVID-19 and vaccination through television, social media, and ministry website. On adjusting models, female gender, longer duration of diabetes and no history of influenza vaccine significantly associated with COVID vaccine uptake.
Conclusion
Participants are willing to vaccinate but show some fear and misinformation. It is imperative that due efforts are made for increasing vaccine willingness, and availability of precise information holds key to success. Otherwise, state will have to continue to funnel in resources towards post-on-set disease management, consuming a lot more resources than preventive measures like vaccination.
Keywords: COVID-19, Diabetes, Acceptance, Hesitancy, Saudi Arabia
1. Introduction
Since the beginning of this pandemic, more than a hundred and seventy million cases and nearly four million deaths have been reported globally [1]. Due to unavailability of an exact treatment, protective measures along with efficacious vaccines form the best strategy to combat this deadly disease. This will help in decreasing spread, reducing hospital and intensive care admission [2]. Four types of vaccines are currently available against COVID-19 including inactivated/weakened virus vaccine, protein-based vaccines, viral vector vaccines, and RNA/DNA vaccines [3]. Therefore, sufficient vaccine coverage and a high acceptance rate will be needed for successful COVID-19 immunization. However, the biggest challenge faced by most governments is vaccine hesitancy. Recent studies worldwide have reported about citizens' mistrust towards health authorities, governments, health professionals, and the misinformation spread through social media [4]. World Health Organization (WHO) listed vaccine hesitancy among ten major threats to health globally [2]. Among the general adult population, the lowest vaccine acceptance rates against COVID-19 were found in Russia, Jordan, Kuwait, European countries, and African countries. At the same time, the highest were reported from Ecuador, Malaysia, China, and Indonesia [1].
Vaccine hesitancy is a term used to define a delay in acceptance or an outright refusal to vaccinate even with accessibility to vaccination services [5]. Many published studies have reported various factors and reasons behind the refusal or hesitancy of vaccine acceptance globally [6,7]. Perceived risks compared to benefits, lack of awareness or knowledge, and religious beliefs are the common reasons for most vaccine refusals [8]. Recent data shows a similar hesitancy against COVID-19 vaccination as well. For instance, a study reported a strong correlation between intention to get vaccinated and its perceived safety [9]. Another study found an association with certain religious beliefs and decreased intent to get a vaccination against COVID-19 [10]. Another study conducted in the UK found that general mistrust in COVID-19 vaccine benefits and fears about any unforeseen side effects in future are the main determinants in achieving mass immunity against COVID-19 while an unwillingness to vaccinate was commonly found in the general population [11].
Vaccine hesitancy is a complex process not driven by any individual factor. World health organization (WHO) EURO Working Group proposed a “3 Cs model including Complacency, Convenience and Confidence” model in 2011 [12]. Complacency is often found be caused by lower perceived risks of the disease, consequently vaccination is considered as unnecessary for prevention. Vaccine convenience is an important factor too; it includes availability, affordability, geographical accessibility, willingness, quality of services, delivery of vaccines, and cultural context. These are the factors that affect the decision of vaccine uptake or vaccine hesitancy. While confidence is the trust in the vaccine effectiveness and safety, motivation of policy-makers, and the competence and reliability of health services and healthcare professionals are important as well [5,12].
Generally, infectious diseases affect patients with diabetes more commonly and with more severity, which results in an increase in mortality and morbidity [13,14]. In COVID-19, the severity of the disease becomes threefold in patients with diabetes [15,16]. A study conducted in Saudi Arabia reported a high prevalence of diabetes (68.3%) among hospitalized COVID-19 disease patients with a higher mortality rate (20.5%) and lower survival time (p 0.016) as compared to non-diabetic patients [14]. Likewise, it was also reported that diabetic patients with COVID-19 suffered from severe metabolic complications (diabetic ketoacidosis and hyperosmolarity) [17,18]. Another study among hospitalized COVID-19 patients in England showed 18.3% had type 2 DM, while 26.4% patients with diabetes died during the survey period (adjusted hazard ratio 1.23, 95% CI 1.14–1.32) [19]. In the light of the above figures, every patient with diabetes needs to receive COVID-19 vaccination. Thus, this survey aimed to assess COVID-19 vaccine acceptance/willingness and hesitancy rate among patients with diabetes and address the barriers and beliefs that affect acceptance to take COVID-19 vaccine among patients with diabetes.
2. Subjects, material and methods
2.1. Study design and study population
We used a quantitative research approach with a cross-sectional study design to evaluate the study objectives. Data were collected from the diabetic population between March 2021 and May 2021. The study included a total of 709 participants who were resident of Saudi Arabia. The study included all the participants aged ≥18 years and who had been diagnosed with Type 1 or 2 Diabetes. In contrast, pregnant women and participants with ages <18 years were excluded from the study. The study participants were assessed for their knowledge and degree of hesitancy to a COVID-19 vaccine.
2.2. Sampling method and data collection tool
The study was conducted in all regions of the Kingdom of Saudi Arabia. Patients with diabetes from all the regions were invited to participate in the study. A convenient sampling technique was used to include all the patients with diabetes who were willing to participate in the study. This survey utilized a structured Arabic version of the questionnaire for data collection. An online, validated and self-administered, questionnaire was developed, and invitation links were disseminated using various social media platforms. The different questions in the questionnaire were adapted and modified from the published study of Sallam, Dababseh (20). More specifically, data were collected on demographics, diabetes, history of other medical complications, the status of glycemic control (HbA1c), knowledge and source of knowledge about COVID-19 vaccination, influenza vaccine. Participants were also asked about the important factors that might make them hesitant towards Covid - 19 vaccines.
Ethical approval
Ethical approval was taken from the Research Ethics Committee of Prince Sattam Bin Abdulaziz University with a reference number REC-HSD-57-2021. Participation in this survey was completely on voluntary basis. Informed consent was a part of the introduction of the survey. Confidentiality of the participants was maintained, and all the data were kept anonymous.
2.3. Statistical analysis
The normality of all continuous variables was assessed. Variables that were not normally distributed were re-coded as categorical variables. Collinearity was assessed with no variables requiring exclusion due to weak association. The frequency and percentage of categorical variables were reported. Univariate association between factors and COVID-vaccine support was tested. All variables with borderline statistical significance (p < 0.25) were considered as potential confounder variables. Results are reported as an Odds Ratio (OR) with a 95% confidence interval (CI). Multivariable binary logistic regression models were used to produce covariate adjusted-OR and 95% CIs. To select the final variables, we included all candidate variables with p value ≤ 0.25 at univariate in the model and then applied purposeful backward elimination for selecting the final model.
3. Results
Total 709 participants participated in the survey of which more than half (59.5%) were females, more than two third were either of age 16–25 and or more than age 45. Of the total participants, almost half had bachelor's degree (53.2%) and were married (50.8%) (Table 1 ).
Table 1.
Sociodemographic characteristics of study participants.
| Sociodemographic | Frequency (%) |
|---|---|
| Gender | |
| Male | 287(40.5) |
| Female | 422(59.5) |
| Age | |
| 16-25 | 245(34.6) |
| 26-35 | 140(19.7) |
| 36-45 | 82(11.6) |
| >45 | 242(34.1) |
| Education | |
| High school | 298(42.0) |
| Bachelors | 377(53.2) |
| Masters | 34(4.8) |
| Marital status | |
| Married | 360(50.8) |
| Single | 349(49.2) |
| Diabetes | |
| Type 1 | 473(66.7) |
| Type 2 | 236(33.3) |
| Duration of Diabetes | |
| <5 years | 262(37.0) |
| 5–10 years | 275(38.8) |
| >10 years | 172(24.3) |
| HbA1c | |
| <7 | 246(34.7) |
| 7-9 | 106(15.0) |
| >9 | 357(50.4) |
More than two third had type 1 diabetes and more than one third had diabetes either for less than 5 years (37.0%) or more than 5–10 years (38.8%). Nearly half of the participants reported having HbA1c between 7 and 9 (Table 1). Around half (49.6%) of the participants had some kind of chronic diseases such as hypertension, asthma, obesity and related cardiovascular diseases.
Information related to COVID 19 and vaccination uptake, 42.2% of participants had a family member with COVID-19 and 14.7% reported that they themselves were exposed to COVID-19. More than one third (34.0%) had been with someone who had COVID-19. More than one third of participants had already taken (34.7%) COVID-19 vaccination or were willing (36.2%) to take one. More than three fourth (79.0%) of the participants supported COVID-19 vaccine (Table 2 ).
Table 2.
COVID-19 vaccine awareness among study participants.
| COVID-19 Vaccine awareness | Frequency (%) |
|---|---|
| Support vaccine | |
| Yes | 560(79.0) |
| No | 149(21.0) |
| Family member having COVID-19 | |
| Yes | 299(42.2) |
| No | 410(57.8) |
| Exposed to COVID-19 | |
| Yes | 104(14.7) |
| No | 605(85.3) |
| Been with someone having COVID-19 | |
| Yes | 241(34.0) |
| No | 468(66.0) |
| Willing to take COVID-19 Vaccine | |
| Yes | 257(36.3) |
| Already taken | 246(34.7) |
| No/Not sure | 200(29.0) |
The main reasons behind the uncertainties towards vaccinations were relatively fast production, not many trials done and uncertainties about the genetic component. Of the total participants, 44.6% got the information about COVID-19 and COVID-19 vaccination through television, social media and ministry website (Fig. 1 ).
Fig. 1.
Sources of information regarding COVID-19 vaccination.
Regarding COVID-19 vaccine uptake, females supported vaccine uptake significantly more than the males (OR: 1.69, 95% CI: 1.15–2.48). Participants with a history of diabetes for 5–10 years and more than 10 years were more inclined towards vaccine uptake as compared to those with the history of less than 5 years, OR: 1.82, 95% CI: 1.18–2.81 and OR: 1.73, 95% CI: 1.06–2.82 respectively. Individuals with type 2 diabetes were more willing to take vaccine as compared to those with type 1 diabetes. However, this association was not significant (OR: 1.36, 95% CI: 0.94–1.98). Individuals with HbA1c > 9 had significant impact on vaccine uptake OR: 1.58, 95% CI: 1.04–2.40 compared to those with HbA1c level<7. Lastly, participants who had the history of taking influenza vaccine did not support COVID-19 vaccine compared to those with no such history (OR: 0.51, 95% CI: 0.35–0.75) (Table 3 ). On adjusting the models with the candidate variables, female gender, longer duration of diabetes and no history of influenza vaccine remained significantly associated with COVID vaccine uptake (Table 3).
Table 3.
Factors influencing COVID vaccine uptake among study participants.
| Sociodemographic |
Support COVID-19 vaccine |
||
|---|---|---|---|
| Frequency (%) | OR (95%CI) | AOR(95%CI) | |
| Gender∗ | |||
| Male | 241(43.0) | Ref | Ref |
| Female | 319(57.0) | 1.69(1.15–2.48)∗∗ | 1.62(1.09–2.41) |
| Age | |||
| </ = 35 | 302(78.4) | 1.07(0.74–1.54) | |
| >35 | 258(79.6) | Ref | |
| Education | |||
| High school | 231(77.5) | 1.16(0.89–1.67)∗∗ | |
| Bachelors/masters | 329(80.0) | Ref | |
| Marital status | |||
| Married | 270(51.8) | 1.21(0.84–1.74) | |
| Single | 290(48.2) | Ref | |
| Diagnosed with diabetes∗ | |||
| <5 years | 222(39.6) | Ref | Ref |
| 5–10 years | 207(37.0) | 1.82(1.18–2.81)∗∗ | 1.76(1.13–2.74) |
| >10 years | 131(23.4) | 1.73(1.06–2.82) | 1.77(1.08–2.91) |
| Type of diabetes | |||
| Type 1 | 382(68.2) | Ref | Ref |
| Type 2 | 178(31.8) | 1.36(0.94–1.98)∗∗ | 1.42(0.97–2.09) |
| HbA1c | |||
| <7 | 206(36.8) | Ref | |
| 7-9 | 273(14.5) | 1.59(0.90–2.78)∗∗ | |
| >9 | 81(48.8) | 1.58(1.04–2.40)∗∗ | |
| Any chronic disease | |||
| Yes | 271(48.4) | 1.27(0.84–1.82) | |
| No | 289(51.6) | Ref | |
| Family member having COVID-19 | |||
| Yes | 238(42.5) | 0.93(0.60–1.35) | |
| No | 322(57.5) | Ref | |
| Exposed to COVID-19 | |||
| Yes | 78(13.9) | 1.30(0.80–2.12) | |
| No | 482(86.1) | Ref | |
| Been with someone with COVID-19 | |||
| Yes | 187(33.4) | 1.13(0.77–1.65) | |
| No | 373(66.6) | Ref | |
| History of taking influenza vaccine∗ | |||
| Yes | 273(48.8) | 0.51(0.35–0.75) | 0.52(0.35–0.76) |
| No | 287(51.2) | Ref | Ref |
∗p value </ = 0.05 for chi square test.
∗∗p value </ = 0.25 at univariate logistic regression.
4. Discussion
This cross-sectional survey aimed to assess the vaccine hesitancy among diabetic individuals, both type 1 and 2. We found that females participated more as compared to males. Almost half of the participants had a family history of COVID-19, while almost one-fifth had already suffered from COVID-19. 71% supported COVID-19 vaccination, while the main reasons behind vaccine hesitancy included its fast production, insufficient vaccine trials, and an uncertainty towards genetic components. Participants reported that the ministry website was their main source of information. The adjusted models with the candidate variables, female gender, longer duration of diabetes, and no history of influenza vaccine remained significantly associated with COVID vaccine uptake. Several recent research articles have shown an increased vulnerability to severe COVID-19 illness in diabetic patients as compared to non-diabetic patients [15,21,22]. For instance, patients with diabetes have three times more chances of hospitalization, the severity of illness, and in-hospital mortality [15,22]. Even good glycemic control (HbA1c before hospitalization) has not been steadily associated with improved outcomes in patients with diabetes admitted to the hospital for COVID-19 [23].
Regarding the vaccination acceptance, we found mixed results. Around two-third were willing or had already vaccinated against COVID-19. Similarly, almost 3/4th of the participants with diabetes supported COVID-19 vaccination. These acceptance rates are similar to most of the general population surveys [1]. However, these were conducted among the general population. These acceptance rates are higher than previously reported rates, showing that 48% and 64% of participants were willing or showed their intention to vaccinate [24,25]. Low uptake rates were reported from Middle East, Africa, some European countries, and Russia among the general population [1]. Studies have shown that overall only a 29.4% vaccine acceptance rate is found in Saudi Arabia, Jordan, and Kuwait [20].
While investigating, we found that the reasons behind vaccine hesitancy include relatively fast production, insufficient vaccine trial, and uncertainty towards genetic components. Almost half of the participants revealed that they received information from television, social media, and ministry website. Social media displayed and circulated misinformation which lead to an increased anxiety and vaccine hesitancy. A large global cross-sectional analysis reported a significant association between foreign disinformation campaigns (anti-vaccination) and decreasing vaccination rates [26]. Similarly, the use of social media to disseminate offline messages is highly associated with the public's belief that vaccines are unsafe. A study found that only YouTube, about 27.5% content about COVID-19 contained misinformation and non-factual information and it had garnered millions of views [27]. Several pieces of research have shown that anti-vaccine and pro-vaccine content differs by platform, but the misinforming content and anti-vaccine content gains more traction among users than its counterpart [28].
Females supported vaccine uptake almost twice as significantly as compared to males. This is consistent with another study where male participants were more hesitant than women regarding vaccine uptake [29]. In contrast, most studies have showed male dominance related to vaccine acceptance [20,30]. Past vaccination has been linked with vaccine intention. Participants who had a history of taking the influenza vaccine did not support the COVID-19 vaccine as compared to those with no such history. In contrast, a study conducted in the UK showed that individuals who had received influenza vaccination showed significant intention to be vaccinated against corona-virus [31]. However, these results are not consistent with other general public studies in which individuals who previously refused any vaccination were less likely to accept the COVID-19 vaccine [30]. This might be due to the previous experience with the vaccination and its side effects.
Participants who have diabetes for 5–10 or more years were twice more inclined towards vaccine uptake than participants with newly diagnosed diabetes (<5 years). Although most of the participants had type 1 diabetes, they were less willing to take the vaccine as compared to type 2 diabetic participants. However, this association was not significant. A significant number of participants who had higher HbA1c levels (>9%) were more eager to vaccinate than those with lower HbA1c levels (<7%). Hitherto, there is little to no information regarding the vaccine acceptance rate in the diabetic population. Another study reported 14.2% vaccine hesitancy among type 2 diabetic patients, most of whom were afraid of previous adverse events or denied vaccinating [32]. Furthermore, rates of reluctance to be vaccinated among patients with diabetes were also seen for influenza vaccination as well [33].
A crucial challenge after the availability of COVID-19 vaccination is the prioritization of groups after healthcare workers as the supply of vaccination is limited for the time being [34]. The covid-age specific mortality risk is higher in younger individuals with diabetes as compared to older. Additionally, higher BMI, duration of diabetes, glycemic control, comorbidities, and type of diabetes further modify COVID-19 risk individually [35]. In this critical time, group-level prioritization is necessary, which is so far what most of the governments have initiated [21]. The WHO Strategic Advisory Group of Experts (SAGE) and Advisory Committee on Immunization Practices (ACIP) priorities vaccination of individuals aged 16–64 years with morbidities which increased risk of complication from COVID-19, and among them, diabetes is one of the medical conditions [36,37]. Similarly, Diabetes UK has also given priority COVID-19 vaccination to individuals with diabetes [38]. Although the Saudi government took a preemptive approach right from the start of the pandemic for curtailment of virus spread, such efforts in themselves are not adequately sufficient. A swift roll-out of the COVID-19 vaccine thus remains a crucial part of a country's overall scheme for putting an end to the pandemic [24]. Results from studies carried out at a national level indicate that uncertainty around vaccines and the general population's hesitation present a significant challenge against the goal of achieving universal coverage required to create herd immunity [39]. Therefore, while designing a vaccination program, it is utterly important to keep vaccine willingness in Saudi Arabia in mind since its healthcare system is publicly funded and corona-virus-related testing and treatment facilities are provided to all Kingdom residents free of cost.
Some limitations of the study include sample representativeness. The survey sample does not include the whole diabetic population, and neither was its representative sample of the general Saudi population. For instance, it consists of a fraction of patients with diabetes participated through an online survey. However, we include participants of all regions of Saudi Arabia.
5. Conclusion
Primary prevention that is timely vaccination and protective measures are the mainstays for alleviating the COVID-19 risk in patients with diabetes. The current study investigates vaccine acceptance in finer detail by exploring more elements like past behavior about vaccinations, health conditions pertaining to the glycemic index, and support for compulsory inoculation. It has become important to assess the diabetic population's acceptance of vaccines at this time since most of the studies were done before the availability of vaccines. This study will help public policy-makers in drafting an evidence-based and informed communication strategy that will be more helpful in bolstering the public's confidence in the vaccine, consequently improving the overall vaccine uptake in the Kingdom. It has become somewhat clear now that, as is the case with all coronaviruses, inoculation will remain the only effective way for controlling COVID-19 as well, and it is unlikely that any specific or drug-based treatment will be available in the near to medium-term future. Hence it is imperative that due efforts are made for increasing vaccine willingness, and the availability of precise information holds the key to the success of such efforts. Otherwise, the state will have to continue to funnel in resources towards post-on-set management of disease, consuming a lot more resources than preventive measures like vaccination.
Availability of data and materials
The dataset generated and analysed to support this study's findings was present within the study results.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contribution
All authors contributed equally to data collection, writing and analyzing the results. The final draft of the manuscript has been approved by all authors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This publication was supported by the Deanship of Scientific Research, Prince Sattam bin Abdulaziz University, Al-Kharj, Saudi Arabia.
References
- 1.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel) 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Organization W.H. World Health Organization; 2019. Ten health issues WHO will tackle this year. [Google Scholar]
- 3.Organization WH. COVID-19 vaccines 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines Available from:
- 4.Palamenghi L., Barello S., Boccia S., GJEjoe Graffigna. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. 2020;35:785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Lane S., MacDonald N.E., Marti M., Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine. 2018;36:3861–3867. doi: 10.1016/j.vaccine.2018.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagner A.L., Masters N.B., Domek G.J., Mathew J.L., Sun X., Asturias E.J. Comparisons of vaccine hesitancy across five low-and middle-income countries. Vaccine. 2019;7:155. doi: 10.3390/vaccines7040155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karafillakis E., Larson H. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35:4840–4850. doi: 10.1016/j.vaccine.2017.07.061. [DOI] [PubMed] [Google Scholar]
- 9.Karlsson L.C., Soveri A., Lewandowsky S., Karlsson L., Karlsson H., Nolvi S. Fearing the disease or the vaccine: the case of COVID-19. Pers Indiv Differ. 2021;172:110590. doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olagoke A.A., Olagoke O.O., Hughes A.M. Intention to vaccinate against the novel 2019 coronavirus disease: the role of health locus of control and religiosity. J Relig Health. 2021;60:65–80. doi: 10.1007/s10943-020-01090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. The Lancet Regional Health-Europe. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Larson H., de Figueiredo A., Karafillakis E., Rawal M. vol. 10. Publications Office of the European Union; Luxembourg: 2018. State of vaccine confidence in the EU 2018; p. 241099. [Google Scholar]
- 13.Klekotka R.B., Mizgała E., Król W. The etiology of lower respiratory tract infections in people with diabetes. Advances in Respiratory Medicine. 2015;83:401–408. doi: 10.5603/PiAP.2015.0065. [DOI] [PubMed] [Google Scholar]
- 14.Alguwaihes A.M., Al-Sofiani M.E., Megdad M., Albader S.S., Alsari M.H., Alelayan A. Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: a single-centre retrospective study. Cardiovasc Diabetol. 2020;19:1–12. doi: 10.1186/s12933-020-01184-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gregory J.M., Slaughter J.C., Duffus S.H., Smith T.J., LeStourgeon L.M., Jaser S.S. COVID-19 severity is tripled in the diabetes community: a prospective analysis of the pandemic's impact in type 1 and type 2 diabetes. Diabetes Care. 2021;44:526–532. doi: 10.2337/dc20-2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aldossari K.K. Diabetes mellitus is an important predictor for hospitalization and mortality from the COVID-19 infection: a substantial interface between two outbreaks. Journal of Endocrinology and Metabolism. 2020;10:74–78. [Google Scholar]
- 17.Li J., Wang X., Chen J., Zuo X., Zhang H., Deng A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metabol. 2020;22:1935–1941. doi: 10.1111/dom.14057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ren H., Yang Y., Wang F., Yan Y., Shi X., Dong K. Association of the insulin resistance marker TyG index with the severity and mortality of COVID-19. Cardiovasc Diabetol. 2020;19:1–8. doi: 10.1186/s12933-020-01035-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dennis J.M., Mateen B.A., Sonabend R., Thomas N.J., Patel K.A., Hattersley A.T. Type 2 diabetes and COVID-19–Related mortality in the critical care setting: a national cohort study in England, March–July 2020. Diabetes Care. 2021;44:50–57. doi: 10.2337/dc20-1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sallam M., Dababseh D., Eid H., Al-Mahzoum K., Al-Haidar A., Taim D. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9:42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGurnaghan S.J., Weir A., Bishop J., Kennedy S., Blackbourn L.A.K., McAllister D.A. Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland. The Lancet Diabetes & Endocrinology. 2021;9:82–93. doi: 10.1016/S2213-8587(20)30405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barron E., Bakhai C., Kar P., Weaver A., Bradley D., Ismail H. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. The lancet Diabetes & endocrinology. 2020;8:813–822. doi: 10.1016/S2213-8587(20)30272-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cariou B., Hadjadj S., Wargny M., Pichelin M., Al-Salameh A., Allix I. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. 2020;63:1500–1515. doi: 10.1007/s00125-020-05180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Mohaithef M., Padhi B.K. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qattan A., Alshareef N., Alsharqi O., Al Rahahleh N., Chirwa G.C., Al-Hanawi M.K. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. 2021;8:83. doi: 10.3389/fmed.2021.644300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Global Health. 2020;5 doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li H.O.-Y., Bailey A., Huynh D., Chan J. YouTube as a source of information on COVID-19: a pandemic of misinformation? BMJ global health. 2020;5 doi: 10.1136/bmjgh-2020-002604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Puri N., Coomes E.A., Haghbayan H., Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccines Immunother. 2020;16:2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alfageeh E.I., Alshareef N., Angawi K., Alhazmi F., Chirwa G.C. Acceptability of a COVID-19 vaccine among the Saudi population. Vaccines. 2021;9:226. doi: 10.3390/vaccines9030226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sherman S.M., Smith L.E., Sim J., Amlôt R., Cutts M., Dasch H. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccines Immunother. 2020:1–10. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guaraldi F., Montalti M., Di Valerio Z., Mannucci E., Nreu B., Monami M. Rate and predictors of hesitancy toward SARS-CoV-2 vaccine among type 2 diabetic patients: results from an Italian survey. Vaccines. 2021;9:460. doi: 10.3390/vaccines9050460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verger P., Bocquier A., Vergélys C., Ward J., Peretti-Watel P. Flu vaccination among patients with diabetes: motives, perceptions, trust, and risk culture - a qualitative survey. BMC Publ Health. 2018;18:569. doi: 10.1186/s12889-018-5441-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powers A.C., Aronoff D.M., Eckel R.H. COVID-19 vaccine prioritisation for type 1 and type 2 diabetes. The Lancet Diabetes & Endocrinology. 2021;9:140–141. doi: 10.1016/S2213-8587(21)00017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Holman N., Knighton P., Kar P., O'Keefe J., Curley M., Weaver A. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. The lancet Diabetes & endocrinology. 2020;8:823–833. doi: 10.1016/S2213-8587(20)30271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anesi J. The advisory Committee on Immunization practices' updated interim recommendation for allocation of COVID-19 vaccine—United States, December 2020. Am J Transplant. 2021;21:897. doi: 10.1111/ajt.16480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pal R., Bhadada S.K., Misra A. COVID-19 vaccination in patients with diabetes mellitus: current concepts, uncertainties and challenges. Diabetes & Metabolic Syndrome: Clin Res Rev. 2021;15:505–508. doi: 10.1016/j.dsx.2021.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coronavirus vaccines and diabetes. https://www.diabetes.org.uk/about_us/news/coronavirus-vaccines Available from:
- 39.Almohaithef M.A., Padhi B.K., Ennaceur S.A. medRxiv; 2021. Demographics of COVID19 vaccine hesitancy during the second wave of COVID-19 pandemic: a cross-sectional web-based survey in Saudi Arabia. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset generated and analysed to support this study's findings was present within the study results.