Abstract
Introduction
The COVID-19 (coronavirus disease 2019)-related pandemic represents a global source of societal and health burden. Yet, the impact of the pandemic on people with severe mental illness, including bipolar disorder (BD), remains unclear, warranting scoping review on the matter.
Methods
The MEDLINE and EMBASE databases were systematically searched from inception up to April 24, 2021, adopting broad inclusion criteria to assess a variety of clinical and public health themes related to people with a primary diagnosis of BD during the COVID-19 pandemics. The present work complying with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) registered in the Open Science Framework (OSF) repository (https://osf.io/7evpx/).
Results
Fourteen papers informed the present scoping review. Four major themes were identified: (i) impact of COVID-19-related stressors on BD; (ii) impact of COVID-19 on mental health service utilization among people with BD; (iii) impact of BD on the risk of acquiring SARS-CoV-2 infection; (iv) engagement in preventative behaviors among people with BD. Additional themes warranting further research were nonetheless detected.
Limitations
Further original studies are needed.
Conclusion
The present study confirmed the high-vulnerability hypothesis concerning people with BD versus the general population, reinforcing the need for further research related to the COVID-19 pandemic. Additional information is warranted to compare the impact of the pandemic period among BD people against pre-pandemic records, the general population, and other severe mental illnesses, namely people with schizophrenia or major depressive disorder, to inform the public health and the delivery of patient-tailored interventions.
1. Introduction
The ongoing COVID-19 (coronavirus disease 2019) pandemic has had an overwhelming deleterious impact on the lives and care of people with severe mental illnesses – SMIs - including bipolar disorders – BDs (Hernández-Gómez et al., 2021; Kozloff et al., 2020). For instance, social distancing regulations and lockdowns may decrease social support and increase loneliness (Smith and Lim, 2020), and may also increase the risk of irregular social and circadian rhythms (Murray et al., 2020; Xue et al., 2020). The burden posed by such downstream outcomes seems particularly relevant to vulnerable populations, such as people living with BD and related conditions. In addition, at least some of the measures employed to control the COVID-19 pandemic may have led to maladaptive coping in a substantial subset of people with BD. These include increased screen time, increased consumption of convenience junk foods (Zajacova et al., 2020) and decreased exercise as well as increased consumption of alcohol and tobacco smoking in some countries which may compromise the course of illness in people living with BDs (Reynolds et al., 2021). People also had reduced access to care for non-primary COVID-19-related conditions, including BD, further compromising long-term adherence to care. In theory, this may inflate the risk for recurring affective episodes and/or suicidal behaviors and the burden posed to caregivers of people with BD (Stefana et al., 2020).
BD is also a well-known risk factor for suicidality (Dong et al., 2019), and the socio-economic impact of the COVID-19 pandemic might have increased suicidality in this population (Banerjee et al., 2021; Phiri et al., 2021). However inconsistent data and ongoing debate exist on this matter, at least in the general population worldwide (Pirkis et al., 2021). Overall, SARS-CoV-2 may inflate the risk for suicidality due to interaction with biological pathways, including central and systemic inflammation (Conejero et al., 2021). Furthermore, a pre-COVID-19 diagnosis of SMI may increase the severity and mortality associated with the SARS COV-2 infection (Toubasi et al., 2021). Finally, there is a recognized gap in the prevention and treatment of physical health comorbidities in people with SMIs (Firth et al., 2019), and concerns have been raised that people with SMI may be less likely to be vaccinated against COVID-19 compared to the general population (Mazereel et al., 2021; Smith et al., 2021).
The COVID-19 pandemic has also dramatically changed the landscape of care for people with SMIs, including BD. For example, a survey of 17 countries has found that the legislation for telepsychiatry has dramatically changed after the COVID-19 pandemic (Kinoshita et al., 2020). Those changes have accelerated the learning curve of the emerging field of digital mental health even though evidence in this area remains limited (Torous et al., 2020). In addition, the COVID-19 pandemic may increase the stigma faced by people with SMI, including BD (Chaimowitz et al., 2021; Lohiniva et al., 2021). The COVID-19 pandemic has also had a tremendously detrimental impact on the mental health of the health care workforce (mainly of frontline workers) (Busch et al., 2021). Arguably, this may also be a driving force for the provision of suboptimal care for people living with SMIs, including BD.
Finally, it has been hypothesized that some psychotropic medications, particularly lithium and fluvoxamine, may play a protective role against the COVID-19 infection (Javelot et al., 2020; Murru et al., 2020). Among other implications, people with BD who fail to receive or to comply with their pharmacological regimen may thus theoretically be more vulnerable to COVID-19 than their treated counterparts.
The goal of the present report is to explore the available evidence and the existing gaps concerning the implications of the COVID-19 pandemic on people with BD. We have decided a priori to focus on BD because this SMI has psychopathological features (for example, affective instability) that may be uniquely and deleteriously influenced by the ongoing pandemic. Since there are several possible interfaces between the COVID-19 pandemic and BD, we have decided to conduct a scoping review of this topic, to pave the ground towards the subsequent design of systematic reviews of the literature in one or more areas under investigation.
2. Methods
A scoping review of the literature on the implications of the COVID-19 pandemic for people with a primary diagnosis of BD was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) statement (Tricco et al., 2018). This statement, developed by expert consensus through a Delphi panel, contains a checklist of 20 essential reporting items and 2 optional items, which is an optimal part of the methodology of all scoping reviews. There is currently a wide heterogeneity of scoping review methodologies, and these varying methodologies are of mixed quality (Tricco et al., 2016). Thus, compliance to the PRISMA-ScR statement represents an essential step to enhance the methodological consistency and uptake of research findings across scoping reviews. The protocol for this scoping review was registered a priori with the Open Science Framework (OSF) repository at: https://osf.io/7evpx/.
2.1. Identification of the research questions
We developed a broad research question for our literature search, asking: “How does the literature inform us about the impact of the COVID-19 pandemic among people with BD?” People with BD represent a vulnerable population, and little is known about the illness course and care during the pandemic. We specifically focused on the following sub-questions, to narrow our inquiry:
-
(1)
What are the effects of pandemic-related social isolation, restrictions, or lifestyle changes on the mental health of people with BD?
-
(2)
What are the barriers to seeking and providing care to people with BD in the COVID-19 era, and what is the likelihood of getting vaccinated against the infection compared to general population counterparts?
-
(3)
What is the prevalence of SARS-CoV-2 infection and the risk of its transmission among people with BD compared to the general population?
-
(4)
What are the possible causes for the different clinical course of BD in people with co-occurring COVID-19, and what are the available solutions?
-
(5)
What is known about the potential pharmacological interactions between the drugs usually used for the treatment of BD and those employed in the treatment of the COVID-19 infection?
2.2. Identification of the relevant studies
For the present scoping review, we included studies of any design that involved people with BD, except narrative reviews and preclinical studies. A diagnosis of BD had to be established by either of the two methods: (1) a coded diagnosis according to major diagnostic criteria, such as the International Classification of Diseases (ICD), or the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria; (2) a structured or semi-structured diagnostic interview based on major diagnostic criteria. No language restriction was applied. Authors were electronically contacted on at least two occasions to obtain necessary data unless already available in the abstracts or the retrieved full-text reprints. We performed a systematic literature search in the MEDLINE and EMBASE databases from inception up to April 24th, 2021. Please refer to Supplementary material n.1 for details about the adopted search strategy. Three investigators (MF, MDP, and MBi) screened the retrieved references for eligibility both at the title/abstract and full-text levels. Disagreements were resolved through consensus with a senior author involved in the present study (AFC).
3. Results
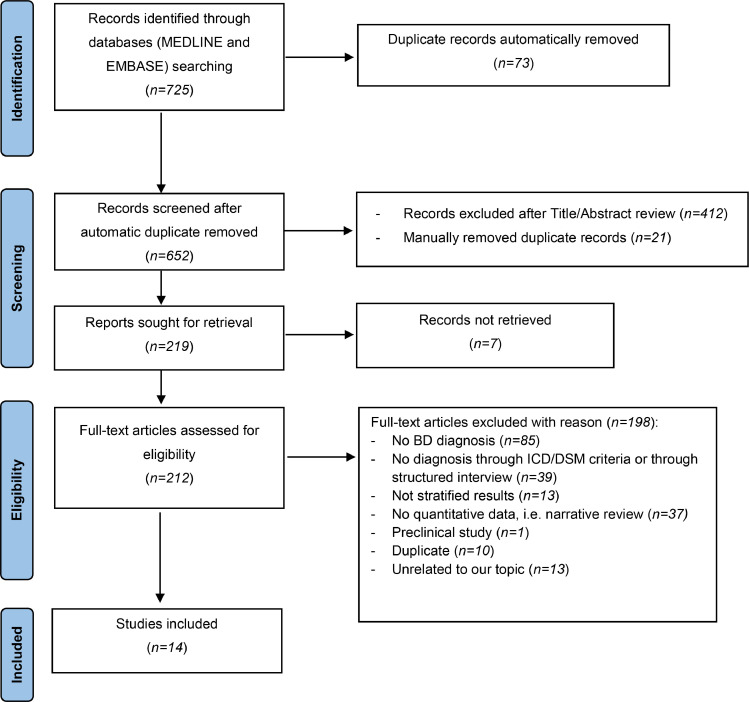
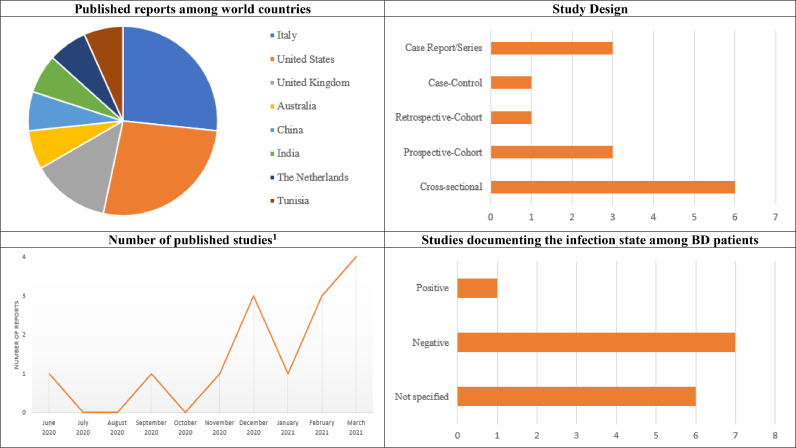
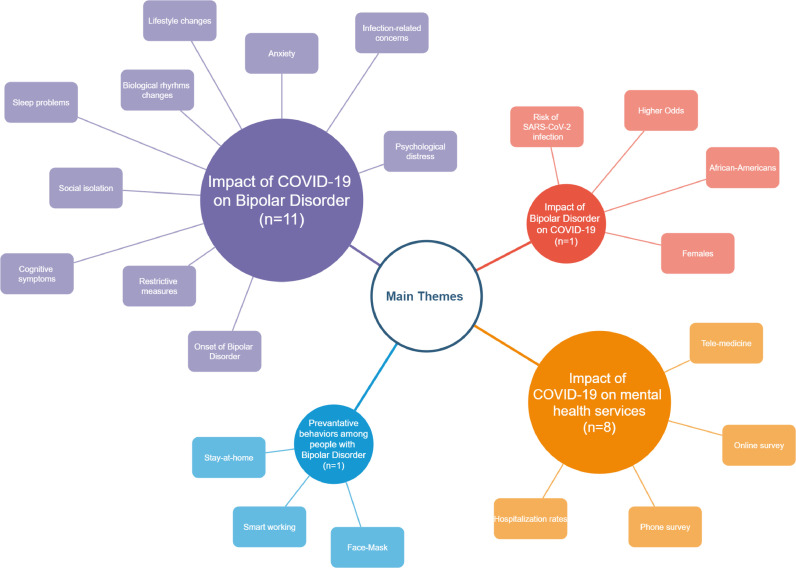
Overall, 725 records were identified across different sources, returning 652 references after automatic exclusion of duplicate records, which underwent further screening. Of these, 440 studies were excluded at the title/abstract level, and an additional 198 records were excluded following full-text review, as detailed in the Supplementary material n.2. A total of 14 studies (Ackerman et al., 2020, 2021; Carmassi et al., 2020; Carta et al., 2021; Dattoli et al., 2020; Karantonis et al., 2021; Korten et al., 2021; Lazzari et al., 2020; McBride et al., 2021; Tundo et al., 2021; Uvais, 2020; Wang et al., 2021; Yin et al., 2020; Yocum et al., 2021) were eligible for inclusion. Please refer to Fig. 1 (study flow) and Table 1 for additional details. Among the included studies, 6 studies (Ackerman et al., 2020; Carmassi et al., 2020; Dattoli et al., 2020; Lazzari et al., 2020; Uvais, 2020; Yin et al., 2020) were published in 2020, and 8 studies (Ackerman et al., 2021; Carta et al., 2021; Karantonis et al., 2021; Korten et al., 2021; McBride et al., 2021; Tundo et al., 2021; Wang et al., 2021; Yocum et al., 2021) were published in the year 2021. A total of 6 studies (Carmassi et al., 2020; Dattoli et al., 2020; Korten et al., 2021; Lazzari et al., 2020; McBride et al., 2021; Tundo et al., 2021) were conducted in Europe, 4 studies (Ackerman et al., 2020, 2021; Wang et al., 2021; Yocum et al., 2021) in North America, 2 studies (Uvais, 2020; Yin et al., 2020) in Asia, one study (Karantonis et al., 2021) in Oceania, and one study included two different samples from independent geographical regions (Europe and Africa) (Carta et al., 2021). Concerning study designs, 6 studies (Ackerman et al., 2021; Carmassi et al., 2020; Dattoli et al., 2020; Karantonis et al., 2021; McBride et al., 2021; Tundo et al., 2021) were cross-sectional, 3 studies (Carta et al., 2021; Korten et al., 2021; Yocum et al., 2021) were prospective cohort studies, one study(Ackerman et al., 2020) was a retrospective cohort study, and one study (Wang et al., 2021) was a case-control study, and 3 studies (Lazzari et al., 2020; Uvais, 2020; Yin et al., 2020) were case reports/series. The diagnosis of BD was validated according to the DSM-5 by 8 studies (Ackerman et al., 2020, 2021; Carmassi et al., 2020; Carta et al., 2021; Dattoli et al., 2020; Tundo et al., 2021; Uvais, 2020; Yin et al., 2020), the DSM-IV or DSM-IV-TR in 3 studies (Karantonis et al., 2021; Korten et al., 2021; Yocum et al., 2021), and the ICD-10 in 3 studies (Lazzari et al., 2020; McBride et al., 2021; Wang et al., 2021); additionally, the Mini-International Neuropsychiatric Interview (MINI) was adopted in 4 studies (Ackerman et al., 2020, 2021; Karantonis et al., 2021; Korten et al., 2021), and the Structured Clinical Interview for DSM-5 (SCID-5) was used in one study (Tundo et al., 2021). The majority of the studies (Ackerman et al., 2020, 2021; Carmassi et al., 2020; Carta et al., 2021; Dattoli et al., 2020; Karantonis et al., 2021; Korten et al., 2021; Tundo et al., 2021; Uvais, 2020; Yocum et al., 2021) were conducted on outpatients, 3 studies (Lazzari et al., 2020; McBride et al., 2021; Yin et al., 2020) were conducted among hospitalized patients, and one study (Wang et al., 2021) has enrolled a mixed sample. Please, see Fig. 2 for additional details. The main themes abstracted from the included papers to answer our a-priori defined sub-questions were: (i) the impact of COVID-19-related stressors on BD (n = 11); (ii) the impact of COVID-19 on mental health services (n = 8); (iii) the impact of BD on the risk of Sars-CoV-2 infection (n = 1), and (iv) the engagement on preventative behaviors among people with BD (n = 1). Sub-questions n.4,5 could not be addressed, while sub-questions n.2,3 could only be partially answered. Please, see Fig. 3 for additional details. Each study was coded according to its relevance to the selected themes. Finally, the PRISMA ScR checklist has been completed (see supplementary material n.3).
Fig. 1.
Study flow based on the 2020 flow diagram for new systematic reviews which included searches of databases and registers only.
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71.
For more information, visit: http://www.prisma-statement.org/
Table 1.
characteristics of the included studies.
| Reference | Month, Year of publication | Country | Study population | Aim of the study | Main results of interest | Measurement |
|---|---|---|---|---|---|---|
| Cross-sectional Studies | ||||||
| (Dattoli et al., 2020) | December 2020 | Italy | 53 adult BD outpatients who were in euthymia for at least six months. | To evaluate the psychological impact of the pandemic in a cohort of remitted patients affected by mood disorders, and to analyze serum 25(OH)D levels as a potential predictive factor influencing the extent of psychological burden. | 19 BD patients reported no psychological distress, 17 BD patients reported mild psychological distress, and 17 BD patients reported moderate-to-severe psychological distress. Compared to the other patients included in the sample affected by the major depressive disorder, BD patients showed significantly lower psychological distress (p = 0.04). In addition, low serum 25(OH)D levels significantly predicted psychological distress severity, but the results were not stratified according to the psychiatric diagnosis. | The diagnoses were made according to DSM-5. The authors adopted the K-10 scales. |
| (McBride et al., 2021) | March 2021 | United Kingdom | 28 adult BD inpatients (12 admitted during 2019 and 16 admitted during 2020). | To assess the impact of the COVID-19 pandemic on acute adult mental health services during 4 weeks starting on March 16, 2020. | 16 BD patients were admitted to a Mental Health Unit from March 16, 2020, to April 16, 2020, and 12 BD patients were admitted to the same Mental Health Unit from March 16, 2019, to April 16, 2019. | The diagnoses were made according to ICD-10. |
| (Carmassi et al., 2020) | December 2020 | Italy | 100 adult BD outpatients (64 females), of whom one was positive to Sars-CoV-2 infection, 32 had a close one at risk of the Sars-CoV-2 infection, 8 had a relative or a close one positive to Sars-CoV-2 infection, and 3 lost a relative or a close one due to COVID-19. Additionally, 23 patients reported a comorbid GAD diagnosis, and 8 patients had comorbid OCD. | To assess and investigate the post-traumatic stress symptoms developed by BD patients in response to the COVID-19 emergency and the possible factors associated with them. The study was conducted in a telepsychiatry setting due to the lockdown and social-distancing measures. | 17 patients reported post-traumatic stress symptoms. Particularly, these were significantly higher in females and in patients who reported work or financial difficulties due to the lockdown. Subjects with post-traumatic stress symptoms showed significantly higher GAD-7 and HAM-D scores. 26 subjects showed moderate to severe anxiety symptoms, of whom 10 (58.8%) showed post-traumatic stress symptoms, compared to 16 (19.3%) who did not (p < 0.01). Moderate/severe depressive symptoms were reported by 17 subjects, of whom 7 (41.2%) showed post-traumatic stress symptoms, compared to 10 (12%) who did not (p < 0.01). In a logistic regression model, the working and economic difficulties, the GAD-7 and YMRS total scores significantly predicted the post-traumatic stress symptoms. | The diagnoses were made according to DSM-5. The authors adopted the IES-r, GAD-7, HAM-D, and YMRS scales. |
| (Karantonis et al., 2021) | March 2021 | Australia | 43 adult BD outpatients (25 BD-I, 7 BD-II, and 11 BD-NOS; 24 females), in any current mood polarity. | To identify the extent to which manic and depressive symptoms, COVID-19 related anxiety, lifestyle and social rhythms changes, subjective cognitive functioning, quality of life, and mental health support use, had been affected by the pandemic in Australian BD patients compared to 24 healthy controls. | BD patients had significantly higher scores on the DASS-21 anxiety (p = 0.04) and stress (p = 0.05) subscales, as well as on the COBRA (p < 0.01). BD participants reported significantly increased suicidal thoughts since the pandemic began (p = 0.01). Scores on the QOLBD were significantly lower in BD patients (p = 0.02). However, only the COBRA retained its significance after multiple comparison corrections. | The diagnoses were made according to DSM-IV and validated through MINI. The authors adopted the SRMI, DASS-21, QOLBD, and COBRA scales. |
| (Ackerman et al., 2021) | February 2021 | USA | 69 adult BD outpatients (49 females). | To identify the prevalence of engaging in specific preventative behaviors (social distancing, smart-working, avoiding public spaces, handwashing, wearing facemasks), among individuals with severe mental illnesses and to examine demographic and psychological factors, such as COVID-19-related anxiety, which may contribute to preventative actions. | BD patients were more likely to use face masks (p = 0.02), to stay home as a precautionary measure (p = 0.03), and to work remotely (p < 0.01), compared to people with a schizophrenia spectrum disorder. The difference remained significant also when limiting the sample to those with reported employment (p < 0.01). These patients did not differ in positively endorsing self-distancing, avoiding in-person visits with friends/family, handwashing or using sanitizer, and cleaning/disinfecting. | The diagnoses were made according to DSM-5 and validated through MINI. The authors adopted the YMRS, MADRS, PANSS, and SUMD scales. |
| (Tundo et al., 2021) | March 2021 | Italy | 194 adult BD outpatients (83 BD-I, 111 BD-II). | To examine in a clinical setting the psychological and psychopathological impact of COVID-19 stress on outpatients with pre-existing BD. | 6 BD-I (7.2%) patients and 4 BD-II (3.6%) patients experienced a relapse or symptoms worsening related to pandemic stress, while 77 BD-I (92.8%) patients and 107 BD-II (96.4%) patients did not. | The diagnoses were made according to DSM-5 and validated through SCID5. The authors adopted the HAM-D, YMRS scales, and a semi-structured interview to evaluate the impact of pandemic stress. |
| Prospective-Cohort Studies | ||||||
| (Korten et al., 2021) | January 2021 | The Netherlands | 81 older adults BD outpatients (45 females). | To assess the impact of social isolation, COVID-19-related concerns, and loneliness on the psychiatric symptoms. In addition, the association between coping styles, neuroticism, and psychiatric symptoms were investigated. Two study times were considered (T0 considering years 2017 and 2018, and T1 considering the year 2020). | Participants showed fewer psychiatric symptoms at T1 (67.9% euthymic) compared to T0 (40.7% euthymic). There was no difference in loneliness between T1 and T0. Not having children, more feelings of loneliness, lower mastery, passive coping style, and neuroticism were associated with more psychiatric symptoms during T1. | The diagnoses were made according to DSM-IV and validated through MINI. The authors adopted the YMRS, BAI, and CES-D scales. |
| (Yocum et al., 2021) | March 2021 | USA | 345 adults BD outpatients from the Pretcher Bipolar Longitudinal Cohort. | To assess the impact of SARS-CoV-2 pandemic and lockdown on individuals with BD in comparison to healthy controls, and to compare pandemic data with pre-pandemic data. | At the beginning (April 30, 2020, 5-weeks into the lockdown), BD subjects were more likely to experience pandemic-related stress (OR=3.74, p < 0.01), to take more than 30 min to fall asleep (OR=3.55, p < 0.01), to have bad sleep quality (OR=2.64, p < 0.01), to take sleep medication (OR=5.36, p < 0.01), to report higher PHQ-9 score and GAD-7 scores (p < 0.01), compared to healthy controls. BD patients reported an improvement of these disruptions over time, but more slowly than healthy controls. When comparing symptoms severity measures collected from the current pandemic era to those from the pre-pandemic period (5 years before 2020), healthy controls show a higher symptom increase than BD patients. BD patients, compared to the pre-pandemic era, showed not significantly higher PHQ-Q and GAD-7 scores. | The diagnoses were made according to the DSM-IV. The authors adopted the CIS, PHQ-9, GAD-7, and PSQI scales. |
| (Carta et al., 2021) | February 2021 | Italy; Tunisia | 40 adult BD outpatients (26 BD-II; 28 females) from the Italian sample, and 30 adult BD outpatients (17 BD-II; 16 females) from the Tunisian sample. | To examine the impact of restriction measures and lockdown due to the COVID-19 pandemic, in terms of daily habits and circadian rhythms alterations, on the clinical course of BD. Two samples were recruited, one from Cagliari, Italy, and one from Tunis, Tunisia, since people from these two countries were experiencing different types of restriction measures. The two cohorts were studied in April 2020 (T0) and in June 2020 (T1). | 18 patients from the Italian sample compared to 0 patients from the Tunisian one had a HAM-D score > 14 at T0 (p < 0.01). 14 patients from the Italian sample compared to 0 patients from the Tunisian one had HAM-D score > 14 at T1 (p < 0.01). BRIAN subscales (Sleep, Activity, and Social), and total scores, were significantly different among the two samples in the two periods considered (T0 and T1), and these differences were higher for the Italian sample. The subgroup with higher HAM-D scores showed significantly higher BRIAN scores. | The diagnoses were made according to DSM-5. The authors adopted the HAM-D and the BRIAN scales. |
| Retrospective-Cohort Studies | ||||||
| (Ackerman et al., 2020) | December 2020 | USA | 56 adult BD outpatients (35 with psychotic features and 21 without) were recruited from ongoing ecological momentary assessment studies. | To compare pre-pandemic symptom ratings to the ones collected in the pandemic period, to identify the impact of the pandemic on mental health among individuals with preexisting severe mental illness. | BD patients showed significantly higher well-being and substance use (p < 0.05) during the pandemic period compared to the pre-pandemic one. No significant difference was found about the sad/depressed, energized/excited, happy, hearing voices, paranoia, and sleep symptoms in these two timeframes. | The diagnoses were made according to DSM-5 and validated through MINI. The authors adopted MADRS, YMRS, PANNS, and SUMD scales. |
| Case-control Studies | ||||||
| (Wang et al., 2021) | February 2021 | USA | 930,280 adult and older adult BD inpatients and outpatients, of whom 87,270 received the diagnosis in the previous year. The data were collected by the IBM Watson Health Explorys from 360 hospitals and 317,000 providers across 50 states in the USA. | To assess the impact of mental disorder on the risk of COVID-19 infection and related mortality, and rates of hospitalization. | Patients with a recent diagnosis of BD had higher odds of being positive to SARS-CoV-2 infection than people without a mental disorder (AOR=5.72, p < 0.01). Among patients with a recent diagnosis of BD, African Americans (AOR=2.23, p < 0.01), and women (AOR=1.34, p < 0.01) had higher odds of being positive to SARS-CoV-2 infection than, respectively, Caucasian and men. | The diagnoses were made according to the ICD-10. |
| Case-report/series | ||||||
| (Lazzari et al., 2020) | September 2020 | United Kingdom | Two adult female inpatients with no previous personal or familial psychiatric history. | To assess the impact of stressful events such as the COVID-19 pandemic on mental disorders. | Fears or concerns about COVID-19 infection and lifestyle related to the pandemic can trigger new presentations of mania and psychosis, through stress induction. The two patients experienced a manic episode with psychotic features and received pharmacological interventions, with a full recovery during the hospitalization. | The diagnoses were made according to the ICD-10. The authors adopted the YMRS and CGI scales. |
| (Uvais, 2020) | June 2020 | India | A 37-year-old female BD patient experienced her last manic episode about 17 years earlier. | To assess the early impact of the COVID-19 pandemic on people with BD. | COVID-19-related concerns and social restriction may trigger a mood episode. The patient experienced a manic episode with psychotic features, and received pharmacological interventions (Sodium Valproate, 700mg/day, and Olanzapine, 7.5mg/day), with a good response after one week. | The diagnosis was made according to the DSM-5. |
| (Yin et al., 2020) | November, 2020 | China | A 32-year-old female inpatient with no previous personal or familial psychiatric history. | To assess the impact of stressful events such as quarantine on the onset of mental disorders. | The onset of the manic episode could be triggered by stressful life events, characterized by disrupting social routines and biological circadian rhythms, especially in vulnerable subjects with a hypersensitive reward system. The patient experienced a manic episode without psychotic features and received pharmacological interventions (Lithium, 900mg/day, and Quetiapine, 400mg/day), with a good response in 3 weeks. | The diagnosis was made according to the DSM-5. The authors adopted the YMRS. |
Legend: BAI= Beck Anxiety Interview; BD=Bipolar Disorder; BRIAN= Biological Rhythms Interview of Assessment in Neuropsychiatry; CES-D= Center for Epidemiologic Studies Depression Scale; CGI=Clinical Global Impressions Scale; CIS=Coronavirus Impact Scale; COBRA=14-item modified version of the Cognitive Complaints in Bipolar Disorder Rating Assessment; COVID-19= Coronavirus Disease 2019; DASS-21=21-item Depression, Anxiety, and Stress Scale; DSM=Diagnostic and Statistical Manual of Mental Disorders (…edition/revision); GAD=Generalized Anxiety Disorder; GAD-7=General Anxiety Disorder-7; HAM-D=Hamilton Depression Rating Scale; IES-r=Impact of Event Scale-Revised; K-10= Kessler 10 Psychological Distress Scale; M.I.N.I.=Mini-International Neuropsychiatric Interview; MADRS=Montgomery–Åsberg Depression Rating Scale; OCD=Obsessive-Compulsive Disorder; PANSS=Positive and Negative Syndrome Scale; PHQ-9= Patient Health Questionnaire; PSQI=Pittsburgh Sleep Quality Index; QOLBD=12-item Brief Quality of Life Scale for Bipolar Disorder; SARS-CoV-2=Severe Acute Respiratory Syndrome Coronavirus 2; SCID (either the patient or clinician edition)=Structured Clinical Interview for DSM; SRMI=48-item Self-report Mania Inventory; SUMD=Scale to Assess Unawareness of Mental Disorder; YMRS=Young Mania Rating Scale.
References for table .1: Ackerman, R.A., Pinkham, A.E., Moore, R.C., Depp, C.A., Harvey, P.D., 2020. A Longitudinal Investigation of the Effects of the COVID-19 Pandemic on the Mental Health of Individuals with Pre-existing Severe Mental Illnesses. Psychiatry Research 294, 113493.
Ackerman, R.A., Pinkham, A.E., Moore, R.C., Depp, C.A., Harvey, P.D., 2021. COVID-19-related psychological distress and engagement in preventative behaviors among individuals with severe mental illnesses. npj Schizophrenia 7, 7.
Carmassi, C., Bertelloni, C.A., Dell'Oste, V., Barberi, F.M., Maglio, A., Buccianelli, B., Cordone, A., Dell'Osso, L., 2020. Tele-Psychiatry Assessment of Post-traumatic Stress Symptoms in 100 Patients With Bipolar Disorder During the COVID-19 Pandemic Social-Distancing Measures in Italy. Frontiers in Psychiatry 11, 580736.
Carta, M.G., Perra, A., Boe, L., Lorrai, S., Cossu, G., Aresti, A., Ouali, U., Ben Cheikh Ahmed, A., Aissa, A., Nacef, F., Preti, A., 2021. Living With Bipolar Disorder in the Time of Covid-19: Biorhythms During the Severe Lockdown in Cagliari, Italy, and the Moderate Lockdown in Tunis, Tunisia. Frontiers in Psychiatry 12, 634765.
Dattoli, L., Pepe, M., Di Nicola, M., Moccia, L., Janiri, L., Sani, G., Janiri, D., Fiorillo, A., 2020. Serum 25-hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID-19 pandemic. Psychoneuroendocrinology 122, 104869.
Karantonis, J.A., Van Rheenen, T.E., Rossell, S.L., Berk, M., 2021. The mental health and lifestyle impacts of COVID-19 on bipolar disorder. Journal of Affective Disorders 282, 442–447.
Korten, N., Paans, N., de Walle, B., Sonnenberg, C., Schouws, S., Orhan, M., van Oppen, P., Kupka, R., Kok, A., Dols, A., 2021. Psychiatric symptoms during the COVID-19 outbreak in older adults with bipolar disorder. International Journal of Geriatric Psychiatry.
Lazzari, C., Nusair, A., Shoka, A., Hein, S.M., Rabottini, M., 2020. Case reports of first psychiatric presentations during CoViD-19 pandemic. Rivista di psichiatria 55, 319–321.
McBride, M., Chari, D., Alam, F., Abbas, M.J., Al-Uzri, M., Brugha, T., Kronenberg, G., Mukaetova-Ladinska, E., 2021. The early impact of the COVID-19 pandemic on acute care mental health services. Psychiatric Services 72, 242–246.
Tundo, A., Betro, S., Necci, R., 2021. What Is the Impact of COVID-19 Pandemic on Patients with Pre-Existing Mood or Anxiety Disorder? An Observational Prospective Study. Medicina (Kaunas, Lithuania) 57.
Uvais, N.A., 2020. Mania Precipitated by COVID-19 Pandemic-Related Stress. The primary care companion for CNS disorders 22.
Wang, Q., Xu, R., Volkow, N.D., 2021. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry 20, 124–130.
Yin, X., Sun, Y., Zhu, C., Zhu, B., Gou, D., Tan, Z., 2020. An Acute Manic Episode During 2019-nCoV Quarantine. Journal of affective disorders 276, 623–625.
Yocum, A.K., Zhai, Y., McInnis, M.G., Han, P., 2021. Covid-19 pandemic and lockdown impacts: A description in a longitudinal study of bipolar disorder. Journal of affective disorders 282, 1226–1233.
Fig. 2.
Number of included records by characteristics.
1 Please note that many studies herein outlined indexed in the year 2021 appaised online early in time.
Fig. 3.
Main themes covered by the included studies.
3.1. Impact of COVID-19-related stressors on bipolar disorder
In this theme, we included 11 studies (Ackerman et al., 2020; Carmassi et al., 2020; Carta et al., 2021; Dattoli et al., 2020; Karantonis et al., 2021; Korten et al., 2021; Lazzari et al., 2020; Tundo et al., 2021; Uvais, 2020; Yin et al., 2020; Yocum et al., 2021) which focused on the impact of social isolation, restrictive measures, lifestyle, and biological circadian rhythms changes due to the COVID-19 pandemic, or infection-related concerns, on the clinical course of BD. Some studies found that BD patients reported low rates of relapse or symptom worsening (Tundo et al., 2021) during the pandemic, or less severe psychiatric symptoms (Korten et al., 2021) and higher feelings of well-being (Ackerman et al., 2020) during the pandemic when compared to the pre-pandemic period. When compared to people diagnosed with major depressive disorder (MDD), BD patients exhibited lower psychological distress in one study (Dattoli et al., 2020). In two studies, people with BD were compared to healthy controls, reporting worse cognitive symptoms (Karantonis et al., 2021), more elevated pandemic-related stress, sleep difficulties, and anxiety (Yocum et al., 2021), and slower improvement after the first months of the pandemic (Yocum et al., 2021). Work-related and financial difficulties due to the lockdown, or more severe social restrictions introduced by some governments, were associated with greater psychological distress (Carta et al., 2021) or even post-traumatic stress symptoms (Carmassi et al., 2020) among people with BD in two studies. Finally, three case reports/series described the onset of manic episodes during the lockdown period in noninfected females with (Uvais, 2020) and without (Lazzari et al., 2020; Yin et al., 2020) previous psychiatric history. Overall, the authors did not report information about the infection state in 5 studies (Ackerman et al., 2020; Carta et al., 2021; Dattoli et al., 2020; Tundo et al., 2021; Yocum et al., 2021); in 6 studies (Carmassi et al., 2020; Karantonis et al., 2021; Korten et al., 2021; Lazzari et al., 2020; Uvais, 2020; Yin et al., 2020) the vast majority of the sample did not screen positive to the SARS-CoV-2 infection.
3.2. Impact of COVID-19 on mental health services utilization
In this theme, we included 8 studies (Ackerman et al., 2020, 2021; Carmassi et al., 2020; Carta et al., 2021; Dattoli et al., 2020; Karantonis et al., 2021; McBride et al., 2021; Yocum et al., 2021) which provided information on new strategies for the clinical assessment of people with BD aimed at ensuring compliance to the social-distancing measures adopted by the respective governments, or the different hospitalization rates experienced by the mental health services in the COVID-19 era. In 7 studies (Ackerman et al., 2020, 2021; Carmassi et al., 2020; Carta et al., 2021; Dattoli et al., 2020; Karantonis et al., 2021; Yocum et al., 2021), the authors specified that they evaluated the included patients in the framework of a telepsychiatry consultation (Carmassi et al., 2020) or by conducting phone (Ackerman et al., 2020, 2021; Carta et al., 2021) or online (Dattoli et al., 2020; Karantonis et al., 2021; Yocum et al., 2021) surveys. One study (McBride et al., 2021) found that during the first four weeks of the pandemic, BD patients were more likely to be hospitalized compared to the pre-pandemic period.
3.3. Impact of bipolar disorder on the risk of Sars-CoV-2 infection
One large-sampled study (Wang et al., 2021) focused on the impact of mental disorders on the risk of SARS-CoV-2 infection, and its related mortality. Patients with a recent diagnosis of BD had higher odds of screening positive for SARS-CoV-2 infection than people without a mental disorder. Among these patients, African Americans and females of any racial background had higher odds of screening positive to the SARS-CoV-2 infection than their Caucasian and male counterparts, respectively.
3.4. Engagement in preventive behaviors among people with bipolar disorder
One study (Ackerman et al., 2021) focused on the assessment of the rates of engagement in specific preventative behaviors among individuals with SMIs. It examined demographic and psychological factors such as COVID-19-related anxiety, an issue expected to affect such engagement. BD patients were more likely to wear face masks, to stay home as a precautionary measure, and to work remotely, compared to people with schizophrenia spectrum disorders. No difference was found concerning self-distancing, avoiding in-person visits with friends/family, hand washing or using sanitizer, and cleaning/disinfecting compared to people with schizophrenia-spectrum disorders.
4. Discussion
Our analysis identified four major thematic topics. A sizeable proportion of the included studies (k=9 out of 14) followed a cross-sectional/case-report/series design, which precludes any causal inferences about the association between an exposure (COVID-19 pandemics period) and a given outcome (e.g., worsening of BD symptoms). However, the following lines highlight the major areas covered in the literature and the ones warranting additional research.
4.1. Appraisal of the main themes detected by the present research
Most of the included studies (k=11 out of 14) focused on the impact of the COVID-19 pandemic on the clinical course/outcomes of BD. Overall, the included studies assessed a range of different outcomes associated with the COVID-19 pandemic among people with a primary diagnosis of BD. Although the exact role of the occupational situation and other issues related to people with a primary diagnosis of BD remains unclear, the appraised literature does not support a worsening of overall function and well-being of BD people during the pandemic compared to the pre-pandemic period, or worse outcomes compared to their MDD counterparts. An opposite trend emerged when people with BD were compared to healthy controls. People with BD possibly have already experienced high rates of stressors compared to healthy controls, thus being less prone to experience subjective worsening of mood.
Concerning the impact of the COVID-19 pandemic on the utilization of mental health services, the present review highlights a substantial dearth of evidence on the matter. Future studies need to ascertain whether people with BD experienced higher hospital admission rates compared to the pre-pandemic period, as suggested by a single study (McBride et al., 2021). In addition, future research should provide head-to-head comparisons of people with a primary diagnosis of BD compared to people with other SMIs in terms of hospital admission and telemedicine utilization rates.
Notwithstanding a very large sample (lifetime BD cases=930,280 patients out of over 61 million people), the evidence documenting the impact of BD on the risk of developing SARS-CoV-2 infection relies on a single report (Wang et al., 2021). Overall, people with BD had a higher risk of developing SARS-CoV-2 infection compared to the general population. However, the odds for people with a recent diagnosis of BD (past-year diagnosis of BD=87,270 people) seems lower than those for people with a primary diagnosis of either MDD, schizophrenia or attention-deficit hyperactivity disorder, respectively. Nonetheless, additional studies are needed to clarify the role of maintenance treatment of BD and enduring illness, as well as the onset/duration of the untreated illness of BD.
Overall, people with a primary diagnosis of BD engaged in specific preventative behaviors more than people with the schizophrenia-spectrum disorder usually did (Ackerman et al., 2021). People with BD who present prominent obsessive-compulsive traits may theoretically be more prone to engage in preventative behaviors. However, the eventual adaptive or non-adaptive role of these features is yet to be fully elucidated (Fornaro et al., 2009), warranting replication studies on the matter.
Furthermore, the present scoping review also suggests the need for additional research on specific areas of COVID-19-related issues experienced by people with a primary diagnosis of BD. Among other issues, virtually no information exists about the likelihood of BD patients to receive vaccination against COVID-19 compared to either the general population or to people living with other SMIs. The stigma surrounding people with SMI may affect their likelihood of access to general medical care. Specifically, further attention is needed concerning the different presentations of BD. In fact, mood polarity at the onset of the pandemic, a history of treatment resistance, suicidal behaviors, and the eventual compliance and availability of maintenance treatment of BD before or during the pandemic; as well as the impact of specific pharmacological or psychotherapeutic interventions on co-occurring SARS-CoV-2 remain largely unknown (Vieta et al., 2020). Little is known about hospitalization rates (both in psychiatric and general medicine units) on the course of BD living during the pandemic compared to the pre-pandemic era and the use of novel resources such as home hospitalization (Garriga et al., 2020). Conversely, the course of BD may theoretically affect the propensity of people with BD to visit their caregivers during the lockdown period, or they may complain of the reduced availability of outpatient (in-person) visits. From this perspective, the long-term role of telemedicine (Pacchiarotti et al., 2020), digital tools (Jagesar et al., 2021), and bipolar-specific internet psychotherapies (Gliddon et al., 2019) should be better appraised. Moreover, the rise of long-term consequences of Covid-19 in some patients (Miskowiak et al., 2021), particularly as regards cognitive impairment and fatigue (Llach and Vieta, 2021), could be particularly harmful to patients with BD. Finally, while most of the appraised evidence herein came from observational studies, the design of randomized clinical trials on BD samples during or after the COVID-19 pandemic is clearly a major area of unmet need. Obviously, the long-term psychosocial and immunological effects of the pandemic on people living with BD could not be captured by the present scoping review due to the limited available evidence, although such goals remain a priority for further research.
4.2. Limitations
As a scoping review, there are no inherent limitations to highlight for the present report. Additional original studies are nonetheless warranted to inform the clinical practice and public health about the management of COVID-19 or its sequalae among people with a primary diagnosis of BD.
4.3. Conclusions
The present scoping review confirmed the clinical suspicions about the overall vulnerability of people with a primary diagnosis of BD compared to the general population, as well as the compelling need for forthcoming studies specifically comparing the impact of the COVID-19 pandemic on BD patients compared to their counterparts living with other SMIs like MDD or schizophrenia. One of the benefits of knowledge synthesis is to inform areas where further research is needed. A range of different topics needs to be investigated as highlighted by this scoping review, ideally by well-designed prospective studies. In the meantime, this report provides guidance to clinical researchers, mental health practitioners as well as policymakers.
CRediT authorship contribution statement
Michele Fornaro: Visualization, Writing – review & editing. Michele De Prisco: Data curation, Writing – review & editing. Martina Billeci: Data curation, Writing – review & editing. Eleonora Ermini: Data curation, Writing – review & editing. Allan H Young: Writing – review & editing. Beny Lafer: Writing – review & editing. Jair C. Soares: Writing – review & editing. Eduard Vieta: Writing – review & editing. Joao Quevedo: Writing – review & editing. Andrea de Bartolomeis: Writing – review & editing. Kang Sim: Writing – review & editing. Lakshmi N Yatham: Writing – review & editing. Michael Bauer: Writing – review & editing. Dan J. Stein: Writing – review & editing. Marco Solmi: Writing – review & editing. Michael Berk: Writing – review & editing. Andre F. Carvalho: Visualization, Writing – review & editing.
Declaration of Competing Interest
MF, MDP, MBi, EE, BL, KS, and AFC have nothing to disclose. AHY independent research is funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. Employed by King's College London; Honorary Consultant SLaM (NHS UK). Deputy Editor, BJPsych Open. Paid lectures and advisory boards for the following companies with drugs used in affective and related disorders: AstraZeneca, Eli Lilly, Lundbeck, Sunovion, Servier, Livanova, Janssen, Allegan, Bionomics, Sumitomo Dainippon Pharma, COMPASS. Consultant to Johnson & Johnson. Consultant to Livanova. Received honoraria for attending advisory boards and presenting talks at meetings organized by LivaNova. Principal Investigator in the Restore-Life VNS registry study funded by LivaNova. Principal Investigator on ESKETINTRD3004: “An Open-label, Long-term, Safety and Efficacy Study of Intranasal Esketamine in Treatment-resistant Depression.” Principal Investigator on “The Effects of Psilocybin on Cognitive Function in Healthy Participants”. Principal Investigator on “The Safety and Efficacy of Psilocybin in Participants with Treatment-Resistant Depression (P-TRD)”. UK Chief Investigator for Novartis MDD study MIJ821A12201. Grant funding (past and present): NIMH (USA); CIHR (Canada); NARSAD (USA); Stanley Medical Research Institute (USA); MRC (UK); Wellcome Trust (UK); Royal College of Physicians (Edin); BMA (UK); UBC-VGH Foundation (Canada); WEDC (Canada); CCS Depression Research Fund (Canada); MSFHR (Canada); NIHR (UK). Janssen (UK). No shareholdings in pharmaceutical companies. JCS discloses the following (past 12-month): a. COMPASS – Research Grant; b. ALKERMES – Research Grant; c. PFIZER – Consultant; d. ALLERGAN – Research Grant; e. SUNOVIAN – Consultant; f. SANOFI – Consultant; g. JOHNSON & JOHNSON – Consultant; h. Livanova – Consultant; i. Boehringer Ingelheim – Consultant. EV has received grants and served as consultant, advisor, or CME speaker for the following entities (unrelated to the present work): AB-Biotics, Abbvie, Aimentia, Angelini, Celon, Dainippon Sumitomo Pharma, Ferrer, Gedeon Richter, GH Research, Glaxo Smith-Kline, Janssen, Lundbeck, Organon, Otsuka, Sage, Sanofi-Aventis, Sunovion, and Takeda. JQ received clinical research support from LivaNova; has speaker bureau membership with Myriad Neuroscience, Janssen Pharmaceuticals, and Abbvie; is consultant for Eurofarma; is a stockholder at Instituto de Neurociencias Dr. Joao Quevedo; and receives copyrights from Artmed Editora, Artmed Panamericana, and Elsevier/Academic Press. AdB has received research support from Otsuka, Lundbeck, Janssen Italy; Pfizer, lecture fees from Takeda, Sunovion, Lundbeck Chiesi, Roche, Mylan-Vitria. Has served as a consultant in advisor boards for Jansen, Lundbeck, Otsuka, Roche, Eli Lilly, Takeda, Recordati, Iqvia, Mylan-Vitria. LNY reported receiving honoraria or research grants from Allergan, CANMAT, Lundbeck, Otsuka, DSP, Sanofi, Intracellular Therapies, AbbVie, Merck, and Sunovion. MBa has received institutional grants from Deutsche Forschungsgemeinschaft (DFG), Bundesministerium für Bildung und Forschung (BMBF), and European Commission. He served in advisory boards for GH Research, Janssen-Cilag, neuraxpharm, Novartis, Sandoz, Shire International, Sumitomo Dainippon, Sunovion, and Takeda, and received speaker honoraria for Aristo, Hexal, Janssen Pharmaceutica NV, Janssen-Cilag, and Sunovion, outside the submitted work. In the past 3 years, Dr. Stein has received research grants and/or consultancy honoraria from Johnson & Johnson, Lundbeck, Servier and Takeda MS received fees/has been a consultant for Lundbeck, Angelini. MBe has received Grant/Research Support from the NIH, Cooperative Research Centre, Simons Autism Foundation, Cancer Council of Victoria, Stanley Medical Research Foundation, Medical Benefits Fund, National Health and Medical Research Council, Medical Research Futures Fund, Beyond Blue, Rotary Health, A2 milk company, Meat and Livestock Board, Woolworths, Avant and the Harry Windsor Foundation, has been a speaker for Abbot, Astra Zeneca, Janssen and Janssen, Lundbeck and Merck and served as a consultant to Allergan, Astra Zeneca, Bioadvantex, Bionomics, Collaborative Medicinal Development, Janssen and Janssen, Lundbeck Merck, Pfizer and Servier – all unrelated to this work.
Acknowledgment
MBe is supported by an NHMRC Senior Principal Research Fellowship (1156072).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.08.091.
Appendix. Supplementary materials
References
- Ackerman R.A., Pinkham A.E., Moore R.C., Depp C.A., Harvey P.D. A longitudinal investigation of the effects of the COVID-19 pandemic on the mental health of individuals with pre-existing severe mental illnesses. Psychiatry Res. 2020;294 doi: 10.1016/j.psychres.2020.113493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackerman R.A., Pinkham A.E., Moore R.C., Depp C.A., Harvey P.D. COVID-19-related psychological distress and engagement in preventative behaviors among individuals with severe mental illnesses. npj Schizophr. 2021;7:7. doi: 10.1038/s41537-021-00136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee D., Kosagisharaf J.R., Sathyanarayana Rao T.S. The dual pandemic' of suicide and COVID-19: a biopsychosocial narrative of risks and prevention. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch I.M., Moretti F., Mazzi M., Wu A.W., Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychother. Psychosom. 2021;90:178–190. doi: 10.1159/000513733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Bertelloni C.A., Dell'Oste V., Barberi F.M., Maglio A., Buccianelli B., Cordone A., Dell'Osso L. Tele-psychiatry assessment of post-traumatic stress symptoms in 100 patients with bipolar disorder during the COVID-19 pandemic social-distancing measures in Italy. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.580736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carta M.G., Perra A., Boe L., Lorrai S., Cossu G., Aresti A., Ouali U., Ben Cheikh Ahmed A., Aissa A., Nacef F., Preti A. Living with bipolar disorder in the time of Covid-19: biorhythms during the severe lockdown in Cagliari, Italy, and the moderate lockdown in Tunis, Tunisia. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.634765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaimowitz G.A., Upfold C., Géa L.P., Qureshi A., Moulden H.M., Mamak M., Bradford J.M.W. Stigmatization of psychiatric and justice-involved populations during the COVID-19 pandemic. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;106 doi: 10.1016/j.pnpbp.2020.110150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conejero I., Nobile B., Olié E., Courtet P. How does COVID-19 affect the neurobiology of suicide? Curr. Psychiatry Rep. 2021;23:1–13. doi: 10.1007/s11920-021-01227-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dattoli L., Pepe M., Di Nicola M., Moccia L., Janiri L., Sani G., Janiri D., Fiorillo A. Serum 25-hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID-19 pandemic. Psychoneuroendocrinology. 2020;122 doi: 10.1016/j.psyneuen.2020.104869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong M., Lu L., Zhang L., Zhang Q., Ungvari G.S., Ng C.H., Yuan Z., Xiang Y., Wang G., Xiang Y.T. Prevalence of suicide attempts in bipolar disorder: a systematic review and meta-analysis of observational studies. Epidemiol. Psychiatr. Sci. 2019;29:e63. doi: 10.1017/S2045796019000593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Siddiqi N., Koyanagi A., Siskind D., Rosenbaum S., Galletly C., Allan S., Caneo C., Carney R., Carvalho A.F., Chatterton M.L., Correll C.U., Curtis J., Gaughran F., Heald A., Hoare E., Jackson S.E., Kisely S., Lovell K., Maj M., McGorry P.D., Mihalopoulos C., Myles H., O'Donoghue B., Pillinger T., Sarris J., Schuch F.B., Shiers D., Smith L., Solmi M., Suetani S., Taylor J., Teasdale S.B., Thornicroft G., Torous J., Usherwood T., Vancampfort D., Veronese N., Ward P.B., Yung A.R., Killackey E., Stubbs B. The lancet psychiatry commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6:675–712. doi: 10.1016/S2215-0366(19)30132-4. [DOI] [PubMed] [Google Scholar]
- Fornaro M., Gabrielli F., Albano C., Fornaro S., Rizzato S., Mattei C., Solano P., Vinciguerra V., Fornaro P. Obsessive-compulsive disorder and related disorders: a comprehensive survey. Ann. Gen. Psychiatry. 2009;8:1–13. doi: 10.1186/1744-859X-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garriga M., Agasi I., Fedida E., Pinzón-Espinosa J., Vazquez M., Pacchiarotti I., Vieta E. The role of mental health home hospitalization care during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020;141:479–480. doi: 10.1111/acps.13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gliddon E., Cosgrove V., Berk L., Lauder S., Mohebbi M., Grimm D., Dodd S., Coulson C., Raju K., Suppes T., Berk M. A randomized controlled trial of MoodSwings 2.0: an internet-based self-management program for bipolar disorder. Bipolar Disord. 2019;21:28–39. doi: 10.1111/bdi.12669. [DOI] [PubMed] [Google Scholar]
- Hernández-Gómez A., Andrade-González N., Lahera G., Vieta E. Recommendations for the care of patients with bipolar disorder during the COVID-19 pandemic. J. Affect. Disord. 2021;279:117–121. doi: 10.1016/j.jad.2020.09.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagesar R.R., Roozen M.C., van der Heijden I., Ikani N., Tyborowska A., Penninx B., Ruhe H.G., Sommer I.E.C., Kas M.J., Vorstman J.A.S. Digital phenotyping and the COVID-19 pandemic: capturing behavioral change in patients with psychiatric disorders. Eur. Neuropsychopharmacol. 2021;42:115–120. doi: 10.1016/j.euroneuro.2020.11.012. [DOI] [PubMed] [Google Scholar]
- Javelot H., Petrignet J., Addiego F., Briet J., Solis M., El-Hage W., Hingray C., Weiner L. Towards a pharmacochemical hypothesis of the prophylaxis of SARS-CoV-2 by psychoactive substances. Med. Hypotheses. 2020;144 doi: 10.1016/j.mehy.2020.110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karantonis J.A., Van Rheenen T.E., Rossell S.L., Berk M. The mental health and lifestyle impacts of COVID-19 on bipolar disorder. J. Affect. Disord. 2021;282:442–447. doi: 10.1016/j.jad.2020.12.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinoshita S., Cortright K., Crawford A., Mizuno Y., Yoshida K., Hilty D., Guinart D., Torous J., Correll C.U., Castle D.J., Rocha D., Yang Y., Xiang Y.T., Kølbæk P., Dines D., ElShami M., Jain P., Kallivayalil R., Solmi M., Favaro A., Veronese N., Seedat S., Shin S., Salazar de Pablo G., Chang C.H., Su K.P., Karas H., Kane J.M., Yellowlees P., Kishimoto T. Changes in telepsychiatry regulations during the COVID-19 pandemic: 17 countries and regions' approaches to an evolving healthcare landscape. Psychol. Med. 2020:1–8. doi: 10.1017/S0033291720004584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozloff N., Mulsant B.H., Stergiopoulos V., Voineskos A.N. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr. Bull. 2020;46:752–757. doi: 10.1093/schbul/sbaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazzari C., Nusair A., Shoka A., Hein S.M., Rabottini M. Case reports of first psychiatric presentations during CoViD-19 pandemic. Riv. Psichiatr. 2020;55:319–321. doi: 10.1708/3457.34465. [DOI] [PubMed] [Google Scholar]
- Llach C.D., Vieta E. Mind long COVID: psychiatric sequelae of SARS-CoV-2 infection. Eur. Neuropsychopharmacol. 2021;49:119–121. doi: 10.1016/j.euroneuro.2021.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohiniva A.L., Dub T., Hagberg L., Nohynek H. Learning about COVID-19-related stigma, quarantine and isolation experiences in Finland. PLoS One. 2021;16 doi: 10.1371/journal.pone.0247962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazereel V., Van Assche K., Detraux J., De Hert M. COVID-19 vaccination for people with severe mental illness: why, what, and how? Lancet Psychiatry. 2021;8:444–450. doi: 10.1016/S2215-0366(20)30564-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride M., Chari D., Alam F., Abbas M.J., Al-Uzri M., Brugha T., Kronenberg G., Mukaetova-Ladinska E. The early impact of the COVID-19 pandemic on acute care mental health services. Psychiatr. Serv. 2021;72:242–246. doi: 10.1176/appi.ps.202000467. [DOI] [PubMed] [Google Scholar]
- Miskowiak K.W., Johnsen S., Sattler S.M., Nielsen S., Kunalan K., Rungby J., Lapperre T., Porsberg C.M. Cognitive impairments four months after COVID-19 hospital discharge: pattern, severity and association with illness variables. Eur. Neuropsychopharmacol. 2021;46:39–48. doi: 10.1016/j.euroneuro.2021.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray G., Gottlieb J., Swartz H.A. Maintaining daily routines to stabilize mood: theory, data, and potential intervention for circadian consequences of COVID-19. Can. J. Psychiatry. 2020;66 doi: 10.1177/0706743720957825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murru A., Manchia M., Hajek T., Nielsen R.E., Rybakowski J.K., Sani G., Schulze T.G., Tondo L., Bauer M. Lithium's antiviral effects: a potential drug for CoViD-19 disease? Int. J. Bipolar Disord. 2020;8:21. doi: 10.1186/s40345-020-00191-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orhan M., Korten N., Paans N., de Walle B., Kupka R., van Oppen P., Kok A., Sonnenberg C., Schouws S., Dols A. Psychiatric symptoms during the COVID-19 outbreak in older adults with bipolar disorder. Int. J. Geriatr. Psychiatry. 2021;36(6):892–900. doi: 10.1002/gps.5489. Epub 2021 Jan 23. [DOI] [PubMed] [Google Scholar]
- Pacchiarotti I., Anmella G., Fico G., Verdolini N., Vieta E. A psychiatrist's perspective from a COVID-19 epicentre: a personal account. BJPsych Open. 2020;6:e108. doi: 10.1192/bjo.2020.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phiri P., Ramakrishnan R., Rathod S., Elliot K., Thayanandan T., Sandle N., Haque N., Chau S.W., Wong O.W., Chan S.S., Wong E.K., Raymont V., Au-Yeung S.K., Kingdon D., Delanerolle G. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine. 2021;34 doi: 10.1016/j.eclinm.2021.100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8:579–588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds C.M.E., Purdy J., Rodriguez L., McAvoy H. Factors associated with changes in consumption among smokers and alcohol drinkers duringthe COVID-19 'lockdown' period. Eur. J. Public Health. 2021 doi: 10.1093/eurpub/ckab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.J., Lim M.H. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res. Pract. 2020;30:3022008. doi: 10.17061/phrp3022008. [DOI] [PubMed] [Google Scholar]
- Smith K., Lambe S., Freeman D., Cipriani A. COVID-19 vaccines, hesitancy and mental health. Evid. Based Ment. Health. 2021;24:47–48. doi: 10.1136/ebmental-2021-300266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefana A., Youngstrom E.A., Chen J., Hinshaw S., Maxwell V., Michalak E., Vieta E. The COVID-19 pandemic is a crisis and opportunity for bipolar disorder. Bipolar Disord. 2020;22:641–643. doi: 10.1111/bdi.12949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J., Jän Myrick K., Rauseo-Ricupero N., Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment. Health. 2020;7:e18848. doi: 10.2196/18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toubasi A.A., AbuAnzeh R.B., Tawileh H.B.A., Aldebei R.H., Alryalat S.A.S. A meta-analysis: the mortality and severity of COVID-19 among patients with mental disorders. Psychiatry Res. 2021;299 doi: 10.1016/j.psychres.2021.113856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O'Brien K., Colquhoun H., Kastner M., Levac D., Ng C., Sharpe J.P., Wilson K., Kenny M., Warren R., Wilson C., Stelfox H.T., Straus S.E. A scoping review on the conduct and reporting of scoping reviews. BMC Med. Res. Methodol. 2016;16:15. doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., Hempel S., Akl E.A., Chang C., McGowan J., Stewart L., Hartling L., Aldcroft A., Wilson M.G., Garritty C., Lewin S., Godfrey C.M., Macdonald M.T., Langlois E.V., Soares-Weiser K., Moriarty J., Clifford T., Tunçalp Ö., Straus S.E. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Tundo A., Betro S., Necci R. What is the impact of COVID-19 pandemic on patients with pre-existing mood or anxiety disorder? An observational prospective study. Medicina. 2021;57:57. doi: 10.3390/medicina57040304. (Kaunas) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uvais N.A. Mania precipitated by COVID-19 pandemic-related stress. Prim. Care Companion CNS Disord. 2020;22:20l02641. doi: 10.4088/PCC.20l02641. [DOI] [PubMed] [Google Scholar]
- Vieta E., Pérez V., Arango C. Psychiatry in the aftermath of COVID-19. Rev. Psiquiatr. Salud Ment. 2020;13:105–110. doi: 10.1016/j.rpsm.2020.04.004. (Engl Ed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20:124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue S., Husain M.I., Ortiz A., Husain M.O., Daskalakis Z.J., Mulsant B.H. COVID-19: implications for bipolar disorder clinical care and research. SAGE Open Med. 2020;8 doi: 10.1177/2050312120981178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin X., Sun Y., Zhu C., Zhu B., Gou D., Tan Z. An acute manic episode during 2019-nCoV quarantine. J. Affect. Disord. 2020;276:623–625. doi: 10.1016/j.jad.2020.07.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yocum A.K., Zhai Y., McInnis M.G., Han P. Covid-19 pandemic and lockdown impacts: a description in a longitudinal study of bipolar disorder. J. Affect. Disord. 2021;282:1226–1233. doi: 10.1016/j.jad.2021.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A., Jehn A., Stackhouse M., Denice P., Ramos H. Changes in health behaviors during early COVID-19 and socio-demographic disparities: a cross-sectional analysis. Can. J. Public Health. 2020;111:953–962. doi: 10.17269/s41997-020-00434-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.