Abstract
Two-dimensional nanomaterials are emerging as promising candidates for a wide range of biomedical applications including tissue engineering, biosensing, pathogen incapacitation, wound healing, and gene and drug delivery. Graphene, due to its high surface area, photothermal property, high loading capacity, and efficient cellular uptake, is at the forefront of these materials and plays a key role in this multidisciplinary research field. Poor water dispersibility and low functionality of graphene, however, hamper its hybridization into new nanostructures for future nanomedicine. Functionalization of graphene, either by covalent or non-covalent methods, is the most useful strategy to improve its dispersion in water and functionality as well as processability into new materials and devices. In this review, recent advances in functionalization of graphene derivatives by different (macro)molecules for future biomedical applications are reported and explained. In particular, hydrophilic functionalization of graphene and graphene oxide (GO) to improve their water dispersibility and physicochemical properties is discussed. We have focused on the anticancer drug delivery of polyfunctional graphene sheets.
Keywords: two-dimensional nanomaterials, graphene, functionalization, anticancer drug delivery, photothermal therapy
Introduction
Cancer is a general name for a group of more than 100 diseases and one of the most serious health risks that is the second-leading cause of death worldwide behind cardiovascular disease.1–5 Cancer is usually caused by abnormal proliferation of different cells in the body that differ significantly in the complexity of treatment. Abnormal cell proliferation leads to tumor formation that can be benign or malignant. A benign tumor (non-cancerous) is not cancerous and remains confined to its original site and does not metastasize to other regions of the body. However, a malignant tumor (cancerous) is an invasive tumor and spreads through the bloodstream or lymphatic system throughout the body. Benign tumors can usually be removed by surgery, but malignant tumors are often resistant to current treatments and are much more dangerous because of their ability to invade and metastasize to different parts of the body.6,7 Many research studies have focused on finding new strategies to reduce the side effects of conventional therapies.8–10 Despite its drawbacks and limitations, chemotherapy plays a significant role in cancer treatment.11 One of the main challenges associated with chemotherapy is low bioavailability of chemotherapeutic agents and drug-resistant tumor cells.12–14 Nanomaterials, due to their unique physicochemical properties, including shape, surface, size, and optical properties, are able to target cancerous tissue and cross the biological barriers with minimal side effects.8,15,16 Different types of nanomaterials such as organic nanoparticles (polymeric micelles, liposomes, and dendrimers) inorganic nanoparticles (quantum dots, carbon nanotubes, magnetic and metal nanoparticles), 2D nanomaterials (graphene and its derivatives, molybdenum disulfide, boron nitride, black phosphorus nanosheets, transition-metal dichalcogenides, transition metal oxides, metal organic frameworks, layered double hydroxides), nanocomposites, and nanogels have been used for this purpose.17–28 To address these problems, anticancer drug delivery systems based on two-dimensional nanomaterials are developed and their ability to target anticancer drugs into tumors is investigated.29 Graphene-based nanomaterials due to their excellent physicochemical and biological properties including high loading capacity, photothermal property, and fast cellular uptake have been used to improve current chemotherapies.30–33 In this review, we have focused on the functionalized graphene sheets as nanocarriers to transport therapeutic agents into tumors along with a brief discussion on the challenges and future trends in this field.
Graphene Platforms: Structure, Chemistry, and Toxicity
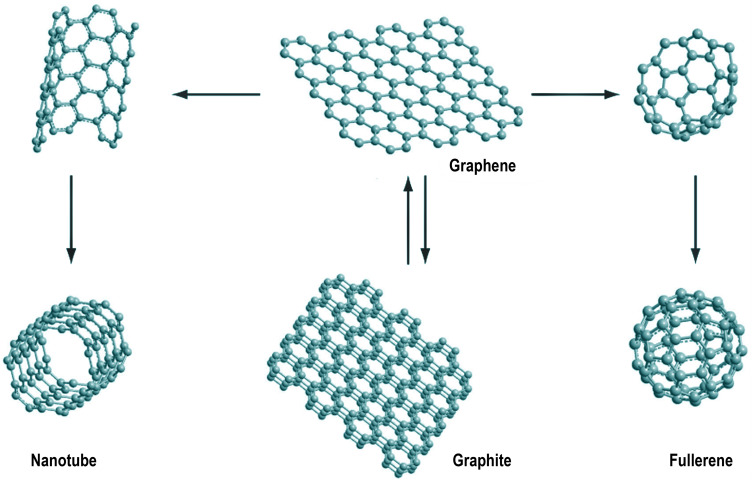
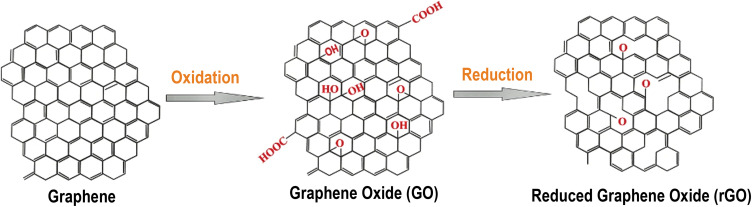
Graphene is a two-dimensional honeycomb network with sp2 carbon atoms. Each atom is bonded to neighboring carbons by σ-bond and out of plane p orbitals are extended over the whole structure. Graphene could be considered as the main backbone of various allotropes of carbon including fullerene, zero dimension (0D), nanotubes, one dimension (1D), and graphite, three dimensions (3D)34 (Figure 1). The unique physicochemical, optical, electrical, and mechanical properties of graphene make it a suitable platform for various applications such as energy storage,35,36 sensors,37–39 biological and medical applications,39–46 cancer therapy,47,48 functional devices,49–51 and drug delivery.52–54 High thermal and electrical conductivity, high elasticity and flexibility, and large surface area are some graphene properties superior to other nanomaterials.55,56 Due to its outstanding properties such as photothermal property, oxidative reactivity, and low price, graphene can be used as an appropriate platform for drug delivery. Also, layer structure of graphene represents a high loading capacity for therapeutic agents.57 Despite the extraordinary properties of graphene, one of the main drawbacks of using it for drug delivery is the low dispersibility of this compound in aqueous solutions. Oxidation to graphene oxide (GO), production of reduced graphene oxide (rGO) or functionalization by hydrophilic functional groups are the main strategies to overcome this problem (Figure 2). GO, an oxidized derivative of graphene, consists of a large number of oxygen containing functionalities such as epoxide, hydroxyl, and carboxylic acid. While epoxide and hydroxyl groups are placed in the basal plane, carboxylic groups are placed along the edges. These functional groups improve dispersibility of GO in water. rGO has much less epoxy due to reduction and it shows a low dispersibility in aqueous solutions.
Figure 1.
Graphite and different allotropic forms of carbon.
Notes: Used with permission of Future Medicine Ltd from Tonelli FM, Goulart VA, Gomes KN, et al. Graphene-based nanomaterials: biological and medical applications and toxicity. Nanomedicine. 2015;10:2423–2450; permission conveyed through Copyright Clearance Center, Inc. 40
Figure 2.
Structure of graphene and its oxidized derivatives.
Notes: Reproduced with permission from Priyadarsini S, Mohanty S, Mukherjee S, Basu S, Mishra M. Graphene and graphene oxide as nanomaterials for medicine and biology application. Journal of Nanostructure in Chemistry. 2018;8:123–137.41 Copyright © 2018, The Authors. Creative Commons CC BY (https://creativecommons.org/licenses/by/4.0/legalcode).
However, one of the main concerns regarding biomedical applications of graphene is the intrinsic toxicity and health risk of this compound.58–61 The toxicity of graphene-based nanomaterials mainly depends on different factors including size, surface charge, shape, number of layers, surface functional groups, and particulate state.58,62–64 While some studies showed no toxicity and side effects of graphene on mouse cells, others indicated considerable toxicity for graphene.65–67 This discrepancy come back to the variation in the structure of graphene derivatives and necessitates more extensive studies to conclude on the toxicity of graphene and its derivatives. Therefore, before any medical applications, a deep understanding of the toxicological profile of graphene-based nanomaterials is required. Cellular studies have shown that graphene and its derivatives can destroy the structures of the cells. For example, graphene caused plasma membrane damage in Hep G2 cells and induced disintegrate the mitochondrial membrane in a dose-time and shape-dependent manner.68,69 Moreover, graphene-based nanomaterials led to DNA fragmentation and chromosomal aberrations in human mesenchymal stem cells and cause side effects in normal cells such as immune system cells.70,71 Graphene causes apoptosis by inducing mitogen-activated protein kinases and the transforming growth factor-β-related signaling pathways.72 Graphene-based nanomaterials have shown dose-dependent hemolytic activity and aggregated graphene particles have shown considerable toxicity. Some studies have shown that graphene and its derivatives increase intracellular ROS and cause cytotoxicity and induce oxidative stress through which proteins, DNA, and lipid destruction have been damaged.73–77
Robert Langer and co-workers played with the functionality of graphene oxide and studied the toxicity effects of different types of graphene oxide on mice. The aim was to find a possible relationship between the amount of oxygen containing functional groups and biocompatibility of graphene oxide. Their results showed that by injecting graphene oxide, this substance becomes a mass in the body. The team found that the mice’s body excreted graphene oxide over time.
Researchers have used standard arrays to study the toxicity effects of graphene oxide and have shown that concentrations less than 1 mg/mL do not show considerable toxicity effects but higher concentrations are toxic to the body. Administration of GO in mice has resulted in chronic toxicity and death from pulmonary granuloma. In addition, dose-dependent pulmonary toxicity, granulomatous lesions, pulmonary edema fibrosis, and inflammatory cell infiltration have also been observed after administration of GO. A pulmonary inflammatory response was also observed in rats after administration of graphene with BSA.78–81
Functionalization of graphene with different functional groups can potentially improve the bioavailability, circulation lifetime and anticancer property of this material.82,83 As previously mentioned, one way to achieve this goal is functionalization of graphene surface by suitable polymers.84 Modification of graphene surface by polymers enhances biocompatibility and circulation times of graphene in vivo. PEG is the most studied polymer for the modification and improvement of biological properties of graphene derivatives. Conjugation of PEG onto graphene sheets reduces toxicity and increases stability of graphene under physiological conditions.85,86 According to the hematological analysis and histological examinations, nanographene modified PEG do not cause appreciable toxicity at dose (20 mg/kg) in a period of 3 months.87
Pharmacokinetics and clearance of graphene nanomaterials from the body has been studied but it needs extensive investigations to achieve a deep understanding of the long-term toxicity of these materials.88,89 The physicochemical properties of graphene derivatives including size, surface charge, surface chemistry, and shape impact their pharmacokinetics dramatically.90 Transmission electron microscope (TEM), Raman spectroscopy, isotopic labeling, and rare-earth elements labeling are some of the methods available for tracking these materials in body.87,91–93 For example, Liang et al used the La/Ce dual elemental labeling method to track the bioaccumulation, transfer, and clearance of polyvinylpyrrolidone (PVP) modified GO in vivo.94 They showed that injected PVP/GO mainly accumulate in the lungs, liver, and spleen, then pass through the glomerular filtration barrier (GFB) of the kidney and can be cleared, likely by both renal and fecal excretion. Similar results have been reported for injected PEGylated 125I-labeled nanographene sheets.87 Injected PEGylated graphene are accumulated in the reticuloendothelial system and gradually cleared from the bloodstream through their sequestration by cells of the mononuclear phagocyte system.
Graphene-Polymer Platforms; Synthesis and Physicochemical Properties
For many biological applications and in order to improve the functionality and dispersibility of graphene, surface of this nanomaterial should be modified and functionalized. Surface modification of graphene platforms using biocompatible polymers endow new properties and effectively improve their performances for biomedical applications. Taking advantage of the huge conjugated π-systems, high specific surface area, and useful functionality, graphene platforms can be used as novel nanocarriers for different therapeutic agents.95–98 Incorporation of polymeric systems into the graphene structure allows tailoring these platforms into new multifunctional systems to deliver a variety of moieties such as therapeutic, targeting, and diagnostic agents.97,99 Non-covalent and covalent functionalization are two major strategies for the modification of graphene and its derivatives.100–106
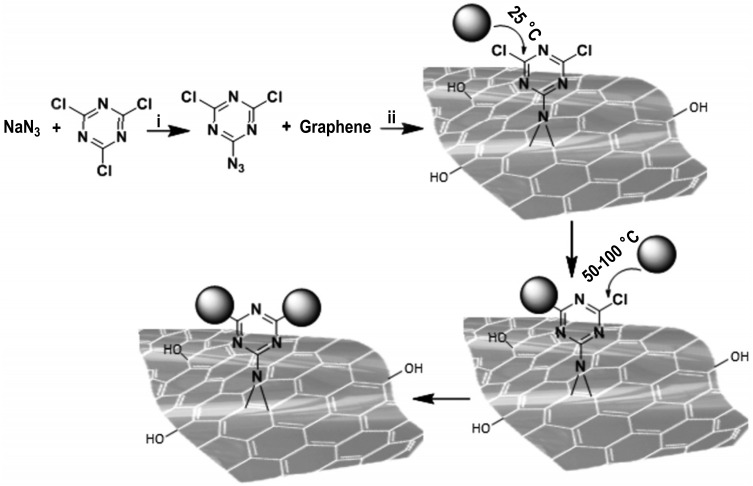
Graphene derivatives can be covalently modified by covalent attachment of polymers through addition of free radicals or dienophiles to their C=C bonds. Macromolecules can also be conjugated to GO through silanization, amidation, esterification, and cycloaddition reactions.107,108 However, challenges have to be addressed regarding non-destructive and covalent functionalization of graphene derivatives, as the methods previously mentioned cause disruption of sp2 network and electronic and optoelectronic features of these graphene-based platforms.109,110 We have previously developed a non-destructive covalent method for the controlled functionalization of nanographene sheets through nitrene [2+1] cycloaddition reaction based on azidodichloro-triazine at ambient conditions.111,112 This strategy allows the controlled non-destructive functionalization of graphene with different polymers and (macro)molecules through conjugated triazine groups and opens up new avenues to construct complex devices for future biomedical applications112 (Figure 3).
Figure 3.
The controlled functionalization of nanographene sheets through nitrene [2+1] cycloaddition reaction at ambient conditions.
Notes: The nucleophilic substitution of chlorine atoms in triazine groups with different polymers and (macro)molecules results in new platforms with defined structures. Reproduced with permission from Gholami MF, Lauster D, Ludwig K, et al. Functionalized graphene as extracellular matrix mimics: toward well‐defined 2D nanomaterials for multivalent virus interactions. Adv Funct Mater. 2017;27:1606477.112 Copyright 2017, Advanced Functional Materials.
Non-covalent functionalization by supramolecular interactions including, π-π stacking, hydrogen bonding, and van der Waals force is another strategy for the modification of graphene and its derivatives. While this approach preserved the π-conjugation and the electronic properties of graphene-based materials, it is unstable and functional groups can be detached upon changes in the environmental conditions.107,108
In the past several years, various types of graphene-polymer platforms have been developed and investigated as nanocarriers for therapeutic agents. Poly(ethylene glycol) (PEG),43,113–115 polyethylenimine (PEI),116,117 chitosan,118,119 and hyaluronic acid (HA)120,121 are common polymers that are employed for surface functionalization of graphene derivatives. Dendrimers and hyperbranched polymers, including polyamidoamine100,122 and polyglycerol9,33,100,123 are other types of polymeric systems that are commonly used in this field. Polymers significantly improve the physicochemical properties, solubility, stability, biocompatibility, and drug loading capacity of graphene.
Graphene-Polymer Platforms in Drug Delivery
Cancer is a major cause of death worldwide and prevention or therapy of this disease is one of the biggest health challenges nowadays. Chemotherapy has been used extensively to treat many types of cancer; however, it is limited by different factors including multidrug resistance, systemic toxicity, immunogenicity, and bioavailability. These limitations could be overcome by drug delivery systems.124–126
Among drug delivery systems and breakthroughs, graphene and its derivatives have been abundantly used for a wide range of biomedical applications owing to their sheet-like structure, high specific surface area, and ease of functionalization.99,127,128 Due to the availability of different functionalization strategies and taking advantage of the multifunctionality of graphene and its derivatives, various drug delivery systems with controllable biological properties can be prepared. Functionalization of graphene derivatives with various polymers could potentially improve their reactivity, biocompatibility, circulation times in vivo and anticancer capacity. Graphene-polymer platforms with high drug loading capacity have opened up new opportunities in the development of novel drug delivery systems for various biomedical applications, where conventional graphene and polymer alone cannot meet all requirements.32,129–131
Functionalization of graphene and its derivatives with PEG have been extensively used for the construction of anticancer drug delivery systems.113 Liu et al initially reported PEG-decorated GO as a nanocarrier to effectively deliver anticancer drugs. They exploited non-covalent interactions to load anticancer hydrophobic drugs and found that the combination of PEG with graphene-based materials can effectively improve biocompatibility, cellular uptake, bioavailability, physiological stability, therapeutic efficacy, and circulation time of drugs in bloodstream.132 On the other hand, PEGylation of graphene reduces aggregates of graphene in RES organs (lungs, liver, spleen, and kidney) as well as its retention and toxicity. Similarly, in another report, 6-armedPEG-functionalized graphene oxide-based nanocarrier has been reported to deliver anticancer drugs such as oridonin and methotrexate (MTX).133 Synthesis of PEG-grafted GO and loading of drugs has been performed via amidation and π-π stacking, respectively. This complex (oridonin or MTX@GO-PEG) exhibited higher cellular uptake and anticancer activity against CAL27 tumor cell in comparison with free drugs. PEGylated graphene has also been developed as dual-drug (DOX and platinum) delivery system with a higher efficiency than the single-drug system.113 The results of these studies showed that the combination of drugs efficiently overcomes the cancer drug resistance and improves their anti-cancer effect. This drug delivery system demonstrated less toxicity and damage to normal cells compared to DOX and platinum-free drugs. Interactions of PEGylated graphene with drugs have been adjustable by polymer chain length.134,135 In another study, PEGylation of GO using PEG copolymer conjugated to multiple pyrenes increased percentage of PEG on GO surface and simultaneously reduce GO to rGO. In-vitro assays of this study revealed that graphene with PEG content higher than 75% and longer PEG chain showed better physicochemical properties than their analogs with shorter PEG chains.134 The combination of PEG with other polymers such as hyaluronic acid, polyethyleneimine, and chitosan have also been intensively investigated in order to improve therapeutic effects of graphene-drug platforms.34–38,136
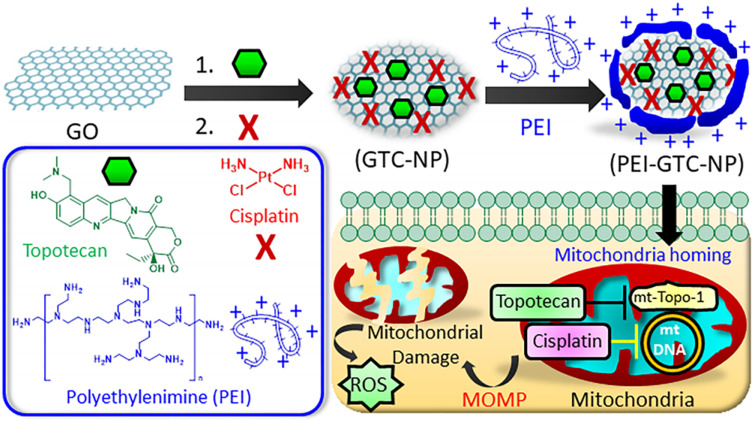
PEI a cationic polymer is another type of widely explored polymers for the surface modification of graphene-based materials.116,137,138 It was found that bare PEI with high molecular weight induced high cytotoxicity due to high cellular uptake and low biodegradability, while its hybridization with carbon materials resulted in a low cytotoxicity. Commonly, PEI is able to form a complex with graphene derivatives via electrostatic interactions and amination methods. PEI-graphene are cationic platforms with multiple advantages including high hydrophilicity, biocompatibility, strong binding to nucleic acids, effective cell uptake, and thermal stability. We report that co-delivery of therapeutic genes and chemotherapy downregulates tumor cell resistance to anticancer drugs and overcome multidrug resistance (MDR).139,140 PEI-conjugated graphene has been developed for co-delivery of DOX drug and p53 tumor suppressor gene in order to inhibit HeLa cell growth. Owing to presence of PEI cationic polymer and synergistic effect of drug and gene, DOX/GO-PEI/p53 complex has been efficiently internalized into HeLa cells via endocytosis and has exhibited higher growth inhibition than the single drug/gene delivery system.141 In 2019, Mallick et al developed an interesting polymer-graphene platform based on self-assembled PEI covered graphene oxide nanoparticle (PEI-GTC-NP) for codelivery of cisplatin and topotecan into mitochondria. This platform is able to target drugs into mitochondria of cancer cells effectively. Reactive oxygen species (ROS) were generated at specific sites in mitochondria, which in turn led to apoptosis of cancer cells (Figure 4).116 Topotecan have been loaded on GO by π-π stacking to visualize nanomaterial in cancer cell’s mitochondria by fluorescence emission. Cisplatin was also applied as chemotherapy medication to treat cervical cancer. Localization of PEI-GTC-NPs into cancer cell resulted in mitochondrial membrane perforation. MTT assay indicated that the half maximal inhibitory concentration (IC50) for nanoparticles in the absence of PEI (GTC-NPs) is higher than PEI-GTC-NPs. This nanoparticle with positive surface charge and suitable size has been able to penetrate into mitochondria of cancer cells specifically and has shown good potential for treatment of cancer.
Figure 4.
GO with PEI coverage coloaded with cisplatin and topotecan for mitochondria targeting of cancer cells.
Notes: Reproduced with permission from Mallick A, Nandi A, Basu S. Polyethylenimine coated graphene oxide nanoparticles for targeting mitochondria in cancer cells. ACS Applied Bio Mater. 2018;2:14–19.116 Copyright 2019, American Chemical Society.
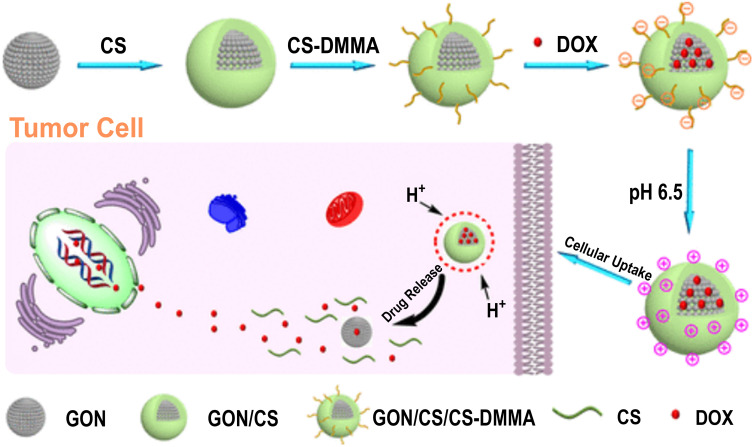
Natural biopolymers owing to their low toxicity, biodegradability, renewability, environmental sensitivity, and biocompatibility are also promising materials to improve the biological properties of graphene-based materials.142–145 Chitosan with anticancer activity and as a pH sensitive polymer has been widely employed in the synthesis of polymer-graphene hybrids.146–148 The produced multifunctional scaffolds have exhibited high loading capacities and functional binding sites for different types of drugs and targeting ligands.147–149 Moreover, graphene-chitosan platforms have been widely studied as a pH-sensitive nanovehicle for the targeted release of drugs into cancer cells. Graphene oxide-chitosan hybrids have been developed by Dhanavel and co-workers for the controlled delivery of 5-Fluorouracil (5-FU) and curcumin (CUR). These systems have been synthesized by conjugation of chitosan to GO nanosheet through tripolyphosphate as a crosslinker. Chitosan/reduced graphene oxide (CS/rGO) has displayed pH-dependent drug release behavior. In 2018, Zhao et al reported a chitosan-graphene drug delivery system. It was a core-shell structure containing graphene oxide nanoparticles (GONs) as core and chitosan as surface charge-reversible shells, which was deposited on graphene core via self-assembly (Figure 5).150 Doxorubicin (DOX) via the non-covalent interactions (π-π stacking) bound to the large π conjugated system of GO and chitosan shells prevents premature secretion of loaded DOX in the medium. Due to the lower pH in cancerous tissue, the coated chitosan was separated, thus accelerating the release of DOX. The charge of these nanomaterials changes from negative at pH= 7.4 in the bloodstream to positive at pH 6.5 in the tumor tissue. Chitosan-graphene platform showed advantages over the usual drug delivery systems including high drug loading capacity (DL), great encapsulation efficiency (EE), long-time circulation in bloodstream, improved cellular uptake, and adjustable controlled release of anticancer therapeutics.
Figure 5.
Schematic representation of the synthesis and cellular uptake of GO nanoparticle/chitosan hybrids as drug delivery system.
Notes: This system was sensitive to changes in pH through which intracellular DOX delivery was controlled. Reproduced with permission from Zhao X, Wei Z, Zhao Z, et al. Design and development of graphene oxide nanoparticle/chitosan hybrids showing pH-sensitive surface charge-reversible ability for efficient intracellular doxorubicin delivery. ACS Appl Mater Interfaces. 2018;10:6608–6617.150 Copyright 2018, American Chemical Society.
While CS has been widely explored in biomedical and environmental fields, there have been some limitations including insolubility at neutral pH and low rate of degradation.148 These problems have been overcome by combining CS with other biopolymers such as cellulose, dextrin, sodium alginate, and so on.151–154 Multilayers of biopolymers can be disposed of on graphene through various techniques.155,156 In a study, layer-by-layer (LbL) self-assembly technique has been explored for deposition of CS and dextrin on graphene surface.157 In this process GO has been first modified with CS, followed by conjugation of dextrin (Dex) via electrostatic interaction with oppositely charged polyelectronic. The GO-CS/Dex conjugate has shown high drug loading capacity, physiological stability, and cellular uptake, compared with GO-CS. In another study, CS has been modified by poly(itaconic acid-copolymerized acrylic acid) in order to increase hydrophilic nature of chitosan.53 This new combination has been used for the modification of GO-amine (AGO) with anticancer drug delivery application. CS-GO hybrid has been prepared via electrostatic interactions between chemically modified chitosan as an anionic polyelectrolyte and AGO which acts as a cationic polyelectrolyte.118 Omidi et al,119 Samadi et al,158 and Lei et al159 have also verified improvement of physicochemical and biological properties of graphene-chitosan composites through integration with other polymers.
HA is recognized as another important polysaccharide for the improvement of the biological properties of graphene-based materials.121,160,161 Biomedical applications of HA and its usage for the production of anticancer drug delivery systems have been widely developed, due to its excellent biocompatibility, biodegradability, as well as strong binding affinity and selective targeting of tumor markers, especially the cluster determinant 44 (CD44) and hyaluronan receptor (HARE).162–164 Yin’s group has prepared redox-sensitive hyaluronic acid-graphene oxide (HSG) composite and studied its ability to target HA-receptor overexpressing tumors and efficiency of redox-sensitive linkages to localize drugs at the target sites. This system was synthesized by conjugation of hyaluronic acid to GO nanosheet using disulfide linkages (HSG). HSG-DOX displayed accelerated release of DOX in acidic environments. Because high activity of hyaluronidase (HAase) in acidic conditions resulted in degradation of hyaluronic acid chains into small pieces and promoted release of DOX. Owing to high drug-loading capacity, photothermally controlled effects, specific targeting of HA receptors overexpressing tumors, and redox-dependent response, HSG-DOX showed amplified chemotherapeutic outcomes.161
Dendrimers and hyperbranched polymers, especially polyglycerol, are able to effectively improve biological properties and biofunctionality of graphene sheets, as demonstrated in our previous studies.51,100,103,112,131,165–167 Our group implemented a new method for functionalization of graphene-based nanomaterials with hyperbranched polyglycerol.14 Thermally reduced GO was functionalized by triazine and consequently conjugated with hyperbranched polyglycerol through triazine functional groups. The polyglycerol-covered nanographene with mitochondria-targeted ligands and pH-triggered surface charges showed a high loading capacity and triggered release of DOX drug in the acidic environment (Figure 6). Owing to photothermal properties of nanographene, this multifunctional drug delivery system exhibited accelerated drug release and enhanced chemotherapeutic effect after NIR irradiation. The authors concluded that the high accumulation of smart multifunctional drug delivery system in mitochondria and nucleus, together with photothermal properties, were the reasons for the enhanced chemotherapeutic effects.14
Figure 6.
(A) The chemical structure of the polyglycerol-covered nanographene with the mitochondria-targeting ligands and charge conversional functional groups. (B) Multifunctional drug delivery system accumulates in mitochondria by targeting ligands and photothermal properties under NIR laser irradiation result in drug release and good therapeutic efficiency.
Notes: Reproduced with permission from Tu Z, Qiao H, Yan Y, et al. Directed Graphene‐based Nanoplatforms for hyperthermia: Overcoming multiple drug resistance. Angewandte Chemie. 2018;130:11368–11372.14 Copyright © 2018 Wiley‐VCH Verlag GmbH & Co. KGaA, Weinheim.
Targeted Drug Delivery
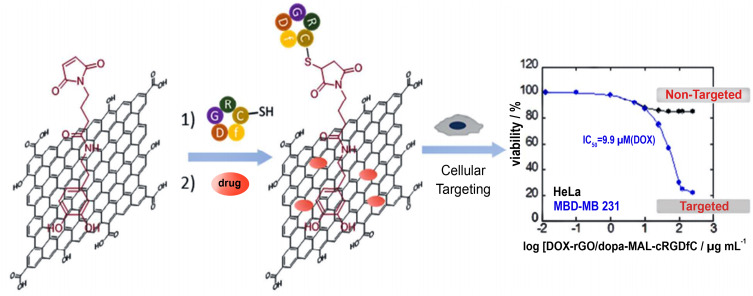
One of the cancer treatment methods that has received a great deal of attention is targeted delivery in which anti-cancer drugs are transported to the target tissues specifically. The method is designed by attaching targeting agents to nanocarriers. Targeting drug delivery systems increases the localization of drugs at tumor sites and diminishes the side effects of chemotherapies. Accordingly, a drug delivery system with targeting ligands and good emission property in visible and infrared has been prepared by loading anticancer drugs onto NGO.168 Zhang et al have developed GO as a drug delivery system by loading DOX and Camptothecin (CPT) on its surface and conjugation of folic acid to transport cargos to the tumor sites. FA-conjugated NGO (FA–NGO) was able to target MCF-7 cells, and human breast cancer cells by interaction with FA receptors.68 Some superparamagnetic nanocarrier based on attaching Fe3O4 as a magnetic nanocarrier on GO and aptamer (APT) as a targeting moiety for MCF-7 cancer cell is prepared and then, paclitaxel (PAC) is loaded as an anti-cancer drug. This system has shown advantages including biocompatibility, pH-responsivity, thermal stability, and high drug loading capacity over similar nanocarriers.169 A rGO-based system with the ability to deliver DOX to human breast adenocarcinoma cancer cells (MDA-MB-231) is also reported. In this system, a thiol maleimide containing catechol (dopa-MAL) is assembled on the surface of rGO by π-π stacking. Then, a cancer cell targeting cyclic peptide is attached to dopa-MAL. This nanostructure has shown a high efficiency against MDA-MB-231 cells with an IC50=58 µg mL−1 for DOX-loaded rGO/dopa-MAL-c (RGDfC), corresponding to an IC50=9.9 µg mL-1 for DOX in the matrix (Figure 7).170
Figure 7.
Functionalized rGO with thiol-maleimide containing catechol (dopa-MAL) as a targeted drug delivery system for DOX to destroy human breast adenocarcinoma cancer cells (MDA-MB-231).
Notes: Reproduced with permission from Oz Y, Barras A, Sanyal R, Boukherroub R, Szunerits S, Sanyal A. Functionalization of reduced graphene oxide via thiol–maleimide “click” chemistry: facile fabrication of targeted drug delivery vehicles. ACS Appl Mater Interfaces. 2017;9:34194–34203.170 Copyright © 2017, American Chemical Society.
Hyaluronic acid (HA) is also used to target GO into cancer cells. GO with HA functionality (GO-HA) has been coloaded with DOX and paclitaxel (Ptx) and the obtained drug delivery system (GO-HA-DOX/Ptx) has been used for the efficient incapacitation of cancer cells.170
Another target drug delivery system is designed based on dopamine (DA) functionalized nGO nanocarrier (DA-nGO). DA improves the delivery of methotrexate (MTX) as an anticancer cargo into target cells.171 Song et al have produced a targeted drug delivery system by loading Fe3O4 nanoparticle on the surface of GO and conjugation of lactoferrin (Lf) as a targeting ligand to this platform. The results have shown that this system (Lf@GO@Fe3O4@DOX) has the ability to deliver drugs into C6 glioma cells effectively.172
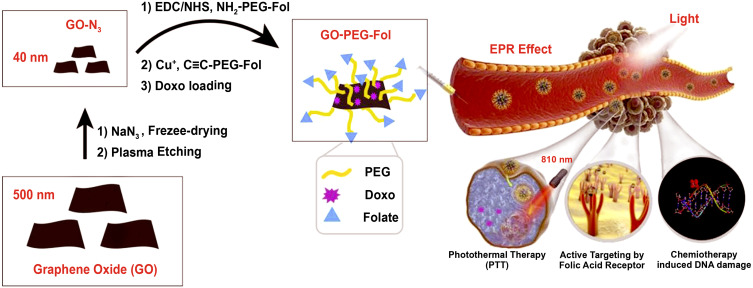
Conjugation of polymers and targeting ligands onto the surface of graphene derivatives improves the therapeutic efficiency of these platforms by increasing their loading capacity and decreasing their side effect as well as efficient localization of drug delivery systems in the targeted cells (Figure 8).173
Figure 8.
Synthesis of folic acid-functionalized PEGylated GO (GO-PEG-Fol), with small size and narrow size distribution (∼30 ± 5 nm), and the ability of efficient converting NIR light into heat.
Notes: GO-PEG-Fol is able to actively target MCF7 and MDA-MB-231 cells. Reprinted from Materials Science and Engineering: C, Vol 107, Mauro N, Scialabba C, Agnello S, Cavallaro G, Giammona G, Folic acid-functionalized graphene oxide nanosheets via plasma etching as a platform to combine NIR anticancer phototherapy and targeted drug delivery, Pages No.,110201 Copyright (2020), with permission from Elsevier.173
Smart Platforms
To overcome the limitations of conventional drug delivery systems such as poor tumor penetration, collateral damage to healthy tissues and uncontrollable drug release, stimuli-responsive drug delivery systems, in which therapeutic agents can be activated by endogenous or exogenous stimuli, have been developed.174,175 Graphene-based platforms can be excellent candidates in this regard, since they are sensitive to changes in tumor microenvironment/intracellular signals and response to physical stimuli factors.175–179
Due to the conversion of glucose to lactose, cancerous tissues are more acidic (pH 6.5–7.2) than both blood and healthy tissues (pH 7.4). Therefore, conjugation of pH-responsive ligands to the platforms results in controlled drug release at tumor sites.180–182 Accordingly, graphene-polymer platforms with pH sensitive functional groups (COOH, -NH2, and -SO3H) have been widely explored to control the release of various therapeutic agents at tumor sites. An example of such systems has been recently reported by our group.14 Graphene-based drug delivery systems with charge conversional property was synthesized through functionalizing polyglycerol-covered nanographene sheets with 2,3-dimethylmaleic anhydride (GPTD) (Figure 6). The surface charge of this system changed from negative at pH 7.4 to positive at pH 6.8. Therefore, it was negatively and positively charged in the blood stream and tumor tissue, respectively. These unique features resulted in a longer-term circulation and increased permeability and retention (EPR) effect of drug delivery systems in body and better localization and controlled release of payloads at tumor sites. This multifunctional drug delivery system showed significant synergistic hyperthermia and chemotherapy effects and showed a high potential in multidrug resistance chemotherapy.14
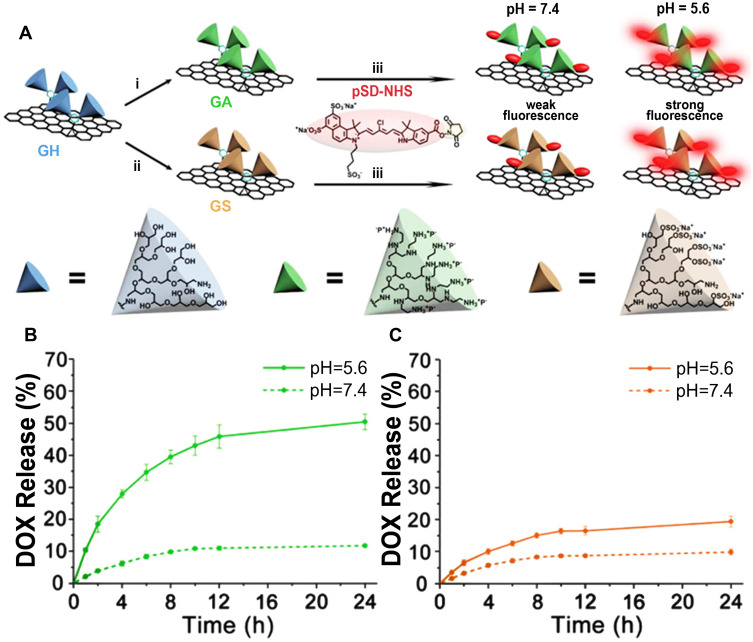
Charge conversional graphene platforms are promising nanocarriers for site-specific delivery of drug because of their charge conversion at reduced pH.183–185 Our group reported a charge conversional graphene platform to promote cellular uptake of loaded drugs166 (Figure 9). In this work, polyglycerol containing sulfate and amino groups were conjugated to GO surface, yielding charge-conversional systems. The protonation of hPG amine in the acidic environment accelerated the release of DOX due to repulsion between protonated DOX and hPG amine. On the other hand, due to weakening π–π stacking and hydrophobic interactions between the graphene-polymer platforms and doxorubicin, as well as increasing solubility of drug in acidic conditions, effective release of drug occurred in this condition.166
Figure 9.
(A) Schematic representation of the synthesis of the polyglycerol amine functionalized graphene sheets (GA), polyglycerol sulfate-functionalized graphene sheets (GS) and conjugation of pH-sensitive dye to the GA and GS (GAD, GSD). Information regarding the synthesis these graphene platforms can be found in ref.166 In vitro release profile of DOX from the GAD (B) and GSD (C) at 37 °C in various media.
Notes: Reproduced with permission of Royal Society of Chemistry from Tu Z, Wycisk V, Cheng C, Chen W, Adeli M, Haag R. Functionalized graphene sheets for intracellular controlled releaseof therapeutic agents. Nanoscale. 2017;9:18931–18939.131 Copyright 2017, Advanced Functional Materials; permission conveyed through Copyright Clearance Center,Inc.
It is known that antioxidant concentration (such as GSH) in intracellular microenvironment of tumor tissues (1−10 mM) is often higher than that in normal tissues (20−40 μM).186,187 This feature is important in the development of graphene-based smart systems. Internalized graphene-based platforms with disulfide bonds and redox properties are able to deliver drugs and release them at tumor sites efficiently. DOX has been linked to PEG/PCL copolymer via disulfide bonds and then decorated on graphene surface through hydrophobic interactions. The release of drugs from this system was controlled by redox factors such as GSH.188
Apart from their ability to provide intracellular responsiveness, graphene platforms also have the capability to respond to some exogenous stimuli189 including light and magnetic fields, which will be discussed later.
Graphene-Polymer Platforms in Bioimaging
Bioimaging techniques have a broad range of biomedical applications, from diagnosing diseases to investigating body tissues at the cellular level.190 Previously, these techniques were mostly used in orthopedic diagnosis. Upon development of imaging tools and methods, other techniques such as magnetic resonance imaging (MRI), X-ray computed tomography (X-ray CT), ultrasound, radio wave technology etc. were also used in various medical fields.191,192 Bioimaging by both optical microscopy such as laser scanning confocal microscopy (LSCM) and electron microscopy such as liquid cell electron microscopy (LC-EM) helps to evaluate living tissues with high magnifications.193,194 Graphene and its derivatives, due to their interesting optical properties, have shown a high potential in this research field.195,196 They can be used for bioimaging in two ways: i) by inherent optical properties such as fluorescence quenching and Raman signals, ii) by loading fluorophores and fluorescent drugs onto their surface.197,198
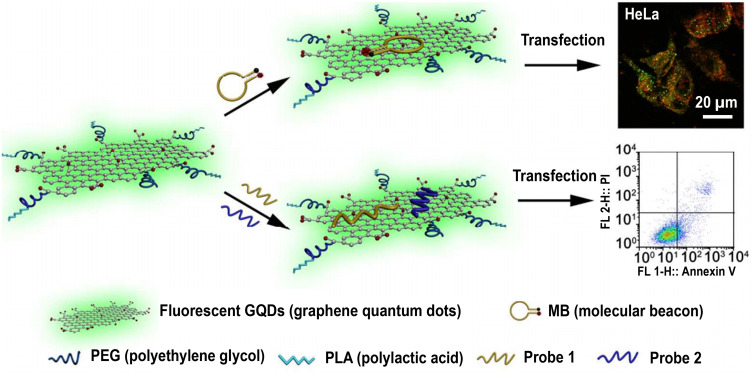
Graphene due to its zero-bandgap energy is not photoluminescent but graphene derivatives such as GO possess a significant band-gap and show the photoluminescence property.199 They emit a broad range of fluorescence from ultra violet (UV) to NIR.200 One of the promising properties of graphene derivatives is their ability to quench most types of fluorescence materials.201 These two features make graphene and its derivatives unique platforms for bioimaging. It is shown that charge transfer from the fluorophore to GO is the main reason for the fluorescence quenching and FERT (resonance energy transfer).202,203 Functionalization by a variety of materials, such as polymers, proteins, nucleic acids, peptides, and nanoparticles improves the physicochemical properties of graphene-based bioimaging probes.204–206 These compounds improve biocompatibility, loading capacity, water solubility, specificity, or sensitivity of graphene-based platforms and improve their performance as bioimaging tools.207 Dong et al have developed a multifunctional graphene quantum dots-polymer for cell imaging.208 They have used poly(L-lactide) (PLA) and PEG-grafted GQDs for microRNAs imaging analysis (Figure 10). Functionalization of GQDs with these polymers has created a nanocomposite with stable photoluminescence over a wide range of pH, which is extremely important for cell imaging. The results of cell experiments have shown low cytotoxicity and high biocompatibility for this nanocomposite, qualifying it for future bioimaging investigations.
Figure 10.
Schematic presentation of the functionalization of QDs by poly(l-lactide)-PEG and their application for cell imaging.
Notes: A strong signal for the functionalized QDs can be seen in HeLa cells. Low toxicity has also been observed for this material. Gene probes were loaded onto the surface of functionalized QDs with π-π interaction. The uptake of probes by HeLa cells can be controlled by the intrinsic photoluminescence of QDs, while the fluorescence of the gene probe applied to identify the target is used to monitor gene regulation. Probe 1 is an inhibitor probe of miRNA-21 and probe 2 is survivin antisense oligodeoxynucleotide. Reproduced with permission from Dong H, Dai W, Ju H, et al. Multifunctional poly (l-lactide)–polyethylene glycol-grafted graphene quantum dots for intracellular microRNA imaging and combined specific-gene-targeting agents delivery for improved therapeutics. ACS Appl Mater Interfaces. 2015;7:11015–11023.208 Copyright © 2015, American Chemical Society.
Graphene-Polymer Platforms in Photothermal and Photodynamic Therapy
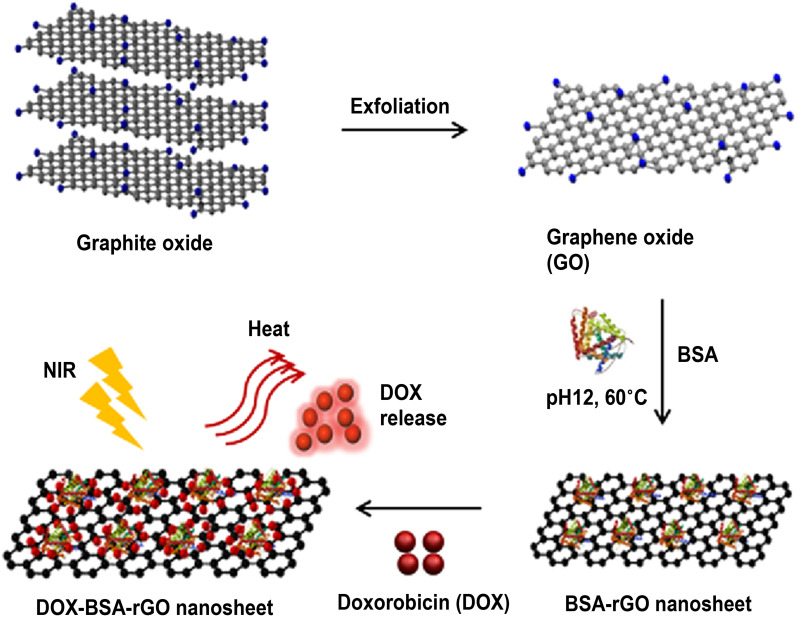
Graphene and its derivatives are able to absorb NIR laser irradiation and generate heat efficiently. Therefore, they have been widely used as photosensitizing agents for photothermal therapy. This technique in combination with chemotherapy shows synergic therapeutic effect.209–214 Cheon et al have developed a combinational photochemotherapy to enhance therapeutic efficacy of DOX.215 The bovine serum albumin (BSA)-functionalized rGO (BSA-rGO) nanosheets have exhibited a high loading efficiency for DOX and absorbance of NIR light (5.5 W/cm2, 808 nm for 300 s). Due to the increased medium temperature at the tumor site under NIR irradiation, drug has been released from BSA-rGO–DOX and low viability of brain tumor cells with reduced chemotherapy side effects has been observed (Figure 11).
Figure 11.
Schematic representation of the synthesis of DOX-BSA-rGO as a light sensitive drug delivery system for chemo-photothermal therapy.
Notes: Albumin is attached onto the surface of exfoliated GO and DOX is loaded onto the surface of BSA-rGO nanosheets. This system has enhanced therapeutic efficacy of DOX drug due to the synergic effect of chemotherapy and photothermal therapy. Reproduced with permission from Cheon YA, Bae JH, Chung BG. Reduced graphene oxide nanosheet for chemo-photothermal therapy. Langmuir. 2016;32:2731–2736.215 Copyright © 2016, American Chemical Society.
Moreover, photochemotherapy of DOX loaded PEGylated GO nanosheets and DOX loaded PEGylated mesoporous carbon nanospheres (MCN) against 4T1 cells is investigated. MCN-PEG/DOX and GO-PEG/DOX have shown less toxicity against 4T1 cells than free DOX. However, when these systems are irradiated by NIR laser (1.0 W/cm2) for 3 min, an increase in toxicity has been observed. Additionally, due to higher photothermal conversion efficiency (η) and drug release rate, MCN-PEG/DOX has shown higher anticancer effect than DOX/GO-PEG.216
A photothermal agent based on folic acid-CS functionalized graphene oxide (FA-CS-GO) with high photostability and tumor-targeting ability has been reported by Jun et al.217 The hybridization of GO and CS-FA hinders the aggregation of GO, promotes cellular uptake and light absorption in this platform, and enhances the PTT effects of FA-CS-GO. The surface temperature of tumors treated with FA-CS-GO increased to 57.6 °C under laser irradiation (2.0 W/cm2) within 5 min. The viability of tumors treated with FA-CS-GO + laser decreased dramatically, in comparison with laser irradiation in the absence of this platform.
The combination of graphene mediated PTT with immunotherapy has resulted in very promising results for the treatment of metastatic tumors. Fe3O4 nanoparticles (FNPs)/rGO/PEG (FNPs/rGO-PEG) nanocomposite are developed as multimodal agents for MRI-guided photothermal-immunotherapy. The combination of FNPs/rGO-PEG nanocomposite with NIR light through reduction of tumor macrophages and photothermal therapy has promoted antitumor immune response.218 The surface tumor temperature in FNPs/rGO-PEG-injected mice has reached to 59°C after NIR laser irradiation (805 nm, 1 W cm2).218
Photodynamic therapy (PDT) is an efficient method for tumor suppression. In this strategy, reactive oxygen species (ROS) are generated by photosensitizer (PS) upon visible light or laser absorption and destroy tumor cells at target sites.219,220 To control ROS generation and enhance cellular uptake of photosensitizers, reactive agents including porphyrins, chlorins, and dyes are conjugated to graphene platforms.219,221,222 Moreover, multimodal therapies combined with PDT such as chemo-photodynamic therapy (PDT), immunotherapies-photodynamic therapy (PDT), and photothermal therapy (PTT)–photodynamic therapy (PDT) have been used for strong antitumor activity. Nanographene oxides (NGOs) with TPE (AIE) photosensitizers were synthesized as powerful tool for multimodal imaging-guided PDT.223 NGP-TPEred nanoparticles under 450 nm laser irradiation have shown a significant tumor inhibition both in vitro and in vivo. In another study, the chemo-PDT mediated by photosensitizer indocyanine green (ICG) and folic acid conjugated GO-PEG co-loaded with MTH1 inhibitor (TH287) and DOX has been developed for the targeted therapy of osteosarcoma tumor. MTH1 protein with controlled ROS production has been shown to be a highly synergistic chemo-photodynamic therapy.224
Furthermore, graphene quantum dots (GQDs) and graphene oxide quantum dots (GOQDs) with the size range of 1.5–5.5 nm have reduced skin cancer (B16F10) cells and breast cancer (MCF-7) cell viability about 90% when combined with UV irradiation (365 nm) for 5 min.225
Graphene-Polymer Hybrids for Gene and Biomolecules Delivery
Some human diseases stem from defective genes. In gene therapy, effective treatments of genetic diseases, nucleic acids, and genetic materials are encapsulated by nanocarriers and delivered to the desired sites in the cell.226 Gene delivery is a process through which foreign DNA is transferred into target cells to express an exogenous gene.227 Due to low bioavailability and enzymatic degradation of DNA, it should be delivered to the cells by a suitable carrier. Gene delivery systems are categorized into: viral, non-viral, and oncolytic viral vectors.228 Viral gene delivery systems are composed of modified viruses which are not able to replicate. The most studied viral vectors for DNA delivery are including adenoviruses (AV), adeno-associated viruses (AAV), retroviruses (RV), lentiviruses (LV), and herpes simplex viruses (HSV). Their analogs for RNA delivery are human foamy virus (HFV), oncoretro-viral vectors, and lenti-viral vectors.229 Another type of gene delivery system is oncolytic viral vectors that represent an ideal platform for gene delivery. These viruses can occur either naturally or can be engineered as natural viruses in the laboratory.230 The first oncolytic virus was approved by the US Food and Drug Administration in 2015.231 In contrast, non-viral vectors are an alternative to virus-based systems, although they have poor transfection efficiency compared to viral vectors. Non-viral vectors, such as polymers, show significantly lower cytotoxicity. They are able to carry large DNA molecules and can be produced cost-effectively in large quantity.232,233 These vectors are generally prepared by both chemical and physical methods. Physical methods are usually performed via physical force to increase permeability of the cell membrane. The most important physical methods are microinjection, electroporation, ultrasound, and gene gun.234,235 Chemical methods utilize cationic polymers, cationic lipids, liposomes, and cell-penetrating peptides to deliver genes into cells.236–238 Many gene delivery systems have been designed based on cationic polymers, such as PEI.239–241 Due to pH buffering capacity, this polymer is one of the most important non-viral polymeric vectors for gene delivery. This sustainable buffering capacity below physiological pH helps condense DNA to escape the endosomal barrier while avoiding lysosomal degradation.242 PEI due to lack of degradability has high toxicity for biomedical applications. To solve this problem, a number of PEI polymers with biodegradable segments in their backbone have been synthesized. Graphene is also used to design non-viral gene transfer systems. These systems have been proposed as efficient 2D non-viral gene transfer vectors, because their outstanding properties243 such as facile and versatile chemical functionalization, protection of nucleic acid from enzymatic degradation, and fast cellular uptake result in efficient gene transfection into the target cells.244–246 In order to improve the biocompatibility and bio-stability of graphene platforms as well as their ability for the efficient transfection of genes, they have been modified with various polymers and ligands.247,248
There are a large number of studies regarding graphene-polymer platforms for gene delivery application. In 2018, an efficient non-viral gene delivery system was designed using PEI functionalized GO (GO-PEI) loaded with miR-7b by Dou et al which exhibited excellent transfection efficiency with low cytotoxicity.249 The results have shown that GO-PEI could efficiently deliver miR-7b plasmid into bone marrow macrophages. Animal study has demonstrated that preserved preosteoclast by GO-PEI-miR-7b enhanced bone vascularization in ovariectomized mice.
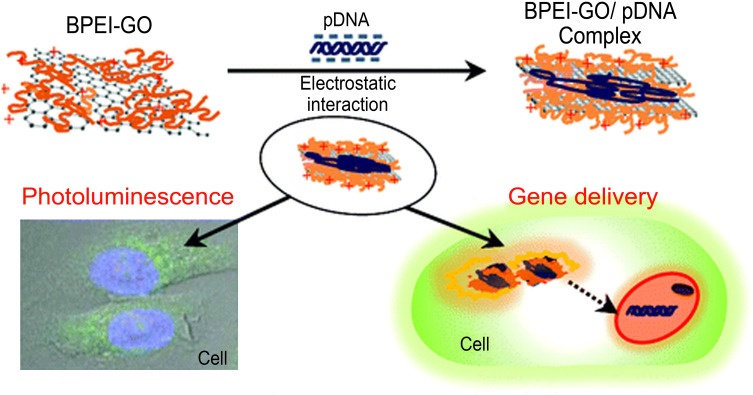
GO-PEI nanostructure has been fabricated as a gene delivery and bioimaging vector by Kim et al.250 Polyethylenimine as a cationic polymer, which has been widely used as a non-viral gene delivery vector, is conjugated to GO surface to improve its interactions with negatively charged genes. Combination of branched PEI and GO results in a hybrid system with enhanced transfection efficiency and photoluminescence property for simultaneous gene delivery and bioimaging (Figure 12). Branched PEI exhibits high transfection efficiency due to enhanced cellular uptake and a high level of endosomal escape. However, due to the high cytotoxicity of high molecular weight branched PEI (HMWBPEI), their use as effective gene delivery systems is limited. In contrast, low molecular weight branched PEI (HMWBPEI) shows poor transfection efficacy, while it has low cytotoxicity. When LMW BPEI is conjugated to GO, it demonstrated good cellular uptake and transfection efficiency with low cytotoxicity. The gene transfection efficiency is evaluated using luciferase gene expression assays. The results exhibited a low gene transfection for the individual pristine GO and LMW BPEI and a high transfection for HMW BPEI and BPEI-GO. High transfection efficiency of BPEI-GO is due to the effect of LMW BPEI conjugated to GO and formation of a stable polyelectrolyte complex with plasmid DNA.
Figure 12.
Schematic presentation of fabrication of GO-based gene delivery system through covalent attachment of LMW BPEI to this platform.
Notes: Conjugation of BPEI to GO enhances the photoluminescence properties of GO and improves the cellular uptake and transfection efficiency of the system. Therefore, BPEI-GO can be applied as bioimaging reagent and non-viral gene delivery vector simultaneously. Reproduced with permission from Kim H, Namgung R, Singha K, Oh IK, Kim WJ. Graphene oxide–polyethylenimine nanoconstruct as a gene delivery vector and bioimaging tool. Bioconjug Chem. 2011;22:2558–2567.250 Copyright © 2011, American Chemical Society.
In general, it can be concluded that polymer-functionalized graphene-based carriers have been widely applied in gene delivery to treat various diseases including cancer,251 osteoporosis,252 and myocardial infarction.253 A variety of macromolecules including cationic polymers, dendrimers, chitosan, and peptides have been used to modify graphene derivatives for efficient gene transfection.254–256
Graphene-Metal Platforms
Graphene derivatives with high surface area provide ideal platforms to immobilize various metal nanoparticles (MNPs) including Au, Fe, Pt, Gd, Pd, etc. in a sheet-like structure.257,258 Graphene/metal hybrids are investigated extensively for cancer therapy and imaging including photoacoustic imaging, PTT, thermomechanical, and surface enhanced Raman signals (SERS). Various approaches including in situ reduction, hydrothermal, electrochemical, physical vapor deposition, ex situ and wrapping MNPs have been reported to synthesize graphene/metal hybrids.259
In this regard, graphene-AuNPs hybrids have attracted a great deal of attention for various medical applications owing to their unique optoelectronic properties.260–262 Graphene-AuNPs hybrids are used as biosensors for the detection and diagnosis of cancer cells, due to their prominent surface plasmon resonance (SPR),263 NIR emission, quenching effect, adsorption of bioreceptors, enzyme mimic-peroxidase activities, improved electron transfer rate, and conductivity of both graphene and AuNPs.264 Moreover, GO-AuNPs are reported as electrochemical immunosensors for detection of various cancer markers including CEA, CA125, P53, PSA, AFP, and Vascular endothelial growth factor (VEGF) 150.265–267 As an example, rGO/thionine/AuNPs hybrid has been used to fabricate immunosensors for the detection of cancer antigen 125 (CA125).268 This fabricated immunosensor has demonstrated low detection limits (0.01 U mL-1), high reliability and accuracy. Moreover, various hybrids of GO-AuNPs are explored for fabrication of geno-biosensors for detection of DNA, miRNA-21, and plasma miR-155.269–271 On the other hand, graphene/AuNPs are widely used for photothermal therapy (PTT) and photodynamic therapy (PDT) owing to the synergic effect of both components such as strong NIR optical absorption, high NIR light-to-heat conversion, and ROS production.272,273
Magnetic graphene hybrids, particularly graphene/iron oxide, have shown synergistic therapeutic effect.274,275 It is demonstrated that graphene/Fe2O3 NPs hybrids can serve as MRI contrast and diagnosis agents.276,277 Besides efficient diagnostic applications, graphene/Fe2O3 NPs hybrids have been investigated as magnetically targeted drug delivery systems with simultaneous photothermal effect.278,279 Many studies have shown that drug-loaded graphene/Fe2O3 systems can be effectively accumulated at the targeted tumor site by applying an external magnetic field.275,280,281 Moreover, under external magnetic field these systems have exhibited enhanced release of the drug at the targeted tumor site owing to heat generated by the Fe3O4 NPs and deformation of the nanocarrier. Based on these outcomes, magnetic graphene hybrids have been supposed as safe and excellent tools for imaging of cancer cells, drug delivery, and hyperthermia.279,282–285
Lanthanide-based nanomaterials, particularly gadolinium, are another class of widely explored metals as contrast agents in MRI.286–288 Conjugation of gadolinium onto the surface of graphene-based materials endows new properties and enhances their magnetic, luminescence, and therapeutic properties. Due to its outstanding properties, graphene/GdNPs hybrid is one of the most promising nanomaterials for biomedicine applications including photodynamic/photothermal therapy, biosensing, and bioimaging.289,290
Extensive studies have pointed out that Pd-based nanomaterials are excellent platforms for promoting the chemotherapeutic effects of graphene drug delivery systems. Tumor model studies have shown a high performance of graphene/PdNPs hybrids for diagnosis and treatment of cancers.291,292
Conclusion
This review aims to explain the advantages and recent progresses in graphene-based platforms for different biomedical applications including drug and gene delivery as well as bioimaging. There is a great deal of attention to use graphene and its derivatives in biomedicine. However, an extensive study on the toxicity and health risks of this class of nanomaterials should be performed to diminish the risk of their long-term side effects. To achieve this goal, the key point is to produce a highly defined graphene family in terms of number of layers, surface area, and functionality.
Acknowledgment
The authors would like to thank Iran's Science Elites Federation for their financial support.
Disclosure
The authors reported no conflicts of interest for this work.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Zaorsky NG, Churilla T, Egleston B, et al. Causes of death among cancer patients. Ann Oncol. 2017;28:400–407. doi: 10.1093/annonc/mdw604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farhood B, Geraily G, Alizadeh A. Incidence and mortality of various cancers in Iran and compare to other countries: a review article. Iran J Public Health. 2018;47:309. [PMC free article] [PubMed] [Google Scholar]
- 4.Nagai H, Kim YH. Cancer prevention from the perspective of global cancer burden patterns. J Thorac Dis. 2017;9:448. doi: 10.21037/jtd.2017.02.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khairunnahar L, Hasib MA, Rezanur RHB, Islam MR, Hosain MK. Classification of malignant and benign tissue with logistic regression. Inform Med Unlocked. 2019;16:100189. doi: 10.1016/j.imu.2019.100189 [DOI] [Google Scholar]
- 7.Teramoto A, Tsujimoto M, Inoue T, et al. Automated classification of pulmonary nodules through a retrospective analysis of conventional CT and two-phase PET images in patients undergoing biopsy. Asia Oceania J Nucl Med Biol. 2019;7:29. doi: 10.22038/AOJNMB.2018.12014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beiranvand Z, Bani F, Kakanejadifard A, et al. Anticancer drug delivery systems based on specific interactions between albumin and polyglycerol. RSC Adv. 2016;6:11266–11277. doi: 10.1039/C5RA25463A [DOI] [Google Scholar]
- 9.Mohammadifar E, Kharat AN, Adeli M. Polyamidoamine and polyglycerol; their linear, dendritic and linear–dendritic architectures as anticancer drug delivery systems. J Mater Chem B. 2015;3:3896–3921. doi: 10.1039/C4TB02133A [DOI] [PubMed] [Google Scholar]
- 10.Pucci C, Martinelli C, Ciofani G. Innovative approaches for cancer treatment: current perspectives and new challenges. Ecancermedicalscience. 2019;13. doi: 10.3332/ecancer.2019.961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chakraborty C, Sharma AR, Sharma G, Sarkar BK, Lee -S-S. The novel strategies for next-generation cancer treatment: miRNA combined with chemotherapeutic agents for the treatment of cancer. Oncotarget. 2018;9:10164. doi: 10.18632/oncotarget.24309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pedrosa P, Mendes R, Cabral R, Martins LM, Baptista PV, Fernandes AR. Combination of chemotherapy and Au-nanoparticle photothermy in the visible light to tackle doxorubicin resistance in cancer cells. Sci Rep. 2018;8:1–8. doi: 10.1038/s41598-018-29870-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liang X-J, Chen C, Zhao Y, Wang PC. Circumventing tumor resistance to chemotherapy by nanotechnology. In: Zhou J, editor. Multi-Drug Resistance in Cancer. Springer; 2010:467–488. doi: 10.1007/978-1-60761-416-6_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tu Z, Qiao H, Yan Y, et al. Directed graphene‐based nanoplatforms for hyperthermia: overcoming multiple drug resistance. Angew Chem. 2018;130:11368–11372. doi: 10.1002/ange.201804291 [DOI] [PubMed] [Google Scholar]
- 15.Yu W, Liu R, Zhou Y, Gao H. Size-tunable strategies for a tumor targeted drug delivery system. ACS Cent Sci. 2020;6:100–116. doi: 10.1021/acscentsci.9b01139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao L, Xing Y, Wang R, Yu F, Yu F. Self-assembled nanomaterials for enhanced phototherapy of cancer. ACS Applied Bio Mater. 2019;3:86–106. doi: 10.1021/acsabm.9b00843 [DOI] [PubMed] [Google Scholar]
- 17.Zhou Q, Zhang L, Wu H. Nanomaterials for cancer therapies. Nanotechnology Reviews. 2017;6:473–496. [Google Scholar]
- 18.Adeli M, Rasoulian B, Saadatmehr F, Zabihi F. Hyperbranched poly (citric acid) and its application as anticancer drug delivery system. J Appl Polym Sci. 2013;129:3665–3671. doi: 10.1002/app.39028 [DOI] [Google Scholar]
- 19.Dang Y, Guan J. Nanoparticle-based drug delivery systems for cancer therapy. Smart Mater Med. 2020;1:10–19. doi: 10.1016/j.smaim.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chegeni BK, Kakanejadifard A, Abedi F, Kabiri R, Daneshnia F, Adeli M. pH-sensitive supramolecular copolydendrimers, new anticancer drug delivery system. Colloid Polym Sci. 2014;292:3337–3346. doi: 10.1007/s00396-014-3398-2 [DOI] [Google Scholar]
- 21.Eskandari M, Hosseini SH, Adeli M, Pourjavadi A. Polymer-functionalized carbon nanotubes in cancer therapy: a review. Iran Polym J. 2014;23:387–403. doi: 10.1007/s13726-014-0228-9 [DOI] [Google Scholar]
- 22.Adeli M, Soleyman R, Beiranvand Z, Madani F. Carbon nanotubes in cancer therapy: a more precise look at the role of carbon nanotube–polymer interactions. Chem Soc Rev. 2013;42:5231–5256. doi: 10.1039/c3cs35431h [DOI] [PubMed] [Google Scholar]
- 23.Souri Z, Adeli M, Mehdipour E. Two-dimensional MoS 2: a platform for constructing three-dimensional structures using RAFT polymerization. New J Chem. 2020;44:17961–17969. doi: 10.1039/D0NJ03285A [DOI] [Google Scholar]
- 24.Faghani A, Gholami MF, Trunk M, et al. Metal-assisted and solvent-mediated synthesis of two-dimensional triazine structures on Gram Scale. J Am Chem Soc. 2020;142:12976–12986. doi: 10.1021/jacs.0c02399 [DOI] [PubMed] [Google Scholar]
- 25.Sattari S, Beyranvand S, Soleimani K, et al. Boronic acid-functionalized two-dimensional MoS2 at biointerfaces. Langmuir. 2020;36:6706–6715. doi: 10.1021/acs.langmuir.0c00776 [DOI] [PubMed] [Google Scholar]
- 26.Daneshnia S, Adeli M, Yari A, Shams A, Donskyi IS, Unger WE. Low temperature functionalization of two-dimensional boron nitride for electrochemical sensing. Mater Res Express. 2019;6:095076. doi: 10.1088/2053-1591/ab317b [DOI] [Google Scholar]
- 27.Daneshnia S, Adeli M, Mansourpanah Y. Gram scale and room temperature functionalization of boron nitride nanosheets for water treatment. Nano. 2019;14:1950107. doi: 10.1142/S1793292019501078 [DOI] [Google Scholar]
- 28.Souri Z, Adeli M, Mehdipour E, et al. Covalent decoration of MoS2 platforms by silver nanoparticles through the reversible addition–fragmentation chain transfer reaction. Langmuir. 2021;37(11):3382–3390. doi: 10.1021/acs.langmuir.0c03518 [DOI] [PubMed] [Google Scholar]
- 29.Patra JK, Das G, Fraceto LF, et al. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnology. 2018;16:1–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orecchioni M, Cabizza R, Bianco A, Delogu LG. Graphene as cancer theranostic tool: progress and future challenges. Theranostics. 2015;5:710. doi: 10.7150/thno.11387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shareena TPD, McShan D, Dasmahapatra AK, Tchounwou PB. A review on graphene-based nanomaterials in biomedical applications and risks in environment and health. Nano Micro Lett. 2018;10:1–34. doi: 10.1007/s40820-017-0154-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Donskyi IS, Chen Y, Nickl P, et al. Self-degrading graphene sheets for tumor therapy. Nanoscale. 2020;12:14222–14229. doi: 10.1039/D0NR02159H [DOI] [PubMed] [Google Scholar]
- 33.Gheybi H, Sattari S, Soleimani K, Adeli M. Graphene-dendritic polymer hybrids: synthesis, properties, and applications. J Iran Chem Soc. 2020;17:735–764. [Google Scholar]
- 34.Schedin F, Geim AK, Morozov SV, et al. Detection of individual gas molecules adsorbed on graphene. Nat Mater. 2007;6:652–655. doi: 10.1038/nmat1967 [DOI] [PubMed] [Google Scholar]
- 35.Olabi A, Abdelkareem MA, Wilberforce T, Sayed ET. Application of graphene in energy storage device–A review. Renew Sustain Energy Rev. 2021;135:110026. [Google Scholar]
- 36.Wang B, Ruan T, Chen Y, et al. Graphene-based composites for electrochemical energy storage. Energy Storage Mater. 2020;24:22–51. [Google Scholar]
- 37.Tehrani Z, Whelan S, Mostert A, et al. Printable and flexible graphene pH sensors utilising thin film melanin for physiological applications. 2D Mater. 2020;7:024008. doi: 10.1088/2053-1583/ab72d5 [DOI] [Google Scholar]
- 38.Farooqi BA, Yar M, Ashraf A, Farooq U, Ayub K. Graphene-polyaniline composite as superior electrochemical sensor for detection of cyano explosives. Eur Polym J. 2020;138:109981. doi: 10.1016/j.eurpolymj.2020.109981 [DOI] [Google Scholar]
- 39.Suvarnaphaet P, Pechprasarn S. Graphene-based materials for biosensors: a review. Sensors. 2017;17:2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tonelli FM, Goulart VA, Gomes KN, et al. Graphene-based nanomaterials: biological and medical applications and toxicity. Nanomedicine. 2015;10:2423–2450. doi: 10.2217/nnm.15.65 [DOI] [PubMed] [Google Scholar]
- 41.Priyadarsini S, Mohanty S, Mukherjee S, Basu S, Mishra M. Graphene and graphene oxide as nanomaterials for medicine and biology application. J Nanostructure Chem. 2018;8:123–137. doi: 10.1007/s40097-018-0265-6 [DOI] [Google Scholar]
- 42.Donskyi IS, Azab W, Cuellar-Camacho JL, et al. Functionalized nanographene sheets with high antiviral activity through synergistic electrostatic and hydrophobic interactions. Nanoscale. 2019;11:15804–15809. doi: 10.1039/C9NR05273A [DOI] [PubMed] [Google Scholar]
- 43.Beyranvand S, Gholami MF, Tehrani AD, Rabe P Jr, Adeli M. Construction and evaluation of a self-calibrating multiresponse and multifunctional graphene biosensor. Langmuir. 2019;35:10461–10474. doi: 10.1021/acs.langmuir.9b00915 [DOI] [PubMed] [Google Scholar]
- 44.Tan KH, Sattari S, Beyranvand S, et al. Thermoresponsive amphiphilic functionalization of thermally reduced graphene oxide to study graphene/bacteria hydrophobic interactions. Langmuir. 2019;35:4736–4746. doi: 10.1021/acs.langmuir.8b03660 [DOI] [PubMed] [Google Scholar]
- 45.Mohammad-Beigi H, Hosseini A, Adeli M, et al. Mechanistic understanding of the interactions between nano-objects with different surface properties and α-synuclein. ACS Nano. 2019;13:3243–3256. doi: 10.1021/acsnano.8b08983 [DOI] [PubMed] [Google Scholar]
- 46.Soleimani K, Tehrani AD, Adeli M, Sattari S. Convenient method for preparation of a new absorbent based on biofunctionalized graphene oxide hydrogels using nitrene chemistry and click reaction. Iran Polym J. 2018;27:689–699. doi: 10.1007/s13726-018-0645-2 [DOI] [Google Scholar]
- 47.Wang Y, Qiu M, Won M, et al. Emerging 2D material-based nanocarrier for cancer therapy beyond graphene. Coord Chem Rev. 2019;400:213041. doi: 10.1016/j.ccr.2019.213041 [DOI] [Google Scholar]
- 48.de Melo-diogo D, Lima-Sousa R, Alves CG, Costa EC, Louro RO, Correia IJ. Functionalization of graphene family nanomaterials for application in cancer therapy. Colloids Surf B Biointerfaces. 2018;171:260–275. doi: 10.1016/j.colsurfb.2018.07.030 [DOI] [PubMed] [Google Scholar]
- 49.Wang W, Meng Z, Liang R, et al. A dynamically tunable plasmonic multi-functional device based on graphene nano-sheet pair arrays. Opt Commun. 2018;415:130–134. doi: 10.1016/j.optcom.2018.01.049 [DOI] [Google Scholar]
- 50.Peng L, Li X-F, Gao X, Jiang X, Li S-M. Methodology for the design of a multi-functional device with switchable absorption and polarization conversion modes by graphene and metallic metasurfaces. Opt Mater Express. 2019;9(2):687–705. doi: 10.1364/OME.9.000687 [DOI] [Google Scholar]
- 51.Tu Z, Guday G, Adeli M, Haag R. Multivalent interactions between 2D nanomaterials and biointerfaces. Adv Mater. 2018;30:1706709. doi: 10.1002/adma.201706709 [DOI] [PubMed] [Google Scholar]
- 52.De D, Das CK, Mandal D, et al. Curcumin complexed with graphene derivative for breast cancer therapy. ACS Applied Bio Mater. 2020;3:6284–6296. doi: 10.1021/acsabm.0c00771 [DOI] [PubMed] [Google Scholar]
- 53.Yadav N, Kannan D, Patil S, Singh S, Lochab B. Amplified activity of artesunate mediated by iron oxide nanoparticles loaded on a graphene oxide carrier for cancer therapeutics. ACS Applied Bio Mater. 2020;3:6722–6736. doi: 10.1021/acsabm.0c00632 [DOI] [PubMed] [Google Scholar]
- 54.Yang Z, Yang D, Zeng K, et al. Simultaneous delivery of antimiR-21 and doxorubicin by graphene oxide for reducing toxicity in cancer therapy. ACS Omega. 2020;5:14437–14443. doi: 10.1021/acsomega.0c01010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu L, Zhang J, Zhao J, Liu F. Mechanical properties of graphene oxides. Nanoscale. 2012;4:5910–5916. doi: 10.1039/c2nr31164j [DOI] [PubMed] [Google Scholar]
- 56.Mousavi SM, Hashemi SA, Ghasemi Y, Amani AM, Babapoor A, Arjmand O. Applications of graphene oxide in case of nanomedicines and nanocarriers for biomolecules: review study. Drug Metab Rev. 2019;51:12–41. doi: 10.1080/03602532.2018.1522328 [DOI] [PubMed] [Google Scholar]
- 57.Wu J, Wang Y-S, Yang X-Y, et al. Graphene oxide used as a carrier for adriamycin can reverse drug resistance in breast cancer cells. Nanotechnology. 2012;23:355101. doi: 10.1088/0957-4484/23/35/355101 [DOI] [PubMed] [Google Scholar]
- 58.Li X, Wang Y, Shi L, et al. A novel ECL biosensor for the detection of concanavalin A based on glucose functionalized NiCo2S4 nanoparticles-grown on carboxylic graphene as quenching probe. Biosens Bioelectron. 2017;96:113–120. doi: 10.1016/j.bios.2017.04.050 [DOI] [PubMed] [Google Scholar]
- 59.Xiao FN, Wang M, Wang FB, Xia XH. Graphene–ruthenium (II) complex composites for sensitive ECL immunosensors. Small. 2014;10:706–716. doi: 10.1002/smll.201301566 [DOI] [PubMed] [Google Scholar]
- 60.Zhu M, Tang Y, Wen Q, Li J, Yang P. Dynamic evaluation of cell-secreted interferon gamma in response to drug stimulation via a sensitive electro-chemiluminescence immunosensor based on a glassy carbon electrode modified with graphene oxide, polyaniline nanofibers, magnetic beads, and gold nanoparticles. Microchim Acta. 2016;183:1739–1748. [Google Scholar]
- 61.Wang C-I, Wu W-C, Periasamy AP, Chang H-T. Sensitive and selective DNA probe based on “turn-on” photoluminescence of C-dots@ RGO. Anal Bioanal Chem. 2014;406:6917–6923. doi: 10.1007/s00216-014-7658-2 [DOI] [PubMed] [Google Scholar]
- 62.Yao J, Wang H, Chen M, Yang M. Recent advances in graphene-based nanomaterials: properties, toxicity and applications in chemistry, biology and medicine. Microchim Acta. 2019;186:1–25. [DOI] [PubMed] [Google Scholar]
- 63.Tong C, Zhao C, Liu B, et al. Sensitive detection of RNase a activity and collaborative drug screening based on rGO and fluorescence probe. Anal Chem. 2018;90:2655–2661. doi: 10.1021/acs.analchem.7b04429 [DOI] [PubMed] [Google Scholar]
- 64.Alizadeh N, Salimi A, Hallaj R, Fathi F, Soleimani F. CuO/WO3 nanoparticles decorated graphene oxide nanosheets with enhanced peroxidase-like activity for electrochemical cancer cell detection and targeted therapeutics. Mater Sci Eng C. 2019;99:1374–1383. doi: 10.1016/j.msec.2019.02.048 [DOI] [PubMed] [Google Scholar]
- 65.Yang K, Feng L, Shi X, Liu Z. Nano-graphene in biomedicine: theranostic applications. Chem Soc Rev. 2013;42:530–547. doi: 10.1039/C2CS35342C [DOI] [PubMed] [Google Scholar]
- 66.Zhang Y, Nayak TR, Hong H, Cai W. Graphene: a versatile nanoplatform for biomedical applications. Nanoscale. 2012;4:3833–3842. doi: 10.1039/c2nr31040f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jia -P-P, Sun T, Junaid M, et al. Nanotoxicity of different sizes of graphene (G) and graphene oxide (GO) in vitro and in vivo. Environ Pollut. 2019;247:595–606. doi: 10.1016/j.envpol.2019.01.072 [DOI] [PubMed] [Google Scholar]
- 68.Zhang L, Xia J, Zhao Q, Liu L, Zhang Z. Functional graphene oxide as a nanocarrier for controlled loading and targeted delivery of mixed anticancer drugs. Small. 2010;6:537–544. doi: 10.1002/smll.200901680 [DOI] [PubMed] [Google Scholar]
- 69.Lammel T, Boisseaux P, Fernández-Cruz M-L, Navas JM. Internalization and cytotoxicity of graphene oxide and carboxyl graphene nanoplatelets in the human hepatocellular carcinoma cell line Hep G2. Part Fibre Toxicol. 2013;10:1–21. doi: 10.1186/1743-8977-10-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Akhavan O, Ghaderi E, Akhavan A. Size-dependent genotoxicity of graphene nanoplatelets in human stem cells. Biomaterials. 2012;33:8017–8025. doi: 10.1016/j.biomaterials.2012.07.040 [DOI] [PubMed] [Google Scholar]
- 71.Li Y, Liu Y, Fu Y, et al. The triggering of apoptosis in macrophages by pristine graphene through the MAPK and TGF-beta signaling pathways. Biomaterials. 2012;33:402–411. doi: 10.1016/j.biomaterials.2011.09.091 [DOI] [PubMed] [Google Scholar]
- 72.Liao K-H, Lin Y-S, Macosko CW, Haynes CL. Cytotoxicity of graphene oxide and graphene in human erythrocytes and skin fibroblasts. ACS Appl Mater Interfaces. 2011;3:2607–2615. doi: 10.1021/am200428v [DOI] [PubMed] [Google Scholar]
- 73.Chowdhury SM, Lalwani G, Zhang K, Yang JY, Neville K, Sitharaman B. Cell specific cytotoxicity and uptake of graphene nanoribbons. Biomaterials. 2013;34:283–293. doi: 10.1016/j.biomaterials.2012.09.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jaworski S, Sawosz E, Kutwin M, et al. In vitro and in vivo effects of graphene oxide and reduced graphene oxide on glioblastoma. Int J Nanomedicine. 2015;10:1585. doi: 10.2147/IJN.S77591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gurunathan S, Han JW, Kim ES, Park JH, Kim J-H. Reduction of graphene oxide by resveratrol: a novel and simple biological method for the synthesis of an effective anticancer nanotherapeutic molecule. Int J Nanomedicine. 2015;10:2951. doi: 10.2147/IJN.S79879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhao J, Wang Z, White JC, Xing B. Graphene in the aquatic environment: adsorption, dispersion, toxicity and transformation. Environ Sci Technol. 2014;48:9995–10009. doi: 10.1021/es5022679 [DOI] [PubMed] [Google Scholar]
- 77.Hu W, Peng C, Luo W, et al. Graphene-based antibacterial paper. ACS Nano. 2010;4:4317–4323. doi: 10.1021/nn101097v [DOI] [PubMed] [Google Scholar]
- 78.Sydlik SA, Jhunjhunwala S, Webber MJ, Anderson DG, Langer R. In vivo compatibility of graphene oxide with differing oxidation states. ACS Nano. 2015;9:3866–3874. doi: 10.1021/acsnano.5b01290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Duch MC, Budinger GS, Liang YT, et al. Minimizing oxidation and stable nanoscale dispersion improves the biocompatibility of graphene in the lung. Nano Lett. 2011;11:5201–5207. doi: 10.1021/nl202515a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Schinwald A, Murphy FA, Jones A, MacNee W, Donaldson K. Graphene-based nanoplatelets: a new risk to the respiratory system as a consequence of their unusual aerodynamic properties. ACS Nano. 2012;6:736–746. doi: 10.1021/nn204229f [DOI] [PubMed] [Google Scholar]
- 81.Zhang S, Yang K, Feng L, Liu Z. In vitro and in vivo behaviors of dextran functionalized graphene. Carbon. 2011;49:4040–4049. doi: 10.1016/j.carbon.2011.05.056 [DOI] [Google Scholar]
- 82.Krasteva N, Keremidarska-Markova M, Hristova-Panusheva K, et al. Aminated graphene oxide as a potential new therapy for colorectal cancer. Oxid Med Cell Longev. 2019;2019:1–15. doi: 10.1155/2019/3738980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Park J, Yan M. Covalent functionalization of graphene with reactive intermediates. Acc Chem Res. 2013;46:181–189. doi: 10.1021/ar300172h [DOI] [PubMed] [Google Scholar]
- 84.Wang B, Su X, Liang J, et al. Synthesis of polymer-functionalized nanoscale graphene oxide with different surface charge and its cellular uptake, biosafety and immune responses in Raw264. 7 macrophages. Mater Sci Eng C. 2018;90:514–522. doi: 10.1016/j.msec.2018.04.096 [DOI] [PubMed] [Google Scholar]
- 85.Charmi J, Nosrati H, Amjad JM, Mohammadkhani R, Danafar H. Polyethylene glycol (PEG) decorated graphene oxide nanosheets for controlled release curcumin delivery. Heliyon. 2019;5:e01466. doi: 10.1016/j.heliyon.2019.e01466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mendonça MCP, Soares ES, de Jesus MB, et al. PEGylation of reduced graphene oxide induces toxicity in cells of the blood–brain barrier: an in vitro and in vivo study. Mol Pharm. 2016;13:3913–3924. doi: 10.1021/acs.molpharmaceut.6b00696 [DOI] [PubMed] [Google Scholar]
- 87.Yang K, Wan J, Zhang S, Zhang Y, Lee S-T, Liu Z. In vivo pharmacokinetics, long-term biodistribution, and toxicology of PEGylated graphene in mice. ACS Nano. 2011;5:516–522. doi: 10.1021/nn1024303 [DOI] [PubMed] [Google Scholar]
- 88.Shi J, Kantoff PW, Wooster R, Farokhzad OC. Cancer nanomedicine: progress, challenges and opportunities. Nat Rev Cancer. 2017;17:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yuan D, He H, Wu Y, Fan J, Cao Y. Physiologically based pharmacokinetic modeling of nanoparticles. J Pharm Sci. 2019;108:58–72. doi: 10.1016/j.xphs.2018.10.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Elci SG, Jiang Y, Yan B, et al. Surface charge controls the suborgan biodistributions of gold nanoparticles. ACS Nano. 2016;10:5536–5542. doi: 10.1021/acsnano.6b02086 [DOI] [PubMed] [Google Scholar]
- 91.Syama S, Paul W, Sabareeswaran A, Mohanan PV. Raman spectroscopy for the detection of organ distribution and clearance of PEGylated reduced graphene oxide and biological consequences. Biomaterials. 2017;131:121–130. doi: 10.1016/j.biomaterials.2017.03.043 [DOI] [PubMed] [Google Scholar]
- 92.Chen L, Wang C, Li H, Qu X, Yang S-T, Chang X-L. Bioaccumulation and toxicity of 13C-skeleton labeled graphene oxide in wheat. Environ Sci Technol. 2017;51:10146–10153. doi: 10.1021/acs.est.7b00822 [DOI] [PubMed] [Google Scholar]
- 93.Peng H, Zhang L, Cai Z, et al. Pharmacokinetics study of isorhamnetin in rat plasma by a sensitive electrochemical sensor based on reduced graphene oxide. RSC Adv. 2017;7:36728–36734. doi: 10.1039/C7RA03632A [DOI] [Google Scholar]
- 94.Liang S, Wang B, Li X, et al. In vivo pharmacokinetics, transfer and clearance study of graphene oxide by La/Ce dual elemental labelling method. NanoImpact. 2020;17:100213. doi: 10.1016/j.impact.2020.100213 [DOI] [Google Scholar]
- 95.Sun X, Huang C, Wang L, et al. Recent progress in graphene/polymer nanocomposites. Adv Mater. 2020:2001105. [Google Scholar]
- 96.Silva M, Alves NM, Paiva MC. Graphene‐polymer nanocomposites for biomedical applications. Polym Adv Technol. 2018;29:687–700. doi: 10.1002/pat.4164 [DOI] [Google Scholar]
- 97.Tadyszak K, Wychowaniec JK, Litowczenko J. Biomedical applications of graphene-based structures. Nanomaterials. 2018;8:944. doi: 10.3390/nano8110944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Donskyi IS, Nie C, Ludwig K, et al. Graphene sheets with defined dual functionalities for the strong SARS‐CoV‐2 interactions. Small. 2021;17(11):2007091. doi: 10.1002/smll.202007091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Song S, Shen H, Wang Y, et al. Biomedical application of graphene: from drug delivery, tumor therapy, to theranostics. Colloids Surf B Biointerfaces. 2020;185:110596. doi: 10.1016/j.colsurfb.2019.110596 [DOI] [PubMed] [Google Scholar]
- 100.Gheybi H, Sattari S, Soleimani K, Adeli M. Graphene-dendritic polymer hybrids: synthesis, properties, and applications. J Iran Chem Soc. 2020:1–30. [Google Scholar]
- 101.Tehrani AD, Adeli M, Sattari S, Soleimani K. Graphene oxide–polymer gels. In: Thakur V, Thakur M, editors. Polymer Gels. Springer; 2018:377–412. [Google Scholar]
- 102.Guday G, Donskyi IS, Gholami MF, et al. Scalable production of nanographene and doping via nondestructive covalent functionalization. Small. 2019;15:1805430. doi: 10.1002/smll.201805430 [DOI] [PubMed] [Google Scholar]
- 103.Bani F, Bodaghi A, Dadkhah A, et al. One-pot exfoliation, functionalization, and size manipulation of graphene sheets: efficient system for biomedical applications. Lasers Med Sci. 2018;33:795–802. doi: 10.1007/s10103-017-2422-4 [DOI] [PubMed] [Google Scholar]
- 104.Faghani A, Donskyi IS, Fardin Gholami M, et al. Controlled covalent functionalization of thermally reduced graphene oxide to generate defined bifunctional 2D nanomaterials. Angew Chem. 2017;129:2719–2723. doi: 10.1002/ange.201612422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Khani M, Mehdipour E, Faghani A, et al. Preparation of graphene oxide by cyanuric chloride as an effective and non-corrosive oxidizing agent. RSC Adv. 2016;6:115055–115057. doi: 10.1039/C6RA23702A [DOI] [Google Scholar]
- 106.Maleki M, Adeli M, Kakanejadifard A, Movahedi S, Bani F. Enzymatic functionalization of nanomaterials: a strategy for engineering their surfaces. Polymer. 2013;54:4802–4806. doi: 10.1016/j.polymer.2013.07.023 [DOI] [Google Scholar]
- 107.Georgakilas V, Otyepka M, Bourlinos AB, et al. Functionalization of graphene: covalent and non-covalent approaches, derivatives and applications. Chem Rev. 2012;112:6156–6214. [DOI] [PubMed] [Google Scholar]
- 108.Nanda SS, Papaefthymiou GC, Yi DK. Functionalization of graphene oxide and its biomedical applications. Crit Rev Solid State Mater Sci. 2015;40:291–315. doi: 10.1080/10408436.2014.1002604 [DOI] [Google Scholar]
- 109.Strom TA, Dillon EP, Hamilton CE, Barron AR. Nitrene addition to exfoliated graphene: a one-step route to highly functionalized graphene. Chem Commun. 2010;46:4097–4099. doi: 10.1039/c001488e [DOI] [PubMed] [Google Scholar]
- 110.Gao C, He H, Zhou L, Zheng X, Zhang Y. Scalable functional group engineering of carbon nanotubes by improved one-step nitrene chemistry. Chem Mater. 2009;21:360–370. doi: 10.1021/cm802704c [DOI] [Google Scholar]
- 111.Setaro A, Adeli M, Glaeske M, et al. Preserving π-conjugation in covalently functionalized carbon nanotubes for optoelectronic applications. Nat Commun. 2017;8:1–7. doi: 10.1038/ncomms14281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gholami MF, Lauster D, Ludwig K, et al. Functionalized graphene as extracellular matrix mimics: toward well‐defined 2D nanomaterials for multivalent virus interactions. Adv Funct Mater. 2017;27:1606477. doi: 10.1002/adfm.201606477 [DOI] [Google Scholar]
- 113.Pei X, Zhu Z, Gan Z, et al. PEGylated nano-graphene oxide as a nanocarrier for delivering mixed anticancer drugs to improve anticancer activity. Sci Rep. 2020;10:1–15. doi: 10.1038/s41598-020-59624-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Xu Z, Wang S, Li Y, Wang M, Shi P, Huang X. Covalent functionalization of graphene oxide with biocompatible poly (ethylene glycol) for delivery of paclitaxel. ACS Appl Mater Interfaces. 2014;6:17268–17276. doi: 10.1021/am505308f [DOI] [PubMed] [Google Scholar]
- 115.Abdollahi Z, Taheri-Kafrani A, Bahrani SA, Kajani AA. PEGAylated graphene oxide/superparamagnetic nanocomposite as a high-efficiency loading nanocarrier for controlled delivery of methotrexate. J Biotechnol. 2019;298:88–97. doi: 10.1016/j.jbiotec.2019.04.006 [DOI] [PubMed] [Google Scholar]
- 116.Mallick A, Nandi A, Basu S. Polyethylenimine coated graphene oxide nanoparticles for targeting mitochondria in cancer cells. ACS Applied Bio Mater. 2018;2:14–19. doi: 10.1021/acsabm.8b00519 [DOI] [PubMed] [Google Scholar]
- 117.Ren T, Li L, Cai X, Dong H, Liu S, Li Y. Engineered polyethylenimine/graphene oxide nanocomposite for nuclear localized gene delivery. Polym Chem. 2012;3:2561–2569. doi: 10.1039/c2py20343j [DOI] [Google Scholar]
- 118.Anirudhan T, Sekhar VC, Athira V. Graphene oxide based functionalized chitosan polyelectrolyte nanocomposite for targeted and pH responsive drug delivery. Int J Biol Macromol. 2020;150:468–479. doi: 10.1016/j.ijbiomac.2020.02.053 [DOI] [PubMed] [Google Scholar]
- 119.Omidi S, Pirhayati M, Kakanejadifard A. Co-delivery of doxorubicin and curcumin by a pH-sensitive, injectable, and in situ hydrogel composed of chitosan, graphene, and cellulose nanowhisker. Carbohydr Polym. 2020;231:115745. doi: 10.1016/j.carbpol.2019.115745 [DOI] [PubMed] [Google Scholar]
- 120.Wen C, Cheng R, Gong T, et al. β-Cyclodextrin-cholic acid-hyaluronic acid polymer coated Fe3O4-graphene oxide nanohybrids as local chemo-photothermal synergistic agents for enhanced liver tumor therapy. Colloids Surf B Biointerfaces. 2020:111510. [DOI] [PubMed] [Google Scholar]
- 121.Lima-Sousa R, de Melo-diogo D, Alves CG, et al. Hyaluronic acid functionalized green reduced graphene oxide for targeted cancer photothermal therapy. Carbohydr Polym. 2018;200:93–99. doi: 10.1016/j.carbpol.2018.07.066 [DOI] [PubMed] [Google Scholar]
- 122.Gu Y, Guo Y, Wang C, et al. A polyamidoamne dendrimer functionalized graphene oxide for DOX and MMP-9 shRNA plasmid co-delivery. Mater Sci Eng C. 2017;70:572–585. doi: 10.1016/j.msec.2016.09.035 [DOI] [PubMed] [Google Scholar]
- 123.Gheybi H, Sattari S, Bodaghi A, Soleimani K, Dadkhah A, Adeli M. Polyglycerols. In: Parambath A, editor.Engineering of Biomaterials for Drug Delivery Systems. Elsevier; 2018:103–171. doi: 10.1016/B978-0-08-101750-0.00005-2 [DOI] [Google Scholar]
- 124.Mu W, Chu Q, Liu Y, Zhang N. A review on nano-based drug delivery system for cancer chemoimmunotherapy. Nano Micro Lett. 2020;12:1–24. doi: 10.1007/s40820-020-00482-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yao Y, Zhou Y, Liu L, et al. Nanoparticle-based drug delivery in cancer therapy and its role in overcoming drug resistance. Front Mol Biosci. 2020;7. doi: 10.3389/fmolb.2020.00193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tu Z, Donskyi IS, Qiao H, et al. Graphene oxide‐cyclic R10 peptide nuclear translocation nanoplatforms for the surmounting of multiple‐drug resistance. Adv Funct Mater. 2020;30:2000933. doi: 10.1002/adfm.202000933 [DOI] [Google Scholar]
- 127.Liu J, Dong J, Zhang T, Peng Q. Graphene-based nanomaterials and their potentials in advanced drug delivery and cancer therapy. J Control Release. 2018;286:64–73. doi: 10.1016/j.jconrel.2018.07.034 [DOI] [PubMed] [Google Scholar]
- 128.Jokar S, Pourjavadi A, Adeli M. Albumin–graphene oxide conjugates; carriers for anticancer drugs. RSC Adv. 2014;4:33001–33006. doi: 10.1039/C4RA05752J [DOI] [Google Scholar]
- 129.Viseu T, Lopes CM, Fernandes E, Real Oliveira MEC, Lúcio M. A systematic review and critical analysis of the role of graphene-based nanomaterials in cancer theranostics. Pharmaceutics. 2018;10:282. doi: 10.3390/pharmaceutics10040282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Fusco L, Gazzi A, Peng G, et al. Graphene and other 2D materials: a multidisciplinary analysis to uncover the hidden potential as cancer theranostics. Theranostics. 2020;10:5435. doi: 10.7150/thno.40068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tu Z, Wycisk V, Cheng C, Chen W, Adeli M, Haag R. Functionalized graphene sheets for intracellular controlled release of therapeutic agents. Nanoscale. 2017;9:18931–18939. doi: 10.1039/C7NR06588D [DOI] [PubMed] [Google Scholar]
- 132.Liu Z, Robinson JT, Sun X, Dai H. PEGylated nanographene oxide for delivery of water-insoluble cancer drugs. J Am Chem Soc. 2008;130:10876–10877. doi: 10.1021/ja803688x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chai D, Hao B, Hu R, et al. Delivery of oridonin and methotrexate via PEGylated graphene oxide. ACS Appl Mater Interfaces. 2019;11:22915–22924. doi: 10.1021/acsami.9b03983 [DOI] [PubMed] [Google Scholar]
- 134.Demirel E, Karaca E, Durmaz YY. Effective PEGylation method to improve biocompatibility of graphene derivatives. Eur Polym J. 2020;124:109504. doi: 10.1016/j.eurpolymj.2020.109504 [DOI] [Google Scholar]
- 135.Zhang Y, Liu C, Shi W, Wang Z, Dai L, Zhang X. Direct measurements of the interaction between pyrene and graphite in aqueous media by single molecule force spectroscopy: understanding the π− π interactions. Langmuir. 2007;23:7911–7915. doi: 10.1021/la700876d [DOI] [PubMed] [Google Scholar]
- 136.Zeng Y, Yang Z, Li H, et al. Multifunctional nanographene oxide for targeted gene-mediated thermochemotherapy of drug-resistant tumour. Sci Rep. 2017;7:43506. doi: 10.1038/srep43506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fávaro WJ, de Souza JG, Ferreira LA, et al. Hybrid graphene oxide as carrier of doxorubicin: cytotoxicity and preliminary in vivo assays against bladder cancer. Adv Nat Sci Nanosci Nanotechnol. 2020;11:025016. [Google Scholar]
- 138.Jiao J, Pan M, Liu X, Liu J, Li B, Chen Q. An ultrasensitive non-enzymatic sensor for quantitation of anti-cancer substance chicoric acid based on bimetallic nanoalloy with polyetherimide-capped reduced graphene oxide. Nanomaterials. 2020;10:499. doi: 10.3390/nano10030499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Liu J, Chen X, Jiang Y, Cheng W. Development of an immune gene prognostic classifier for survival prediction and respond to immunocheckpoint inhibitor therapy/chemotherapy in endometrial cancer. Int Immunopharmacol. 2020;86:106735. doi: 10.1016/j.intimp.2020.106735 [DOI] [PubMed] [Google Scholar]
- 140.Soheili N, Eshghi M, Emadi-Baygi M, Mirzaei SA, Heidari R, Hosseinzadeh M. Design and evaluation of biological gate circuits and their therapeutic applications in a model of multidrug resistant cancers. Biotechnol Lett. 2020:1–11. [DOI] [PubMed] [Google Scholar]
- 141.Xie B, Yi J, Peng J, et al. Characterization of synergistic anti-tumor effects of doxorubicin and p53 via graphene oxide-polyethyleneimine nanocarriers. J Mater Sci Technol. 2017;33:807–814. doi: 10.1016/j.jmst.2017.05.005 [DOI] [Google Scholar]
- 142.Pooresmaeil M, Namazi H. β-Cyclodextrin grafted magnetic graphene oxide applicable as cancer drug delivery agent: synthesis and characterization. Mater Chem Phys. 2018;218:62–69. doi: 10.1016/j.matchemphys.2018.07.022 [DOI] [Google Scholar]
- 143.Kalkhoran AHZ, Naghib SM, Vahidi O, Rahmanian M. Synthesis and characterization of graphene-grafted gelatin nanocomposite hydrogels as emerging drug delivery systems. Biomed Phys Eng Express. 2018;4:055017. doi: 10.1088/2057-1976/aad745 [DOI] [Google Scholar]
- 144.Ma N, Liu J, He W, et al. Folic acid-grafted bovine serum albumin decorated graphene oxide: an efficient drug carrier for targeted cancer therapy. J Colloid Interface Sci. 2017;490:598–607. doi: 10.1016/j.jcis.2016.11.097 [DOI] [PubMed] [Google Scholar]
- 145.Wan Y, Lin Z, Zhang Q, et al. Incorporating graphene oxide into biomimetic nano-microfibrous cellulose scaffolds for enhanced breast cancer cell behavior. Cellulose. 2020:1–15. [Google Scholar]
- 146.Khoshoei A, Ghasemy E, Poustchi F, Shahbazi M-A, Maleki R. Engineering the pH-sensitivity of the graphene and carbon nanotube based nanomedicines in smart cancer therapy by grafting trimetyl Chitosan. Pharm Res. 2020;37:1–13. doi: 10.1007/s11095-020-02881-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Abbasian M, Roudi -M-M, Mahmoodzadeh F, Eskandani M, Jaymand M. Chitosan-grafted-poly (methacrylic acid)/graphene oxide nanocomposite as a pH-responsive de novo cancer chemotherapy nanosystem. Int J Biol Macromol. 2018;118:1871–1879. doi: 10.1016/j.ijbiomac.2018.07.036 [DOI] [PubMed] [Google Scholar]
- 148.Gooneh-Farahani S, Naghib SM, Naimi-Jamal MR. A critical comparison study on the pH-sensitive nanocomposites based on graphene-grafted chitosan for cancer theragnosis. Multidiscip Cancer Invest. 2019;3:5–16. doi: 10.30699/acadpub.mci.3.1.5 [DOI] [Google Scholar]
- 149.Dhanavel S, Revathy T, Sivaranjani T, et al. 5-Fluorouracil and curcumin co-encapsulated chitosan/reduced graphene oxide nanocomposites against human colon cancer cell lines. Polym Bull. 2020;77:213–233. doi: 10.1007/s00289-019-02734-x [DOI] [Google Scholar]
- 150.Zhao X, Wei Z, Zhao Z, et al. Design and development of graphene oxide nanoparticle/chitosan hybrids showing pH-sensitive surface charge-reversible ability for efficient intracellular doxorubicin delivery. ACS Appl Mater Interfaces. 2018;10:6608–6617. doi: 10.1021/acsami.7b16910 [DOI] [PubMed] [Google Scholar]
- 151.Yang H, Bremner DH, Tao L, Li H, Hu J, Zhu L. Carboxymethyl chitosan-mediated synthesis of hyaluronic acid-targeted graphene oxide for cancer drug delivery. Carbohydr Polym. 2016;135:72–78. doi: 10.1016/j.carbpol.2015.08.058 [DOI] [PubMed] [Google Scholar]
- 152.Xie M, Zhang F, Liu L, et al. Surface modification of graphene oxide nanosheets by protamine sulfate/sodium alginate for anti-cancer drug delivery application. Appl Surf Sci. 2018;440:853–860. doi: 10.1016/j.apsusc.2018.01.175 [DOI] [Google Scholar]
- 153.Sattari S, Tehrani AD, Adeli M, Soleimani K, Rashidipour M. Fabrication of new generation of co-delivery systems based on graphene-g-cyclodextrin/chitosan nanofiber. Int J Biol Macromol. 2020;156:1126–1134. doi: 10.1016/j.ijbiomac.2019.11.144 [DOI] [PubMed] [Google Scholar]
- 154.Wang C, Li B, Niu W, et al. β-Cyclodextrin modified graphene oxide–magnetic nanocomposite for targeted delivery and pH-sensitive release of stereoisomeric anti-cancer drugs. RSC Adv. 2015;5:89299–89308. doi: 10.1039/C5RA13082D [DOI] [Google Scholar]
- 155.Xie M, Zhang F, Peng H, et al. Layer-by-layer modification of magnetic graphene oxide by chitosan and sodium alginate with enhanced dispersibility for targeted drug delivery and photothermal therapy. Colloids Surf B Biointerfaces. 2019;176:462–470. doi: 10.1016/j.colsurfb.2019.01.028 [DOI] [PubMed] [Google Scholar]
- 156.Zhang F, Xie M, Zhao Y, et al. Chitosan and dextran stabilized GO-iron oxide nanosheets with high dispersibility for chemotherapy and photothermal ablation. Ceram Int. 2019;45:5996–6003. doi: 10.1016/j.ceramint.2018.12.070 [DOI] [Google Scholar]
- 157.Xie M, Lei H, Zhang Y, et al. Non-covalent modification of graphene oxide nanocomposites with chitosan/dextran and its application in drug delivery. RSC Adv. 2016;6:9328–9337. doi: 10.1039/C5RA23823D [DOI] [Google Scholar]
- 158.Samadi S, Moradkhani M, Beheshti H, Irani M, Aliabadi M. Fabrication of chitosan/poly (lactic acid)/graphene oxide/TiO2 composite nanofibrous scaffolds for sustained delivery of doxorubicin and treatment of lung cancer. Int J Biol Macromol. 2018;110:416–424. doi: 10.1016/j.ijbiomac.2017.08.048 [DOI] [PubMed] [Google Scholar]
- 159.Lei H, Xie M, Zhao Y, Zhang F, Xu Y, Xie J. Chitosan/sodium alginate modificated graphene oxide-based nanocomposite as a carrier for drug delivery. Ceram Int. 2016;42:17798–17805. doi: 10.1016/j.ceramint.2016.08.108 [DOI] [Google Scholar]
- 160.Guo Y, Xu H, Li Y, et al. Hyaluronic acid and Arg-Gly-Asp peptide modified graphene oxide with dual receptor-targeting function for cancer therapy. J Biomater Appl. 2017;32:54–65. doi: 10.1177/0885328217712110 [DOI] [PubMed] [Google Scholar]
- 161.Yin T, Liu J, Zhao Z, et al. Redox sensitive hyaluronic acid‐decorated graphene oxide for photothermally controlled tumor‐cytoplasm‐selective rapid drug delivery. Adv Funct Mater. 2017;27:1604620. doi: 10.1002/adfm.201604620 [DOI] [Google Scholar]
- 162.Kim JH, Moon MJ, Kim DY, Heo SH, Jeong YY. Hyaluronic acid-based nanomaterials for cancer therapy. Polymers. 2018;10:1133. doi: 10.3390/polym10101133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kim K, Choi H, Choi ES, Park M-H, Ryu J-H. Hyaluronic acid-coated nanomedicine for targeted cancer therapy. Pharmaceutics. 2019;11:301. doi: 10.3390/pharmaceutics11070301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Wickens JM, Alsaab HO, Kesharwani P, et al. Recent advances in hyaluronic acid-decorated nanocarriers for targeted cancer therapy. Drug Discov Today. 2017;22:665–680. doi: 10.1016/j.drudis.2016.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Tan KH, Sattari S, Donskyi IS, et al. Functionalized 2D nanomaterials with switchable binding to investigate graphene–bacteria interactions. Nanoscale. 2018;10:9525–9537. doi: 10.1039/C8NR01347K [DOI] [PubMed] [Google Scholar]
- 166.Tu Z, Achazi K, Schulz A, et al. Combination of surface charge and size controls the cellular uptake of functionalized graphene sheets. Adv Funct Mater. 2017;27:1701837. doi: 10.1002/adfm.201701837 [DOI] [Google Scholar]
- 167.Movahedi S, Adeli M, Fard AK, Maleki M, Sadeghizadeh M, Bani F. Edge-functionalization of graphene by polyglycerol; A way to change its flat topology. Polymer. 2013;54:2917–2925. doi: 10.1016/j.polymer.2013.04.014 [DOI] [Google Scholar]
- 168.Sun X, Liu Z, Welsher K, et al. Nano-graphene oxide for cellular imaging and drug delivery. Nano Res. 2008;1:203–212. doi: 10.1007/s12274-008-8021-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Hussien NA, Işıklan N, Türk M. Aptamer-functionalized magnetic graphene oxide nanocarrier for targeted drug delivery of paclitaxel. Mater Chem Phys. 2018;211:479–488. doi: 10.1016/j.matchemphys.2018.03.015 [DOI] [Google Scholar]
- 170.Oz Y, Barras A, Sanyal R, Boukherroub R, Szunerits S, Sanyal A. Functionalization of reduced graphene oxide via thiol–maleimide “click” chemistry: facile fabrication of targeted drug delivery vehicles. ACS Appl Mater Interfaces. 2017;9:34194–34203. doi: 10.1021/acsami.7b08433 [DOI] [PubMed] [Google Scholar]
- 171.Masoudipour E, Kashanian S, Maleki N. A targeted drug delivery system based on dopamine functionalized nano graphene oxide. Chem Phys Lett. 2017;668:56–63. doi: 10.1016/j.cplett.2016.12.019 [DOI] [Google Scholar]
- 172.Song -M-M, Xu H-L, Liang J-X, Xiang -H-H, Liu R, Shen Y-X. Lactoferrin modified graphene oxide iron oxide nanocomposite for glioma-targeted drug delivery. Mater Sci Eng C. 2017;77:904–911. doi: 10.1016/j.msec.2017.03.309 [DOI] [PubMed] [Google Scholar]
- 173.Mauro N, Scialabba C, Agnello S, Cavallaro G, Giammona G. Folic acid-functionalized graphene oxide nanosheets via plasma etching as a platform to combine NIR anticancer phototherapy and targeted drug delivery. Mater Sci Eng C. 2020;107:110201. doi: 10.1016/j.msec.2019.110201 [DOI] [PubMed] [Google Scholar]
- 174.Wang F, Xiao J, Chen S, et al. Polymer vesicles: modular platforms for cancer theranostics. Adv Mater. 2018;30:1705674. doi: 10.1002/adma.201705674 [DOI] [PubMed] [Google Scholar]
- 175.Gu Z, Zhu S, Yan L, Zhao F, Zhao Y. Graphene‐based smart platforms for combined Cancer therapy. Adv Mater. 2019;31:1800662. doi: 10.1002/adma.201800662 [DOI] [PubMed] [Google Scholar]
- 176.Ye M, Zhang Z, Zhao Y, Qu L. Graphene platforms for smart energy generation and storage. Joule. 2018;2:245–268. doi: 10.1016/j.joule.2017.11.011 [DOI] [Google Scholar]
- 177.Yang K, Feng L, Liu Z. Stimuli responsive drug delivery systems based on nano-graphene for cancer therapy. Adv Drug Deliv Rev. 2016;105:228–241. doi: 10.1016/j.addr.2016.05.015 [DOI] [PubMed] [Google Scholar]
- 178.Yu X, Cheng H, Zhang M, Zhao Y, Qu L, Shi G. Graphene-based smart materials. Nat Rev Mater. 2017;2:1–13. doi: 10.1038/natrevmats.2017.46 [DOI] [Google Scholar]
- 179.Sattari S, Dadkhah Tehrani A, Adeli M. pH-responsive hybrid hydrogels as antibacterial and drug delivery systems. Polymers. 2018;10:660. doi: 10.3390/polym10060660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.He X, Li J, An S, Jiang C. pH-sensitive drug-delivery systems for tumor targeting. Ther Deliv. 2013;4:1499–1510. doi: 10.4155/tde.13.120 [DOI] [PubMed] [Google Scholar]
- 181.Kavitha T, Abdi SIH, Park S-Y. pH-sensitive nanocargo based on smart polymer functionalized graphene oxide for site-specific drug delivery. Phys Chem Chem Phys. 2013;15:5176–5185. doi: 10.1039/c3cp00008g [DOI] [PubMed] [Google Scholar]
- 182.Liu J, Huang Y, Kumar A, et al. pH-sensitive nano-systems for drug delivery in cancer therapy. Biotechnol Adv. 2014;32:693–710. doi: 10.1016/j.biotechadv.2013.11.009 [DOI] [PubMed] [Google Scholar]
- 183.Li L, Sun W, Zhong J, et al. Multistage nanovehicle delivery system based on stepwise size reduction and charge reversal for programmed nuclear targeting of systemically administered anticancer drugs. Adv Funct Mater. 2015;25:4101–4113. doi: 10.1002/adfm.201501248 [DOI] [Google Scholar]
- 184.Han SS, Li ZY, Zhu JY, et al. Dual‐pH sensitive charge‐reversal polypeptide micelles for tumor‐triggered targeting uptake and nuclear drug delivery. Small. 2015;11:2543–2554. doi: 10.1002/smll.201402865 [DOI] [PubMed] [Google Scholar]
- 185.Zhou Z, Shen Y, Tang J, et al. Charge‐reversal drug conjugate for targeted cancer cell nuclear drug delivery. Adv Funct Mater. 2009;19:3580–3589. doi: 10.1002/adfm.200900825 [DOI] [Google Scholar]
- 186.Ballatori N, Krance SM, Notenboom S, Shi S, Tieu K, Hammond CL. Glutathione dysregulation and the etiology and progression of human diseases. Biol Chem. 2009;390:191–214. doi: 10.1515/BC.2009.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Dringen R. Metabolism and functions of glutathione in brain. Prog Neurobiol. 2000;62:649–671. [DOI] [PubMed] [Google Scholar]
- 188.Ma N, Song A, Li Z, Luan Y. Redox-sensitive prodrug molecules meet graphene oxide: an efficient graphene oxide-based nanovehicle toward cancer therapy. ACS Biomater Sci Eng. 2019;5:1384–1391. doi: 10.1021/acsbiomaterials.9b00114 [DOI] [PubMed] [Google Scholar]
- 189.Yao J, Feng J, Chen J. External-stimuli responsive systems for cancer theranostic. Asian J Pharm Sci. 2016;11:585–595. doi: 10.1016/j.ajps.2016.06.001 [DOI] [Google Scholar]
- 190.Moradi M. Design and Evaluation of a GUI for Signal and Data Analysis of Mobile Functional Near-Infrared Spectroscopy Systems. Wichita State University; 2020. [Google Scholar]
- 191.Yang H, Zhang Y, Chen S, Hao R. Micro-optical components for bioimaging on tissues, cells and subcellular structures. Micromachines. 2019;10:405. doi: 10.3390/mi10060405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Sreejith S, Huong TTM, Borah P, Zhao Y. Organic–inorganic nanohybrids for fluorescence, photoacoustic and Raman bioimaging. Sci Bull. 2015;60:665–678. doi: 10.1007/s11434-015-0765-4 [DOI] [Google Scholar]
- 193.Pei Y, Wei M-Y. Newly-engineered materials for bio-imaging technology: a focus on the hybrid system of ultrasound and fluorescence. Front Bioeng Biotechnol. 2019;7:88. doi: 10.3389/fbioe.2019.00088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Han Z, Porter AE. In situ electron microscopy of complex biological and nanoscale systems: challenges and opportunities. Front Nanotechnol. 2020;2:20. doi: 10.3389/fnano.2020.606253 [DOI] [Google Scholar]
- 195.Zhu X, Liu Y, Li P, Nie Z, Li J. Applications of graphene and its derivatives in intracellular biosensing and bioimaging. Analyst. 2016;141:4541–4553. doi: 10.1039/C6AN01090C [DOI] [PubMed] [Google Scholar]
- 196.Godin AG, Setaro A, Gandil M, et al. Photoswitchable single-walled carbon nanotubes for super-resolution microscopy in the near-infrared. Sci Adv. 2019;5:eaax1166. doi: 10.1126/sciadv.aax1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Gao X, Cheng L, Jiang W, Li X-K, Xing F. Graphene and its derivatives-based optical sensors. Front Chem. 2021;9:5. doi: 10.3389/fchem.2021.615164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Tomita S, Ishihara S, Kurita R. A multi-fluorescent DNA/graphene oxide conjugate sensor for signature-based protein discrimination. Sensors. 2017;17:2194. doi: 10.3390/s17102194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Nurunnabi M, Khatun Z, Reeck GR, Lee DY, Lee Y-K. Photoluminescent graphene nanoparticles for cancer phototherapy and imaging. ACS Appl Mater Interfaces. 2014;6:12413–12421. doi: 10.1021/am504071z [DOI] [PubMed] [Google Scholar]
- 200.Zheng P, Wu N. Fluorescence and sensing applications of graphene oxide and graphene quantum dots: a review. Chem Asian J. 2017;12:2343–2353. doi: 10.1002/asia.201700814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Treossi E, Melucci M, Liscio A, Gazzano M, Samorì P, Palermo V. High-contrast visualization of graphene oxide on dye-sensitized glass, quartz, and silicon by fluorescence quenching. J Am Chem Soc. 2009;131:15576–15577. doi: 10.1021/ja9055382 [DOI] [PubMed] [Google Scholar]
- 202.Wang Y, Kurunthu D, Scott GW, Bardeen CJ. Fluorescence quenching in conjugated polymers blended with reduced graphitic oxide. J Phys Chem C. 2010;114:4153–4159. doi: 10.1021/jp9097793 [DOI] [Google Scholar]
- 203.Alava T, Mann JA, Théodore C, et al. Control of the graphene–protein interface is required to preserve adsorbed protein function. Anal Chem. 2013;85:2754–2759. doi: 10.1021/ac303268z [DOI] [PubMed] [Google Scholar]
- 204.Gollavelli G, Ling Y-C. Multi-functional graphene as an in vitro and in vivo imaging probe. Biomaterials. 2012;33:2532–2545. doi: 10.1016/j.biomaterials.2011.12.010 [DOI] [PubMed] [Google Scholar]
- 205.Younis MR, He G, Lin J, Huang P. Recent advances on graphene quantum dots for bioimaging applications. Front Chem. 2020;8. doi: 10.3389/fchem.2020.00424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Bellet P, Gasparotto M, Pressi S, et al. Graphene-based scaffolds for regenerative medicine. Nanomaterials. 2021;11:404. doi: 10.3390/nano11020404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Liu Z, Guo Z, Zhong H, Qin X, Wan M, Yang B. Graphene oxide based surface-enhanced Raman scattering probes for cancer cell imaging. Phys Chem Chem Phys. 2013;15:2961–2966. doi: 10.1039/c2cp43715e [DOI] [PubMed] [Google Scholar]
- 208.Dong H, Dai W, Ju H, et al. Multifunctional poly (l-lactide)–polyethylene glycol-grafted graphene quantum dots for intracellular microRNA imaging and combined specific-gene-targeting agents delivery for improved therapeutics. ACS Appl Mater Interfaces. 2015;7:11015–11023. doi: 10.1021/acsami.5b02803 [DOI] [PubMed] [Google Scholar]
- 209.de Melo-diogo D, Lima-Sousa R, Alves CG, Correia IJ. Graphene family nanomaterials for application in cancer combination photothermal therapy. Biomater Sci. 2019;7:3534–3551. doi: 10.1039/C9BM00577C [DOI] [PubMed] [Google Scholar]
- 210.Palmieri V, Spirito MD, Papi M. Graphene-based scaffolds for tissue engineering and photothermal therapy. Nanomedicine. 2020;15:1411–1417. doi: 10.2217/nnm-2020-0050 [DOI] [PubMed] [Google Scholar]
- 211.Li Z, Lei H, Kan A, Xie H, Yu W. Photothermal applications based on graphene and its derivatives: a state-of-the-art review. Energy. 2020:119262. [Google Scholar]
- 212.Chen Y-W, Su Y-L, Hu S-H, Chen S-Y. Functionalized graphene nanocomposites for enhancing photothermal therapy in tumor treatment. Adv Drug Deliv Rev. 2016;105:190–204. doi: 10.1016/j.addr.2016.05.022 [DOI] [PubMed] [Google Scholar]
- 213.Guday G, Nickl P, Adeli M, Haag R. Reversible photothermal homogenization of fluorous biphasic systems with perfluoroalkylated nanographene. ACS Appl Nano Mater. 2020;3:1139–1146. doi: 10.1021/acsanm.9b01611 [DOI] [Google Scholar]
- 214.Bani F, Adeli M, Movahedi S, Sadeghizadeh M. Graphene–polyglycerol–curcumin hybrid as a near-infrared (NIR) laser stimuli-responsive system for chemo-photothermal cancer therapy. RSC Adv. 2016;6:61141–61149. doi: 10.1039/C6RA05917A [DOI] [Google Scholar]
- 215.Cheon YA, Bae JH, Chung BG. Reduced graphene oxide nanosheet for chemo-photothermal therapy. Langmuir. 2016;32:2731–2736. doi: 10.1021/acs.langmuir.6b00315 [DOI] [PubMed] [Google Scholar]
- 216.Wang Y, Zhang H, Xie J, Liu Y, Wang S, Zhao Q. Three dimensional mesoporous carbon nanospheres as carriers for chemo-photothermal therapy compared with two dimensional graphene oxide nanosheets. Colloids Surf A Physicochem Eng Asp. 2020;590:124498. doi: 10.1016/j.colsurfa.2020.124498 [DOI] [Google Scholar]
- 217.Jun SW, Manivasagan P, Kwon J, et al. Folic acid–conjugated chitosan-functionalized graphene oxide for highly efficient photoacoustic imaging-guided tumor-targeted photothermal therapy. Int J Biol Macromol. 2020;155:961–971. doi: 10.1016/j.ijbiomac.2019.11.055 [DOI] [PubMed] [Google Scholar]
- 218.Wang L, Wang M, Zhou B, et al. PEGylated reduced-graphene oxide hybridized with Fe 3 O 4 nanoparticles for cancer photothermal-immunotherapy. J Mater Chem B. 2019;7:7406–7414. doi: 10.1039/C9TB00630C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Lu D, Tao R, Wang Z. Carbon-based materials for photodynamic therapy: a mini-review. Front Chem Sci Eng. 2019;13:310–323. doi: 10.1007/s11705-018-1750-7 [DOI] [Google Scholar]
- 220.Rizwan M, Rasheed T, Raza A, et al. Photodynamic-based therapeutic modalities to fight against cancer–A review from synergistic viewpoint. J Drug Deliv Sci Technol. 2019;51:70–82. doi: 10.1016/j.jddst.2019.02.014 [DOI] [Google Scholar]
- 221.Hu Z, Wang C, Zhao F, et al. Fabrication of a graphene/C 60 nanohybrid via γ-cyclodextrin host–guest chemistry for photodynamic and photothermal therapy. Nanoscale. 2017;9:8825–8833. doi: 10.1039/C7NR02922E [DOI] [PubMed] [Google Scholar]
- 222.Liu J, Liu K, Feng L, Liu Z, Xu L. Comparison of nanomedicine-based chemotherapy, photodynamic therapy and photothermal therapy using reduced graphene oxide for the model system. Biomater Sci. 2017;5:331–340. doi: 10.1039/C6BM00526H [DOI] [PubMed] [Google Scholar]
- 223.Sun X, Zebibula A, Dong X, et al. Aggregation-induced emission nanoparticles encapsulated with PEGylated nano graphene oxide and their applications in two-photon fluorescence bioimaging and photodynamic therapy in vitro and in vivo. ACS Appl Mater Interfaces. 2018;10:25037–25046. doi: 10.1021/acsami.8b05546 [DOI] [PubMed] [Google Scholar]
- 224.Huang X, Chen J, Wu W, et al. Delivery of MutT homolog 1 inhibitor by functionalized graphene oxide nanoparticles for enhanced chemo-photodynamic therapy triggers cell death in osteosarcoma. Acta Biomater. 2020;109:229–243. doi: 10.1016/j.actbio.2020.04.009 [DOI] [PubMed] [Google Scholar]
- 225.Ahirwar S, Mallick S, Bahadur D. Photodynamic therapy using graphene quantum dot derivatives. J Solid State Chem. 2020;282:121107. doi: 10.1016/j.jssc.2019.121107 [DOI] [Google Scholar]
- 226.Goswami R, Subramanian G, Silayeva L, et al. Gene therapy leaves a vicious cycle. Front Oncol. 2019;9:297. doi: 10.3389/fonc.2019.00297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Kamimura K, Suda T, Zhang G, Liu D. Advances in gene delivery systems. Pharmaceut Med. 2011;25:293–306. doi: 10.1007/BF03256872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Ramamoorth M, Narvekar A. Non viral vectors in gene therapy-an overview. J Clin Diag Res. 2015;9:GE01. doi: 10.7860/JCDR/2015/10443.5394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Mogler MA, Kamrud KI. RNA-based viral vectors. Expert Rev Vaccines. 2015;14:283–312. [DOI] [PubMed] [Google Scholar]
- 230.Hemminki O, Hemminki A. A century of oncolysis evolves into oncolytic immunotherapy. Oncoimmunology. 2016;5:e1074377. doi: 10.1080/2162402X.2015.1074377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Ledford H. Cancer-fighting viruses win approval. Nat News. 2015;526:622. doi: 10.1038/526622a [DOI] [PubMed] [Google Scholar]
- 232.Kang Z, Meng Q, Liu K. Peptide-based gene delivery vectors. J Mater Chem B. 2019;7:1824–1841. [DOI] [PubMed] [Google Scholar]
- 233.Dehshahri A, Sadeghpour H, Oskuee RK, et al. Interleukin-12 plasmid DNA delivery using l-thyroxine-conjugated polyethylenimine nanocarriers. J Nanoparticle Res. 2014;16:1–14. doi: 10.1007/s11051-014-2423-1 [DOI] [Google Scholar]
- 234.Bono N, Ponti F, Mantovani D, Candiani G. Non-viral in vitro gene delivery: it is now time to set the bar! Pharmaceutics. 2020;12:183. doi: 10.3390/pharmaceutics12020183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Meacham JM, Durvasula K, Degertekin FL, Fedorov AG. Physical methods for intracellular delivery: practical aspects from laboratory use to industrial-scale processing. J Lab Autom. 2014;19:1–18. doi: 10.1177/2211068213494388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Liu C, Zhang L, Zhu W, et al. Barriers and strategies of cationic liposomes for cancer gene therapy. Mol Ther Methods Clin Dev. 2020;18:751–764. doi: 10.1016/j.omtm.2020.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Dharmalingam P, Rachamalla HKR, Lohchania B, et al. Green transfection: cationic lipid nanocarrier system derivatized from vegetable fat, palm stearin enhances nucleic acid transfections. ACS Omega. 2017;2:7892–7903. doi: 10.1021/acsomega.7b00935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Taylor RE, Zahid M. Cell penetrating peptides, novel vectors for gene therapy. Pharmaceutics. 2020;12:225. doi: 10.3390/pharmaceutics12030225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Zavradashvili N, Sarisozen C, Titvinidze G, et al. Library of cationic polymers composed of polyamines and arginine as gene transfection agents. ACS Omega. 2019;4:2090–2101. doi: 10.1021/acsomega.8b02977 [DOI] [Google Scholar]
- 240.Van Bruggen C, Hexum JK, Tan Z, Dalal RJ, Reineke TM. Nonviral gene delivery with cationic glycopolymers. Acc Chem Res. 2019;52:1347–1358. doi: 10.1021/acs.accounts.8b00665 [DOI] [PubMed] [Google Scholar]
- 241.Zakeri A, Kouhbanani MAJ, Beheshtkhoo N, et al. Polyethylenimine-based nanocarriers in co-delivery of drug and gene: a developing horizon. Nano Rev Exp. 2018;9:1488497. doi: 10.1080/20022727.2018.1488497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Jiang C, Qi Z, Jia H, et al. ATP-responsive low-molecular-weight polyethylenimine-based supramolecular assembly via host–guest interaction for gene delivery. Biomacromolecules. 2018;20:478–489. doi: 10.1021/acs.biomac.8b01395 [DOI] [PubMed] [Google Scholar]
- 243.Vincent M, De Lázaro I, Kostarelos K. Graphene materials as 2D non-viral gene transfer vector platforms. Gene Ther. 2017;24:123–132. doi: 10.1038/gt.2016.79 [DOI] [PubMed] [Google Scholar]
- 244.Gong X, Liu G, Li Y, Yu DYW, Teoh WY. Functionalized-graphene composites: fabrication and applications in sustainable energy and environment. Chem Mater. 2016;28:8082–8118. doi: 10.1021/acs.chemmater.6b01447 [DOI] [Google Scholar]
- 245.Mukherjee S, Bytesnikova Z, Ashrafi A, Adam V, Richtera L. Graphene oxide as a nanocarrier for biochemical molecules: current understanding and trends. Processes. 2020;8:1636. doi: 10.3390/pr8121636 [DOI] [Google Scholar]
- 246.Mugnano M, Lama G, Castaldo R, et al. Cellular uptake of mildly oxidized nanographene for drug-delivery applications. ACS Appl Nano Mater. 2019;3:428–439. doi: 10.1021/acsanm.9b02035 [DOI] [Google Scholar]
- 247.Hoseini-Ghahfarokhi M, Mirkiani S, Mozaffari N, et al. Applications of graphene and graphene oxide in smart drug/gene delivery: is the world still flat? Int J Nanomedicine. 2020;15:9469. doi: 10.2147/IJN.S265876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Imani R, Mohabatpour F, Mostafavi F. Graphene-based nano-carrier modifications for gene delivery applications. Carbon. 2018;140:569–591. doi: 10.1016/j.carbon.2018.09.019 [DOI] [Google Scholar]
- 249.Dou C, Ding N, Luo F, et al. Graphene‐based microRNA transfection blocks preosteoclast fusion to increase bone formation and vascularization. Adv Sci. 2018;5:1700578. doi: 10.1002/advs.201700578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Kim H, Namgung R, Singha K, Oh I-K, Kim WJ. Graphene oxide–polyethylenimine nanoconstruct as a gene delivery vector and bioimaging tool. Bioconjug Chem. 2011;22:2558–2567. doi: 10.1021/bc200397j [DOI] [PubMed] [Google Scholar]
- 251.Yin F, Hu K, Chen Y, et al. SiRNA delivery with PEGylated graphene oxide nanosheets for combined photothermal and genetherapy for pancreatic cancer. Theranostics. 2017;7:1133. doi: 10.7150/thno.17841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Sun Y, Ye X, Cai M, et al. Osteoblast-targeting-peptide modified nanoparticle for siRNA/microRNA delivery. ACS Nano. 2016;10:5759–5768. doi: 10.1021/acsnano.5b07828 [DOI] [PubMed] [Google Scholar]
- 253.Paul A, Hasan A, Kindi HA, et al. Injectable graphene oxide/hydrogel-based angiogenic gene delivery system for vasculogenesis and cardiac repair. ACS Nano. 2014;8:8050–8062. doi: 10.1021/nn5020787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Zhi F, Dong H, Jia X, et al. Functionalized graphene oxide mediated adriamycin delivery and miR-21 gene silencing to overcome tumor multidrug resistance in vitro. PLoS One. 2013;8:e60034. doi: 10.1371/journal.pone.0060034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Zhang H, Yan T, Xu S, et al. Graphene oxide-chitosan nanocomposites for intracellular delivery of immunostimulatory CpG oligodeoxynucleotides. Mater Sci Eng C. 2017;73:144–151. doi: 10.1016/j.msec.2016.12.072 [DOI] [PubMed] [Google Scholar]
- 256.Dowaidar M, Abdelhamid HN, Hällbrink M, Zou X, Langel Ü. Graphene oxide nanosheets in complex with cell penetrating peptides for oligonucleotides delivery. Biochim Biophys Acta Gen Subj. 2017;1861:2334–2341. doi: 10.1016/j.bbagen.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 257.Yang M, Liu Y, Fan T, Zhang D. Metal-graphene interfaces in epitaxial and bulk systems: a review. Prog Mater Sci. 2020;110:100652. [Google Scholar]
- 258.Cusati T, Fiori G, Gahoi A, et al. Electrical properties of graphene-metal contacts. Sci Rep. 2017;7:1–11. doi: 10.1038/s41598-017-05069-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Bai S, Shen X. Graphene–inorganic nanocomposites. RSC Adv. 2012;2:64–98. [Google Scholar]
- 260.Al-Ani LA, AlSaadi MA, Kadir FA, Hashim NM, Julkapli NM, Yehye WA. Graphene–gold based nanocomposites applications in cancer diseases; Efficient detection and therapeutic tools. Eur J Med Chem. 2017;139:349–366. [DOI] [PubMed] [Google Scholar]
- 261.Assali A, Razzazan S, Akhavan O, Mottaghitalab F, Adeli M, Atyabi F. The bio-interface between functionalized Au NR@ GO nanoplatforms with protein corona and their impact on delivery and release system. Colloids Surf B Biointerfaces. 2019;173:891–898. doi: 10.1016/j.colsurfb.2018.10.042 [DOI] [PubMed] [Google Scholar]
- 262.Assali A, Akhavan O, Adeli M, et al. Multifunctional core-shell nanoplatforms (gold@ graphene oxide) with mediated NIR thermal therapy to promote miRNA delivery. Nanomedicine. 2018;14:1891–1903. doi: 10.1016/j.nano.2018.05.016 [DOI] [PubMed] [Google Scholar]
- 263.Huang J, Zhang L, Chen B, et al. Nanocomposites of size-controlled gold nanoparticles and graphene oxide: formation and applications in SERS and catalysis. Nanoscale. 2010;2:2733–2738. doi: 10.1039/c0nr00473a [DOI] [PubMed] [Google Scholar]
- 264.Pham TA, Choi BC, Lim KT, Jeong YT. A simple approach for immobilization of gold nanoparticles on graphene oxide sheets by covalent bonding. Appl Surf Sci. 2011;257:3350–3357. doi: 10.1016/j.apsusc.2010.11.023 [DOI] [Google Scholar]
- 265.Sangili A, Kalyani T, Chen S-M, Nanda A, Jana SK. Label-free electrochemical immunosensor based on one-step electrochemical deposition of AuNP-RGO nanocomposites for detection of endometriosis marker CA 125. ACS Applied Bio Mater. 2020;3:7620–7630. doi: 10.1021/acsabm.0c00821 [DOI] [PubMed] [Google Scholar]
- 266.Zhang X, Li F, Wei Q, Du B, Wu D, Li H. Ultrasensitive nonenzymatic immunosensor based on bimetallic gold–silver nanoclusters synthesized by simple mortar grinding route. Sens Actuators B Chem. 2014;194:64–70. doi: 10.1016/j.snb.2013.12.065 [DOI] [Google Scholar]
- 267.Chen H, Tang D, Zhang B, Liu B, Cui Y, Chen G. Electrochemical immunosensor for carcinoembryonic antigen based on nanosilver-coated magnetic beads and gold-graphene nanolabels. Talanta. 2012;91:95–102. doi: 10.1016/j.talanta.2012.01.025 [DOI] [PubMed] [Google Scholar]
- 268.Fan Y, Shi S, Ma J, Guo Y. A paper-based electrochemical immunosensor with reduced graphene oxide/thionine/gold nanoparticles nanocomposites modification for the detection of cancer antigen 125. Biosens Bioelectron. 2019;135:1–7. doi: 10.1016/j.bios.2019.03.063 [DOI] [PubMed] [Google Scholar]
- 269.Ye Y, Yan W, Liu Y, et al. Electrochemical detection of Salmonella using an invA genosensor on polypyrrole-reduced graphene oxide modified glassy carbon electrode and AuNPs-horseradish peroxidase-streptavidin as nanotag. Anal Chim Acta. 2019;1074:80–88. doi: 10.1016/j.aca.2019.05.012 [DOI] [PubMed] [Google Scholar]
- 270.Shamsipur M, Samandari L, Farzin L, Molaabasi F, Mousazadeh MH. Dual-modal label-free genosensor based on hemoglobin@ gold nanocluster stabilized graphene nanosheets for the electrochemical detection of BCR/ABL fusion gene. Talanta. 2020;217:121093. doi: 10.1016/j.talanta.2020.121093 [DOI] [PubMed] [Google Scholar]
- 271.Mobed A, Hasanzadeh M, Shadjou N, Hassanpour S, Saadati A, Agazadeh M. Immobilization of ssDNA on the surface of silver nanoparticles-graphene quantum dots modified by gold nanoparticles towards biosensing of microorganism. Microchem J. 2020;152:104286. doi: 10.1016/j.microc.2019.104286 [DOI] [Google Scholar]
- 272.Wang Z, Sun X, Huang T, Song J, Wang Y. A sandwich nanostructure of gold nanoparticle coated reduced graphene oxide for photoacoustic imaging-guided photothermal therapy in the second NIR window. Front Bioeng Biotechnol. 2020;8:655. doi: 10.3389/fbioe.2020.00655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Cheng Y, Chang Y, Feng Y, et al. Simulated sunlight‐mediated photodynamic therapy for melanoma skin cancer by titanium‐dioxide‐nanoparticle–gold‐nanocluster–graphene heterogeneous nanocomposites. Small. 2017;13:1603935. doi: 10.1002/smll.201603935 [DOI] [PubMed] [Google Scholar]
- 274.Lin C-W, Wei K-C, Liao S-S, et al. A reusable magnetic graphene oxide-modified biosensor for vascular endothelial growth factor detection in cancer diagnosis. Biosens Bioelectron. 2015;67:431–437. doi: 10.1016/j.bios.2014.08.080 [DOI] [PubMed] [Google Scholar]
- 275.Huang Y-S, Lu Y-J, Chen J-P. Magnetic graphene oxide as a carrier for targeted delivery of chemotherapy drugs in cancer therapy. J Magn Magn Mater. 2017;427:34–40. doi: 10.1016/j.jmmm.2016.10.042 [DOI] [Google Scholar]
- 276.Gonzalez-Rodriguez R, Campbell E, Naumov A. Multifunctional graphene oxide/iron oxide nanoparticles for magnetic targeted drug delivery dual magnetic resonance/fluorescence imaging and cancer sensing. PLoS One. 2019;14:e0217072. doi: 10.1371/journal.pone.0217072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Li Y, Dong H, Tao Q, et al. Enhancing the magnetic relaxivity of MRI contrast agents via the localized superacid microenvironment of graphene quantum dots. Biomaterials. 2020;250:120056. doi: 10.1016/j.biomaterials.2020.120056 [DOI] [PubMed] [Google Scholar]
- 278.Meng J, Chen X, Tian Y, Li Z, Zheng Q. Nanoscale metal–organic frameworks decorated with graphene oxide for magnetic resonance imaging guided photothermal therapy. Chem Eur J. 2017;23:17521–17530. doi: 10.1002/chem.201702573 [DOI] [PubMed] [Google Scholar]
- 279.Liu H, Li C, Qian Y, et al. Magnetic-induced graphene quantum dots for imaging-guided photothermal therapy in the second near-infrared window. Biomaterials. 2020;232:119700. doi: 10.1016/j.biomaterials.2019.119700 [DOI] [PubMed] [Google Scholar]
- 280.Han S, Teng F, Wang Y, Su L, Leng Q, Jiang H. Drug-loaded dual targeting graphene oxide-based molecularly imprinted composite and recognition of carcino-embryonic antigen. RSC Adv. 2020;10:10980–10988. doi: 10.1039/D0RA00574F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Liang W, Huang Y, Lu D, et al. β-cyclodextrin–hyaluronic acid polymer functionalized magnetic graphene oxide nanocomposites for targeted photo-chemotherapy of tumor cells. Polymers. 2019;11:133. doi: 10.3390/polym11010133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Hatamie S, Shih P-J, Zomorod MS, Heravi P, Ahadian MM, Hatami N. Hyperthermia response of PEGylated magnetic graphene nanocomposites for heating applications and accelerate antibacterial activity using magnetic fluid hyperthermia. Appl Phys A. 2020;126:1–10. doi: 10.1007/s00339-020-3454-3 [DOI] [Google Scholar]
- 283.Yao X, Niu X, Ma K, et al. Graphene quantum dots‐capped magnetic mesoporous silica nanoparticles as a multifunctional platform for controlled drug delivery, magnetic hyperthermia, and photothermal therapy. Small. 2017;13:1602225. doi: 10.1002/smll.201602225 [DOI] [PubMed] [Google Scholar]
- 284.Wang H, Revia R, Wang K, et al. Paramagnetic properties of metal‐free boron‐doped graphene quantum dots and their application for safe magnetic resonance imaging. Adv Mater. 2017;29:1605416. doi: 10.1002/adma.201605416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Kooti M, Sedeh AN, Motamedi H, Rezatofighi SE. Magnetic graphene oxide inlaid with silver nanoparticles as antibacterial and drug delivery composite. Appl Microbiol Biotechnol. 2018;102:3607–3621. doi: 10.1007/s00253-018-8880-1 [DOI] [PubMed] [Google Scholar]
- 286.Chen H, Qiu Y, Ding D, et al. Gadolinium‐encapsulated graphene carbon nanotheranostics for imaging‐guided photodynamic therapy. Adv Mater. 2018;30:1802748. doi: 10.1002/adma.201802748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Chawda N, Basu M, Majumdar D, Poddar R, Mahapatra SK, Banerjee I. Engineering of gadolinium-decorated graphene oxide nanosheets for multimodal bioimaging and drug delivery. ACS Omega. 2019;4:12470–12479. doi: 10.1021/acsomega.9b00883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Zeng Y, Li H, Li Z, et al. Engineered gadolinium-based nanomaterials as cancer imaging agents. Appl Mater Today. 2020;20:100686. [Google Scholar]
- 289.Lee BH, Hasan MT, Lichthardt D, Gonzalez-Rodriguez R, Naumov AV. Manganese–nitrogen and gadolinium–nitrogen Co-doped graphene quantum dots as bimodal magnetic resonance and fluorescence imaging nanoprobes. Nanotechnology. 2020;32:095103. doi: 10.1088/1361-6528/abc642 [DOI] [PubMed] [Google Scholar]
- 290.Usman MS, Hussein MZ, Kura AU, Fakurazi S, Masarudin MJ, Ahmad Saad FF. Graphene oxide as a nanocarrier for a theranostics delivery system of protocatechuic acid and gadolinium/gold nanoparticles. Molecules. 2018;23:500. doi: 10.3390/molecules23020500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Thapa RK, Soe ZC, Ou W, et al. Palladium nanoparticle-decorated 2-D graphene oxide for effective photodynamic and photothermal therapy of prostate solid tumors. Colloids Surf B Biointerfaces. 2018;169:429–437. doi: 10.1016/j.colsurfb.2018.05.051 [DOI] [PubMed] [Google Scholar]
- 292.Ruiyi L, Tinling P, Hongxia C, Jinsong S, Zaijun L. Electrochemical detection of cancer cells in human blood using folic acid and glutamic acid-functionalized graphene quantum dot-palladium@ gold as redox probe with excellent electrocatalytic activity and target recognition. Sens Actuators B Chem. 2020;309:127709. doi: 10.1016/j.snb.2020.127709 [DOI] [Google Scholar]