Introduction
The prolonged hospitalization and comorbidities associated with allogeneic hematopoietic stem cell transplantation (HSCT) result in high rates of psychological distress[1] and diminished positive psychological well-being (PPWB; e.g., optimism, gratitude).[2] Low levels of PPWB have been associated with poor clinical outcomes including decreased quality of life (QOL)[3] and diminished immune response,[4] even after controlling for negative psychological factors (e.g., depression) and sociodemographic characteristics. PPWB can be promoted through positive psychology interventions (PPIs). PPIs utilize intentional and systematic activities (e.g., gratitude letter) to enhance PPWB,[5] and they have resulted in better clinical outcomes in medical populations.[6] Compared to cognitive behavioral treatments delivered by mental health clinicians, which can be labor- and time-intensive, PPIs entail 15–20 minutes sessions[6] and can be delivered by individuals with different training backgrounds, including bachelor’s-level clinicians, nurses, physicians or psychologists, allowing for easy scalability. However, PPIs have been underutilized and understudied in HSCT and other cancer populations.[7] Our group’s prior work found that a group-based phone-delivered PPI was feasible and acceptable in long-term HSCT survivors. However, no prior studies have examined the feasibility of PPIs in allogeneic transplant recipients in early recovery post-transplant, despite the high prevalence of distress and diminished PPWB in this population. Accordingly, we conducted a single-arm, proof-of-concept trial (NCT03654404) approved by the Dana-Farber Harvard Cancer Center Institutional Review Board (18–225) to assess the feasibility and acceptability of a novel, 8-week, phone-delivered PPI, the Positive psychology for Allogeneic Transplantation of Hematopoietic stem cells (PATH) study. Based on prior work in medical populations,[6] we hypothesized that the PATH intervention would meet a priori benchmarks for feasibility and acceptability and would show pre-post improvements on patient-reported outcome measures.
Methods
Participants, recruited and consented between September 2018 and November 2019, were adults (≥18 years of age) who spoke English, had the ability to read and complete study procedures, and had access to a phone. We excluded patients with an active psychosis or substance use disorder (diagnosed by the Mini International Neuropsychiatric Interview [MINI][8]), cognitive deficits (assessed with a six‐item cognitive screen[9]), or medical conditions impeding ability to provide informed consent or participate adequately in study procedures. Following discharge from the HSCT hospitalization, we called participants monthly (3 times) to remind them of the study, then scheduled them for an in-person visit coinciding with their 100-day post-transplant visit. During this visit, participants completed baseline assessment measures (Supplemental Table-1), received an intervention manual, and were introduced to the PATH intervention (Supplemental Table-2 for details on intervention delivery, content, and fidelity) by the interventionist (HA). After this visit, participants completed eight weekly positive psychology (PP) exercises (Table 1) and phone sessions with the interventionist. Upon intervention completion (approximately 160-days post HSCT), participants completed self-reported post-intervention outcome assessments and an exit interview with study staff. For our primary outcome, feasibility, we hypothesized that the intervention would be feasible if >50% of eligible patients enrolled in the study and >50% of participants who did baseline assessments completed 5/8 intervention sessions.
Table 1. Description of Positive Psychology Exercises in PATH Intervention.
Provides the description of positive psychology exercises in the PATH intervention - a novel eight-week phone delivered positive psychology intervention comprised of three thematic modules with activities based in gratitude, strengths, and meaning.
| PPWB Construct | PP Exercise | Description | |
|---|---|---|---|
| Session 1 | Gratitude | Gratitude for positive events | Participants recall and describe three positive events they experienced within the last week |
| Session 2 | Expressing gratitude | Participants write a thank you letter to a person who has been kind to them | |
| Session 3 | Strengths | Recalling a past success | Participants recall a successful event and articulate their role in achieving the success |
| Session 4 | Using a personal strength | Participants identify a personal strength and use it in a new way over the next week | |
| Session 5 | Using perseverance | Participants pick a challenging task they used perseverance to complete | |
| Session 6 | Meaning | Enjoyable and meaningful activities | Participants complete three activities: one enjoyable activity alone, one enjoyable activity with another person, and a meaningful activity |
| Session 7 | Describing a good life | Participants describe what their best life a year from the intervention will look like | |
| Session 8 | Planning for the future | Participants review their favorite activities and draft a plan on how to integrate skills learned in daily life |
PPWB: Positive psychological wellbeing; PP: Positive psychology
Results
Of 45 eligible participants, 25 (55.6%) enrolled in the study, 20 (80%) completed baseline assessments, 15 (75%) started the intervention, and 12 (60%) completed the intervention and all follow-up assessments (Figure 1). Participants who completed the baseline assessments were White (n=19; 95%), non-Hispanic (n=20; 100%) with a mean (SD) age of 52.6 (12.78) years. The majority were female (n=11; 55%), married (n=15; 75%), had diagnoses of acute myeloid leukemia (n=9; 45%), acute lymphocytic leukemia (n=6; 30%), myelodysplastic syndrome (n=4; 20%), and non-Hodgkin lymphoma (n=1; 5%); Supplemental Table-3 for patient characteristics. Eligible patients who declined study participation were mostly female (n=12; 60%) with mean (SD) age 45.1 (16.1) years. Among those who completed baseline assessments, 60% (n=12) completed 100% (8/8 sessions) of the PP exercises, surpassing the a priori threshold (>50% completing 5/8 sessions)]. Weekly participant ratings [ease; (B=7.98, 95% CI= 6.92 to 9.04, p<0.001); utility (B=8.34, 95% CI=7.50 to 9.15, p<0.001)] of PP exercises also exceeded our a priori threshold of ≥7/10; Supplemental Table-4. The intervention led to very small-to-medium effect-size improvements in patient-reported outcomes [physical function (d=0.083), QOL (d=0.14), fatigue (d=0.19), positive affect (d=0.26), depression (d=−0.29), anxiety (d=−0.31), and optimism (d=0.32)] summarized in Supplemental Table-5.
Figure 1. Consort Diagram.
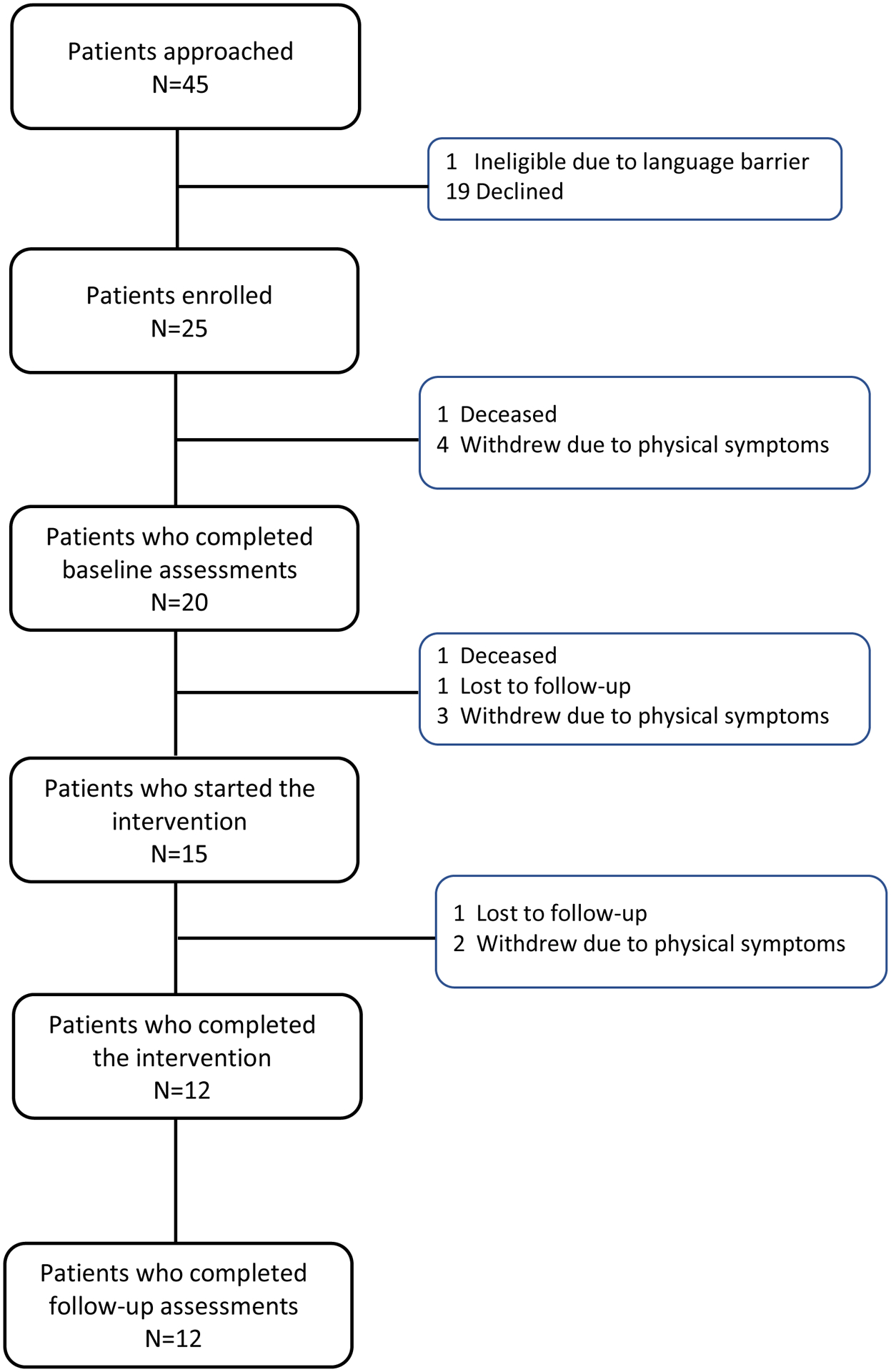
represents the consort diagram that outlines participant flow through each stage of the trial from enrollment, baseline assessment, intervention, and follow-up assessment with reasons for attrition at each stage. Of 45 eligible participants, 25 (55.6%) enrolled in the study, 20 (80%) completed baseline assessments, 15 (75%) started the intervention, and 12 (60%) completed the intervention and all follow-up assessments.
Discussion
In this study of patients with hematologic malignancies undergoing an allogeneic HSCT, a novel, 8-week, telephone-delivered PPI was feasible, acceptable, and associated with modest improvements in psychological outcomes. Participants’ completion rates and ratings of ease and utility of all PP exercises exceeded our a priori feasibility threshold of >50% exercise completion and ≥7/10 (on a 10-point scale) of ease and utility. Our results are consistent with prior work in medically ill patients finding that PPIs are feasible.[6] These findings also complement our prior study of a group phone-based PPI in HSCT survivors that found that PPIs could potentially improve the mental health of allogeneic transplant patients in long-term recovery.[2,10] This initial study of an individual-level PPI provided several useful insights for future research in this population. First, more than half (25/45) of approached patients enrolled in the study, and 40% of the enrolled participants dropped out of the study before intervention initiation. One primary reason for the low recruitment rate and high attrition after enrollment was a high burden of physical symptoms and fatigue in the early recovery following HSCT. Thus, future similar studies should consider approaching patients for study enrollment closer to 100-days post-HSCT to allow sufficient time for recovery since recovery from the acute HSCT hospitalization is complicated by significant physical symptoms, medical comorbidities (e.g., infections, graft-versus-host disease), and risk of mortality. Second, while only 60% (12/20) of participants who completed baseline assessments completed the intervention and follow-up assessments, all participants who actually started the intervention completed all (8/8) PP sessions. Although prior supportive care interventions in this population have been less than four weeks in duration,[11] participants’ completion of every PP exercise in this 8-week intervention suggests that the PATH intervention was relevant and engaging. Third, while we used a phone-delivered format for this intervention, careful consideration of intervention delivery (e.g., comparing phone-based vs. text message-based vs. mobile application-based vs. web-based applications) is important for scalability and cost effectiveness of PPIs in this population. Fourth, writing down reflections could be laborious for HSCT patients who may experience more fatigue, tremors, or other substantial physical symptoms compared to patients with chronic medical illnesses (e.g., diabetes). Hence, testing a variety of options (e.g., audio recordings) for the reflective components of the intervention could improve the ease of the intervention exercises. Although we observed pre-post-intervention improvements in psychological symptoms and PPWB, with effect sizes for individual constructs similar to PPI effect sizes observed in other medical populations,[12] larger controlled trials are needed to test the efficacy of PPIs in HSCT survivors. Our study had several limitations detailed in Supplemental Table-6. Briefly, as participants reported relatively low psychological distress and moderate QOL and function at baseline, their perception and experience of the intervention could vary from patients with significant psychological distress and poor functioning.
In conclusion, PPIs present a potential treatment to bolster PPWB that can both buffer against distress symptoms and positively impact clinical outcomes in the HSCT population. Additional studies are needed to address the issues identified in this initial trial and to more rigorously test efficacy.
Supplementary Material
Funding:
This work was supported by the National Cancer Institute through grant K08CA251654 (to Dr. Amonoo) and by the National Heart, Lung, and Blood Institute through grant R01HL113272 (to Dr. Huffman).
Footnotes
Conflict of Interest statement: All other authors declare that they have no competing financial interests.
References
- 1.El-Jawahri AR, Vandusen HB, Traeger LN, Fishbein JN, Keenan T, Gallagher ER, et al. Quality of life and mood predict posttraumatic stress disorder after hematopoietic stem cell transplantation. Cancer. 2016;122(5):806–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amonoo HL, Barclay ME, El-Jawahri A, Traeger LN, Lee SJ, Huffman JC. Positive Psychological Constructs and Health Outcomes in Hematopoietic Stem Cell Transplantation Patients: A Systematic Review. Biol Blood Marrow Transplant. 2019January;25(1):e5–e16. [DOI] [PubMed] [Google Scholar]
- 3.Kenzik K, Huang IC, Rizzo JD, Shenkman E, Wingard J. Relationships among symptoms, psychosocial factors, and health-related quality of life in hematopoietic stem cell transplant survivors. Support Care Cancer 2015March;23(3):797–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knight JM, Moynihan JA, Lyness JM, Xia Y, Tu X, Messing S, et al. Peri-transplant psychosocial factors and neutrophil recovery following hematopoietic stem cell transplantation. PLoS One 2014;9(6):e99778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seligman ME, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol 2005Jul-Aug;60(5):410–21. [DOI] [PubMed] [Google Scholar]
- 6.Celano CM, Albanese AM, Millstein RA, Mastromauro CA, Chung W-J, Campbell KA, et al. Optimizing a Positive Psychology Intervention to Promote Health Behaviors After an Acute Coronary Syndrome: The Positive Emotions After Acute Coronary Events III (PEACE-III) Randomized Factorial Trial. Psychosom Med 2018Jul-Aug;80(6):526–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amonoo HL, Brown LA, Scheu CF, Millstein RA, Pirl WF, Vitagliano HL, et al. Positive psychological experiences in allogeneic hematopoietic stem cell transplantation. Psychooncology. 2019August;28(8):1633–1639. [DOI] [PubMed] [Google Scholar]
- 8.Pinninti NR, Madison H, Musser E, Rissmiller D. MINI International Neuropsychiatric Schedule: clinical utility and patient acceptance. Eur Psychiatry 2003November;18(7):361–4. [DOI] [PubMed] [Google Scholar]
- 9.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002September;40(9):771–81. [DOI] [PubMed] [Google Scholar]
- 10.Amonoo HL, Kurukulasuriya C, Chilson K, Onstad L, Huffman JC, Lee SJ. Improving Quality of Life in Hematopoietic Stem Cell Transplantation Survivors Through a Positive Psychology Intervention . Biol Blood Marrow Transplant 2020June;26(6):1144–1153. [DOI] [PubMed] [Google Scholar]
- 11.El-Jawahri A, LeBlanc T, VanDusen H, Traeger L, Greer JA, Pirl WF, et al. Effect of Inpatient Palliative Care on Quality of Life 2 Weeks After Hematopoietic Stem Cell Transplantation: A Randomized Clinical Trial. JAMA 2016November22;316(20):2094–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown L, Ospina JP, Celano CM, Huffman JC. The Effects of Positive Psychological Interventions on Medical Patients’ Anxiety: A Meta-analysis. Psychosom Med. 2019Sep;81(7):595–602. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


