Abstract
Objectives:
We investigate how caregiving for grandchildren is associated with cognitive function among rural South Africans, and whether the association differs by gender. We further investigate whether measures of physical activity or social engagement mediate this association.
Methods:
Data were from interviews with 3668 Black, South African grandparents in the “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” study, conducted between 2014 and 2015.
Results:
We find that caregiving grandparents have better cognitive function than non-caregiving grandparents, and this association does not differ by grandparent gender. Although grandchild caregiving is associated with physical activity and social engagement measures, and some of these measures are associated with cognitive function, we do not find conclusive evidence of mediation.
Discussion:
Providing care for grandchildren may stimulate cognitive function for both grandmothers and grandfathers. Neither physical activity nor social engagement explains the association between caregiving and cognitive function.
Keywords: grandparents, caregiving, cognitive function, social support, physical activity
Introduction
As populations across the globe experience aging at a rapid pace, concerns over the health and well-being of older adults are at an all-time high (Bengtson, 2003; King & Guralnik, 2010). There is a particular focus on cognitive health due to its critical role in maintaining older adults’ independence and well-being. As people age, they often experience changes in their roles and social environment that can lead them to become less physically active and more socially isolated, which can accelerate cognitive decline (Bonsang et al., 2012; Middleton et al., 2010; Rantakokko et al., 2013). However, even as aging adults transition out of their former roles, they often take on new roles that have the potential to protect against cognitive decline, such as caregiving for their grandchildren. We seek to develop a better understanding of the association between caring for grandchildren and cognitive function in order to inform whether or not caring for grandchildren may be a route through which older adults can delay declines in their cognitive health.
We focus on grandparents in rural South Africa, where this caregiving is usually done on a full-time basis (Freeman & Nkomo, 2006; Parker & Short, 2009). Given the presence of comorbid diseases, it is especially important to understand the factors impacting cognitive health (Clark et al., 2015; Kabudula et al., 2014). We use some of the first data on cognitive function in this region to investigate whether caring for grandchildren is associated with better cognitive function among a cohort of adults aged 40 years and older. We further investigate whether this association differs for grandmothers versus grandfathers, and whether physical activity or social engagement mediates this association.
Background
We focus on a setting in rural northeastern South Africa: a cluster of villages in and near the Agincourt subdistrict, in Mpumalanga province. This region was a former “homeland” of forced racial segregation during apartheid, to which Black South Africans belonging to the Shangaan ethnic group were forcibly moved (Blalock, 2014). The high burden of both communicable and noncommunicable disease in South Africa means that life expectancy at birth is relatively low, at 61 and 67 for men and women, respectively (PRB, 2018). The HIV epidemic hit the country hard, predominantly affecting the middle generation of Black South Africans and peaking between the mid-1990s and mid-2000s (Kahn et al., 2007; Mee et al., 2016).
Due to the high prevalence of HIVas well as out-migration of young adults for work in the Agincourt study area, the middle generation is often unavailable to provide full-time care to their children (Madhavan & Gross, 2013; Nyasani et al., 2009). As a result, many children are left in the care of their grandparents (Kabudula et al., 2014; Mtshali, 2015; Schatz & Ogunmefun, 2007). In 2015, approximately half of South African children, nationwide, who did not live with their parents were living with grandparents (Statistics South Africa, 2017). The South African government offers financial assistance, some of which these grandparents are eligible to claim, including old-age pensions, child support grants, and foster child grants (Delany et al., 2008). These grants can support grandparents in caring for dependent children but often fall short of their needs (Schatz & Ogunmefun, 2007). This caregiving responsibility can create financial and social stress for grandparents (Ice et al., 2012, 2010) and may have important and lasting implications for cognitive health. These effects may be especially pronounced among this population, as South Africans often transition to grandparenthood and grandchild care beginning at relatively young ages (Margherio, 2019).
Grandchild Caregiving, Health, and Cognition
Studies have been mixed as to how grandchild caregiving can impact health. Research often shows that full-time grandchild care can lead to detrimental health outcomes, such as poorer cognitive functioning in verbal fluency (although not in numeracy or word recall) (Arpino & Bordone, 2014); issues with pain and mobility, greater stress, and lower life satisfaction (Bowers & Myers, 1999; Clottey et al., 2015); and accelerated health decline (Chen & Liu, 2012). On the other hand, Hughes et al. (2007) found null effects of full-time caregiving on health outcomes. Less intensive grandchild care is often associated with improved outcomes, such as lower risk of mortality (Hilbrand et al., 2017); healthier behaviors and better mental health (Hughes et al., 2007); and lower burden and stress (Bowers & Myers, 1999). However, less intensive care has also been found to lead to poorer self-rated health (in random effects, but not fixed effects models) (Ates, 2017). To date, the majority of these studies have been focused in the United States and other high-income settings.
When grandparents in sub-Saharan Africa take on caregiving of their grandchildren, it is typically assumed on a full-time basis, and often due to HIV-related deaths of their children (Boon et al., 2010; Ice et al., 2008; Matovu & Wallhagen, 2018; Ssengonzi, 2007). In the United States, grandparents sometimes assume full-time care due to stressful events, as well, such as incarceration of parents (Baker et al., 2008). However, full-time care is more normative, and multigenerational family structures are more common in sub-Saharan Africa (Ice et al., 2012). The normative nature of such dynamics may mean that full-time care is less stressful in this setting. In fact, studies among the elderly in Uganda have revealed that grandparent caregivers often feel a sense of fulfillment and satisfaction from this role (Matovu et al., 2020; Stella & Annet, 2019). Similarly, caregiving of grandchildren in rural Kenya has been found to be associated with better nutrition for grandmothers (Ice et al., 2011; Ice et al., 2008) and better mental health for grandparents (Ice et al., 2008)—especially for grandparents involved in more intensive caregiving (Ice et al., 2010).
On the other hand, sub-Saharan African grandparents, particularly grandmothers (Chazan, 2008; Mtshali, 2015; Ssengonzi, 2007), take on a great deal of emotional, physical, and financial burden when they assume care of their grandchildren (Boon et al., 2010; Matovu et al., 2020). Grandchild caregiving in this region is often undertaken with little social support and significant physical demands that can impact physical functioning (Boon et al., 2010). This caregiving has been linked to physical health issues and elevated stress (Ice et al., 2010, 2008; Matovu & Wallhagen, 2018), especially when full-time and intensive (Ice et al., 2012; Oburu, 2005).
Grandchild caregiving in South Africa looks similar to other sub-Saharan African settings, in terms of the reasons that grandparents take on this role and the intensity of it (Kahn et al., 2007; Mtshali, 2015; Schatz & Ogunmefun, 2007). Although this role can be stressful, grandparents may take on the care of their grandchildren out of a sense of obligation (Dolbin-MacNab & Yancura, 2018). In fact, there is a long history of intergenerational childcare and fostering in South Africa (Dolbin-MacNab & Yancura, 2018; Zimmerman, 2003), which may translate to the expectation and mental preparedness for grandparents to assume this role (Bowers & Myers, 1999). This sense of obligation and expectation, combined with evidence in similar settings that this role may offer fulfillment and a feeling of purpose to grandparents (Ice et al., 2010; Matovu & Wallhagen, 2020; Stella & Annet, 2019), leads us to hypothesize that grandchild caregiving among rural South African grandparents is associated with better cognitive health. Still, given the mixed evidence of how this role impacts other aspects of grandparent health, we treat this hypothesis as exploratory.
Hypothesis 1:
We expect that caregiving grandparents will have better cognitive function than non-caregiving grandparents.
Grandparent Gender and Caregiving
Women tend to take on greater caregiving responsibilities than men (Bondi, 2008). Perhaps, as a result of this gender skewedness, we know little about gender differences in the impact of caregiving on grandparents’ health. In sub-Saharan Africa, too, women assume care responsibilities, and men are less likely to consider these responsibilities as in their domain (Ice et al., 2008; Ssengonzi, 2007). It is possible that grandmothers may feel less burden from this role, as they hold a greater expectation of taking it on, and social norms are more supportive of their caregiving work (Ice et al., 2008). This may result in a more positive impact of grandchild caregiving on women’s cognitive function than on men’s.
Hypothesis 2:
We expect that women who care for their grandchildren will have better cognitive function than their male counterparts.
Mechanisms: Physical Activity and Social Engagement
There are several possible mechanisms through which grandchild caregiving may influence cognitive health, and we will test two of these: physical activity and social engagement. Grandchild caregiving might impact grandparents’ cognitive health through increased physical activity (or reduced physical inactivity) (Stella & Annet, 2019). Spending time with grandchildren likely requires grandparents to be more physically active than they otherwise would be (Waldrop & Weber, 2001). Physical activity is thought to influence cognitive health, in turn, by increasing blood perfusion to the brain and decreasing risk of hypertension, stroke, and other cerebrovascular conditions (Carvalho et al., 2014; Colcombe et al., 2004; Rea, 2017).
Hypothesis 3:
We expect that physical activity (or inactivity) will mediate the association between grandchild caregiving and cognitive function.
Similarly, spending time with grandchildren may facilitate greater social engagement for grandparents (Chen & Liu, 2012), which can further enhance their cognitive function. We focus on two aspects of social engagement: social interaction and social support. When they care for their grandchildren, grandparents may get out of the house more often and interact with people outside of their home. This social interaction can, in turn, buffer against cognitive decline by stimulating cognitive skills, like memory retrieval and executive function, which may make the brain more resilient to age-related decline (Arpino & Bordone, 2014; Ertel et al., 2008; Glei et al., 2005; Haslam et al., 2016; Shankar et al., 2013). Caregiving grandparents may also seek social support to help them in their caregiving (Oburu & Palmérus, 2005), and receipt of such support may play a similarly important role in their cognitive health (La Fleur & Salthouse, 2016; Rodakowski et al., 2012; Zahodne et al., 2014) by bolstering cognitive reserve via an increase in positive psychosocial resources and an influence on health behaviors (Reblin & Uchino, 2008; Zahodne et al., 2014). Moreover, social support may promote healthier management of stress and may reduce stress and depressive symptoms (Cohen, 2004; Dickinson et al., 2011). By extension, the number of people from which grandparents receive this kind of support may have important impacts on their cognitive resilience and health.
Hypothesis 4:
We expect that the amount of social interaction and number of people providing social support to grandparents will mediate the association between grandchild caregiving and cognitive function.
Methods
Data and Sample
We use data from the “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI) study. Participants were randomly sampled from the existing framework of the Agincourt Health and Socio-Demographic Surveillance System (Agincourt HDSS) site in Mpumalanga province. Adults aged 40 years and older as of July 1, 2014 who were permanently living in the study area during the 12 months previous to the 2013 Agincourt census update were eligible. A total of 6281 women and men were sampled; 391 of them had moved outside of the study site or were deceased at the time of the attempted interview. From the remaining 5890 eligible individuals, 5059 participated in the baseline survey. Data were collected between November 2014 and November 2015, involving computer-assisted personal interviewing (CAPI) and collection of anthropometric measurements and biomarkers.
Our analytic sample includes all respondents who had grandchildren at the time of the interview (n = 4187) and had complete information on measures used in our models, leaving us with an analytic sample of 3668. Although people under the age of 60 years are not typically considered to be “older adults” in high-income settings, men and women experience about 16 years shorter life expectancy in South Africa than in high-income countries (PRB, 2020), suggesting that the experiences associated with aging, such as cognitive decline, may occur at younger ages in South Africa. The difference is likely to be even more pronounced in rural contexts, among Black South Africans. Moreover, grandparenting occurs at relatively young ages in this setting, where women often bear children in their early 20s (Eyre et al., 2018). Hence, it is appropriate that our sample includes grandparents aged 40 years or older.
Measures
Dependent measure.
We operationalize cognitive function using a score that ranges from 0 to 24. This measure is the sum of immediate recall of 10 words (up to 10 points), recall of those 10 words after a 1-minute delay (up to 10 points), and four orientation items (ability to state the correct year, month, date, and name of the current South African president; up to 4 points total). These cognitive battery items were adapted from those used in the US Health and Retirement Study (HRS) (Crimmins et al., 2011). Word recall and orientation are important domains, as they are sensitive to age- and dementia-related cognitive decline. These measures have been used ubiquitously on cognitive screening measures in aging populations worldwide (Lyness et al., 2014; Ofstedal et al., 2005), allowing for comparability with other studies. The construct validity of word recall as an indicator of overall brain aging has been demonstrated in a variety of contexts, including other low- and middle-income countries (Prince et al., 2003; Skirbekk et al., 2012). Our cohort exhibits similar distributions of these measures compared with the HRS (Kobayashi et al., 2019), despite lower overall mean scores, and also exhibits strong associations with functional competence (Harling et al., 2019; Kobayashi et al., 2020). Moreover, these measures of word recall and orientation have good internal consistency in our sample (Cronbach’s alpha of 0.69). Furthermore, operationalizing cognitive function using only immediate and delayed word recall produces similar results to those we discuss below (see Supplementary Table 1).
We use a z-standardized version of this score, centering the mean at zero and SD at one, similar to other work (Avila et al., 2019; Kobayashi et al., 2017; Ospina-Romero et al., 2019; Zahodne et al., 2011). Standardizing the cognitive outcome measure facilitates comparison with other literature that also uses z-standardization by placing the cognitive outcome variable in within-sample SD units.
Independent measure.
Our key independent measure is an indicator of whether the respondent, hereafter referred to as the grandparent, provided care for their grandchild(ren) in the past year. The variable is coded from an item in the survey that asked respondents, who had reported that they have any grandchildren, “Did you spend any time taking care of your grandchildren last year?” We code this measure as binary, to reflect any care given in the last year.
We chose to code this measure as binary because, as discussed above, grandchild caregiving in this setting tends to be on a full-time basis, with very few grandparents reporting less than full-time care. In our sample of 1164 grandparents who reported providing any care to grandchildren in the past year, 1060 reported the number of weeks in that year and the number of days in those weeks (i.e., 104 had missing information on those measures). These 1160 caregiving grandparents reported an average of 44.1 weeks of care and a median of 52 weeks of care in the past year, and an average of 6.8 days per week and median of 7 days per week during those weeks. Moreover, of the grandparents who reported providing care, 96% also reported coresidential grandchildren.
In order to further assess the appropriateness of coding this measure as binary, we tested a model (not shown) using three dummy measures to indicate amount of care: (1) no care in the past year, (2) care for at least half of the year (i.e., at least 26 weeks; 86% of caregivers with non-missing information), and (3) care for less than half the year. We also tested a similar model using a caregiving cutoff of three-quarters of the year (i.e., at least 39 weeks; 83% of caregivers with non-missing information fall into this category). We found that those who provided care for less than half or less than three-quarters of the past year, in respective models, did not perform differently on the cognitive battery than grandparents who provided care for a greater amount of time (see Supplementary Tables 2 and 3.). Given the small proportion of grandparents giving only part-time care, and given the similar results of those part-time caregivers to grandparents providing full-time care, we find justification for our binary coding of our measure of grandparent caregiving.
Physical activity.
We code two measures of physical activity, to reflect both active and inactive time. First, we code a measure to reflect the number of hours spent walking or cycling on a usual day. This comes from survey items, first asking “Do you walk or use a bicycle (for at least 10 minutes at a time) to get to and from places?,” then “On a usual day, how many hours do you spend walking or cycling for travel?” Data were collected on both the number of hours and minutes spent walking or cycling. We code a “no” on the first item (i.e., less than 10 minutes of walking/cycling in a day) as 0; more than 10 minutes of walking/cycling is coded to the next greatest hour. The measure is top code at 3 hours (12% reported more than 3 hours of walking/cycling in a day). Although this measure is less ideal than concurrent reporting of time use, similar measures of physical activity that require respondent recall of time use have been found to be reliable in similar settings (Craig et al., 2003; Sobngwi et al., 2001).
The second measure indicates the time spent sitting, from a survey item that asked “On a usual week day, how many hours did you spend sitting or reclining (excluding sleep)? This may include time sitting on a chair or bench, visiting friends, reading, sitting in church, sitting down to watch television.” Data were collected on the number of hours and minutes that the grandparent reported sitting. We code this measure to the next greatest hour, then top code at more than 6 hours (11% reported more than 6 hours of sitting in a day).
Social engagement and number of sources of social support.
We code a measure of social engagement that indicates the average number of days per month that the grandparent interacts with up to seven named social contacts. Respondents were asked to name up to six adults with whom they have been in communication (in person, by phone, or by internet) over the previous 6 months. If the respondent was married and did not name their spouse, their spouse became their last (and, in some cases, seventh) contact. The respondent then answered how frequently they interacted with each of those named contacts, in turn, over the past 6 months. Response options included “every day or almost every day,” “a few times per week,” “once per week,” “a few times per month,” “once per month,” “a few times in the past 6 months,” and “not at all.” We coded these categories into numbers reflecting days per month (i.e., 30, 12, 4, 3, 1, 0.5, or 0, respectively). We then added the reported frequency of interaction across all named contacts and divided by the number of contacts named. We then collapsed this continuous measure into a categorical measure, with a code of 1 indicating 10 or fewer days per month (only 7 people reported 0 days per month, on average), 2 indicating 11–20 days per month, and 3 indicating 21–30 days per month.
Next, we coded a measure to reflect the number of sources, or social contacts, from whom grandparents reported receiving either emotional, financial, physical, or informational support. After respondents named up to 7 social contacts, as described above, they were then asked: “Which of the following answers best describes how often you typically received emotional support from (social contact N), such as when you are feeling sad or anxious or upset, over the past 6 months?” They were then asked a similar question about receipt of physical support (“such as when you have needed help with chores around the house or at work, taking care of yourself, or going from one place to another”), informational support (“such as receiving advice about important health issues and employment issues”), and financial support (“such as borrowing money, receiving food, being given a job, or anything else related to money or in-kind transfers”) from each named contact. Response options mirrored those for our measure of social engagement. We code this measure to reflect the total number of contacts that grandparents reported to have provided them with any type of support at least a few times per month in the past 6 months.
Controls.
We include several covariates in our models. First, in order to help account for possible selection of healthier grandparents into caregiving status, our full models control for measures of grandparents’ physical health, mental health, and comorbidities. The first of these health indicators is a measure of self-rated health. The item originally ranged from 1 to 5. However, due to few (20%) reporting moderate, bad, or very bad health, we coded the measure to range from 1 to 3, with 1 indicating “moderate, bad, or very bad,” 2 indicating “good,” and 3 indicating “very good” health. We also control for whether grandparents had at least one of five limitations in their activities of daily living (ADLs), including difficulty with walking, bathing, eating, getting in/out of bed, and using the toilet. We code this measure as 1 if they reported having at least one ADL limitation and 0 otherwise. We also account for depressive symptoms using the 8-item Center for Epidemiologic Studies Depression (CES-D) scale (Turvey et al., 2005). We code this measure as the total number of symptoms reported. Next, we control for number of comorbidities, including HIV (from blood), diabetes (either self-reported or confirmed in blood glucose), angina (self-reported), and/or hypertension (from blood pressure). Because only one person had more than three comorbidities, we top code this measure at 3. Moreover, because many people are missing on this measure due to refusals related to HIV measurement or inconclusive blood tests, we assign them a code of 0 and include a dummy variable indicating missing information on comorbidities.
Next, we account for number of children, as grandparents with a greater number of children may be more likely to take on grandchild caregiving. This measure is top-coded at 8 or more children because few grandparents (8%) had more than 8 children. Additionally, we control for the number of children that were born alive but are deceased, top-coded at 2 or more. This measure helps account for selection—as grandparents often take on the care of their grandchildren when the parents have died—and confounding that can result from the stress of a child’s death in the associations we investigate (Boon et al., 2010). Next, we control for the number of grandchildren under the age of 16 years, and top code this measure at 9 because few (8%) reported having more than 9 grandchildren under age 16 years. Nearly a fifth of the sample of grandparents reported that they did not know how many grandchildren they had under the age of 16 years, and so we assign these grandparents a code of 0 on this measure and include a dummy variable reflecting this “don’t know” response.
We also account for demographic characteristics of the grandparents. In models of the full sample of grandparents, we control for the grandparents’ gender, coded as 1 if female and 0 if male. In all models, we also control for age, with a continuous measure reflecting years of the grandparent’s age. We control for their marital status, as well, with a series of dummy variables indicating whether the grandparent was never married, married or living with a partner, separated or divorced, or widowed at the time of the survey.
Next, we control for socioeconomic measures. We account for grandparents’ education, coded into three dummy variables to indicate that they had (1) no formal education, (2) some or completed primary education, or (3) some secondary or higher education. We also control for grandparents’ primary employment status. These measures come from a survey item in which respondents could check as many response options as applied to them. We code employment status as four dummy variables to indicate (listed in order of how we prioritized responses): (1) employed, (2) home manager (originally meant to indicate “homemaker,” but translated to be understood as “one who manages the home”), (3) retired, or (4) not working. We additionally control for individual income and transfers, as this helps to account for formalized financial support that the grandparent may be receiving via pensions, which may help mitigate stress associated with caregiving. This measure is coded into three categories, such that 1 = 0 RAND, 2 = 1–1400 RAND, and 3 = over 1400 RAND.
We also account for household characteristics and other caregiving burden. We control for a five category measure of household wealth quintiles. Households were ranked according to the scores from principal component analysis of household ownership of items such as televisions, refrigerators, livestock, and vehicles as well as housing characteristics, and type of water and sanitation facilities (Riumallo-Herl et al., 2019). We also control for whether the grandparent was providing care to adults in the household, coded 1 if so and 0 if not. Next, we control for household size with a measure coded 0 if the grandparent was living alone, 1 if living with one other person, 2 if living with two to five other people, and 3 if living with six or more other people.
Last, we control for the consecutive month of fieldwork in which the interview was conducted. We include this control measure because of evidence from the HAALSI study that the recorded survey responses, particularly for items regarding social engagement and social support, were impacted by the timing of interviews during the progression of fieldwork (Harling et al., 2018).
Analytic Approach
We use ordinary least squares (OLS) regression to estimate the association between grandparent caregiving and cognitive function, to test interactions with gender, and to test possible mechanisms.
Results
Bivariate Results
Table 1 displays the mean values of each measure in our analyses, for the full sample as well as for grandmothers and grandfathers, separately. Grandmothers have lower cognitive function than grandfathers in our sample, mirroring gender differences found in other work (Andersen et al., 1999). Twenty-nine percent of grandparents in our sample report providing care to their grandchild in the past year, with more grandmothers (35%) than grandfathers (22%) reporting this care. Also noteworthy, grandparents reported 3.61 hours of sitting on a usual day, with grandmothers reporting slightly less sitting (3.52 hours) than grandfathers (3.71 hours). Grandparents reported 1.66 hours of walking/cycling, with grandmothers reporting slightly less than grandfathers (1.57 vs. 1.76 hours). Grandparents also reported an average of just over 2 days per month of social interaction with their named contacts in the last 6 months, with grandmothers again reporting less than grandfathers (2.13 vs. 2.29). Finally, grandparents reported receiving social support from an average of about three people, at least a few times per month in the past 6 months, with grandfathers reporting slightly more sources of support than grandmothers (3.37 vs. 3.20). Although some of these gender differences on the measures mentioned here appear to be small, each is significant at p < .05.
Table 1.
Descriptive Statistics of the Sample, Caregiving and Non-Caregiving Grandparents Compared.
| All grandparents (n = 3668) |
Grandmothers (n = 2053) |
Grandfathers (n = 1615) |
Range | |
|---|---|---|---|---|
| Cognition | ||||
| Total cognitive score (standardized) | 0.00 (1.00) | −0.05 (1.02) | 0.07 (0.97) | −2.66–2.94 |
| Grandchild caregiving | ||||
| Cares for grandchildren | 0.29 | 0.35 | 0.22 | 0–1 |
| Physical activity and social engagement | ||||
| Time spent sitting | 3.61 (1.87) | 3.52 (1.84) | 3.71 (1.90) | 0–7 |
| Time spent walking or cycling | 1.66 (1.23) | 1.57 (1.18) | 1.76 (1.28) | 0–4 |
| Frequency of social interaction | 2.20 (0.79) | 2.13 (0.81) | 2.29 (0.76) | 1–3 |
| Social support, number of sources | 3.28 (1.57) | 3.20 (1.54) | 3.37 (1.61) | 1–7 |
| Controls | ||||
| Health conditions | ||||
| Self-rated health | 1.88 (0.71) | 1.86 (0.71) | 1.90 (0.71) | 1–3 |
| Has at least one limitation in activities of daily living | 0.08 | 0.08 | 0.08 | 0–1 |
| Depressive symptoms | 1.45 (1.61) | 1.49 (1.69) | 1.40 (1.50) | 0–8 |
| Comorbidities | 1.00 (0.69) | 1.04 (0.68) | 0.94 (0.69) | 0–3 |
| Missing | 0.10 | 0.10 | 0.11 | 0–1 |
| Family characteristics | ||||
| Number of children | 4.90 (2.08) | 4.61 (2.01) | 5.27 (2.11) | 0–8 |
| Number of children born alive who later died | 0.99 (0.86) | 1.06 (0.86) | 0.91 (0.86) | 0–2 |
| Number of grandchildren under the age of 16 years | 3.60 (3.06) | 3.71 (3.09) | 3.47 (3.01) | 0–9 |
| Doesn’t know how many grandchildren under the age of 16 years | 0.18 | 0.17 | 0.19 | 0–1 |
| Demographics | ||||
| Female | 0.56 | 1.00 | 0.00 | 0–1 |
| Age | 63.79 (11.88) | 62.73 (12.32) | 65.13 (11.16) | 40–90 |
| Marital status | ||||
| Married or living with partner | 0.55 | 0.38 | 0.76 | 0–1 |
| Never married | 0.02 | 0.03 | 0.01 | 0–1 |
| Separated or divorced | 0.11 | 0.12 | 0.10 | 0–1 |
| Widowed | 0.32 | 0.47 | 0.13 | 0–1 |
| Socioeconomic indicators | ||||
| Education | ||||
| No formal | 0.46 | 0.49 | 0.42 | 0–1 |
| Primary | 0.37 | 0.35 | 0.38 | 0–1 |
| Secondary | 0.17 | 0.16 | 0.20 | 0–1 |
| Employment status | ||||
| Employed | 0.14 | 0.13 | 0.15 | 0–1 |
| Home manager | 0.12 | 0.14 | 0.09 | 0–1 |
| Retired | 0.21 | 0.18 | 0.26 | 0–1 |
| Not working | 0.53 | 0.55 | 0.50 | 0–1 |
| Individual earnings and transfers | 1.76 (0.83) | 1.63 (0.77) | 1.92 (0.87) | 1–3 |
| Household and caregiving characteristics | ||||
| Household wealth index | 3.06 (1.43) | 3.03 (1.41) | 3.11 (1.44) | 1–5 |
| Provides care to adult in household | 0.04 | 0.04 | 0.03 | 0–1 |
| Number of people in household | 2.10 (0.87) | 2.14 (0.80) | 2.04 (0.95) | 0–3 |
| Interview month | 5.52 (3.05) | 5.37 (3.01) | 5.72 (3.09) | 1–12 |
Note. Standard deviation shown in parentheses for continuous variables.
It is also important to note differences in health by caregiving status, which might be suggestive of selection into caregiving. We tested differences on health indicators (not shown). These tests revealed that, among grandmothers, self-rated health, CES-D score, and comorbidities did not differ by caregiving status at p < .10 or better. However, caregiving grandmothers are more likely to have an ADL limitation than their non-caregiving counterparts (6.3% vs. 8.6% with ADL; p < .01). Among grandfathers, caregivers had significantly lower CES-D score than their non-caregiving counterparts (score of 1.23 vs. 1.44; p < .05).
Multivariate Results
Association between grandchild caregiving and cognitive function.
Table 2 displays results from OLS, in which z-standardized total cognitive score is the dependent variable. In Model 1, we test the association between grandchild caregiving and cognitive function for all grandparents, net of the indicators for health, family characteristics, demographics, socioeconomic status, and household and caregiving characteristics. We find a strong positive association between grandchild caregiving and cognition: Grandparents who provide care to their grandchildren perform 0.22 SDs higher on the cognitive test than grandparents who do not. This supports Hypothesis 1.
Table 2.
Ordinary Least Squares Regression of Grandchild Caregiving on Cognitive Function (Standardized).
| Model 1 All grandparents |
Model 2 Grandmothers |
Model 3 Grandmothers |
||||
|---|---|---|---|---|---|---|
| B | 95% CI | B | 95% CI | B | 95% CI | |
| Intercept | 0.33* | (0.06, 0.59) | 0.47** | (0.13, 0.81) | 0.25 | (−0.16, 0.67) |
| Grandchild caregiving | ||||||
| Cares for grandchildren | 0.22*** | (0.15, 0.28) | 0.22*** | (0.14, 0.30) | 0.18*** | (0.07, 0.28) |
| Controls | ||||||
| Health conditions | ||||||
| Self-rated health | 0.19*** | (0.14, 0.23) | 0.14*** | (0.08, 0.19) | 0.24*** | (0.17, 0.30) |
| Has at least one limitation in activities of daily living | −0.29*** | (−0.39, −0.18) | −0.30*** | (−0.44, −0.16) | −0.28*** | (−0.43, −0.12) |
| Depressive symptoms | −0.03*** | (−0.05, −0.02) | −0.02 | (−0.04, 0.01) | −0.06*** | (−0.09, −0.03) |
| Comorbidities | 0.05* | (0.01, 0.09) | 0.004 | (−0.05, 0.06) | 0.10** | (0.03, 0.16) |
| Missing | −0.01 | (−0.10, 0.09) | −0.04 | (−0.17, 0.08) | 0.05 | (−0.09, 0.19) |
| Family characteristics | ||||||
| Number of children | 0.03** | (0.01, 0.04) | 0.02+ | (−0.001,0.04) | 0.02* | (0.001, 0.05) |
| Number of children who have died | −0.05** | (−0.09, −0.01) | −0.08** | (−0.12, −0.03) | −0.03 | (−0.08, 0.03) |
| Number of grandchildren under the age of 16 years | 0.01 | (−0.004, 0.02) | 0.01 | (−0.01, 0.02) | 0.01 | (−0.01, 0.03) |
| Doesn’t know how many grandchildren under the age of 16 years | 0.15** | (0.05, 0.25) | 0.07 | (−0.07, 0.20) | 0.26*** | (0.11, 0.41) |
| Demographics | ||||||
| Female | −0.07* | (−0.14, −0.01) | ||||
| Age | −0.02*** | (−0.02, −0.02) | −0.02*** | (−0.02, −0.01) | −0.02*** | (−0.02, − 0.01) |
| Marital status (Ref: Married or living with partner) | ||||||
| Never married | 0.05 | (−0.13, 0.23) | 0.14 | (−0.07, 0.35) | −0.22 | (−0.58, 0.14) |
| Separated or divorced | −0.05 | (−0.14, 0.05) | 0.09 | (−0.03, 0.21) | −0.25** | (−0.41, −0.09) |
| Widowed | −0.14*** | (−0.21, −0.07) | −0.12** | (−0.21, −0.04) | −0.05 | (−0.18, 0.09) |
| Socioeconomic indicators | ||||||
| Education (Ref: No formal) | ||||||
| Primary | 0.37*** | (0.30, 0.43) | 0.44*** | (0.35, 0.52) | 0.29*** | (0.19, 0.39) |
| Secondary | 0.63*** | (0.53, 0.72) | 0.68*** | (0.55, 0.80) | 0.56*** | (0.43, 0.69) |
| Employment status (Ref: Not working) | ||||||
| Employed | −0.02 | (−0.12, 0.08) | −0.05 | (−0.19, 0.08) | −0.02 | (−0.16, 0.13) |
| Home manager | −0.10* | (−0.19, −0.01) | −0.06 | (−0.18, 0.05) | −0.14+ | (−0.30, 0.02) |
| Retired | −0.08* | (−0.15, −0.004) | −0.08 | (−0.19, 0.02) | −0.09 | (−0.19, 0.02) |
| Individual earnings and transfers | −0.03 | (−0.07, 0.01) | −0.002 | (−0.06, 0.05) | −0.05+ | (−0.10, 0.01) |
| Household and caregiving characteristics | ||||||
| Household wealth index | 0.05*** | (0.03, 0.07) | 0.06*** | (0.03, 0.09) | 0.04* | (0.01, 0.07) |
| Provides care to adult in household | −0.09 | (−0.24, 0.05) | −0.17+ | (−0.35, 0.01) | 0.02 | (−0.22, 0.26) |
| Number of people in household | −0.03+ | (−0.07, 0.003) | −0.03 | (−0.08, 0.02) | −0.05+ | (−0.11, 0.01) |
| Interview month | 0.02*** | (0.01, 0.03) | 0.02*** | (0.01, 0.03) | 0.03*** | (0.01, 0.04) |
| R 2 | 0.31 | 0.36 | 0.26 | |||
| F | 64.34*** | 47.44 *** | 22.83*** | |||
| N | 3668 | 2053 | 1615 | |||
Note. Two-tailed tests,
p<.10,
p<.05,
p<.01,
p<.001.
In order to check for whether these results are specific to younger or older grandparents, we also tested a model identical to Model 1, but with an interaction between grandchild caregiving and a binary measure of whether the grandparent is aged 65 years or older (shown in Supplemental Table 4). That interaction term was not significant, suggesting that the association between caregiving and cognitive function is similar for younger and older grandparents, in our sample aged 40 plus.
Models 2 and 3 of Table 2 are identical to Model 1, except that grandparents are split into separate samples, by gender. These models reveal that caregiving grandmothers (Model 2) and grandfathers (Model 3) both perform higher on the cognitive test than their non-caregiving counterparts (0.22 SDs higher for caregiving grandmothers and 0.18 higher for caregiving grandfathers). We also tested an interaction between caregiving and grandparent gender among the pooled sample (not shown), and found that the impact of caregiving on cognitive function did not significantly differ by grandparent gender. Thus, Hypothesis 2 is not supported. Nonetheless, given that there are likely to be important underlying gender differences, we split the subsequent analyses by gender.
The Mediating Roles of Physical and Social Factors
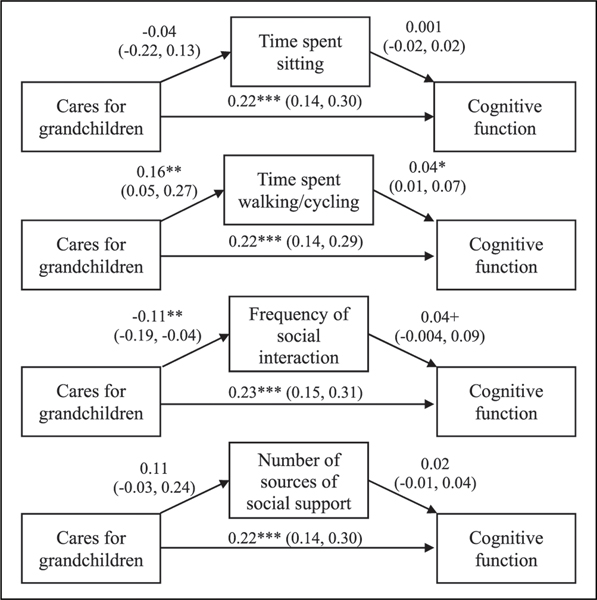
Next, we test whether physical activity, frequency of social interaction, and number of sources of social support mediate the association between grandchild caregiving and cognitive function. We do this using the approach outlined by Baron and Kenny (1986). Figure 1 displays the key results of these mediation models for the sample of grandmothers. The top row of Figure 1 shows that, in the fully adjusted model that treats time spent sitting as the dependent variable, caring for grandchildren is not significantly associated with time spent sitting at p ≤ .10 (β = −0.04 (where the measure of time spent sitting ranges from 0 to 7). Moreover, time spent sitting is not significantly associated with cognitive function (β = 0.001). Finally, including time spent sitting in the same model as grandchild caregiving does not change the magnitude or significance of the association between caregiving and cognitive function (β = 0.22*** ), as compared with the coefficient for caregiving in Model 2 of Table 2. Hence, we do not find evidence that time spent sitting mediates the association between grandchild caregiving and cognitive function.
Figure 1.
Association between grandchild caregiving and cognitive function, as mediated by indicators of physical and social activity, grandmothers (n = 2053). Each arrow corresponds to separate, fully adjusted models. Coefficients and confidence intervals from ordinary least squares.
Results displayed in the subsequent two rows of Figure 1 suggest that caregiving is positively and significantly associated with time spent walking/cycling (β = 0.16**, where the measure of time spent walking/cycling ranges from 0 to 4), and negatively associated with frequency of social interaction (β = −0.11**, where the measure of frequency of social interaction ranges from 0 to 3). Moreover, both of these possible mediators are significantly and positively associated with cognitive function (β = 0.04* and β = 0.04+, respectively). However, including each of these possible mediators, in turn, in the model with grandchild caregiving does not affect the magnitude or significance of the association between caregiving and cognitive function (β = 0.22*** and 0.23***, respectively). As shown in the final row of Figure 1, we also find no evidence that the number of sources of social support is a mediator in the association between grandmothers’ caregiving and cognitive function.
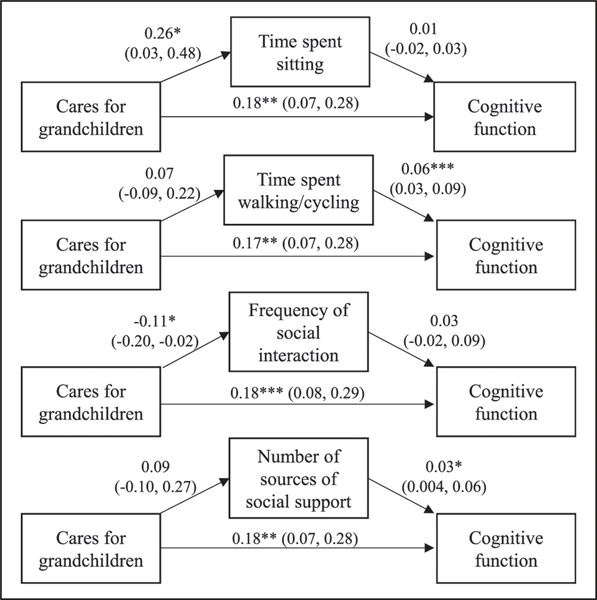
Figure 2 shows results from the same set of models among the sample of grandfathers. The first row suggests that, for grandfathers, caregiving is significantly associated with more time spent sitting (β = 0.26* ), but time spent sitting is not significantly associated with cognitive function. Including time spent sitting in the model with caregiving does not affect the magnitude or significance of the association between caregiving and cognitive function (β = 0.18** ), as compared with the coefficient for caregiving in Model 3 of Table 2. Similarly, in the third row of Figure 2, we find that caregiving for grandchildren is significantly negatively associated with frequency of social interaction (β = −0.11*), but social interaction is not significantly associated with cognitive function. Moreover, accounting for frequency of social interaction does not change the significance or magnitude of the association between grandchild caregiving and cognitive function. Results displayed in the second and last rows of Figure 2 suggest that caregiving is not significantly associated with time spent walking/cycling or number of sources of social support. Although time spent walking/cycling and number of sources of social support are significantly associated with cognitive function (β = 0.06** and β = 0.03*, respectively), the inclusion of either measure in the model with grandchild caregiving does not affect the magnitude or significance of the association between caregiving and cognitive function.
Figure 2.
Association between grandchild caregiving and cognitive function, as mediated by indicators of physical and social activity, grandfathers (n = 1615). Each arrow corresponds to separate, fully adjusted models. Coefficients and confidence intervals from ordinary least squares.
Hence, results shown in Figures 1 and 2 suggest that Hypotheses 3 and 4 are not supported. We also formally tested each of the four possible mediators for both grandmothers and grandfathers using the Sobel test of mediation (Preacher & Hayes, 2004). This test confirmed that none of the hypothesized mediating factors function as mediators in the association between grandchild caregiving and cognitive function.
Discussion
This study aimed to broaden the understanding of how providing care for grandchildren may impact cognitive health among grandparents aged 40 years and older in rural South Africa. We theorized that grandparents may fare better, cognitively, when providing care to grandchildren because of the mental stimulation associated with this caregiving, via such mechanisms as physical activity and social engagement. Our results offer support for the expectation that grandchild caregiving is associated with better cognitive function. However, although grandchild caregiving is significantly associated with certain indicators of physical activity and social engagement for either grandmothers or grandfathers, and some of these indicators are further associated with cognitive function, none of the indicators we tested mediate the direct association between caregiving and cognitive function.
Research in high-income settings has speculated that less frequent caregiving might be beneficial to grandparents’ health, while more intensive caregiving might become too burdensome and detrimental to health (Arpino & Bordone, 2014; Bachman & Chase-Lansdale, 2005). However, research among smaller samples of sub-Saharan African grandparents has suggested that more intensive caregiving, which is most common in this region (Boon et al., 2010), may actually be associated with better health outcomes (Ice et al., 2010, 2011). Contrary to the more extensive work in high-income settings, but in congruence with the more limited work in sub-Saharan African settings, we find that our measure of grandchild caregiving in the past year—reflecting mostly full-time caregiving—is associated with better cognitive outcomes. One reason for the positive association that we find may be the ubiquity of grandparent caregiving in this setting. Grandparents in rural South Africa, like many parts of sub-Saharan Africa that have been impacted by HIV, may be more prepared for the caregiving role than grandparents in settings without such high death rates among the middle generation (Ice et al., 2012). Similarly, they may see this role as an obligation within the multigenerational family systems in this setting (Dolbin-MacNab & Yancura, 2018; Ice et al., 2012) and may thus be mentally prepared to take it on. As a result, their burden and stress associated with the caregiving role may be lower than in settings where such full-time care is less normative, and this may enhance their associated cognitive health outcomes.
We tested indicators of physical activity and social engagement as possible mechanisms through which grandparent caregiving is associated with cognitive function. These factors were not evidenced to mediate the association between caregiving and cognitive function. One possible explanation could be related to measurement. Although we did our best to capture physical activity (and inactivity), the survey measures we used may not accurately capture the types of activity likely to be enhanced for caregiving grandparents in this setting (i.e., steady constant motion involved in to providing care for children and running a household). Perhaps, a measure that captures this type of activity might reveal differences in physical activity levels between caregiving and non-caregiving grandparents that could help to explain cognitive benefits. Similarly, our measures of social engagement may not have captured the relevant setting-specific characteristics of this indicator. Family and other social ties are strong here, and isolation is unlikely (Dolbin-MacNab & Yancura, 2018; Schatz & Ogunmefun, 2007). A measure of social engagement via social activities and volunteering may have revealed more of a mediation effect, as other studies have found these types of engagement to positively predict cognition (Glei et al., 2005; Hughes et al., 2012).
Although we did not find physical activity or social engagement to mediate the association between caregiving and cognitive function, our stepwise analyses of mediation provided useful insight into associations between caregiving and both physical activity and social engagement, and how these associations can differ for grandmothers compared with grandfathers. Both grandmothers and grandfathers who care for their grandchildren experienced reduced social interactions with other adults, relative to their non-caregiving counterparts. However, this caregiving role is associated with greater inactivity for grandfathers (i.e., more time spent sitting), but greater activity for grandmothers (i.e., more time spent walking/cycling). Hence, grandchild caregiving may take different physical and emotional tolls on men versus women. This merits further exploration.
The main limitation of this study is its cross-sectional nature, preventing us from identifying the temporal aspects of cognitive function and caregiving. Grandparents who are healthier may be selected into caring for their grandchildren (Arpino & Bordone, 2014; Ates, 2017), and evidence from our t-tests suggest that this is the case (i.e., caregiving grandmothers were less likely to have an ADL limitation and caregiving grandfathers had lower CES-D scores than their non-caregiving counterparts). However, our multivariate results are robust to adjustment for indicators of physical and mental health. In this setting with high death rates of the middle generation, even grandparents in poor cognitive health may be forced to take on this care because there is no alternative. Another limitation is that we are unable to examine effects of caregiving on domain-specific aspects of cognitive function, as these were not measured in the HAALSI baseline data. The single measure of global cognition that we use may be less sensitive to effects of caregiving and social connectedness than a more comprehensive battery.
Overall, our findings suggest that the provision of regular care to grandchildren may be associated with better cognitive health among grandparents in this setting, and this association is similar for both grandmothers and grandfathers. This study provides some of the first evidence from a large scale survey on caregiving and cognitive health in sub-Saharan Africa, which faces a rapidly aging population and a high prevalence of grandparent fostering of children. Moreover, this study offers some of the first insight into gender differences (or lack thereof) in impacts of grandparent caregiving. As such, we can draw important conclusions that may offer benefit to other settings, especially other low- and middle-income settings that face rapid aging, and/or where grandparent care is highly intensive. Our findings suggest that policies geared toward encouraging the involvement of grandparents in their grandchildren’s lives might be beneficial for the elderly in certain settings. Of course, before implementing policy change, policymakers would benefit from longitudinal evidence to get closer to understanding whether these associations are indicative of causal links.
Supplementary Material
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funding from the National Institute on Aging for the HAALSI Study (grant number P01 AG041710). HAALSI is nested within the Agincourt Health and Demographic Surveillance System site, which is supported by the University of the Witwatersrand and Medical Research Council, South Africa, and the Wellcome Trust, UK (grant numbers 058893/Z/99/A, 069683/Z/02/ Z, 085477/Z/08/Z, 085477/B/08/Z). None of the authors have a conflict of interest.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- Andersen K, Launer LJ, Dewey ME, Letenneur L, Ott A, Copeland JRM, Dartigues JF, Kragh-Sorensen P, Baldereschi M, Brayne C, Lobo A, Martinez-Lage JM, Stijnen T, & Hofman A. (1999). Gender differences in the incidence of AD and vascular dementia: The EURODEM studies. Neurology, 53(9), 1992. [DOI] [PubMed] [Google Scholar]
- Arpino B, & Bordone V. (2014). Does grandparenting pay off? The effect of child care on grandparents’ cognitive functioning. Journal of Marriage and Family, 76(2), 337–351. [Google Scholar]
- Ates M. (2017). Does grandchild care influence grandparents’ self-rated health? Evidence from a fixed effects approach. Social Science & Medicine, 190(Supp C), 67–74. [DOI] [PubMed] [Google Scholar]
- Avila JF, Vonk JMJ, Verney SP, Witkiewitz K, Arce Rentería M, Schupf N, Mayeux R, & Manly JJ (2019). Sex/gender differences in cognitive trajectories vary as a function of race/ethnicity. Alzheimer’s & Dementia, 15(12), 1516–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachman HJ, & Chase-Lansdale PL (2005). Custodial grandmothers’ physical, mental, and economic well-being: Comparisons of primary caregivers from low-income neighborhoods*. Family Relations, 54(4), 475–487. [Google Scholar]
- Baker LA, Silverstein M, & Putney NM (2008). Grandparents raising grandchildren in the United States: Changing family forms, stagnant social policies. Journal of Societal & Social Policy, 7, 53–69. [PMC free article] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- Bengtson V. (2003). Global aging and challenges to families. Routledge. [Google Scholar]
- Blalock CL (2014). Labor migration and employment in post-apartheid rural South Africa. Sociology Graduate Theses & Dissertations. [Google Scholar]
- Bondi L. (2008). On the relational dynamics of caring: A psychotherapeutic approach to emotional and power dimensions of women’s care work. Gender, Place & Culture, 15(3), 249–265. [Google Scholar]
- Bonsang E, Adam S, & Perelman S. (2012). Does retirement affect cognitive functioning?. Journal of Health Economics, 31(3), 490–501. [DOI] [PubMed] [Google Scholar]
- Boon H, Ruiter RAC, James S, van den Borne B, Williams E, & Reddy P. (2010). Correlates of grief among older adults caring for children and grandchildren as a consequence of HIV and AIDS in South Africa. Journal of Aging and Health, 22(1), 48–67. [DOI] [PubMed] [Google Scholar]
- Bowers BF, & Myers BJ (1999). Grandmothers providing care for grandchildren: Consequences of various levels of caregiving. Family Relations, 48(3), 303–311. [Google Scholar]
- Carvalho A, Rea IM, Parimon T, & Cusack BJ (2014). Physical activity and cognitive function in individuals over 60 years of age: A systematic review. Clinical Interventions in Aging, 9, 661–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chazan MAY (2008). Seven ‘deadly’ assumptions: Unravelling the implications of HIV/AIDS among grandmothers in South Africa and beyond. Ageing and Society, 28(7), 935–958. [Google Scholar]
- Chen F, & Liu G. (2012). The health implications of grandparents caring for grandchildren in China. The Journals of Gerontology: Series B, 67B(1), 99–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark SJ, Gómez-Olivé FX, Houle B, Thorogood M, Klipstein-Grobusch K, Angotti N, Kabudula C, Williams J, Menken J, & Tollman S. (2015). Cardiometabolic disease risk and HIV status in rural South Africa: Establishing a baseline. BMC Public Health, 15(1), 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clottey EN, Scott AJ, & Alfonso ML (2015). Grandparent caregiving among rural African Americans in a community in the American South: Challenges to health and wellbeing. Rural Remote Health, 15(3), 3313. [PubMed] [Google Scholar]
- Cohen S. (2004). Social relationships and health. American Psychologist 59(8), 676–684. [DOI] [PubMed] [Google Scholar]
- Colcombe SJ, Kramer AF, Erickson KI, Scalf P, McAuley E, Cohen NJ, Webb A, Jerome GJ, Marquez DX, & Elavsky S. (2004). Cardiovascular fitness, cortical plasticity, and aging. Proceedings of the National Academy of Sciences of the United States of America, 101(9), 3316–3321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, & Oja P. (2003). International physical activity questionnaire: 12-country reliability and validity. Medicine & Science in Sports & Exercise, 35(8), 1381–1395. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, Langa KM, & Weir DR (2011). Assessment of cognition using surveys and neuropsychological assessment: The health and retirement study and the aging, demographics, and memory study. The Journals of Gerontology: Series B, 66B(suppl_1), i162–i171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delany A, Ismail Z, Graham L, & Ramkissoon Y. (2008). Review of the child support grant: Uses, implementation and obstacles. [Google Scholar]
- Dickinson WJ, Potter GG, Hybels CF, McQuoid DR, & Steffens DC (2011). Change in stress and social support as predictors of cognitive decline in older adults with and without depression. International Journal of Geriatric Psychiatry, 26(12), 1267–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolbin-MacNab ML, & Yancura LA (2018). International perspectives on grandparents raising grandchildren: Contextual considerations for advancing global discourse. The International Journal of Aging and Human Development, 86(1), 3–33. [DOI] [PubMed] [Google Scholar]
- Ertel KA, Glymour MM, & Berkman LF (2008). Effects of social integration on preserving memory function in a nationally representative US elderly population. American Journal of Public Health, 98(7), 1215–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyre RW, House T, Gómez-Olivé FX, & Griffiths FE (2018). Modelling fertility in rural South Africa with combined non-linear parametric and semi-parametric methods. Emerging Themes in Epidemiology, 15(1), 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman M, & Nkomo N. (2006). Guardianship of orphans and vulnerable children. A survey of current and prospective South African caregivers. AIDS Care, 18(4), 302–310. [DOI] [PubMed] [Google Scholar]
- Glei DA, Landau DA, Goldman N, Chuang YL, Rodriguez G, & Weinstein M. (2005). Participating in social activities helps preserve cognitive function: an analysis of a longitudinal, population-based study of the elderly. International journal of epidemiology, 34(4), 864–871. [DOI] [PubMed] [Google Scholar]
- Harling G, Payne CF, Davies JI, Gomez-Olive FX, Kahn K, Manderson L, Mateen FJ, Tollman SM, & Witham MD (2019). Impairment in activities of daily living, care receipt, and unmet needs in a middle-aged and older rural South African population: Findings from the HAALSI study. Journal of Aging and Health, 32(5–6), 296–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harling G, Perkins JM, Gómez-Olivé FX, Morris K, Wagner RG, Montana L, Kabudula CW, Bärnighausen T, Kahn K, & Berkman L. (2018). Interviewer-driven variability in social network reporting: Results from health and Aging in Africa: A longitudinal study of an INDEPTH community (HAALSI) in South Africa. Field Methods, 30(2), 140–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam C, Cruwys T, Milne M, Kan CH, & Haslam SA (2016). Group ties protect cognitive health by promoting social identification and social support. Journal of Aging and Health, 28(2), 244–266. [DOI] [PubMed] [Google Scholar]
- Hilbrand S, Coall DA, Gerstorf D, & Hertwig R. (2017). Caregiving within and beyond the family is associated with lower mortality for the caregiver: A prospective study. Evolution and Human Behavior, 38(3), 397–403. [Google Scholar]
- Hughes TF, Flatt JD, Fu B, Chang CH, & Ganguli M. (2012). Engagement in social activities and progression from mild to severe cognitive impairment: The MYHAT study. International Psychogeriatrics, 25(4), 587–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, LaPierre TA, & Luo Y. (2007). All in the family: The impact of caring for grandchildren on grandparents’ health. The Journals of Gerontology: Series B, 62(2), S108–S119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ice GH, Heh V, Yogo J, & Juma E. (2011). Caregiving, gender, and nutritional status in Nyanza Province, Kenya: Grandmothers gain, grandfathers lose. American Journal of Human Biology, 23(4), 498–508. [DOI] [PubMed] [Google Scholar]
- Ice GH, Sadruddin AFA, Vagedes A, Yogo J, & Juma E. (2012). Stress associated with caregiving: An examination of the stress process model among Kenyan Luo elders. Social Science & Medicine, 74(12), 2020–2027. [DOI] [PubMed] [Google Scholar]
- Ice GH, Yogo J, Heh V, & Juma E. (2010). The impact of caregiving on the health and well-being of Kenyan Luo grandparents. Research on Aging, 32(1), 40–66. [Google Scholar]
- Ice GH, Zidron A, & Juma E. (2008). Health and health perceptions among Kenyan grandparents. Journal of Cross-Cultural Gerontology, 23(2), 111–129. [DOI] [PubMed] [Google Scholar]
- Kabudula CW, Tollman S, Mee P, Ngobeni S, Silaule B, Gómez-Olivé FX, Collinson M, Kahn K, & Byass P. (2014). Two decades of mortality change in rural northeast South Africa. Global Health Action, 7(1), 25596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn K, Garenne ML, Collinson MA, & Tollman SM (2007). Mortality trends in a new South Africa: Hard to make a fresh start. Scandinavian Journal of Public Health, 35(−69_suppl), 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, & Guralnik JM (2010). Maximizing the potential of an aging population. JAMA, 304(17), 1944–1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi L, Farrell M, Langa K, Mahlalela N, Wagner R, & Berkman L. (2020). Incident cognitive impairment during aging in rural South Africa: Evidence from the HAALSI cohort 2014 to 2019. Innovation in Aging, 4, 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi LC, Glymour MM, Kahn K, Payne CF, Wagner RG, Montana L, Mateen FJ, Tollman SM, & Berkman LF (2017). Childhood deprivation and later-life cognitive function in a population-based study of older rural South Africans. Social Science & Medicine, 190, 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi LC, Mateen FJ, Montana L, Wagner RG, Kahn K, Tollman SM, & Berkman LF (2019). Cognitive function and impairment in older, rural South African adults: Evidence from “health and aging in Africa: A longitudinal study of an INDEPTH community in rural South Africa”. Neuroepidemiology, 52(1–2), 32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Fleur CG, & Salthouse TA (2016). Which aspects of social support are associated with which cognitive abilities for which people?. The Journals of Gerontology: Series B, 72(6), 1006–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyness SA, Lee AY, Zarow C, Teng EL, & Chui HC (2014). 10-minute delayed recall from the modified mini-mental state test predicts alzheimer’s disease pathology. Journal of Alzheimer’s Disease, 39, 575–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhavan S, & Gross M. (2013). Kin in daily routines: Time use and childrearing in rural South Africa. Journal of Comparative Family Studies, 44(2), 175–191. [PMC free article] [PubMed] [Google Scholar]
- Margherio C. (2019). Centering female agency while investigating contraceptive use: A case study in Agincourt, South Africa. International Journal for Equity in Health, 18(1), 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matovu S, Rankin S, & Wallhagen M. (2020). Ugandan Jajjas: Antecedents and rewards of caring for grandchildren in the context of HIV. International Journal of Older People Nursing, 15(2), Article e12304. [DOI] [PubMed] [Google Scholar]
- Matovu S, & Wallhagen M. (2018). Loss as experienced by Ugandan grandparent-caregivers of children affected by HIV/AIDS. Journal of Loss and Trauma, 23(6), 502–515. [PMC free article] [PubMed] [Google Scholar]
- Matovu SN, & Wallhagen MI (2020). Perceived caregiver stress, coping, and quality of life of older Ugandan grandparent-caregivers. Journal of Cross-Cultural Gerontology, 35(3), 311–328. [DOI] [PubMed] [Google Scholar]
- Mee P, Kahn K, Kabudula CW, Wagner RG, Gómez-Olivé FX, Madhavan S, Collinson MA, Tollman SM, & Byass P. (2016). The development of a localised HIV epidemic and the associated excess mortality burden in a rural area of South Africa. Global Health, Epidemiology and Genomics, 1, Article e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middleton LE, Barnes DE, Lui L, & Yaffe K. (2010). Physical activity over the life course and its association with cognitive performance and impairment in old age. Journal of the American Geriatrics Society, 58(7), 1322–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mtshali MNG (2015). The relationship between grandparents and their grandchildren in the black families in South Africa. Journal of Comparative Family Studies, 46(1), 75–83. [Google Scholar]
- Nyasani E, Sterberg E. a., & Smith H. (2009). Fostering children affected by AIDS in Richards Bay, South Africa: A qualitative study of grandparents’ experiences. African Journal of AIDS Research, 8(2), 181–192. [DOI] [PubMed] [Google Scholar]
- Oburu PO (2005). Caregiving stress and adjustment problems of Kenyan orphans raised by grandmothers. Infant and Child Development, 14(2), 199–210. [Google Scholar]
- Oburu PO, & Palmérus K. (2005). Stress related factors among primary and part-time caregiving grandmothers of Kenyan grandchildren. The International Journal of Aging and Human Development, 60(4), 273–282. [DOI] [PubMed] [Google Scholar]
- Ofstedal MB, Fisher GG, & Herzog AR (2005). Documentation of cognitive functioning measures in the health and retirement study. University of Michigan. [Google Scholar]
- Ospina-Romero M, Abdiwahab E, Kobayashi L, Filshtein T, Brenowitz WD, Mayeda ER, & Glymour MM (2019). Rate of memory change before and after cancer diagnosis. JAMA Network Open, 2(6), Article e196160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker EM, & Short SE (2009). Grandmother coresidence, maternal orphans, and school enrollment in sub-Saharan Africa. Journal of Family Issues, 30(6), 813–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PRB. (2018). World population data sheet. Population Reference Bureau. [Google Scholar]
- PRB. (2020). 2020 world population data sheet. Population Reference Bureau. [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, InstrumentsComputers, 36(4), 717–731. [DOI] [PubMed] [Google Scholar]
- Prince M, Acosta D, Chiu H, Scazufca M, & Varghese M. (2003). Dementia diagnosis in developing countries: A cross-cultural validation study. The Lancet, 361(9361), 909–917. [DOI] [PubMed] [Google Scholar]
- Rantakokko M, Manty M, & Rantanen T. (2013). Mobiltiy decline in old age. Exercise & Sport Sciences Reviews, 41(1), 19–25. [DOI] [PubMed] [Google Scholar]
- Rea IM (2017). Towards ageing well: Use it or lose it: Exercise, epigenetics and cognition. Biogerontology, 18(4), 679–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reblin M, & Uchino BN (2008). Social and emotional support and its implication for health. Current opinion in psychiatry, 21(2), 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riumallo-Herl C, Canning D, & Kabudula C. (2019). Health inequalities in the South African elderly: The importance of the measure of social-economic status. The Journal of the Economics of Ageing. 14, 100191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodakowski J, Skidmore ER, Rogers JC, & Schulz R. (2012). Role of social support in predicting caregiver burden. Archives of Physical Medicine and Rehabilitation, 93(12), 2229–2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E, & Ogunmefun C. (2007). Caring and contributing: The role of older women in rural South African multi-generational households in the HIV/AIDS Era. World Development, 35(8), 1390–1403. [Google Scholar]
- Shankar A, Hamer M, McMunn A, & Steptoe A. (2013). Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the english longitudinal study of ageing. Psychosomatic medicine, 75(2), 161–170. [DOI] [PubMed] [Google Scholar]
- Skirbekk V, Loichinger E, & Weber D. (2012). Variation in cognitive functioning as a refined approach to comparing aging across countries. Proceedings of the National Academy of Sciences, 109(3), 770–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobngwi E, Mbanya JCN, Unwin NC, Aspray TJ, & Alberti K. (2001). Development and validation of a questionnaire for the assessment of physical activity in epidemiological studies in sub-saharan Africa. International Journal of Epidemiology, 30(6), 1361–1368. [DOI] [PubMed] [Google Scholar]
- Ssengonzi R. (2007). The plight of older persons as caregivers to people infected/affected by HIV/AIDS: Evidence from Uganda. Journal of Cross-Cultural Gerontology, 22(4), 339–353. [DOI] [PubMed] [Google Scholar]
- Statistics South Africa. (2017). Survey of activities of young people, 2015. [Google Scholar]
- Stella N, & Annet N. (2019). In need of care but providers of care: Grandparents giving fulltime care to their grandchildren in rural Uganda. Anthropology Open Journal, 4(1), 1–8. [Google Scholar]
- Turvey CL, Wallace RB, & Herzog R. (2005). A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics, 11(2), 139–148. [DOI] [PubMed] [Google Scholar]
- Waldrop DP, & Weber JA (2001). From grandparent to caregiver: The stress and satisfaction of raising grandchildren. Families in Society, 82(5), 461–472. [Google Scholar]
- Zahodne LB, Glymour MM, Sparks C, Bontempo D, Dixon RA, MacDonald SWS, & Manly JJ (2011). Education does not slow cognitive decline with aging: 12-year evidence from the victoria longitudinal study. Journal of the International Neuropsychological Society: JINS, 17(6), 1039–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne LB, Nowinski CJ, Gershon RC, & Manly JJ (2014). Which psychosocial factors best predict cognitive performance in older adults?. J Int Neuropsychol Soc, 20(5), 487–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman FJ (2003). Cinderella goes to school: The effects of child fostering on school enrollment in South Africa. Journal of Human Resources, XXXVIII(3), 557–590. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.