Abstract
Background
Currently syphilis is considered an epidemic disease worldwide. The objective of this study was to identify intra-urban differentials in the occurrence of congenital and acquired syphilis and syphilis in pregnant women in the city of Natal, in northeast Brazil.
Methods
Cases of syphilis recorded by the municipal surveillance system from 1 January 2011 to 30 December 2018 were analysed. Spatial statistical analyses were performed using the kernel density estimator of the quadratic smoothing function (weighted). SaTScan software was applied for the calculation of risk based on a discrete Poisson model.
Results
There were 2163 cases of acquired syphilis, 738 cases of syphilis in pregnant women and 1279 cases of congenital syphilis. Kernel density maps showed that the occurrence of cases is more prevalent in peripheral areas and in areas with more precarious urban infrastructure. In 2011–2014 and 2015–2018, seven statistically significant clusters of acquired syphilis were identified. From 2011 to 2014, the most likely cluster had a relative risk of 3.54 (log likelihood ratio [LLR] 38 895; p<0.001) and from 2015 to 2018 the relative risk was 0.54 (LLR 69 955; p<0.001).
Conclusions
In the municipality of Natal, there was a clustered pattern of spatial distribution of syphilis, with some areas presenting greater risk for the occurrence of new cases.
Keywords: kernel density estimation, SaTScan, sociospatial inequalities in health, syphilis
Introduction
Despite the widespread publicity of the risks of sexually transmitted infections (STIs), there is still a high burden of these diseases worldwide. According to the World Health Organization (WHO), it is estimated that more than one million cases of STIs occur every day worldwide, with an average of 357 million new infections every year, including chlamydia, gonorrhoea, syphilis and trichomoniasis.1
Among STIs, syphilis stands out as a re-emerging infection caused by the bacterium Treponema pallidum of the subspecies pallidum, which can be manifested in the acquired or congenital forms and in pregnant women.2 Syphilis is a disease considered an emergency problem for both individual and public health. It causes direct morbidity, increases the risk of infection for human immunodeficiency virus (HIV) and can cause complications throughout the life of children born to infected mothers.3 Syphilis can be transmitted through sexual contact and through the transplacental route at any stage of pregnancy (ranging from 70 to 100% in the primary and secondary stages and 30% in the late and tertiary latent stages), even during the passage of the foetus through the birth canal in the presence of active lesions.2
Worldwide, >5 million new cases of syphilis are diagnosed each year, with the majority of infections occurring in low- and middle-income countries. Led by the WHO, with screening programs such as prenatal care, there has been a reduction in maternal and child mortality from syphilis by more than a third, and congenital syphilis was eliminated in at least one nation (Cuba). In higher-income countries the infection is less common and occurs disproportionately in people living in poverty, people with poor access to healthcare and in ethnic and sexual minorities.4
Syphilis infection is a common problem in low- and middle-income countries, being a substantial source of morbidity, including adverse pregnancy outcomes and accelerated HIV transmission.5 In Western Europe and the Americas, the rates of this disease have dramatically increased again, with periodic fluctuation trends, occurring disproportionately in pregnant women and in men who have sex with other men (MSM), challenging public health professionals to reinforce control measures.6
From this perspective, it is observed that syphilis is a re-emerging infection also in developed countries, as in the case of Italy and the USA. In Latin America, Africa and Asia, its incidence remains high and the control focuses on prenatal care, which calls attention to the need for screening of all pregnant women during prenatal care and timely treatment in order to control congenital infection.7
In Brazil, there has been a considerable increase in syphilis among pregnant women and congenital syphilis cases in the last decade. In 2018, the detection rate of syphilis in pregnant women in Brazil was 21.4 per 1000 live births, the incidence of congenital syphilis was 9.0 per 1000 live births and the mortality rate for congenital syphilis was 8.2 per 100 000 live births. These increases were attributed in part to increases in testing coverage, the use of rapid tests, unprotected sex and resistance of primary healthcare professionals to administer penicillin. In addition to these factors, the use of a surveillance system may reflect the increase in reported cases, considering that acquired syphilis is a condition of compulsory notification since 2010.1,8
Some studies have shown that the incidence of syphilis is higher in populations with lower socio-economic status, including areas with less educational attainment, higher concentrations of socio-economically disadvantaged minorities and impoverished living conditions.9–11 The area covered in the present study, located in the northeast region of Brazil, reveals a high degree of inequality expressed both in the economic dimension and in relation to access to public services, education and housing.12 The precarious access to health services in this region may be associated with the characteristics of the health system, the socio-economic level of the population, education, cultural aspects, geographical characteristics and belonging to specific groups.13,14 These characteristics are highly prominent in this area and provide the conditions for the occurrence of diseases because of the convergence of processes related to health, living conditions and environment.10
Studies on syphilis in Brazil have described different scenarios and associated factors, which combined with other results, may contribute to a better understanding of the disease.10 However, few studies have considered the spatial behaviour of the disease and its geographical relationship with extrinsic factors and potential application in the management of health services. Studies of spatial analysis using information from morbidity indicators contribute to the analysis of socio-environmental risks and to the identification of the most vulnerable areas for the occurrence of diseases of great relevance, with a view to making decisions and implementing measures before the factors predisposing to their occurrence.15
Knowing that syphilis is still a highly prevalent infection and that Brazil is currently experiencing an epidemic, this study aimed to identify intra-urban differentials in the occurrence of congenital and acquired syphilis and syphilis in pregnant women in an urban area in northeastern Brazil.
Methods
This study was carried out in the city of Natal, capital of the state of Rio Grande do Norte, located in the northeast of Brazil (latitude 05°47′42′′S, longitude 35°12′34′′W), 38 m above sea level and with a Human Development Index of 0.763. According to population projections by the Brazilian Institute of Geography and Statistics, the population projected for the study area for the year 2017 was 884 626 inhabitants, of which 47.56% were men and 52.43% were women, occupying 171.15 km2 of urban area.16
This is a retrospective study using records of congenital and acquired syphilis and syphilis in pregnant women from the epidemiological surveillance system of the municipality of Natal for an 8-y period from 1 January 2011 to 31 December 2018. The data came from reports of cases of syphilis in health institutions of the Municipal Health Secretariat registered in the Disease Notification System.
Health institutions register syphilis cases according to the requirements of the Ministry of Health of Brazil. Acquired syphilis is defined as symptomatic or non-symptomatic disease with a reactive treponemal or non-treponemal test at any titration. Congenital syphilis is defined as occurring in the following situations: newborn, stillbirth or abortion in a woman with syphilis not treated or treated inappropriately or with microbiological evidence of infection by Treponema pallidum. Every individual <13 y of age with the following serological evidence is considered to have syphilis: ascending titres (non-treponemal tests) and/or reactive non-treponemal tests after 6 months of age (except in the case of therapeutic follow-up) and/or reactive treponemal tests after 18 months of age and/or non-treponemal test titration higher than that of the mother or an individual <13 y of age with reactive non-treponemal test and clinical or cerebrospinal fluid or radiological evidence of congenital syphilis. Syphilis in pregnant women is indicated in any symptomatic or asymptomatic woman who during prenatal care, delivery and/or puerperium presents at least one reactive treponemal or non-treponemal test at any titration, regardless of syphilis symptomatology and previous treatment.17
Population data by census tract were used as the population at risk to calculate the annual incidence rate. To calculate the detection rate of acquired syphilis, the number of cases of acquired syphilis in individuals ≥13 y of age was considered in relation to the total resident population. For this calculation, the population considered for the period from 2011 to 2014 was the population of 2010 and the population projection for the year 2017 was considered for the period from 2015 to 2018. Because there is no information on the number of live births at the census tract level, it was decided not to carry out this analysis for syphilis in pregnant women and congenital syphilis.
Population data and the map of polygons at the census tract level were obtained from the Brazilian Institute of Geography and Statistics (2018).
All cases were geocoded using a geographic information system (GIS) and cases that did not correspond to the street level for geolocation were excluded from the analysis.
Spatial statistical analyses through the kernel density estimator were performed to estimate the densities of the events within the study area. The quadratic smoothing function (weighted) with 100, 200 and 300 m of bandwidth and a regular grid composed of 500×322 cells were used in the present is study. The intensity kernel descriptor allows estimating the number of events per unit area in each cell of a regular grid covering the studied region. This non-parametric technique not only estimates the intensity of the occurrence of cases across the analysed surface, but also allows filtering the variability of a data set at the same time it retains its main local characteristics.18
SaTScan software version 9.6 (March 2018) was used to verify the excess risk for the occurrence of syphilis cases using a spatial retrospective analysis based on a discrete Poisson model [Cz ∼ Poisson (λz=pnz)]. This discrete scan statistic considers the number of cases Cz as a random variable whose parameter λz represents the expected number of bm under the unknown H0 (null hypothesis), where the number of expected cases is equal to the total number of ‘observed observations’ multiplied by the size of the scanning window divided by the size of the total study area.
This scan statistic described by Kulldorff19 considers the distribution and the statistical significance of the clusters through a Monte Carlo test with 999 permutations, guaranteeing adequate power to define the clusters, with an α significance level <0.05 to test if the cluster was significant. The maximum cluster size is defined as 50% of the population at risk. In the present study, the number of syphilis cases per census tract from 2011–2014 and 2015–2018 was used as a case file, the population of the sector (2010 and 2017) was used as the population file and the latitude and longitude of the centroid of each sector were used as the coordinate file. The distribution of excess risk was described using the standard morbidity ratio (relative risk [RR]), which was calculated as the ratio of observed cases to the expected cases in each census tract, considering that the spatial locations of all cases are independent. The model was adjusted to purely spatial groupings. From this analysis, the geographical coordinates and the RRs with their statistical significance were identified.
Statistical analyses were performed using Excel (Microsoft, Redmond, WA, USA), SaTScan and Quantum GIS version 2.18.2 Las Palmas (QGIS Development Team, 2015). The Excel spreadsheet was used to organize the data, excess risk was analysed using the SaTScan software and the kernel density and the maps were produced in QGIS 2.18.2.
Results
A total of 2163 cases of acquired syphilis, 738 cases of syphilis in pregnant women and 1279 cases of congenital syphilis were reported to the epidemiological surveillance system from 2011 to 2018. For acquired syphilis, the mean age of the cases was 31 years (29 y for women and 33 y for men), with 50.5% of cases occurring in females and 53.8% in black individuals. In the case of syphilis in pregnant women, the mean age was 24 y, with 66.6% of cases occurring in black women.
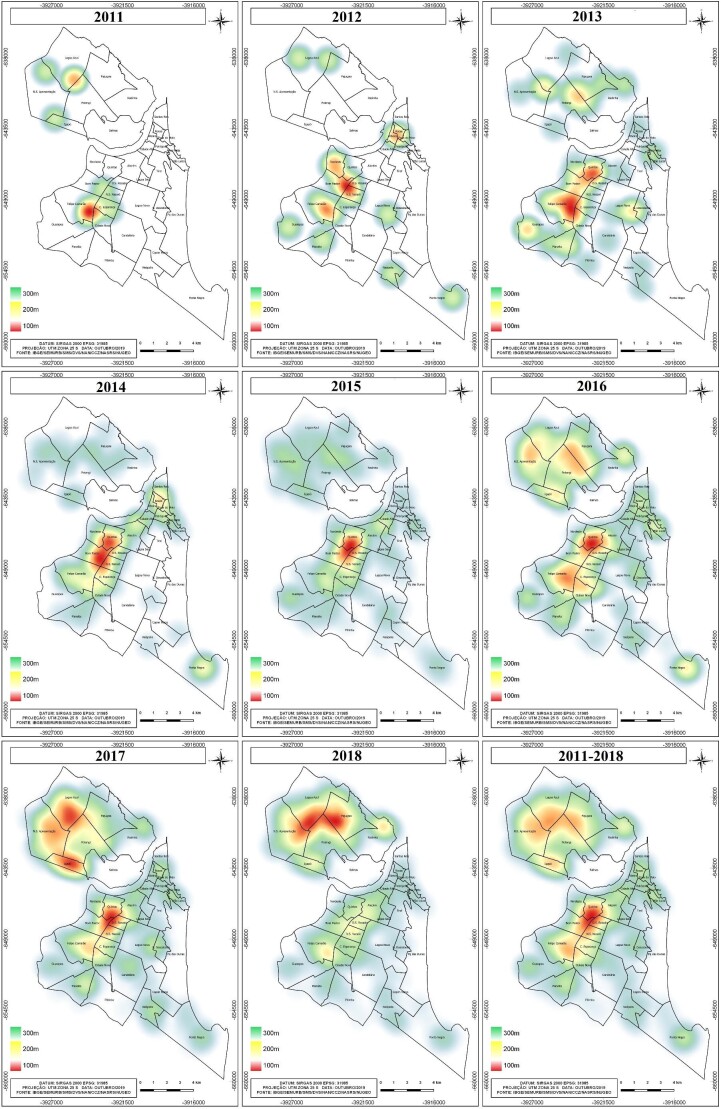
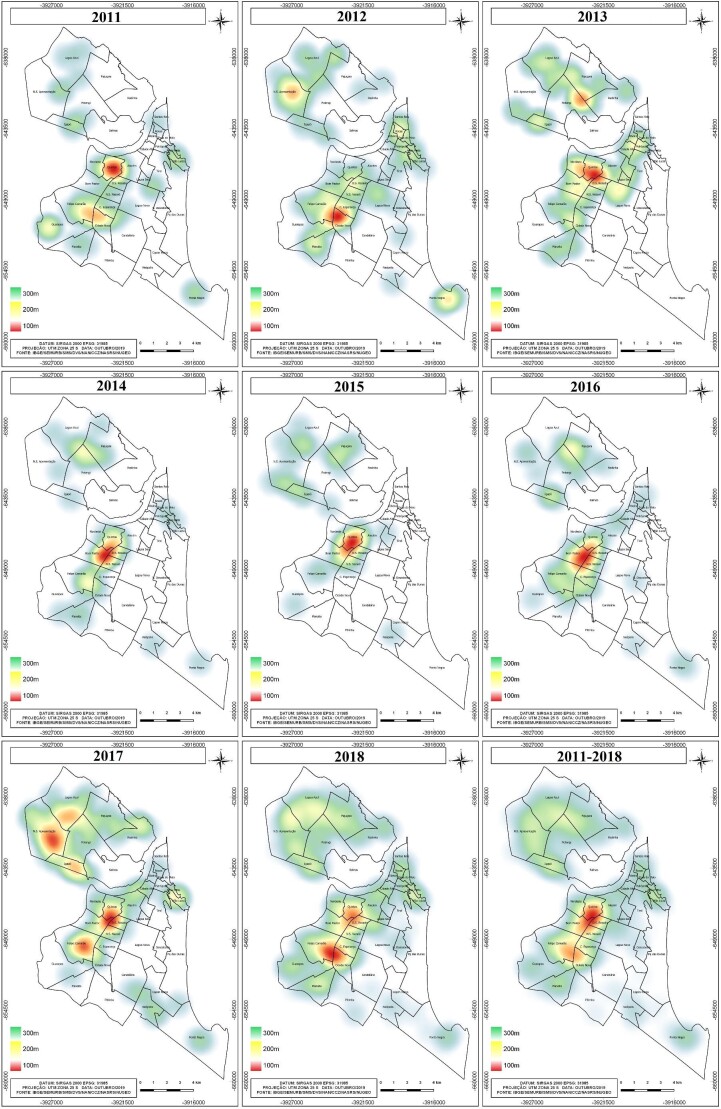
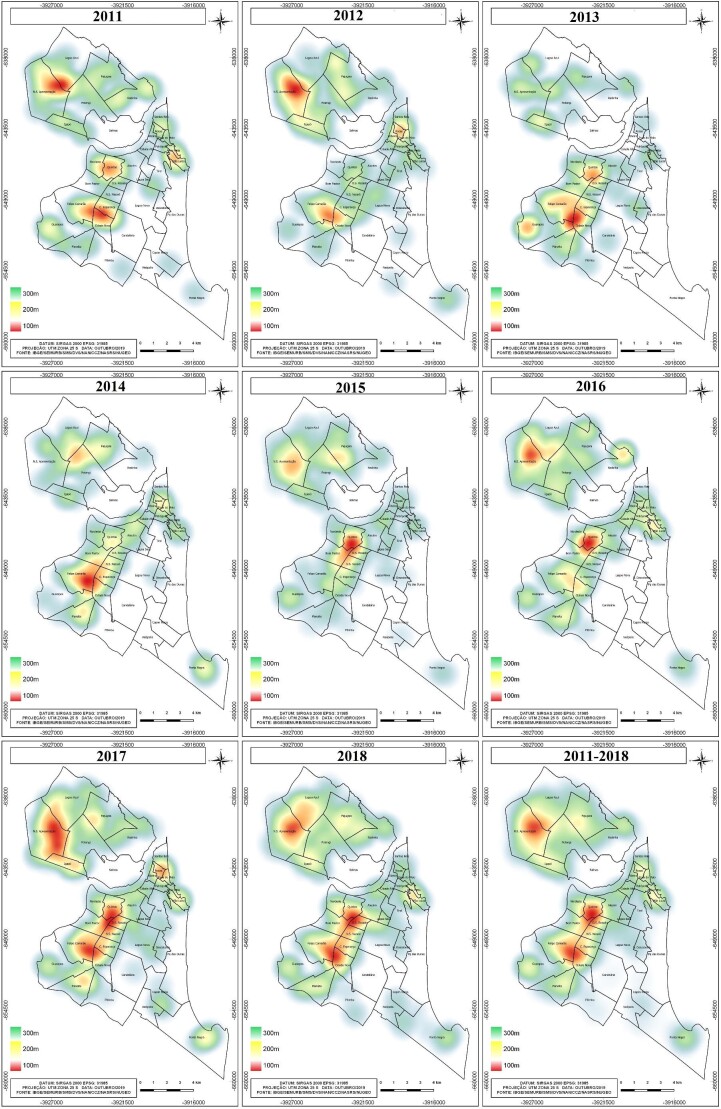
Kernel density maps showed that the occurrence of cases was more prevalent in peripheral areas, especially in areas located in the north and west regions of the city, with some persistent points of occurrence over the years. There was a concomitance of areas with the highest density of cases of acquired syphilis (Figures 1), in pregnant women (Figures 2) and congenital syphilis (Figures 3).
Figure 1.
Kernel density map for cases of syphilis acquired in the city of Natal, Rio Grande do Norte, Brazil: annual and accumulated distribution for the period 2011–2018.
Figure 2.
Kernel density map for syphilis cases in pregnant women in the city of Natal, Rio Grande do Norte, Brazil: annual and accumulated distribution for the period 2011–2018.
Figure 3.
Kernel density map for cases of congenital syphilis in the city of Natal, Rio Grande do Norte, Brazil: annual and accumulated distribution for the period 2011–2018.
The excess risk map showed the distribution of the RR and the areas that did not form clusters. The spatial pattern of syphilis was considered non-random. For acquired syphilis, seven statistically significant clusters were identified in the period 2011–2014 and seven in the period 2015–2018. The light pink areas presented a lower risk than expected, as indicated by the excess risk of values <1 (Figure 4). On the other hand, the orange and red areas showed higher-than-expected values or excess risk (>1). The census tracts with excessive risk were located in the peripheral areas of the north and west districts of the city.
For acquired syphilis, in the period 2011–2014, the most likely cluster had a relative risk of 3.54 (p<0.001) and a log likelihood ratio of 38.895 074, with a window base diameter of 3.01 km. The cluster window was centred at 5.811 188 S, 35.254 226 W. For the 2015–2018 period, the most likely cluster had a relative risk of 0.54 (p<0.001) and a log likelihood ratio of 69.955 548, with a window base diameter of 12 km. The cluster window was centred at 5.897 198 S, 35.162 987 W. The description of the clusters is listed in Table 1.
Table 1.
Spatial clusters statistically significant for the occurrence of syphilis acquired in the municipality of Natal in the periods 2011–2014 and 2015–2018
| Cluster | Population | Coordinates/radius | Observeda | Expectedb | RR | LLR | p-Value |
|---|---|---|---|---|---|---|---|
| 2011–2014 | |||||||
| 1 | 147 239 | (5.811 188 S, 35.254 226 W)/3.01 km | 97 | 40.15 | 3.54 | 38.895 074 | <0.001 |
| 2 | 118 770 | (5.806 588 S, 35.250 154 W)/2.55 km | 81 | 32.39 | 3.38 | 32.606 713 | <0.001 |
| 3 | 168 187 | (5.830 921 S, 35.188 606 W)/4.64 km | 14 | 45.86 | 0.26 | 18.016 481 | <0.001 |
| 4 | 266 154 | (5.729 634 S, 35.279 379 W)/5.29 km | 34 | 72.58 | 0.37 | 17.480 579 | <0.001 |
| 5 | 97 935 | (5.807 158 S, 35.207 299 W)/2.18 km | 4 | 26.71 | 0.13 | 16.401 575 | <0.001 |
| 6 | 117 339 | (5.769 705 S, 35.263 225 W)/2.85 km | 8 | 32.00 | 0.22 | 14.384 601 | <0.001 |
| 7 | 105 743 | (5.867 310 S, 35.214 250 W)/4.02 km | 8 | 28.83 | 0.25 | 11.679 087 | 0.010 |
| 2015–2018 | |||||||
| 1 | 307 784 | (5.897 198 S, 35.162 987 W)/12.00 km | 437 | 676.72 | 0.54 | 69.955 548 | <0.001 |
| 2 | 441 129 | (5.761 811 S, 35.259 347 W)/6.25 km | 1224 | 969.90 | 1.71 | 67.139 405 | <0.001 |
| 3 | 167 027 | (5.854 170 S, 35.206 499 W)/4.43 km | 195 | 367.24 | 0.48 | 57.877 136 | <0.001 |
| 4 | 164 327 | (5.789 125 S, 35.243 941 W)/3.69 km | 510 | 361.30 | 1.56 | 34.308 087 | <0.001 |
| 5 | 74 272 | (5.742 760 S, 35.253 512 W)/1.41 km | 260 | 163.30 | 1.68 | 26.897 320 | <0.001 |
| 6 | 8 015 | (5.744 758 S, 35.206 318 W)/0.97 km | 52 | 17.62 | 3.00 | 22.198 747 | <0.001 |
| 7 | 33 333 | (5.799 787 S, 35.199 903 W)/1.38 km | 27 | 73.29 | 0.36 | 19.894 736 | <0.001 |
LLR: log likelihood ratio.
Number of observed cases in a cluster.
Number of expected cases in a cluster.
Discussion
The present study identified intra-urban differentials of congenital and acquired syphilis and syphilis in pregnant women in the analysed area. The spatial pattern of syphilis was considered non-random, with the formation of areas of high density of cases and areas of greater risk in the peripheral areas of Natal, particularly in the western and northern districts of the city. Furthermore, a gradual increase in the number of syphilis cases was observed over the study period.
According to the Ministry of Health, acquired syphilis has obtained greater relevance in terms of reports in Brazil. In the period from 2017 to 2018 in the northeast of the country, the detection rate went from 27.4 to 46.9 per 100 000 inhabitants.8 According to data from the Municipal Department of Health of Natal, in a period shorter than this study, between 2014 and 2017, 685 cases of congenital syphilis and 250 cases of syphilis in pregnant women were identified by the Disease Notification System. In 2014, the detection rate was 12.1 cases for every 1000 live births and in 2017 it was 14.4 cases for every 1000 births.20 This information and the findings of the present study confirm the increasing trend in the number of syphilis cases observed in Brazil.
Some studies have confirmed the increase in the number of cases in different regions of Brazil, namely, in the states of Amazonas, Ceará, Espírito Santo, Rio de Janeiro, Rio Grande do Sul and the Federal District21 and in Palmas.22 This trend is also evident at the international level, as observed in the USA, where an increase from 0.9 cases of primary and secondary syphilis infection per 100 000 women to 1.9 cases per 100 000 women was registered in the period from 2012 to 2016. The rate of congenital syphilis also increased, from 8.4 cases per 100 000 live births to 15.7 cases per 100 000 live births.23
Given this scenario, the Ministry of Health and the Pan American Health Organization signed an agreement in which the goal for 2015 was to reduce this incidence to 0.5 cases per every 1000 live births.24 However, it is noticeable that the incidence found in Brazil and its different states is not only above the target, but is also higher than the rates observed in other countries.
From this perspective, the Ministry of Health of Brazil developed an agenda of strategic actions to reduce syphilis. This document presented a renewal of actions, also expanding the commitment to new partnerships and the inclusion of joint actions with the interministerial strategy of rapid response to syphilis in health care networks, with the objective of reducing acquired syphilis, syphilis in pregnant women and congenital syphilis in Brazil. The implementation was coordinated by the Department of Surveillance, Prevention and Control of STIs, HIV/AIDS and Viral Hepatitis (DIAHV/SVS/MS) for execution in 2018–2019. In this agenda, six lines of action for reducing syphilis were established: rapid response to syphilis in health care networks; educational communication; qualification of strategic information; strengthening of the partnership between the Ministry of Health and other actors; expansion of the committees of vertical transmission of HIV, syphilis and viral hepatitis; and strengthening of health care networks.17
Despite numerous attempts to reduce the incidence of the disease, there is a need for actions on the part of health professionals to promote better screening, control of cases of the disease from an effective active search, correct treatment of sexual partners and notification of cases.25
The profile of women with syphilis in the municipality of Natal is mainly composed of young black women. This profile was demonstrated in studies where African Americans were the majority in cases of gestational syphilis and congenital syphilis.26,27 In addition, the Epidemiological Bulletin of Syphilis, published in 2018, indicates that the most affected population group is women, mainly black and young women ages 20–29 y, who account for 14.4% of all cases of acquired syphilis and syphilis in pregnant women.28
The increase in cases among young women is especially worrying, being directly associated with the conditions of vulnerability to which they are subjected. In the period from 2012 to 2016, Japan faced a resurgence of syphilis, registering >4000 cases in 2016.28 The authors explained that the recurrence was mainly due to the increase in sexual relations between men, and between men and women, where women ages 20–24 y are at high risk of contracting an STI. The authors also said that there is special concern about the transmission of syphilis from mother to child, requiring prevention strategies directed at young women, mainly because they correspond to a population in which many are still in full reproductive capacity.
The results of the present study demonstrated that high kernel density zones of cases of acquired syphilis, congenital syphilis and syphilis in pregnant women were concentrated in peripheral areas. These regions are characterized by marked precariousness of socio-economic conditions that substantially determine the health situation of this population, making them vulnerable.
This study shows that the process of formation of these vulnerable areas is directly related to the metropolitan expansion of the city of Natal, with the emergence of a rich region in the south and a poor region in the north.29 This perspective is corroborated by the analysis carried out by Araújo and Cândido,30 who researched the quality of life in the neighbourhoods of Natal, using indicators of socio-economic conditions and urban and environmental infrastructure, and found that the neighbourhoods with the lowest quality of life were the ones evidenced in the present study.
Using SaTScan software, it was possible to see the distribution of the RR of the census tracts from the formation of clusters, showing an increase in the risk areas in the municipality between the first and second period. It was possible to identify that the greatest risks were concentrated in the peripheral areas in north and west Natal, areas characterized by a high population density. In addition, a study carried out using the same geographic base of census sectors in Natal observed that these areas are the ones with the most socially vulnerable neighbourhoods, as assessed by the density of people per household, precarious income and greater precariousness in urban infrastructure.31 Such factors can be associated with a low level of education and limited access to health services, which hinders early recognition of the disease and immediate treatment, consequently increasing the risk of spread.
It should also be noted that the profile of individuals with a less favoured socio-economic condition and with less access to quality healthcare becomes a potential factor for the presence of STIs. However, it cannot be said that syphilis is a risk condition exclusively of poorer populations. On the contrary, regardless of social or economic condition, every person can acquire the infection; however, the risk is greater in more vulnerable populations.32 It is important to note that other factors may be associated with the epidemic, such as cultural and behavioural aspects.33
In addition to the factors listed, it is also necessary to highlight the low coverage of primary healthcare in the municipality of Natal. Neves et al.34 evaluated the time trends in the coverage of the Family Health Strategy (FHS) in the regions of Brazil and Federation Units in the period from 2006 to 2016 and observed that in Natal, the FHS coverage remained stable through the entire historical series. The authors explain that this pattern may occur due to fluctuations in coverage from year to year, not showing an increase progression over time.
There are districts where the existing health units are not in line with the demographic growth of each region of the city. This factor directly reflects the access to health services and the work process of the active teams and the scarcity of equipment and human resources. It can be said that there is an insufficient number of health units in the municipality, given the needs and demands of each territory, which results in a significant number of people with precarious access to these services.35
In this work we sought to identify the spatial distribution pattern and analyse the risk areas for congenital and acquired syphilis and syphilis in pregnant women in the municipality of Natal, capital of the state of Rio Grande do Norte. The results showed statistical evidence of spatial clusters, with a pattern formed in the most precarious and vulnerable areas of the city, which makes them sites of potential risk for transmission of this infection. Thus it is necessary to emphasize the need to implement strategies to reduce the incidence in these areas so that early diagnosis and treatment can be guaranteed.
With respect to early diagnosis, it is should be noted that the rapid syphilis test makes it possible to diagnose individuals efficiently and at low cost. The results found suggest that strategic actions must be carried out in these areas in order to guarantee broad access of the population to rapid testing services, in addition to priority actions and those already recommended by the Ministry of Health for realization of the rapid test in pregnant women.
In addition, the advanced spatial statistical methods used in the present study are complementary tools for the epidemiological surveillance of infectious diseases to guide prevention and control efforts. Thus the analysis of surveillance data using these techniques provides useful information for public health planners in decision making, as it allows the appropriate allocation of scarce health resources in developing countries in order to implement specific and more effective interventions.
When using data from secondary sources, we assume the risks of the limits imposed by the database that are due to the technical and operational conditions of municipal epidemiological surveillance in the production of data on cases of syphilis, often contributing to underreporting of cases. It should be noted that failure to fill in some fields on the form, especially with regard to the item race/skin colour, is also characterized as a limitation of the study, considering that the absence of this type of information makes it difficult to carry out different analyses and consequently limits information about the health conditions of certain population groups.
Although some limitations have been identified, it should be noted that considerable improvements have been achieved in recent years in the quality of the information system in Brazil,36 especially in the last decade, generating considerable success. It is important to highlight that there was no reporting bias and therefore the results of this study allow a description of the epidemiological situation of syphilis in the city of Natal.
Acknowledgements
This study was supported by Coordination of Superior Level Staff Improvement (CAPES) with a postdoctoral scholarship for AAM (process 88887.372306/2019-00) and by the Federal University of Mato Grosso do Sul. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Contributor Information
Talita Araujo de Souza, Health Sciences Postgraduate Program, Federal University Of Rio Grande do Norte, Natal, Rio Grande do Norte 59056-150, Brazil.
Karen Kaline Teixeira, Health Surveillance Department, Municipal Health Secretary, Natal, Rio Grande do Norte 59025-090, Brazil.
Reginaldo Lopes Santana, Health Surveillance Department, Municipal Health Secretary, Natal, Rio Grande do Norte 59025-090, Brazil.
Cinthia Barros Penha, Health Surveillance Department, Municipal Health Secretary, Natal, Rio Grande do Norte 59025-090, Brazil.
Arthur de Almeida Medeiros, Integrated Health Institute, Federal University of Mato Grosso do Sul, Campo Grande 79070-900, Brazil; Public Health Postgraduate Program, Federal University of Rio Grande do Norte, Natal, Rio Grande do Norte 59056-000, Brazil.
Kenio Costa de Lima, Public Health Postgraduate Program, Federal University of Rio Grande do Norte, Natal, Rio Grande do Norte 59056-000, Brazil.
Isabelle Ribeiro Barbosa, Public Health Postgraduate Program, Federal University of Rio Grande do Norte, Natal, Rio Grande do Norte 59056-000, Brazil.
Author’s contributions
IRB, KKT, RLS and CBP conceived of the study and compiled the data used in the analyses. IRB, TAS and AAM conducted analyses and drafted the manuscript. IRB, TAS, KKT, RLS, CBP, AAM and KCL assisted with interpretation of the data and provided feedback for the manuscript. All authors read and approved the final manuscript.
Funding
This research was funded by the Ministry of Health and the Laboratório de Inovação Tecnológica em Saúde (LAIS/HUOL/UFRN), Project: ‘Syphilis No.’ TED 54/2017.
Competing interests
None declared.
Ethical approval
Not required.
Data availability
All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Kennedy T, Jones R. Effect of obesity on esophageal transit. Am J Surg. 1985;149(1):177–81. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Orientaciones mundiales sobre los criterios y procesos para la validación de la eliminación de la transmisión maternoinfantil del VIH y la sífilis. Geneva: World Health Organization; 2015. [Google Scholar]
- 3.Peeling RW, Mabey D, Kamb MLet al. Syphilis. Nat Rev Dis Primers. 2017;3:17073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forrestel AK, Kovarik CL, Katz KA. Sexually acquired syphilis: Laboratory diagnosis, management, and prevention. J Am Acad Dermatol. 2020 Jan;82(1):17–28. [DOI] [PubMed] [Google Scholar]
- 5.Hook EW 3rd. Syphilis. Lancet. 2017;389(10078):1550–7. [DOI] [PubMed] [Google Scholar]
- 6.Newman L, Rowley J, Vander Hoorn Set al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015;10(12):e0143304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . Report on Global Sexually Transmitted Infection Surveillance 2015. Geneva: World Health Organization; 2016. [Google Scholar]
- 8.Lafetá KRG, Martelli Júnior H, Silveira MFet al. Sífilis materna e congênita, subnotificação e difícil controle. Rev Bras Epidemiol. 2016;19(1):63–74. [DOI] [PubMed] [Google Scholar]
- 9.Brasil Ministério da Saúde . Boletim Epidemiológico. Sífilis. Brasília: Ministério da Saúde; 2019. [Google Scholar]
- 10.Araújo CL, Shimizu HE, Sousa AIAet al. Incidência da sífilis congênita no Brasil e sua relação com a Estratégia Saúde da Família. Rev Saúde Pública. 2012;46(3):479–86. [DOI] [PubMed] [Google Scholar]
- 11.Reis GJD, Barcellos C, Pedroso MDMet al. Diferenciais intraurbanos da sífilis congênita: análise preditiva por bairros do Município do Rio de Janeiro, Brasil. Cad Saúde Pública. 2018;34(9):00105517. [DOI] [PubMed] [Google Scholar]
- 12.Macêdo VCD, Lira PICD, Frias PGDet al. Fatores de risco para sífilis em mulheres: estudo caso-controle. Rev Saúde Pública. 2017;51:78.28832758 [Google Scholar]
- 13.Arantes LJ, Shimizu HE, Merchán-Hamann E. Contribuições e desafios da Estratégia Saúde da Família na Atenção Primária à Saúde no Brasil: revisão da literatura. Cien Saud Colet. 2016;21(5):1499–10. [DOI] [PubMed] [Google Scholar]
- 14.Pavão ALB, Coeli CM, Lopes CSet al. Uso de serviços de saúde segundo posição socioeconômica em trabalhadores de uma universidade pública. Rev Saúde Pública. 2012;46(1):98–103.22218759 [Google Scholar]
- 15.Botelho FC, França Junior I. Como a atenção primária à saúde pode fortalecer a alimentação adequada enquanto direito na América Latina? Rev Panam Salud Publica. 2018;42:e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barbosa IR, Pereira LMS, Medeiros PFDMet al. Análise da distribuição espacial da tuberculose na região Nordeste do Brasil, 2005–2010. Epidemiol Serv Saúde. 2013;22(4):687–5. [Google Scholar]
- 17.Instituto Brasileiro de Geografia e Estatística . Malhas de Setores Censitários - Divisões Intramunicipais, Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2018. [Google Scholar]
- 18.Brasil Ministério da Saúde . Agenda de ações estratégicas para redução da sífilis no Brasil. Brasília: Ministério da Saúde; 2017. [Google Scholar]
- 19.Silverman BW.Density estimation. New York: Chapman & Hall; 1986. [Google Scholar]
- 20.Kulldorff M.A spatial scan statistic. Comm Stat Theor Meth. 1997;26(6):1481–6. [Google Scholar]
- 21.Prefeitura de Natal . Secretaria Municipal de Saúde. Plano Municipal de Saúde. 2018–21. [Google Scholar]
- 22.Saraceni V, Pereira GFM, Silveira MFet al. Vigilância epidemiológica da transmissão vertical da sífilis: dados de seis unidades federativas no Brasil. Rev Panam Salud Publica. 2017;41:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cavalcante PADM, Pereira RBDL, Castro JGD.. Sífilis gestacional e congênita em Palmas, Tocantins, 2007–2014. Epidemiol Serv Saúde. 2017;26(2):255–4. [DOI] [PubMed] [Google Scholar]
- 24.Fan SR, Wang AL, Wang LH.. Elimination of mother-to-child transmission of syphilis: challenge and solution. Matern Fetal Med. 2019;1(2):95–104. [Google Scholar]
- 25.Pan American Health Organization .Análisis de la situación al año 2010: eliminación de la transmisión materno infantil del VIH y de la sífilis congénita en la Región de las Américas. Washington, DC: Pan American Health Organization; 2012. [Google Scholar]
- 26.Oliveira DR, Figueiredo MSN.. Abordagem conceitual sobre a sífilis na gestação e o tratamento de parceiros sexuais. Enfermagem Foco. 2011;2(2):108–11. [Google Scholar]
- 27.Matthias JM, Rahman MM, Newman DRet al. Effectiveness of prenatal screening and treatment to prevent congenital syphilis, Louisiana and Florida, 2013–2014. Sex Transm Dis. 2017;44(8):498–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DiOrio D, Kroeger K, Ross A.. Social vulnerability in congenital syphilis case mothers: qualitative assessment of cases in Indiana, 2014 to 2016. Sex Transm Dis. 2018;45(7):447–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takahashi T, Arima Y, Yamagishi Tet al. Rapid increase in reports of syphilis associated with men who have sex with women and women who have sex with men, japan, 2012 to 2016. Sex Transm Dis. 2018;45(3):139–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Silva AFC, Bastos NSM.. Novas (e velhas) fronteiras: os espaços de pobreza e a expansão da cidade de Natal-RN. Anais Encontros Nacionais da ANPUR. 2013;10:1–2. [Google Scholar]
- 31.Araújo MCC, Cândido GA.. Índices de qualidade de vida urbana de Natal-RN. Geoconexões. 2015;1:51–66. [Google Scholar]
- 32.Barbosa IR, Gonçalves RCB, Santana RL.. Mapa da vulnerabilidade social do município de Natal-RN em nível de setor censitário. J Hum Growth Dev. 2019;29(1):48–6. [Google Scholar]
- 33.Rufino EC, Andrade SSC, Leadebal ODCPet al. Women's knowledge about STI/Aids: working with health education. Cienc Cuid Saúde. 2016;15:304–11. [Google Scholar]
- 34.Kuchenbecker R, Grangeiro A, Veras MA.. Global targets, local epidemics: the ultimate challenge for aids in Brazil? Rev Bras Epidemiol. 2015;18(Suppl 1):5–9. [DOI] [PubMed] [Google Scholar]
- 35.Neves RG, Flores TR, Duro SMSet al. Tendência temporal da cobertura da Estratégia Saúde da Família no Brasil, regiões e Unidades da Federação, 2006–2016. Epidemiol Serv Saude. 2018;27(3):e2017170. [DOI] [PubMed] [Google Scholar]
- 36.Hoffmann E, Carvalho TKF, Oliveira FMM.. Atenção Primária à Saúde em Natal (RN): particularidades das ações e dos serviços. Argumentum. 2015;7(2):178–93. [Google Scholar]
- 37.Tiago ZDS, Picoli RP, Graeff SVBet al. Subnotificação de sífilis em gestantes, congênita e adquirida entre povos indígenas em Mato Grosso do Sul, 2011–2014. Epidemiol Serv Saude. 2017;26(3):503–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.