Abstract
Patients with bidirectional patellar instability who are unresponsive to conservative management may benefit from a medial patellofemoral ligament (MPFL) reconstruction and lateral patellofemoral ligament (LPFL) reconstruction. If an isolated MPFL reconstruction does not provide adequate stabilization intraoperatively, combined MPFL and LPFL reconstruction allows independent reconstruction, which can be performed with a facile, reproducible technique. The purpose of this report was to describe our technique for performing an MPFL reconstruction with a concurrent soft-tissue LPFL reconstruction combined with a distalizing tibial tubercle osteotomy to correct patella alta.
Technique Video
This video is a narrated step-by-step approach to performing a concomitant MPFL and LPFL reconstruction. The MPFL reconstruction is performed first via an osseous based approach with graft fixation with 2 PEEK SutureTak anchors along the medial aspect of the patella and an interference screw in the femur. After this, a soft tissue–based LPFL is performed by making incisions in the iliotibial band, quadriceps tendon, and patellar tendon, looping the graft through these and suturing it down. (LPFL, lateral patellofemoral ligament; MPFL, medial patellofemoral ligament.)
Introduction
Lateral patellar instability is a common orthopaedic pathology, comprising 2% to 3% of all knee injuries, and most commonly affects young, female patients.1, 2, 3 The medial patellofemoral ligament (MPFL) and lateral patellofemoral ligament (LPFL) act in conjunction to provide lateral and medial patellar restraint, particularly in the first 20° of flexion.4 Historically, lateral retinacular release (LRR) has been used to remove an overly tight lateral retinaculum in isolation or in conjunction with an MPFL repair or reconstruction to treat lateral patellar instability.1
Unfortunately, LRRs have been associated with a high rate of iatrogenic medial instability—occurring in up to 57% of patients—and also can increase lateral patellar displacement due to the synergistic contributions of the LPFL and MPFL in restraining the patella.5, 6, 7 In this setting, it may be necessary to perform a lateral-sided reconstruction. While a range of techniques have been described resulting in good outcomes, our preference is to perform a soft tissue–based LPFL reconstruction.8, 9, 10 Due to the paucity of literature as well as the varied anatomical descriptions, for the purposes of discussion in this manuscript, the term LPFL reconstruction will refer to any augmentation technique of the lateral retinaculum to treat medial patellar instability.
In a patient with recurrent lateral and medial instability who is nonresponsive to conservative management with a brace worn as a medal and then as a lateral stabilizer, it may be necessary to reconstruct both the medial and lateral patellar restraints concurrently if an isolated MPFL reconstruction does not provide adequate stabilization intraoperatively and the lateral retinacular tissue quality is too poor to repair. In addition, any aberrant anatomy associated with patellar instability, such as an increased Caton–Deschamp Index greater than 1.2 or tibial tubercle–trochlea groove distance greater than 20 mm, should be evaluated to mitigate the risk of postoperative redislocation.11,12 The purpose of this report was to describe our technique for performing an MPFL reconstruction with a concurrent soft-tissue LPFL reconstruction in combination with a distalizing tibial tubercle osteotomy to correct patella alta (Video 1).
Surgical Technique
Positioning and Examination Under Anesthesia
The patient is placed in the supine position, and general anesthesia is induced. Bilateral examination under anesthesia is performed to compare the operative and contralateral knees. Examination of range of motion of the hip and knee as well as patellar stability testing both medially and laterally throughout range of motion is determined. Specifically, the normal knee should be evaluated for eversion and quadrants of media and lateral translation. Assuming this side has been unaffected, this can be used to determine the need for reconstruction on the affected knee. Patients with a history of lateral patellar instability who undergo an LRR and have subsequent medial patellar instability without continued lateral patellar instability may only require an LPFL reconstruction. Patellar eversion is typically 0 to 15° and medial translation 2-3 quadrants with a soft end point in the unaffected knee. The contralateral leg is placed in the lithotomy position with bony prominences padded. The operative leg is secured with a high thigh tourniquet and circumferential leg holder. A leg positioner is attached to the operative side of the bed (Spider; Smith & Nephew, Andover, MA). The operative leg is then prepared and draped in the standard sterile fashion and the foot is secured in the leg holder. An Esmarch is used to exsanguinate the leg and the tourniquet is inflated.
Approach and Diagnostic Arthroscopy
Diagnostic arthroscopy is performed in the standard fashion through the incision via anterolateral and anteromedial portals. The patellofemoral joint is visualized to evaluate the articular morphology and chondral surfaces. Any necessary intra-articular work is performed at this time including debridement, loose body removal, and cartilage repair or restoration. A standard midline anterior approach is used for reconstruction beginning at the proximal patellar pole and extending distally to the distal pole of the patella. This incision may be extended as needed to address concomitant tibial tubercle osteotomy. Full-thickness skin flaps are made medially to the medial patella and laterally to the lateral epicondyle. Importantly, any concomitant tibial tubercle osteotomy is completed at this time before ligament reconstruction to ensure appropriate ligament length relationships.
Graft Preparation
Graft preparation is performed with 2 separate hamstring allografts for both the MPFL and LPFL. The MPFL graft is prepared by tubularizing one end of a semitendinosis graft with a #2 FiberLoop (Arthrex, Naples, FL) and the doubled size is determined (typically 6-7 mm). The LPFL semitendinosis graft is trimmed of any loose tissue and is also tubularized at each end with a #2 FiberLoop.
Medial Patellofemoral Ligament Reconstruction
The superior medial patellar pole is exposed using electrocautery to a depth between the second and third layers of the medial knee. Care is taken not to enter the capsule for appropriate extra-articular graft passage. A small anterior-based flap is raised 2 to 3 mm on the patellar side for later closure. A rongeur is used to partially decorticate the proximal half of the medial patella to improve biologic graft incorporation. Two 3.0-mm PEEK (polyether ether ketone) SutureTak (Arthrex) anchors are placed at the midpoint and superomedial corner of the patella (Fig 1). A soft-tissue tunnel is created between layers 2 and 3 of the medial knee, to allow access to the femoral attachment of the medial patellofemoral complex (Fig 2).
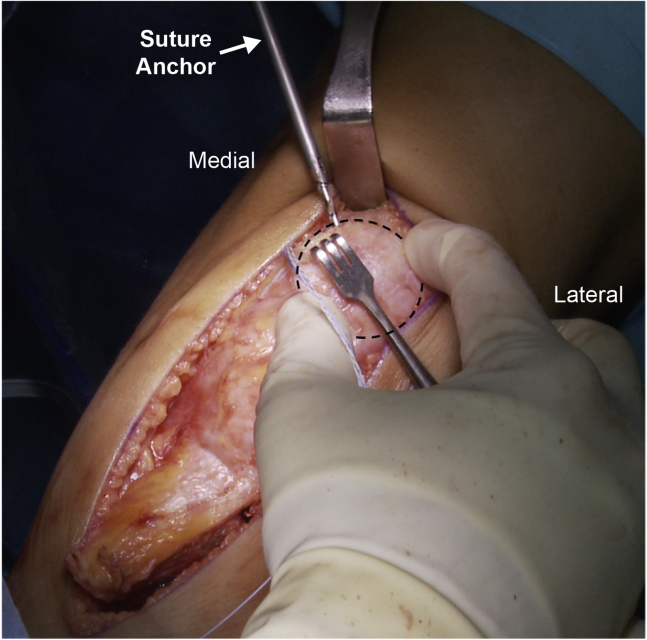
Fig 1.
The patient is placed in the supine position on the operating table. On the left knee, after the superior medial patellar pole is exposed, a rongeur is used to partially decorticate the proximal half of the medial patella and two 3.0-mm PEEK SutureTak anchors are inserted into the medial aspect of the patella. Dotted line indicates the patellar circumference
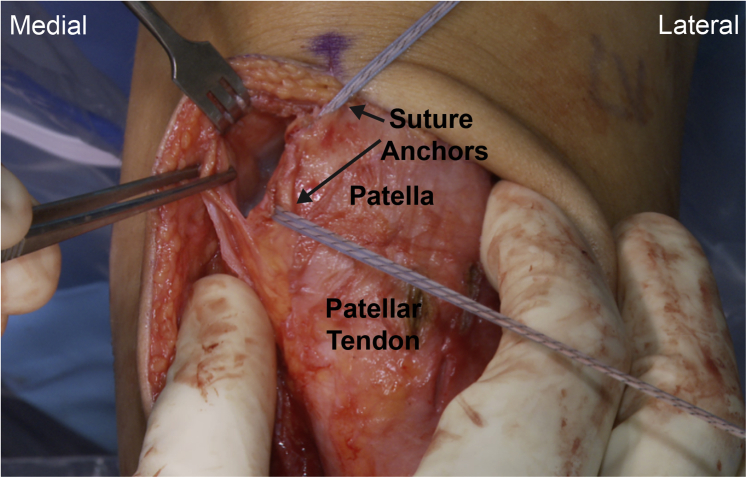
Fig 2.
The patient is placed in the supine position on the operating table. On the medial aspect of the left knee, dissection is performed between layers 2 and 3 to allow for graft passage from the patella to the femur.
A perfect lateral of the knee is obtained using the leg positioner and the femoral tunnel entrance is identified according to the original technique described by Schöttle et al.13 A 3-cm incision is made and dissection is carried down to the medial femur. The plane between layers 2 and 3 determined at the patella is carried deep with blunt dissection and can be connected to the femoral incision near Schöttle’s point. After this dissection is complete, the medial epicondyle and adductor tubercle should then be readily palpable. The guide pin is then placed just posterior to the saddle point between the medial epicondyle and adductor tubercle. This is then checked for its proximity to Schöttle’s point. Between the radiographic location and anatomic landmarks, the most optimal position should be determined based on the specific patient’s anatomy. The guide pin is placed aiming 30° anterior and 30° proximal (Fig 3), and then length changes are tested and can range from being isometric to 5 to 7 mm of loosening with flexion. Ultimately, length changes should trump any radiographic or anatomy-based placement, as the graft cannot tighten in flexion. The femoral tunnel is over-reamed 1 mm larger than the sized graft to the far cortex. The graft is then temporarily placed between layers 2 and 3 and is looped around the pin and the free ends are brought over the anchors on the patella in full extension. The graft is trimmed with at least 25 mm of extra distance on both limbs assuming the femoral tunnel reaming is at least that deep. Making the tunnel size larger than the graft not only allows for easy graft passage but also can limit graft wrapping during screw insertion. The remaining free end of the graft is then prepared with a whip stitch and the middle of the graft is determined. The graft is then doubled, and the looped side is placed on the patella centered between the 2 anchors.
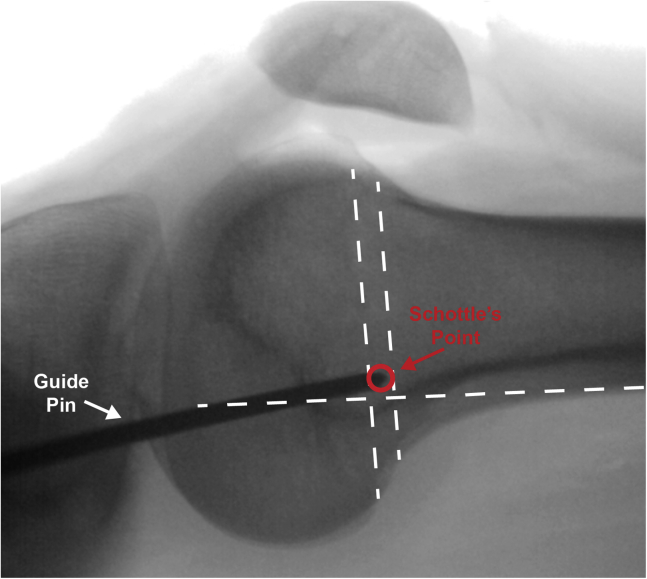
Fig 3.
Perfect lateral radiograph of the left knee of a patient who is placed supine on the operating table. Radiographic identification of the femoral tunnel for the MPFL is based on the technique described by Schöttle et al.13 To identify Schöttle’s point, 3 lines are drawn (white dotted lines): one along the posterior cortex, one intersecting the most posterior aspect of Blumensaat’s line, and one at the intersection of the transition point from the posterior cortex to the medial condyle. (MPFL, medial patellofemoral ligament.)
The graft is secured to the patella using a modified Mason–Allen stitch and placed through the soft-tissue tunnel to the femur. The knee is then brought into full extension and a proximalizing force is placed on the patella, keeping it in line with the trochlear groove. Using a pull-through technique, both free ends of the graft are passed through the femoral tunnel one at a time. The knee is then brought through a full range of motion and after this is complete, appropriate lateral translation is checked, which is typically 1-2A. The graft is then secured in full extension with proximal force on the patella with a 7 × 23-mm PEEK interference screw. The patella should also be stabilized with laterally directed counterpressure on the patella to ensure the graft doesn’t pull into the femur and overtension the reconstruction. Range of motion should then be checked a final time as well as lateral translation in full extension.
Lateral Patellofemoral Ligament Reconstruction
The second gracilis allograft is used for the lateral reconstruction. Medial translation and lateral patellar tilt should be re-evaluated after MPFL reconstruction is complete to determine whether LPFL reconstruction is still necessary. While the contralateral side should be used as a guide, tilt is typically less than 10 to 15° and medial translation 2-3B. Typically, the rent in the lateral retinaculum can be easily visualized and appears as a prominence of the capsule, which a bluish tint. To ensure adequate fixation, the graft should be fixed through tissue adjacent to this. Two small vertical 5- to 7-mm incisions are made through both the quadriceps and patellar tendons at the proximal and distal lateral edges of the patella, respectively. Two counter-incisions are then made through the iliotibial band (ITB) at the lateral epicondyle (Fig 4). The graft is then shuttled with the looped end through the ITB with the distal limb through the patellar incisions (Fig 5) and the proximal limb through the quadriceps incisions (Fig 6). These free ends are then looped back on each other and a temporary VICRYL suture (Ethicon, Somerville, NJ) is placed to check anisometry of the graft throughout knee range of motion. The graft should loosen with flexion and allow for lateral patellar tilt equal to the normal contralateral side. The graft is then sutured with nonabsorbable suture in interrupted figure-of-8 fashion at the ITB, quadriceps, and patellar tendons, and excess graft is removed (Fig 7). Final examination is performed for medial and lateral patellar stability through full knee range of motion. The arthroscope is reintroduced to confirm central patellar tracking and neutral tilt throughout range of motion.
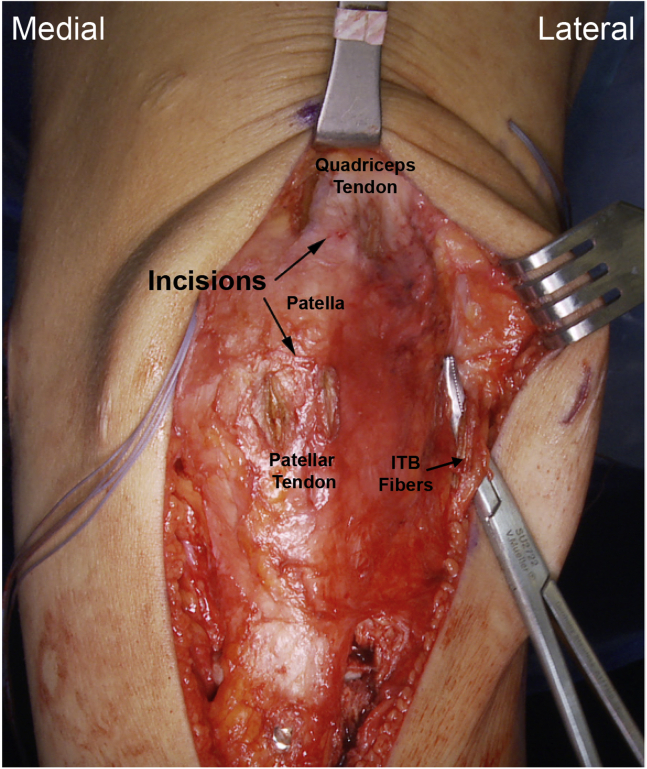
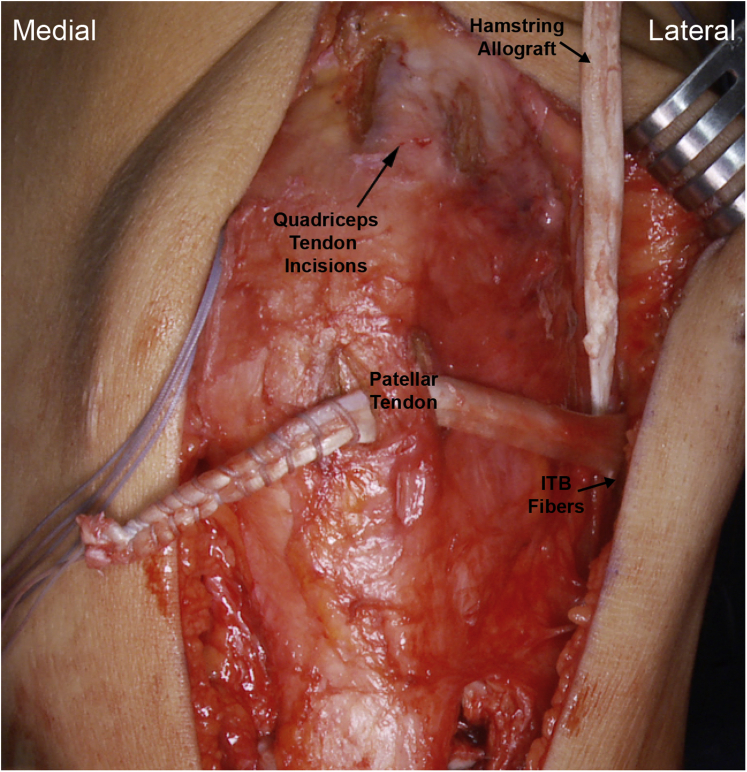
Fig 4.
The patient is placed in the supine position on the operating table. On the left knee, the curved snap shows the two 1-cm incisions that are made in parallel with the ITB fibers in the distal aspect of the ITB at the lateral femoral epicondyle with a 1-cm bridge between the incisions. Also, proximally and distally 2 similar incisions are made through the quadriceps and patellar tendon, respectively. (ITB, iliotibial band.)
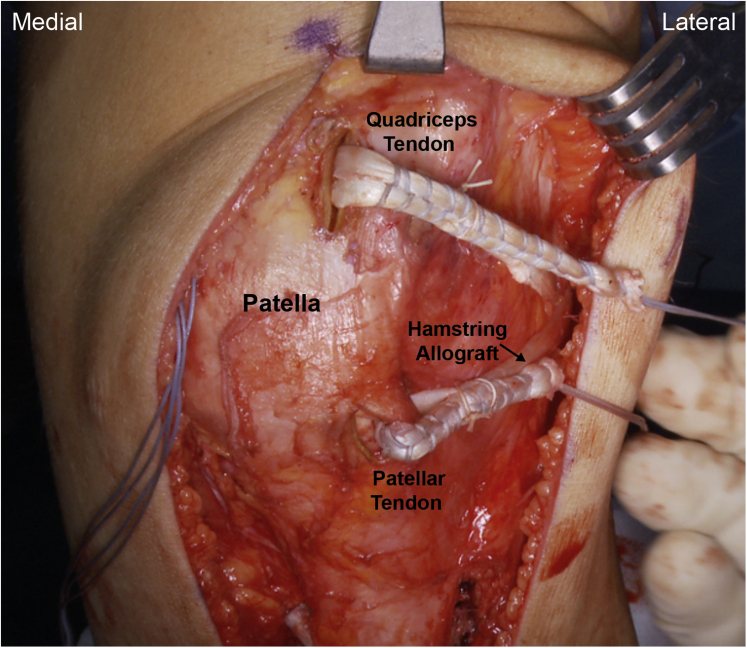
Fig 5.
The patient is placed in the supine position on the operating table. On the left knee, the LPFL graft is passed through the ITB incision and the distal limb is passed through the distal patellar tendon incision and proximal quadriceps tendon incision (arrow). (ITB, iliotibial band; LPFL, lateral patellofemoral ligament.)
Fig 6.
The patient is placed in the supine position on the operating table. On the left knee, the proximal limb of the LPFL graft is placed through the quadriceps incision. Both limbs are then looped back upon themselves to allow for appropriate tensioning of the lateral knee. (LPFL, lateral patellofemoral ligament.)
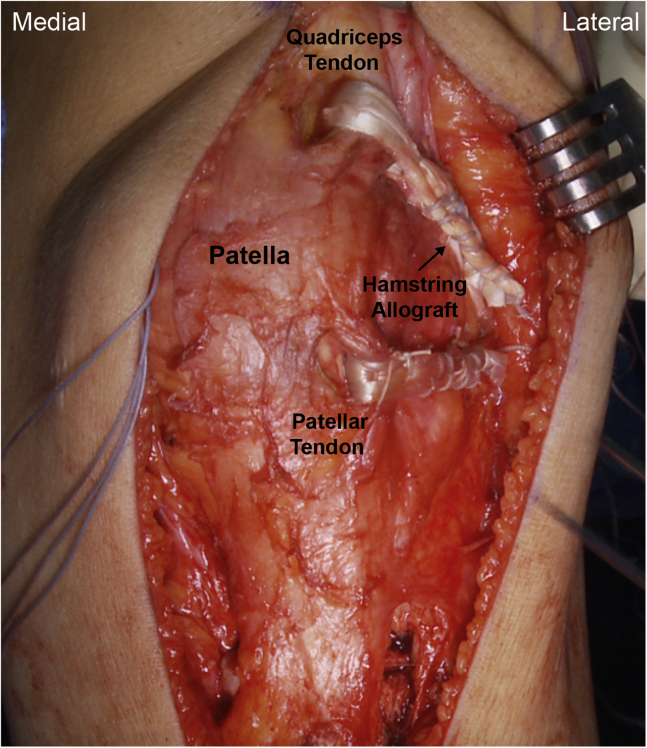
Fig 7.
The patient is placed in the supine position on the operating table. This figure demonstrates the final LPFL graft placement on a left knee. The proximal and distal limbs are tensioned appropriately, held in place, and sutured at the quadriceps, patellar, and ITB loops. (ITB, iliotibial band; LPFL, lateral patellofemoral ligament.)
Closure and Bracing
All incisions are thoroughly irrigated and closed in standard sequential fashion. A 2-0 MONOCRYL (Ethicon) is used to reapproximate the subcutaneous later, and a 3-0 PROLENE running suture (Ethicon) is used to secure the epidermal layer. A standard sterile dressing is applied followed by an ACE wrap for compression. A hinged range of motion brace locked in extension is placed over the knee for initial protection.
Rehabilitation
A standardized rehabilitation protocol is followed addressing bracing, motion, strengthening, stabilization, and function. Without osteotomy, full weight-bearing is allowed immediately with the hinged range of motion brace locked in extension with crutches as needed for support for the first 6 weeks. The patient works on full range of motion immediately after surgery with no restrictions in motion. The brace is discontinued after 6 weeks when a full straight leg raise can be performed independently. Formal physical therapy is started immediately after surgery, with the initial focus on range of motion and core strengthening exercises. Closed chain strengthening is initiated after 6 weeks. Progressive strengthening, stability, and sport-specific exercises are introduced after 3 to 4 months.
Discussion
In patients with combined medial and lateral patellar instability that is refractory to nonoperative management, surgical correction with MPFL and LPFL reconstruction can provide significant functional improvement. A thorough preoperative workup and examination under anesthesia is crucial to allow for a technically successful surgery and optimal outcome. Importantly, any concomitant local (osteochondral), regional (alignment), or systemic (neuromuscular) modifiable risk factors should be addressed along with ligamentous reconstruction. Table 1 provides an overview of technical pearls and pitfalls for combined reconstruction.
Table 1.
Tips, Pearls, Indications, and Pitfalls
Tips and Pearls
|
Indications
|
Pitfalls
|
LPFL, lateral patellofemoral ligament; MPFL, medial patellofemoral ligament.
A number of surgical techniques have previously been described for MPFL reconstruction using different approaches, graft options, tensioning, and fixation.14, 15, 16, 17, 18, 19, 20 As knowledge of the pathology has progressed, MPFL reconstruction has evolved into a reproducible technique, although controversy still exists over the optimal surgical methods. Even with these variations, MPFL reconstruction has been repeatedly validated as a highly successful surgery restoring stability and improving knee function when performed under the correct indications.21,22
In contrast to MPFL reconstruction, few surgical techniques have been published for LPFL reconstruction. Teitge and Spak23 described an early technique using a central quadriceps tendon autograft with a patellar bone block and reported no recurrence but noting 3 of 60 patients sustained patellar fractures, and 2 required subsequent fixation. Saper and Shneider24 reported a similar technique with quadriceps autograft leaving the distal portion attached to the patella in three patients, showing no recurrence at 1 year postoperatively. Borbas et al.25 reported one case in a total knee arthroplasty using a gracilis autograft tunneled through the patella and fixed on the femur with patellar stability 1 year postoperatively. Unfortunately, outcome data were very limited in these studies.
A few retrospective studies have looked at outcomes in LPFL reconstruction. Moatshe et al.10 published a case series of 13 knees using a technique combining autograft lateral patellar tendon and ITB, showing improvement in Lysholm and Western Ontario and McMaster Universities Arthritis Index scores at 2 years postoperatively with a mean satisfaction of 8.2/10. Sanchis-Alfonso et al.8 reported on 17 knees at 18 to 48 months postoperatively using ITB autograft and found similarly improved Lysholm scores and improved psychometrics postoperatively. Beckert et al.9 described yet another technique using a hamstring allograft with suspensory femoral fixation and sutured patellar fixation in 19 knees, showing no postoperative apprehension and improved Knee Injury and Osteoarthritis Outcome Score. Although these early results are promising, further research is needed to determine optimal techniques and evaluate long-term outcomes.
Only 1 previous technique has been published on simultaneous MPFL and LPFL reconstruction. Saper and Shneider reported on 46 knees using a single continuous hamstring allograft spanning from the MPFL origin through the distal aspect of the quadriceps tendon to the LPFL origin.26 They found 95.6% of patients were stable without subluxation at 1 year with no complications, although they reported no other outcome measures. While the stability results are encouraging, there are a number of weaknesses to this technique. As a single nonanatomic continuous reconstruction, the allograft cannot be independently tensioned to optimized patellar centralization throughout range of motion. In addition, the reconstruction effectively tethers the patella inferiorly, which may result in a significant extensor lag. Given these limitations, alternative surgical techniques may have a role in optimizing functional outcomes for patients with combined medial and lateral patellar instability.
The principles of our technique were designed with anatomical reconstruction in mind based on previous evaluations of the MPFL and LPFL. Regarding the MPFL, our patellar attachment sites are analogous to those described by Steensen et al.,27 who found the MPFL spans 38.8% of the patellar length starting an average of 6 mm distal to the superior pole. Our femoral insertion is based on the reproducible radiographic landmarks described by Schöttle et al.,13 and anisometry is confirmed before fixation as described by Bollier et al.16 Regarding the LPFL, our reconstruction restores the strongest aspect of the lateral retinaculum based on anatomic studies.28
There are a number of benefits to this technique that warrant mentioning. Our anatomic MPFL reconstruction technique is based on successful, validated outcome studies.14, 15, 16 Our anatomic LPFL reconstruction technique provides patellar fixation similar to the native LPFL.29 The LPFL graft also avoids osseous tunnels, which are high risk for cortical and articular penetration on the lateral side. Both grafts allow for independent tensioning based on individual anatomy, thus patient-specific stabilization is possible. Based on these benefits, we have confidence this technique will allow for improved patient outcomes, though more robust studies are certainly needed to validate this technique.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.B.Y. reports grants from Arthrex, personal fees from CONMED Linvatec, personal fees from JRF Ortho, personal fees from Olympus, grants from Organogenesis, other from PatientIQ, other from Smith & Nephew, and grants from Vericel, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video is a narrated step-by-step approach to performing a concomitant MPFL and LPFL reconstruction. The MPFL reconstruction is performed first via an osseous based approach with graft fixation with 2 PEEK SutureTak anchors along the medial aspect of the patella and an interference screw in the femur. After this, a soft tissue–based LPFL is performed by making incisions in the iliotibial band, quadriceps tendon, and patellar tendon, looping the graft through these and suturing it down. (LPFL, lateral patellofemoral ligament; MPFL, medial patellofemoral ligament.)
References
- 1.Casteleyn P.P., Handelberg F. Arthroscopy in the diagnosis of occult dislocation of the patella. Acta Orthop Belg. 1989;55:381–383. [PubMed] [Google Scholar]
- 2.Jaquith B.P., Parikh S.N. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthoped. 2017;37:484–490. doi: 10.1097/BPO.0000000000000674. [DOI] [PubMed] [Google Scholar]
- 3.Christensen T.C., Sanders T.L., Pareek A., Mohan R., Dahm D.L., Krych A.J. Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med. 2017;45:2105–2110. doi: 10.1177/0363546517704178. [DOI] [PubMed] [Google Scholar]
- 4.Desio S.M., Burks R.T., Bachus K.N. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 5.Hautamaa P.V., Fithian D.C., Kaufman K.R., Daniel D.M., Pohlmeyer A.M. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;349:174–182. doi: 10.1097/00003086-199804000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Song G.-Y., Hong L., Zhang H., Zhang J., Li Y., Feng H. Iatrogenic medial patellar instability following lateral retinacular release of the knee joint. Knee Surg Sports Traumatol Arthrosc. 2016;24:2825–2830. doi: 10.1007/s00167-015-3522-y. [DOI] [PubMed] [Google Scholar]
- 7.Cancienne J., Christian D., Redondo M., et al. The biomechanical effects of limited lateral retinacular and capsular release on lateral patellar translation at various flexion angles in cadaveric specimens. Arthrosc Sports Med Rehabil. 2019;1:e137–e144. doi: 10.1016/j.asmr.2019.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanchis-Alfonso V., Montesinos-Berry E., Monllau J.C., Merchant A.C. Results of isolated lateral retinacular reconstruction for iatrogenic medial patellar instability. Arthroscopy. 2015;31:422–427. doi: 10.1016/j.arthro.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Beckert M., Crebs D., Nieto M., Gao Y., Albright J. Lateral patellofemoral ligament reconstruction to restore functional capacity in patients previously undergoing lateral retinacular release. World J Clin Cases. 2016;4:202. doi: 10.12998/wjcc.v4.i8.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moatshe G., Cram T.R., Chahla J., Cinque M.E., Godin J.A., LaPrade R.F. Medial patellar instability: Treatment and outcomes. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117699816. 232596711769981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berruto M., Ferrua P., Carimati G., Uboldi F., Gala L. Patellofemoral instability: classification and imaging. Joints. 2013;1:7–14. [PMC free article] [PubMed] [Google Scholar]
- 12.Williams A.A., Elias J.J., Tanaka M.J., et al. The relationship between tibial tuberosity-trochlear groove distance and abnormal patellar tracking in patients with unilateral patellar instability. Arthroscopy. 2015;32:55–61. doi: 10.1016/j.arthro.2015.06.037. [DOI] [PubMed] [Google Scholar]
- 13.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 14.Astur D.C., Gouveia G.B., de Souza Borges J.H., et al. Medial patellofemoral ligament reconstruction: A longitudinal study comparison of 2 techniques with 2 and 5-years follow-up. Open Orthop J. 2015;9:198–203. doi: 10.2174/1874325001509010198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carnesecchi O., Neri T., Iorio A.D., Farizon F., Philippot R. Results of anatomic gracilis MPFL reconstruction with precise tensioning. Knee. 2015;22:580–584. doi: 10.1016/j.knee.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Bollier M., Fulkerson J., Cosgarea A., Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27:1153–1159. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 17.Csintalan R.P., Latt L.D., Fornalski S., Raiszadeh K., Inacio M.C., Fithian D.C. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2013;27:139–146. doi: 10.1055/s-0033-1360652. [DOI] [PubMed] [Google Scholar]
- 18.Feller J.A., Richmond A.K., Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2470–2476. doi: 10.1007/s00167-014-3132-0. [DOI] [PubMed] [Google Scholar]
- 19.Fink C., Veselko M., Herbort M., Hoser C. MPFL reconstruction using a quadriceps tendon graft Part 2: Operative technique and short term clinical results. Knee. 2014;21:1175–1179. doi: 10.1016/j.knee.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Gomes J.E. Comparison between a static and a dynamic technique for medial patellofemoral ligament reconstruction. Arthroscopy. 2008;24:430–435. doi: 10.1016/j.arthro.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Schneider D.K., Grawe B., Magnussen R.A., et al. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations. Am J Sports Med. 2016;44:2993–3005. doi: 10.1177/0363546515624673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weber A.E., Nathani A., Dines J.S., et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98:417–427. doi: 10.2106/JBJS.O.00354. [DOI] [PubMed] [Google Scholar]
- 23.Teitge R.A., Spak R.T. Lateral patellofemoral ligament reconstruction. Arthroscopy. 2004;20:998–1002. doi: 10.1016/j.arthro.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Saper M.G., Shneider D.A. Lateral patellofemoral ligament reconstruction using a quadriceps tendon graft. Arthrosc Tech. 2014;3:e445–e448. doi: 10.1016/j.eats.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borbas P., Koch P.P., Fucentese S.F. Lateral patellofemoral ligament reconstruction using a free gracilis autograft. Orthopedics. 2014;37:e665–e668. doi: 10.3928/01477447-20140626-66. [DOI] [PubMed] [Google Scholar]
- 26.Saper M.G., Shneider D.A. Simultaneous Medial and Lateral Patellofemoral Ligament Reconstruction for Combined Medial and Lateral Patellar Subluxation. Arthrosc Tech. 2014;3(2):e227–e231. doi: 10.1016/j.eats.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steensen R.N., Dopirak R.M., McDonald W.G. The anatomy and isometry of the medial patellofemoral ligament. Am J Sports Med. 2004;32:1509–1513. doi: 10.1177/0363546503261505. [DOI] [PubMed] [Google Scholar]
- 28.Merican A.M., Sanghavi S., Iranpour F., Amis A.A. The structural properties of the lateral retinaculum and capsular complex of the knee. J Biomech. 2009;42:2323–2329. doi: 10.1016/j.jbiomech.2009.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Capkin S., Zeybek G., Ergur I., Kosay C., Kiray A. An anatomic study of the lateral patellofemoral ligament. Acta Orthop Traumatol Turc. 2017;51:73–76. doi: 10.1016/j.aott.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video is a narrated step-by-step approach to performing a concomitant MPFL and LPFL reconstruction. The MPFL reconstruction is performed first via an osseous based approach with graft fixation with 2 PEEK SutureTak anchors along the medial aspect of the patella and an interference screw in the femur. After this, a soft tissue–based LPFL is performed by making incisions in the iliotibial band, quadriceps tendon, and patellar tendon, looping the graft through these and suturing it down. (LPFL, lateral patellofemoral ligament; MPFL, medial patellofemoral ligament.)
This video is a narrated step-by-step approach to performing a concomitant MPFL and LPFL reconstruction. The MPFL reconstruction is performed first via an osseous based approach with graft fixation with 2 PEEK SutureTak anchors along the medial aspect of the patella and an interference screw in the femur. After this, a soft tissue–based LPFL is performed by making incisions in the iliotibial band, quadriceps tendon, and patellar tendon, looping the graft through these and suturing it down. (LPFL, lateral patellofemoral ligament; MPFL, medial patellofemoral ligament.)